Dupuytren’s Disease
a well-known but poorly understood clinical entity involving the palmar
and digital fascia of the hand. From the patient’s perspective, this
disease begins as small nodules or lumps in the palm or fingers, which
may eventually develop into longitudinally oriented cords or bands that
contract. When this happens, a condition known as Dupuytren’s contracture results (Figure 4-1).
disease involved the palmar fascia. He recommended fasciotomy—as did
his student, Astley Cooper of London. However, it was in 1831, at the
Hotel Dieu in Paris, that Dupuytren presented a lecture, later
transcribed by one of his students, that described the disease within
the palmar fascia. Dupuytren recommended open fasciotomy through a
transverse incision, and also recommended it be left open to heal.
Northern European and Scandinavian ancestry, and is more common in
males than females. It has a genetic etiology and has been associated
with seizure disorders, alcohol and tobacco use, and HIV. Hormones such
as peptides (cytokines) may play a role in the development of DD and
may promote transformation of fibroblasts into myofibroblasts.
fibrous bundles of the fascia. During the active stage of the disease
when progressive joint contracture occurs, myofibroblasts are the
predominant cells. These cells demonstrate cell-to-cell and
cell-to-stroma attachments. The myofibroblasts contain contractile
elements called alpha smooth muscle actin. Figure 4-2 depicts the cellular model of contracture in DD.
collagen found in DD is type III. That’s the same type of collagen
identified in scar tissue. Normal palmar fascia is mainly type I
collagen with only small amounts of type III collagen. Type IV and VI
collagen with fibronectin are seen in early stages of DD, when
myofibroblasts proliferate.
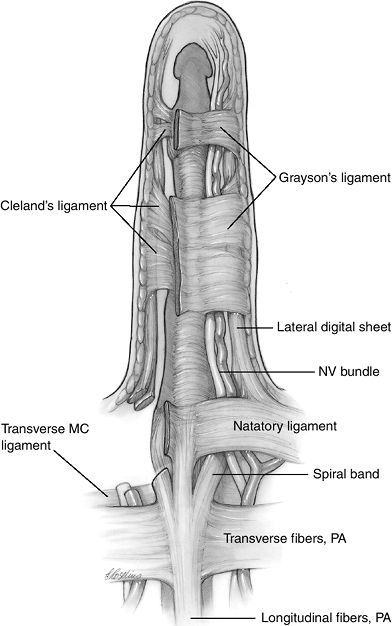
portion of the palm with longitudinal, transverse, and vertical fibers.
It is distinguished from the covering of the thenar and hypothenar
eminences by its triangular shape and greater thickness. The
longitudinal fibers of the palmar fascia represent the distal
continuation of the palmaris longus (when present). These fibers, which
begin as a conjoined apex at the base of the palm, form bundles in the
middle and distal palm that run to the corresponding four fingers and,
in some instances, to the thumb. The longitudinal fibers are
essentially parallel to the deeper flexor tendons; because of this
arrangement, they are sometimes called pretendinous bands. The four bundles of longitudinally oriented fibers overlay transverse fibers
in the palm, which are located at the junction of the middle and distal
thirds of the palm and over the metacarpophalangeal (MCP) joints. The
transverse fibers of the PA course beneath the longitudinal cords, from
the ulnar side of the small finger to the radial side of the index
finger. In the thumb-index finger web space, the proximal commissural ligament (PCL) is the radial continuation of these transverse fibers. The more distal counterpart of the PCL is the distal commissural ligament
(DCL), which is more longitudinally oriented and which spans the space
between the MCP joint of the thumb and index finger. Both the PCL and
DCL course toward the thumb’s MCP joint, where they send attachments to
the undersurface of the skin. The deep portion of the DCL sends fibers
to attach on both sides of the flexor pollicis longus (FPL) sheath. The
more longitudinal orientation of the DCL may be a factor in its more
likely involvement in DD, although both the DCL and PCL may be involved
in Dupuytren’s contracture. The PCL and DCL
are
usually thinner and less noticeable than the transverse fibers between
the fingers. Both the longitudinal and transverse fibers course through
the vertical septa to reach the transverse metacarpal ligament. The
third component of the palmar fascia consists of the nine vertical
(sagittal) septa, called the fibers of Legueu and Juvara, which are
located deep to the transverse fibers. They form the sides of eight
canals, four of which contain the underlying finger flexor tendons, and
four adjacent ones that contain the lumbrical muscles and neurovascular
bundles. These paratendinous septa, along with the transverse palmar
aponeurosis, form a fibrous tunnel system that has been described as
the palmar aponeurosis pulley. These nine vertical septa are anchored
to the transverse metacarpal ligament, palmar interosseous, and
adductor fascia, and they divide the distal portion of the central
palmar space into eight canals. The normal anatomy of the palmar fascia
is depicted in Figure 4-3.
