Median Nerve
related to a variety of causes. Some have placed it in the category of
repetitive stress syndrome, but it is beyond the scope of this chapter
to discuss this issue. This chronic condition is appropriately contrasted to acute median nerve compression seen most commonly in association with fractures about the wrist.
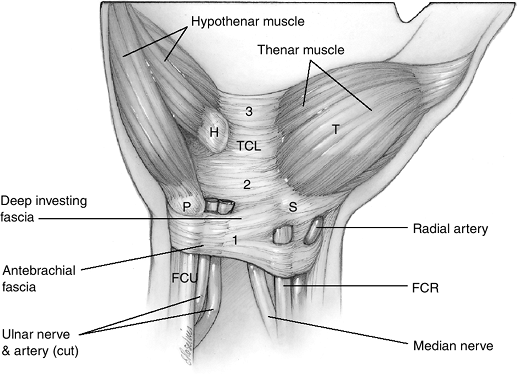
wrist through a fibroosseous canal or tunnel. The floor and sides of
this tunnel are formed by the pronator quadratus muscle and the carpal
bones. Figure 7.1-1 shows the roof of this structure, which is formed by the flexor retinaculum. The flexor retinaculum is composed of the following:
-
Proximally, the antebrachial fascia and deep investing forearm fascia.
-
The central portion is the transverse
carpal ligament that is defined by its attachments to the pisiform and
hook process of the hamate ulnarly, and radially to the tuberosity of
the scaphoid and ridge of the trapezium. -
The distal portion is the aponeurosis between the thenar and hypothenar muscles.
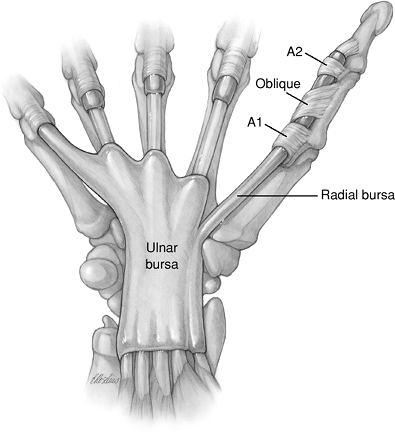
this canal. These tendons are covered by a synovial sheath called the
ulnar and radial bursa (Figure 7.1-2). The reader is referred to the suggested reading list for details of the complex anatomy of this region
distally, it acts as a closed compartment. Chronic median nerve
compression results when pressure levels exceed those normally
tolerated by the median nerve. Carpal tunnel (CT) pressure levels in
normal subjects have been recorded at 2.5 to 10 mm Hg, whereas CTS
patients may exhibit levels of approximately 30 mm Hg. It is unclear,
and experts have debated, if the underlying cause of nerve dysfunction
is the relationship between mechanical factors or ischemia. It has been
observed that nerve compression of 20 to 30 mm Hg will block venous
blood flow and axonal transport, and compression of 60 to 80 mm Hg will
block intraneural blood flow. Nerve conduction block occurs at 130 to
150 mm Hg.
are affected by finger, wrist, and forearm position, and activities
such as pinching and grasping. Carpal tunnel (CT) pressure increases
with wrist flexion and with extension. Anatomic studies have noted
incursion of the distal muscle bellies of the FDS when the fingers are
extended. They have also noted similar incursion of the lumbrical
muscles when the fingers are flexed. This may partly explain the
pressure changes noted in various finger and wrist positions.
 |
|
Figure 7.1-1
The anatomy of the flexor retinaculum. 1, antebrachial and deep investing forearm fascia; 2, central portion of the transverse carpal ligament (TCL); 3, distal aponeurosis. H, hook process of hamate; P, pisiform; S, scaphoid; T, thenar eminence. |
 |
|
Figure 7.1-2
The synovial tissue that surrounds the nine flexor tendons as they pass through the carpal tunnel is called the ulnar and radial bursa. |
also factors leading to CTS in patients with diabetes, chronic renal
failure, hypothyroidism, and pregnancy. Rheumatoid, gouty, or other
inflammatory arthritis can cause hyperplasia of the tenosynovium, which
can diminish the space available in the carpal canal for the median
nerve. This compresses the nerve. Diabetic patients have a predilection
to develop CTS because of increased nerve susceptibility to injury, and
because of a lower pressure threshold for blockage of fast axonal
transport.
and the carpus, are the most common causes of acute compression of the
median nerve. These injuries are often characterized as space-occupying
lesions in terms of the carpal canal and the median nerve. A volarly
displaced lunate or a fragment of a Colles fracture may significantly
compromise the volume of the CT. This may compress the median nerve
against the flexor retinaculum. As part of a Colles fracture treatment,
a hematoma block and extreme wrist flexion have both been shown to
further increase pressure within the canal. Post-traumatic edema
associated with these injuries also plays a significant role in the
production of acute CTS.
