Foot Disorders
bean-shaped configuration. The lateral border of the foot is curved
rather than straight. The forefoot is deviated inward relative to the
hindfoot. The hindfoot is in neutral or slight valgus. The ankle is
supple. Metatarsus adductus is usually noted at birth but it may be
present at any age. Metatarsus adductus is a common cause of in-toeing
in otherwise normal newborns and infants.
intrauterine compression or “packaging”. This etiology has not been
proven. Presumably, the feet are compressed during intrauterine
development.
adductus. The condition may persist longer in premature babies.
First-born babies, large babies, and twinning may predispose to
metatarsus adductus due to intrauterine crowding. Metatarsus adductus
is reportedly seen in association with developmental dysplasia of the
hip, although several large series have not borne this out.
Theoretically, the packaging problem that leads to metatarsus adductus
can also affect the adducted hip. Therefore, the child presenting with
metatarsus adductus should have a careful hip examination. Pelvic
imaging is necessary only if there is a positive finding on the hip
examination.
adduction of the metaphysis of the second through the fifth
metatarsals, and medial deviation of the articular surface of the
medial cuneiform have been demonstrated in stillborn infants with
metatarsus adductus.
flexibility of the deformity. The three classification grades are:
actively correctable, passively correctable, or rigid. Actively
correctable feet straighten out when the lateral border of the foot is
stroked by the examiner’s finger and the muscles of the child’s foot
contract correcting the C-shape to neutral. The passively correctable
foot straightens out with gentle manipulation. To manipulate the foot,
grasp the heel with one hand and push the inward-turning forefoot
outward with your other hand in order to realign the foot in a straight
position and reverse the C-shaped outer border of the foot. The rigid
metatarsus adductus does not correct with manipulation. The rigid case
typically has a medial soft tissue crease at the tarsometatarsal level
with a medial soft tissue contracture. As the forefoot is pushed
laterally, the great toe will abduct and a tight abductor hallucis can
be palpated medially.
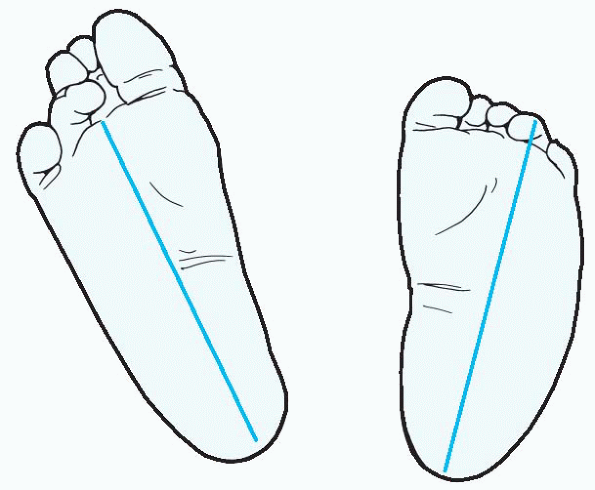
This heel bisector should hit between the second and third rays of the
foot. If it hits the third ray, the metatarsus adductus is mild; the
fourth ray, moderate; and the fifth ray, severe. This measurement can
be used to follow the deformity over time.
 |
|
Figure 4.1-1
Severity of metatarsus adductus can be assessed by extrapolating from a line that bisects the heel and extends through the toes. In normal feet (left) this line hits between the second and third rays of the foot. With the line hitting the fourth ray, the degree of adduction in the root on the right is moderate. |
Radiographs are rarely needed. The outer border of the foot is curved
or C-shaped. When viewed from the dorsal surface, the entire foot
appears to be turned inward. When the foot is viewed from the plantar
surface, the sole of the foot has the shape of a bean. The base of the
fifth metatarsal may appear prominent. The arch may appear high. The
space between the first and second toe may appear wide. The first toe
often seems to be reaching medially. The ankle joint and heel alignment
are normal or in slight valgus in metatarsus adductus. If the foot
demonstrates a fixed valgus hindfoot then the child does not have
metatarsus adduction: instead the diagnosis of skewfoot (forefoot
adductor, midfoot abduction, and heel valgus) should be considered. The
ankle joint is supple in metatarsus adductus. For example, the foot
could easily dorsiflex above the neutral position. If the foot
demonstrates fixed equinus and cannot dorsiflex, and the hindfoot is in
a varus position, then the child does not have metatarsus adductus:
instead the diagnosis of clubfoot should be considered.
