Spine II: Staying Out of Trouble with Kyphosis, Spondylolysis/Spondylolisthesis, and Back Pain
– Spine and Hip > 20 – Spine II: Staying Out of Trouble with
Kyphosis, Spondylolysis/Spondylolisthesis, and Back Pain
|
|
conditions that can be a source of major trouble for the orthopaedist:
kyphosis, spondylolysis/spondylolisthesis, and back pain. Much of the
trouble associated with the management of kyphosis and
spondylolisthesis are surgical/technical, while most trouble with
pediatric back pain relates to diagnostic pitfalls.
spine surgeons. Although it is much less common than scoliosis,
kyphosis is associated with a disproportionately larger amount of
trouble. From a diagnostic standpoint, measurement of kyphosis can be
quite difficult, particularly due to problems visualizing the upperend
vertebra.
and Type 3 (mixed for rotary subluxation). Of these, failure of
formation is the most difficult type to manage and is associated with
the highest rate of neurologic injury during surgical treatment.
 |
|
▪ FIGURE 20-1
Congenital kyphosis: less trouble. The full imaging evaluation showed this to be a Type II kyphosis, with failure of segmentation. There is no protrusion into the posterior spinal canal. This creates a deformity problem, but not too much of a neurologic risk. |
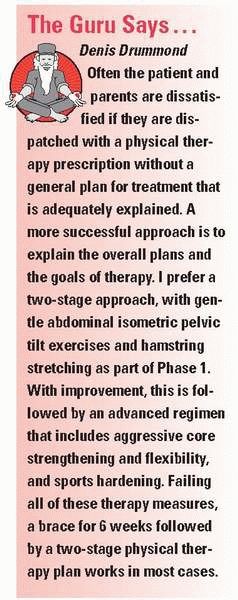
children with congenital kyphosis. Before operating on a large
congenital kyphosis, consider urodynamic testing, as it may detect
subtle preexisting myelopathy in the high-risk patients (particularly
younger children). Flexion/extension lateral radiographs, especially
extension over a bolster, can be very valuable to determine the
flexibility at the site of the deformity. To stay out of trouble, an
MRI is recommended for defining the congenital abnormality and the
effect of that abnormality on the spinal cord (Figs. 20-2 and 20-3). A recent study2
focused on the diagnostic tests that should be performed on a patient
who presents with congenital spinal anomalies. The authors concluded
that “magnetic resonance imaging and echocardiography should be an
essential part of the evaluation of patients with congenital
spinal deformity, with special attention to patients with segmentation abnormalities, mixed defects, and kyphosis.”
 |
|
▪ FIGURE 20-2
Congenital kyphosis: more trouble. Type I congenital kyphosis with failure of formation. The congenitally abnormal vertebra protrudes posteriorly, creating a deformity and some neurologic risk. |
radiographic followup. Bracing does not have the ability to lead to any
correction. Sometimes a brace is used for the compensatory deformity,
as in congenital scoliosis. Keep in mind that even if the absolute
magnitude of the kyphotic deformity is not increasing, its flexibility
may worsen over time. This also may be an indication for earlier
surgical management.
