Glenohumeral Joint Subluxations, Dislocations, and Instability
Two – Upper Extremity > 38 – Glenohumeral Joint Subluxations,
Dislocations, and Instability
allows the glenohumeral joint to be used as a stable fulcrum for
placing the upper extremity at various positions in three-dimensional
space. A consequence of this flexibility, however, is the propensity
for the joint to become unstable. As such, the shoulder is believed to
be the most commonly dislocated major joint in the human body, with the
reported incidence being 8.2 to 23.9 per 100,000 persons per year.128,196,203,251
Understandably, therefore, the diagnosis and the treatment of
glenohumeral instability have been well documented in the history of
mankind. The first description of shoulder dislocation is believed to
have occurred as early as 3000 BCE.295
In addition, prehistoric drawings from 1200 BCE show figures that are
extremely similar to a shoulder reduction maneuver commonly used today.107
Detailed descriptions regarding the pathology and the treatment of
shoulder instability can also be found in the teachings of Hippocrates
who lived around 450 BCE.25,92,93
To treat patients with shoulder instability, he recommended the
judicious insertion of a hot iron poker into the axilla to form “eschar
tissue.”
activities, the incidence of glenohumeral instability may be
increasing. In accordance, the amount of information in the orthopaedic
literature regarding this condition has also seen a significant gain.
Recent publications have greatly augmented the
knowledge
base on the diagnosis, natural history, treatment, and expected outcome
of glenohumeral instability. Experiences with various repair
techniques, including both open and arthroscopic, have also provided
additional options in the surgical management of this condition. Thus,
despite the fact that it has been widely recognized and treated over
the long course of human history, treatment for glenohumeral
instability is continuing to evolve.
of injury that resulted in shoulder instability. This may be true in
patients with underlying ligamentous laxity or in patients whose
shoulder musculature has been deconditioned. For these patients, the
onset of instability can be associated with minimal or no significant
trauma.66,215,239
In most patients, however, shoulder instability occurs after a clear
traumatic insult. According to one estimate, up to 96% of acute
shoulder dislocations were traumatic in origin.236
For these patients, it is important to estimate the amount of energy
that produced the instability. Some cases of instability are the result
of a violent high-energy trauma, and may be associated with other
soft-tissue or bony damage.
in subluxations or dislocations, instability usually occurs after an
indirect force is applied to the shoulder. In the cadet population at
West Point, for example, subluxations are much more common than frank
dislocations and are associated with activities including throwing
punches, collisions, and falls.203
As such, unexpected force to the arm when the glenohumeral joint is in
a susceptible position is often the cause of instability. For many
anterior shoulder dislocations, the shoulder is typically in some
combination of abduction, external rotation, and extension when a
sudden load is applied to the arm. For posterior instability, on the
other hand, the shoulder is usually in flexion, adduction, and internal
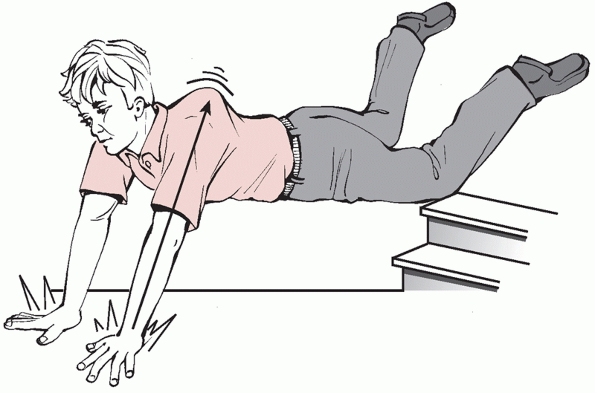
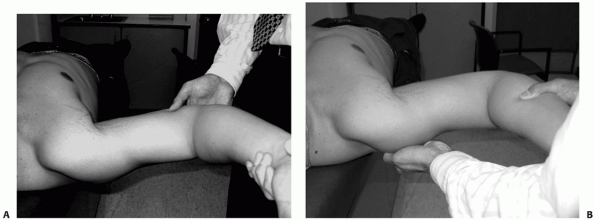
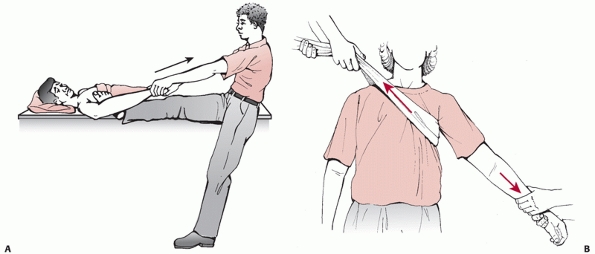
rotation when an axial load is applied (Fig. 38-1). Other much less common mechanisms such as seizures and electrical shock can also cause glenohumeral joint instability.33,248
With these mechanisms, wherein all the muscles about the joint are
cocontracted, the external rotators of the shoulder can overpower the
internal rotators to cause posterior dislocations.
 |
|
FIGURE 38-1
Mechanism of injury for posterior glenohumeral dislocation. An axial load to the arm when the shoulder is in flexion, adduction, and internal rotation places the humeral head in a position susceptible to posterior dislocation. |
instability. Most are thought to occur during the initial episode of
dislocation or subluxation, and can involve either soft tissue or the
bony structures. They include, but are not limited to, humeral head
defects, tuberosity fractures, glenoid fractures, humeral neck
fractures, rotator cuff tears, vascular compromise, and neurologic
injuries. Identification of these injuries is extremely important
because they can often affect patient management and outcome. As such,
all patients must be scrutinized for any associated injuries. Of these,
some occur more commonly and merit special attention.
With the trauma of the dislocation, the humeral head is forced upon the
glenoid rim and the relatively soft bone of the humeral head is
crushed. The end result is an impression of the glenoid rim that is
made on the humeral head. As such, these defects are often referred to
as “impression fractures.” With subsequent muscle spasms, these
fractures can enlarge. In patients with initial shoulder dislocations,
the incidence of a humeral head defect is noted to be between 38% and
47%.32,237 In patients with recurrent instability, the reported incidence is even higher at 50% to 67%.259
created on the posterolateral aspect of the humeral head and are
referred to as Hill-Sachs lesions (Fig. 38-2).91
With posterior shoulder dislocations, the defects are created on the
anteromedial aspect of the humeral head and are sometimes called
reverse Hill-Sachs lesions. As such, location of these defects can
demonstrate the direction of the instability. In addition, presence of
these defects also suggests a traumatic dislocation as they are
relatively uncommon in patients with nontraumatic instability. Although
most small humeral head defects do not influence treatment, large
defects warrant special attention as they may require specific surgical
intervention.
association with shoulder dislocations is unknown; however, it appears
to increase dramatically with age. Although the overall rate of rotator
cuff tear may be as low as 15%, its incidence in patients older than 40
years has been estimated to be between 35% and 40%.210,286 In patients older than 60 years of age, the incidence of concomitant rotator cuff tears may be as high as 80%.286
These patients typically present with weakness of shoulder abduction
and external rotation. Often their presentation may be confusing and
misdiagnosed as a neurologic injury.119,192
Nonetheless, any patient who demonstrates weakness after shoulder
dislocation must be evaluated for a rotator cuff tear because prompt
identification and management is crucial to the overall outcome.210
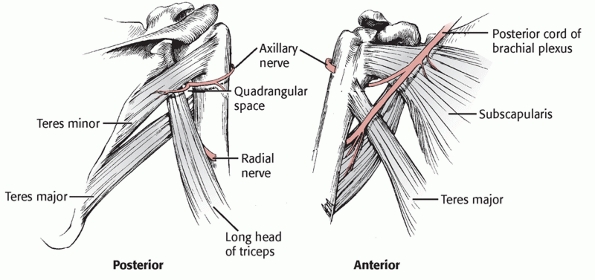
joint, the axillary nerve and the brachial plexus are susceptible to
injury during shoulder dislocations (Fig. 38-3).
Based on electrophysiological findings, the rate of injury may be as
high as 65%. The incidence of clinically evident neurologic injury,
however, is believed to be much lower, with the reported rates between
5% and 25%.26,47,172,260
These studies also demonstrated that the axillary nerve is the most
commonly injured neurologic structure after a shoulder dislocation and
that this rate of injury is increased in older individuals.
Nevertheless, as demonstrated in an electrophysiological study, some
patients with axillary nerve injury exhibited completely normal
sensation about the shoulder.17
Therefore, relying on sensory testing alone for axillary nerve function
may be misleading. Examination of the axillary nerve must include
specific testing of both the sensory (sensation about the lateral
deltoid area) and the motor (isometric contraction of the deltoid)
components. If a neurologic injury is suspected, an
electrophysiological examination should be obtained to establish the
baseline of injury. For these patients, most authors typically
recommend close observation rather than early surgical intervention
because neurologic recovery over the course of 3 to 6 months is
anticipated.17,26,260
If repeated electrophysiological studies do not demonstrate signs of
recovery by 2 to 3 months, nerve exploration may then be considered.286
 |
|
FIGURE 38-2 The Hill-Sachs lesion associated with anterior shoulder dislocation. Normal anatomic relationships (A). Anterior dislocation without a compression fracture defect (B). A small posterolateral defect (C). A large compression fracture defect (D). After reduction, the defect is quite evident and has deformed the normal articular surface of the humeral head (E). After shoulder reduction, the lesion can be appreciated in a routine AP radiograph with the arm in internal rotation (F). Arthroscopic evaluation shows that the lesion can be quite extensive and possibly re-engage the glenoid rim (arrow) with external rotation (G).
|
 |
|
FIGURE 38-3
Anatomy of the axillary nerve as it passes through the “quadrangular space.” Because of its nearby location, the axillary nerve is the most commonly injured neurologic structure after a shoulder dislocation. |
identification of the injury. Often the patient may be able to clearly
recount the shoulder position as well as the direction of the applied
force. In other instances, this information may be more clearly
obtained from an eyewitness. Additional information regarding prior
shoulder injury, prior episodes of instability, and prior treatments
should all be documented. Hand dominance, occupation, activity level,
and general health history should also be obtained. A general survey of
the patient, including an adequate examination of the spinal column,
should then be performed. Inspection of the shoulder may reveal an open
wound, localized swelling, or a gross deformity. Often these
deformities can be best visualized by inspecting the patient from
behind, with the patient in a sitting position. With an anterior or
posterior glenohumeral dislocation, the humeral head may be palpable
beneath the skin.
because of pain and muscle spasms. Whenever possible, however, the
limits of shoulder motion should be established as they may provide
insight into both the severity and the direction of the instability.
Patients with an anterior dislocation, for example, will typically
demonstrate limitations in internal rotation and abduction. In
contrast, patients with a posterior dislocation will often demonstrate
limitations in external rotation. In very rare instances, referred to
as luxatio erecta humeri, the patient may suffer from inferior glenohumeral dislocation with the arm locked in fully abducted position (Fig. 38-4).45,268,292
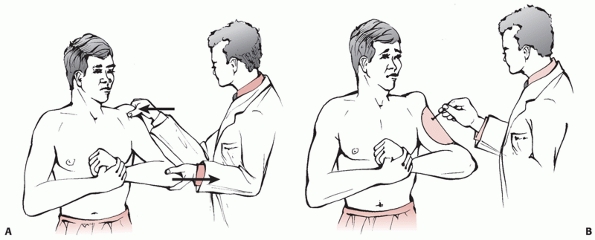
Before any manipulation, a complete neurovascular examination of the
upper extremity must be performed and documented. The axillary nerve is
the most commonly injured nerve after an anterior glenohumeral
dislocation, with some electrodiagnostic studies reporting rates as
high as 60%.17,260 Therefore, both the motor and the sensory component of this nerve must be examined (Fig. 38-5). Although quite rare, vascular injuries following shoulder dislocations have also been reported.65,148
variety of clinical symptoms. Some may present for definitive care
after being treated at a local emergency room for an acute shoulder
dislocation. Some may present with a recent exacerbation of a recurrent
instability. Others may present with a vague history of pain without
clinical suspicion or prior diagnosis of instability. Because of this
variability in presentation, the importance of an accurate and complete
history cannot be overemphasized.
general orthopaedic information should be obtained first. This includes
age, occupation, hand dominance, level of sporting or recreational
activity, presence of any previous injury or surgery, and functional
impairments because of shoulder symptoms. If pain is the predominant
complaint, its characteristics such as severity, location, duration,
and precipitating position and/or activity must be clearly defined. In
contrast, if instability is the predominant complaint, the frequency
and the severity of the instability as well as the susceptible shoulder
positions should be elicited. Often these patients have been avoiding
specific tasks that involve placing their shoulder in a position
vulnerable to dislocations. As such, details of their functional
limitations may provide clues to the direction and the severity of the
instability.
should be defined clearly. This includes the timing, the amount of
applied energy, the position of the shoulder at the time of the impact,
and the degree of instability. For patients with recurrent instability,
the severity of force associated with a recent exacerbation may be
slight such as raising the arm or reaching for an object. Any history
of previous shoulder instability should prompt questions regarding the
nature of the injury as well as any prior treatments. Clinical
evaluation of patients with recurrent instability should include
questions regarding voluntary instability. Any issues regarding a
secondary gain from shoulder instability should also be defined. If a
patient can dislocate the shoulder voluntarily, it should be observed
firsthand in order to identify the position of the arm, the amount of
needed effort, and the direction of dislocation. In addition, these
patients should be queried for any associated neurologic signs such as
weakness, numbness, and tingling sensations.
challenging. Some of the findings may be subtle, and the ultimate
diagnosis may be difficult to establish. In patients who have suffered
a recent instability episode, associated symptoms may be severe enough
to preclude an adequate examination. For these patients, a basic
examination to document glenohumeral joint reduction and neurologic
status may be all that can be accomplished during the initial visit. If
so, they should be evaluated more thoroughly at a later date when
majority of the pain has subsided. A detailed neurologic examination of
the upper extremity must be performed and documented during all
clinical evaluations.
inspection. Any abnormalities such as asymmetry, muscular atrophy,
localized edema, or ecchymosis should be noted. This is usually
followed by manual palpation for localized tenderness and bony defects.
Range of motion of the affected shoulder should be obtained and
compared with the contralateral shoulder. In addition, differences
between active and passive range of motion should be noted. If
possible, the etiology of this difference, whether caused by pain,
weakness, or both, should be determined. General strength testing is
performed with specific maneuvers to identify rotator cuff weakness.
This is particularly important for an older individual, because the
association between
rotator cuff tears and shoulder dislocations increases significantly with age.191
Findings consistent with a generalized systemic laxity are also noted.
These include elbow hyperextension, hyperflexion of the wrist (thumb to
forearm maneuver), hyperextension of the metacarpophalangeal joints,
and knee hyperextension (Fig. 38-6).
Provocative maneuvers for shoulder instability are typically reserved
for the end of the examination as they may reproduce the clinical
symptoms of pain and apprehension. For most techniques, the maneuver
should be performed bilaterally to compare and contrast the symptomatic
shoulder with the asymptomatic shoulder.
 |
|
FIGURE 38-4 Locked inferior dislocation of the glenohumeral joint, also known as luxatio erecta.
With hyperabduction of the arm, the lateral acromion acts as a lever against the proximal humerus to dislocate the shoulder inferiorly (A). After dislocation, the humeral head is locked inferior to the glenoid rim (B). In these patients the rotator cuff tendons are typically detached from the humeral head, and there may also be an associated fracture of the greater tuberosity. |
 |
|
FIGURE 38-5
Technique for testing axillary nerve function. With the arm adducted and stabilized by the examiner, the patient is asked to actively abduct the arm. The motor component (A) of the axillary nerve is documented by observing or palpating deltoid muscle contraction. The sensory component (B) of the axillary nerve is documented by testing the sensation to the lateral aspect of the upper arm. |
 |
|
FIGURE 38-6 A-D. Examples of patients with generalized ligamentous laxity.
|
is the “drawer” test. This maneuver can be performed either with the
patient in the sitting or supine position. It can be used to assess
both anterior and posterior instability. It has been suggested that
this maneuver is most reliable if the arm is held in 80 to 120 degrees
of abduction, 0 to 20 degrees of forward flexion, and 0 to 30 degrees
of external rotation.8 If the
patient is supine, the entire shoulder should be off the table to allow
free access to the shoulder girdle. While the shoulder girdle is
manually stabilized with one hand, the other hand manipulates the
humeral head for anterior translation (Fig. 38-7).
For normal shoulders this translation should be smooth with a firm
endpoint. If the translation is excessive in comparison with the
contralateral shoulder, or if the maneuver reproduces the clinical
symptoms of apprehension or pain, a presumed diagnosis of anterior
instability can be established. This is a reliable test when the
patient is able to relax the shoulder muscle sufficiently and allow the
maneuver to be performed without tension.55
In addition to anterior instability, the same maneuver can also be
adjusted to test for posterior instability. This is accomplished by
manually translating the humeral head posteriorly. Again, posterior
instability is suspected if the maneuver reproduces pain or
apprehension. In this fashion, the “drawer” test can be used to test
for instability in multiple directions.
Unlike the “drawer” test, the arm is placed in 20 degrees of abduction
and 20 degrees of forward flexion. Rotation is maintained at neutral,
and longitudinal pressure is applied to the humeral head in order to
load the glenohumeral joint. Similar to the “drawer” test, the humeral
head is then grasped and translated in either the anterior or posterior
direction to assess for laxity and pain.8
laxity, the “sulcus” test is often positive in many patients with
multidirectional instability (Fig. 38-8).187
This maneuver is performed in the sitting position with the shoulder
fully adducted. By manually placing downward traction on the arm,
inferior translation of the humeral head is created. Significant
translation will produce a noticeable “dimple” or “sulcus” at the
lateral edge of the acromion. By placing the shoulder in external
rotation, the sulcus test can also be used to estimate the integrity of
the rotator interval structures such as the coracohumeral ligament and
the superior glenohumeral ligament. External rotation of the shoulder
should place these structures under tension and allow them to act as a
restraint to inferior translation. As such, a positive sulcus sign with
the shoulder in external rotation would suggest excessive laxity within
the structures of the rotator interval.8
to cause the feeling of imminent dislocation (apprehension) in patients
as their shoulder is placed in a position that is vulnerable to
dislocation. The patient is placed in the supine position with the
shoulder slightly off of the table. The shoulder is then positioned in
90 to 100 degrees of abduction and neutral rotation. From this point,
the shoulder is externally rotated until it reaches its maximal limit
or until the feeling of apprehension is reported by the patient (Fig. 38-9A).
Some patients may report pain instead of apprehension. Although pain
may be used as an indicator for instability, it is typically not as
specific or as reliable as apprehension in documenting anterior
instability.55,155
Modifications of this maneuver that try to either exaggerate or
diminish the instability have also been described. As such, the
“fulcrum” (Fig. 38-9B) and the “crank” test (Fig. 38-10)
are similar to the “apprehension” test, but an anteriorly directed
force is placed on the posterior aspect of the shoulder to exaggerate
the instability. In contrast, in the “relocation test,” a posteriorly
directed force is placed on the anterior aspect of the shoulder to
eliminate the feeling of apprehension (Fig. 38-11).
Finally, the “surprise” test is another variation of the apprehension
test where the examination starts with a posteriorly directed force on
the anterior shoulder. As this force is manually stabilizing the
glenohumeral joint, the patient does not experience apprehension even
when the shoulder is placed in abduction and maximal external rotation.
By abruptly removing this force, the patient will suddenly experience
apprehension or pain. Although all these maneuvers can detect anterior
instability, a recent study has suggested that the surprise test may be
the most accurate.155
 |
|
FIGURE 38-7
The drawer test. While stabilizing the scapula with one hand, the other hand grasps the humeral head. A gentle pressure is then applied toward the center of the glenoid. At the same time, the humeral head is manually translated in the anterior and in the posterior direction. |
 |
|
FIGURE 38-8
The sulcus test for inferior instability of the shoulder. With the patient in the sitting position, a downward traction is placed on the adducted arm (A). With a positive test (B), excessive inferior translation produces a dimple (arrow) on the lateral aspect of the acromion. By performing this test with the arm in external rotation, the maneuver can also be used to test the integrity of the rotator interval structures. |
 |
|
FIGURE 38-9
The apprehension and the fulcrum tests for anterior instability. In the apprehension test, the shoulder is abducted and externally rotated such that it is in a position vulnerable to dislocation with the patient in supine position (A). Symptomatic patients will report the sensation of apprehension or “getting ready to dislocate.” In the fulcrum test, this sensation of instability is accentuated by placing an anteriorly directed force on the posterior humeral head (B). |
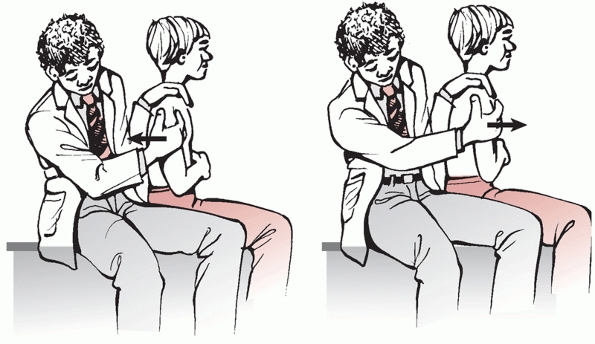
instability, the “jerk” test is a provocative maneuver for posterior
glenohumeral instability (Fig. 38-12).133
This maneuver can be carried out with the patient in either the sitting
or supine position. Again, if the patient is in the supine position,
the shoulder should be slightly off the table. After elevating the
shoulder to 90 degrees in the plane of the scapula, an axial load is
placed on the humerus such that the humeral head is compressed against
the glenoid. This can be easily accomplished by pushing axially against
the flexed elbow. By gradually adducting the shoulder, the humeral head
may subluxate or even dislocate posteriorly and produce a sudden jerk.
When the shoulder is taken out of adduction, the humeral head will
abruptly reduce back onto the glenoid and produce another jerk. The
findings from this test can be quite dramatic in patients with
posterior instability. Because of guarding, however, a positive finding
may be difficult to elicit in an awake patient. As such, instead of the
jerk, the test can also be considered positive if the maneuver elicits
the sensations of apprehension or pain.
voluntary or involuntary guarding may compromise the reliability of the
examination. If a clear diagnosis of instability cannot be established,
examination under anesthesia should be considered in select cases.
