Upper Extremity Landmarks
-
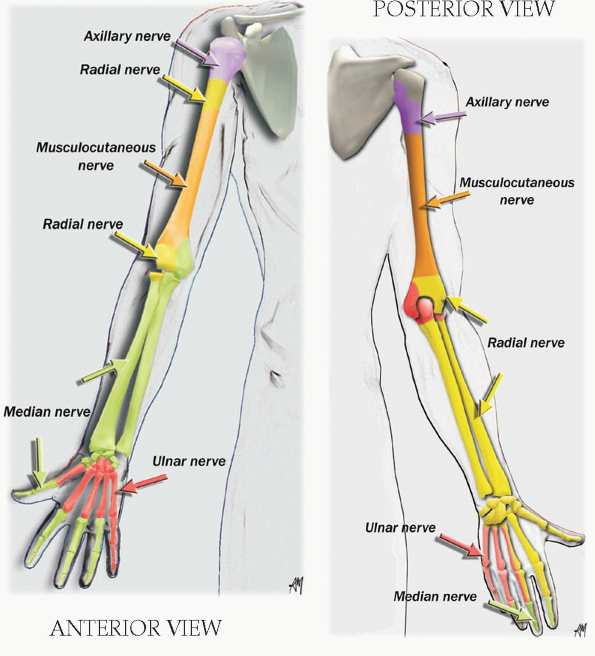
Formed from anterior primary rami of C5-T1.
-
5 roots, 3 trunks, 3 cords, 5 nerves.
-
3 trunks: upper (C5, C6), middle (C7),
and lower (C8, T1) in the interscalene space, anterior to scalenus
medius and posterior to scalenus anterior. -
The trunks pass over the lateral border
of the first rib and under the clavicle; each trunk (superior, middle,
and inferior) divides into anterior and posterior branches. The
branches reunite to form cords. -
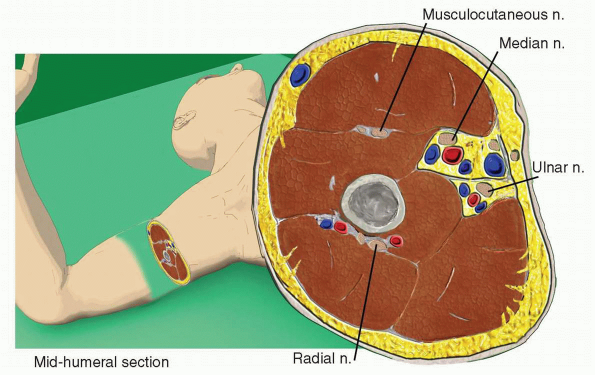
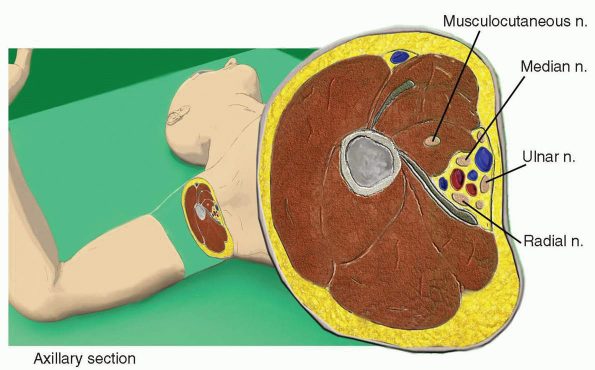
3 cords around the axillary artery:
-
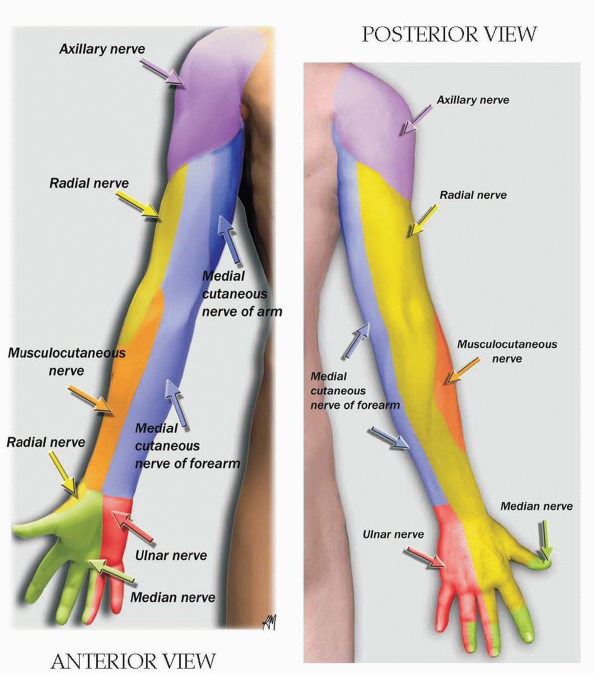
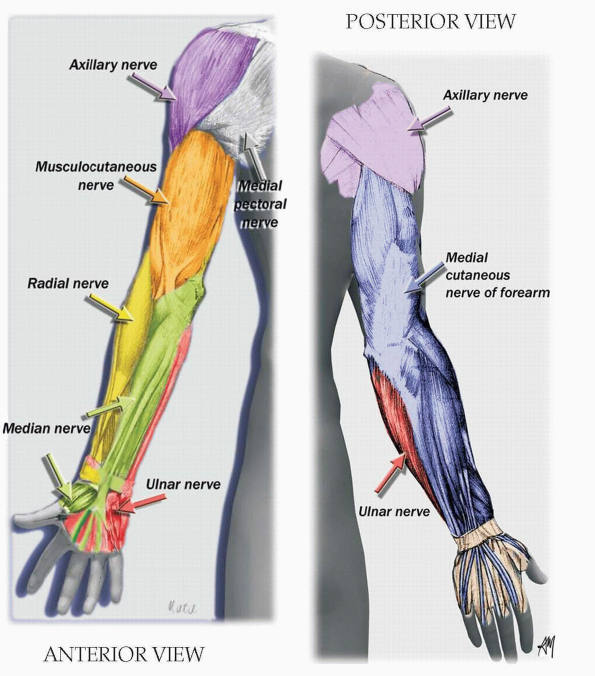