-
Patients with CTS often present with multiple complaints, but the most common is numbness and tingling in the fingers and thumb.
-
The patient is often unable to tell the examiner which digits tingle.
-
The numbness may be constant or
intermittent, and commonly occurs 2 to 3 hours after retiring for the
night. These nocturnal symptoms have been ascribed to the fact that the
normal use of the hand during the day promotes the flow of
well-oxygenated blood
P.100to
the median nerve. At night, however, venous stasis occurs, and oxygen
tension in the nerve decreases to a level that promotes or triggers the
symptoms. This concept is supported by the fact that patients often
relieve the numbness through vigorous massage or by shaking their hands.
-
-
Patients often complain of dropping things, and they sometimes complain of pinch or grip weakness.
-
Predisposing or associated conditions
should be asked about. Those include occupational and sports
activities, as well as associated disorders such as rheumatoid
arthritis, diabetes, and thyroid disease. Other peripheral neurological
disorders that may produce hand numbness are cervical radiculopathy,
brachial plexopathy, thoracic outlet syndrome, apical lung tumor,
pronator syndrome, cubital and ulnar tunnel syndrome, and peripheral
neuropathy. -
Bilateral CTS in a young male should prompt an investigation for acromegaly.
-
Sensory evaluation may be by static or moving two-point discrimination (2PD) and Semmes-Weinstein (SW) monofilaments.
-
The static 2PD evaluates the status of
slowly adapting large myelinated fibers, while the moving 2PD evaluates
the fast adapting large myelinated fibers. -
SW monofilaments are threshold tests that evaluate sensory end organ function.
-
-
The SW test is more sensitive in
identifying compressive neuropathy than 2PD; when abnormal 2PD is
present, the disease is more severe.
-
Motor evaluation consists of looking for thenar atrophy and strength testing the abductor pollicis brevis.
-
The disease is considered severe and is usually longstanding when there is thenar muscle atrophy.
-
Atrophy is seldom, if ever, recovered following CT release.
-
Commonly used provocative tests for CTS
include Phalen’s and Tinel’s signs, the CT compression test (Durkan’s
sign), the tourniquet test, and a combined Phalen’s maneuver with SW
monofilament testing. These and other useful tests are given in Table 7.1-1.
-
Electrodiagnostic studies include nerve conduction velocity (NCV) and electromyography (EMG).
-
An abnormal nerve conduction result
includes decreased action potential amplitude, increased distal
latency, and decreased velocity. -
A distal motor latency of >4.5 ms and
a sensory latency of >3.5 ms constitute and abnormal result. These
measurements are achieved using an orthodromic stimulus and recording
across the wrist. -
Additional diagnostic accuracy has been
shown with nerve conduction measurements assessing short nerve segments
(such as the inching technique or the comparison of palm-to-digit and
wrist-to-digit latencies). In the case of CTS, measurements are made by
isolating the wrist segment. -
Electromyography measures insertional activity, resting potential, and muscle activation.
-
Increased insertional activity,
fibrillations at rest, positive sharp waves, complex repetitive
discharges, and decreased motor unit recruitment are all consistent
with nerve compromise.
-
a patient can be diagnosed with CTS depends on the population being
studied. They observed that a combination of findings in the history
and physical exam was more accurate than the same findings in
isolation. The CTS was accurately diagnosed 86% of the time when night
pain, a positive SW monofilament test, a positive Durkan’s test, and a
positive Brigham hand diagram were all present; the probability of
having CTS was 0.68% when all of these tests were negative. These
authors noted that electrodiagnostic studies did not add to the
diagnostic power of this combination of tests.
only objective evidence, and equate it to the “gold standard” for
diagnosis of CTS. But not all agree. These tests may be positive in
asymptomatic individuals, and negative in individuals with classic
signs and symptoms. Some observers have noted that a significant number
of patients diagnosed with CTS on clinical grounds—but with negative
electrodiagnostic studies—have improved following a CTR.
from acute CTS, because delayed release of an acute CTS may result in a
poor outcome. Contusion may be treated by observation, whereas acute CT
syndrome requires immediate release.
