Patellar Dislocation
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Patellar Dislocation
Patellar Dislocation
Simon C. Mears MD, PhD
Bill Hobbs MD
Description
-
Patellar dislocation usually refers to
lateral displacement of the patella out of its normal alignment in the
trochlear groove of the femur. -
The patella is held stable by ligamentous forces, muscular forces, and bony anatomy.
-
Disruption of any of these 3 components can lead to recurrent patellar instability.
-
-
Classification:
-
Subluxation: Patella sits on the edge of the femoral groove, but not out of the track.
-
Dislocation: Patella is completely displaced out of the patellofemoral groove, usually laterally.
-
Epidemiology
-
Seen primarily in young patients (10–17 years old)
-
Occurs more often in females than in males
Incidence
-
The incidence is difficult to quantitate because many knees relocate spontaneously and are misdiagnosed.
-
A 9% incidence of a positive family history (1) is noted.
Risk Factors
-
Positive family history
-
Participation in football, basketball, baseball, gymnastics, or dancing
-
Age 10–17 years (2)
-
High level of activity or competition in a youth
-
Mechanism other than a direct blow
-
Hypermobility of the patella
-
Previous dislocations (49% of patients with a dislocation have a history of a previous dislocation) (2)
-
Patella alta (50% of patients) (1)
-
Shallow patellofemoral groove
-
Excessive Q angle
-
Ligamentous laxity
-
Excessive femoral anteversion
-
Vastus medialis dysplasia
-
Excessive genu valgus
Genetics
A congenital predisposition to knee malalignment and propensity to patellar dislocation is thought to exist.
Pathophysiology
-
Patellar dislocation can disrupt the medial patellofemoral ligament.
-
Chondral injury or fracture can occur from the impact of the patella on the trochlea (3).
Etiology
-
A direct blow to the medial aspect of the patella
-
Severe valgus injury to the knee
-
Twisting injury or other minor trauma, usually associated with congenital deficiencies
Associated Conditions
-
Connective tissue disease with ligamentous laxity, such as Ehlers-Danlos and Marfan syndromes
-
Femoral anteversion and pes planus
Signs and Symptoms
-
Patients with acute dislocation may present with the knee held in a flexed position as a result of hamstring spasms.
-
The femoral condyles may be prominent medially.
-
Often, the patella has spontaneously reduced, with the following findings:
-
Diffuse parapatellar tenderness
-
Positive apprehension test
-
Palpable defect at the insertion of the vastus medialis muscle
-
Hemarthrosis
-
History
-
Direct blow to the knee
-
Twisting injury to the leg
Physical Exam
-
After the acute symptoms subside, examine the knee for the following:
-
Effusion
-
Apprehension, with patellar translation both medially and laterally
-
Lateral tracking of the patella (in the shape of a “J”) with the knee extended from a flexed position (Fig. 1)
-
Injury to the medial, collateral, or cruciate knee ligaments
-
Lateral tilt
-
Tests
Imaging
-
Radiography:
-
Postreduction plain radiographs are obtained for evidence of osteochondral fragments.
-
Axial views of the bilateral patella may show substantial lateral tracking.
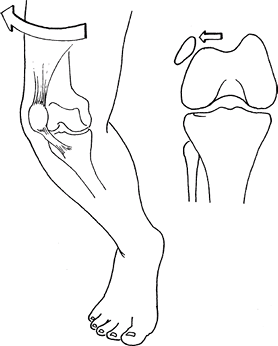 Fig. 1. Patellofemoral dislocation is almost always lateral.
Fig. 1. Patellofemoral dislocation is almost always lateral.
-
-
MRI or CT can reveal osteochondral injury and rupture of the medial patellofemoral ligament.
Pathological Findings
-
Abnormalities in the patellofemoral
articulation allow the pull of the vastus lateralis and lateral
retinaculum muscles to overcome that of the vastus medialis, even
during minor trauma. -
This unbalanced pulling often tears the medial retinaculum and vastus medialis insertion.
Differential Diagnosis
-
Cruciate ligament injury
-
Patellar fracture
-
Patellofemoral pain syndrome
-
Osteochondral fracture
General Measures
-
Reduce acute dislocations and then immobilize the knee.
-
Reduce acute dislocation by gentle,
steady extension of the knee, facilitated with the patient prone and
the patient’s hip extended to relax the hamstrings. -
Avoid forceful manipulation.
-
Once the knee is reduced, immobilize it in extension with a compression dressing.
-
Evaluate the medial retinacular structure for tenderness every 2 weeks for up to 6 weeks.
-
When the patient is comfortable, apply a Neoprene sleeve with a laterally based felt pad.
-
-
Surgical stabilization is recommended for the following:
-
Recurrent dislocations
-
Dislocations in carefully selected, highly active, competitive athletes
-
Acute dislocations with avulsive detachment of the vastus medialis muscle by bony fragment, seen on radiographs
-
Activity
-
Patients may bear weight after relocation.
-
Crutches should be supplied to facilitate weightbearing as tolerated.
-
Twisting motions should be avoided.
Special Therapy
Physical Therapy
-
The main goal of therapy is to strengthen the injured extensor mechanism and to improve patellofemoral tracking.
-
Straight-leg raises may begin immediately with appropriate support.
