Developmental Dysplasia of the Hip
|
|
of staying out of trouble with developmental dysplasia of the hip (DDH)
is making the diagnosis early. Delay in diagnosis may lead to a worse
outcome, more invasive treatment, and legal action. A wonderful summary
of the early diagnosis of DDH has been published by the American
Academy of Pediatrics (AAP).1
including the associated risk factors for DDH such as breech delivery,
family history of DDH and torticollis, is essential. While the presence
of risk factors should heighten a clinician’s suspicion of DDH,
remember that the majority of cases of DDH have no risk factors
present, and the majority of infants with risk factors do not have DDH.
-
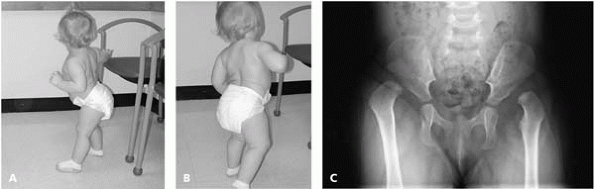
In the newborn with
bilateral dislocated hips, the Galeazzi test is normal and abduction
equal and possibly normal. With bilateral dislocated hips in a newborn,
absence of normal hip flexion contractures may be the only finding that
suggests DDH on physical exam. In an older child, lordosis and a
waddling gait suggest bilateral DDH (Fig. 21-1). -
Examine the baby on
a table when performing the Galeazzi and abduction test for maximum
accuracy. Plaintiffs’ attorneys know this. A screaming baby is easier
to examine on the mother’s lap, but this is a less accurate test. -
If the child is
irritable throughout the examination and a good exam could not be
performed, document this and schedule a return appointment. -
Perform the Ortolani and Barlow tests multiple times—these tests may be difficult to interpret.
-
The Ortolani and
Barlow tests will not pick up fixed dislocations, as may occur in older
children, nor will they unveil teratologic dislocations. Asymmetric
abduction and a positive Galeazzi test should be performed in these
children. -
Look for underlying
conditions. A dislocated hip in a child with hypotonic neuromuscular
disease may be treated quite differently from DDH in an otherwise
normal child.
 |
|
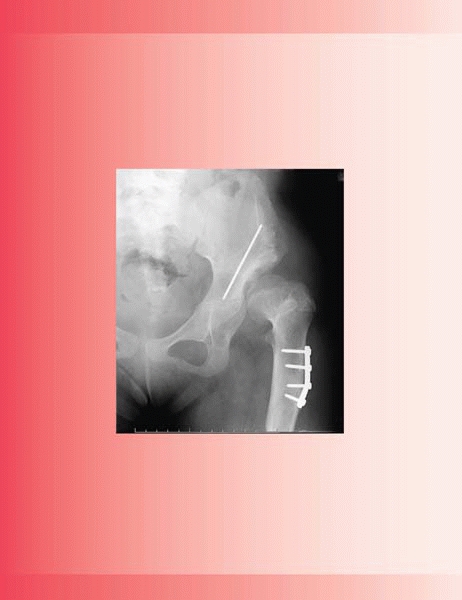
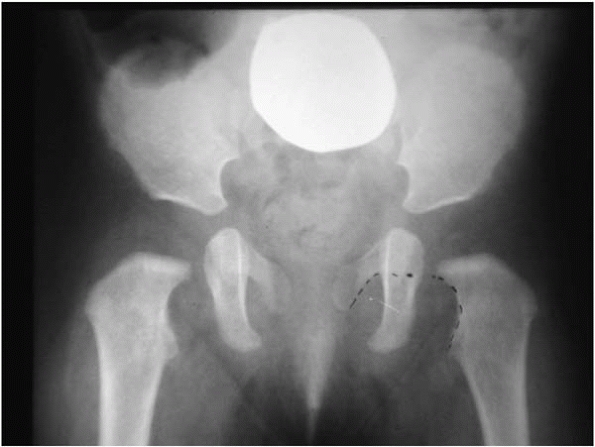
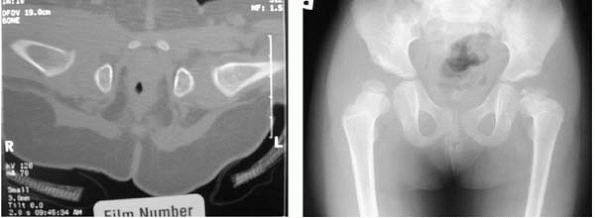
▪ FIGURE 21-1 (A,B)
The parents of this 16-month-old girl were concerned that she was not walking right. She has significant lordosis and a waddling gait. Dislocated hips were discovered incidentally on a urethrogram. An AP radiograph of the pelvis demonstrates bilateral dislocated hips (C). |
controversial from a public health standpoint. The following guidelines
are not based on rigid science, but rather a snapshot of our
interpretation of the current literature reflected in our actual
practice. The statistics are taken from the American Academy of
Pediatrics Practice Guideline.1
-
Positive family history (newborn risk with family history for boys is 9.4/1000 and for girls is 44/1000).