Lateral cord: lateral portion of the median nerve and musculocutaneous nerve.
-
Medial cord: medial portion of the median
nerve, ulnar nerve, medial cutaneous nerve of the forearm, and medial
cutaneous nerve of the arm. -
Posterior cord: axillary and radial nerves.
-
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
The contraction of the supinator and brachioradialis muscles innervated by the radial gives a flexion and supination of the forearm. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
-
Elbow joint innervation = radial, median, and ulnar.
-
Wrist joint innervation = radial (posterior interosseous), median, and ulnar (deep terminal branch).
-
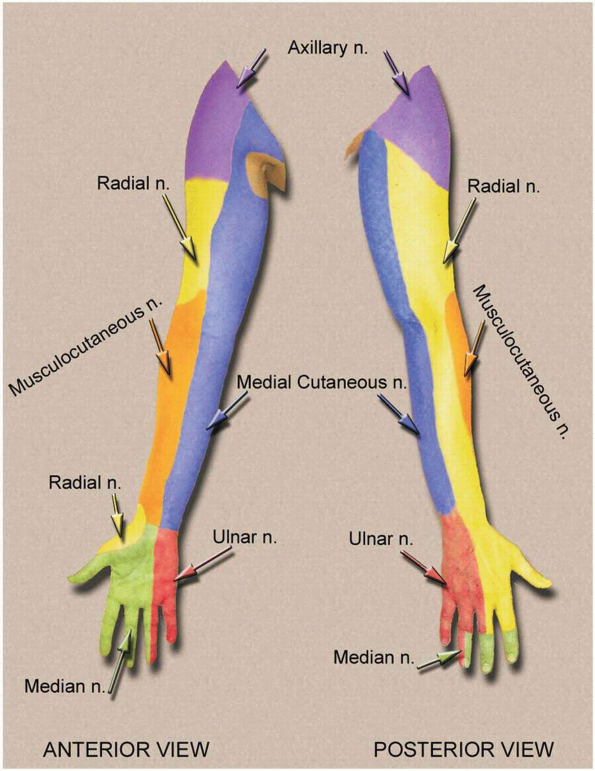
Medial cutaneous nerve of arm and forearm arise from the medial cord (C8-T1 roots).