-
Signs and symptoms of contusion appear immediately,
in contrast to those of compression that may occur later, as swelling
increases. Thus, initial and careful sensory evaluation is mandatory. -
SW or 2PD tests are useful.
-
In some cases, direct pressure
measurements are indicated. Pressure greater than 40 mm Hg as measured
by a wick catheter in the CT indicates the need for immediate CT
release.
mild CTS, and is initially indicated for moderate cases. Any associated
conditions should be identified and treated as indicated.
-
Treatment is aimed at the underlying
process, and may include activity modification such as ergonomic
studies and corrections, splints that immobilize the wrist in a neutral
position, and oral nonsteroidal medication. In some cases, treatment
includes a short course of steroidal anti-inflammatory medication.P.101Table 7.1-1 Tests for Carpal Tunnel Syndrome (CTS)Test How Performed Condition Tested Interpretation of Positive Result Positive Result Phalen’s test Elbows on table, forearms vertical, wrists flexed Paresthesia in response to position Numbness or tingling on radial digits within 60 seconds Probable CTS (sens 0.75, spec 0.47) Percussion test (Tinel sign) Lightly tap along median nerve from proximal to distal Site of nerve lesion “Electric” tingling response in fingers Probable CTS if positive at the wrist (sens 0.60, spec 0.67) Carpal tunnel compression test (Durkan) Direct compression of median nerve at carpal tunnel Paresthesia in response to compression Paresthesia within 30 seconds Probable CTS (sens 0.87, spec 0.90) Hand diagram Patient marks site of pain or altered sensation on outlined hand diagram Patient’s perception of symptoms Markings on palmar side of radial digits, without markings in palm Probable CTS (sens 0.96, spec 0.73, negative predictive value 0.91) Hand volume stress test Hand volume measured by displacement, repeat after 7-minute stress test and a rest of 10 minutes Hand volume Hand volume increased by 10 mL or greater Probable dynamic CTS Direct measurement of carpal tunnel pressure Wick or infusion catheter placed in carpal tunnel Hydrostatic pressure in resting and provocative positioning Resting pressure 25 mm Hg or more (variable and technique related) Hydrostatic compression is felt to be probable cause of CTS Static 2-point discrimination Determine minimum separation of two distinct points when applied to palmar fingertip Innervation density of slow-adapting fibers Failure to determine separation of at least 5 mm Advanced nerve dysfunction Moving 2-point discrimination As above, with movement of the points Innervation density of fast-adapting fibers Failure to determine separation of at least 4 mm Advanced nerve dysfunction Vibrometry Vibrometer placed on palmar
side of digit, amplitude set to 120 Hz, and increase to threshold of
perception; compare median and ulnar bilaterallyThreshold of fast-adapting fibers Asymmetry compared to contralateral hand or median to ulnar in ipsilateral hand Probable CTS (sens 0.87) Semmes-Weinstein monofilaments Monofilaments of increasing diameter touched to palmar side of digit until patient can determine which digit is touched Threshold of slowly adapting fibers Value greater than 2.83 Median nerve impairment (sens 0.83) Distal sensory latency and conduction velocity Orthodromic stimulus and recording across wrist Latency, conduction of sensory fibers Latency greater than 3.5 msec, or asymmetry of conduction velocity of greater than 0.5 msec versus opposite hand Probable CTS Distal motor latency and conduction velocity Orthodromic stimulus and recording across wrist Latency, conduction velocity of motor fibers of median nerve Latency greater than 4.5 msec, or asymmetry of conduction velocity of greater than 1.0 msec Probable CTS Electromyography Needle electrodes placed in muscle Denervation of thenar muscles Fibrillation potentials, sharp waves, increased insertional activity Advanced motor median nerve compression Sens,
sensitivity; spec, specificity. (From Abrams R, Meunier, M. Carpal
tunnel syndrome. In: Trumble TE, ed. Hand surgery update 3, hand,
elbow, shoulder. Rosemont, IL: American Society for Surgery of the
Hand, 2003:299–312.) -
Steroid injection or steroid
iontophoresis into the CT, along with splinting, may give short-term
benefit. It occasionally gives long-term benefit. -
A positive response affirms the diagnosis, and may be a predictor of a satisfactory surgical outcome, if required.