 |
|
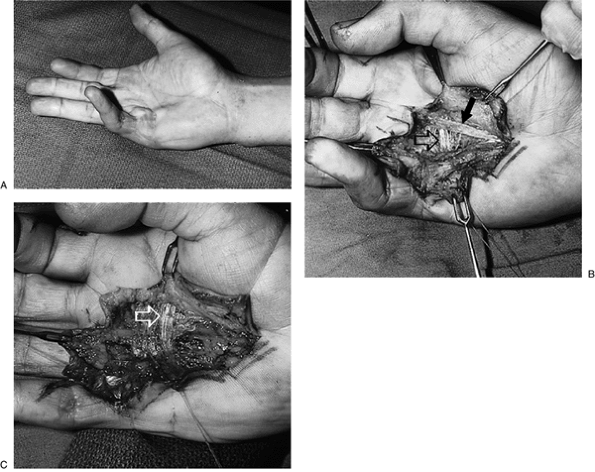
Figure 4-1 Clinical appearance of Dupuytren’s disease. (A)
An elderly male with a several year history of progressive “drawing down” of his left little finger. Note the prominent cord that begins in the palm and extends into the finger and that limits passive and active extension of the finger. (B) Another patient with recurrent Dupuytren’s disease showing contracture of the web space between the left ring and little finger (arrow), and “dimpling” of the skin (arrow) in the palm on the right hand. |
 |
|
Figure 4-2 Diagrammatic depiction of the pathogenesis of Dupuytren’s disease. (A) The perivascular fibroblast in an early nodule, surrounded by fibrillary material penetrating into the palmar fascia. (B) The myofibroblast that appears when clinical contracture is apparent. (C) The myofibroblasts have cell-to-cell and cell-to-stroma connections. (D)
The mature cord consists of longitudinally oriented type III collagen, with a few residual cells of fibroblasts and myofibroblasts. (Redrawn after Chiu HF, McFarlane RM. Pathogenesis of Dupuytren’s contracture: a correlative clinical-pathological study. J Hand Surg 1978;3A:1–10.) |
 |
|
Figure 4-3 The palmar fascia and its associated ligaments. See the text for details.
|
structures must note that these structures are only a part of a complex
tissue consortium designed to meet a variety of functional demands.
This complex three-dimensional network may be considered a fibrous
skeleton or framework designed to assist in the hand’s mechanical
functions. Compression loading is a common force applied to the hand,
and requires a system of shock absorption. In the hand, one method of
shock absorption is to contain somewhat compliant tissues, such as fat
or muscle, in compartments that can change shape but not volume. This
is amply demonstrated in the palm, with its various layers of
multidirectional fascia that contain and compartmentalize fat and
muscle while conforming to the shape or contour of the object being
grasped or manipulated.
to flex while maintaining the skin in position. The skin folds at
prominent creases that are minimally anchored; this contrasts to the
skin on the adjacent sides of the crease, which possess multiple strong
anchor points. This allows the relatively unanchored skin to fold,
while the anchored skin is held in place. These fascial anchors may be
vertical, horizontal, or oblique, depending on the specific need of the
skin envelope. A good example is the horizontal attachments of the
superficial fibers of the pretendinous bands, which attach to the
dermis of the distal palm. This arrangement resists horizontal shearing
forces in gripping actions, such as holding a hammer or a golf club.