 |
|
UPPER EXTREMITY: DERMATOMES
|
-
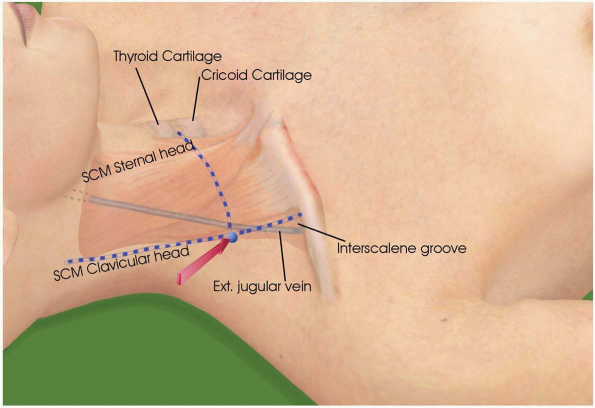
Line along the lateral border of the clavicular head of the sternocleidomastoid muscle (SCM).
-
Line between the thyroid and cricoid cartilages (C5-C6).
-
Intersection of these 2 lines.
-
1- or 2-inch needle.
-
The clavicular head of the SCM is easily identified by asking the patient to lift up his or her head.
-
Needle is directed caudal, posterior, and medial with a 45-degree angle.
-
If the needle tip is inserted too posterior, a contraction
of the levator scapulae muscle by stimulation of the dorsal scapular
nerve can be confused with a deltoid contraction. Placing one hand over
the scapula can make a differential. -
Contraction of the diaphragm
by stimulation of the phrenic n., which runs over the lateral border of
scalenus anterior m. behind the prevertebral fascia, means that the
needle tip is inserted too anteriorly. -
The roots C8 and T1 (median and ulnar nerves) are partially blocked or not blocked with this approach.
-
A catheter can be inserted for a continuous interscalene block.
-
Side effects: Horner’s syndrome (stellate ganglion
![image]() block), hoarse voice (recurrent laryngeal nerve), 100% ipsilateral paralysis of the diaphragm (phrenic nerve).
block), hoarse voice (recurrent laryngeal nerve), 100% ipsilateral paralysis of the diaphragm (phrenic nerve). -
Can occur:
 |
|
INTERSCALENE APPROACH
|
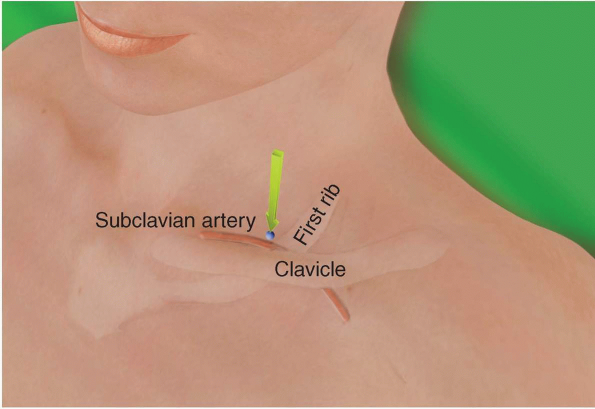
-
Line along the lateral border of the clavicular head of the SCM.
-
Line along the clavicle.
-
Intersection of these two lines.
-
Subclavian artery in the supraclavicular fossa.
-
2-inch needle (plexus is located at a depth of 2 to 4 cm).
-
Point of needle insertion is posterior and lateral to the subclavian artery.
-
Position of needle is parallel to the neck and directed toward the first rib.
-
Point of needle insertion is posterior and lateral to the SCM at its insertion on the clavicle.
-
Position of needle is perpendicular to the neck and directed with a 30-degree angle in the caudal direction.
-
Nerve stimulation resulting in movements of the hand is essential (radial, median, or ulnar).
-
A contraction of the arm muscles is not sufficient.