-
Stretching, strengthening, and
flexibility exercises may also play a significant role in recovery and
avoidance of surgery in selected patients.
-
Surgical treatment of CTS is indicated
for patients who have failed conservative treatment, and for patients
with thenar muscle weakness, atrophy, or with signs of motor
denervation on electrodiagnostic studies.
-
The incision for open CT release is a
longitudinal incision that begins at the wrist flexion crease and ends
about 1 cm proximal to the proximal palmar crease. Its axis is somewhat
parallel to the radial border of the ring finger.-
Others have tried to identify the ideal
site of placement, and have noted that the depression between the
thenar and hypothenar eminence is the ideal site for the incision. -
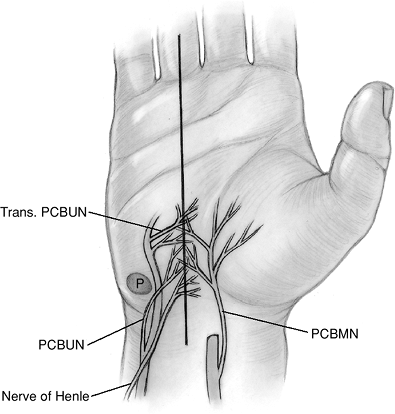
This sought-after zone is the zone in which the least number of superficial nerves are present. But there is no true internervous or nerve-free zone for this incision (Figure 7.1-3).
-
The incision just described places the
dissection to the ulnar side of the CT, which is considered to be the
relatively safe side for entering the canal and releasing the TCL.
-
-
Some surgeons have used smaller, single-
or two-portal incisions to accomplish exposure and release of the TCL.
Many of these techniques use special blade-guide instruments to
facilitate section of the TCL.
ulnar margin of the TCL without injury to vital structures such as the
median nerve and its branches—including the recurrent or motor
branch—and the superficial palmar arch that is just distal to the
distal end of the TCL. The technical details of the various CT release
techniques are beyond the scope of this text.
the arthroscope to assist in TCL section. Single- and two-portal
techniques have been used with success.
suggested that there is earlier functional recovery in the endoscopic
technique compared to open techniques. However, there is no current
evidence available to show that the endoscopic technique is superior in
terms of final outcome to the open technique.
 |
|
Figure 7.1-3
Cutaneous innervation of the palm as it relates to open carpal tunnel release. Four nerves are at risk (all nerves that may be cut or pass within 2 mm of the incision): the palmar cutaneous branch of the median nerve (PCBMN); the palmar cutaneous branch of the ulnar nerve (PCBUN); the nerve of Henle; and transverse palmar branches (Trans. PCBUN) from the ulnar nerve in Guyon’s canal. |
means, including open, limited-open with or without special guide
instruments, and endoscopic release, have all been associated with
complications.
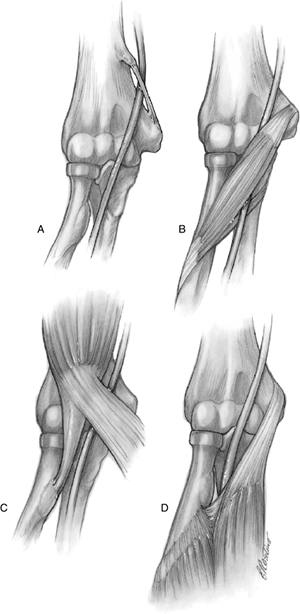
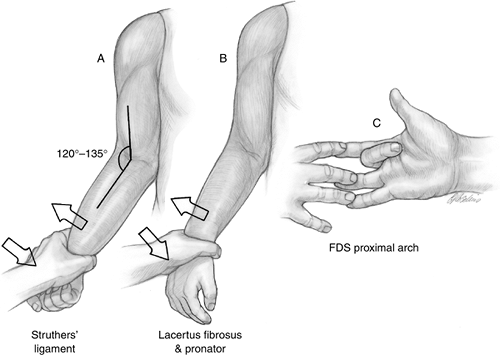
compression: two are in the distal arm and three are in the proximal
forearm (Figure 7.1-4).
an abnormal proximal origin of the superficial head of the pronator
teres from the supracondylar ridge rather than the medial epicondyle.