-
Breech position in
utero (even if c-section)—absolute risk of 12% for DDH, hip
abnormalities may develop later in older age, consider radiographs
beyond 6 months. -
Congenital muscular
torticollis (this recommendation is not supported from a public health
viewpoint, but even if the 8 to 20% association of torticollis with DDH
is double or triple the reality, it still seems prudent to ultrasound
infants’ hips with torticollis.) -
Wait until over 6
weeks of age if exam is normal but risk factors are present. There is
an increased rate of false-positive examinations if an ultrasound of
the hips is performed at a younger age. -
Perform the study at an experienced center; the quality of an ultrasound of an infant’s hip is very user dependent.
around 4 to 6 months of age. Before this age ultrasound is the most
common radiologic study to assess hip development. Plain radiographs of
the hips prior to ossification of the femoral heads may demonstrate a
frank dislocation of the femoral head, but they cannot verify that the
hips are normal. Plain radiographs of infants can be misleading if one
confuses an absence of a frank dislocation to be a sign of a normal hip
(Figs. 21-2 and 21-3).
 |
|
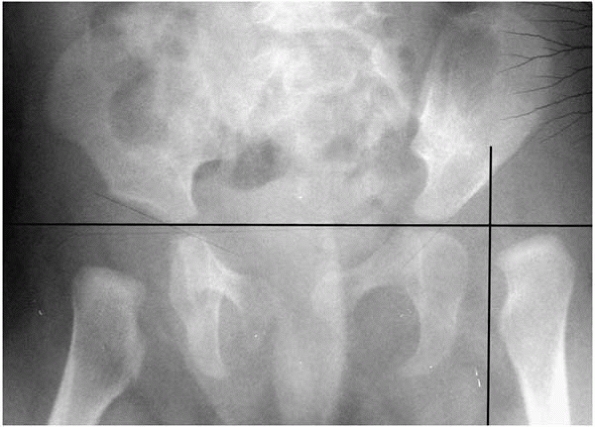
▪ FIGURE 21-2 A radiograph of a normal pelvis in a child prior to ossification of the femoral heads. A continuous “Shenton’s Line” (dotted line)
from the proximal femoral neck to the pubic bone suggests that the hips are well located. A grossly broken line is highly suggestive of a dislocated hip. An ultrasound (or MRI or CT) gives more reliable information. |
 |
|
▪ FIGURE 21-3
AP radiograph of a 1-month-old girl with a dislocated left hip. The medial proximal femoral metaphysis is lateral to the Perkins line (vertical black line at lateral edge of acetabulum), demonstrating the lateral displacement of a dislocated hip. |
femoral rotation on a hip radiograph. Shenton’s line breaks with
external rotation and may suggest DDH (Fig. 21-4).
Another pitfall of external rotation of the hip on a hip radiograph is
that it creates the illusion of hip valgus. Do not consider doing a
varus derotational osteotomy (VDRO) until seeing a true AP of the hip.