 |
|
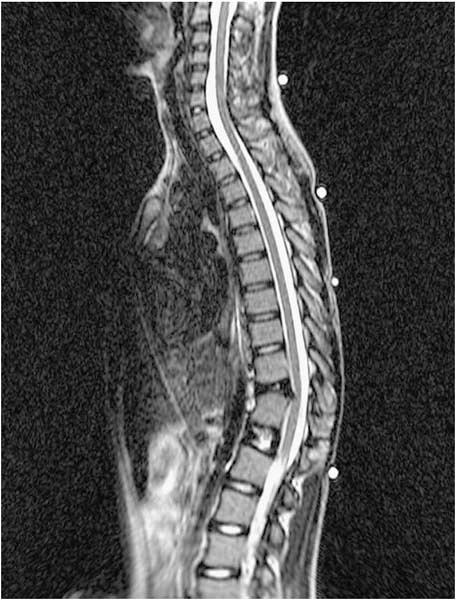
▪ FIGURE 20-3
Congenital kyphosis—maximum trouble. Severe congenital kyphosis with spinal cord impingement and deteriorating neurologic function (A), treated with anterior decompression and fusion, followed by posterior fusion (B). (Case courtesy of D. Drummond, MD.) |
source of trouble for the pediatric spine surgeon. Year after year, the
Scoliosis Research Society (SRS) Morbidity and Mortality data
identifies kyphosis as the condition most commonly associated with
neurologic injury during surgery. Because of the risk of neurologic
injury, hypotensive anesthesia is contraindicated in the surgical
management of kyphosis. The operative plan should avoid distraction or
lengthening of the spinal canal. A study by Kim et al3
found that the risk of neurologic injury with anterior and posterior
fusion for kyphotic deformity was associated with greater age, more
severe deformity, and preexisting spinal cord compromise. Unlike
idiopathic scoliosis surgery, in which instrumentation is used to
effect a major deformity correction, in congenital kyphosis surgery,
the instrumentation is used primarily as an internal splint.
degrees, posterior fusion only is usually recommended. All involved
vertebrae, plus an extra vertebra above and below, should be included
in the fusion. If the curve is greater than 55 degrees, an anterior and
posterior fusion has been the classic recommendation. These
recommendations were supported in a long-term study by McMaster and
Singh,4 who reviewed data from 65
patients and concluded “all patients with a Type I or Type III
congenital kyphosis or kyphoscoliosis should be treated by a posterior
arthrodesis before the age of 5 years and before the kyphosis exceeds
50 degrees. A kyphosis that does not reduce to less than 50 degrees as
measured on the lateral spine radiograph made with the patient supine
requires an anterior release and arthrodesis with strut grafting
followed by posterior arthrodesis with instrumentation.”
compression, anterior decompression is indicated, not laminectomy. If
there is some scoliosis and a strut is being placed, consider
approaching the spine on the concave (not the typical convex) side. By
approaching on the concave side, the graft will be under compression.
posterior closing wedge osteotomies may totally destabilize the spine.
In these cases, a temporary rod can be placed posteriorly to stabilize
the spine. In this way, after you remove the final bit of posterior
osteotomy the spine will not move in an uncontrolled fashion.
kyphosis variant is segmental spinal dysgenesis. This spinal disorder
combines deformity, instability and stenosis. Once recognized, surgical
treatment is recommended to prevent progressive neurologic
deterioration.5,6
kyphosis. The physical examination can help distinguish these two. A
child with postural kyphosis will have a smooth round curve to his back
on forward bend. A sharper kyphosis should alert the examiner to the
possibility of serious underlying pathology. To stay out of trouble,
get good quality, full-length spine radiographs even if the examination
suggests a round back. Coned-down laterals may be needed to clarify the
cause of the kyphosis.
can be trouble. Although there is no published evidence that any sort
of exercise treatment or brace can lead to the resolution of postural
kyphosis, the parents expect a full explanation, and possibly some sort
of training for their hunched-over teen. Giving the parents some
postural exercises, or a referral to a therapist who can
work
with the teen, can keep you out of trouble. The parents will respect
and understand that you have taken the visit seriously.
kyphosis, greater than 40 degrees on radiographs, with wedging of 3 or
more adjacent vertebra and endplate irregularities. The natural history
of Scheuermann kyphosis is usually quite favorable when the deformity
is in the thoracic region, although back pain is a common problem when
the deformity is at the thoracolumbar region.
neurologic exam on children with Scheuermann kyphosis. Full length
standing AP and lateral radiographs of the entire spine should be
obtained and studied closely for any additional pathology. There is a
50% incidence of spondylolysis in Scheuermann kyphosis.7
perhaps even more controversial than the brace management. To stay out
of trouble, be aware that many of these children are overweight and the
operative times can be fairly long. Careful positioning at the time of
surgery is critical. Femoral nerve and vascular compression have been
reported, leading to serious morbidity.