After adequate anesthesia and sedation, patients are unable to guard
against instability and the same provocative maneuvers can be performed
in a controlled environment. In addition, even with an established
diagnosis, examination under anesthesia should always be performed
prior to initiating any surgical procedure in order to confirm the
diagnosis.
 |
|
FIGURE 38-10
The crank test for anterior instability. The shoulder is abducted and externally rotated such that it is in a position vulnerable to anterior dislocation with the patient in sitting position. With an anteriorly directed force on the posterior humeral head, the instability is accentuated to cause the sensation of apprehension or “getting ready to dislocate.” |
 |
|
FIGURE 38-11
The relocation test for anterior instability. With the patient supine, the shoulder is abducted and externally rotated such that it is in a position vulnerable to dislocation (A). With a positive relocation test, the apprehension is reduced with a posteriorly directed force on the shoulder (B). |
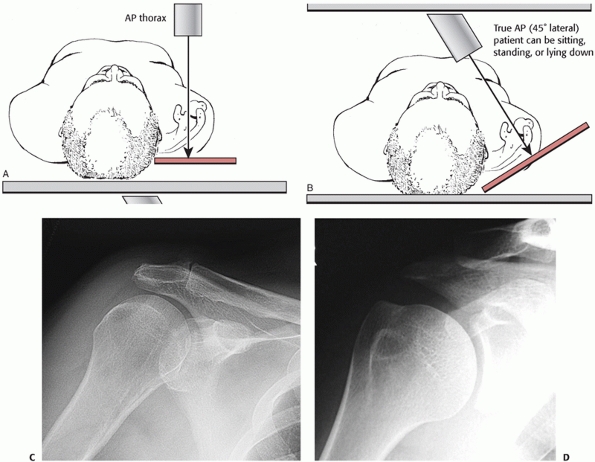
routine radiographs should be obtained to assess the direction of the
instability and to identify any associated fractures or bony defects.
Because of the oblique position of the scapula on the thorax, a routine
anteroposterior (AP) radiograph will display the glenoid fossa as an
ellipse (Fig. 38-13A). Therefore, in normal
shoulders, the articular surface of the humeral head will overlap this
elliptical shadow of the glenoid. A dislocated glenohumeral joint is
suggested when this overlap is significantly altered. As such, a
distance between the anterior glenoid rim and the humeral head that is
greater than 6 millimeters is highly suggestive of a posterior shoulder
dislocation, and is referred to as a “positive rim” or as a “vacant
glenoid” sign.6,231 A “true” AP radiograph of the shoulder is obtained when the x-ray beam is perpendicular to the plane of the scapula (Figure 38-13B).231
Thus the x-ray beam is angled 35 to 45 degrees oblique to the sagittal
plane of the body. In this view, the glenohumeral joint is profiled so
that there is no overlap between the glenoid and the
humeral
head. In normal shoulders a concave contour of the glenoid fossa should
match the convex articular surface of the humeral head. If any overlap
between the glenoid and the humeral head is identified in this view,
dislocation should be suspected.
 |
|
FIGURE 38-12 The jerk test for posterior instability. With the patient in either sitting (A) or supine (B)
position, the arm is abducted and internally rotated. An axial load is then placed on the humerus while the arm is moved horizontally across the body. With a positive test, a sudden jerk occurs when the humeral head slides off of the back of the glenoid and when it is reduced back onto the glenoid. |
 |
|
FIGURE 38-13 Technique for obtaining AP thorax (A) and true AP (B)
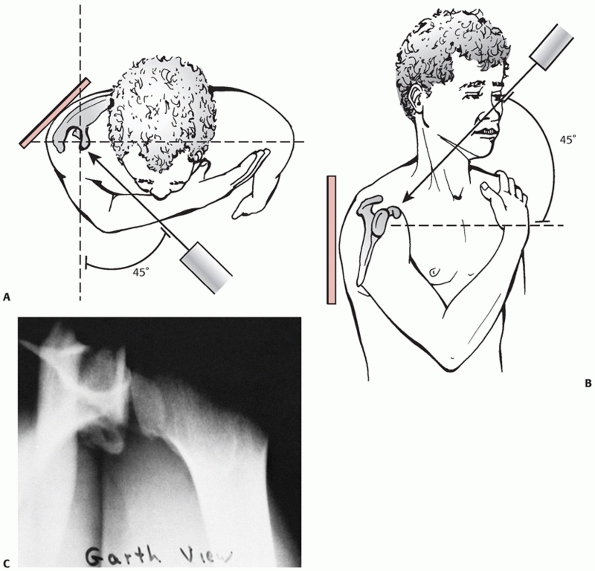
radiographs of the shoulder. In an AP view, the radiograph actually represents an oblique view of the shoulder joint. In a true AP view, the x-ray beam is parallel to the joint so that there is minimal overlap between the humeral head and the glenoid surface. The radiographic views of the shoulder AP (C) and shoulder true AP (D) are demonstrated. |
shoulder must be accompanied by another orthogonal view to document the
location of the humeral head. An axillary view radiograph is preferable
because it can readily display the location of the humeral head
relative to the glenoid, as well as allowing clear visualization of the
bony anatomy. This radiograph is obtained by placing the cassette on
the superior aspect of the shoulder while directing the x-ray beam
between the thorax and the abducted arm (Fig. 38-14A).145
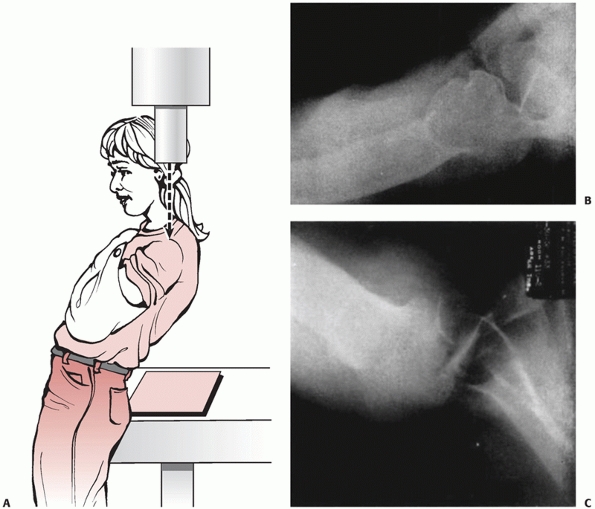
For patients who cannot abduct the arm, two additional techniques have
also been described. These modified radiographs, called the trauma
axillary lateral view (Fig. 38-14B) and the Velpeau axillary lateral view (Fig. 38-15), require minimal abduction of the arm and provide comparable views of the shoulder.18
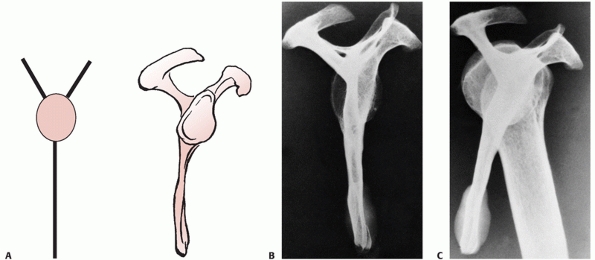
obtained, a scapula lateral view radiograph may also display the
location of the humeral head.170,231
This radiograph is obtained by placing the cassette on the lateral
aspect of the shoulder and directing the x-ray beam parallel to the
spine of the scapula (Fig. 38-16). This view is orthogonal to the “true” AP view of the scapula, and outlines the scapula as the letter “Y” (Fig. 38-17A).
Hence, the scapula lateral view is sometimes referred to as the scapula
“Y” view. The two upper limbs of the letter Y represent the scapula
spine and the coracoid process, respectively, whereas the inferior limb
of the Y represents the scapula body. The glenoid fossa is located in
the center of the Y where all the limbs intersect (Figure 38-17B). Therefore, the humeral head should reside within this central portion of the Y in normal shoulders (Figure 38-17C).
In addition to the scapula lateral view, another lateral radiograph
that can be obtained is the transthoracic lateral view. For this view
the x-ray beam is directed through the thoracic cavity and projected
onto a cassette that is placed lateral to the shoulder. As expected,
this view is often difficult to interpret because of the presence of
other anatomic structures. Hence it is typically not recommended for
evaluation of an unstable shoulder.
closely scrutinized for associated fractures and deformities. If other
structural defects are suspected, additional radiographs must be
obtained to fully characterize the injury. When a glenoid bony defect
is suspected, the West Point axillary view should be considered (Fig. 38-18).
This radiograph is taken with the patient in a prone position with the
involved shoulder slightly elevated on a pillow. With the cassette
placed on the superior aspect of the shoulder, the x-ray beam is
directed toward the axilla in a 25 degrees downward and a 25 degrees
inward direction. This radiograph provides a tangential view of the
anterior glenoid and can be quite useful in identifying anterior
glenoid rim fractures.235 Another radiograph that can be helpful in detecting glenoid defect is the apical oblique view.67
This radiograph is similar to the “true” AP view of the shoulder, but
the x-ray beam is angled approximately 45 degrees downward (Fig. 38-19). In this fashion, a tangential view of the anterior glenoid rim can be obtained for analysis.
 |
|
FIGURE 38-14 Techniques for obtaining axillary lateral (A) and trauma axillay lateral (B) view radiographs. The radiographic view of the axillary lateral (C) is demonstrated.
|
visualized on routine or “true” AP radiographs of the shoulder. Since a
Hill-Sachs lesion is located in the posterolateral aspect of the
humeral head, internal rotation of the shoulder should improve the
visualization of the defect on an AP radiograph. For further
characterization, a Stryker notch view can be considered (Fig. 38-20).82
For this radiograph, the patient is placed supine, and the arm is
forward flexed such that the elbow is directed over the face. The elbow
is usually flexed so the hand can rest on top of the head. The x-ray
beam is then angled approximately 10 degrees downward and projected
onto a cassette that is placed on the posterior aspect of the shoulder.
Studies have demonstrated that this view can greatly improve the
ability to identify and characterize a Hill Sachs lesion.82,240
(CT) scan should be considered. In fact, for the majority of
orthopaedic surgeons, CT scans have become the imaging modality of
choice for characterizing associated fractures. CT scan images can
provide details regarding the size and the extent of the bony defects.
In addition, with the recent advances in CT technology,
three-dimensional reconstructions of the shoulder can provide exquisite
details of the bony anatomy and identify defects that were previously
underappreciated.257
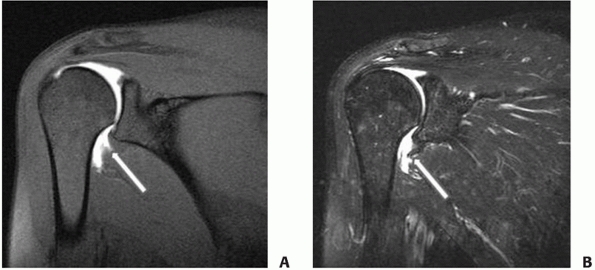
resonance imaging (MRI) is the modality of choice for assessing soft
tissue injuries. MRI provides high resolution images along different
body axes to fully illustrate the defect. Multiple authors have
reported on the usefulness of MRI for identifying rotator cuff tears as
well as labral defects. According to one study, MRI showed 100%
sensitivity and 95% specificity in the diagnosis of full thickness
rotator cuff tears. In addition, MRI demonstrated 88% sensitivity and
93% specificity in the diagnosis of labral pathology.111
A more recent study supported this finding as the authors observed 100%
agreement between the MRI readings and the arthroscopic findings for
the presence of an anterior
labral lesion as well as a Hill-Sachs lesion.134
Sensitivity of identifying intra-articular soft tissue lesions with an
MRI may be augmented by the injection of intra-articular contrast.
These studies, termed MR-arthrograms, can be very helpful in
delineating structural defects within the joint and can be a useful
adjunct for appropriate preoperative planning (Fig. 38-21).36,84,272
 |
|
FIGURE 38-15 A. Positioning of the patient for the Velpeau axillary lateral view radiograph. B. Note the posterior dislocation of the humeral head. C.
Note the posterior dislocation of the humeral head with reverse Hill-Sach lesion. (Part A modified with permission from Bloom and Obata. J Bone Joint Surg 1967;49-A: 943-949.) |
 |
|
FIGURE 38-16
Technique for obtaining a scapula lateral, also known as the “Y”, view radiograph. With the cassette placed on the anterior lateral aspect of the shoulder (A), the x-ray beam is directed parallel to the plane of the scapula (B). |
 |
|
FIGURE 38-17
Interpretation of the scapula lateral, also known as the “Y” view radiograph. The obtained view of the scapula is projected as the letter Y. As shown in the schematic (A), the lower limb represents the scapula body whereas the upper limbs represent the coracoid process and the scapular spine. Scapula lateral radiograph of a cadaveric scapula (B) highlights the fact that the glenoid surface lies in the middle of the letter Y. Therefore in these radiographs, the humeral head should lie directly over the glenoid in the middle of the Y (C). |
 |
|
FIGURE 38-18
West Point view for the identification of a glenoid rim lesion. This radiograph is taken with the patient in the prone position. The beam is angled approximately 25 degrees from the midsagittal plane (A) in order to provide a tangential view of the glenoid. In addition, the beam is angled 25 degrees downward (B) in order to highlight the anterior and posterior aspects of the glenoid. In this fashion, the entire glenoid rim can be clearly visualized (C). |
 |
|
FIGURE 38-19
Apical oblique view for the identification of a glenoid rim lesion. This radiograph is taken with the beam angled approximately 45 degrees (A) in order to provide a “true AP” view of the glenoid. In addition, the beam is angled 45 degrees downward (B) in order to highlight the anterior inferior aspect of the glenoid. As such, a bony defect in the anterior inferior aspect of the glenoid (C) can be easily visualized. (Modified with permission from Garth et al. J Bone Joint Surg 1984;66-A: 1450-1455.) |
 |
|
FIGURE 38-20
Stryker notch view for humeral head defects. The patient is in the supine position with the arm flexed to 120 degrees so that the hand can be placed on top of the head (A). The x-ray beam is then angled approximately 10 degrees. The radiograph (B) can clearly reveal the presence of any osseous defects (arrow). (Modified with permission from Hall et al. J Bone Joint Surg 1959;41:489-494.) |
 |
|
FIGURE 38-21 The humeral avulsion of the glenohumeral ligament, or HAGL Lesion. T1- (A) and T2-weighted (B) MRIs clearly demonstrate that the inferior glenohumeral ligament (arrow) is detached from the humeral neck.
|
In general, instability is classified based on severity (subluxation or
dislocation), duration (acute or chronic), occurrence (single or
recurrent), mechanism (traumatic or nontraumatic), and direction
(anterior, posterior, or multidirectional). Because these
classifications are mostly descriptive, multiple terms can be applied
to a single patient. For example, glenohumeral instability in a patient
may be described as an acute traumatic anterior dislocation or as a
recurrent nontraumatic posterior subluxation.
the humeral head against the glenoid without a complete separation of
the articular surfaces. As such, the joint will spontaneously reduce
back to its anatomic position when the distracting force is no longer
present. A certain amount of humeral head translation is expected
during normal glenohumeral motion and thus, a precise definition for
subluxation is difficult to establish. Nevertheless, excessive
translation that causes symptoms of apprehension and pain should be
considered abnormal. In contrast, glenohumeral dislocation is defined
as excessive translation of the humeral head that results in complete
separation of the articular surfaces. In these instances, even after
the distracting force is eliminated, the joint will not spontaneously
reduce back to its anatomic position. In rare cases, some patients
suffer from instability patterns that cannot be classified into either
of these two categories. Such is the case when the humeral head
translates against the glenoid surface and remains “perched” on the
glenoid rim. Configuration of the deformity is stable so that no change
will occur when the distracting force is eliminated. With minimal
additional force, however, the humeral head can either completely
dislocate or return back to its anatomic position. As such, this state
of instability cannot be easily defined as either a subluxation or a
dislocation.
|
TABLE 38-1 Classifications of Shoulder Instability
|
||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||
if the condition has occurred within 24 to 36 hours of the initial
medical evaluation. An attempt at closed reduction is more likely to be
successful for an acute dislocation than a chronic dislocation. Thus,
chronic dislocations, especially those greater than 4 weeks, are highly
unlikely to be reduced in a closed manner.74
If a patient has suffered multiple instability episodes, the
instability is considered to be recurrent. This definition applies to
both dislocations and subluxations.
dislocation has occurred. In patients with anterior dislocations, the
humeral head is often located inferior to the coracoid process. In
addition to these subcoracoid dislocations, other anterior shoulder
dislocations such as subglenoid, subclavicular, and intrathoracic have
also been described.45,72,244
In patients with less severe instability, the direction of instability
may be subtle and more difficult to identify. Some patients may exhibit
unidirectional instability in anterior, posterior, or inferior
direction only. Others, however, may have generalized ligamentous
laxity that results in multidirectional instability.188
Although it may be difficult to establish, clear identification of the
instability pattern is crucial to the formation of an appropriate
treatment plan.
revised the comprehensive classification system for fractures and
dislocations (Fig. 38-22) originally published
in 1996.161 This system can be applied to shoulder dislocations by
utilizing a two digit numerical identifier of “10.” The first digit of
“1” specifies the shoulder girdle whereas the second digit of “0”
specifies dislocation. Then, a letter is used to identify the specific
joint (“A” = glenohumeral, “B” = sternoclavicular, “C” =
acromioclavicular, “D” = scapulothoracic), followed by another number
to describe the direction (“1” = anterior, “2” = posterior, “3” =
lateral, “4” = medial, “5” = other). Thus, for example, an anterior
glenohumeral dislocation would be classified as “10-A1” using the OTA
classification system. Although
this
system provides a simple method to describe a dislocation, it does not
provide other relevant information regarding shoulder instability such
as severity, duration, recurrence, and mechanism.
 |
|
FIGURE 38-22
The Orthopaedic Trauma Association Classification for glenohumeral dislocations. The numeral “10” signifies the shoulder dislocation and the letter “A” specifies the glenohumeral joint. Anterior Dislocation is classified as 10-A1 (A,B). Posterior Dislocation is classified as 10-A2 (C,D). Lateral Dislocation, 10-A3 is theoretical and not seen clinically. Medial Dislocation classified as 10-A4, is also theoretical and not seen clinically. Inferior Dislocation, also known as luxatio erecta, is classified as 10-A5 (E,F). |
as a fulcrum for the use of the upper extremity in three-dimensional
space. A critical element of establishing this fulcrum is the presence
of a stable glenohumeral joint. Stability of the joint, in turn, is
provided by various bony and soft tissue structures. Anatomic
constraints to shoulder motion and translation are referred to as
static stabilizers. In contrast, structures whose normal physiologic
action creates a stabilizing effect on the shoulder are referred to as
dynamic stabilizers. Ultimately, stability of the glenohumeral joint is
the result of a complex interplay among these static and dynamic
stabilizers.
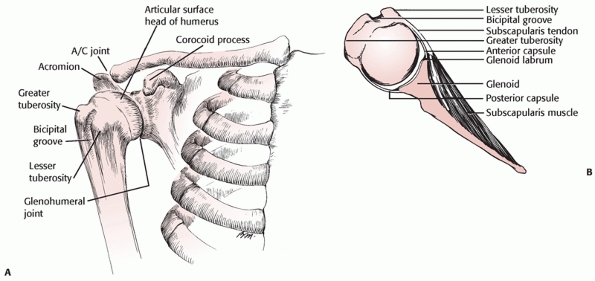
Notable parts of the scapula include the body, the spine, the acromion,
the glenoid, and the coracoid process (Fig. 38-23A).
Parts of the scapula articulate with the distal clavicle and the
humeral head to form the acromioclavicular and the glenohumeral joints,
respectively. The scapula rests on the posterior aspect of the thoracic
cage and is stabilized by the periscapular musculature. The glenoid
surface is located on the lateral aspect of the scapula such that its
surface has a slightly superior inclination relative to the vertical
axis of the body. This inclination has been shown to play an important
role in augmenting inferior stability of the glenohumeral joint.115
In addition, the scapula is anteverted 30 to 40 degrees in respect to
the coronal axis of the body, whereas the glenoid surface is roughly
orthogonal to the plane of the scapula.37
Therefore, the glenoid surface is anteverted 30 to 40 degrees and faces
anterolaterally in respect to the coronal axis of the human body. This
glenoid anteversion, in turn, is matched by the retroversion of the
humeral head. With the humerus in neutral rotation (i.e., the forearm
pointing forward in respect to the body), the humeral head faces
posteromedially. In this fashion, the perpendicular axis of the humeral
head corresponds to the perpendicular axis of the glenoid fossa in
normal shoulders (Figure 38-23B).
be elliptical, with a vertical diameter that is greater than its
horizontal diameter. Unlike a typical symmetric ellipse, the inferior
glenoid
surface has a slightly greater horizontal dimension than the superior
glenoid surface. In fact, the inferior 2/3 of the glenoid roughly
approximates a circle, whereas the overall glenoid surface is “pear
shaped.”108
The size of the humeral head can vary widely between individuals;
however, there appears to be a direct correlation between height and
the diameter of the humeral head such that a taller person typically
has a larger humeral head.110
Morphology of the humeral head is nearly spherical in shape, but the
articular cartilage has variable thickness along different axes. Thus,
the peripheral contour of its articular surface is also slightly
elliptical.110
 |
|
FIGURE 38-23 Coronal (A) and axial (B) views of the shoulder bony anatomy.
|
fossa has been intensely scrutinized and found to be very precise. For
most shoulder movements, the center of the humeral head is located
within 1 millimeter from the central axis of the glenoid cavity.105
This is somewhat surprising because the overall size of the humeral
head is significantly greater than that of the glenoid. As such, at any
given position, the majority of the humeral head does not contact the
glenoid and remain “uncovered.”
surface also does not correspond to that of the humeral head. On
average, the radius of curvature of the glenoid is greater (less
curved) by 2.3 millimeters.110
Although this mismatch in size and radius of curvature may produce
decreased joint stability, it also prevents impingement of the proximal
humerus against the periphery of the glenoid. The end result,
therefore, is increased range of shoulder motion.
inherent constraints that allow for a large range of motion. The
majority of glenohumeral stability, therefore, is provided by the
various soft tissue structures that surround the joint. One of the most
important of these stabilizing structures is the glenoid labrum. The
labrum is a dense fibrous tissue which circumferentially surrounds the
glenoid. It is contiguous with the glenoid rim and interacts with the
glenohumeral ligaments and the intra-articular synovium (Fig. 38-24). The importance of the labral tissue to the overall joint stability has been well described in the literature.11,12,146
Correlation between traumatic anterior shoulder dislocations and an
anteroinferior labral defect is extremely high. As such, this labral
defect has been termed the “essential lesion.”11,12
mechanism by which the labrum confers stability to the glenohumeral
joint is somewhat unclear. The anterior labrum may augment stability of
the joint by providing a secure attachment site for the glenohumeral
ligaments. Some earlier studies demonstrated that if the ligament
attachment sites can be maintained, excision of the labrum did not seem
to affect glenohumeral stability.219,269
Anatomically, the labrum effectively enlarges and deepens the glenoid
surface by 1 centimeter and 50%, respectively, and provides additional
surface to interact against the humeral head.104
Therefore, the labrum may provide stability to the joint by creating
additional surface for humeral head translation. Recent cadaveric
studies support this hypothesis as they demonstrated that if a labral
defect is created, the humeral head is no longer centered within the
glenoid fossa and the joint becomes increasingly unstable.57,146
glenohumeral capsule. The joint capsule is generally loose and
redundant at most shoulder positions. At extremes of motion, however,
the capsule tightens and provides stability to the joint. Thus,
depending on the position of the shoulder, certain portions of the
capsule will tighten and act as a restraint against humeral head
translation. Studies have confirmed that different parts of the
glenohumeral capsule can act as a primary or a secondary stabilizer
against shoulder dislocation in all directions.201,247
it maintains a stable and finite joint volume. In normal shoulders,
this finite volume provides stabilizing force on the joint, as
distracting the humeral head away from the glenoid will create a
relative vacuum within the capsule. In fact, physiologic
intra-articular pressure within the glenohumeral joint is slightly
negative.