-
Can occur: pneumothorax, if needle is directed too medial and too posterior.
 |
|
SUPRACLAVICULAR APPROACH
|
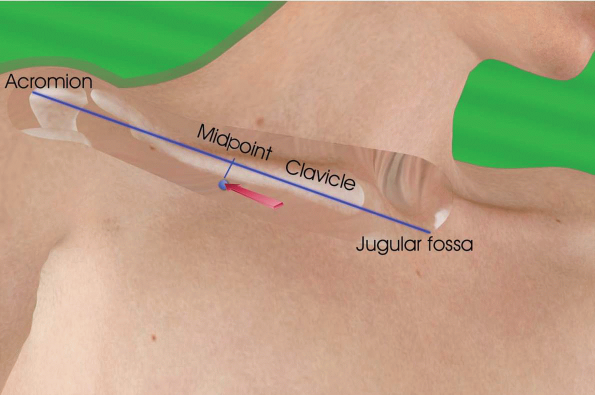
-
Midpoint of a line between ventral border of acromion of the scapula (lateral landmark) and fossa jugularis (medial landmark).
-
Just below or 1 cm caudal to the clavicle.
-
Strictly vertical to the supine position of the patient.
-
Can occur: pneumothorax, if needle directed too medial and deeper than 6 cm.
 |
|
VERTICAL INFRACLAVICULAR APPROACH
|
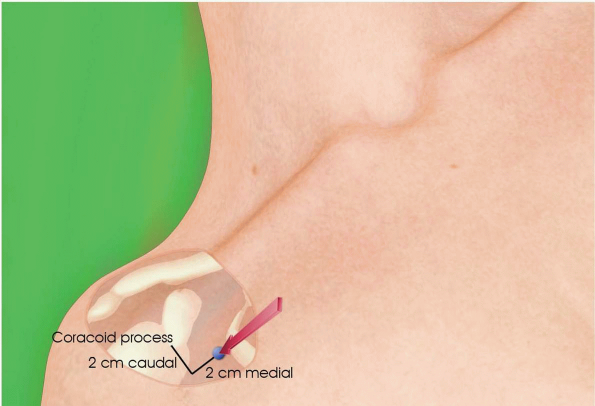
-
Ventral border of the coracoid process (fingertip on the tip of the coracoid process).
-
2 cm caudal and 2 cm medial, needle perpendicular to the skin or directed slightly cephalad.
-
2- to 4-inch needle (4- to 6-cm depth depending on the needle’s angle).
-
Obtaining a movement of the hand is essential (radial, median, or ulnar).
-
A musculocutaneous stimulation (biceps
contraction) indicates an approach of the lateral part of the plexus
(lateral cord). The needle must be directed more medially to obtain a
median stimulation and posteriorly to obtain a radial stimulation
(posterior cord). -
A multistimulation technique (lateral and posterior cord) increases the success rate of this block.
-
A catheter can be inserted for a continuous infraclavicular block.
 |
|
PARACORACOID APPROACH
|
-
Lateral border of the pectoralis major.
-
Axillary crease.
-
Brachial artery.
-
Brachial artery is palpated high in the axilla crease.
-
The needle is inserted directly above the
artery, pointing almost parallel to the artery in a proximal direction
with a 30- to 45-degree angle to the skin. A median, ulnar, or radial
stimulation is elicited. (Do not accept a musculocutaneous stimulation.) -
A separate injection for the musculocutaneous nerve (see below) is advised.
-
Slow and fragmented injection of the total dose of the local anesthetic solution with frequent aspiration.
-
The needle is inserted directly above the
artery, pointing to the artery in a proximal and medial direction at a
30- to 45-degree angle to the skin. A median stimulation is elicited
(15 mL of local anesthetic). -
Above the artery and anterior into the
coracobrachialis muscle a musculocutaneous stimulation is elicited (5
mL of local anesthetic). -
Then the needle is inserted directly
below the artery, pointing to the artery in a proximal and lateral
direction at a 30- to 45-degree angle to the skin. A radial or ulnar
(more superficial) stimulation is elicited (15 mL of local anesthetic). -
Anterior and posterior subcutaneous ring infiltration on the inner aspect of the axilla for the cutaneous nerves of the arm.
 |
|
AXILLARY APPROACH
|
-
Large nerve, very superficial, can be felt under the skin.