Remember this pitfall particularly in the cerebral palsy population.2
 |
|
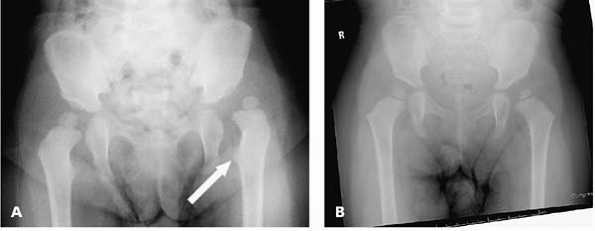
▪ FIGURE 21-4 (A)
AP pelvis of a 3-year-old girl who has no history of DDH. Based on this radiograph, open reduction of the hip was recommended. By noting the prominence of the lesser trochanter (arrow), we know that the hip is in significant external rotation. (B) The family sought a second opinion. A repeat AP radiograph of the girl paying strict attention to keeping the patella forward during the radiograph shows the hip is much better located. While the hip is still a bit lateral, observation was recommended. These radiographs demonstrate the wide variability in appearance of hip location as a function of hip rotation. In addition, note that the femoral neck angle of this radiograph appears significantly better when there is neutral rotation. |
effective first-line treatment for children up to about 6 months of age
with DDH.3 For truly dislocated hips, placing the Pavlik harness as early as is practical is probably best. Harding, et al4
reported that beginning Pavlik harness treatment within the first 21
days of life improved the chances of successful treatment threefold
compared to children in whom treatment was begun after the age of 21
days.
just over 90 degrees and posterior straps as limiting adduction to no
more than neutral, which should maintain the hips in a reduced position
and reduce likelihood of redislocation (Fig. 21-5).
The anterior and posterior straps may be taped into position to prevent
an unwanted change in hip position by caretakers “adjusting” the
straps. Too much hip flexion can cause inferior subluxation of the
femoral head.5 Too much hip flexion
can also cause a femoral nerve palsy. Check that the knees actively
extend at each office visit (legs kicking) while in the harness to
demonstrate that a femoral nerve palsy is not present. If a femoral
nerve palsy is noted, prompt decrease in hip flexion should allow the
nerve to recover. Brachial plexus injury has been reported with Pavlik
harness use that promptly resolved when the harness was removed.6
 |
|
▪ FIGURE 21-5
Pavlik harness. Healthy infants grow quickly, thus the harness will require adjustments for growth so it does not become too tight. Adjust chest strap to allow three adult fingers to be easily slid between the chest strap and chest (white arrow). Adjust leg straps so that an adult finger can fit between the harness straps and leg (black arrow). |
harness treatment, and may be related to the initial magnitude and
position of hip displacement rather than the method of treatment.7
It has also been hypothesized that too much abduction in the harness
may lead to AVN, though in most western series clinically significant
AVN is rare.
despite the fact that the hips are not reduced. An ultrasound should be
performed in the Pavlik harness to confirm reduction of the hips at 1
to 2 weeks after starting treatment if possible. If the hip remains
dislocated while in the Pavlik harness, this may further destabilize
hip and lessen the chance of an effective closed reduction. In a series
of 19 patients who had a Pavlik harness in place for >8 weeks with
no evidence of reduction, 13 of these patients went on to need an open
reduction. The authors concluded that prolonged positioning of the
dislocated hip in flexion and abduction potentiates dysplasia,
particularly of the posterolateral acetabulum, and increases the
difficulty of obtaining a stable closed reduction.8
reduction of the hip by Pavlik harness. Those infants whose hips could
not be reduced by physical exam, combined with ultrasound coverage of
<20%, uniformly failed Pavlik harness treatment in one report.9
Particular vigilance to Pavlik failure and an early change in treatment
may be indicated in this group. If Pavlik harness treatment fails,
switching to an abduction brace led to successful hip reduction in 12
of 15 patients in one series.5
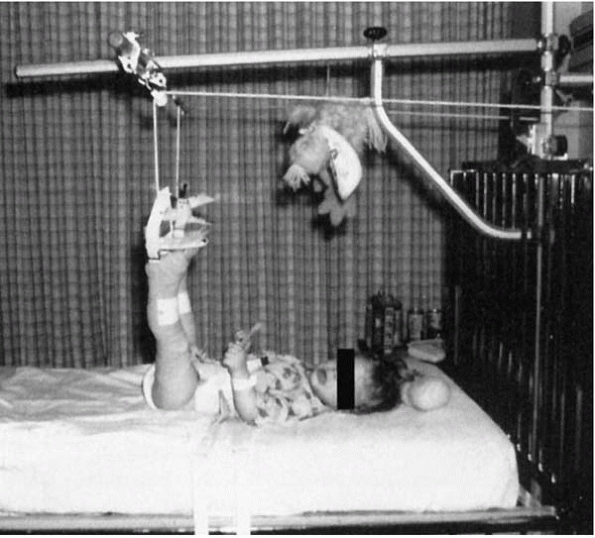
supervised over a period of several weeks seemed to bring high hips
lower, and many believe decreased the incidence of AVN. However, there
is little conclusive evidence that traction works; beware that if
improperly applied it can hurt. Traction should not be initiated with 90 degrees of hip flexion and straight knees (Fig. 21-6), as this has been associated with neurovascular compromise, skin necrosis and compartment syndrome.
