Musculoskeletal Radiography
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Musculoskeletal Radiography
Musculoskeletal Radiography
William W. Scott Jr MD
Description
-
Plain radiography has been the primary musculoskeletal imaging technique for >100 years (1).
-
X-ray beams generated by an x-ray tube
pass through the body part to be imaged, and differential absorption
and scattering of the x-ray beams occur. -
The exiting beam carries information about the density of the material traversed.
-
This information is captured by:
-
Film (almost always with intensifying screens to reduce radiation dose to the patient) or
-
Another receptor system such as CR or DR,
in which the x-ray energy is converted into electrical energy in a
pattern reflecting the x-ray absorption of the traversed structure.
-
-
The advantages of digital images such as those produced by CR and DR or by digitizing conventional film images are:
-
They can be transmitted easily and stored electronically.
-
Multiple individuals at multiple locations can view the images simultaneously.
-
The problem of “lost” or misplaced films is lessened.
-
Signs and Symptoms
History
-
The specific reason for obtaining the
imaging study and the coexistence of other important illnesses are
important factors in the interpretation of imaging studies.-
This information must be provided to the
radiologist interpreting the studies to maximize the possibility of a
correct diagnosis. -
Providing this information also has become a legal requirement in studies of Medicare and Medicaid patients.
-
-
The best practice is for the radiologist to interpret the images 1st without the history and then again with the history.
Physical Exam
-
In musculoskeletal imaging, the exact
site of point tenderness is often the most important facet of the
clinical information in fracture detection and may help with other
types of abnormalities as well. -
Soft-tissue masses easily palpated on physical examination may not be seen on plain radiographs.
-
Absence on radiographs does not mean masses do not exist.
-
MRI should be obtained for suspected soft-tissue masses if additional imaging is necessary.
-
Diagnostic Procedures/Surgery
-
Cautions
-
1 view is almost always unsatisfactory.
-
Injured patients may have difficulty moving as requested.
-
Be certain that orthogonal projections were obtained.
-
-
Complex body parts such as the pelvis, especially when obscured by bowel content, often require CT for satisfactory imaging.
-
-
Sequences
-
For suspected fractures, dislocations, congenital bone abnormalities:
-
Imaging of bony structures is done with
relatively low kilovoltage (compared with that used for chest
radiography) to provide better contrast between bone and soft tissue. -
Long bones (femur, tibia and fibula,
radius, and ulna, etc.) require 2 radiographs at 90° to one another
(orthogonal projections). -
Joints should be imaged in 3 projections (frontal, lateral, and oblique).
-
-
For suspected bone tumor:
-
Orthogonal plain radiographs usually provide the diagnosis.
-
MRI provides detailed information on extent of lesion and involvement of neighboring structures.
-
CT may best show calcified tumor matrix.
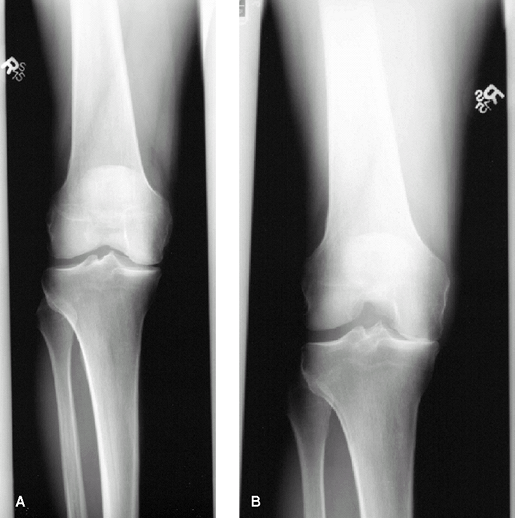 Fig. 1. Patient with chronic knee pain believed to be secondary to osteoarthritis. A: Standing AP view does not show substantial medial compartment narrowing. B: Standing posterior flexed view shows marked medial compartment narrowing and articular cartilage loss.
Fig. 1. Patient with chronic knee pain believed to be secondary to osteoarthritis. A: Standing AP view does not show substantial medial compartment narrowing. B: Standing posterior flexed view shows marked medial compartment narrowing and articular cartilage loss.
-
-
For suspected soft-tissue tumor:
-
Orthogonal radiographs show calcification within the lesion (if present) and effects on neighboring bony structures.
-
Large, fatty lesions may be identified on
orthogonal radiographs, but MRI is far better for lesion
characterization (except for calcification). -
MRI also shows the relation of lesion to surrounding structures.
-
-
For suspected osteomyelitis:
-
Orthogonal radiographs that show definite
bone destruction, sequestrum formation, or periosteal reaction without
other explanation in the appropriate clinical setting are relatively
specific for osteomyelitis, although not sensitive. -
MRI and radionuclide bone scans provide better sensitivity.
-
-
For suspected arthritis:
-
3 views (frontal, lateral, and oblique) of the symptomatic hand and wrist are helpful.
-
Plain radiographic examination can show
cartilage narrowing, erosions, osteophytes, soft-tissue calcifications,
and pattern of joint involvement and frequently can identify the cause
of the arthritis. -
In long-standing knee arthritis, decision
about the appropriate intervention is aided by standing posteroanterior
radiographs with the knees flexed 28°, the position in which cartilage
wear usually is most marked (Fig. 1).