correct the kyphotic deformity into the normal range. One previous
study showed that correcting the deformity by more than 50% risks
hardware failure.9 Consider using
the strongest bone anchor constructs in your arsenal, particularly in
heavier children. Keep implants out of the canal at the apex. The
fusion should be extended beyond the first vertebra below a disk that
is in lordosis (Fig. 20-4). A shorter fusion may lead to failure. If you plan to do an anterior thoracoscopic release, be aware that
releasing the disk on the far side of the deformity may be much more
difficult than in scoliosis, where the spine is rotated towards you.
 |
|
▪ FIGURE 20-4 Avoiding trouble in Scheuermann kyphosis (A)
includes careful patient selection, correction into normal sagittal alignment (but not overcorrection), instrumenting one level beyond the first lordotic vertebra, using strong anchors, and keeping instrumentation out of the canal at the apex (B). Many believe that shortening posteriorly is more important than release anteriorly. |
types. The dysplastic type is a congenital deficiency of the L5-S1
facet joints, allowing forward slippage of L5 on S1. This variety has a
higher likelihood of neurologic problems because the pars
intra-articularis is intact. The second type, the isthmic type, is much
more common. In these cases, there is a pars defect; neurologic
deterioration is rare. In the vast majority of cases, the
spondylolisthesis has progressed to its endpoint by the time the
patient initially presents to the orthopaedist. To stay out of trouble,
recognize those cases at highest risk for progression, particularly
children who have a higher slip angle (lumbosacral kyphosis). A higher
grade of slip also correlates with progression, as does a higher grade
of pelvic incidence.11 It is
important to understand these factors, so that you don’t limit sports
participation in an otherwise healthy teenager with a low-grade
asymptomatic spondylolisthesis.
spondylolysis and spondylolisthesis. Physical exam findings usually
include tight hamstrings and a large popliteal angle. To stay out of
trouble, be certain that there is not another cause of back pain. Be
careful not to blame back pain of another etiology on an asymptomatic
spondylolysis. Bone scan is a very valuable test to determine if there
is an active attempt to heal the pars lesion (Fig. 20-5). Bone scan can also help to rule out other pathology. A CT scan with fine cuts may best define the lesion (Fig. 20-6). A CT scan can also be used to follow up healing after brace treatment, although this is not a routine for many orthopaedists.
 |
|
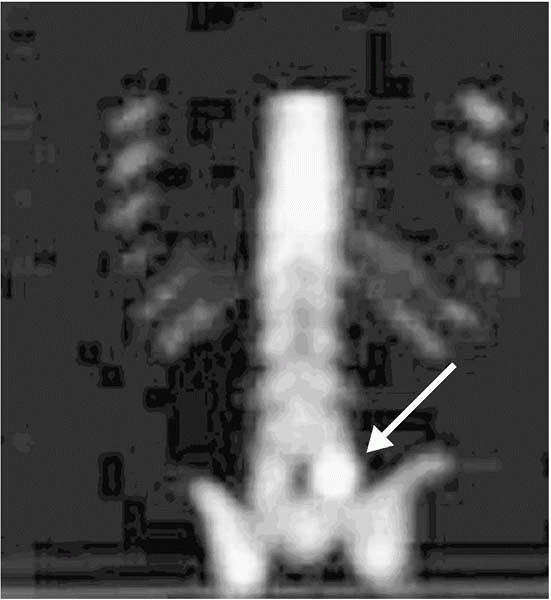
▪ FIGURE 20-5 Bone scan diagnostic of unilateral spondylolysis (arrow).