Pavlik harness failure in younger children, or primarily in children
from 6 months old up to about 2 years of age. The difficulty of placing
a spica cast on a 6-month-old to hold 1 or 2 hips in a reduced position
is underrated. In reality, it requires more skill than many surgeries
we perform. Having sufficient assistance, including a skilled cast
technician, is invaluable.
 |
|
▪ FIGURE 21-6 This type of traction is associated with neurovascular compromise, compartment syndrome, and skin problems, thus is generally not recommended. (Reprinted with permission from Morrissy RT, Weinstein SL, eds. Lovell & Winter’s Pediatric Orthopaedics, 5th ed. Philadelphia: Lippincott Williams & Wilkins, 2001.)
|
gentle reduction attempted. The key question is how good (or bad) of a
reduction can be accepted. Race and Herring10
reported that a medial dye pool of less than 5 to 7 mm indicated a
concentric reduction and was associated with a good outcome in 11 of 13
hips. Only 5 of 23 hips with a larger dye pool had an acceptable
outcome, with a 57% incidence of osteonecrosis. Stay out of trouble and
do not accept dye >7 mm of medial dye pool. In reality, measuring
dye pool with the possibility of variation due to image magnification
is inexact.
the hip reduced. It is often a technical challenge to maintain Salter’s
recommended 100 degrees of hip flexion during casting. The application
of padding and cast material into the anterior hip crease tends to
extend the hip.
noted the subsequent development of AVN was statistically associated
with hip-abduction angles >55 degrees as measured on postreduction
CT scans, with 20% of the involved hips developing AVN on subsequent
follow-up (Fig. 21-7). In reality, often >55
degrees of hip abduction is needed to keep a hip reduced. The surgeon
must weigh the risks and benefits of more hip abduction in a closed
reduction versus an open reduction. Certainly, abduction of 80 to 90
degrees should be avoided if possible. A pitfall in spica cast
application is assuming hip abduction is OK because the combined hip
abduction is less than 110 degrees. As the surgeon pushes up on the
greater trochanter, the infant’s pelvis has a tendency to tilt upwards
on that side,
and
one hip may end up abducted 90 degrees and the other at 20 degrees.
Keeping the patient’s pelvis level on the spica cast table is important
to judging abduction.
 |
|
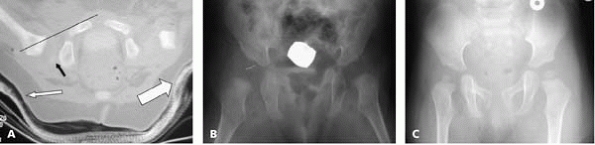
▪ FIGURE 21-7 (A)
Note the position of excessive abduction of both hips in this CT scan following closed reduction of the right hip and spica casting. (B) Three years later there is iatrogenic AVN in the right hip, which was not the dislocated hip. Immaturity of the patient’s left acetabulum may be noted. |
 |
|
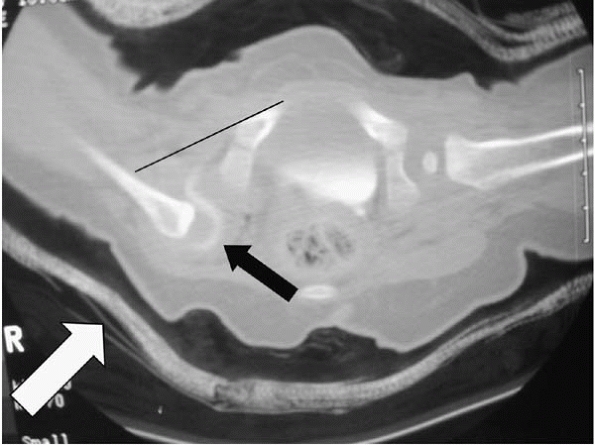
▪ FIGURE 21-8 (A)
CT scan following closed reduction and arthrogram of the right hip. The hip is located as judged by a line along the anterior cortex of the pubis intersecting the proximal femoral metaphysis (thin black line). The small black arrow demonstrates the characteristic apparent posterior subluxation of the femoral head within the acetabulum, which is present even when the hip is located. The small white arrow demonstrates mediocre molding of the cast under the greater trochanter to help keep the hip reduced. The trochanteric molding on the other hip (large white arrow) is actually better in this patient. A substantial trochanteric mold can help maintain the hip in a reduced position. (B) AP radiograph three months following closed reduction and casting. (C) AP radiograph 12 months following closed reduction. The right femoral head is smaller than the contralateral unaffected side, which may persist for a long time despite correct treatment. |
the spica cast that you are losing hip flexion, there is asymmetric hip
abduction, or too much hip abduction, take off the casting material and
start again. It is a lot better to redo the spica cast during the first
anesthesia than the second.