Osmotic
action of the synovium is believed to remove free fluid from the joint,
thus creating a slightly negatively intra-articular joint pressure.149
When the capsule is vented and opened to the atmosphere, the force
necessary to translate the humeral head decreases significantly.71,81,139
The stabilizing force generated by the finite joint volume and the
associated negative intra-articular pressure may be as high as 146 N.
During a dislocation, the capsule undergoes a plastic deformation,
which may result in increased capsular volume.49 This static stabilizing force has been demonstrated to be diminished in patients with shoulder instability.81
 |
|
FIGURE 38-24 A.
Cross-sectional anatomy of a normal shoulder. Note the close relationship between the subscapularis tendon and the anterior capsule. B. A magnified view of the anterior joint shows that the labrum is essentially devoid of fibrocartilage and is composed of tissues from nearby hyaline cartilage, capsule, synovium, and periosteum. |
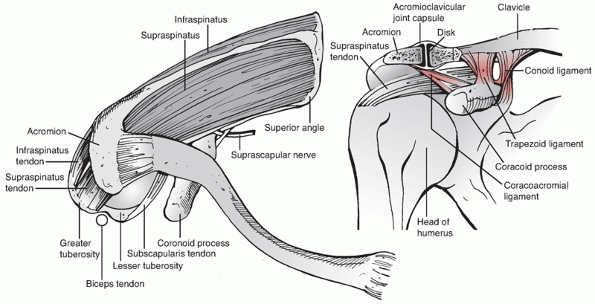
important static stabilizers of the glenohumeral joint. They include
the superior glenohumeral ligament, the middle glenohumeral ligament,
the inferior glenohumeral ligaments, and the coracohumeral ligament.
All three glenohumeral ligaments are intimately associated with the
joint capsule. In fact, these ligaments were once believed to be variable thickenings within the joint capsule.40
Multiple studies, however, have demonstrated that the glenohumeral
ligaments are consistently present and that they are clearly
distinguishable from the capsule.171,220
anterior superior aspect of the glenoid and extends to the anterior
aspect of the humeral head just superior to the lesser tuberosity.
Biomechanical studies have demonstrated that this ligament acts as the
primary restraint to inferior translation in the adducted shoulder, and
as a secondary restraint to posterior humeral head translation.247,277
The middle glenohumeral ligament has a variable origin as it can arise
from the supraglenoid tubercle, anterosuperior aspect of the labrum, or
the scapular neck. It can be quite dense and “cord-like” in some
patients but practically nonexistent in others.186
This ligament often becomes confluent with the tendon of the
subscapularis muscle and attaches to the inferior aspect of the lesser
tuberosity. In addition to acting as a secondary stabilizer against
anterior humeral head translation, the middle glenohumeral ligament
also appears to provide a restraint to excessive external rotation when
the shoulder is in approximately 45 degrees of abduction.247
The inferior glenohumeral ligament consists of three different
components: the superior band, the anterior axillary pouch, and the
posterior axillary pouch.197 This
ligament originates from the anteroinferior aspect of the labrum and
extends to the inferior aspect of the lesser tuberosity. The inferior
glenohumeral ligament complex has been compared to a hammock-like swing
that surrounds and supports the humeral head when the shoulder is
abducted.199 As such, this ligament
has been demonstrated to be the primary stabilizer against anterior and
posterior translation of the humeral head, as well as being a restraint
against excessive external rotation of the abducted shoulder.23,198,219
are compromised from their origin at the glenoid. It has also been
demonstrated, however, that the ligaments and the capsule may be
damaged in midsubstance or at their insertion in the humeral head.182,193 Both of these injuries may occur as an isolated entity or in conjunction with other lesions such as labral defects.224
coracohumeral ligament originates from outside the joint. It arises
from the lateral aspect of the coracoid process, passes within the
interval between the subscapularis and the supraspinatus tendons (i.e.,
the rotator interval), and attaches to the lesser and greater
tuberosities.124 This structure is
tight when the shoulder is adducted and becomes loose when the shoulder
is abducted. 13 Therefore, the coracohumeral ligament is believed to
prevent
excessive external rotation when the arm is adducted. In addition, this
ligament is also believed to stabilize the joint against inferior
subluxation when the arm is adducted.13,202
 |
|
FIGURE 38-25 The glenohumeral anatomy and ligaments.
|
Although these structures are generally considered to be dynamic
stabilizers of the glenohumeral joint, their tendons surround the joint
and often interdigitate with the joint capsule.39 Therefore, even without muscle contractions, they can also act as static stabilizers of the glenohumeral joint.
a displacing force across the glenohumeral joint. Contraction of the
anterior deltoid muscle, for example, produces a posteriorly directed
force on the humeral head. If left unbalanced, this force can create
posterior shoulder instability. To counteract these forces, the rotator
cuff muscles selectively contract to maintain the humeral head centered
within the glenoid fossa. Thus, the rotator cuff muscles counterbalance
the displacing forces created by the contractions of other shoulder
girdle muscles. In this fashion, they act to dynamically stabilize the
glenohumeral joint.141,186,259
contractions of the rotator cuff muscles also generate a medially
directed force on the humeral head. This results in compression of the
humeral head against the glenoid fossa, which in turn provides
additional joint stability. Dynamic stability conferred by joint
compression appears to be active throughout all shoulder motion.147,154,276 In fact, sufficient joint compression can even overcome the destabilizing effects of ligament sectioning and joint venting.276
Thus, dynamic stability provided by the rotator cuff muscles may be
able to compensate for the loss of other stabilizing structures.
supraglenoid tubercle, courses along the rotator interval, and exits
the glenohumeral joint into the bicipital groove of the humerus. The
physiologic role of the proximal biceps tendon has received much
attention, but remains somewhat controversial. Experimental studies
have shown that loading of the biceps tendon can decrease the tension
on the inferior glenohumeral ligament.233 Loading of the biceps tendon can also decrease humeral head translation in all directions, especially in the adducted shoulder.113,204
In fact, a cadaveric study demonstrated that loading of the biceps
tendon can prevent anterior shoulder dislocation even when the joint is
destabilized by venting or by creating a labral lesion.113
Thus, loading of the biceps tendon appears to provide a stabilizing
effect on the glenohumeral joint. Notably, a recent electromyographic
study demonstrated that when forearm position is controlled, the biceps
muscle remains electrically silent during all shoulder motion.152
This has led to the conclusion that, physiologically, the biceps tendon
may not be under any significant tension during normal shoulder motion.
Without significant loading, it is unclear whether the biceps tendon
confers any additional stability to the glenohumeral joint.
maintained within the confines of the coracoacromial arch. This arch is
formed by the coracoid process, the coracoacromial ligament, and the
acromion. These structural constraints limit the extent of
anterosuperior, superior, and posterosuperior translation of the
humeral head. In patients with a large rotator cuff tear, for example,
this arch often represents the last restraint to anterosuperior
glenohumeral dislocation. In normal shoulders with intact rotator cuff
tendons, there also appears to be contact and load transfer between the
coracoacromial arch and the rotator cuff tendons.62,290
Therefore, during normal shoulder motion, a downward force is exerted
by the coracoacromial arch, through the rotator cuff tendons, onto the
humeral head to limit superior translation.
In most patients, the surgical incision can be placed in line with the
axillary fold for improved cosmesis. After the skin incision and
subcutaneous dissection, the interval between the anterior deltoid and
the pectoralis major muscle is identified. This area, also referred to
as the deltopectoral interval, is outlined by the cephalic vein which
must be dissected and retracted away from the surgical field (Fig. 38-26B).
The cephalic vein is typically retracted laterally as most small
feeding vessels originate from the deltoid muscle. The underlying
clavipectoral fascia can then be incised to gain access to the shoulder
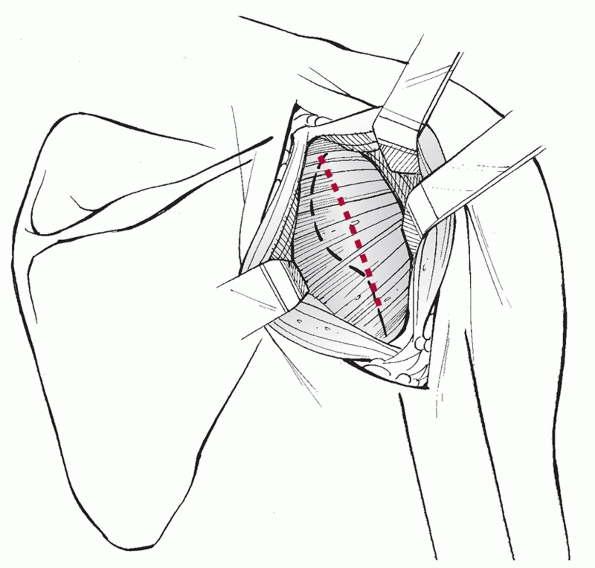
(Fig. 38-26C). The overlying subscapularis
tendon may be split in line with its fibers or it can be released just
medial to its insertion at the lesser tuberosity (Fig. 38-26D).
It must be stressed that rigid and anatomic repair of the subscapularis
tendon must be completed at the end of the procedure as good surgical
results correlate with subscapularis function.243 At this
point, the capsule is vertically incised to expose the joint and the anterior glenoid margin.
 |
|
FIGURE 38-26 Anterior approach to the shoulder. A. The incision extends from the coracoid to the axillary fold. B. The deltopectoral interval is identified and developed, taking the cephalic vein laterally with the deltoid. C. The conjoined tendon and subscapularis are identified. D. A subscapularis tenotomy is made vertically, separating the subscapularis tendon from the underlying capsule.
|
posterolateral corner of the acromion, extending to the axillary
crease. For access to the glenohumeral joint, traditional approaches
have released the deltoid muscle from its origin on the acromion.
Recent modifications of the approach, however, specifically avoid the
release of the deltoid origin. For most patients, adequate exposure can
be obtained by splitting the deltoid from the posterior acromion to the
upper border of the teres minor (Fig. 38-27). The theoretical advantage of this modification is the preservation of strength and function of the posterior deltoid.284
Once the rotator cuff tendons are exposed, the infraspinatus tendon can
be incised and reflected medially. Excessive medial reflection should
be avoided in order to prevent injury to the suprascapular nerve (Fig. 38-28).
In situations where the infraspinatus tendon is very lax, it may be
possible to simply retract the tendon superiorly instead of releasing
it. The teres minor muscle fibers are then retracted inferiorly to gain
exposure to the posterior capsule. Care must be taken when handling the
teres minor because the axillary nerve and the posterior humeral
circumflex vessels lie just inferior to this structure in the
quadrilateral space. Once the posterior capsule is isolated, it is
incised to expose the joint.
based on a multitude of factors. For every patient, the potential for
failing nonoperative therapy is considered against the risks of
surgical intervention and its anticipated outcome. As such,
nonoperative treatment is generally recommended for patients who should
respond successfully to rehabilitation and have a low likelihood of
developing symptomatic recurrent instability.
 |
|
FIGURE 38-27
The posterior approach to the shoulder. After the skin incision, the deltoid muscle can be split along its fibers from the acromion to the upper border of the teres minor. Underlying rotator cuff tendons can then be incised to gain access to the shoulder capsule and joint. |
 |
|
FIGURE 38-28
Anatomy of the suprascapular artery and nerve. During a posterior approach to the shoulder, excessive medial retraction of the rotator cuff tendons can damage these structures. |
dislocation, the overall rate of recurrent instability has been
reported to be between 26% and 48%.97,260
Recent 25-year follow-up data of 229 shoulders in 227 patients suggest
that 42% of patients with a first time dislocation never have another
event, whereas 7% have only one additional dislocation or subluxation
event.99 It has also been
demonstrated that various factors affect the likelihood of developing
recurrent instability. They include several patient-related factors
such as age, level of sporting or recreational activity, compliance,
and associated injuries. Of these, the single most important risk
factor for developing recurrent instability appears to be age. In
patients under 20 years of age, the incidence of recurrent dislocation
has been reported to be between 55% and 95%.95,172,173,236,260 In contrast, for patients older than 40 years of age, the reported rate of recurrent dislocation is less than 6%.173,237,260
One recent study reported a 3% recurrence rate at 25-year follow-up in
patients 30 to 40 years of age at the time of their initial dislocation.99
identified as an independent factor for developing recurrent
instability. As such, even in patients under 20 years of age, the rate
of recurrent instability in nonathletic patients was only 30%. In
contrast, in the same group of patients who did participate in athletic
activities, the recurrence rate reached 80%. Because of this relatively
high rate of recurrent instability after traumatic dislocation, for the
young and active patients nonoperative treatment should be recommended
with caution. To describe this group of patients, the acronym TUBS has been widely used (Table 38-2). This term represents patients who have been suffering from Traumatic Unidirectional instability that is often associated with a Bankart lesion, and whose treatment often requires Surgery.262
In the cadet population of patients at West Point, for example, there
is 85% to 92% rate of recurrent instability after an initial
dislocation.46,279 Therefore some authors have recommended immediate surgical stabilization of the shoulder in such high-risk patients.122,230
In contrast, however, other authors have found that surgical
stabilization is requested by only a minority of patients and
recommended against immediate surgery.242
|
TABLE 38-2 Acronyms for Types of Recurrent Shoulder Instability
|
||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||
bilateral shoulder instability, the onset of symptoms usually does not
include a traumatic incident. Generally, these patients demonstrate
signs of general systemic laxity, which in turn may also be associated
with “loose” shoulder ligaments and capsule. As such, the glenohumeral
ligaments may be incompetent, and predispose the patients to developing
symptomatic shoulder instability. By strengthening the dynamic
stabilizers, it should be possible to overcome the inherent
glenohumeral joint laxity. Thus, for example, one study noted that 80%
of patients with atraumatic shoulder instability were successfully
treated with a specific set of exercises to strengthen the shoulder
musculature.31 According to another
study, patients with unilateral instability, functional impairments,
and higher grades of laxity were unlikely to respond to therapy, and
patients who did respond to therapy typically demonstrated improvements
within three months of starting their rehabilitation.180
If physical rehabilitation does not provide adequate improvement,
however, these patients often require surgical tightening of the entire
shoulder capsule with the inferior capsular shift procedure. To
describe this group of patients, another popular acronym of AMBRI has been developed (Table 38-2). The term represents patients who have been suffering from Atraumatic Multidirectional glenohumeral instability that can be Bilateral, and whose condition should be treated with Rehabilitation or, if necessary, Inferior capsular shift.262
on an individual basis. The likelihood of developing recurrent
instability as well as the likelihood of successful nonoperative
management must be considered based on various patient related factors.
Thus, for example, treatment of a 21-year-old professional basketball
player with recurrent traumatic glenohumeral dislocations is likely to
involve a surgical procedure. On the other hand, initial treatment
recommendation for a 35-year-old recreational tennis player who suffers
from atraumatic multidirectional instability will primarily be
nonoperative, focusing on physical rehabilitation.
requires emergent care. The joint should be reduced to its anatomic
position as soon as possible, and a closed reduction should be
attempted for most patients. In the select patients with concomitant
proximal humerus fractures, however, reduction under anesthesia should
be considered. The likelihood of a successful closed reduction is
dependent on multiple factors, including the presence of muscle spasm,
duration of the dislocation, presence of interposing structures, and
the availability of adequate assistance.
during shoulder reduction, intravenous analgesic and sedation agents
are often used. Although these agents can be extremely valuable, their
use necessitates careful patient monitoring. In rare circumstances,
excessive sedation may even lead to a respiratory compromise that
requires formal airway protection. As such, administration of
intravenous agents typically requires the use of significant clinical
resources. Recently, some authors have reported that intra-articular
injection of lidocaine, rather than intravenous agents, can be used to
effectively control pain and muscle spasms during shoulder reduction.
They demonstrated that closed reduction after intra-articular lidocaine
injection had high rates of success, especially if the attempts were
performed within 5.5 hours after the dislocation.176
When compared with those who received intravenous agents, these
patients were also shown to spend less time in the emergency room and
incur less expense.176
intravenous analgesia, a closed reduction can be attempted. A number of
different reduction techniques and maneuvers have been described in the
literature.286 Some of the more
commonly utilized techniques are described below. All of these
techniques rely on appropriate positioning of the shoulder with gentle,
slow, and sustained traction on the arm. Sudden or forceful
manipulations are avoided because they can lead to significant
complications. If initial shoulder reduction is unsuccessful, the
degree of sedation and analgesia must be evaluated to ensure that
adequate muscle relaxation has been obtained. If closed reduction is
not successful, the patient should then be taken to the operating room
on an emergent basis for either closed or open reduction. Once closed
reduction is accomplished, anatomic reduction of the glenohumeral joint
must be confirmed with radiographs. In addition, postreduction
documentation of the neurovascular status must also be performed.
This method utilizes the concept of traction and countertraction to
distract the glenohumeral joint and is applicable for most shoulder
dislocations. If performed by a single person, countertraction can be
provided by a foot that is placed on the thorax just inferior to the
axilla. If assistance is available, countertraction can also be
provided by a sheet that is placed around the upper thorax and held
steady by an assistant (Fig. 38-29B). Against this countertraction, slow and steady traction is applied to the arm
to distract the humeral head away from the glenoid. Upon disengagement
of the humeral head from the glenoid rim, the traction is released, and
the joint is allowed to reduce back to its anatomic position. In some
instances, gentle rotation or manipulation of the humeral head may be
required to mobilize the humeral head.
 |
|
FIGURE 38-29 Techniques for closed shoulder reduction. The Hippocratic method (A)
utilizes a downward traction on the arm against the countertraction provided by the foot on the thorax. Care must be taken to avoid placing the foot in the axilla as it can cause damage to the underlying neurovascular structures. A modification of this technique (B) uses a hand-held sheet around the thorax to provide countertraction. |
Following its original description, this technique has undergone a few
modifications. The patient is placed in prone position with the
affected arm hanging free over a table (Fig. 38-30).
In this manner, the table provides a stable base against which a gentle
downward traction is placed on the arm. The traction can be applied
manually or by attaching weights to the wrist. Typically, 5 pounds is
sufficient for most patients. Depending on the size of the patient,
however, the amount of weight can be varied accordingly. By applying
this traction for a period of time (10 to 20 minutes), the shoulder
musculature will fatigue and allow sufficient relaxation for humeral
head disengagement. The traction is then released, and the joint is
allowed to reduce back to its anatomic position.
Unlike some of the other maneuvers, this technique relies on shoulder
position rather than distraction. The maneuver can be performed with
the patient in either supine or prone position. Upon administration of
analgesia and moderate traction, the arm is abducted and externally
rotated. The dislocated humeral head is then manually manipulated back
into the joint. Various authors have reported that this method is
associated with a high rate of success and with minimal complications.142,241
radiographs, the arm should be immobilized for a period of time.
Although most surgeons agree that a brief period of immobilization
is
required for patient comfort and protection, the exact protocol for
immobilization is still controversial. Thus recommendations regarding
the type, duration, and position of immobilization have yet to be
firmly established.
 |
|
FIGURE 38-30
The Stimson technique for closed shoulder reduction. With the patient prone, weight is hung from the wrist to distract the shoulder joint. Eventually, with sufficient fatigue in the shoulder musculature, the joint easily reduces. |
Velpeau dressing, which includes a sling and a swath, does not appear
to alter the subsequent development of recurrent instability.52
Therefore, since more rigid orthoses tend to be quite cumbersome, a
simple sling is preferred for most patients. As for the duration of
immobilization, some series have reported no correlation between the
duration of immobilization and the development of recurrent instability.98,172
In a prospective randomized study, for example, Hovelius and colleagues
showed that the type and duration of initial immobilization had no
affect on the development of recurrent instability.97
In contrast, other studies have reported decreased rates of recurrent
instability in patients whose shoulders were immobilized for a short
period of time. For example, one study showed that patients who were
immobilized for more than 1 week demonstrated a significantly decreased
rate of recurrent instability in comparison with their nonimmobilized
counterparts.128 In other studies,
the incidence of recurrent instability in patients who were immobilized
for less than 3 weeks was nearly twice that of those who were
immobilized for 3 weeks or longer.136,256
One of these studies also demonstrated that the duration of
immobilization affected recurrent instability only in patients younger
than 30 years of age. For older patients immobilization had minimal
impact on recurrent instability.136 Therefore, age of the patient should also be considered when deciding on the duration of postreduction immobilization.
the position of immobilization has also received significant attention.
A simple sling places the shoulder in internal rotation. Some studies
have suggested that this position may not be optimal in preventing
recurrent instability. In patients who sustained a traumatic anterior
shoulder dislocation, position of the anterior labrum after reduction
appears to be more anatomic if the arm is positioned in slight external
rotation.116 This radiographic
observation has been supported by a clinical study which demonstrated
that, at a relatively short-term follow-up period of 15 months,
patients immobilized in external rotation did not develop recurrent
instability. In contrast, patients who were immobilized in the
traditional internally rotated position demonstrated a recurrent
dislocation rate of 30%.112 This
difference was even more striking for patients younger than 30 years of
age, as the rates of recurrent dislocation in the external and the
internal rotation groups were 45% and 0%, respectively.112
more recent studies have demonstrated no such advantage for
immobilization in external rotation. As such, a surgically created
Bankart lesion placed in external rotation did not demonstrate any
change in pressure between the glenoid and the capsulelabral complex.153
Also, a recent study directly compared sling immobilization against
external rotation immobilization after a primary dislocation event in
patients less than 35 years old. Over 2-year follow-up, no significant
difference was noted between the groups, with the sling group having
27% rate of recurrent instability and the external rotation group
having a 23% rate of recurrent instability.282
With seemingly contradictory data, it appears that the consequences of
immobilization in external rotation are incompletely understood.