-
To avoid penetrating the nerve, the needle is inserted parallel to the skin and then redirected more perpendicularly.
-
A “pop” can be felt when the needle penetrates the common sheath between the humeral artery and median nerve.
-
6 to 8 mL of local anesthetic solution.
-
A catheter can be inserted for a continuous brachial plexus block.
-
Deeper (1 to 2 cm) into the coracobrachialis muscle just above the median nerve (n.).
-
Small nerve, easily blocked; 4 to 5 mL of local anesthetic is usually adequate.
-
Needle angled 45 degrees posterior.
-
1 to 2 cm deep.
-
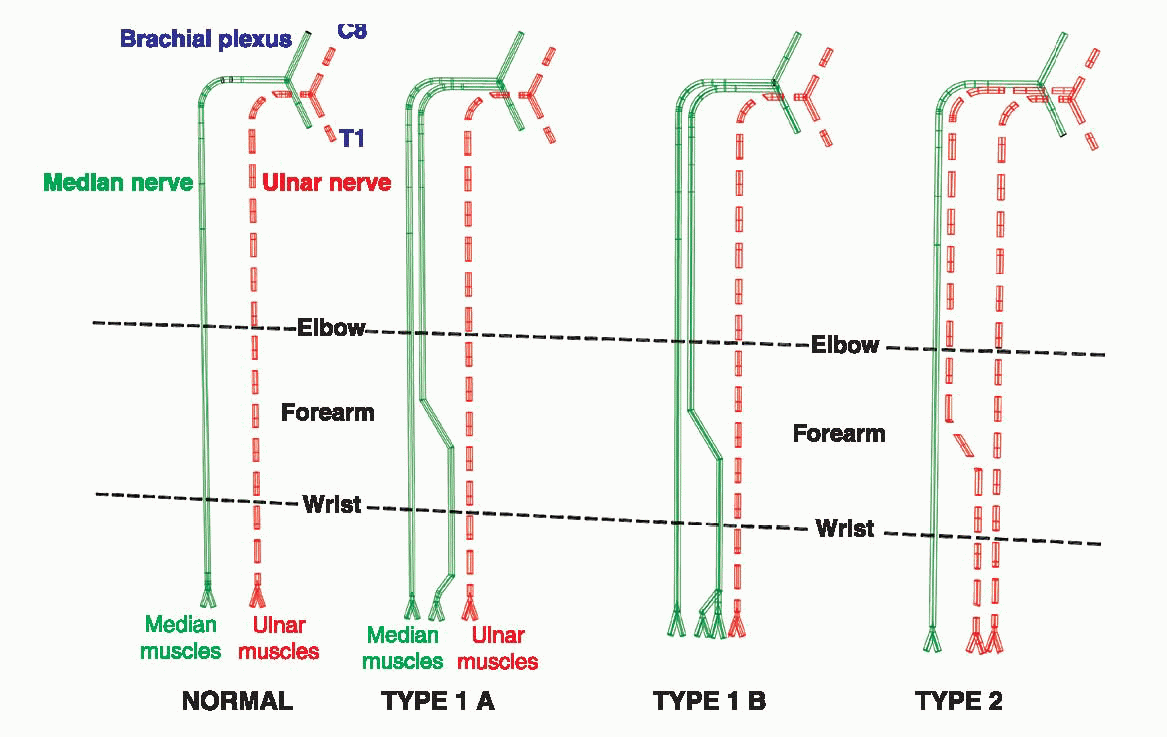
Possible Martin and Gruber anastomosis.
-
At the same level as the ulnar n.
-
Needle redirected perpendicular to the skin.
-
Nerve is posterior to the humerus (bone contact), 5 to 10 mm deeper.
-
Sometimes the nerve can be reached only
by doing a slow external rotation of the arm or a more posterior
insertion of the needle.
