Tibial Plafond Fracture
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Tibial Plafond Fracture
Tibial Plafond Fracture
Jason W. Hammond MD
Peter R. Jay MD
Description
-
Tibial plafond (or pilon) fractures, a
subset of ankle fractures, are intra-articular fractures of the distal
tibia involving varying degrees of articular and metaphyseal injury (Fig. 1).-
The word “pilon” comes from the French
root meaning “pestle” or “rammer,” conveying the idea that the talus
drives into the tibial articular surface. -
The distal tibia also is known as the plafond (roof) over the talus; thus, these fractures also are called “plafond fractures.”
-
-
These high-energy, often-devastating injuries:
-
Often are associated with marked soft-tissue injury
-
Can be associated with substantial neurovascular compromise
-
Can be associated with other lower extremity, spinal, pelvic, abdominal, thoracic, or cranial injuries
-
Are associated with the population at risk for high-level trauma (i.e., young males)
-
-
Practitioners should be even more
vigilant about open injuries and vascular or tissue compromise in
elderly or debilitated patients. -
Multiple classification systems exist, but the Ruedi and Allgower (1) system is the most commonly used:
-
Type I: Nondisplaced or minimally displaced intra-articular fracture
-
Type II: Displaced intra-articular fracture with minimal comminution
-
Type III: Displaced fracture with marked comminution
-
-
The Ruedi and Allgower (1) classification system has clinical and prognostic implications:
-
Type I can be treated with splint or cast immobilization; good prognosis
-
Types II and III require surgical intervention; associated with a more guarded prognosis
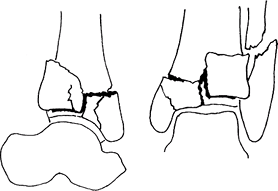 Fig. 1. Tibial plafond fracture.
Fig. 1. Tibial plafond fracture.
-
Epidemiology
Incidence
-
These rare injuries are associated with high-energy trauma.
-
Anecdotally, the incidence has been increasing with the advent of the automobile airbag.
Risk Factors
-
Individuals at risk for high-level trauma (e.g., young males, alcohol abuse, drug use)
-
Individuals who work at heights
Etiology
-
High-energy injuries:
-
Motor vehicle accident
-
Fall from height
-
High-energy axial loading is the common denominator.
-
-
Some low-energy (e.g., skiing) injuries
Associated Conditions
Patients are at high risk for associated pelvic, spinal, abdominal, thoracic, or cranial injuries.
Signs and Symptoms
History
-
Severe pain
-
Swelling
-
Inability to bear weight
Physical Exam
-
1st, perform a complete trauma assessment
with a primary survey of airway, breathing, circulation and then a
secondary survey of the head, neck, chest, abdomen, spine, pelvis, and
all extremities per the ATLS protocol (2). -
Evaluate soft-tissue status, including swelling, fracture blisters, open fracture.
-
Perform a careful neurovascular examination.
-
Monitor for compartment syndrome.
-
Use the wrinkle test: Swelling is decreased and ready for surgery when the skin wrinkles with pinching.
Tests
Lab
-
Order appropriate tests for the level of injury:
-
Hematocrit
-
Type and cross-match
-
Urine and stool check for blood, as indicated
-
All preoperative laboratory tests necessary for age group, level of injury, and institution
-
Imaging
-
Plain radiographs:
-
AP, lateral, and mortise views of the ankle
-
AP and lateral views of the foot
-
Tibia-fibula
-
Some surgeons find that radiographs of the opposite extremity assist in reconstruction in severe cases.
-
-
If displacement or comminution is present, a CT scan can be helpful for surgical planning.
Differential Diagnosis
-
Ankle fracture
-
Talus fracture
-
Tibial shaft fracture
-
Calcaneus fracture
-
Midfoot fracture
-
Forefoot fracture
General Measures
-
The soft tissue often is the limiting factor, as well as the major cause for complications.
-
Type I: Nondisplaced fracture:
-
Responds well to closed therapy, including a well-padded splint, ice, elevation, nonweightbearing
-
The splint can be converted to a cast when swelling begins to subside.
-
-
Types II and III: Displaced fractures:
-
Require surgical intervention
-
Are associated with poor results and multiple complications
-
Debate continues on whether to perform
open reduction with internal fixation or external fixation with or
without limited internal fixation. -
The current trend is toward external
fixation with limited internal fixation because of its equivalent
clinical results and lower complication rate. -
Treatment may use a staged approach.
-
Initial treatment with an external fixator is important to prevent limb shortening.
-
Limited percutaneous fixation may provide some fracture fixation.
-
After soft-tissue swelling has decreased, the fixator may be removed, and the fracture may be plated.
-
-
With severe injuries, primary arthrodesis rarely has a role.
-
-
Weightbearing is delayed until fracture union, no matter what mode of therapy is used.
-
The time frame often is 3–4 months, but it can be shorter for type I fractures treated nonsurgically.