This abnormal muscle position results in lateral displacement of the
neurovascular bundle, and has the potential for compression of the
underlying median nerve and brachial artery.
is represented by a supracondylar process and a ligament of Struthers,
which spans between the supracondylar process and the medial
epicondyle, thus creating an arcade that contains the median nerve and
brachial artery. The supracondylar process is a hook-shaped projection
of bone from the
anteromedial
aspect of the distal humerus. It arises 3 to 5 cm proximal to the
medial epicondyle and is 2 to 20 mm in length. Its incidence is
approximately 1%, and it is a rare cause of pressure on the under lying
median nerve and brachial artery.
 |
|
Figure 7.1-4 Sites of compression of the median nerve in the arm/forearm. (A) The ligament of Struthers from an anomalous supracondylar process to the medial epicondyle. (B) The pronator teres. (C) The lacertus fibrosus (the least common cause). (D) A fibrous arch in the flexor digitorum superficialis of the middle finger.
|
compressed at one of three levels, in the following order of frequency:
the pronator teres, the flexor superficialis arch, and the lacertus
fibrosus.
a fibrous band on the dorsum of the superficial head of the pronator
overlying the median nerve, or a fibrous band as a component of the
deep ulnar head of the pronator when the latter was present, or, when
the deep head was absent, a separate fibrous band attached to the
coronoid process of the ulna proximally. In some instances, fibrous
bands were noted on both heads, which formed a definite fibrous arcade.
of the dissections spanning from the proximal margin of the FDS to the
middle finger.
fibrosus is the least common cause of median nerve entrapment in the
proximal forearm. It may be secondary to hypertrophy or enlargement of
the lacertus
-
If complaints are produced by flexion of
the elbow against resistance between 120 and 135 degrees of elbow
flexion, compression may be in the distal arm beneath a ligament of
Struthers. -
Compression by the lacertus fibrosus may
be aggravated by active flexion of the elbow against resistance when
the arm is pronated. -
If symptoms are increased by resisted
pronation of the forearm (usually combined with wrist flexion to relax
the FDS), the nerve may be compressed between the pronator. -
If the symptoms are aggravated by resisted flexion of the FDS to the middle finger, compression may be at the FDS proximal arch.
-
The operative technique for treatment of
pronator syndrome includes complete exploration of the median nerve,
from the distal arm to the proximal forearm. -
The median nerve is explored from the
region of a possible anomalous supracondylar process and an associated
ligament of Struthers to the proximal edge of the FDS, with release of
all potentially constricting structures, including the ligament of
Struthers and the lacertus fibrosus. -
At the level of the PT, compression may be because of muscle hypertrophy or constricting muscle fascial bands.
-
Further decompression of the median nerve
is achieved by tracing the median nerve into the substance of the PT,
and then releasing any areas of constriction. -
The final site of possible constriction
is in the proximal edge of the FDS, which may be exposed by entering
the interval between the FCR and the PT. -
The median nerve may be constricted here beneath a fibrous tissue arch along the leading edge of the FDS.
-
A persistent median artery has also been
observed as a cause of pronator syndrome. Reported cases have
demonstrated penetration of the median nerve by the median artery, and
constriction of the nerve by vascular leashes from the median artery.
 |
|
Figure 7.1-5 Localizing tests for median nerve compression in the proximal forearm. (A) Test for presence of a ligament of Struthers. (B) Test for lacertus fibrosus and pronator teres compression. (C) Test for median nerve compression by fibrous tissue arch of flexor digitorum superficialis of the middle finger (see text).
|
characteristically results in complete or partial loss of function of
the FPL and the flexor digitorum profundus (FDP) of the index finger
and long fingers, as well as of the PQ. This occurs without any sensory
deficits. These findings may be associated with vague complaints of
discomfort in the proximal forearm. In the complete AIN syndrome
(AINS), the affected patient assumes an unusual pinch posture with the
distal joint of the index and thumb in extension. Although the FPL and
FDP of the index are innervated exclusively by the AIN, the FDP of the
long finger is exclusively innervated by the AIN only 50% of the time.
In the remaining 50%, the long finger FDP is at least partially
innervated by the ulnar nerve. Variations from the classic AINS include
isolated paresis or paralysis in either the index profundus or the FPL.
In both complete and partial types, there is often an antecedent
history of unusual muscular exertion, blunt trauma, or edema in the
extremity.