-
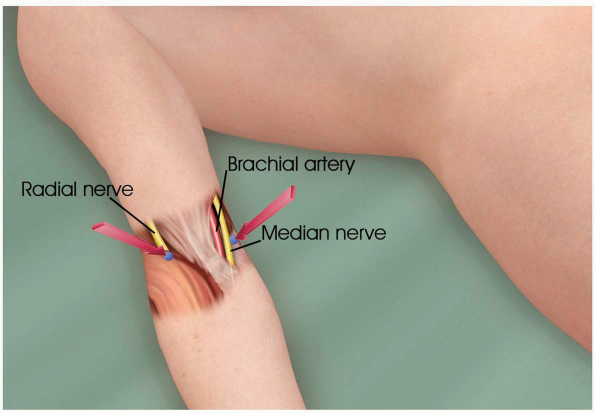
Elbow flexion crease.
-
Medial to the brachial artery and biceps tendon.
-
Tip of the index finger against the
medial side of the biceps tendon, above the brachial artery. Needle is
inserted medial to the fingertip perpendicular to the skin.Nerve will be located at 1 to 2 cm depth. -
Motor response similar to above.
-
Elbow flexion crease.
-
Intercondylar fold.
-
1 cm lateral to the biceps tendon.
-
Tip of the index finger against the lateral side of the biceps tendon.Needle is inserted lateral to the fingertip perpendicular to the skin.
-
An extension and supination of the
forearm will occur when the deep radial branch is stimulated. The deep
radial branch innervates the forearm musculature and the posterior part
of carpal bones.
 |
|
RADIAL AND MEDIAN AT THE ELBOW
|
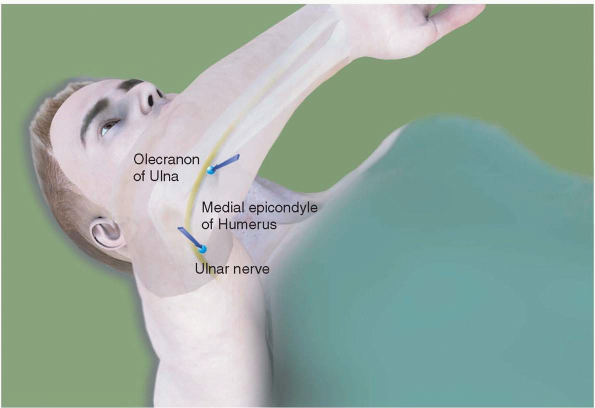
-
Ulnar groove.
-
With the elbow flexed, the needle is
introduced at the apex of a triangle, with the line from the medial
epicondyle to the olecranon process as a base.
-
DO NOT inject between the medial epicondyle of the humerus and the olecranon process.
-
Motor response similar to above.
 |
|
ULNAR AT THE ELBOW
|
-
Below the elbow, the musculocutaneous n.
emerges lateral to the tendon of the biceps and descends over the
lateral aspect of forearm (lateral cutaneous n. of the forearm). At
this level it is a purely sensory nerve. -
Subcutaneous infiltration at the level of the elbow crease, under the cephalic vein, from the biceps tendon to the radial head.
-
Neurostimulation (1 msec): elicits a paresthesia in the musculocutaneous territory.
-
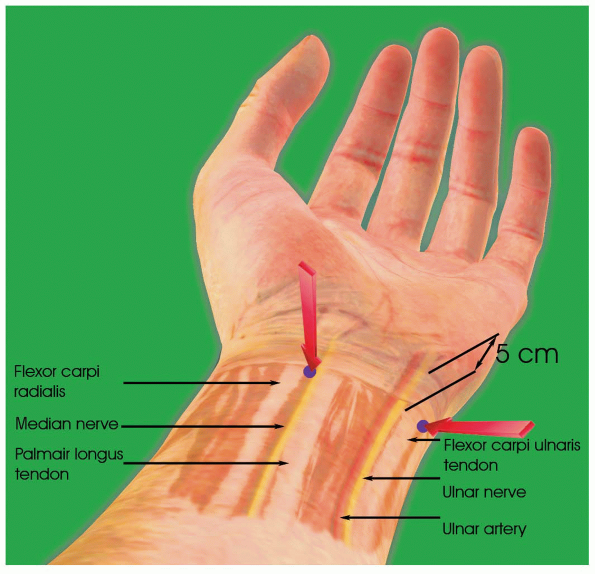
Lateral to the palmaris longus tendon.