P.455
Activity
Fractures should be splinted and the limb kept elevated.
Nursing
-
Always evaluate the neurovascular and soft-tissue status.
-
Compartment syndrome checks
Special Therapy
Physical Therapy
Physical therapy to address ankle ROM, leg strengthening, and gait after fracture healing
Medication
Patients require pain medication in the acute setting.
Surgery
-
In general, most plafond fractures are treated using a staged surgical protocol.
-
Staged treatment using initial external
fixation followed by later internal fixation has decreased complication
rates, especially those related to soft-tissue healing (3). -
External fixation:
-
A spanning fixator is placed using calcaneal transfixion PINS and tibial half-pins.
-
A ringed fixator may be used with thin wires.
-
The fibula must be brought out to length.
-
If the lateral skin is not too swollen, the fibula should be fixed with a plate.
-
The tibial articular surface should be aligned with traction and ligamentous taxis.
-
Limited percutaneous fixation should be considered to reduce the fracture further.
-
The external fixator allows the soft tissues to heal for later definitive plating and bone grafting.
-
-
Open reduction and internal fixation:
-
Soft-tissue swelling must be resolved before an open approach to the distal tibia, which may require waiting several weeks.
-
An anterior approach often is necessary to expose the fracture and allow precise reduction.
-
Reconstruct the distal tibial articular surface with lag screws.
-
Bone graft the tibial metaphyseal defect.
-
Stabilize the distal articular surface to the proximal tibia.
-
Contoured plates are available that fit the medial or lateral surface of the tibia.
-
Modern plates allow for percutaneous subperiosteal placement and the use of locking technology.
-
Prognosis
-
High-energy pilon fractures have a devastating effect on patients.
-
In 1 study at 3 years after injury, patients had decreased SF-36 scores, and 40% were not able to work (4).
-
Negative effects of the fracture can remain at the 5-year follow-up (5).
-
Complications
-
Chronic ankle pain
-
Early ankle degenerative joint disease
-
Need for revision operations or ankle arthrodesis
-
Compartment syndrome
-
Soft-tissue coverage issues
-
Wound dehiscence
-
Superficial wound infection
-
Pin infection with external fixation
-
Deep wound infection
-
Osteomyelitis
-
Posttraumatic arthrosis
Patient Monitoring
-
Patients are monitored for wound-healing
problems, maintenance of fracture reduction, radiographic union of
fracture, and advancement of weightbearing status. -
Patients should be treated with DVT prophylaxis after injury and while immobilized.
References
1. Ruedi TP, Allgower M. Fractures of the lower end of the tibia into the ankle-joint. Injury 1969;1:92–99.
2. American
College of Surgeons Committee on Trauma. Advanced Trauma Life Support
Program for Doctors, 6th ed. Chicago: American College of Surgeons,
1997.
College of Surgeons Committee on Trauma. Advanced Trauma Life Support
Program for Doctors, 6th ed. Chicago: American College of Surgeons,
1997.
3. Sirkin
M, Sanders R, DiPasquale T, et al. A staged protocol for soft tissue
management in the treatment of complex pilon fractures. J Orthop Trauma 2004;18:S32–S38.
M, Sanders R, DiPasquale T, et al. A staged protocol for soft tissue
management in the treatment of complex pilon fractures. J Orthop Trauma 2004;18:S32–S38.
4. Pollak AN, McCarthy ML, Bess RS, et al. Outcomes after treatment of high-energy tibial plafond fractures. J Bone Joint Surg 2003;85A:1893–1900.
5. Marsh JL, Weigel DP, Dirschl DR. Tibial plafond fractures. How do these ankles function over time? J Bone Joint Surg 2003;85A:287–295.
Additional Reading
Borrelli J Jr, Ellis E. Pilon fractures: Assessment and treatment. Orthop Clin North Am 2002;33:231–245.
Codes
ICD9-CM
823.8 Tibial plafond fracture
Patient Teaching
Patients are counseled on the risk of posttraumatic arthritis and the risk of long-term pain and disability.
FAQ
Q: Is a pilon fracture more severe than an ankle fracture?
A:
Yes. A pilon fracture is a high-energy fracture affecting the
weightbearing articular surface of the ankle. Patients are at high risk
for long-term ankle pain and dysfunction.
Yes. A pilon fracture is a high-energy fracture affecting the
weightbearing articular surface of the ankle. Patients are at high risk
for long-term ankle pain and dysfunction.
Q: Should all pilon fractures be treated with open reduction and internal fixation?
A:
No. Skin integrity is the overriding concern. If the ankle is very
swollen, open reduction should be delayed and the ankle treated in a
staged manner with external fixation and limited percutaneous fixation.
No. Skin integrity is the overriding concern. If the ankle is very
swollen, open reduction should be delayed and the ankle treated in a
staged manner with external fixation and limited percutaneous fixation.