-
AINS, especially the incomplete type,
must be distinguished from flexor tendon rupture, flexor tendon
adhesion, and stenosing tenosynovitis. -
If a Martin-Gruber connection is present between the AIN and the ulnar nerve, there may be intrinsic muscle paresis or atrophy.
-
The incomplete type of AINS may be
distinguished from rupture of the FPL by noting passive flexion of the
interphalangeal joint of the thumb with wrist and metacarpophalangeal
(MCP) joint hyperextension in AINS, in contrast to absence of thumb
interphalangeal joint flexion in rupture of the FPL.
-
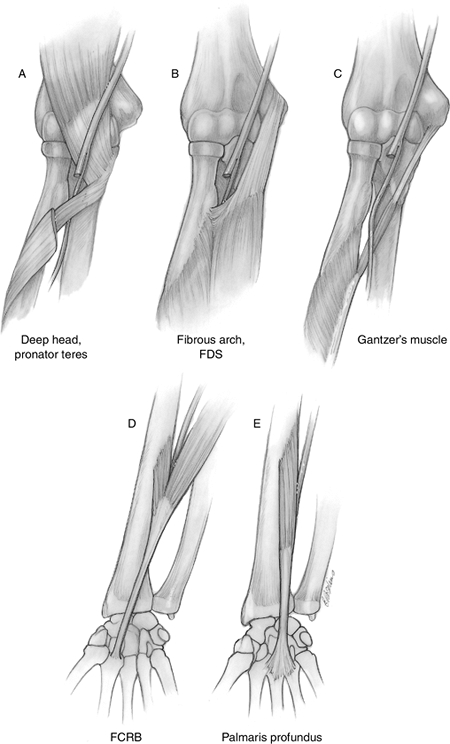
The nerve is usually compressed by
fibrous bands that run from the deep (most common) or superficial head
of the PT to the brachialis fascia (Figure 7.1-6). -
Other sites of compression have been
identified, including the fibrous tissue arcade of the FDS, which the
AIN passes beneath to sit on the interosseous membrane (IOM). -
Other reported causes of compression
include enlarged bursae or tumors, aberrant or thrombosed vessels, a
double lacertus fibrosus overlying the nerve, compression of the nerve
as it runs deep to both heads of the PT, and fractures of the forearm
and distal humerus. -
Three aberrant muscles have been
identified in association with AINS, including an accessory head of the
FPL called Gantzer’s muscle, the palmaris profundus, and the flexor
carpi radialis brevis (FCRB).-
Although an accessory head of the FPL
(Gantzer’s muscle) has been identified as a cause of AINS, some
observers have noted that Gantzer’s muscle always is posterior to the
median nerve and AIN. However, in dissections of the forearm in which
Gantzer’s muscle was present, the authors demonstrated the possibility
of a pincer-like effect between this abnormal posterior head and the
adjacent anterior FDS. This could produce compression of the median
nerve, as well as the AIN. The median nerve and AIN passed through the
interval between these two muscles, which share a common origin on the
medial epicondyle.
-
-
The common denominator in this condition
appears to be localized edema, superimposed on an anatomic abnormality
that is either congenital or acquired.
without surgery. This is especially true in children with AINS associated with fractures of the forearm and elbow region.
 |
|
Figure 7.1-6 Anterior interosseous nerve compression sites. (A) Deep head of the pronator teres. (B) Fibrous arch of the middle finger flexor digitorum superficialis. (C) Gantzer’s muscle. (D) Abnormal flexor carpi radialis brevis (FCRB). (E) Abnormal palmaris profundus muscle. FDS, flexor digitorum superficialis.
|
-
Exploration and decompression is advised
in patients who present with complete paralysis of either muscle tendon
unit and who have shown no improvement, as determined by physical
examination or repeat EMG after 12 weeks of observation. -
The AIN is exposed through a curved incision beginning at the antecubital flexion crease just medial to the biceps tendon.
-
The median nerve is traced distally to
its entrance between the two heads of the PT, and the superficial head
of the PT is mobilized and retracted to reveal the usual site of origin
of the AIN, from the posterior aspect of the median nerve. -
The site of compression may be identified
by noting a pale discoloration in the nerve, with or without a
concomitant indentation of the nerve. -
All potential sites of compression are released; it is not necessary to perform an internal neurolysis.
-
It may be necessary to divide the
insertion of the PT, in order to facilitate exposure of the AIN at the
superficialis fibrous arcade.