-
Spontaneous active medial deviation of the foot
-
High arch
-
Concave medial border of the foot
-
Separation of the first and second toes
-
Fixed adduction of the forefoot when the hindfoot is held in neutral
-
Bean-shaped sole of the foot
diagnosis or treatment of metatarsus adductus. Radiographs are taken in
the rare case undergoing surgery or in the patient being evaluated for
possible skewfoot. Radiographs should be taken in the weightbearing
position. Metatarsus adductus radiographs show medial deviation of the
metatarsals at the tarsometatarsal joints and in some cases medial
deviation of the metatarsal shafts. Radiographs in adults followed
long-term for metatarsus adductus demonstrate obliquity of the medial
cuneiform-metatarsal joint.
not require treatment. About 90% of metatarsus adductus is flexible and
actively correctable. These cases correct spontaneously during the
first 2 years of normal growth and development. Reassurance and
education for the parents about the natural history of the deformity is
indicated.
adductus is controversial. Some authors recommend observation of the
foot and reassurance and education for the parents because many of
these feet will correct without intervention. Other authors recommend
that the passively correctable foot with metatarsus adductus can be
treated by passive stretching exercises of the foot by the child’s
parents. The exercises are performed by holding the heel in one hand
and pushing the forefoot outward to correct the C-shape of the foot.
The foot is stretched in this manner for about 3 seconds and repeated 5
times. The exercises can be easily performed at each diaper change.
Reverse last shoes can be used to maintain correction. Although
exercises and reverse last shoes are commonly used, their efficacy has
not been proven.
metatarsus adductus that has failed an attempt at stretching exercises
for 3 months can be treated with serial manipulation and casting.
Short-leg or long-leg casts have both been used successfully. Casts are
removed and the foot is remanipulated at 1- to 2-week intervals until
the convexity of the lateral border of the foot is straightened.
Correct molding of the cast is very important. After application of the
plaster, molding is performed with the lateral fulcrum at the
calcanealcuboid joint. The calcaneus is pushed medially and the
forefoot is pushed laterally. Once correction is achieved, reverse last
shoes can be used to maintain the correction. Adding a Denis Browne bar
to the reverse last shoe is not recommended because of the tendency
of
the bar to produce correction through the subtalar joint resulting in
hindfoot valgus and a flatfoot. Casting is reported to be most
effective in children younger than 8 months of age; however,
improvement has been reported in children as old as 2 years of age. A
Wheaton brace, a removable plastic version of a stretch cast, is also
an option.
at presentation and documenting the changes in the shape of the foot
over time during observation or active treatment involves taking
photocopies of the foot in the weightbearing position.
surgical correction. Surgical indications include the rigid foot that
has failed serial casting and the older child who presents with fixed
adduction deformity and shoe-fitting problems.
treatment of rigid metatarsus adductus. Outcomes are reportedly good in
most cases; however a standardized outcome measure does not exist.
Surgery can include tendon releases, joint releases, osteotomies or
combinations of any of these. In the young child the simplest surgical
procedure includes release of the abductor hallucis tendon with or
without capsulotomy of the first tarsometatarsal joint followed by
casting. Release of the tarsometatarsal joints of all five toes has
also been reported. However, reports of the development of degenerative
arthritis at the operated joints have tempered enthusiasm for this
once-popular operation. In the older child, metatarsal osteotomies can
be performed. Complications specific to this procedure include
cross-union of the osteotomies and iatrogenic closure of the proximal
first metatarsal physis. In the child older than 5 years of age, a
lateral closing wedge osteotomy of the cuboid combined with a medial
opening wedge osteotomy of the first cuneiform can be performed. The
graft from the cuboid can be used to hold the medial osteotomy open.
reverse last shoes is commonly practiced following surgical correction
of metatarsus adductus. The recommended duration of bracing or special
shoe wear varies by author but can last for up to 2 years.