Therefore, further studies are still needed to optimize the
postreduction immobilization protocol.
instability relies on the principles of immobilization, protection, and
rehabilitation. Immobilization allows for general recovery of the
shoulder from the traumatic incident. In addition, immobilization also
allows for the initial healing of the static stabilizers. As discussed
in the previous section, the optimal protocol for the position and
duration of immobilization has not been clearly defined.
protection. A brief period of immobilization is designed to protect the
shoulder from additional episodes of instability. Subsequent to this
initial phase, activity level of the patient must be modified to allow
for the healing of the static stabilizers. Activity patterns are
altered so that the shoulder is not placed in positions vulnerable to
dislocation. Typically, this is accomplished by limiting the range of
shoulder motion as well as refraining from participating in any
high-risk activities. Experiments in primates demonstrated that 3
months were required to restore normal collagen structural patterns in
the shoulder capsule, and that 4 to 5 months were required to restore
normal tensile strength.219 Therefore, this may provide a reasonable guideline for the period of protection.
rehabilitation. Dynamic stabilizers are strengthened to provide
additional stability for the compromised joint. Compression of the
glenohumeral joint by the rotator cuff muscles, for example, can
overcome the destabilizing effects of ligament sectioning and joint
venting.276 As such, muscle
rehabilitation may be able to compensate for the loss of some static
stabilizers. Specific protocols for rehabilitation of the shoulder can
vary; however, most protocols concentrate on strengthening the rotator
cuff as well as the deltoid muscles.31,286
In addition, some authors have also stressed the importance of
strengthening the periscapular musculature, as they allow the scapula
to function as a stable platform for shoulder motion.31,73
shoulder instability can vary widely, depending on a multitude of
factors. For example, those with associated injuries such as rotator
cuff tear or a bony defect are less likely to be amenable to
nonoperative management. Misamore evaluated nonoperative treatment of
multi-directional instability and found that patients who were likely
to improve with therapy did so within 3 months of initiating a therapy
program. Patients who had unilateral symptoms, symptoms with activities
of daily living, and high grades of laxity were likely to fail
conservative treatment and require surgical intervention.180
In a long-term follow-up study, Hovelius recently noted that 42% of
patients treated with therapy had no recurrent instability, whereas an
additional 7% had only one additional dislocation.99
is generally recommended for patients who have the following
conditions: (i) failed appropriate nonoperative therapy, (ii) recurrent
dislocation at a young age, (iii) irreducible dislocation, (iv) open
dislocation, and (v) unstable joint reduction. In addition, even after
a first time dislocation, young patients who actively participate in
high-demand activities may also be considered for operative
treatment.
Again, although the general principles are clear, the exact indications
for surgery are relatively arbitrary, and the specific criteria will
likely vary among individual surgeons. In addition, patient
expectations may also vary, as some would prefer an early surgical
intervention rather than to continue with nonoperative management that
may not be successful.
made, a number of surgical options are available. They include
arthroscopic techniques, open techniques with soft tissue repair or
augmentation, and open techniques with bony augmentation.
Traditionally, open anterior shoulder stabilization procedures have
been the “gold standard,” with many studies reporting good to excellent
outcomes in the vast majority of patients. In comparison with these
open procedures, early reports of arthroscopic stabilization procedures
produced results that were notably inferior. With the development of
newer instruments and techniques, however, the results of arthroscopic
stabilizations have improved. As such, some recent studies of
arthroscopic stabilizations have reported outcomes that are nearly
equivalent to those after an open procedure.53,127,129
Therefore, provided that the surgery is performed with adequate
expertise, the choice between open and arthroscopic procedure may not
significantly affect the overall outcome.
stabilization include shorter operative time, shorter hospitalization,
decreased morbidity, lower incurred cost, less pain in the early
postoperative period, and decreased rate of postoperative complications
(Table 38-3).19,53,78,162
It should be noted, however, that the amount of time required for
adequate healing is not significantly altered with an arthroscopic
technique. Therefore, these patients still need an adequate period of
protection and rehabilitation similar to that after an open procedure.
would preferentially utilize open techniques. They include situations
where the procedure would involve isolation and fixation of a bony
fragment. As such, for cases with either a large Hill-Sachs lesion or a
substantial glenoid defect, open techniques are typically recommended.
Another pathology that may not be optimal for an arthroscopic repair is
the humeral avulsion of the glenohumeral ligament (HAGL lesion).
Finally, for many surgeons, open procedures are preferred for patients
whose anatomy has been altered because of deformity or previous surgery.177
the entire joint to clearly identify the structural defects.
Significant bony defects in the glenoid or the humeral head must be
documented, as their presence may require conversion to an open
procedure. According to some studies, a glenoid defect greater than 21%
to 30% of the surface area or a Hill-Sachs defect that engages the
anterior glenoid rim with abduction and external rotation is associated
with a high likelihood of recurrent instability.30,114,129
In addition, the labrum must be carefully examined for any damage, and
the capsule should be assessed for redundancy and notable defects. Some
surgeons have utilized the “drive thru” sign to describe a loose joint.206,209
This sign is positive if the arthroscope can be easily passed from the
posterior portal, through the joint, into the anteroinferior quadrant.
Unfortunately, although this sign is associated with shoulder laxity,
it is not specific for shoulder instability and its accuracy for
diagnosing shoulder instability is less than 50%.166
Upon completion of the diagnostic arthroscopy, the necessary portals
are established. Although surgical techniques vary among surgeons, most
tend to utilize the posterior portal for the arthroscope and anterior
portals for the instruments. If an anteroinferior capsulolabral lesion,
also known as the “Bankart” lesion, is identified, the defect must be
repaired (Fig. 38-31A). The medially displaced labrum should be mobilized and reattached to the glenoid rim in its anatomic position (Fig. 38-31B,C). This surgery is often referred to as the arthroscopic Bankart procedure.
|
TABLE 38-3 Advantages and Disadvantages of Arthroscopic Stabilization for Anterior Shoulder Instabilitya
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||
to reattach the labrum. Unfortunately, this technique was associated
with relatively high rates of complications (12%) and recurrent
instability (33%).48,120,143
Others have described an arthroscopically assisted transglenoid suture
technique to reattach the labrum. Although short-term follow-up data
indicated excellent results with this procedure in the majority of
patients, at a midterm follow-up of 2 to 8 years, the results
deteriorated with reported recurrent instability in 17% of the patients.168,266
More recently, arthroscopic stabilization techniques have utilized
suture anchors that can be placed at the anterior glenoid rim. These
anchors provide a stable base to reattach the capsulolabral complex.
Using suture anchors to address an isolated an anterior labral lesion
and mild capsular redundancy, various authors have reported good to
excellent results in the vast majority of patients, including those
with a “high demand” shoulder such as collegiate and professional
overhead athletes.34,53,130,214,222
With relatively short-term follow-up, these studies also reported very
low rates of recurrent instability between 0% and 10% for most patients
and 12.5% to 16.5% for high-demand “collision” athletes.34,53,130,164,265,355 At mid-term follow-up of 2 to 6 years, the rate of recurrent instability was still only 4% to 7%.129,144,230
Negative prognostic factors for arthroscopic anterior stabilization
include bone loss, inferior laxity or multidirectional instability, and
total number of anchors used in the repair being less than four.20
associated defects are noted in the capsule or the humeral attachments
of the ligaments, they must also be repaired as well. A midsubstance
tear in the capsule can occur in up to 4% of the cases and require an
anatomic repair for optimal results.182,226
Similar to the midsubstance tears, HAGL lesions can occur in 1% to 9%
of cases of recurrent shoulder instability and may be the defect
responsible for persistent instability after surgical stabilization.28,264,289
Although most surgeons would prefer repairing this defect using an open
technique, some authors have described an arthroscopic repair of the
lesion with early favorable outcome.137,228,253
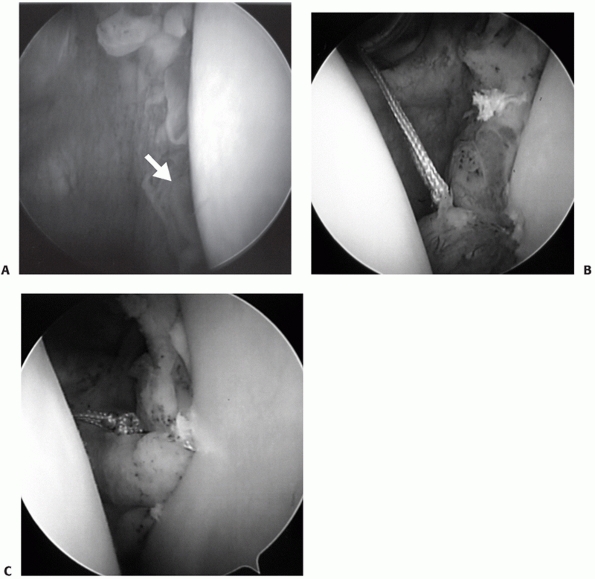 |
|
FIGURE 38-31 Intraoperative photographs of an arthroscopic Bankart procedure. Diagnostic arthroscopy (A) reveals detached and displaced labrum (arrow)
on the anterior inferior quadrant of the glenoid. Using suture anchors, the labrum is reattached to the glenoid rim starting at the most inferior position (B). This process is repeated until the labrum is completely restored to its original position on the glenoid rim (C). |
a number of surgeons have recently reported on their experience
performing arthroscopic surgeries on shoulders that were traditionally
addressed with open techniques. As such, patients who have previously
failed a surgical procedure have been stabilized with arthroscopic
methods with reasonable outcomes.22,189 Arthroscopic techniques have also been used to repair anterior glenoid bone defects associated with “bony Bankart” lesions.258
interval must also be scrutinized during any stabilization procedure.
Biomechanical studies have demonstrated that these structures
contribute to the stability of the humeral head against posterior
translation, inferior translation, and excessive external rotation.13,212,277,291 In addition, thermal shrinkage of the interval tissue has been shown to decrease anterior translation of the humeral head.249 Thus, defects within the rotator interval may contribute to instability in multiple directions.59,195 Several surgeons have described arthroscopic techniques for the evaluation and imbrication of the rotator interval tissue.69,126,212,270
For patients with clinical or arthroscopic findings consistent with an
interval defect, the rotator interval tissue should be imbricated. This
should be performed at least 1 cm lateral to theglenoid surface in
order to avoid tethering the coracohumeral ligament that can result in
loss of external rotation.212 In
patients who continue to demonstrate symptoms consistent with
instability without a prior dislocation, isolated interval closure may
lead to good and excellent outcomes.59
In the majority of the patients, however, rotator interval closure
represents a supplemental stabilization technique that is performed in
conjunction with repair of other lesions.291
requires significant surgical expertise. In order to simplify the
procedure, an arthroscopic technique called thermal capsulorrhaphy was
developed. By applying a source of heat, from either a laser or a
radiofrequency probe, the capsular tissue can be caused to contract.54,261 The end result of the process is to decrease capsular redundancy, decrease joint volume, and reduce glenohumeral translation.274
Initial enthusiasm for thermal capsular shrinkage was due, in part, to
the fact that the technology can be applied to all parts of the
glenohumeral capsule and required less surgical expertise than other
arthroscopic procedures. Hence even surgeons without extensive
arthroscopic experience were able to use this technology to treat
patients with shoulder instability. Unfortunately, however, the
procedure has been associated with unpredictable outcomes.178 Some authors have reported good to excellent clinical outcomes after a relatively short follow-up period.181,223 Even for overhead athletes, good to excellent results were obtained in 88% of
the patients.223 In contrast, other authors have reported clearly inferior results with recurrent instability in 24% to 47% of the patients.43,88,179,207 According to one prospective study, an unsatisfactory outcome was documented in 37% of the patients.43 In addition, anatomic studies have raised concerns regarding possible thermal damage to the nearby axillary nerve.80,165
Clinical studies have substantiated these concerns. In one study
axillary nerve neuropathy was observed in 21% of the patients who were
treated with thermal capsulorrhaphy.179 In addition, significant capsular thinning or necrosis may also result, requiring soft tissue grafting.3,178,207 Other noteworthy complications of this procedure include excessive stiffness as well as extensive chondrolysis (Fig. 38-32).38,88,117,151,179
Because of these issues, thermal capsulorrhaphy has experienced a
significant decline in popularity. Thus, although this technology may
play a role in augmenting other stabilization constructs, most authors
do not recommend its use as the primary procedure for shoulder
stabilization.88
to treat patients with anterior glenohumeral instability, the open
Bankart procedure is perhaps the most commonly performed surgery. In
this procedure, the anterior labral defect is identified, mobilized,
and then reattached to its original anatomic site on the anterior
inferior glenoid rim.11,12
Reattachment of the labrum to the glenoid rim can be achieved using a
number of different methods. In the original description by Bankart,
drill holes in the glenoid were utilized. He reported no recurrent
dislocations in 27 consecutive patients who were treated with this
technique.12 Other authors,
utilizing the same technique, were also able to duplicate this success.
The reported rate of recurrent dislocation after this procedure is
roughly 2% with good to excellent results in the vast majority of
patients.103,225
Recently, instead of drill holes, surgeons have utilized suture anchors
to reattach the labrum. Using this technique, good to excellent results
have been reported in 88% to 94% of the patients, with recurrent
dislocations in only 0% to 9.7% of the patients at short- to midterm
follow-up.* With a long-term follow-up at 29 years,
recurrent instability rate after this procedure was still low at 10%.
Joint arthrosis was noted in surprisingly high 40% of the patients, but
symptomatic in only 16.6% of the patients. Overall, despite the joint
arthrosis, 100% of patients were satisfied with the surgery.208
 |
|
FIGURE 38-32
Iatrogenic complication of thermal capsulorrhaphy resulting in endstage arthrosis of the shoulder. Approximately 6 months after the procedure, an AP radiograph (A) and MRI (B) of the shoulder reveal a complete loss of articular cartilage that is later confirmed during the intraoperative examination (C). (Copyright JP Iannotti, MD, PhD.) |
have also recommended reduction of the capsular redundancy. Termed the
“capsulolabral reconstruction,” this technique utilizes a similar
surgical approach to correct the pathoanatomic changes in both the
labrum and the capsule.118,140,183 After
standard anterior exposure, the capsule is isolated from the
subscapularis. At this point a “T”-shaped incision is made on the
capsule which includes both a horizontal and a vertical incision (Fig. 38-33).
The vertical incision can be placed laterally near the humeral head or
medially next to the glenoid rim depending on the specific technique to
be performed. With the additional horizontal incision, two separate
flaps of capsule, one superior and one inferior, are created. If a
labral defect is present, it is repaired as described previously. The
two flaps of the capsule are then imbricated onto each other by
shifting the inferior flap superiorly and the superior flap inferiorly.
In this fashion, parts of the capsule are overlapped on each other, and
the overall capsular volume can be significantly reduced. It should be
emphasized that the capsular plication is performed only to remove the
redundancy in the tissue. Excessive anterior capsular tightening can
alter the biomechanical characteristics of the joint, including
increased posterior humeral head translation and increased joint
contact forces with arm elevation, which in turn may lead to premature
joint arthrosis.275 Using this
technique, various authors have reported good to excellent outcomes in
the vast majority of patients with extremely low rates of recurrent
dislocation. Even in patients with high functional demands, this
procedure has been associated with good to excellent results in 92% to
96% of the patients, with recurrent dislocation in only 0% to 4% of the
patients.118,121,183,205
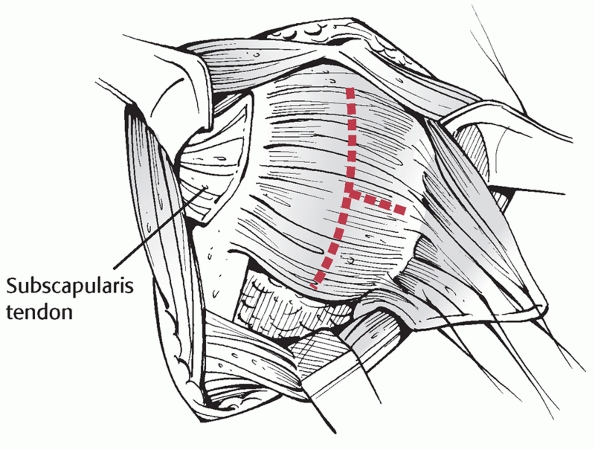 |
|
FIGURE 38-33 “T” capsular incision for anterior capsulorrhaphy.
|
is to restore the normal anatomy of the capsulolabral complex. The
subscapularis tendon is not imbricated during the procedure because it
is not a part of the pathoanatomy. Rather, it is usually repaired back
to its original length. In the Putti-Platt procedure, however, the
capsular defects are essentially ignored. Rather, the primary focus is
shifted to the subscapularis tendon, as it is divided at its midpoint
and imbricated upon itself.200 After
making a vertical incision 2 to 3 centimeters medial to the lesser
tuberosity, the lateral stump of the tendon is fixed to the glenoid rim
with sutures around the capsule and the labrum. The medial stump is
then laid on top and repaired to the lateral stump. In this fashion,
the subscapularis tendon is significantly shortened, and the amount of
external rotation is greatly reduced. Compared with the Bankart and the
capsulolabral reconstruction procedures, results after the Putti-Platt
procedure appear to be clearly inferior. As such, good to excellent
results were found in only 55% to 85% of the patients, and recurrent
instability was observed in 9% and 35% of the patients.63,135,138,294 This procedure is also associated with loss of shoulder strength and motion.63,135,273,294
Although loss of external rotation can exceed 40 degrees in some
patients, most studies have reported an average loss of 9 to 23 degrees.41,135,273,294
Finally, long-term follow-up of patients who underwent the Putti-Platt
procedure demonstrated a high incidence of progressive and symptomatic
glenohumeral arthritis (Fig. 38-34). According
to several studies, mild to moderate osteoarthritis was seen in 26% to
30% of the patients, and the severity of the arthritis correlated
directly to the duration of follow up.1,135,273
It has been suggested that the development of arthritis is related to
the loss of external rotation and posterior subluxation secondary to
overtightening of the anterior shoulder structures. Nonetheless, a
recent study of patients who had the Putti-Platt procedure also showed
that shoulders without a significant loss of motion can still develop
symptomatic joint arthrosis.86
In this procedure, the insertion of the subscapularis tendon is
transferred from the lesser tuberosity to a position that is lateral to
the bicipital groove. With this technique, the primary goal
is
to create a tight anterior soft tissue sling that will support the
humeral head against anterior translation. Proponents of this procedure
demonstrate that good to excellent results can be obtained in 90% to
97% of the patients, with low rates of recurrent dislocations.2,89,175 Even with long-term follow-up, reported rates of recurrent instability have been less than 5%.125,234
Although these results are impressive, nonphysiological means of
shoulder reconstructions have generally fallen into disfavor since they
alter the normal biomechanics of the glenohumeral joint and do not
directly address the underlying pathoanatomy. As expected, the
Magnuson-Stack procedure is associated with a loss of external rotation
and forward elevation. In comparison with the patients who underwent
the Putti-Platt procedure, however, this loss was fairly minimal at 5
to 10 degrees.221,234
Other reported complications of the procedure include excessive
anterior tightening with posterior glenohumeral subluxation, damage to
the biceps tendon, and early joint arthrosis.1,77,86
 |
|
FIGURE 38-34 Long-term complication of the Putti-Platt procedure that resulted in endstage arthrosis of the shoulder. AP (A) and axillary (B) radiographs reveal large osteophytes and posterior subluxation with loss of joint space.
|
different bony procedures have been described to treat patients with
anterior glenohumeral instability. Defects greater than 30% of the
glenoid surface may be associated with persistent instability.114,184
Therefore, if these defects are present, they can be addressed by
placing a piece of bone on the glenoid neck in order to provide an
additional surface to interact against the humeral head and to act as a
buttress against anterior dislocation. Even without a glenoid bone
defect, however, surgeons have utilized various bony procedures to
stabilize the glenohumeral joint with varying degrees of success.
been utilized in two of the more commonly performed bony procedures.
The first is the Bristow procedure in which the tip of the coracoid
process, with the conjoined tendons attached, is transferred through a
split in the subscapularis muscle and fixed onto the anterior inferior
glenoid rim just outside the capsule.90 A subsequent modification of the procedure transfers the coracoid process over the superior border of the subscapularis tendon.267
Usually, the rim of the glenoid is exposed and decorticated in order to
enhance bony union between the cut surface of the coracoid process and
the glenoid rim. Because of the remaining capsule, however, some
portion of the transferred bone will not directly interact with the
exposed glenoid rim. Patient satisfaction rate at early and midterm
follow up after this procedure has been reported to be between 82% and
97%.10,58,267 Recurrent dislocations after the procedure were very uncommon, with the reported incidence between 0% and 6%.58,96,156,267 If episodes of subluxations are also included, however, the rate of recurrent instability is much higher at 8.5% to 21%.10,58,96,267
With an extended long-term follow up of 26 years, one study has
demonstrated that both patient satisfaction and joint stability
deteriorated to 70% and 85%, respectively.245
In addition, the Bristow procedure is also associated with high rates
of complications that include loss of external rotation, problems
related to the screw fixation, residual pain, and graft nonunion.58,267 In fact, the rate of screw-related complications was reported to be as high as 24% in one study.194
Because of these concerns, some authors have recommended that the
Bristow procedure not be performed for routine anterior stabilization
of the shoulder.245,293
process is the Latarjet procedure. In comparison with the Bristow
procedure, a significantly larger portion of the coracoid process is
transferred to the neck of the glenoid. The bone is placed in an
extracapsular position, laid on its side, and fixed to the scapula with
screws. At a long-term follow-up evaluation, good to excellent clinical
results were found in 88% to 93% of the patients who were treated with
this procedure.4,252 Rates of recurrent instability, including both subluxation and dislocation, have been reported to be between 2% to 10%.4,100 Ninetyeight percent patient satisfaction has been described at 15-year follow-up.102
Despite these clinical results, however, the procedure is also
associated with the subsequent development of joint arthrosis. Although
the majority of the changes were classified as mild, glenohumeral
arthrosis was reported in 30% to 71% of the patients.4,100,101 In one study, moderate to severe arthrosis was described in 14% of patients with a Latarjet procedure at 15-year follow-up.101
The original description as well as the modification of the procedure
places an iliac crest bone graft on the anterior aspect of the glenoid.
Therefore, the humeral head must translate further to dislocate.