The PA, which includes the nine vertical septa anchored to the deep
transverse metacarpal ligament, is tensed with power grip and thus
anchors the skin to the skeleton of the hand.
mentioned transverse metacarpal ligament that attaches to the palmar
plates of the MCP joints plays a role in maintaining the transverse
metacarpal arch, as do the transverse fibers of the palmar fascia and
the natatory ligaments.
thumb may play a role in limiting abduction, and thus may indirectly
limit the impact of potentially destabilizing forces that might be
applied to the digits.
surrounding substantial fibrous tissue and fat pads. When the hand is
compressed, as in making a fist, the incompressible fascia may act as a
venous pumping mechanism. This is in contrast to the large dorsal veins
on the dorsum of the hand, which are surrounded by loose areolar
tissue. The nerves in the palm are protected by fascial structures;
those near the base of the fingers are protected by fat pads
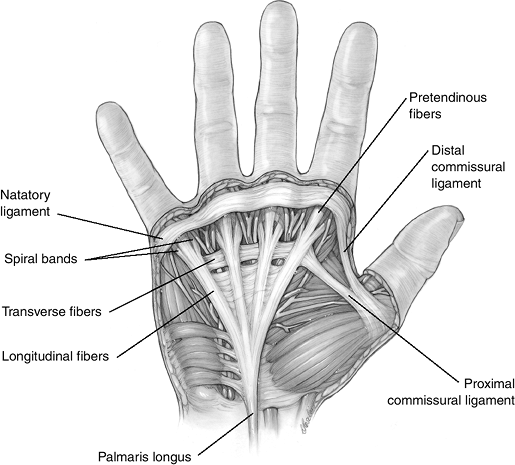
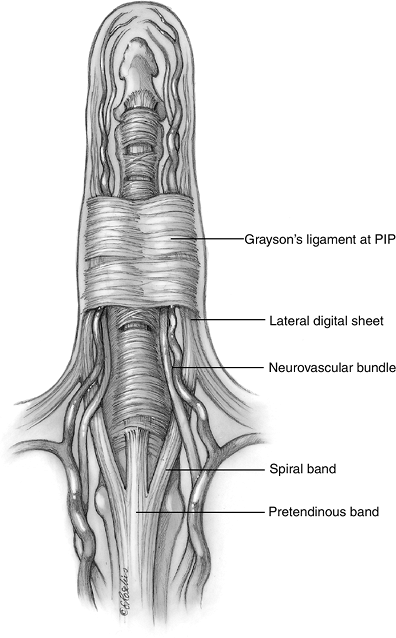
passes on each side of the flexor sheath to the region of the MCP
joint. The natatory ligaments have transverse as well as curved fibers
that follow for the contour of the webs. The curved or distal
continuations of these fibers join the lateral digital sheet. The
lateral digital sheet is a condensation of the superficial digital
fascia on each side of the finger; it receives fibers from the natatory
ligament, the spiral band, and Grayson’s ligament. The retaining skin ligaments of Grayson and Cleland
stabilize the skin during flexion and extension of the finger.
Grayson’s ligaments are palmar to the neurovascular bundles, and pass
from the skin to the flexor tendon sheath. These ligaments form a tube
from the proximal aspect of the finger to the distal interphalangeal
joint, where the digital nerves and vessels always can be found during
surgical dissection. The distal palmar and digital fascia is depicted
in Figure 4-4.
-
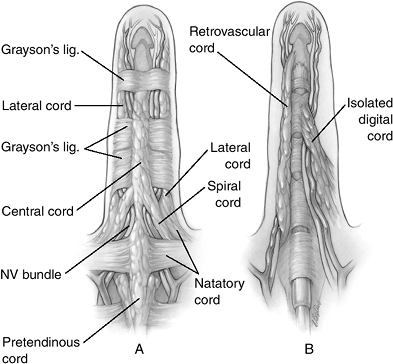
DD begins in the palm as a nodule that represents the early manifestation of the disease in the longitudinal fibers of the PA.
-
Histologically, nodules are a collection of fibroblasts and myoblasts in a fibrous tissue matrix.
-
These nodules may coalesce to form cords that contract and produce the characteristic contracture deformity.
-
This may appear clinically as a nontender nodule in the palm, or a skin dimple of retracted skin.
-
The nodules form in and along the longitudinal axis of the rays. The ring and little finger are most commonly involved.
![]() Figure 4-4 Distal palmar and digital fascia. See the text for details.
Figure 4-4 Distal palmar and digital fascia. See the text for details. -
As the disease progresses, it spreads to
the fingers and produces the typical contracture of the MCP and often
the proximal interphalangeal (PIP) joints. -
Recognition of the distinct anatomic
separation of the longitudinal (involved) and transverse (noninvolved)
fibers of the PA, and the distal separation of the longitudinal fibers
into three layers, allows the surgeon to selectively excise the
diseased tissue instead of all fascial tissue.
-
The pretendinous bands of the PA are the most common places for Dupuytren’s contracture to occur.
