Osteogenesis Imperfecta
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Osteogenesis Imperfecta
Osteogenesis Imperfecta
Paul D. Sponseller MD
Description
-
OI is a collagen disorder causing osseous fragility.
-
May affect bones, teeth, eyes, hearing, and soft tissue
-
The Sillence classification (1,2) is the most widely accepted.
-
Type I: Mild, common form:
-
Fractures occur in later childhood and decrease toward adolescence.
-
Patients with type IA do not have dentinogenesis imperfecta; those with type IB do.
-
-
Type II: Lethal in the perinatal period
-
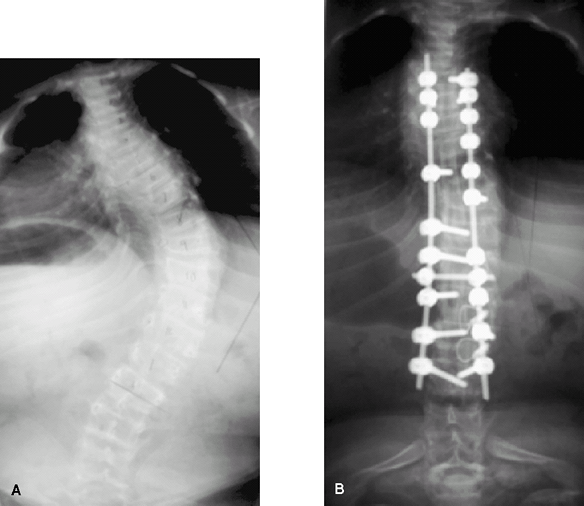
Type III (Fig. 1): Most severe survivable form
-
Type IV: Moderately severe
-
Type V: Moderately severe, with dislocated radial heads and hyperplastic callus
 Fig. 1. Typical features of type III OI include long, thin, bowed, osteopenic bones.
Fig. 1. Typical features of type III OI include long, thin, bowed, osteopenic bones.
-
Pediatric Considerations
-
Types II and III are diagnosed at birth with perinatal death or intrauterine fractures, respectively.
-
Types I and IV may be diagnosed after birth, but generally in early childhood.
-
In the milder forms, the incidence of fractures decreases with age.
Epidemiology
Prevalence
Overall, affects ~1 per 10,000 persons (1)
Risk Factors
None, other than heredity
Genetics
-
All types have a moderately high rate of spontaneous mutation.
-
Type I: Autosomal dominant with variable penetrance and expressivity
-
Type II: Autosomal recessive or dominant
-
Type III: Autosomal recessive
-
Type IV: Autosomal dominant with variable penetrance and expressivity
-
Type V: Autosomal dominant
Etiology
-
Defects in type I collagen
-
Type I collagen:
-
Is the main collagen in bone matrix
-
Is a triple helix
-
Has glycine as every 3rd amino acid:
-
Substitutions of this amino acid impair coiling of the nonmutated product and exert a dominant negative effect.
-
-
Associated Conditions
-
Platybasia, potential brainstem compression
-
Dentinogenesis imperfecta
-
Hypermobile joints with increased incidence of joint dislocation
-
Inguinal, umbilical, and diaphragmatic hernias
Signs and Symptoms
-
Fragility of bone
-
Short stature
-
Scoliosis, back pain
-
Defective dentinogenesis of deciduous or permanent teeth, or both, resulting in soft, translucent, and brownish teeth
-
Middle-ear deafness
-
Laxity of ligaments, which results in hypermobile joints and potential ankle instability
-
Blue sclerae
-
Skull: Patients may have a widened cranium and small, triangular faces.
-
Increased incidence of musculoskeletal pain in adulthood
-
Symptoms of basilar invagination may
include respiratory depression, dyscoordination, spasticity, weakness,
contracture, and changes in voice.
Physical Exam
-
OI is diagnosed by fractures of unusual frequency or mechanism.
-
A positive family history and signs such
as abnormal dentition, blue sclerae, ligament laxity, scoliosis, or
bone bowing/fragility are helpful.
Tests
Lab
-
Cultures of dermal fibroblasts for
characterization of type I collagen may be part of the workup; absence
of matching may not exclude diagnosis. -
DNA mutation analysis (blood test) is available through specialized labs.
P.293
Imaging
-
Radiography may reveal systemic osteopenia.
-
Other radiographic findings may include
long bones with narrow diaphyses and bowing, protrusio acetabuli,
vertebral or other fractures, scoliosis, and a “concertina” femur. -
Bones are gracile and osteopenic.
-
The pelvis may have a trefoil shape, and protrusio acetabuli is common.
-
The osteopenic vertebrae may fracture
easily, resulting in a flattened or biconcave shape; severe scoliosis
and kyphosis may develop. -
The skull may exhibit wormian bones (inclusions in the suture lines).