a spica cast, CT or MRI should be used to confirm reduction of the hip.
Do not be fooled by the fact that the reduced hip usually looks
posteriorly subluxed in the acetabulum on these studies. Use the
modified Shenton’s line to confirm reduction12 (Fig. 21-8). When it remains dislocated, it is usually clear (Fig. 21-9).
 |
|
▪ FIGURE 21-9
CT scan following arthrogram and closed reduction of the right hip. Note that obtaining the CT scan shortly after the intraoperative arthrogram helps outline the femoral head. The right hip is dislocated as judged by a line along the anterior cortex of the pubis not intersecting the proximal femoral metaphysis (thin black line). There is no molding under the greater trochanter (white arrow). Better molding of the cast under the greater trochanter may have aided in holding the hip in a reduced position. The extreme abduction of the contralateral hip is undesirable and could result in AVN. |
irritability in a spica cast, the skin must be fully examined. This may
be accomplished with a flashlight, but if necessary the spica cast may
need to be removed. Preverbal children cannot always communicate where
they are feeling pain, and severe ulceration and infection can develop
under the cast, particularly in casts soiled by feces and urine (Fig. 21-10).
 |
|
▪ FIGURE 21-10 This infant had a spica cast for six weeks following open reduction of the hip. A full thickness ulcer resulted.
|
the chances of a lessthan-perfect outcome go way up. Establish parental
expectations from the beginning that multiple surgeries over the course
of the child’s lifetime should be anticipated. Make certain that they
understand you will do everything possible to prevent problems, but
AVN, prolonged stiffness, pain, and limping occur despite the best
treatment possible.
importance to what surgery is done under the skin. A few suggestions to
stay out of trouble with the various approaches are warranted.
-
Do not use a medial approach for high dislocation, as a capsulorraphy or other procedures cannot be done.
-
Avoid ligating the medial circumflex artery, as many believe this may increase the risk of AVN.
-
It is surprisingly easy to forget to
release the psoas and adductor tendons when your attention is diverted
in the hip joint. Release them early during the procedure so you do not
forget.-
A true inverted limbus is uncommon, and
it is rare for this to impede reduction. If you think this is impeding
reduction, look for other causes, like an incomplete release of the
transverse acetabular ligament or psoas tendon.
-
-
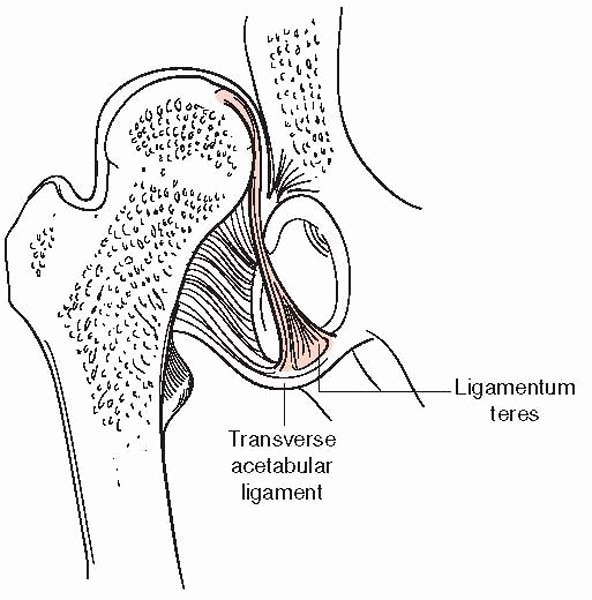
Make certain the transverse acetabular
ligament is incised so your finger can pass by its former location, and
feel the horseshoe-shaped opening of the inferior medial acetabulum.