This 11-year-old boy presented with classic physical examination features of spondylolysis and an MRI that was read as normal. Even in retrospect the consulting orthopaedist and another radiologist could not see any evidence of spondylolysis on the MRI. |
 |
|
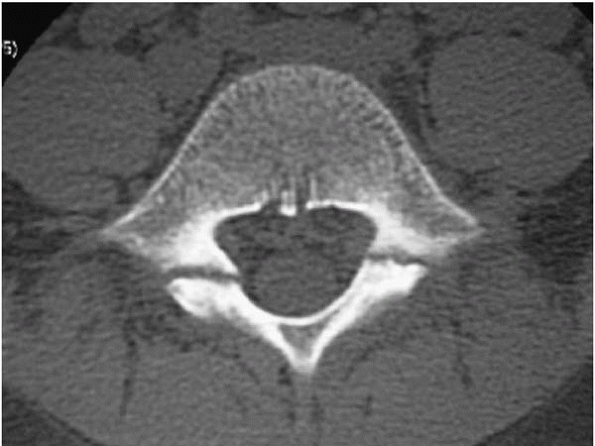
▪ FIGURE 20-6
CT scan showing bilateral pars defects. There is significant sclerosis, and the edges of the defect appear rounded and remodeled. CT gives you and the patient much information not available with other imaging. In this case, it suggests that the lesion is chronic; many would say this is one that would be difficult to completely “heal.” |
on the lateral film. Classically, a “Scotty dog sign” is diagnostic on
the oblique radiographs. In practice, oblique radiographs can be
difficult to interpret and expose the child to significant (and perhaps
unnecessary) radiation.
pain. Many children present from their pediatrician with a normal MRI,
but with classic physical exam findings for spondylolysis. To stay out
of trouble, understand the limits of a typical MRI study for this
condition. The increased edema in the pars can be a very subtle finding
that many radiologists will miss unless they are specifically looking
for it. Often, the adult radiologist provides an exhaustive description
of each lumbar disc in an 11-year-old, but misses the increased edema
in the pars.
spondylolisthesis is nonoperative for Grade 0, 1, and 2. Bracing,
followed by core strengthening, is effective in relieving pain for most
patients. Children with Grades 0, 1, and 2 asymptomatic
spondylolisthesis require no treatment. In situ L5-S1 bilateral lateral
fusion is used for children with continued pain after failed
nonoperative measures for Grade 0, 1, and 2 spondylolisthesis. Classic
methods include bone grafting and postoperative casts or brace wear.
Increasingly, a high nonunion rate is being recognized with bone graft
and bracing or casting alone. For L4 spondylolysis, a direct repair of
the defect can be performed. The Gill procedure should not be the sole
treatment for spondylolysis in children. Children and adolescents with
a Grade 3, 4, or 5 spondylolisthesis should be fused at L4 to S1. A
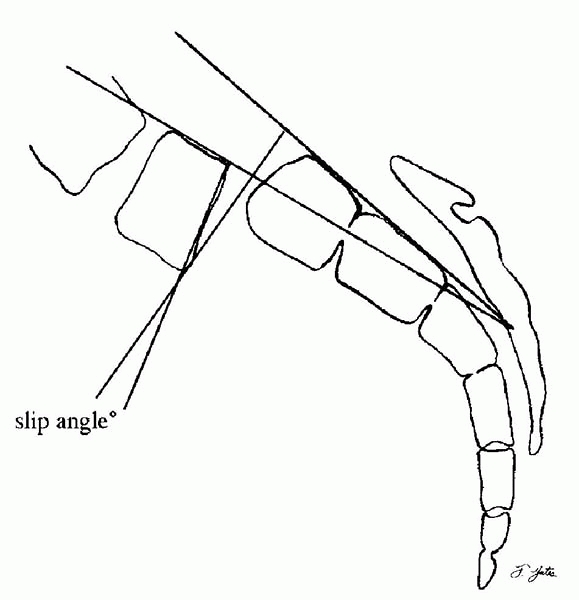
partial reduction, especially of the slip angle (Fig. 20-7), is usually part of the procedure in higher grades of spondylolisthesis.