R, Stevens PM. Idiopathic forefoot-adduction deformity: medial
capsulotomy and abductor hallucis lengthening for resistant and severe
deformities. J Pediatr Orthop 1997;17:496-500.
DS, Levitsky DR. Cuneiform and cuboid wedge osteotomies for correction
of residual metatarsus adductus: a surgical review. J Foot Ankle Surg
1995;34:371-378.
P, Weinstein SL, Ponseti IV. The long-term functional and radiographic
outcomes of untreated and non-operatively treated metatarsus adductus.
J Bone Joint Surg 1994;76A:257-265.
JB, Johanson JE, Winter RB. The Heyman-Herndon tarsometatarsal
capsulotomy for metatarsus adductus: results in 48 feet. J Pediatr
Orthop 1987;7:305-310.
hindfoot equinus, forefoot adduction, subtalar joint varus, and cavus
of the foot. It is present at birth and the affected foot may exhibit
varying degrees of deformity and rigidity. This condition is also known
as congenital talipes equinovarus. Clubfoot has been described since
antiquity, and the early literature recommended manipulation and
immobilization for treatment. These concepts remain the basis of
clubfoot treatment today.
-
7 per 1,000 in South Pacific Islanders
-
1.2 per 1,000 in Caucasians
-
0.5 per 1,000 in Asians
-
Male:female ratio of 2:1
-
50% bilateral
-
Intrauterine molding
-
Myopathic process
-
Neuropathic process
-
Retracting fibrosis
-
Bone dysplasia (germ plasm defect theory)
-
Prenatal viral infection
-
Primary vascular defect
recognize both environmental and genetic factors. A neuropathic process
is supported by histologic studies that demonstrate abnormal muscle
fiber type within the clubfoot, with a predominance of type I muscle
fiber and a deficiency of type IIb fibers. This fiber type predominance
as well as the presence of abnormal fiber grouping and other
cytostructural changes are cited as evidence of a neuropathic etiology
of clubfeet. An abnormal number of myofibroblasts have also been
reported in the deltoid ligament resected in children with clubfeet.
These cells are involved in wound and scar contracture and it has been
hypothesized that the myofibroblasts may cause a localized soft tissue
contracture contributing to the clubfoot.
The precise mechanism of transmission has not been elaborated, but it
is thought to be either autosomal dominant with variable penetrance or
multifactorial.
-
If both parents have normal feet and have
one affected child with clubfoot, there is a 2% to 5% chance of the
next child having clubfoot. -
If one parent has a clubfoot and one child has a clubfoot, there is 10% to 25% risk of subsequent children having clubfeet.
-
There is a concordance rate of 32.5% in monozygotic twins, compared to a concordance rate of 2.9% in heterozygotic twins.
-
Clubfeet may also occur in conjunction
with other neuromuscular and genetic conditions such as arthrogryposis,
spina bifida, and myotonic muscular dystrophy.
extremity, with much of the clinically significant pathologic anatomy
involving the hindfoot and midfoot. There is controversy about some of
the anatomic findings in the clubfoot, but there are also areas of
general agreement (Box 4.2-2).