-
A palpable nodule may progress to a prominent pretendinous cord, which may produce a flexion contracture of the MCP joint.
-
Although the pretendinous cord is the primary cause of flexion contracture of the MCP joint, it may join the central cord of the finger that extends well beyond the PIP joint.
-
The central cord originates from the superficial fibrofatty digital fascia on the flexor side of the finger.
-
The central cord always is in continuity with the pretendinous cord.
-
Only the longitudinal fibers (pretendinous bands) of the PA are involved; the transverse fibers are ideally left behind during excision of the diseased palmar fascia.
-
The transverse fibers to the thumb web,
the PCL, and the DCL, which are more obliquely oriented and subject to
tension, may contract. The loss of abduction and extension of the thumb
can result.
-
The natatory ligaments frequently are
diseased. Because they not only span the finger web space but also send
fibers distally into the fingers, they may be responsible for web space
contracture as well as PIP joint contracture.
the fibrofatty fascia on the flexor aspect of the fingers; the distal
continuation of the pretendinous fibers, called the spiral band;
the distal (longitudinal) extension of the natatory ligaments;
Grayson’s ligament (as terminal attachment for the spiral bands); and
the lateral digital sheet.
-
This tissue forms the central cord in the
finger, joining the pretendinous cord of the palm to form a continuous
cord from the palm to the middle phalanx. -
It often divides into two tails that attach to the flexor sheath and osseous middle phalanx.
-
The fibers (layer two) are the deep and distal continuation of the pretendinous band on each side of the flexor sheath.
-
They pass deep to the neurovascular
bundle as they proceed to the lateral side of the finger, and then
migrate superficial to the neurovascular bundle to attach to the middle
phalanx by means of Grayson’s ligament. -
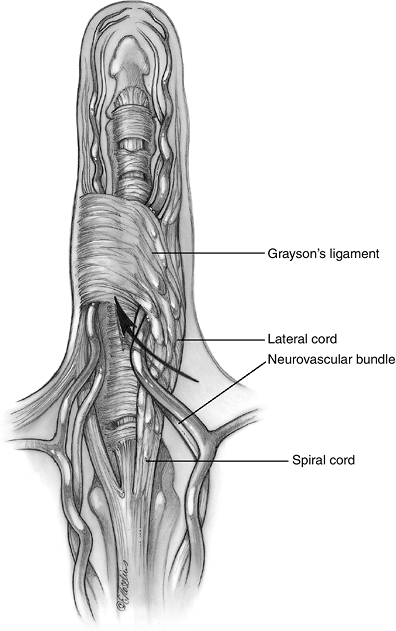
This configuration progressively
displaces the neurovascular bundle with increasing PIP joint
contracture, first toward the midline, then proximally, and then
superficially. This places the neurovascular bundle at considerable
risk during surgery because the neurovascular bundle spirals around
this fascial structure, called the spiral cord. -
The spiral cord is either a continuation
of the spiral band or arises from the musculotendinous junction of an
intrinsic muscle; it attaches distally to the flexor sheath and bone in
the middle phalanx.
-
Disease and contracture of the transverse
elements of the natatory ligaments form the natatory cords that produce
contracture of the finger web spaces, with loss of abduction of the
fingers. -
The distal digital extension of the
natatory ligament joins the spiral band, and these two bands
subsequently join the lateral digital sheet to form the lateral cord.
-
Grayson’s ligaments, located in the
middle and proximal phalanges, pass from the digital flexor sheath,
palmar to the neurovascular bundle, to the lateral digital sheet. They
are in the same fascial plane as the natatory ligaments. -
They provide attachment for the spiral cords to the middle phalanx.
-
The lateral digital sheet is a condensation of the superficial fascia on either side of the finger.
-
It receives fibers from the natatory and spiral ligaments, as well as from Grayson’s and Cleland’s ligaments.
-
When diseased, it is known as the lateral cord.
-
The lateral cord runs from the natatory ligament to the lateral digital sheet.
-
It usually does not cause PIP joint
contracture, except on the ulnar side of the small finger. There it
attaches to an abductor cord overlying the ADM and can cause PIP joint
contracture.
-
This cord lies deep to the neurovascular
bundle. It arises from the periosteum of the lateral base of the
proximal phalanx, passes close to the PIP joint, and ends at the
lateral aspect of the distal phalanx. -
It is the usual cause of DIP joint contracture, and an occasional cause of PIP joint contracture.