surgeon should focus on reducing the slip angle and getting a solid
arthrodesis without putting the child at undue risk for a neurologic
catastrophe. Improving the slip angle is much more important—and
safer—than completely reducing the translation.12
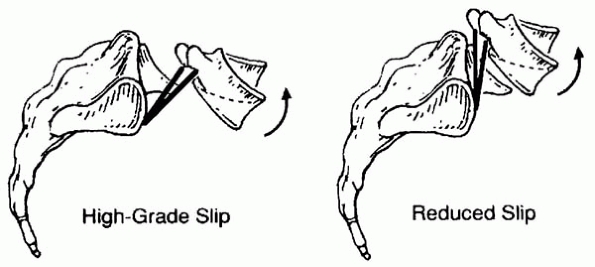
spondylolisthesis, understand that neurologic injury rates increase
precipitously when reduction of the anterior translation is part of the
procedure. The slip angle can usually be improved safely with
intraoperative positioning alone, or the judicious use of posterior
instrumentation
and careful neurologic monitoring. Petraco et al.13
found that the risk of stretch injury to the L5 nerve root with
reduction of high-grade spondylolisthesis is not linear. Seventy-one
percent of the total L5 nerve strain occurs during the second half of
the reduction. These investigators concluded that partial reduction may
be significantly safer than complete reduction treatment for high-grade
spondylolisthesis (Figs. 20-8 and 20-9).
 |
|
▪ FIGURE 20-7
Slip angle, shown here, measures the sagittal rotation of L5 on the sacrum. Correcting the slip angle during surgical management helps to improve biomechanics, and hence decrease the rate of pseudoarthrosis and postoperative progression. |
problems may develop both intraoperatively and postoperatively. The
most common nerve deficit is L5,
which
may not occur or even be detected until postoperative day 1 or 2, when
the patient stands. Late nerve injury is common even with a documented
postoperative normal examination and normal intraoperative SSEPs. Cauda
equina syndrome is another dreaded complication. It has been reported
even after in situ fusion.14
To stay out of trouble, put this complication on your list when
providing informed consent. Cauda equina syndrome can occur even when
there are no preoperative neurologic findings. Some believe it is due
to the relaxation of spastic muscles while under anesthesia. Modern
sophisticated neurologic monitoring is advised in all cases of surgical
management.
 |
|
▪ FIGURE 20-8 Comparison of the relative effect of partial slip reduction on a high-grade slip and a slip that is almost completely reduced. x is the horizontal distance separating the two reference points on the L5 nerve; y is the vertical distance. L is the diagonal of this triangle (nerve length). The change in x is equal to the distance of reduction. The contribution of x
is small in high-grade slips but much larger as L5 is reduced progressively. (Reprinted with permission from Petraco DM, Spivak JM, Cappadona JG, et al. An anatomic evaluation of L5 nerve stretch in spondylolisthesis reduction. Spine. 1996;21(10):1133-1138.) |
 |
|
▪ FIGURE 20-9
Sketch of L5 in kyphosis superimposed on L5 in lordosis for a high-grade slip and for a slip that is nearly fully reduced. In the high-grade slip, lordosis slackens the nerve. In the reduced slip, lordosis stretches the nerve. (Reprinted with permission from Petraco DM, Spivak JM, Cappadona JG, et al. An anatomic evaluation of L5 nerve stretch in spondylolisthesis reduction. Spine. 1996;21(10):1133-1138.) |
posterior S1 contouring, strut grafting, anterior support, and
vertebrectomy have all been proposed as ways of decreasing the trouble
associated with the surgical management of high-grade
spondylolisthesis, because progression of the deformity,
pseudoarthrosis, and neurologic injuries have been such common
complications. Fibular dowel grafts (either allograft or autograft)
have been used successfully, and are a standard part of the procedure
at many centers.15 The Scoliosis
Research Society Morbidity & Mortality Committee found that since
1996, there has been a trend towards reduction of spondylolisthesis; as
might be expected, there has been a concomitant >100% increase in
iatrogenic neurologic injury.16
occulta associated with spondylolysis and spondylolisthesis. The defect
can be wide enough to present a surgical danger if it is not recognized
or anticipated.17
implied that there is a very high likelihood of finding serious
pathology in a child or adolescent who presents with back pain. This
philosophy has encouraged exhaustive workups on each patient. In fact,
when looking at epidemiologic studies of large populations, the rate of
mechanical low back pain in children and adolescents approaches the
rate in adults.