-
Severe cases: Metaphyses may appear cystic.
Diagnostic Procedures/Surgery
-
Dermal punch biopsy to analyze collagen if routine diagnostic criteria are inconclusive (1)
-
The synthesis and structure of type I collagen produced by the cultured fibroblasts obtained from biopsy then can be analyzed.
-
The mutation can be characterized by specialized lab tests, from DNA in a blood test.
Pathological Findings
-
The bone often appears woven and only occasionally has a normal lamellar pattern.
-
The cortices are thin, and the trabeculae in the metaphyses are markedly attenuated.
-
The collagen fibers of the cornea and skin have a looser arrangement than normal (1).
Differential Diagnosis
-
Infant with very low birth weight
-
Primary hyperparathyroidism
-
Scurvy
-
Hypophosphatasia
-
Achondrogenesis
-
Chondroectodermal dysplasia
-
Juvenile osteoporosis
-
Nonaccidental injury (child abuse)
-
Congenital syphilis
-
Malignancy (e.g., leukemia)
-
Rickets
-
It may be difficult to discern child abuse from OI (1,3).
-
Fractures from child abuse occur most frequently in children <1 year old (3).
-
Multiple fractures at different stages of
healing, posterior rib fractures, and metaphyseal corner fractures are
highly specific for nonaccidental injury.
-
-
A positive family history and signs such
as abnormal dentition, blue sclerae, or systemic osteopenia revealed by
radiographs may be helpful in the diagnosis of OI.
General Measures
-
Treatment depends on the type of OI.
-
Type I may have little impact on the patient.
-
Type II: Lethal perinatal OI:
-
Has some degree of variability
-
In the most severe cases, early death
-
-
Types III and IV:
-
Greatest therapeutic challenges (3–8).
-
Treatment with growth hormone, calcium, and calcitonin has shown little benefit (1,4).
-
-
-
Diphosphonates treatment (pamidronate,
alendronate, etc.) may improve (but will not normalize) bone density,
decrease fracture frequency, and improve quality of life in children
but not adults (1,4,8). -
Molecular treatments are a goal for the future.
-
Exercise: A physical therapist should be
involved with most children to assess their abilities and plan
realistic goals, working to develop ambulatory potential and proceeding
with appropriate seating, including a wheelchair if required (3). -
Fractures:
-
Usually treated nonoperatively:
-
Fractures heal readily.
-
A fracture is less likely to heal well if substantial angulation develops (1,5).
-
Use of lightweight splints or braces may help in getting the child to bear weight quickly.
-
-
Internal fixation may be used if management by closed treatment proves difficult (5,8,9).
-
Intramedullary fixation is superior to plates and screws because screws tend to dislodge from the weakened bone.
-
A new fracture is more likely to occur at the end of a plate (“stress riser” effect).
-
-
Special Therapy
Physical Therapy
-
Important component of treatment plan (3):
-
Goals for physical therapy: Muscle and bone strengthening, standing, and ambulation
-
Hydrotherapy for extremities allows active motion and strengthens musculature (3).
-
Orthotics are an important adjunct (3).
-
Braces should be lightweight and total contact in design, with joint hinges (3).
-
Medication
First Line
Diphosphonates
P.294
Surgery
-
Anesthesia:
-
Patients with OI are at high risk for
many reasons: Restricted neck and jaw mobility, pulmonary function
abnormalities from thoracic cage distortion, dentinogenesis imperfecta,
and valvular heart disease -
Avoid anticholinergic agents because they can cause malignant hyperthermia.
-
-
Osteotomy:
-
At ~5 years of age, corrective osteotomies of larger bones with intramedullary fixation may be performed if indicated (5).
-
The Bailey-Dubow or Fassier elongating rod (Fig. 2) diminishes the reoperation rate (5).
-
Intramedullary nail placement is optimal for children with the potential to stand who have severe bowing or repeated fractures.
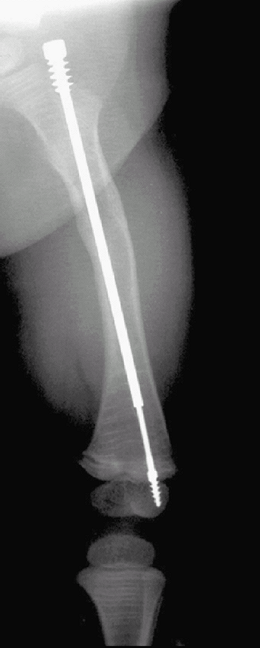 Fig.
Fig.
2. The Fassier rods are telescoping and expand with growth. Also note
multiple transverse lines in bone from diphosphonate administration. -
No absolute rule exists for when
intramedullary nail placement should be performed; risk-to-benefit
analysis should consider recurrent fracture and deformity versus
infection, pain, and the need for nail replacement (5).