-
Isolated cords may arise in the fingers as single or double cords without any attachments in the palm.
-
These cords arise from the periosteum at the base of the proximal phalanx in conjunction with adjacent ligaments.
-
They pass distally to displace and then
cross the neuro-vascular bundle, inserting on the tendon sheath or bone
of the middle phalanx. -
These cords may result in a significant loss of extension of the PIP joint, and cause isolated contractures.
-
Figure 4-5 demonstrates the pathologic tissues in the distal palm and finger in DD.
-
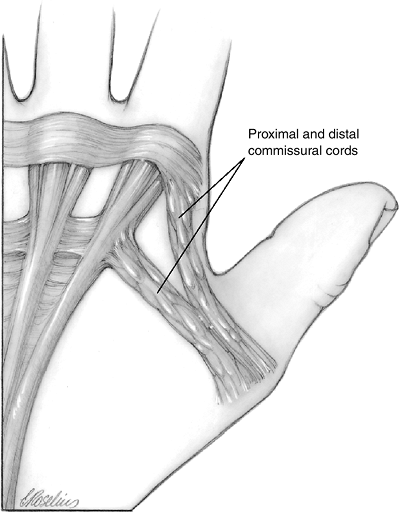
Although only the longitudinal fibers
(pretendinous bands) of the palmar fascia are involved in the hand, the
transverse fibers to the thumb web, PCL, and DCL are more obliquely
oriented and are subject to tension. -
If diseased, they may contract and be responsible for loss of abduction and extension of the thumb (Figure 4-6).
 |
|
Figure 4-5 Pathological anatomy of the distal palmar and digital anatomy. (A) The more superficial diseased elements. (B) The deeper diseased elements.
|
 |
|
Figure 4-6 Fascial involvement in the first web.
|
relationship between fascial bands/ligaments, cords, and the clinical
result of cord formation. The convention adopted here is that fascial
bands or ligaments are normal structures and that cords are their
pathological counterparts
currently available. Recurrence is likely, and surgery may be
associated with complications such as vascular compromise to a digit,
skin necrosis, hematoma, infection, nerve injury, failure to completely
relieve the contracture, and irreversible stiffness with or without
reflex sympathetic dystrophy. DD that presents at an early age carries
a greater potential for recurrence. Contractures in younger patients
are often more severe, and repeated surgery is often required. The
long-term prognosis for a suitable result is diminished when the
disease begins at an early age.
the surgeon and the patient, and are based on the progression of the
disease and the loss of function. Manifestations of functional loss may
include difficulty or embarrassment while shaking hands, placing the
hand in tight places, such as the pocket, or a variety of functional
activities related to everyday use. Some surgeons use a certain or set
degree of contracture to propose surgery. This may be useful in some
circumstances, but must be tailored to the individual needs of the
patient.
the most difficult to treat and obtain a satisfactory release. However,
the MCP joint seldom manifests a permanent contracture after release.
An experienced DD surgeon has noted that when the PIP joint contracture
was less than 30 degrees, the patient was more often made worse with surgery than made better.
into the cords that are causing contracture is currently under study.
The technique involves injection of the material into the substance of
the cord, followed by passive extension of the affected joint to
stretch or rupture the cord.
is not a definitive procedure. It may, however, serve the needs of some
selected patients. It can serve as a preliminary procedure to release a
finger from the palm for hygiene purposes prior to a more comprehensive
fasciectomy. Fasciotomy may also be used as
a definitive procedure in those patients who have associated medical
problems that would dictate a less comprehensive approach. A fasciotomy
may be performed under local anesthesia and the wound left open
followed by early motion. This approach may serve the needs of some
patients better than a more comprehensive procedure. Although closed or
blind fasciotomy was used in the past, open fasciotomy is more commonly
used today.
Prophylactic removal of normal or nondiseased fascia is not indicated,
and may increase the probability of postoperative complications.
|
Table 4-1 Dupuytren’s disease: fascial bands that may form contracture cords
|
||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||
with DD in each patient. Such plans must include management of the
skin, of the diseased fascia, and of joint contracture. Various
techniques will be used based on the surgeon’s experience and the needs
of the patient. Open techniques, skin grafts, Z-plasties, and PIP joint
release may be required.
-
The diseased fascia is incised rather than excised, and the wounds are left open to heal by secondary intention.
-
Sterile dressings protect the incisions and healing usually occurs within 3 weeks.
-
Immediate closure of the incisions would result in a recurrence of the flexion posture, especially at the MCP joints.