-
-
For suspected osteonecrosis:
-
Plain radiographs of the hips should
include frontal and lateral views; frequently, deformity of the
articular surface of the femoral head is better seen on the lateral
view. -
MRI is the most sensitive imaging study
for early detection of AVN, but plain radiographs, when positive, are
quite specific for the diagnosis. -
When articular surface collapse is shown,
the joint will eventually need prosthetic replacement, so the expense
of MRI can be avoided.
-
P.269 -
-
A fat-fluid level in a joint after trauma
is a strong indication of the presence of intra-articular fracture, and
identification or documentation of a fracture should be pursued
aggressively.-
This situation most commonly involves the knee.
-
If frontal and lateral views are negative, obtain oblique views.
-
If oblique views are negative, obtain a CT scan.
-
Joint effusion in the elbow after trauma,
as indicated by a positive “fat pad” sign, is highly correlated with
the presence of fracture, especially in adult patients (2). -
Follow-up imaging after 10–14 days of treatment is advised.
-
-
Suspected scaphoid fracture with initial negative radiographs should be reimaged after 10–14 days of treatment.
-
For rare circumstances in which 10–14
days of treatment causes logistic difficulty, as for the professional
athlete, an MRI scan can provide an immediate answer at greater expense. -
For a suspected hip fracture, especially
in elderly individuals, negative plain radiographs and even negative CT
cannot rule out the possibility of fracture.-
Only a negative MRI exam can exclude the possibility of fracture immediately postinjury.
-
Although MRI is expensive, overall care
may cost less because the patient will not have to be kept
nonweightbearing for a prolonged period.
-
Pediatric Considerations
-
Ionizing radiation used in imaging has
the potential to cause tumors, an especially important consideration in
pediatric patients. -
Effort should be made to use the least
radiation and number of exposures consistent with obtaining the
necessary diagnostic information. -
Most experienced pediatric radiologists
only rarely obtain comparison views of the contralateral extremity in
cases of suspected fracture. -
Scoliosis views can be obtained in the
posteroanterior rather than the AP projection to limit radiation
exposure to the breast in young female patients who may need multiple
follow-up studies. -
To limit the radiation dose to tiny
pediatric patients, CT scans can be performed with exposure factors
different than those used in adults.
Pregnancy Considerations
-
Female patients should always be questioned directly about the possibility of pregnancy.
-
Radiation to the pregnant patient, especially during the 1st trimester, can cause fetal abnormalities (3).
-
Exposure of the developing fetus to the
direct x-ray beam is the most damaging, so exposures of the pelvic
region should be limited as much as possible (3). -
Extremity examinations usually pose little hazard to the fetus.
-
Studies sometimes can be delayed without compromising care.
-
Alternative studies, such as MRI and ultrasound, should be considered if they can provide the needed information.
-
Should a pregnant patient receive a
number of examinations to the pelvic region (lumbar spine, multiple
views of pelvis, CT, etc.), a medical physicist should be consulted.-
The radiation dose to the fetus can be estimated, and appropriate counseling can be given to the patient.
-
References
1. Kotzur IM. W. C. Rontgen: a new type of ray. Radiology 1994;193:329–332.
2. O’Dwyer
H, O’Sullivan P, Fitzgerald D, et al. The fat pad sign following elbow
trauma in adults: its usefulness and reliability in suspecting occult
fracture. J Comput Assist Tomogr 2004;28: 562–565.
H, O’Sullivan P, Fitzgerald D, et al. The fat pad sign following elbow
trauma in adults: its usefulness and reliability in suspecting occult
fracture. J Comput Assist Tomogr 2004;28: 562–565.
3. Janower ML, Linton OW, eds. Radiation Risk: A Prime. Reston, VA: American College of Radiology, 1996.
FAQ
Q: What is the most important piece of clinical information in the evaluation of bony structures for possible trauma?
A: The location of point tenderness indicates where to examine the images most carefully.
Q: When should one obtain flexed posteroanterior standing views of the knees?
A:
These views are always valuable in patients with relatively severe
disease to show “bone on bone” narrowing, which indicates that
arthroscopy is unlikely to be of benefit. Patients with severe symptoms
that do not correlate with the apparent degree of joint cartilage
narrowing on AP standing views are also likely to benefit from the
flexed posteroanterior standing views.
These views are always valuable in patients with relatively severe
disease to show “bone on bone” narrowing, which indicates that
arthroscopy is unlikely to be of benefit. Patients with severe symptoms
that do not correlate with the apparent degree of joint cartilage
narrowing on AP standing views are also likely to benefit from the
flexed posteroanterior standing views.
Q: Will CT “rule out” a hip fracture?
A:
No. There is a temptation to use CT to look for hip fractures in
elderly fall victims. However, if CT shows a fracture, it is
diagnostic, but a negative CT does not exclude fracture. MRI should be
obtained to exclude fracture.
No. There is a temptation to use CT to look for hip fractures in
elderly fall victims. However, if CT shows a fracture, it is
diagnostic, but a negative CT does not exclude fracture. MRI should be
obtained to exclude fracture.
Q: What imaging modality is most specific for diagnosing the specific types of bone neoplasm?
A:
Plain radiographs should always be obtained when evaluating a possible
bone neoplasm because they are the most specific for identifying the
type of tumor.
Plain radiographs should always be obtained when evaluating a possible
bone neoplasm because they are the most specific for identifying the
type of tumor.