Long-term studies of this procedure have shown good to excellent
results in 75% to 85% of the patients.27,217,218 Reported rates of recurrent dislocations have been mixed, with some authors reporting only 4% and others reporting up to 33%.27,138,218
Unfortunately, after long-term follow-up evaluation in excess of 15
years, several authors have reported joint arthrosis in 47% to 89% of
the patients.217,218
Thus the Eden-Hybbinette procedure has lost much of its popularity as a
primary procedure for routine anterior shoulder stabilization.
outside the joint, another option is to place the bone graft within the
joint. Intra-articular bone grafts are typically inserted to restore,
rather than to enlarge, the glenoid surface. Although individual
techniques can vary, most surgeons place the bone against decorticated
glenoid neck and then fix the graft using several metallic screws. The
fixed graft is subsequently contoured to match the surface of the
native glenoid. Finally, the anterior capsule and the subscapularis
tendon are restored to their anatomic position. A limited series of
patients treated in this fashion demonstrated good results with absence
of apprehension and return to preinjury level of athletic activities.
The authors noted that intra-articular placement of grafts improved the
likelihood of graft union as well as allowing improved matching of the
glenoid surface.278 Hence, although
long-term clinical data are still lacking, this technique may provide a
promising alternative to addressing symptomatic glenoid bony defects.
As such, the clinical history and examination must be thoroughly
reviewed in order to ensure that the instability is isolated to the
posterior direction only. For these patients, indications for surgery
include failure of nonoperative management, open dislocations,
irreducible dislocations, and unstable reductions. In some patients,
traumatic posterior dislocations may be associated
with
a large bony defect in either the glenoid or the anteromedial humeral
head (reverse Hill-Sachs lesion). With these defects, even after a
concentric reduction is obtained, joint stability may be compromised
enough to warrant operative management.
established, there are multiple available surgical options. Surgical
stabilization may be performed arthroscopically, through an open
anterior approach, or through an open posterior approach. To date, no
single approach or technique has been associated with conclusively
superior results. As such, the choice of any specific procedure should
be based on patient expectations as well as surgeon-related factors
such as familiarity, technical expertise, and available equipment and
personnel.
identify and document any structural defects. Although specific
protocols may vary among surgeons, most utilize an anterior portal for
the arthroscope and two posterior portals for the instruments. If a
posterior capsulolabral detachment is identified, it should be
mobilized and reattached to the posterior glenoid rim. Recently use of
suture anchors has become the technique of choice for capsulolabral
reattachment. Unlike anterior instability, however, a posterior
capsulolabral detachment is a much less common finding. For posterior
instability, capsular redundancy seems to play a more critical role. As
such, this redundancy should be addressed by performing arthroscopic
posterior capsulorrhaphy.21
good to excellent results in 86% to 96% of the patients at shortto
midterm follow up.131,281,288 Rates of recurrent instability in these studies have ranged from 0% to 12%.21,24,75,131,216,281
One recent study confirmed that frank posterior dislocations after
surgery were very rare; however, clinically significant posterior
subluxations may be more common. In this study 11% of the patients
failed clinical stability tests and 8% pursued revision surgery for
persisting pain, instability, or decreased function.24
some authors have recommended the use of thermal capsulorrhaphy to
reduce posterior capsular redundancy. As mentioned previously, however,
this technology may be associated with unacceptable risks for clinical
failures and complications, frequently resulting in persisting pain,
instability, and damaged capsular tissue. As such, routine use of this
technique as a primary stabilizing procedure has fallen into disfavor.
instability whose primary complaint is in the posterior direction, an
anterior approach for posterior shoulder stabilization has been
described.285,286
This procedure is performed in a manner similar to the inferior
capsular shift procedure for patients with multidirectional
instability. The anterior deltopectoral approach is utilized to expose
the shoulder. After releasing the subscapularis tendon and isolating
the capsule, the capsule is released from the humeral neck as far
posteriorly as possible. The capsule is then advanced anteriorly and
superiorly in order to remove the redundancy in the anterior, inferior,
and posteroinferior aspects of the joint. In addition to the capsular
imbrication, the anterior approach also provides an opportunity to
address the concomitant laxity in the rotator interval. In this
fashion, humeral head translation is reduced in all directions. At a
midterm follow up of 5 years, a case series reported good to excellent
results in 9 of the 10 patients who were treated with this technique.285
bony defect in the anterior aspect of the humeral head (also known as
the reverse Hill-Sachs lesion) may be present. If the defect is large,
it may engage the posterior glenoid rim during internal rotation,
resulting in recurrent episodes of instability. Therefore although an
anatomic joint reduction can be initially obtained, stable and
congruent motion may not be maintained. For these patients, the bony
defect is the primary pathology and it can be addressed with the
McLaughlin procedure (Fig. 38-35A). The
original description of the procedure includes an anterior approach
with release of the subscapularis tendon from the lesser tuberosity.
The released tendon is then transferred into the bony lesion to fill
the defect and to prevent the humeral head from engaging the posterior
glenoid rim.170 A modification of this procedure, described by Neer (Fig. 38-35B),
does not release the subscapularis tendon. Rather, the lesser
tuberosity is osteotomized with the attached tendon so that it can be
transferred into the bony defect.60,286
Although similarly filling the defect, this modification creates a more
stable construct with improved potential for healing. Although only a
few studies
have
been published, authors have reported stable shoulders with congruent
motion in the majority of patients who were treated with this operation.60,170
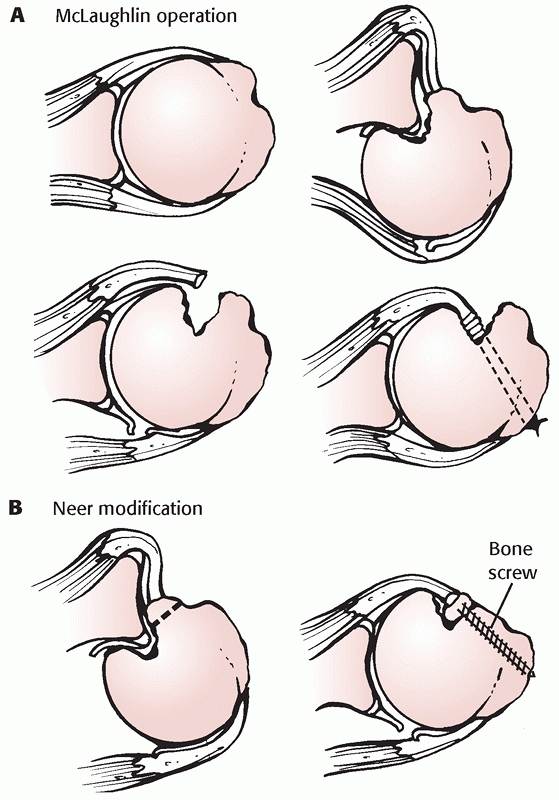 |
|
FIGURE 38-35 A.
The McLaughlin operation. In the presence of a large anterior humeral head lesion, the subscapularis tendon can be transferred into the defect. B. A subsequent modification by Neer transfers the lesser tuberosity with the attached subscapularis tendon. |
or for those with multidirectional instability whose primary symptoms
are in the posterior direction, a posterior approach to the shoulder
can be utilized. Upon exposure of the joint, if a clear capsulolabral
detachment is present, it should be repaired. In addition, posterior
capsular redundancy is addressed by performing posterior capsulorrhaphy
in a manner similar to anterior capsulorrhaphy. For these procedures
meticulous surgical technique must be utilized, because the posterior
capsule is often very thin and fragile.
metallic staples for fixation. According to one series, however,
unsatisfactory results were reported in 9 of the 20 (45%) patients.263
The authors suggested that the high rate of failures may be related to
general ligamentous laxity and unrecognized multidirectional
instability.263 Regardless, the use of a staple has been abandoned in favor of suture capsulorrhaphy.263
Results following posterior suture capsulorrhaphy are more encouraging.
Studies have reported good to excellent results in 80% to 92% of the
patients who were treated with this procedure. Rates of recurrent
instability have been reported to be between 11% and 23% in these
studies.16,64,227
recurrent posterior instability may possess excessive glenoid
retroversion, and that this retroversion may be responsible for the
high rates of surgical failures.64,106,132,287
If excessive retroversion (e.g., greater than 30 degrees) does exist,
normal glenoid version can be restored by performing a posterior
glenoid osteotomy. This procedure utilizes a similar surgical approach
as described above. After exposing the joint, an opening wedge
osteotomy is performed at the posterior scapular neck. The opening
wedge can be stabilized with a bone graft from either the iliac crest
or the posterior acromion. Surgical exposure of the scapular neck must
be performed with caution as the suprascapular nerve lies in close
proximity and is susceptible to injury during the procedure.
287 A recent report of 32 patients who were treated with this procedure
also noted good to excellent results in 82% of the patients.76 Rates of recurrent instability after the procedure have been reported to be between 12% and 17%.76,85
Unfortunately, however, this procedure is also associated with a
variety of complications including anterior subluxation, coracoid
impingement, glenohumeral arthrosis, and intra-articular glenoid
fracture.64,70,76,85
Therefore some authors have suggested that the procedure be performed
only in patients whose glenoid shows significant retroversion in excess
of 30 degrees.286
difficult diagnosis to establish. In many instances, patients exhibit
signs of generalized ligamentous laxity and the onset of their shoulder
symptoms are not preceded by significant trauma. In other instances,
however, patients exhibit signs of generalized ligamentous laxity but
sustain an injury that produces unidirectional instability. As such, it
is difficult to determine whether these patients should be categorized
and treated in a manner similar to unidirectional or multidirectional
instability. These nuances in establishing a clear diagnosis have
contributed to the lack of a true consensus for surgical management of
these patients. Most surgeons do agree, however, that the primary
treatment for patients with atraumatic multidirectional instability
should be nonoperative, with a primary focus on shoulder
rehabilitation. Strengthening of the dynamic shoulder stabilizers has
the potential to compensate for the generalized laxity of the static
shoulder stabilizers. Operative treatment for these patients is
indicated only when nonoperative management has been unsuccessful.
Although the specific indications may vary among surgeons, operative
management is generally recommended for patients who suffer from
continued pain and/or disability despite participation in a structured
physical rehabilitation program for greater than 3 to 6 months.
been established, the procedure may be performed arthroscopically or as
an open procedure. For open procedures, some surgeons preferentially
utilize an anterior approach, whereas others utilize either an anterior
or a posterior approach based on the primary direction of instability.
The “gold standard” for surgical management of multidirectional
instability has been the open stabilization. With recent technological
advances, results after arthroscopic stabilizations are clearly
improving. A recent study of arthroscopic capsulorrhaphy demonstrated a
fairly low rate of instability at 10.5%.160
Nevertheless, to date, long-term outcome studies after arthroscopic
techniques are still lacking and have yet to replicate those of open
surgery (Table 38-4).*
confirm the diagnosis, a diagnostic arthroscopy is performed to
document the pathology. In the vast majority of patients with
atraumatic multidirectional instability, a clear capsulolabral
detachment is not present. The most common finding is the presence of
redundant capsule in the anterior, inferior, and posterior aspects of
the joint, all of which must be addressed. For arthroscopic
capsulorrhaphy in the anterior region, the arthroscope is typically
placed through a posterior portal whereas the instruments and the
sutures are managed through anterior portals. In contrast, for
posterior capsulorrhaphy, the arthroscope is placed through the
anterior portal whereas the instruments and the sutures are managed
through posterior portals. Again, the capsulorrhaphy typically starts
in the inferiormost aspect of the joint and progresses superiorly until
the redundancy in the capsule has been sufficiently removed.
using transglenoid suture technique has been associated with 88% good
to excellent results and 12% recurrent instability.271
Subsequently, surgeons have slightly modified the technique to perform
the entire capsulorrhaphy using suture tying techniques. With a
relatively short follow up of approximately 3 years, two studies have
reported good to excellent results in 94% to 95%
of the patients. In addition, they reported very low rates of recurrent instability at 2% to 5%.68,169
Mid- and long-term follow-up studies of this technique, however, are
still lacking. Rotator interval closure may be added to capsular
plication in the setting of multidirectional instability in order to
further limit humeral head translation.
|
TABLE 38-4 Results after Arthroscopic and Open Stabilizations for Multidirectional Instability
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
treat patients with multidirectional instability is thermal
capsulorrhaphy. As noted in the previous sections, outcomes after this
procedure have been mixed. Various studies have reported recurrent
instability in 19% to 47% of the patients.43,56,61,179
In addition to these high rates of recurrent instability, this
procedure has also been associated with high rates of complications.
Therefore, routine use of this technique for patients with
multidirectional instability has fallen into disfavor.
instability through an open anterior approach. This procedure is
performed in a manner similar to open anterior capsulolabral
reconstruction, as described in the previous section. The primary
difference, however, is the focus on the inferior aspect of the
shoulder capsule. As such, inferior capsular redundancy must be
addressed by first releasing the capsule from the humeral neck all the
way to the posterior inferior quadrant of the joint. The released
capsule is then advanced anteriorly and superiorly to remove the global
capsular redundancy. The original description of this inferior capsular
shift procedure was reported by Neer et al.187
In their preliminary series, satisfactory results were reported in 39
of the 40 patients, with only one patient developing recurrent
instability. Several subsequent studies have reported comparable
results with good to excellent results in over 90% and recurrent
instability in less than 10% of the patients.9,42
In one report, the authors also noted that the failures occurred early
and that the overall outcomes did not deteriorate over time.42
Biomechanical analysis of the inferior capsular shift demonstrated that
glenohumeral mechanics and contact pressures did not change
significantly, compared with normal joints.275,280 Therefore, even with long-term follow-up, development of glenohumeral arthrosis will hopefully remain minimal.
patients, some surgeons recommend approaching the shoulder from the
direction of primary instability. As such, if a patient exhibits signs
of multidirectional instability but has a primary complaint of
posterior instability, a posterior approach is suggested. A posterior
capsular shift procedure is performed as described previously. Again,
particular attention should be given to the inferior capsule in order
to remove the global capsular redundancy. Utilizing either an anterior
or a posterior approach based on the direction of primary instability,
authors have reported good to excellent results in 85% to 94% of the
patients.35,83,213
Although the rate of recurrent instability was relatively low in two of
these studies (4% to 9%), one study reported recurrent instability in
26% of the patients.83 These authors
also showed that the recurrent instability tended to occur early and
that the successful results were maintained over time.83
After adequate assessment is completed, closed reduction of the
shoulder is attempted. In order to obtain muscle relaxation and pain
control, we prefer the use of intra-articular lidocaine injection. If
needed, light supplemental intravenous sedation can also be given.
Although many different reduction techniques can be used, our initial
technique of choice is the traction-countertraction method as described
previously (see Fig. 38-29B). The maneuver is
performed with slow and sustained traction. Sudden and forceful
manipulations must be avoided because they can lead to additional
injuries. Typically, a successful reduction is accompanied by a “clunk”
sensation. Once completed, closed reduction is confirmed with
postreduction radiographs.
unsuccessful, the patient is re-examined to determine the degree of
muscle relaxation. If adequate muscle relaxation can be obtained,
another closed reduction may be attempted. If the second reduction is
still unsuccessful or if adequate muscle relaxation cannot be ensured,
the patient will require general anesthesia in the operating room for
either closed or open reduction.
outside a clinical facility, it may be unclear whether the closed
reduction should be attempted immediately or wait until a formal
evaluation can be completed. Thus, for example, an orthopaedic surgeon
who is on “the field” supervising a high level athletic competition may
witness a player who sustains a shoulder dislocation. In this
situation, after initial assessment and examination, the surgeon may
consider immediate closed reduction. Possible advantages of immediate
reduction include the relative ease of reduction prior to onset of
muscle spasms, immediate relief of pain, and relief of pressure on the
adjacent neurovascular structures. In contrast, possible disadvantages
of immediate reduction include suboptimal assistance, potential damage
to the neurovascular structures during the reduction maneuver, and
displacement of unrecognized fractures. Without necessary personnel and
equipment, it would be difficult to address any complications caused by
improper reduction techniques. Therefore, if a clinical facility is
readily available, a thorough evaluation of the injury, including
radiographs, should be completed first. Attempts at a closed shoulder
reduction can then be performed in a controlled environment with
adequate analgesia. Emergent attempts of closed reduction on “the
field” should only be considered in situations when transfer to a
clinical facility is not readily available and/or the viability of the
upper extremity is threatened by a vascular injury.
following patients: (i) all patients who sustained a first time
traumatic dislocation regardless of age, (ii) patients older than 40
years of age with recurrent instability, (iii) all patients who are
suffering from atraumatic instability. In young and/ or active patients
with traumatic dislocations, however, the high likelihood of developing
recurrent instability is thoroughly discussed. In addition, for older
patients, rotator cuff tendon function is carefully examined to
identify the possibility of an acute tear. If needed, an MRI is
obtained to document the status of the rotator cuff tendons.
is immobilized for approximately 3 weeks. For patients between 30 and
40 years of age, the shoulder is immobilized for 1 to 2 weeks. For
patient older than 40 years of age, the shoulder is immobilized for
only 1 week. We believe that prolonged immobilization in the elderly
patients should be avoided as it can readily lead to shoulder
stiffness. For most patients, a simple sling is utilized for
immobilization. For those with isolated posterior instability, the arm
in placed in a “gunslinger” type of orthosis that places the arm in
neutral rotation and 20 degrees of abduction. Patients are allowed to
remove the immobilization for hygiene purposes. In addition, they are
also allowed to perform simple and nonstressful waist level activities
such as writing and typing. For patients with atraumatic instability,
immobilization is often not required unless they are experiencing
significant pain. If so, their shoulders are immobilized in a similar
pattern.
avoid positions that place their shoulders at risk for instability. As
such, patients with anterior instability should limit external rotation
to less than 30 degrees and abduction to less than 60 degrees. For
patients with posterior instability, they are instructed avoid flexion
greater than 60 degrees and internal rotation greater than 30 degrees.
They are also specifically instructed to avoid cross body adduction.
These restrictions are gradually decreased to provide additional motion
over the course of 6 to 9 weeks. Typically, full range of motion is
allowed by 3 months.
strengthening exercises is instituted. Although supervised physical
therapy may be useful, it must be stressed to patients that they take
responsibility for their own rehabilitation and that the exercises are
performed daily. During the rehabilitation phase, patients are
instructed to avoid any sporting or other high-risk activities.
Gradually, as they gain strength and stability in the shoulder,
patients can return to low-demand recreational activities. They should
not, however, return to high impact activities until adequate
conditioning of the shoulder musculature is restored. For most
patients, this will require at least 6 months of rehabilitation.
whose instability symptoms have become a disability despite adequate
nonoperative therapy. In selected young patients with a high functional
demand of the shoulder, immediate surgical stabilization may be
considered without a course of nonoperative treatment because they
possess a high risk of recurrent instability. Before the operative
procedure, a complete examination under anesthesia is performed to
confirm both the direction and the degree of the instability. By
performing the sulcus test with the shoulder in external rotation, the
integrity of the rotator interval is also examined. For most patients
we prefer arthroscopic techniques for anterior stabilization of the
shoulder. Open procedures are generally reserved for patients who have
undergone previous shoulder surgery, those with a large bony defect in
either the glenoid or the humeral head, and those with a HAGL lesion.
examination of the joint. If there is a glenoid bony defect greater
than 25% of the surface, the procedure is immediately converted to an
open procedure. In addition, an open procedure is also preferred if the
humeral head defect is large enough to clearly engage the anterior
glenoid rim with abduction and external rotation. After examination of
the joint, two anterior portals are established in the rotator
interval. One portal is created immediately superior to the
subscapularis tendon, whereas the other is placed at the superior edge
of the rotator interval. These portals are used interchangeably
for
instruments and sutures. If these portals do not provide sufficient
access to the inferior capsule, an accessory posterior inferior portal
is also created.
identified. In most patients with traumatic instability, the
capsulolabral complex is typically detached and displaced medially. The
complex must be released and mobilized from the glenoid neck until it
can be easily advanced back onto its anatomic position on the anterior
inferior glenoid rim. A suture anchor is then inserted onto the glenoid
rim. Typically, the stabilization begins in the inferior portion of the
joint and progress superiorly. In rare cases, the most inferior suture
anchor cannot be adequately placed through the inferior portal. If so,
a separate stab incision should be placed on the skin so that the
anchor can be passed through the subscapularis tendon. Caution must be
taken, however, to ensure that no instruments enter the joint inferior
to the subscapularis tendon since the nearby axillary nerve may be
injured. After the anchor has been placed, one of the suture ends is
passed through the capsulolabral complex. For most patients capsular
redundancy can be addressed simultaneously by grasping a portion of the
capsule with the same suture. The sutures are then tied using various
arthroscopic knot tying techniques. This process is repeated until the
entire capsulolabral complex is restored onto its anatomic position on
the glenoid rim. If preoperative examination is consistent with a
rotator interval laxity (i.e., positive sulcus sign compared with
contralateral shoulder with the arm in adduction and external rotation)
and if there is excessive glenohumeral translation after the
arthroscopic Bankart procedure, an arthroscopic rotator interval
closure is then performed. In our experience, the sutures should be
placed at least one centimeter lateral to the glenoid rim in order to
avoid excessive tethering of the coracohumeral ligament which may, in
turn, limit external rotation.
through the deltopectoral interval as described. Whenever the anatomy
is difficult to decipher, the coracoid process is used as the defining
landmark. It is termed the “lighthouse” of the anterior shoulder, and
provides a palpable guide to the deltopectoral interval as well as the
coracoacromial arch. The coracoid process is also the origin for the
conjoined tendon of the coracobrachialis and the short head of the
biceps muscles. The brachial plexus and the major vessels to the upper
extremity lie immediately medial to this structure. As such, surgical
exploration of the shoulder joint should remain lateral to the coracoid
process and the conjoined tendon. After adequate exposure is achieved,
additional dissection must be performed to isolate the glenohumeral
capsule and the joint.
reconstruction. This is carried out by first developing the interval
between the subscapularis and the anterior capsule. This interval may
be easier to define and develop near the glenoid, where the
subscapularis is mostly muscular. The subscapularis tendon is then
released near its insertion on the lesser tuberosity. An adequate stump
of the tendon must be maintained laterally for a tendon to tendon
repair at the end of the procedure. After isolation of the anterior
capsule, a vertical incision is made laterally near the humeral head 5
to 7 millimeters medial to the site of subscapularis tenotomy. A
horizontal incision is then created to expose the joint. In this
fashion, a “T”-shaped incision is created on the capsule (see Fig. 38-33).
The joint is then examined to identify the capsulolabral pathology. The
displaced capsulolabral complex is mobilized and reattached to its
anatomic position using suture anchors. Subsequently, the capsule is
imbricated and closed. Redundancy in the capsule is removed during this
imbrication. If a HAGL lesion is present, the repair can be completed
at this stage as well. Typically, the shoulder is maintained in 45
degrees of abduction and 45 degrees of external rotation while the
capsular repair is being performed. The subscapularis tendon is then
repaired anatomically.
than 25%, our procedure of choice is to utilize an iliac crest bone
graft to fill the defect (Fig. 38-36). We
prefer an intracapsular graft placement in order to accurately fill the
defect and to contour the surface appropriately. Appropriate sizing of
the graft is important since an inappropriately large graft will
prevent a complete closure of the capsule. The graft is then fixed to
the scapula using metallic screws. Prior to final tightening of the
screws, however, a suture is placed around each of the screw heads.