-
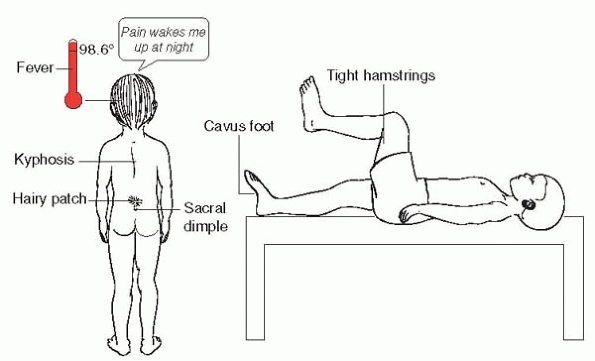
Night pain
-
Pain in young children, especially if they stop playing
-
Frequent pain at
rest (at rest does not include sitting; pain with prolonged sitting in
school is extremely common in teens with mechanical low back pain [LBP]) -
Back pain associated with an abnormal gait, limp, unsteadiness on feet, etc.
-
Any associated constitutional symptoms: e.g., fever, lethargy, weight loss, loss of appetite
-
Atypical
location—especially thoracic rather than lumbar pain (although pain up
in the trapezius/periscapular m. is often over-worked-up and is often
due to backpacks -
On history, is it getting better, worse, or staying the same? The ones that are getting worse are more worrisome.
-
Any neurologic symptoms or physical finding (this includes cavus foot, etc.)
-
Kyphosis (but not really scoliosis)
-
Important associated cutaneous findings: high and deep dimple, hairy patch, café-au-lait spots suggestive of neurofibromatosis.
-
The “finger test.”
If child localizes pain to one spot with the point of a finger, worry.
If the child demonstrates a broad area, particularly transverse over
low back, welcome that child to adulthood. -
Positive coin test—have child keep back straight when picking something up
-
Listing to side on Adams forward bend
-
Tight hamstrings—popliteal angle greater than 50 degrees
 |
|
▪ FIGURE 20-10 Other red flags for kids with back pain.
|
radiographic evaluation with good quality radiographs of the spine:
standing AP and lateral scoliosis radiographs. If the problem clearly
localizes just to the lumbosacral junction, lumbosacral plain films may
be best. On these radiographs, look for widening of the pedicles, signs
of diastematomyelia, absent pedicles, or an abnormal vertebra.
children doesn’t have to come from the spine. Get the primary doctor in
the loop if the symptoms are unclear. Could the problem be renal or
urologic? Abdominal? Gynecologic? Perhaps within the realm of
hematology/oncology? (Remember that lymphoma and leukemia can present
as back pain.) The bone scan is a very valuable and
commonly
used test to screen for an organic cause of pediatric back pain.
Although not very specific, bone scan is much more sensitive for
detecting spondylolysis than MRI. Adding an MRI to your evaluation
makes sense if there are either neurologic history or physical
findings, or elevated inflammatory markers (erythrocyte sedimentation
rate, C-reactive protein), or night pain or other concerning symptoms
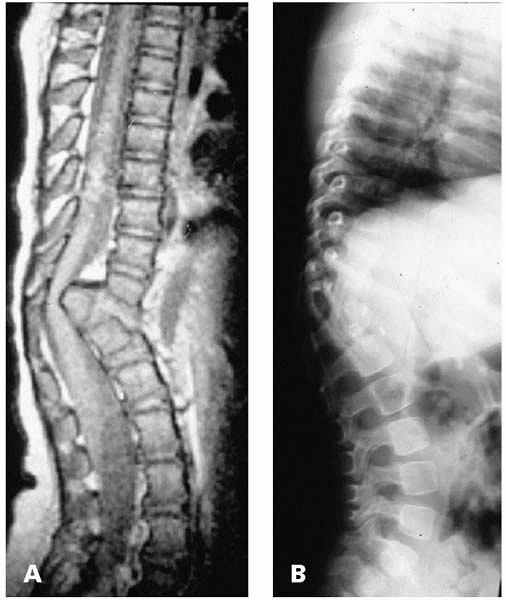
of an infection or tumor (Fig. 20-11).