-
-
Scoliosis:
-
Curves tend to advance relentlessly; bracing has little effect on deformity progression.
-
New instrumentation methods are changing the approach to scoliosis in OI (7) (Fig. 3).
-
Curves may be fused early (at 40°) to
halt the relentless progression; this procedure is important in
maintaining function and in preventing respiratory complications.
-
-
A less obvious area of spinal involvement is at the craniocervical junction.
-
Basilar invagination may result and present with neurologic signs resulting from brainstem compression (7).
-
Once diagnosed, decompression and spinal stabilization are recommended.
![]() Fig. 3. Scoliosis in osteogenesis before (A) and after (B) surgical correction with rods and screws.
Fig. 3. Scoliosis in osteogenesis before (A) and after (B) surgical correction with rods and screws.
-
Because of multiple potential deformities, patients with OI are best managed in a specialized clinic.
Prognosis
-
Type II disease is lethal perinatally.
-
Type III (next most severe form) patients often require multiple orthopaedic procedures.
-
Types I and IV are milder forms of OI, with type I being the mildest.
-
The fracture rate in all types decreases around puberty.
-
Presenile hearing loss may be the most severe long-term handicap in patients with type I disease.
Complications
A softened base of the skull may lead to platybasia and potential neurologic sequelae (7).
Patient Monitoring
-
Scoliosis:
-
Patients with OI must be followed closely from an early age to monitor the development and progression of scoliosis.
-
Continue to monitor patients as adults.
-
-
Neurologic signs: Patients must be
followed for neurologic signs of brainstem compression that may be
caused by basilar invagination (7).
P.295
References
1. Cole WG. Advances in osteogenesis imperfecta. Clin Orthop Relat Res 2002;401:6–16.
2. Sillence
DO, Rimoin DL, Danks DM. Clinical variability in osteogenesis
imperfecta–variable expressivity or genetic heterogeneity. Birth Defects Orig Artic Ser 1979;15:113–129.
DO, Rimoin DL, Danks DM. Clinical variability in osteogenesis
imperfecta–variable expressivity or genetic heterogeneity. Birth Defects Orig Artic Ser 1979;15:113–129.
3. Marini JC, Gerber NL. Osteogenesis imperfecta. Rehabilitation and prospects for gene therapy. JAMA 1997;277:746–750.
4. Glorieux FH, Bishop NJ, Plotkin H, et al. Cyclic administration of pamidronate in children with severe osteogenesis imperfecta. N Engl J Med 1998;339:947–952.
5. Luhmann
SJ, Sheridan JJ, Capelli AM, et al. Management of lower-extremity
deformities in osteogenesis imperfecta with extensible intramedullary
rod technique: a 20-year experience. J Pediatr Orthop 1998;18:88–94.
SJ, Sheridan JJ, Capelli AM, et al. Management of lower-extremity
deformities in osteogenesis imperfecta with extensible intramedullary
rod technique: a 20-year experience. J Pediatr Orthop 1998;18:88–94.
6. Ring D, Jupiter JB, Labropoulos PK, et al. Treatment of deformity of the lower limb in adults who have osteogenesis imperfecta. J Bone Joint Surg 1996;78A:220–225.
7. Sawin
PD, Menezes AH. Basilar invagination in osteogenesis imperfecta and
related osteochondrodysplasias: medical and surgical management. J Neurosurg 1997;86:950–960.
PD, Menezes AH. Basilar invagination in osteogenesis imperfecta and
related osteochondrodysplasias: medical and surgical management. J Neurosurg 1997;86:950–960.
8. Seikaly MG, Kopanati S, Salhab N, et al. Impact of alendronate on quality of life in children with osteogenesis imperfecta. J Pediatr Orthop 2005;25:786–791.
9. Stott NS, Zionts LE. Displaced fractures of the apophysis of the olecranon in children who have osteogenesis imperfecta. J Bone Joint Surg 1993;75A:1026–1033.
Codes
ICD9-CM
756.51 Osteogenesis imperfecta
Patient Teaching
-
Understanding the necessity of muscle strengthening and ROM exercises is important.
-
Family members must monitor the skin around braces and casts.
-
They must also try to recognize when fractures occur and be compliant with frequent follow-up.
FAQ
Q: Does exercise improve bone density in OI?
A: It improves it, but not to a normal degree.
Q: When, if ever, should patients with OI be treated with intramedullary nails?
A:
If they have repeated fractures, the bowing interferes with function,
and the age and size allows durable correction. Some patients have such
severe OI that surgery is not successful.
If they have repeated fractures, the bowing interferes with function,
and the age and size allows durable correction. Some patients have such
severe OI that surgery is not successful.