These sutures are subsequently used to attach the capsulolabral complex
onto the graft. Intraoperative fluoroscopy can be quite useful in
assessing the length and the location of the screws. After fixation of
the graft and imbrication of the capsule, the subscapularis tendon is
repaired anatomically. Because of pliability of its muscle fibers,
anatomic closure of the subscapularis tendon around the graft is
typically not difficult.
either arthroscopic or open, the involved shoulder is immobilized for
approximately 4 to 6 weeks in a simple sling. Patients are allowed to
remove the sling during this period to perform passive motion exercises
and for hygiene purposes. The limits of passive motion may vary
depending on the stability of the repair. Immediately after the
procedure, however, flexion and external rotation are typically limited
to 90 and 20 degrees, respectively. These limits are gradually
increased to gain near full motion by 8 to 10 weeks. When the period of
immobilization is completed, active motion is gradually instituted.
Resistive strengthening exercises can be started by 10 to 12 weeks
after the procedure. Patients are typically allowed full use of their
shoulder by 6 months after the procedure; however, participation in
high demand activities and contact sports may be delayed up to 9 months.
infrequent problem. As such, the diagnosis must be clearly established
prior to initiating a specific treatment plan. Our indications for
surgical stabilization include failure of nonoperative therapy, an
unstable or incongruent reduction, and open dislocations. For all
patients undergoing operative management, following induction of
anesthesia, an examination must be performed to confirm the diagnosis
of unidirectional posterior instability.
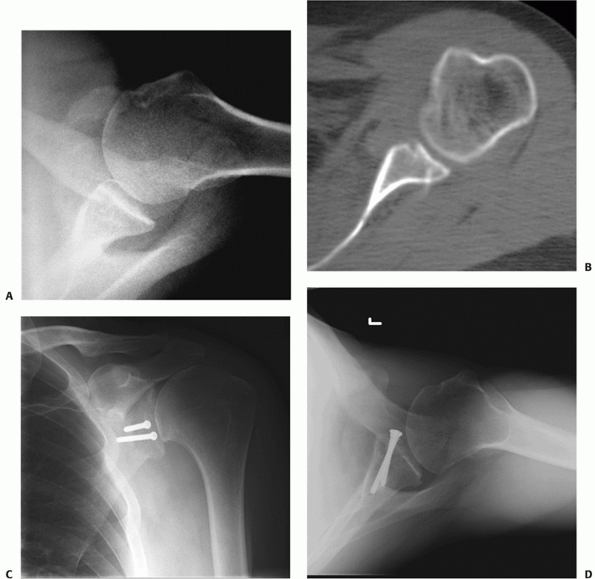 |
|
FIGURE 38-36 Radiographs of a patient with recurrent anterior shoulder instability caused by a glenoid rim defect. Axillary view radiograph (A) and CT-scan image (B)
reveal an osseous defect in the anterior glenoid rim. Using a standard delto-pectoral approach, the defect was identified and filled with a tricortical iliac crest bone graft. Postoperative radiographs (C,D) show that the graft, fixed with two screws, is coplanar with the native glenoid. |
preferred method of stabilization is arthroscopic posterior
capsulorrhaphy. A diagnostic arthroscopy is first performed to document
the structural defects. To gain better visualization of the posterior
structures, the arthroscope is placed through an anterior portal.
Typically, two portals are established on the posterior aspect of the
shoulder for instruments and suture management. If a posterior
capsulolabral detachment is identified, the displaced labrum is
released and mobilized. After mobilization, it is reattached to its
anatomic site on the glenoid rim using suture anchors. Sutures from
these anchors are also passed through the capsule to perform a capsular
plication. If a capsulolabral detachment is not present, an isolated
capsular plication is performed using monofilament sutures. To augment
the plication, these sutures are typically passed through the labrum
for enhanced fixation.
capsulorrhaphy cannot be adequately performed, we prefer open posterior
capsulorrhaphy using a posterior approach. For this procedure, the
patient is placed in a lateral decubitus position. The affected
shoulder is tilted slightly anteriorly so that clear visualization of
the posterior shoulder is possible. After the skin incision, we
typically split the deltoid muscle in line with its fibers. Sometimes,
in patients whose deltoid muscle contains significant bulk and resting
tone, adequate exposure of the shoulder may not be possible by simply
splitting the muscle. In these rare circumstances, the posterior
deltoid is released from its origin on the acromion, and then
reattached at the end of the procedure using bone tunnels. Upon
visualization of the rotator cuff tendons, the infraspinatus tendon is
incised approximately 1 centimeter lateral to its musculotendinous
junction. In this fashion subsequent repair can be
performed
through the tendinous portion, and its insertion at the greater
tuberosity can be spared. The infraspinatus must be reflected with
caution as the underlying capsule can be very thin and friable. The
capsule is then incised vertically the midpoint between the humeral
head and the glenoid rim. The incision must be extended in order to
include the inferior aspect of the capsule. The medial capsular flap is
then shifted laterally and superiorly, and imbricated to reduce any
redundancy. At this point, if the infraspinatus tendon is felt to be
excessively loose, it can also be slightly shortened by imbricating
upon itself. Typically, capsular plication and infraspinatus repair are
performed with the shoulder in neutral rotation.
excessive glenoid retroversion. Since the procedure is associated with
a high rate of complication, we often reserve its use for patients who
have previously undergone a posterior capsulorrhaphy and failed. As
such, glenoid osteotomy is considered for patients who have (i) glenoid
retroversion greater than 20 degrees, (ii) failed extended and
continuous nonoperative rehabilitation, and (iii) recurrent instability
after previous posterior capsulorrhaphy. For patients who meet these
criteria, computed tomography is routinely obtained for preoperative
planning. The correction necessary to achieve neutral glenoid version
is determined from the images. Patient positioning and surgical
procedure is performed as described by Rockwood and colleagues (Fig. 38-37).286
Before performing the osteotomy, a straight blunt instrument is
inserted into the joint so that it rests on the anterior and posterior
glenoid rim. With the instrument held steady, the osteotomy is made
parallel to this instrument approximately 8 to 10 millimeters medial to
the glenoid rim. The initial cut of the osteotomy can be made with an
osteotome or with an oscillating saw. Once the anterior cortex is
engaged, an osteotome is used to complete the cut and the osteotomy
site is opened to the desired correction. To stabilize the osteotomy
site, we utilize a bone graft from the posterior corner of the
acromion. Typically, insertion of the graft stabilizes the osteotomy,
and the construct does not require additional fixation. After the
osteotomy has been completed, a posterior capsulorrhaphy is also
performed.
 |
|
FIGURE 38-37 Posterior glenoid osteotomy. A. An osteotome is placed in the joint to use as a parallel guide. A second osteotome is then used to begin the osteotomy. B. The osteotome is advanced approximately 90% the distance across the glenoid, being sure to leave an anterior hinge of bone. C. The osteotome is removed. D. The osteotomy is then bone grafted to maintain the desired change in version. E. The posterior capsule and infraspinatus are repaired. F. Note the change in version which is maintained by the bone graft.
|
are immobilized in an orthosis with the arm in neutral rotation for
approximately 6 weeks. Patients who underwent a soft tissue procedure
are allowed to remove the immobilization during this period for hygiene
purposes and for daily passive motion exercises. They are instructed to
avoid internal rotation beyond the neutral position. Patients who
underwent
a
bony procedure, however, are only allowed to remove their
immobilization for personal hygiene and do not start passive motion
exercises until 3 to 4 weeks after the procedure. The limits of passive
motion may vary depending on the stability of the repair and/or
construct. Immediately after the procedure, however, flexion and
internal rotation are typically limited to 60 degrees and neutral,
respectively. These limits are gradually increased to gain near full
motion by 8 to 10 weeks. When immobilization is discontinued, active
motion is gradually instituted. Active strengthening exercises are
started by 10 to 12 weeks after the procedure. Patients are typically
allowed to use their shoulder without restrictions by 6 to 8 months
after the procedure; however, participation in high-demand activities
and contact sports is prevented for at least 9 months in most patients.
stress the importance of nonoperative management with a structured and
supervised rehabilitation program. Surgical stabilization is only
considered if the patient has been compliant with the program for
greater than 6 months and continues to be symptomatic. An examination
under anesthesia is first performed to confirm the direction and degree
of instability.
open inferior capsular shift utilizing an anterior approach. After
reflecting the subscapularis tendon from the underlying capsule, a
horizontal capsulotomy is performed. Then, the capsule is incised
vertically near its insertion on the humeral head. The capsule is
released inferiorly along the humeral neck to the posterior inferior
quadrant. Often, traction sutures are used to maintain tension on the
capsule as it is being released. The capsule is then mobilized
superiorly and laterally as to remove global capsular redundancy. The
superior capsular flap is advanced inferiorly to place additional
tension on the inferior capsule. The capsular advancement should be
performed with the shoulder held at approximately 30 degrees of
abduction and 30 degrees of external rotation. The subscapularis tendon
is then repaired anatomically. Finally, the rotator interval is closed
to further stabilize the joint. In our experience, sutures for rotator
interval closure should be placed at least 1 centimeter lateral to the
glenoid rim. Otherwise, the coracohumeral ligament may be tethered by
the suture and limit external rotation.
is immobilized in an orthosis in neutral rotation and 20 degrees of
abduction for approximately 6 weeks. Patients are allowed to remove the
immobilization during this period for hygiene purposes. Passive motion
is instituted at 3 weeks after the surgery. The limits of motion may
vary depending on the stability of the repair. Shortly after the
procedure, however, flexion, external rotation, and internal rotation
are typically limited to 90, 30, and 10 degrees, respectively. These
limits are gradually increased to gain near full motion by 8 to 10
weeks. Upon removal of immobilization, active motion is instituted.
Active strengthening exercises may be started by 10 to 12 weeks after
the procedure. Patients are typically allowed full use of their
shoulder by 6 months after the procedure; however, participation in
high-demand activities and contact sports is prevented for at least 9
months in most patients.
on the evaluation and treatment of glenohumeral instability. As such,
management of patients with shoulder instability is continuing to
evolve. Despite these changes, however, certain principles in the
management of shoulder instability have remained constant and form the
foundation for approaching this clinical problem. In our experience,
the following “pearls and pitfalls” have been useful reminders to
ensure appropriate evaluation and treatment of shoulder instability.
-
When evaluating patients with acute
dislocations, a complete set of radiographs must be obtained and
evaluated. These radiographs should include orthogonal views of the
joint in order to clearly identify the location of the humeral head. -
All closed reduction techniques should
utilize slow, gentle, and sustained maneuvers. Any sudden and forceful
manipulations can lead to additional injuries to the shoulder girdle. -
Both the motor and the sensory component
of the axillary nerve function must be tested and documented. Intact
sensation in the lateral aspect of the shoulder does not guarantee
intact axillary nerve function. -
All patients with shoulder instability
should be questioned regarding voluntary instability as this condition
may have significant implications in the overall treatment plan and the
anticipated outcome. -
All patients who sustained a traumatic
shoulder dislocation should be carefully examined for a rotator cuff
tear. This is especially important for patients older than 40 years of
age, because the incidence of a concomitant rotator cuff tear is
alarmingly high in this population. If the clinical examination is
unclear, an MRI should be obtained to document clearly the status of
the rotator cuff tendons. -
Initial treatment for patients with
atraumatic multidirectional instability should focus primarily on
physical rehabilitation. By strengthening the dynamic stabilizers, it
should be possible to overcome the inherent glenohumeral joint laxity
and obtain a stable shoulder. -
It is crucial to identify all the
pathological defects that are associated with the instability. In
addition to a detailed physical examination, imaging modalities such as
MR-arthrogram are extremely helpful to clearly delineate the cause of
instability. -
Prior to starting any surgical procedure,
an examination under anesthesia should be performed to confirm the
clinical diagnosis and document the direction and degree of instability. -
Surgical stabilization techniques should
address all the underlying pathoanatomy responsible for the
instability. If the structural defects are not adequately addressed,
recurrent instability may occur. -
Although patients who underwent
arthroscopic procedures may experience decreased pain and morbidity in
the early post-operative period, healing of their repaired tissues is
not likely to be substantially different than their counterparts who
underwent open procedures. As such, arthroscopic procedures do not
necessarily justify early or condensed rehabilitation. -
An appropriate postoperative protocol is
crucial to the overall outcome. Initial periods of immobilization and
protection should precede any aggressive rehabilitation. In addition,
although supervised physical therapy can be very useful, we routinely
stress to patients that they are responsible for their own
rehabilitation and cannot rely solely on the therapists.
is an uncommon complication following a shoulder stabilization
procedure. For example, review of all anterior shoulder stabilizations
performed at the Mayo Clinic between 1980 and 2001 identified only six
infections.254 Similarly, review of
the recent literature on arthroscopic shoulder stabilizations has
demonstrated an infection rate less than 0.25%.7,44,53,129,281
Because of this low incidence, etiological factors that may predispose
patients to infection are difficult to identify. Nevertheless,
potential predisposing factors could include inadequate skin
preparation prior to the procedure, contamination during the procedure,
and development of a postoperative hematoma. Although compromised
immune status may also increase the likelihood of postoperative
infection, the majority of the patients with shoulder instability are
young and healthy, and do not possess such risk factors.
postoperative infection may be minimized even further by utilizing
meticulous surgical technique. Another common prophylaxis against
infection is the use of perioperative antibiotics. Since many of these
surgeries are performed as an outpatient procedure, most patients only
receive a single dose of intravenous antibiotics immediately before the
start of the procedure. For those patients who stay overnight, a second
and/or third dose may be given, but this is generally based on surgeon
preference rather than empirical data.
operative evacuation should be considered. Although the decision must
be individualized for each patient, surgical evacuation may prevent the
hematoma from being seeded with bacteria and becoming a source for deep
abscess. If definite postoperative infection has been identified, it
should be treated urgently. In order to prevent the development of
septic arthritis and to protect the surgical construct, the underlying
infection must be treated aggressively. For simple and isolated
cellulitis, treatment with intravenous or oral antibiotics may be
sufficient. On the other hand, if there is evidence to suggest a deeper
infection, prompt irrigation and surgical débridement is indicated.
This can be performed either arthroscopically or as an open procedure.
In general, regardless of whether the initial stabilization surgery was
performed arthroscopically or open, an arthroscopic evaluation should
be considered. The joint can be irrigated and, based on the findings, a
more invasive débridement can then be performed.
traction or direct injury. Neurological injury associated with an open
anterior shoulder repair is a relatively uncommon complication.
According to one study, for example, a neurological injury occurred in
8.2% of the 282 patients who underwent an open anterior stabilization
surgery.94 The incidence of
neurological deficit following an arthroscopic stabilization, however,
has been variable. Some of the earlier studies report an incidence as
high as 30%.5,167,211,325
In these reports, predisposing factors include traction in the lateral
decubitus position, compression secondary to fluid extravasation, and a
tourniquet effect following excessively tight wrapping of the arm.
Fortunately, most injuries were neuropraxias that resolved
spontaneously.232 In some of the
recent series of arthroscopic stabilizations, the incidence of
neurological injury has been reported to be approximately 3%.68,75,129,131,214,281
surgical repair, the musculocutaneous and the axillary nerves are
commonly involved. The musculocutaneous nerve is likely to be injured
due to excessive retraction on the conjoined tendons. In most
instances, these injuries are neuropraxias that resolve spontaneously.
Injury to the axillary nerve can occur during dissection of the
shoulder capsule in the anterior inferior quadrant of the glenoid. When
traction is the cause of the injury, spontaneous recovery can be
expected. Nonetheless, direct injury to the axillary nerve has been
reported, and the likelihood of a spontaneous recovery is less
optimistic.163 Minimizing the risk
of injury to the axillary nerve can be accomplished by palpating or
visually identifying the nerve during the procedure. In addition,
placement of a retractor between the inferior capsule and the axillary
nerve can generally protect the nerve from a direct injury. Less
commonly, the suprascapular nerve can be injured. In anterior bone
grafting surgeries, for example, screws that are used to fix the graft
penetrate posterior superior aspect of the glenoid and can come within
4 mm of the nerve.159 For open
posterior approaches, this nerve can be injured if the surgical
dissection is carried out significantly medial to the glenoid rim. For
any of the nerves, if a direct injury or laceration is suspected, early
exploration of the nerve should be considered.
a variety of reasons. Nonanatomic reconstructions, such as the
Putti-Platt and the Magnusson-Stack procedures, are designed to
restrict motion. As such, these procedures have fallen into disfavor
and been replaced by capsular procedures that address the underlying
pathoanatomy. Unfortunately, even the anatomic capsulolabral
reconstruction procedures can result in stiffness. Immediately after
the reconstruction, it is important to document that normal joint
motion has been maintained and that excessive capsular tightening has
not occurred. Although excessive tightening can also occur after
arthroscopic repairs, it is generally believed to occur at a lower rate.53,79,185
stabilization surgery include prolonged immobilization and poor
compliance with the rehabilitation program. Duration of immobilization
following shoulder surgery can vary widely depending on multiple
factors. In addition, individual patients tend to display variable
abilities in regaining normal shoulder motion. It is important to
initiate a rehabilitation program that focuses on motion as soon as
possible following the repair. The need for early motion, however, must
be balanced against placing the underlying surgical construct at risk
for failure. Patients are
expected
to regain their motion on a gradual basis during the first 3 months
following shoulder surgery. Patients who do not regain the desired
motion within 6 to 9 months should be considered for a surgical
release. Although closed manipulation under anesthesia is widely
utilized, we tend to avoid this procedure because of its uncontrolled
nature and the risk of additional damage. Rather, we prefer an
arthroscopic evaluation with controlled release of the scar tissue and
any overly tightened structures.
excessively tight reconstructions can lead to long-term complications.
The Putti-Platt procedure, for example, has been associated with the
development of symptomatic degenerative arthritis. Excessive tightening
of the anterior structures is believed to result in permanent posterior
humeral head subluxation and incongruent motion, which in turn leads to
glenohumeral arthritis. In addition to the Putti-Platt procedure, any
nonanatomic reconstructions causing excessive tightening of the
anterior structures can, in theory, lead to the same long-term
complications. The best approach to avoid this problem is prevention
(i.e., avoiding excessive tightening of the anterior structures during
the surgical repair).
noncapsular procedures has been associated with a significant rate of
hardware complications.296 Types of
hardware complications can be broadly classified as (i) incorrect
placement of the implant, (ii) migration after placement, (iii)
loosening, and (iv) breakage of the device. In a series of 37 patients
who developed complications related to the use of screws and staples,
35 patients underwent a procedure for anterior instability. Twenty-one
patients had problems from the screws, whereas 14 patients had problems
related to the use of staples (Fig. 38-38).
Common complaints included shoulder pain, decreased motion, crepitus,
and radiating paresthesias. The time interval between surgery and the
onset of symptoms ranged from 4 weeks to 10 years. In this series,
hardware had been incorrectly placed in 10 patients, had migrated or
loosened in 22, and fractured in 3. Thirty-two patients required a
second surgical procedure to address these complications. At the time
of the reoperation, 43% of the patients were noted to have significant
injury to their articular cartilage. Fortunately, hardware-related
complications from screws and staples are now fairly uncommon. This
decrease is partly because of the fact that many surgeons, now being
aware of the potential problems, have significantly decreased their use
of these devices. In addition, as noncapsular procedures have been
performed less frequently, the need for their use has also
significantly decreased.
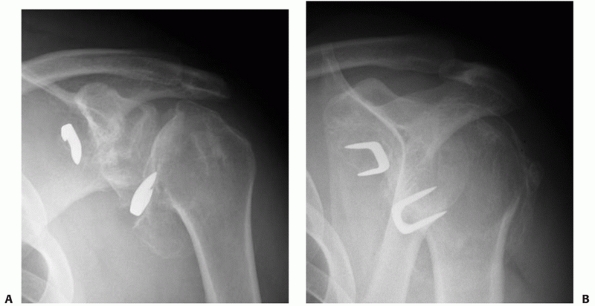 |
|
FIGURE 38-38 Complications associated with the use of metallic staples. AP (A) and scapula lateral (B) views reveal loose staples, with the onset of joint arthrosis.
|
procedures and the advent of arthroscopic techniques have resulted in
the development of new devices for shoulder surgery. Currently, one of
the most commonly used devices for shoulder stabilization surgery is
the suture anchor. Metallic suture anchors can be associated with
similar hardware complications such as incorrect placement, migration,
loosening, and breakage. Incorrect placement can be readily identified
in postoperative radiographs, but may remain asymptomatic. Broken or
loose hardware, however, tends to cause enough symptoms to warrant
further evaluation and possible treatment. When symptoms related to
metallic anchors are present, prompt evaluation must be performed in
order to limit the potential for articular cartilage injury.
Incorrectly placed or migrated anchors should be removed, which can
often be accomplished arthroscopically. An anchor that has migrated and
remains embedded in the inferior aspect of the joint, away from the
articular cartilage, may not cause any additional damage. As such, if
additional migration does not occur and the symptoms remain minimal,
the anchor may not need to be removed. It must be stressed, however,
that these patients must be monitored on a regular basis for at least 4
to 6 months to ensure that the anchor remains in a fixed position.
has decreased the risk of these hardware-related complications. Thus,
for example, a loose anchor may be resorbed prior to causing any
symptoms or permanent damage. Despite these
advantages, however, bioabsorbable anchors can still cause hardware complications including foreign body reaction.29,51 Fortunately, this complication is believed to occur very infrequently with minimal long-term sequelae.
report a history of traumatic incident. The trauma may involve fall
from a height, motor vehicle accident, or less commonly, electrical
shock or seizure episodes. These accidents cause an acute shoulder
dislocation which is associated with significant pain. In most
patients, this pain is sufficient enough to seek immediate medical
attention. Chronic shoulder dislocations occur in situations when the
initial dislocation was unappreciated or when the patient did not or
could not seek adequate medical care. As such, chronic dislocations may
be observed in patients with extremely high tolerance of pain, patients
with decreased mental ability to recognize or verbalize their pain, and
patients with additional injuries that are more obvious or
life-threatening.
will start to dissipate. With the resolution of symptoms, patients may
start using their arm at waist level for functional activities. This
improvement can often be mistaken as the initial step in their
recovery. Despite these improvements, however, shoulder motion will
continue to be limited. Patients with an anterior dislocation typically
lack internal rotation and abduction, whereas those with a posterior
dislocation often lack external rotation and abduction. If the humeral
head remains engaged on the glenoid rim, shoulder motion will often be
associated with a mechanical block as well as crepitus. Because of this
limitation in motion, these patients can be misdiagnosed as having a
posttraumatic adhesive capsulitis or a “frozen shoulder.”87,246 As the improvement in shoulder function reaches a plateau, a more serious injury is eventually suspected.
from varying degrees of pain. Thus, some patients may report
surprisingly little pain whereas others will complain of excruciating
pain. In addition, their functional capacity can also vary widely with
some patients reporting fairly reasonable use of their arm, especially
at waist level. As a general group, however, these patients suffer from
significant shoulder dysfunction. Perhaps the most consistent of their
symptoms include stiffness, crepitus, deformity, and failure to use the
arm for overhead activities.
challenge. Primary goals of treatment are satisfactory pain relief and
optimization of functional recovery. It is crucial for the surgeon to
establish reasonable expectations for the treatment. This information
must be thoroughly discussed with the patient and family. Desire to
perform aggressive, and often technically demanding, interventions
should be tempered by the patient’s expectations, general health,
anticipated functional recovery, and ability to participate in
postoperative rehabilitation.
may be appropriate for patients with minimal pain and disability.