the physical examination. In all cases, a thorough physical exam,
including a neurologic examination, should be performed in order to
exclude other conditions associated with a clubfoot. In patients with
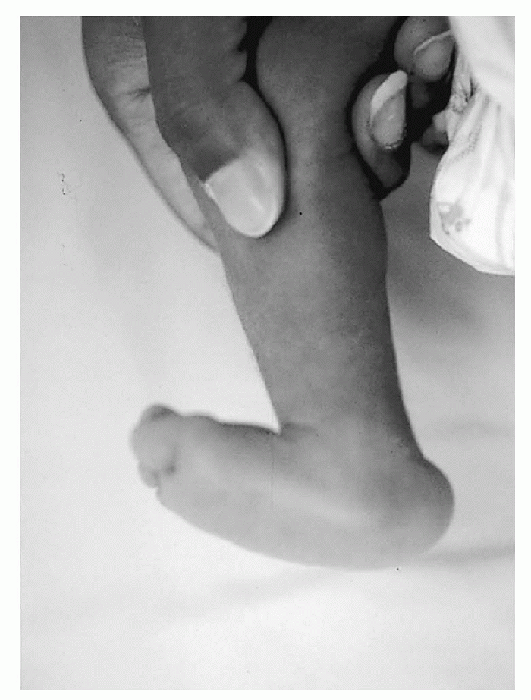
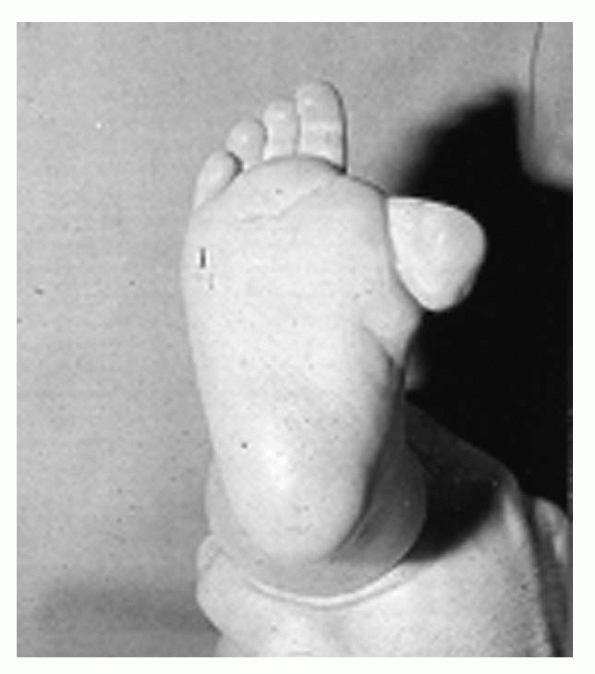
idiopathic clubfoot, positive physical findings include the following (Fig. 4.2-1):
-
Shortening of the entire lower extremity
-
Calf atrophy
-
In unilateral cases the clubfoot will be shorter and wider than the normal foot.
patient’s family at the onset of treatment. Other physical findings include:
-
Cavus, forefoot adductus, subtalar joint varus, and hindfoot equinus, (mnemonic = CAVE)
-
Empty calcaneal fat pad due to proximal migration of the calcaneus
-
Head of talus palpable on dorsolateral foot
-
A medial plantar skin crease, which denotes a more rigid foot
-
The neck of the talus is medially rotated, shortened, and plantarflexed.
-
The subtalar joint is held in internal rotation, equinus, and supination by soft tissue contractures.
-
The calcaneus is rotated medially about the talocalcaneal interosseous ligament and is pulled into equinus.
-
The plane of the talocalcaneal joint is oblique. Medial rotation of the calcaneus results in simultaneous adduction and varus of the calcaneus.
-
This medial rotation of the calcaneus
also results in approximation of the posterior tuberosity of the
calcaneus to the fibula with resulting contractures of the calcaneofibular ligament. -
The navicular is medially displaced and there may be a pseudoarticulation present between the navicular and the medial malleolus.
-
The cuboid may exhibit medial subluxation or dislocation secondary to a medial tilt of the calcaneocuboid joint.
-
The soft tissues
of the clubfoot are also contracted and fibrotic. There are
contractures of the spring ligament, the posterior tibial tendon, the
Achilles tendon, the flexor digitorum longus tendon, the flexor
hallucis longus tendon, the plantar fascia, the short plantar muscles,
tendon sheaths, and the talocalcaneal interosseous ligament. -
Joint capsules, particularly involving the posterior ankle and subtalar joint have contractures in the rigid clubfoot.