-
-
Patients with recurrent dislocations often advance more quickly with physical therapy for quadriceps strengthening.
Medication
Advise the patient that analgesics may be taken in the acute phase.
P.309
Surgery
-
Several procedures have been attempted for treatment of patellar dislocation (4).
-
Patients with acute dislocations and disruption of the medial patellofemoral ligament have been treated with acute repair (5).
-
Lateral release for patellar instability has poor results (6).
-
Patients with excessive Q angles
(>150°) and recurrent dislocation may benefit from distal
realignment via the Elmslie-Trillat or Fulkerson procedure. -
To prevent distal migration of the tibial
tubercle, procedures that involve the tibial physis should be avoided
in children with open physeal plates. -
Arthroscopy does not have a place in the
treatment of patellar dislocation other than for intra-articular
assessment of patellofemoral tracking or the treatment of associated
injuries.
Prognosis
-
Overall, 75% of patients are treated successfully with nonoperative means (2).
-
The key is to identify patients at risk for recurrence and to treat them more aggressively early in the course.
-
Long-term results after surgical treatment do not seem to be better than those after nonoperative treatment (7,8).
-
Long-term results of the Elmslie-Trillat osteotomy show improvement of instability, but results deteriorate over time (9).
Complications
-
Recurrent dislocations
-
Chronic anterior knee pain
-
Reflex sympathetic dystrophy
-
Hemarthrosis with a lateral release
-
Patellofemoral arthritis
-
Osteochondral fractures
Patient Monitoring
Patients are followed at 2–4-week intervals to monitor the progress of quadriceps rehabilitation.
References
1. Atkin
DM, Fithian DC, Marangi KS, et al. Characteristics of patients with
primary acute lateral patellar dislocation and their recovery within
the first 6 months of injury. Am J Sports Med 2000;28:472–479.
DM, Fithian DC, Marangi KS, et al. Characteristics of patients with
primary acute lateral patellar dislocation and their recovery within
the first 6 months of injury. Am J Sports Med 2000;28:472–479.
2. Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 2004;32:1114–1121.
3. Nomura E, Inoue M, Kurimura M. Chondral and osteochondral injuries associated with acute patellar dislocation. Arthroscopy 2003;19:717–721.
4. Fithian DC, Paxton EW, Cohen AB. Indications in the treatment of patellar instability. J Knee Surg 2004;17:47–56.
5. Mikashima
Y, Kimura M, Kobayashi Y, et al. Clinical results of isolated
reconstruction of the medial patellofemoral ligament for recurrent
dislocation and subluxation of the patella. Acta Orthop Belg 2006;72:65–71.
Y, Kimura M, Kobayashi Y, et al. Clinical results of isolated
reconstruction of the medial patellofemoral ligament for recurrent
dislocation and subluxation of the patella. Acta Orthop Belg 2006;72:65–71.
6. Panni AS, Tartarone M, Patricola A, et al. Long-term results of lateral retinacular release. Arthroscopy 2005;21:526–531.
7. Buchner
M, Baudendistel B, Sabo D, et al. Acute traumatic primary patellar
dislocation: long-term results comparing conservative and surgical
treatment. Clin J Sport Med 2005;15:62–66.
M, Baudendistel B, Sabo D, et al. Acute traumatic primary patellar
dislocation: long-term results comparing conservative and surgical
treatment. Clin J Sport Med 2005;15:62–66.
8. Nikku
R, Nietosvaara Y, Aalto K, et al. Operative treatment of primary
patellar dislocation does not improve medium-term outcome: a 7-year
follow-up report and risk analysis of 127 randomized patients. Acta Orthop 2005;76:699–704.
R, Nietosvaara Y, Aalto K, et al. Operative treatment of primary
patellar dislocation does not improve medium-term outcome: a 7-year
follow-up report and risk analysis of 127 randomized patients. Acta Orthop 2005;76:699–704.
9. Carney
JR, Mologne TS, Muldoon M, et al. Long-term evaluation of the
Roux-Elmslie-Trillat procedure for patellar instability: a 26-year
follow-up. Am J Sports Med 2005;33:1220–1223.
JR, Mologne TS, Muldoon M, et al. Long-term evaluation of the
Roux-Elmslie-Trillat procedure for patellar instability: a 26-year
follow-up. Am J Sports Med 2005;33:1220–1223.
Additional Reading
Hinton RY, Sharma KM. Acute and recurrent patellar instability in the young athlete. Orthop Clin North Am 2003;34:385–396.
Codes
ICD9-CM
836.3 Patellar dislocation
Patient Teaching
Discuss the risk factors for recurrent dislocation with
a possible recommendation that the patient avoid high-risk activities
or sports.
a possible recommendation that the patient avoid high-risk activities
or sports.
Prevention
Patients who are at high risk or have had previous
instability should keep their quadriceps strong and consider bracing or
taping.
instability should keep their quadriceps strong and consider bracing or
taping.
FAQ
Q: What is the treatment for a 1st-time patellar dislocation?
A:
Treatment is nonsurgical with relocation, quadriceps strengthening, and
gentle return to activity. Surgical intervention should be considered
with care and only if specific indications are present.
Treatment is nonsurgical with relocation, quadriceps strengthening, and
gentle return to activity. Surgical intervention should be considered
with care and only if specific indications are present.