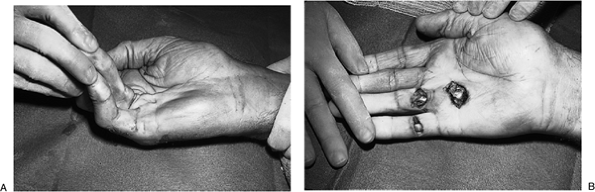 Figure 4-7 Open fasciotomy. (A) Preoperative appearance showing significant contractures at the MCP and PIP joints of the ring and little fingers. (B) Release of the contractures. The incisions were left open,
Figure 4-7 Open fasciotomy. (A) Preoperative appearance showing significant contractures at the MCP and PIP joints of the ring and little fingers. (B) Release of the contractures. The incisions were left open,
and kept covered with nonadherent sterile dressings until healed at 3
weeks. This technique is useful for patients that may not tolerate a
more comprehensive procedure. -
Exercises are initiated immediately after surgery.
-
An open fasciotomy is illustrated in Figure 4-7.
-
This technique was first published in
1964, and has proved to be a useful method for dealing with apparent
skin loss following palmar, or even digital, fasciotomy or fasciectomy. -
Closure of these incisions often results in a flexed posture at the MCP and/or the PIP joints because of skin contracture.
-
Leaving the incisions open avoids this problem of, or the necessity for, a skin graft.
-
The method is used based on the experience of the surgeon and the needs of the patient.
-
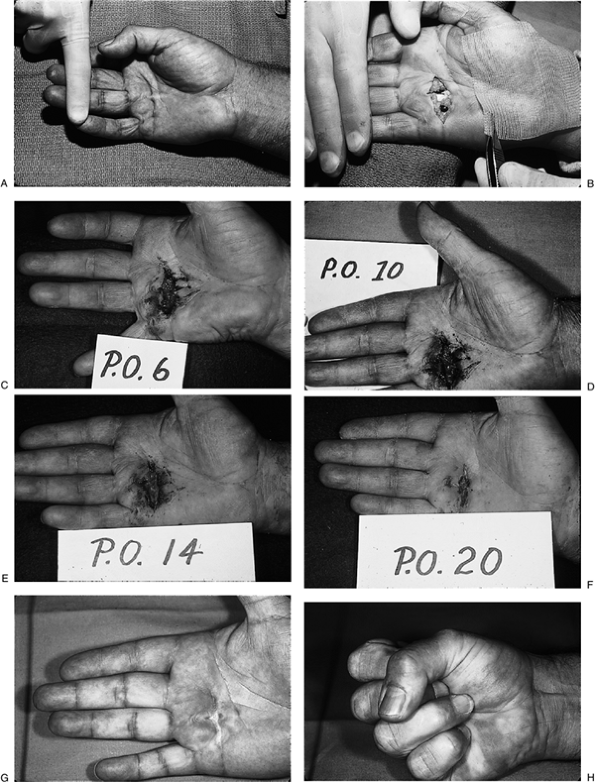
Figure 4-8 depicts the preoperative and postoperative healing sequence using this method.
 |
|
Figure 4-8 The open (or McCash) technique. (A) Preoperative appearance. (B) Appearance immediately after fasciectomy and just before application of the non-adherent sterile dressing. (C) Appearance at postoperative day 6, (D)day 10, (E) day 14, and (F) day 20. (G–H) Postoperative appearance at 2 months showing good extension and flexion.