 |
|
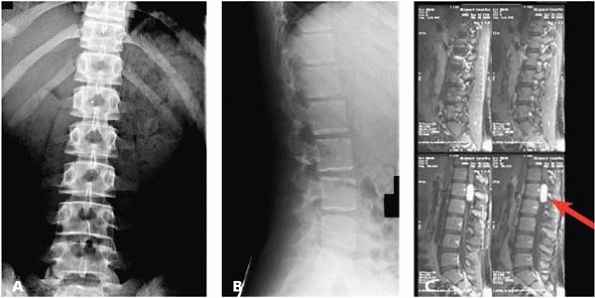
▪ FIGURE 20-11
The back pain trouble everyone fears: serious pathology masquerading as typical teenage mechanical back pain. This 13-year-old presented with a month of back pain. She had no constitutional symptoms, no concerning complaints and no neurologic findings on a very thorough, well documented physical exam (a 3-page note by a very thorough pediatric orthopaedist). AP (A) and lateral (B) radiographs were normal. The family was given exercises and instructed to return in 4 weeks for reevaluation. On their own, they had an MRI done (C) that showed a spinal cord tumor, most likely an appendemoma (arrow). |
an MRI is a reflex with back pain, because they think “herniated disc.”
Likewise, the default protocol at many community MRI centers, and the
radiologists report, will focus on the intervertebral disc. A herniated
disc is actually a very unusual cause of back pain in children and
adolescents. For every teenager with a herniated disc, there are
perhaps a hundred with “bulging discs” or “mild degeneration.” These
terms frighten families and create the need for counseling and
education. To stay out of trouble, look out for the adolescent endplate
fracture, a.k.a., the “hard disc” that may symptomatically masquerade
as a herniated nucleus pulposis, but can be harder to diagnose. These
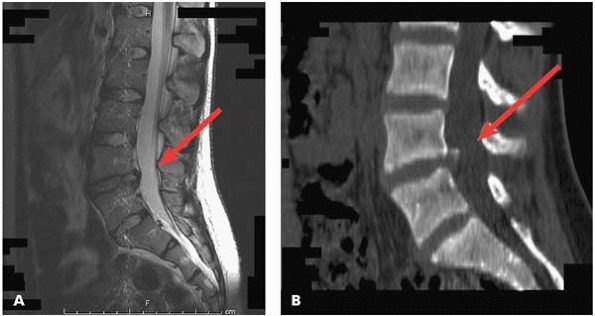
kids rarely get better without excision of the fragment (Fig. 20-12).
 |
|
▪ FIGURE 20-12 This 14-year-old girl presented with back pain and sciatica. The MRI (A) showed a mild “bulging disc” at L4, with some canal effacement (arrow). The CT (B) showed the bony endplate fragment that had displaced from the inferior endplate of L4 (arrow). She had complete relief after fragment excision.