There have been failed open reductions when this ligament has not been
sufficiently released. It is deep in the wound, but may be safely
excised (Fig. 21-11).
-
Femoral shortening in combination with an open hip reduction decreases the risk of AVN.14
-
Consider a femoral shortening if the hip
rests superior to the acetabulum in an unreduced position, or if
reduction of the hip requires force. -
Beware of too much derotation of the
femur, particularly in combination with a Salter osteotomy, as it may
direct the femoral head out the back. We usually prefer a pure
shortening of the femur when combined with an open reduction of the hip.
When dissecting periosteum off the outer table in very little kids, the
sciatic notch may be surprisingly
close.
If you have a significant bleeder in the notch, packing with Gelfoam
and thrombin for 20 minutes while proceeding with other parts of the
procedure will be sufficient at times. Considerations for the various
pelvic osteotomies are presented below.
 |
|
▪ FIGURE 21-11
The transverse acetabular ligament may be found by following the ligamentum teres to its origin in the inferior medial edge of the acetabulum, on the transverse acetabular ligament. The transverse acetabular ligament is often hypertrophied in dislocated hips, and must be incised to allow full reduction of the hip. |
-
Salter: Provides mainly anterior coverage at the expense of posterior coverage.
-
Dega: Make certain you are high enough
above acetabular rim when starting your cut. The osteotome tends to
drift downward, and leaves too little bone to push against when wedging
open the osteotomy. Rotation of the superior acetabulum occurs in part
through the triradiate cartilage, so consider other procedures if the
triradiate cartilage is closed. -
Steel: Remember that the goal is to medialize the hip. This often requires resection of some ischial bone to achieve this goal.
-
Ganz: This osteotomy is technically more
difficult and involves blind cuts. It should be avoided by surgeons
lacking specialized training, and is contraindicated with open
triradiate cartilage, as the cuts would go through the cartilage. -
Chiari or shelf: These are salvage
procedures. They optimally produce increased weight-bearing surface
nearly continuous with the acetabulum. If the procedures are done
significantly superior to the sourcil, there is little benefit.
orthopaedics is determining if acetabular development is sufficient
following reduction of a hip. An acetabular index of 35 degrees or more
two years after reduction of the hip was associated with an 80%
probability of becoming a Severin grade III/IV hip in one series, so
this may serve as some objective measure.16
Unfortunately, the acetabular index is subject to significant
variability. A subjective criterion we have found useful to confirm
maturation of the acetabulum is increased concavity of the acetabulum
over time (Fig. 21-12).
 |
|
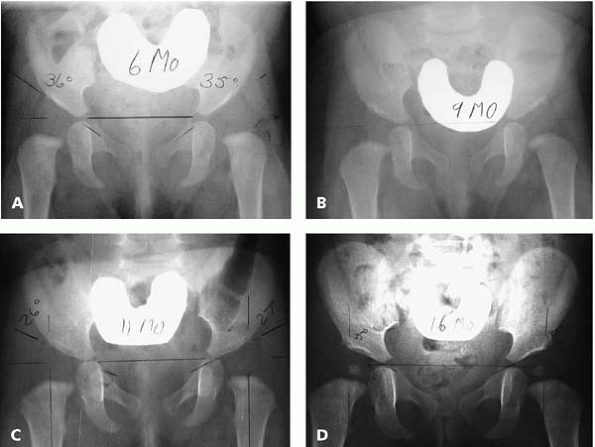
▪ FIGURE 21-12
Maturation of the hips during 10 months of abduction bracing for acetabular dysplasia. Note that the acetabular angle improves, and the acetabulum becomes more concave over time. If these changes are not taking place over a period of many months, further intervention may be needed. (A) Radiograph of 6-month-old patient at start of abduction bracing. (B) Same patient at 9 months old. (C) Same patient at 11 months old. (D) Same patient at 16 months old, at end of bracing treatment. |
often of no clinical consequence. Have patience and observe without
panicking, as there is little that can be done at early stages anyway.