|
 |
|
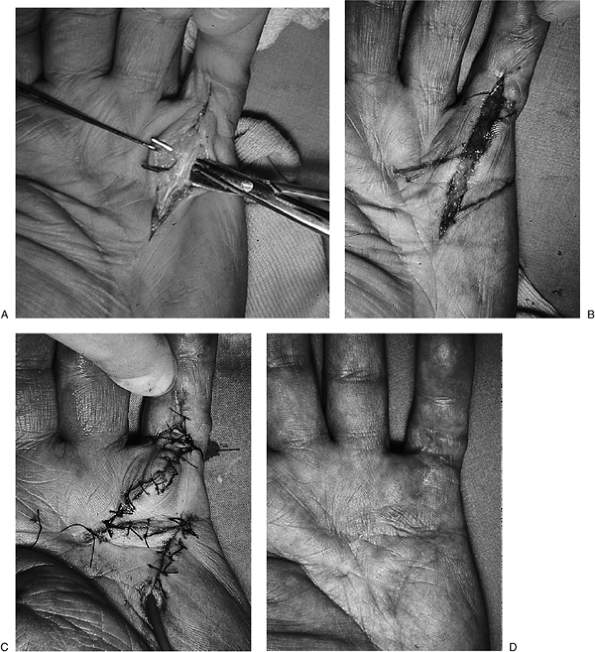
Figure 4-9 The longitudinal skin incision with Z-plasty closure. (A) Note the isolated diseased cord of palmar fascia elevated by the scissors. (B)
A double-running Z-plasty has been laid out in proximity to the distal palmar crease and the MCP flexion crease of the little finger. (C) The flaps are rotated and sutured in place. (D) The result 2 months postoperatively. |
-
In addition to the transverse incisions previously noted in Figures 4-7 and 4-8, longitudinal incisions with Z-plasty closures may be used to excise the diseased fascia in the palm and digit.
-
Such incisions are ideally suited for single ray involvement (Figure 4-9).
-
The longitudinal incision with a Z-plasty
closure may also be used for more than one ray involvement of disease
confined to the palm. -
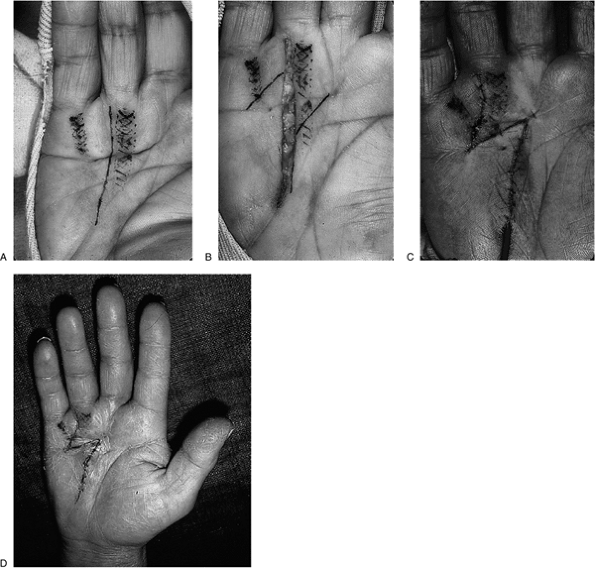
Figure 4-10 illustrates the use of a longitudinal incision in the palm, with Z-plasty closure for involvement of two rays.
-
The Z-plasty should be laid out with reference to the palmar and digital flexion creases.
-
Surgeons should handle the flaps carefully, keeping them as thick as possible to preserve their blood supply.
-
These longitudinal
incisions that cross the flexion creases should never be used without
Z-plasty closure, because a pronounced scar that is associated with
significant contracture will result.
 |
|
Figure 4-10 The longitudinal incision and Z-plasty closure for disease encompassing two rays in the palm. (A)
The longitudinal incision is laid out between the ring and little finger rays. The cross-hatched marks denote the underlying fascial cords. (B) The cords have been removed and the Z-plasty is laid out centered about the distal palmar crease. Note that the oblique limbs of the Z are carried to the distal palmar crease, and that the incision axis and two oblique limbs are equidistant. (C) The flaps are rotated and the distal palmar crease is restored. (D) The result at 8 days postoperative, showing that the flaps are viable and healing satisfactorily. |
-
This incision is widely used to expose palmar and digital diseased cords.
-
Although it resembles a longitudinal
incision, its multidirectional configuration avoids longitudinal
tension lines and is well tolerated by the palmar and digital tissues. Figure 4-11 shows the zigzag incision and the postoperative result.
-
Skin grafts may be used to replace badly diseased skin or to fill a skin defect following fasciectomy.
-
Full-thickness skin grafts are used most often because they are less likely to contract.