-
Medial to the flexor carpi radialis tendon.
-
Insertion of the needle 5 to 6 cm above the wrist flexion crease.Proximal to the wrist flexion crease, the median n. gives off a palmar cutaneous branch (lateral palmar skin).
-
Median at the wrist is 70% to 80% sensory (anterior) and 20% to 30% motor (posterior). A needle inserted perpendicular to the skin can elicit paresthesia without motor nerve stimulation. Nerve stimulation at 1 msec is used to elicit paraesthesia.
-
Motor response = translation of the thumb.
-
Insert needle perpendicular to the skin, below the carpi ulnaris tendon and 4 to 5 cm above the wrist flexion crease.
-
Same motor response as above.
-
Interosseous or hypothenor eminence muscles contraction.
-
Absence of adduction of the wrist (ulnar inclination of the wrist).
 |
|
MEDIAN AND ULNAR AT THE WRIST
|
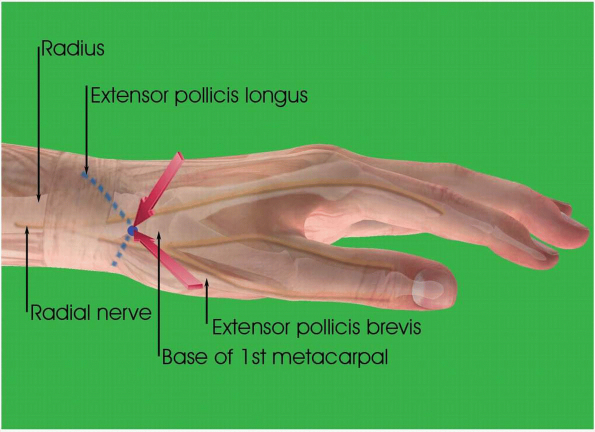
-
Subcutaneous infiltration anteriorly and posteriorly at the level of the radial styloid.
-
Below the wrist, the radial nerve is purely sensory.
 |
|
RADIAL AT THE WRIST
|
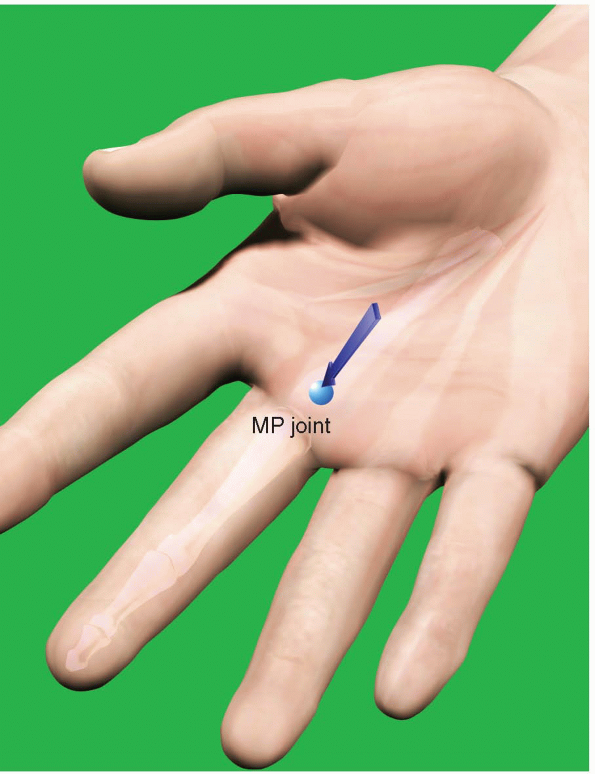
-
Metacarpophalangeal (MP) joint of the third digit.
-
Flexor tendon.
-
Surgical block for 2nd, 3rd, and 4th fingers.
-
Subcutaneous needle, bevel anterior.
-
45 degrees to the skin until the flexor tendon is reached.
-
A passive flexion of the third finger brings the needle into a vertical position.
-
The needle is slowly withdrawn. The contact with the tendon is lost but the needle is still in the sheath.
-
5 to 8 mL of local anesthetic solution.
-
No epinephrine.
 |
|
FLEXOR DIGITORUM SHEATH BLOCK
|