Following the resolution of pain from the initial injury, elderly
patients with a low functional demand may demonstrate excellent
adaptation. With a functional contralateral upper extremity, these
patients may be able to perform activities of daily living despite
limitations in their shoulders. Nonoperative management may also be
desirable for patients with an unacceptably high medical risk for
surgery, patients with an uncontrollable seizure disorder, and patients
who are physically or mentally unable to comply with postoperative
instructions and rehabilitation. For these patients, initial treatments
should concentrate on supportive care. As such, they should undergo a
brief period of immobilization. Once they recover from the initial
injury, gradual rehabilitation that focuses on the restoration of
function should be instituted. As such, active assisted and active
motion exercises should be augmented with occupational therapy that
emphasizes activities of daily living. Aggressive passive stretching
exercises should be avoided as they can lead to further injuries.
chronic shoulder dislocations contain a small number of patients. As
such, firm conclusions are difficult to establish. In general, however,
these studies show that rarely is enough motion regained for overhead
activities.74,87,170
Patients with a chronic posterior dislocation appear to have a more
favorable outcome than those with a chronic anterior dislocation.
Because of these findings, it must be stressed to the patient that the
treatment is based on achieving “limited goal” outcomes with tolerable
pain and function. As such, unrealistic patient expectations for a
normal shoulder must be addressed prior to the initiation of any
treatment.
can vary widely. The choice to proceed with any specific procedure is
dependent on multiple factors including the chronicity of the injury,
associated bony injuries, and associated soft tissue injuries. Other
patient-related factors such as age, hand dominance, vocational
requirements, and medical comorbidities also play a significant role.
Because of this variability, no single procedure has been
preferentially used to treat patients with a chronic shoulder
dislocation.
joint. An attempt at closed reduction, even under general anesthesia,
is unlikely to be successful.74,246
If the joint cannot be reduced, an open surgical reduction can then be
performed. In most situations, the deltopectoral interval is used for
an anterior approach to the shoulder. After exploration of the joint
and removal of any interposed tissues, the humeral head is reduced back
onto the glenoid. Because of soft tissue contractures, joint reduction
may not be stable. In these situations, appropriate soft tissue
releases must be performed. In a classic article by Rowe and Zarins,
appropriate soft tissue release and postoperative immobilization were
sufficient to maintain concentric shoulder reduction.238
For patients with chronic anterior dislocations, the arm was
immobilized anterior to the coronal plane of the body after the
surgical reduction. Conversely, for patients with chronic posterior
dislocations, the arm was immobilized posterior to the coronal plane of
the body. Of the seven shoulders that were treated in this fashion,
they observed good to excellent results in five shoulders and fair
results in two shoulders.238
dislocation, the shoulders were surgically reduced and then fixed with
percutaneously placed Kirschner wires through the acromion into the
humeral head. This construct was augmented with a Bristow procedure in
all patients. The Kirschner wires were left in place for 4 weeks during
which the patients were immobilized in a body bandage. At a follow up
of greater than 2 years, the author reported stable joint reductions in
all patients with a good to excellent clinical result in 8 of the 10
patients.74
 |
|
FIGURE 38-39 A patient with a chronic anterior shoulder dislocation. Preoperative AP (A) and axillary (B) view radiographs confirm anterior dislocation of the shoulder. Intraoperative inspection (C) clearly reveals a deformity (arrow) that is confirmed to be the dislocated humeral head (D).
The humeral head was found to be resting on fractured coracoid process that caused a humeral head defect. Therefore the patient was treated with shoulder hemiarthroplasty. Postoperative AP (E) and axillary (F) view radiographs confirm concentric reduction of the prosthesis. |
significant bony injury, the defect may need to be surgically
addressed. Based on the location and the size of the defect, a number
of different procedures may be considered. They include the McLaughlin
procedure, disimpaction and bone grafting, and resection arthroplasty.87,123,190,238 If degenerative changes are present within the joint, shoulder replacement surgery can also be considered (Fig. 38-39).
Unfortunately, to date, no single procedure has clearly demonstrated a
superior outcome compared to others for the chronically dislocated
shoulder.
CS, Wang VM, Sugalski MT, et al. Biomechanics of shoulder
capsulorrhaphy procedures. J Shoulder Elbow Surg 2005;14(1 Suppl
S):12S-18S.
A. The Magnuson-Stack operation for recurrent anterior dislocation of
the shoulder: a review of 38 cases. J Bone Joint Surg 1987;69-B:111-114.
JG, Powell SE, Tibone JE. Revision anterior capsular shoulder
stabilization using hamstring tendon autograft and tibialis tendon
allograft reinforcement: minimum two-year follow-up. J Shoulder Elbow
Surg 2007;16(3):268-272.
J, Goutallier D, Glorion C. Long-term results of the Latarjet procedure
for the treatment of anterior instability of the shoulder. J Bone Joint
Surg 1998;80-A:841-852.
K, Spring B, Henderson J. Inferior capsular shift procedure in athletes
with multidirectional instability based on isolated capsular and
ligamentous redundancy. Am J Sports Med 2000;28:466-471.
M, Dalldorf P, Sebastianelli W, et al. Long-term follow-up of the
modified Bristow procedure. Am J Sports Med 1993;21:666-671.
J, Bazant F. Factors preventing downward dislocation of the adducted
shoulder joint. J Bone Joint Surg 1959;41-A:1182-1186.
TD, Wolterbeek R, Pilot P, et al. The open modified Bankart procedure:
outcome at follow-up of 10 to 15 years. J Bone Joint Surg Br
2007;89(8):1064-1068.
J, Vegter J. Glenoplasty for recurrent posterior shoulder instability.
Good results in 13 cases followed for 1 to 16 years. Acta Orthop Scand
1995;66:535-537.
L, Pollock R, McIlveen S, et al. Shift of the posteroinferior aspect of
the capsule for recurrent posterior glenohumeral instability. J Bone
Joint Surg 1995;77-A: 1011-1020.
S, Dahlback L. Nerve injuries in dislocations of the shoulder joint and
fractures of the neck of the humerus. A clinical and
electromyographical study. Acta Chir Scand 1970;136(6):461-466.
M, Obata W. Diagnosis of posterior dislocation of the shoulder with use
of Velpeau axillary and angle-up roentgenographic views. J Bone Joint
Surg 1967; 49-A(5):943-949.
M, Brinkman T, Ruhmann O, et al. [Open versus arthroscopic shoulder
stabilization. An analysis of the treatment cost]. Orthopade
2003;32:654-658.
P, Villalba M, Hery JY, et al. Risk factors for recurrence of shoulder
instability after arthroscopic Bankart repair. J Bone Joint Surg Am
2006;88(8):1755-1763.
CR, Franks BR, Moore JH, et al. Operative stabilization of posterior
shoulder instability. Am J Sports Med 2005;33(7):996-1002.
CR, Smith EL, Berkowitz MJ, et al. Arthroscopic versus open shoulder
stabilization for recurrent anterior instability: a prospective
randomized clinical trial. Am J Sports Med Nov 2006;34(11):1730-1737.
M, Warren R. Ligamentous control of shoulder stability based on
selective cutting and static translation experiments. Clin Sports Med
1991;10:757-782.
JP, Baker CL, 3rd, Kline AJ, et al. Arthroscopic capsulolabral
reconstruction for posterior instability of the shoulder: a prospective
study of 100 shoulders. Am J Sports Med 2006;34(7):1061-1071.
W, Griffiths D. Orthopaedic surgery in the 16th and 17th centuries:
Luxations of the shoulder. J Bone Joint Surg 1948;30-B:365-375.
J, Finnanger A, Merckoll E, et al. Satisfactory long-term results after
Eden-Hybbinette-Alvik operation for recurrent anterior dislocation of
the shoulder: 6 to 20 years’ follow-up of 52 patients. Acta Orthop
Scand 2003;74:180-185.
LT, Banks KP, Taylor DC. Humeral avulsion of the glenohumeral
ligaments: the HAGL lesion. Am J Sports Med 2007;35(11):1960-1966.
S, De Beer J. Traumatic glenohumeral bone defects and their
relationship to failure of arthroscopic Bankart repairs: significance
of the inverted-pear glenoid and the humeral head engaging Hill-Sachs
lesion. Arthroscopy 2000;16:677-694.
J, Baker C, Uribe J. The incidence of Hill-Sachs lesions in initial
anterior shoulder dislocations. Arthroscopy 1989;5:254-257.
DS, Mazzocca AD, Oryhon J, et al. A prospective outcome evaluation of
arthroscopic Bankart repairs: minimum 2-year follow-up. Am J Sports Med
2006;34(5): 771-777.
C, Ogilvie-Harris D. Inferior capsular shift operation for
multidirectional instability of the shoulder in players of contact
sport. Br J Sports Med 2002;36:290-294.
CB, Sorenson S, Dwek JR, et al. Humeral avulsion of the posterior band
of the inferior glenohumeral ligament: MR arthrography and clinical
correlation in 17 patients. AJR Am J Roentgenol 2004;183(2):355-359.
R, Brems J, Kotschi H. Glenoid size, inclination, and version: an
anatomic study. J Shoulder Elbow Surg. 2001;10:327-332.
WJ 2nd, Weinstein DM, Elias JJ. Glenohumeral chondrolysis following
thermal capsulorrhaphy. Orthopedics 2007;30(2):158-160.
J, Harryman D. Tendons, ligaments, and capsule of the rotator cuff.
Gross and microscopic anatomy. J Bone Joint Surg 1992;74-A:713-725.
E. Rupture of the supraspinatus tendon and other lesions in or about
the subacromial bursa. The Shoulder. Boston: Thomas Todd, 1934.
K, Capito C, Cross M. The use of the Putti-Platt procedure in the
treatment of recurrent anterior dislocation, with special reference to
the young athlete. Am J Sports Med 1986;14:380-382.
R, Brems J. The inferior capsular shift procedure for multidirectional
instability of the shoulder. J Bone Joint Surg 1992;74-A:1516-1521.
D, Bradley J, Fleischli J, et al. Prospective evaluation of thermal
capsulorrhaphy for shoulder instability: indications and results, 2- to
5-year follow-up. Am J Sports Med 2004;32:21-33.
G, Ogilvie-Harris D. Septic arthritis following arthroscopy, with
cost/benefit analysis of antibiotic prophylaxis. Arthroscopy
1988;4:10-14.
TM, Arciero RA, Taylor DC. Arthroscopic stabilization of acute initial
anterior shoulder dislocation: the West Point experience. J South
Orthop Assoc 1996; 5(4):263-271.
A, Silberstein C. Results following a modified Magnuson procedure in
recurrent dislocation of the shoulder. Surg Clin North Am
1963;43:1651-1653.
CB, McCormick F, Bell SJ, et al. An analysis of capsular area in
patients with anterior, posterior, and multidirectional shoulder
instability. Am J Sports Med 2008; 36(3):515-522.
R. Operation der habituellen schulterluxation unter mitteilung eines
neuen verfahrens bei abriss am inneren pfannenrande. Dtsch Z Chir
1918;144:269-280.
D, Hoy G, Saies A, et al. Adverse reaction to an absorbable shoulder
fixation device. J Shoulder Elbow Surg 1994;3:230-233.
K. [Has the duration of cast fixation after shoulder dislocations an
influence on the frequency of recurrent dislocation? (author’s
translation)]. Arch Orthop Unfallchir 1977;89:187-190.
G, Milano G, Demontis A, et al. Arthroscopic versus open treatment of
Bankart lesion of the shoulder: a prospective randomized study.
Arthroscopy 2004; 20:456-462.
AJ, Castillo R, Clough M, et al. Clinical assessment of three common
tests for traumatic anterior shoulder instability. J Bone Joint Surg Am
2006;88(7):1467-1474.
P, Langenderfer M, Colosimo A, et al. Arthroscopic laser-assisted
capsular shift in the treatment of patients with multidirectional
shoulder instability. Am J Sports Med 2002;30:322-328.
E, Schmidt G, Boorman R, et al. The anteroinferior labrum helps center
the humeral head on the glenoid. J Shoulder Elbow Surg 2003;12:53-58.
L, Warren R, O’Brien S, et al. Isolated closure of rotator interval
defects for shoulder instability. Am J Sports Med 1995;23:557-563.
J, Waddell J, O’Driscoll S, et al. Acute posterior fracture
dislocations of the shoulder treated with the Neer modification of the
McLaughlin procedure. J Orthop Trauma 1995;9:190-193.
B, Watson B, Lapoint J. The use of thermal capsulorrhaphy in the
treatment of multidirectional instability. J Shoulder Elbow Surg
2002;11:108-113.
E, Soslowsky L, Ticker J, et al. Excursion of the rotator cuff under
the acromion. Patterns of subacromial contact. Am J Sports Med
1994;22:779-788.
A-S, Tegner Y. Results of the Putti-Platt operation for recurrent
anterior dislocation of the shoulder. Int Orthop 1991;15:185-188.
B, Jost B, Gerber C. Posterior-inferior capsular shift for the
treatment of recurrent, voluntary posterior subluxation of the
shoulder. J Bone Joint Surg 2000;82-A:16-25.
W, Allman F, Armstrong W. Occult anterior subluxations of the shoulder
in noncontact sports. Am J Sports Med 1987;15:579-585.
W, Slappey C, Ochs C. Roentgenographic demonstration of instability of
the shoulder: the apical oblique projection. A technical note. J Bone
Joint Surg 1450-1455 1984;66-A.
G, Roddey T, Hammerman S. Arthroscopic treatment of multidirectional
glenohumeral instability: 2- to 5-year follow-up. Arthroscopy
2001;17:236-243.
G, Taverna E, Hammerman S. Arthroscopic rotator interval repair in
glenohumeral instability: description of an operative technique.
Arthroscopy 1999;15: 330-332.
C, Ganz R, Vinh T. Glenoplasty for recurrent posterior shoulder
instability: an anatomic appraisal. Clin Orthop 1987;216:70-79.
R, Jobe F, Tibone J, et al. Dynamic electromyographic analysis of the
throwing shoulder with glenohumeral instability. J Bone Joint Surg
1988;70-A:220-226.
J, Iserin A, Duranthon L, et al. A four-portal arthroscopic
stabilization in posterior instability. J Shoulder Elbow Surg
2003;12:337-341.
H, Koydl P, Zichner L. Effectiveness of glenoid osteotomy in atraumatic
posterior instability of the shoulder associated with excessive
retroversion and flatness of the glenoid. Int Orthop 1999;23:95-99.
A, Norris T. Shoulder arthroplasty for advanced glenohumeral arthritis
after anterior instability repair. J Shoulder Elbow Surg
2001;10:593-545.
M, Christensen K. Arthroscopic Bankart procedure: 2- to 5-year
follow-up with clinical correlation to severity of glenoid labral
lesion. Am J Sports Med 1995;23(3): 276-281.
M, Christensen K. Arthroscopic versus open Bankart procedures: a
comparison of early morbidity and complications. Arthroscopy
1993;9:371-374.
P, Burks R, Schickendantz M, et al. Axillary nerve injury after thermal
capsular shrinkage of the shoulder. J Shoulder Elbow Surg
2001;10:231-235.
P, Schuller U, Wiedemann E. The intra-articular pressure of the
shoulder: an experimental study on the role of the glenoid labrum in
stabilizing the joint. Arthroscopy 1992;8:166-172.
R, Isaac F, Booth C. Dislocations of the shoulder with special
reference to accompanying small fractures. J Bone Joint Surg
1959;41-A:489-494.
K, Fukuda H, Nakajima T, et al. The inferior capsular shift operation
for instability of the shoulder. Long term results in 34 shoulders. J
Bone Joint Surg 1999; 81-B:218-225.
SS, Fleckenstein C, Albright J. Open treatment of posterior humeral
avulsion of the glenohumeral ligaments: a case report and review of the
literature. J Shoulder Elbow Surg 2007;16(4):e3-5.
R. Glenoid osteotomy for recurrent posterior subluxation of the
shoulder: assessment by computed axial tomography. J Shoulder Elbow
Surg 1996;5:393-400.
R, Angelo R. Glenohumeral osteoarthrosis. A late complication of the
Putti-Platt repair. J Bone Joint Surg 1990;72-A:1193-1197.
RJ, Krishnan SG, Karas SG, et al. Electrothermal arthroscopic shoulder
capsulorrhaphy: a minimum 2-year follow-up. Am J Sports Med
2007;35(9):1484-1488.
S, Grimberg B, Chesar J, et al. [Magnuson Stack operation for chronic
anterior shoulder instability]. Harefuah 1996;130:300-304.
H, Sachs M. The grooved defect of the humeral head. A frequently
unrecognized complication of dislocations of the shoulder joint.
Radiology 1940;35:690-700.
E, Cofield R, Balm M, et al. Neurologic complications of surgery for
anterior shoulder instability. J Shoulder Elbow Surg 1999;8:266-270.
L. Anterior dislocation of the shoulder in teenagers and young adults.
Five-year prognosis. J Bone Joint Surg 1987;69-A:393-399.
L, Akermark C, Albrektsson B, et al. Bristow-Laterjet procedure for
recurrent anterior dislocation of the shoulder. A 2- to 5-year
follow-up study on the results of 112 cases. Acta Orthop Scand
1983;54:284-290.
L, Augustini B, Fredin H, et al. Primary anterior dislocation of the
shoulder in young patients. A 10-year prospective study. J Bone Joint
Surg 1996;78-A:1677-1684.
L, Eriksson K, Fredin H, et al. Recurrences after initial dislocation
of the shoulder. Results of a prospective study of treatment. J Bone
Joint Surg 343-349 1983; 65-A(3).
L, Olofsson A, Sandstrom B, et al. Nonoperative treatment of primary
anterior shoulder dislocation in patients 40 years of age and younger:
a prospective 25-year follow-up. J Bone Joint Surg Am
2008;90(5):945-952.
L, Sandstrom B, Rosmark D, et al. Long-term results with the Bankart
and Bristow-Latarjet procedures: recurrent shoulder instability and
arthropathy. J Shoulder Elbow Surg 2001;10:445-452.
L, Sandstrom B, Saebo M. One hundred eighteen Bristow-Latarjet repairs
for recurrent anterior dislocation of the shoulder prospectively
followed for 15 years: study II—the evolution of dislocation
arthropathy. J Shoulder Elbow Surg 2006;15(3): 279-289.
L, Sandstrom B, Sundgren K, et al. One hundred eighteen
Bristow-Latarjet repairs for recurrent anterior dislocation of the
shoulder prospectively followed for fifteen years: study I—clinical
results. J Shoulder Elbow Surg 2004;13(5):509-516.
L, Thorling J, Fredin H. Recurrent anterior dislocation of the
shoulder: results after the Bankart and Putti-Platt operations. J Bone
Joint Surg 1979;61-A:566-569.
S, Galinat B, Renzi A, et al. Normal and abnormal mechanics of the
glenohumeral joint in the horizontal plane. J Bone Joint Surg
1988;70-A:227-232.
J, Anderson T, Dear W, et al. Posterior shoulder instability. Surgical
versus conservative results with evaluation of glenoid version. Am J
Sports Med 1992;20: 392-400.
PE, Haen PS, Kidd M, et al. The shape of the inferior part of the
glenoid: a cadaveric study. J Shoulder Elbow Surg 2006;15(6):759-763.
S. De la transplantation d’un fragment osseux pour remedier aux
luxations recidivantes de l’epaule: constatations et resultats
operatoires. Acta Chir Scand 1932; 71:411-445.
J, Zlatkin M, Esterhai J, et al. Magnetic resonance imaging of the
shoulder. Sensitivity, specificity, and predictive value. J Bone Joint
Surg 1991;73-A:17-29.
E, Hatakeyama Y, Kido T, et al. A new method of immobilization after
traumatic anterior dislocation of the shoulder: a preliminary study. J
Shoulder Elbow Surg 2003; 12:413-415.
E, Kuechle D, Newman S, et al. Stabilising function of the biceps in
stable and unstable shoulders. J Bone Joint Surg 1993;75-B:546-550.
E, Lee S, Berglund L, et al. The effect of a glenoid defect on
anteroinferior stability of the shoulder after Bankart repair: a
cadaveric study. J Bone Joint Surg 2000;82-A: 35-46.
E, Motzkin N, Morrey B, et al. Scapular inclination and inferior
stability of the shoulder. J Shoulder Elbow Surg 1992;1:131-139.
E, Sashi R, Minagawa H, et al. Position of immobilization after
dislocation of the glenohumeral joint. J Bone Joint Surg
2001;83-A:661-667.
J, Aldawoudy AM. Chondrolysis of the glenohumeral joint following
arthroscopic capsular release for adhesive capsulitis: a case report.
Knee Surg Sports Traumatol Arthrosc Mar 2007;15(3):292-294.
F, Giangarra C, Kvitne R, et al. Anterior capsulolabral reconstruction
of the shoulder in athletes in overhand sports. Am J Sports Med
1991;5:428-434.
J, Bayley J. Early complications of acute anterior dislocation of the
shoulder in the middle-aged and elderly patient. Injury 1982;13:431-434.
B, Pelet S, Farron A. Traumatic recurrent anterior dislocation of the
shoulder: two to four year follow up of an anatomic open procedure. J
Shoulder Elbow Surg 2004;13:30-34.
KJ, Wiesel B, Ganley TJ, et al. Functional outcomes of early
arthroscopic bankart repair in adolescents aged 11 to 18 years. J
Pediatr Orthop 2007;27(2):209-213.