-
The amount and direction of tibial torsion and rotation of the body of the talus in the ankle mortise are controversial.
 |
|
Figure 4.2-1 (A) Six-week-old boy with bilateral clubfoot. Note the cavus, adduction, varus, and equinus position of the foot. (B) The arrow indicates a medial crease in the midfoot.
|
well. The presence of rigid hindfoot equinus differentiates a clubfoot
from metatarsus adductus. Several classification systems have been
proposed but none are universally accepted.
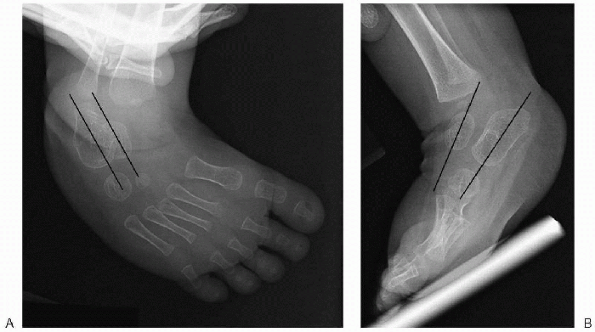
evaluation and treatment of clubfoot. The bones in an infant’s foot are
primarily cartilaginous and any ossification centers present are
frequently located eccentrically, making radiographic interpretation
difficult. Radiographs, however, may have a role intraoperatively or in
the older infant or child to confirm correction or to analyze
deformity. Anteroposterior (AP) and lateral foot radiographs should be
taken in a weightbearing position. In children who are not yet
standing, this is enacted through simulated weightbearing radiographs
done with maximum ankle dorsiflexion. In severe deformity separate
radiographs may be needed of the ankle and foot, since orthogonal
radiographs of one area may result in oblique views of the other. The
AP and lateral talocalcaneal angles should be measured. On both of
these projections this angle will be decreased (normal is 25 to 45
degrees) and there will be increased parallelism between the talus and
calcaneus (Fig. 4.2-2).
With ambulation, weightbearing occurs on the dorsolateral aspect of the
foot and ankle. Normal shoe wear is not possible and a callus and bursa
forms over the dorsolateral foot. This typically becomes painful over
time and makes ambulation difficult.
nonoperative. Techniques using serial manipulation with casting,
splinting, taping, physical therapy, and the use of continuous passive
range of motion machines have all been described. Serial manipulation
and casting is currently the standard for initial treatment in the
United States. There are two prevailing schools of thought regarding
serial casting. The Kite technique corrects the foot through the use of
short leg casts changed every 1 to 2 weeks. The foot is rotated about
the calcaneocuboid joint and the clubfoot is corrected in a specific
order: adduction is corrected first, followed by varus and equinus.
Success rates for this technique have been reported to be between 15%
and 50%. The Ponseti technique has recently become popular due to its
reported high success rate and low complication rate in the treatment
of clubfeet. This currently is the preferred technique. The Ponseti
method relies on serial casting, and incorporates several very
important differences when compared to the Kite technique.
Conceptually, the Ponseti
technique
emphasizes external rotation of the midfoot and forefoot about the
talus while initially maintaining the foot in supination. This is
achieved by:
 |
|
Figure 4.2-2 Anteroposterior (A) and lateral (B) radiographs of clubfoot in a 1-year-old child. Both views show parallelism between the talus and the calcaneus.
|
-
Using weekly manipulations and long leg casts. The foot is corrected in a precise order.
-
Dorsiflexing the first ray to stretch the
plantar fascia and to unlock the talonavicular joint, which loosens the
foot and allows for correction. -
Supinating the foot for the initial casts.
-
Abducting the forefoot around the talus
using the talar head as the center of rotation. This results in
simultaneous correction of supination, adduction, and varus as the
calcaneus midfoot and forefoot rotate about the talus. -
Dorsiflexing the hindfoot once the other components have been corrected.
correct hindfoot equinus. This may be done as an outpatient procedure
in the office. Patients are then maintained fulltime in a Denis Browne
bar until they start to stand and nighttime bracing is continued for 2
to 3 years. Due to recurrence, 30% of patients require a transfer of
the anterior tibialis tendon at 3 to 4 years of age.