A particular type of AVN to be aware of is a lateral arrest, which
occurs at a mean age of 9 years. This further emphasizes the importance
of long-term followup for children with DDH.
overgrowth of the greater trochanter, avoid a useless operation by
remembering that a greater trochanter physeal arrest will only be of
benefit under age 8, as in older children there is not sufficient
growth remaining for an epiphysiodesis to have a meaningful effect. In
children 8 years old and older, a trochanteric transfer is preferable
to an epiphysiodesis.17 A technical
point for a trochanteric transfer is to plan on extensive release of
soft tissues to allow for sufficient movement of the greater trochanter.
-
Consider an
ultrasound of the hips in infants with the following risk factors for
DDH: breech position in utero, family history, and congenital muscular
torticollis. -
The Ortolani and
Barlow tests may be challenging. Do not hesitate to repeat these tests
multiple times. If a baby is crying or irritable, it is impossible to
do a good hip exam. -
With Pavlik harness
treatment, confirm reduction of hips within 1 to 3 weeks of placement
of harness. If hips are not reduced, abandon Pavlik harness treatment. -
Avoid excessive abduction in a spica cast as this increases the risk of AVN of the femoral head.
-
Establish parental expectations for an open reduction of the hip to include multiple surgeries.
-
If in doubt, shorten the femur.
on Quality Improvement, Subcommittee on Developmental Dysplasia of the
Hip. American Academy of Pediatrics. Clinical practice guideline: early
detection of developmental dysplasia of the hip. Pediatrics. 2000;105(4 Pt 1):896-905.
JP, Round J, Taylor T, et al. The natural history of developmental
dysplasia of the hip after early supervised treatment in the Pavlik
harness: a prospective, longitudinal follow-up. J Bone Joint Surg Br. 2002;84(3):418-425.
D, Kasser J, Emans J. Use of an abduction brace for developmental
dysplasia of the hip after failure of Pavlik harness use. J Pediatr Orthop. 2003;23(2):175-177.
S, Kashiwagi N, Kasahara Y, et al. Avascular necrosis and the Pavlik
harness: the incidence of avascular necrosis in three types of
congenital dislocation of the hip as classified by ultrasound.” J Bone Joint Surg Br. 1996;78(4):631-635.
JA, Emans JB, Millis MB, et al. Early failure of Pavlik harness
treatment for developmental hip dysplasia: clinical and ultrasound
predictors [see comment]. J Pediatr Orthop. 2001;21(3):348-353.
BG, Millis MB, Hey LA, et al. Postreduction computed tomography in
developmental dislocation of the hip, part II: predictive value for
outcome. J Pediatr Orthop. 1997;17(5):631-636.
BG, Kasser JR, Hey LA, et al. Postreduction computed tomography in
developmental dislocation of the hip: part I: analysis of measurement
reliability. J Pediatr Orthop. 1997;17(5):626-630.
PL, Strecker WB. Congenital dislocation of the hip in children.
Comparison of the effects of femoral shortening and of skeletal
traction in treatment. J Bone Joint Surg Am. 1984;66(1):21-27.
SM, Szoke G, Murray DW, et al. (1996). Femoral remodelling after
subtrochanteric osteotomy for developmental dysplasia of the hip. J Bone Joint Surg Br. 1996;78(6):917-923.
J, Dolan LA, Spratt KF, et al. Acetabular dysplasia after treatment for
developmental dysplasia of the hip: implications for secondary
procedures. J Bone Joint Surg Br. 2004;86(6):876-886.
S, Garfin S, Vance R, et al. Pitfalls in the use of the Pavlik harness
for treatment of congenital dysplasia, subluxation, and dislocation of
the hip. J Bone Joint Surg Am. 1981;63(8):1239-1248.
RG, Birch JG, Herring JA, et al. Use of the Pavlik harness in
congenital dislocation of the hip: an analysis of failures of
treatment. J Bone Joint Surg Am. 1990;72:238.