|
negative and the pain is just “muscular” (or in some cases due to
depression, obesity, etc.), don’t continue to torture the child or teen
with additional tests and visits to the orthopaedic surgeon. Instead,
help child and family members focus on rehabilitation with physical
therapy. Ask the family to report back to their primary doctor, so that
the primary care physician can collect all information and decide if
other consultations are warranted. Many adolescents with LBP have
psychosocial problems that are better handled through their primary
care doctor than through the orthopaedic surgeon. In fact, a recent
prospective cohort study found that adverse psychosocial factors and
the presence of other preexisting somatic pain symptoms were predictive
of future LBP in children, just as in adults. In contrast, there was
little evidence of an increase in short-term risk associated with
mechanical load across the range of weights commonly carried by
children to school.18
-
When following
congenital kyphosis in the immature spine, small and incremental
progression may be very difficult to appreciate. Put several sequential
radiographs up on the view box together in order to better appreciate
an increase in the deformity. -
Before operating on
a large congenital kyphosis, consider urodynamic testing, as it may
detect subtle preexisting myelopathy in the high-risk patients
(particularly younger children). -
Because of the risk
of neurologic injury, hypotensive anesthesia is contraindicated in
congenital kyphosis. The operative plan should avoid distraction or
lengthening of the spinal canal. -
The risk for
neurologic complication in kyphosis surgery is correlated with long
complex surgeries, hypotension, and ligation of segmental arteries. Try
to preserve the segmental arteries. Sometimes, it’s better to stage
surgeries, stopping after the anterior portion is complete. -
Counsel the family
that the round back deformity frequently resolves with time. Core
strengthening and postural training may be valuable. You will find that
this is time well spent. -
In the surgical
management of Scheuermann kyphosis, careful positioning in the
operating room is critical. Femoral nerve and vascular compression have
been reported, leading to serious morbidity. -
In the surgical
management of Scheuermann kyphosis, consider using the strongest bone
anchor constructs in your arsenal, keeping implants out of the canal at
the apex. This is particularly important in heavier children. The
fusion should be extended beyond the first vertebra below a disk that
is in lordosis.
-
Recognize those
cases that are at the highest risk of progression. These will be those
children who have a higher slip angle (lumbosacral kyphosis). A higher
grade of slip also correlates with progression, as does a higher grade
of pelvic incidence. -
When managing
high-grade spondylolisthesis, the focus should be about reducing the
slip angle and getting a solid arthrodesis without putting the child at
undue risk for a neurologic catastrophe. Improving the slip angle is
much more important—and safer— than completely reducing the translation. -
To stay out of
trouble, counsel the families that nerve problems may develop
intraoperatively and postoperatively. The most common nerve deficit is
L5, and may not occur or even be detected until postoperative day 1 or
2, when the patient stands.
-
Know the red flags of pediatric back pain.
-
Back pain in children doesn’t have to come from the spine. Get the primary doctor in the loop if the symptoms are unclear.
-
Once you are
confident that the workup for back pain is normal and the pain is just
“muscular” (or in some cases due to depression, obesity, etc.), don’t
continue to torture the child or teen with additional tests and visits
to the orthopaedic surgeon. Instead, focus the child and family on a
physical therapy and rehab approach and have them report back to their
primary doctor to coordinate further treatment.
DJ, Stollsteimer GT, Betz RR. The value of the measurement from T5 to
T12 as a screening tool in detecting abnormal kyphosis. J Spinal Disord. 1996;9(3):220-222.
TG, Kasten MD. An analysis of sagittal curves and balance after
Cotrel-Dubousset instrumentation for kyphosis secondary to
Scheuermann’s disease: a review of 32 patients. Spine. 1994;19(15):1680-1685.
CB. Transient paraparesis: a complication of the surgical management of
Scheuermann’s kyphosis secondary to thoracic stenosis. Spine. 2001;26(9):1086-1089.
H, Roussouly P, Berthonnaud E, et al. Spondylolisthesis, pelvic
incidence, and spinopelvic balance: a correlation study. Spine. 2004;29(18):2049-2054.
PL, Cole HO, Herring JA, et al. Cauda equina syndrome after in situ
arthrodesis for severe spondylolisthesis at the lumbosacral junction. J Bone Joint Surg Am. 1990;72(3):369-377.
DC, Boachie-Adjei O, Donaldson WF III, et al. SRS Morbidity and
Mortality Committee Analysis of Changing Surgical Treatment Trends for
Spondylolisthesis 1996 to 2002. Presented at SRS 38th Annual Meeting. 2002. Quebec City, Canada.
GT, Watson KD, Silman AJ, et al. Predictors of low back pain in British
schoolchildren: a population-based prospective cohort study. Pediatrics. 2003;111(4 Pt 1):822-828.
RW, Bridwell KH, Lenke LG, et al. Complications in the surgical
treatment of pediatric high-grade, isthmic dysplastic
spondylolisthesis. A comparison of three surgical approaches. Spine. 1999;24(16):1701-1711.