J. Recurrent traumatic anterior dislocation of the shoulder. Two
hundred eighteen consecutive cases treated by a modified Magnuson-Stack
procedure and follow for 2 to 18 years. Acta Orthop Scand Suppl
1997;275:69-71.
S. Arthroscopic rotator interval repair and anterior portal closure: an
alternative technique. Arthroscopy 2002;18:436-439.
J, Magnusson L, Ejerhed L, et al. Comparison of open and arthroscopic
stabilization for recurrent shoulder dislocation in patients with a
Bankart lesion. Am J Sports Med 2001;29:538-542.
S, Ha K, Cho Y, et al. Arthroscopic anterior stabilization of the
shoulder. Two-to six-year follow-up. J Bone Joint Surg
2003;85-A:1511-1518.
S, Ha K, Kim K. Bankart repair in traumatic anterior shoulder
instability: open versus arthroscopic technique. Arthroscopy
2002;18:755-763.
S, Ha K, Park J, et al. Arthroscopic posterior labral repair and
capsular shift for traumatic unidirectional recurrent posterior
subluxation of the shoulder. J Bone Joint Surg 2003;85-A:1479-1487.
SH, Noh KC, Park JS, et al. Loss of chondrolabral containment of the
glenohumeral joint in atraumatic posteroinferior multidirectional
instability. J Bone Joint Surg Am 2005;87(1):92-98.
SH, Park JC, Park JS, et al. Painful jerk test: a predictor of success
in nonoperative treatment of posteroinferior instability of the
shoulder. Am J Sports Med 2004;32(8): 1849-1855.
A, Litchfield R, Thain L, et al. Agreement between magnetic resonance
imaging and arthroscopic evaluation of the shoulder joint in primary
anterior dislocation of the shoulder. Clin J Sport Med 2003;13:148-151.
J, Mersich I, Perlaky G, et al. The results of the Putti-Platt
operation with particular reference to arthritis, pain, and limitation
of external rotation. J Shoulder Elbow Surg 1998;7:495-500.
O, Pasila M, Jaroma H, et al. Immobilization after primary dislocation
of the shoulder. Acta Orthop Scand 1980;51:915-919.
Y, Shiozaki H, Sugaya H. Arthroscopic repair of a humeral avulsion of
the glenohumeral ligament lesion. Arthroscopy 2005;21(5):632.
D, Rutt J, Treml O, et al. Osteoarthritis and recurrences after
Putti-Platt and Eden-Hybbinetter operations for recurrent dislocation
of the shoulder. Int Orthop 1997;21: 72-76.
V, Balasubramaniam P. The role of atmospheric pressure in stabilizing
the shoulder: an experimental study. J Bone Joint Surg
1985;67-B:719-721.
JE, Lee TQ, Debski RE, et al. Stability and instability of the
glenohumeral joint: the role of shoulder muscles. J Shoulder Elbow Surg
2005;14(1 Suppl S):32S-38S.
T, Crawford H. Reduction of anterior dislocations of the shoulder by
means of the Milch abduction technique. J Bone Joint Surg
1952;34-A:108-109.
BK, Yung PS, Ho EP, et al. The surgical outcome of immediate
arthroscopic Bankart repair for first time anterior shoulder
dislocation in young active patients. Knee Surg Sports Traumatol
Arthrosc 2008;16(2):188-193.
M, Sidles J, Harryman D, et al. Effect of a chondral-labral defect on
glenoid concavity and glenohumeral stability. A cadaveric model. J Bone
Joint Surg 1996;78-A:94-102.
S, Kim K, O’Driscoll S, et al. Dynamic glenohumeral stability provided
by the rotator cuff muscles in the midrange and end-range motion. A
study in cadavera. J Bone Joint Surg 2000;82-A:849-857.
W, Richmond J, Donaldson W. Use of the suture anchor in open Bankart
reconstruction. A follow-up report. Am J Sports Med 1994;22:723-726.
WN, Clark AM, Jr., D’Alessandro DF, et al. Chondrolysis following
arthroscopic thermal capsulorrhaphy to treat shoulder instability. A
report of two cases. J Bone Joint Surg Am Mar 2005;87(3):616-621.
A, Kelly B, Lintner S, et al. Function of the long head of the biceps
at the shoulder: electromyographic analysis. J Shoulder Elbow Surg
2001;10:250-255.
O, Yang BY, Hosseinzadeh P, et al. The effect of glenohumeral position
on the shoulder after traumatic anterior dislocation. Am J Sports Med
2008;36(4): 775-780.
S, Vanderhooft J, Harris S, et al. Glenohumeral stability from
concavitycompression: a quantitative analysis. J Shoulder Elbow Surg
1993;2(1):27-35.
I, Nonweiler B, Woolfrey M, et al. An evaluation of the apprehension,
relocation, and surprise test for anterior shoulder instability. Am J
Sports Med 2004;32:301-307.
S, Kerlan R, Jobe F, et al. The modified Bristow procedure for
recurrent dislocation of the shoulder. J Bone Joint Surg
1976;58-A(2):256-261.
GJ, Gerber C, Schneeberger AG. Suprascapular nerve palsy after the
Latarjet procedure. J Shoulder Elbow Surg 2007;16(2):e13-15.
B, Potzl W, Witt KA, et al. A modified capsular shift for atraumatic
anteriorinferior shoulder instability. Am J Sports Med
2005;33(7):1011-1015.
JL, Slongo TF, Agel J, et al. Fracture and dislocation classification
compendium —2007: Orthopaedic Trauma Association classification,
database, and outcomes committee. J Orthop Trauma 2007;21(10
Suppl):S1-133.
L, Vetter W, Oweida S, et al. Arthroscopic staple capsulorrhaphy for
recurrent anterior shoulder instability. Arthroscopy 1988;4:106-111.
AD, Brown FM, Jr., Carreira DS, et al. Arthroscopic anterior shoulder
stabilization of collision and contact athletes. Am J Sports Med
2005;33(1):52-60.
E, Warren R, Deng X, et al. Temperature along the axillary nerve during
radiofrequency induced thermal capsular shrinkage. Am J Sports Med
2004;32: 909-914.
E, Neira C, Gutierrez M, et al. Clinical significance of the
arthroscopic drivethrough sign in shoulder surgery. Arthroscopy
2001;17:38-43.
L, Caspari R. The rationale and technique for arthroscopic
reconstruction of anterior shoulder instability using multiple sutures.
Orthop Clin North Am 1993;24: 55-58.
L, Caspari R, Savoie F. The arthroscopic treatment of multidirectional
shoulder instability: 2-year results of a multiple suture technique.
Arthroscopy 1997;13: 418-425.
L, Donahue J, Good R, et al. The Magnuson-Stack procedure for treatment
of recurrent glenohumeral dislocations. Am J Sports Med
1984;12(2):133-137.
S, Cleeman E, Auerbach J, et al. Comparison of intra-articular
lidocaine and intravenous sedation for reduction of shoulder
dislocations: a randomized, prospective study. J Bone Joint Surg
2002;84-A:2135-2139.
PJ, Clavert P, Warner JJ. Open operative treatment for anterior
shoulder instability: when and why? J Bone Joint Surg Am
2005;87(2):419-432.
A, McBirnie J. Thermal capsular shrinkage for treatment of
multidirectional instability of the shoulder. J Bone Joint Surg
2003;85-A:2283-2287.
GW, Sallay PI, Didelot W. A longitudinal study of patients with
multidirectional instability of the shoulder with 7- to 10-year
follow-up. J Shoulder Elbow Surg 2005;14(5):466-470.
D, Fanton G. Two-year outcome of arthroscopic Bankart repair and
electrothermal assisted capsulorrhapy for recurrent traumatic anterior
shoulder instability. Arthroscopy 2001;17:844-849.
N, Yoneda M, Hayashida K, et al. Recurrent anterior shoulder
dislocation caused by a midsubstance complete capsular tear. J Bone
Joint Surg Am 2005;87(12): 2717-2723.
W, Jobe F. Functional outcome in athletes after modified capsulolabral
reconstruction. Am J Sports Med 1994;22:353-358.
WH, Jr., Wahl M, Hettrich C, et al. Anteroinferior bone-grafting can
restore stability in osseous glenoid defects. J Bone Joint Surg Am Sep
2005;87(9): 1972-1977.
H, Overgaard B. The anterior capsular mechanism in recurrent anterior
dislocation of the shoulder. J Bone Joint Surg 1962;44-B(4):913-926.
C, Foster C. Inferior capsular shift for involuntary inferior and
multidirectional instability of the shoulder. A preliminary report. J
Bone Joint Surg 1980;62-A:897-908.
CSI. Involuntary inferior and multidirectional instability of the
shoulder etiology, recognition, and treatment. Instr Cour Lect
1985;34:232-238.
R, Neviaser T, Neviaser J. Concurrent rupture of the rotator cuff and
anterior dislocation of the shoulder in the older patient. J Bone Joint
Surg 1988;70-A: 1308-1311.
A, Nielsen K. The modified Bristow procedure for recurrent anterior
dislocation of the shoulder. Results and complications. Acta Orthop
Scand 1982;53:229-232.
A, Petersson CJ. Incidence and causes of shoulder girdle injuries in an
urban population. J Shoulder Elbow Surg 1995;4(2):107-112.
S, Neves M, Arnoczky S, et al. The anatomy and histology of the
inferior glenohumeral ligament complex of the shoulder. Am J Sports Med
1990;18:449-456.
S, Schwartz R, Warren R, et al. Capsular restraints to
anterior-posterior motion of the abducted shoulder: a biomechanical
study. J Shoulder Elbow Surg 1995;4: 298-308.
BD, Duffey ML, Nelson BJ, et al. The incidence and characteristics of
shoulder instability at the United States Military Academy. Am J Sports
Med 2007;35(7): 1168-1173.
M, Deng X, Warren R, et al. Role of the long head of the biceps brachii
in glenohumeral stability: a biomechanical study in cadavera. J
Shoulder Elbow Surg 1996;5:255-262.
M, Dome D. Surgical treatment of traumatic anterior shoulder
instability in American football players. J Bone Joint Surg
2002;84-A:711-715.
S, Jolles BM, Farron A. Bankart repair for recurrent anterior
glenohumeral instability: results at 29 years’ follow-up. J Shoulder
Elbow Surg 2006;15(2):203-207.
C, Altchek D, Warren R. Operative arthroscopy. In: Rockwood C, Matsen
F, eds. The Shoulder. 2nd Ed. Philadelphia: WB Saunders, 1998.
T, Hunter R, Freeman J. Primary traumatic anterior shoulder dislocation
in patients 40 years of age and older. Arthroscopy 1998;14:289-294.
M, Nainzedeh N, Ergas E, et al. The use of somatosensory evoked
potentials for detection of neuropraxia during shoulder arthroscopy.
Arthroscopy 1988;4:250-255.
D, Bravman JT, Heywood C, et al. Arthroscopic rotator interval closure:
effect of sutures on glenohumeral motion and anterior-posterior
translation. Am J Sports Med 2006;34(10):1656-1661.
R, Owens J, Flatow E, et al. Operative results of the inferior capsular
shift procedure for multidirectional instability of the shoulder. J
Bone Joint Surg 2000;82-A:919-928.
W, Witt K, Hackenberg L, et al. Results of suture anchor repair of
anteroinferior shoulder instability: a prospective clinical study of 85
shoulders. J Shoulder Elbow Surg 2003;12:322-326.
MT, Bell SJ, Menzel KA, et al. Arthroscopic treatment of posterior
shoulder instability: results in 33 patients. Am J Sports Med
2005;33(10):1463-1471.
F, Ogon M, Wimmer C, et al. Glenohumeral osteoarthrosis after the
Eden-Hybbinette procedure. Clin Orthop 2000;373:135-140.
H, Wikblad L, Nowak J, et al. Long-term clinical and radiologic results
after Eden-Hybbinette operation for anterior instability of the
shoulder. J Shoulder Elbow Surg 2003;12:15-19.
B. Experiments on the tensile strength of the anterior capsular
structures of the shoulder in man. J Bone Joint Surg 1968;50-B:858-865.
W, Webster-Bogaert S, Hawkins R, et al. Comparative functional analysis
of the Bristow, Magnuson-Stack, and Putti-Platt procedure for recurrent
dislocations of the shoulder. Am J Sports Med 1989;17:42-48.
M, Koudela K. [Posttraumatic anterior shoulder instability—arthroscopic
stabilization method using bone anchors]. Acta Chir Orthop Traumatol
Cech 2004;71:37-44.
M, Wilk K, Hooks T, et al. Thermal assisted capsular shrinkage of the
glenohumeral joint in overhead athletes: a 15 to 47 months follow-up. J
Orthop Sports Phys Ther 2003;33:455-467.
YG, Cho NS. Anterior shoulder instability with humeral avulsion of the
glenohumeral ligament lesion. J Shoulder Elbow Surg 2007;16(2):188-192.
YG, Ha JH, Cho NS. Anterior shoulder stabilization in collision
athletes: arthroscopic versus open Bankart repair. Am J Sports Med
2006;34(6):979-985.
YG, Ha JH, Park KJ. Clinical outcome of anterior shoulder instability
with capsular midsubstance tear: a comparison of isolated midsubstance
tear and midsubstance tear with Bankart lesion. J Shoulder Elbow Surg
2006;15(5):586-590.
YG, Lee DH, Lim CT. Posterior capsulolabral reconstruction in posterior
shoulder instability: deltoid saving. J Shoulder Elbow Surg
2005;14(4):355-360.
DP, Burkhart SS. Arthroscopic humeral avulsion of the glenohumeral
ligaments (HAGL) repair. Arthroscopy 2004;20(Suppl 2):134-141.
J, Donaldson W, Fu F, et al. Modification of the Bankart reconstruction
with a suture anchor. Report of a new technique. Am J Sports Med
1991;19:343-346.
CM, Jenkins PJ, White TO, et al. Primary arthroscopic stabilization for
a first-time anterior dislocation of the shoulder. A randomized,
double-blind trial. J Bone Joint Surg Am Apr 2008;90(4):708-721.
C, Wirth M. Subluxations and dislocations about the glenohumeral joint.
In: Rockwood C, Green D, Bucholz R, et al., eds. Rockwood and Green’s
Fractures in Adults. Philadelphia: Lippincott-Raven, 1996; 1193-1339.
M, Harner C, Fu F. The role of the long head of the biceps muscle and
superior glenoid labrum in anterior stability of the shoulder. Am J
Sports Med 1994; 22:121-130.
Merchan E, Ortega M. The Magnuson-Stack operation for recurrent
anterior dislocation of the shoulder. A long-term follow-up of 44
operations. Int Orthop 1994; 18:356-358.
J, Feagin J, Abbott H. Modified axillary roentgenogram: a useful
adjunct in the diagnosis of recurrent instability of the shoulder. Clin
Orthop 1972;82:84-86.
P, DeBakker H, Obermann W. Radiographic views in recurrent anterior
shoullder dislocation: comparison of six methods for identification of
typical lesions. Acta Orthop Scand 1986;57:328-330.
J, Holmes E, Keller D, et al. Reduction of acute anterior shoulder
dislocations using the Milch technique. A study of ski injuries. J
Trauma 1981;21:802-804.
RA, Lin D, Stone ML, et al. Can the need for future surgery for acute
traumatic anterior shoulder dislocation be predicted? J Bone Joint Surg
Am 2007;89(8): 1665-1674.
RA, Williams B, Stone ML, et al. Open Bankart repair: correlation of
results with postoperative subscapularis function. Am J Sports Med
2005;33(10):1458-1462.
DT, Provencher MT, Mologne TS, et al. The modified Bristow procedure
for anterior shoulder instability: 26-year outcomes in Naval Academy
midshipmen. Am J Sports Med 2006;34(5):778-786.
R, O’Brien S, Warren R, et al. Capsular restraints to anterior
posterior motion in the shoulder. Orthop Trans 1988;12:727.
M, Tibone J, Yang B, et al. Glenohumeral joint translation after
arthroscopic thermal capsuloplasty of the rotator interval. J Shoulder
Elbow Surg 2003;12:139-143.
JF, Hawkins RJ. Classification and physical diagnosis of instability of
the shoulder. Clin Orthop Relat Res 1993(291):7-19.
WT, Melton LJ 3rd, Cofield RH, et al. Incidence of anterior shoulder
dislocation in Olmsted County, Minnesota. Clin Orthop Relat Res
1984(186):186-191.
G, Kirkland P, Emery R. Coracoid transposition for recurrent anterior
instability of the shoulder. A 20-year follow-up study. J Bone Joint
Surg 1995;77-B:73-76.
JT, Karas SG. The HAGL lesion: an arthroscopic technique for repair of
humeral avulsion of the glenohumeral ligaments. Arthroscopy
2005;21(4):498-502.
K, Senn E, Simmen B, et al. [Recurrence frequency after the first
traumatic shoulder dislocation]. Helv Chir Acta 1980;47:85-88.
H, Moriishi J, Dohi M, et al. Glenoid rim morphology in recurrent
anterior glenohumeral instability. J Bone Joint Surg 2003;85-A:878-884.
H, Moriishi J, Kanisawa I, et al. Arthroscopic osseous Bankart repair
for chronic recurrent traumatic anterior glenohumeral instability.
Surgical technique. J Bone Joint Surg Am 2006;88(Suppl 1 Pt 2):159-169.
P. The significance of the subscapularis muscle in the pathogenesis of
recurrent anterior dislocations of the shoulder. J Bone Joint Surg
1972;54-B:476-483.
Slaa R, Wijffels M, Brand R, et al. The prognosis following acute
primary glenohumeral dislocation. J Bone Joint Surg 2004;86-B:58-64.
S, Matsen F. An approach to the repair of glenohumeral ligament
avulsion in the management of traumatic anterior glenohumeral
instability. J Bone Joint Surg 1989; 71-A:506-513.
J, Ting A. Capsulorrhaphy with a staple for recurrent posterior
subluxation of the shoulder. J Bone Joint Surg 1990;72-A:999-1002.
PF, Steinbach LS, Feller JF, et al. Humeral avulsion of the anterior
shoulder stabilizing structures after anterior shoulder dislocation:
demonstration by MRI and MR arthrography. Skeletal Radiol
1996;25(8):743-748.
FP, Abboud JA, Hasan SA, et al. Arthroscopic and open Bankart repairs
provide similar outcomes. Clin Orthop Relat Res 2006;446:227-232.
M, Caspari R, Asselmeier M, et al. Arthroscopic transglenoid multiple
suture repair: 2- to 8-year results in 150 shoulders. Arthroscopy
1997;13:609-619.
J, Balduini F, Bonci C, et al. A modified Bristow-Helfet-May procedure
for recurrent dislocation and subluxation of the shoulder. Report of
212 cases. J Bone Joint Surg 1987;69-A(6):904-913.
P, Simon G, Stratford W, et al. Luxatio erecta: Persistent displacement
of the greater tuberosity after reduction. Orthop Rev 1993;22:855-858.
GA, Hou DD. MR arthrography of the posterior labrocapsular complex:
relationship with glenohumeral joint alignment and clinical posterior
instability. AJR Am J Roentgenol 2003;180(2):369-375.
der Zwaag H, Brand R, Obermann W, et al. Glenohumeral osteoarthrosis
after Putti-Platt repair. J Shoulder Elbow Surg 1999;8:252-258.
B, Deutsch A, Protomastro P, et al. The effects of radiofrequency
thermal capsulorrhaphy on glenohumeral translation, rotation, and
volume. J Shoulder Elbow Surg 2004;13:138-145.
VM, Sugalski MT, Levine WN, et al. Comparison of glenohumeral mechanics
following a capsular shift and anterior tightening. J Bone Joint Surg
Am 2005;87(6): 1312-1322.
J, Bowen M, Deng X, et al. Effect of joint compression on inferior
stability of the glenohumeral joint. J Shoulder Elbow Surg 1999;8:31-36.
J, Deng X, Warren R, et al. Static capsuloligamentous restraints to
superiorinferior translation of the glenohumeral joint. Am J Sports Med
1992;6:675-685.
JJ, Gill TJ, O’Hollerhan J D, et al. Anatomical glenoid reconstruction
for recurrent anterior glenohumeral instability with glenoid deficiency
using an autogenous tricortical iliac crest bone graft. Am J Sports Med
2006;34(2):205-212.
JH, Ryan JB, Arciero RA, et al. Arthroscopic versus nonoperative
treatment of acute shoulder dislocations in young athletes. Arthroscopy
1989;5(3):213-217.
JM, Vibert BT. Glenohumeral joint volume reduction with progressive
release and shifting of the inferior shoulder capsule. J Shoulder Elbow
Surg 2007;16(6): 810-814.
R, Strickland S, Cohen M, et al. Arthroscopic repair for traumatic
posterior shoulder instability. Am J Sports Med 2003;31:203-209.
KR. A randomized evaluation of immobilization in external rotation
after primary shoulder dislocation. Proceedings of the 75th Annual
Meeting of the American Academy of Orthopaedic Surgeons. San Francisco,
CA: AAOS; 2008.
M, Groh G, Rockwood C. Capsulorrhaphy through an anterior approach for
the treatment of atraumatic posterior glenohumeral instability with
multidirectional laxity of the shoulder. J Bone Joint Surg
1998;80-A:1570-1578.
M, Rockwood C. Subluxations and dislocations about the glenohumeral
joint. In: Bucholz R, Heckman J, eds. Rockwood and Green’s Fractures in
Adults. Philadelphia: Lippincott Williams & Wilkins, 2001;
1109-1207.
M, Seltzer D, Rockwood C. Recurrent posterior glenohumeral dislocation
associated with increased retroversion of the glenoid. A case report.
Clin Orthop 1994;308: 98-101.
EM, Cheng JC, Dickson K. Humeral avulsion of glenohumeral ligaments as
a cause of anterior shoulder instability. Arthroscopy
1995;11(5):600-607.
N, Itoi E, Tuoheti Y, et al. Effect of rotator interval closure on
glenohumeral stability and motion: a cadaveric study. J Shoulder Elbow
Surg 2006;15(6):750-758.
T, Yoshiya S, Kurosaka M, et al. Luxatio erecta (inferior dislocation
of the shoulder): a report of five cases and a review of the
literature. Am J Orthop 2003;32: 601-603.
S, Marcacci M, Loreti I, et al. Results of the original Putti-Platt
procedure for shoulder instability: review of Putti’s scholar
experience. Knee Surg Sports Traumatol Arthrosc 2000;8:314-319.
L, Veith I. Great Ideas in the History of Surgery: Clavicle, Shoulder,
and Shoulder Amputations. Baltimore: Williams & Wilkins, 1961.
J, Matsen F. Complications about the glenohumeral joint related to the
use of screws and staples. J Bone Joint Surg 1984;66-A:175-180.