-
Figure 4-12 shows a patient with severe contracture in whom skin closure was facilitated by full thickness skin grafts.
recommendations regarding the noninvolved nature of the transverse
elements of the palmar fascia in patients with DD. This concept focused
the attention of surgeons on the need to remove only those tissues that
are diseased. In many instances, this results in less trauma to the
hand, and preserves the parts of the palmar fascia that could continue
to play an important role in the hand. Figure 4-13
demonstrates the relationship of the diseased longitudinal cords to the underlying transverse fibers of the palmar fascia
 |
|
Figure 4-11 The zigzag incision for Dupuytren’s disease. (A)
Comprehensive incision from the proximal palm to the DIP joint for removal of the single-ray palmar and digital cords in Dupuytren’s disease. (B) The end result at 3 months with nearly full extension and good skin healing in the palm and finger. |
 |
|
Figure 4-12 Full-thickness skin graft to facilitate closure in Dupuytren’s disease. (A) The preoperative appearance of severe Dupuytren’s disease, with contracture in the left hand. (B) Intraoperative appearance as the procedure progresses. (C)
A palmar skin graft has been applied in the palm, while a second graft (not shown) will be applied to the defect in the proximal phalanx of the little finger. The ring finger was left open. (D) The end result at 3 months. |
 |
|
Figure 4-13 The Skoog principle of preservation of the transverse fibers of the palmar fascia in fasciectomy. (A) Clinical appearance of Dupuytren’s disease in the right little finger ray. (B) The transverse fibers (open arrow) can be seen between and beneath the longitudinal cords (solid arrow) of the palmar fascia. (C) The end result after removal of the longitudinal cords. Note the preserved transverse fibers (arrow) and the underlying nerves and vessels.
|
dissection in relatively normal tissue and progress to the site of
maximum disease involvement. Thus, dissection often begins in the
proximal palm, where the cords are more easily identified and their
relationship to associated structures is more evident. Wise and
experienced surgeons look for vital structures such as the common and
proper digital vessels and nerves in the palm. Surgeons focus on this
as the dissection enters the region of the distal palm and fingers, in
order to avoid injury to these structures.
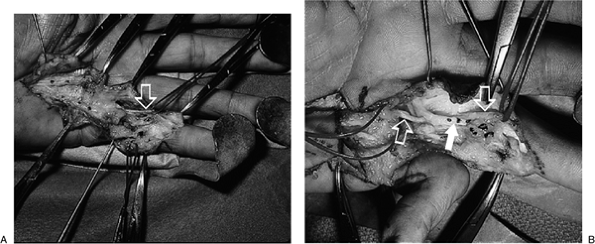
palm and finger is appropriate here. The pretendinous band splits into
two spiral bands just proximal to the first annular pulley. These bands
then continue distally as the spiral band, where they join the lateral
digital sheet. That sheet in turn may join the fibers of Grayson’s
ligament (Figure 4-14).
It is this composite structure that “spirals” around the digital nerve
and vessel and, with increasing contracture, progressively draws the
neurovascular bundle toward the midline, proximally and superficially (Figure 4-15).
It is here, in the region of the proximal phalanx and PIP joint, that
the neurovascular bundle is at risk. The digital nerve and cord are not
easily distinguished because they are similar in color. The nerve is
soft compared to the firmer nature of the cord, and the color of the
blood vessel (even under tourniquet control) may provide some
distinguishing features. A useful technique is to identify the nerve
and vessel in the distal palm, and then trace them distally.
 |
|
Figure 4-14
The anatomy of the normal tissues that may form the spiral cord: Pretendinous band; spiral band; lateral digital sheet; and Grayson’s ligament. |
 |
|
Figure 4-15 The spiral cord and its relationship to the neurovascular bundle.
|
 |
|
Figure 4-16 Clinical examples of cords and their relationship to the neurovascular bundles in the finger. (A) Note the proximity of the digital nerves (retraction loops) to the cords (arrow) in this little finger. (B) Note the proximity of the digital nerves and vessels (open arrows) to the digital cord (closed arrow) in this ring finger.
|
HF, McFarlane RM. Pathogenesis of Dupuytren’s contracture: a
correlative clinical-pathological study. J Hand Surg 1978;3A: 1–10.
JR. Palmar Hand. In: Doyle JR, Botte MJ, eds. Surgical anatomy of the
hand and upper extremity. Philadelphia: Lippincott Williams &
Wilkins, 2002:532–641.
T. The transverse elements of the palmar aponeurosis in Dupuytren’s
contracture. Their pathological and surgical significance. Scand J
Plast Reconstr Surg 1967;1:51–63.
J, Rayan GM. Correlation of alpha-smooth muscle actin expression and
contracture in Dupuytren’s disease fibroblasts. J Hand Surg
1995;20A:450–455.
JD. Dupuytren’s disease. In: Trumble, TE, ed. Hand surgery update 3,
hand, elbow, shoulder. Rosemont, IL: American Society for Surgery of
the Hand, 2003:393–401.