success rate, with 78% good or excellent results at an average 30-year
follow-up. Regardless of the method chosen casting should begin within
the first few weeks of life. Complications of casting include:
-
Rocker bottom foot formation with dorsiflexion occurring through the midfoot instead of the ankle
-
Deformation of the cartilage resulting in joint stiffness
-
Physeal injury
casting is required to avoid complications and achieve the best results.
with clubfeet secondary to neuromuscular or congenital condition often
require operative intervention. Surgery is generally done between 6 to
12 months of age. Multiple surgeries have been described for clubfoot
and many surgeons will tailor the procedure to the needs of the
individual, creating an “a la carte” approach to clubfoot surgery.
Multiple incisions have also been described for the surgery. The two
most commonly used incisions are:
-
The Cincinnati incision, which is a circumferential incision around the posterior of the foot.
-
A two-incision (medial and lateral) technique can also be safely and effectively used.
either approach; in all cases, this phrase applies: “the decision (of
which structures to release) is more important than the incision.”
-
Release of the plantar structures including the plantar fascia to correct cavus.
-
A medial and posteromedial release with
lengthening of the posterior tibial tendon, the flexor hallucis longus
tendon, the flexor digitorum longus tendon, and release of their tendon
sheaths into the knot of Henry. The abductor hallucis muscle is taken
down and released. A
P.24talonavicular
joint capsulotomy is performed to allow reduction of the navicular onto
the talar head. A medial subtalar joint release is also performed while
preserving the talocalcaneal interosseous ligament (although some
surgeons release this ligament as well). -
A posterior release including Achilles
tendon lengthening, posterior ankle capsulotomy and posterior subtalar
join capsulotomy is also performed to correct the equinus. -
Posterolateral and lateral releases are
also often performed during surgical correction of a clubfoot. A
posterolateral release involves dividing the calcaneofibular ligament
and peroneal tendon sheath to allow external rotation of the calcaneus.
A calcaneocuboid capsulotomy may also be performed in order to realign
the cuboid with the long axis of the calcaneus and produce a straight
lateral border of the foot.
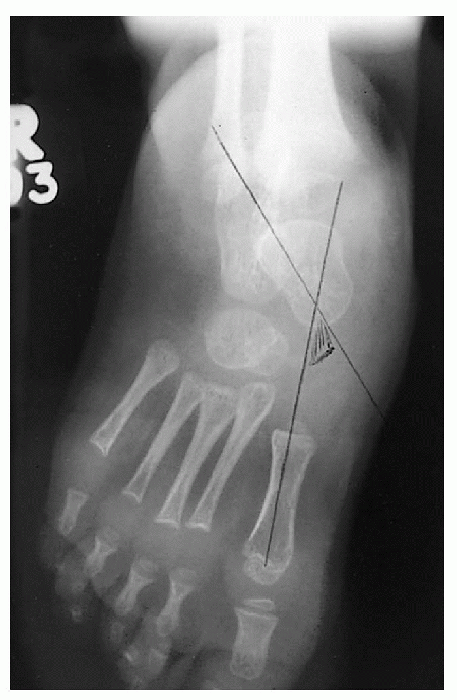
after surgery, particularly after more extensive releases. Typically, a
smooth 0.062-inch Kirschner wire is used to transfix the talonavicular
joint for 4 to 6 weeks. Postoperative casting and care varies.
Generally some type of bracing is used after surgery, but the type and
duration varies widely from surgeon to surgeon.
-
Neurovascular injury
-
Cartilage damage
-
Direct bone injury
-
Avascular necrosis of the talus and navicular
-
Wound healing problems
-
Recurrence
-
Stiffness
-
Dorsal bunion
-
Undercorrection
-
Overcorrection
-
Residual deformity—the most common residual deformity after clubfoot surgery is forefoot adduction.
be individualized. Repeat soft tissue releases, tendon transfers,
osteotomies, and fusions may all be used alone or in combination to
treat the recurrent, residual, or overcorrected clubfoot.
S, Chesney D, Miedzbrodzka Z, et al. Genetics and epidemiology of
idiopathic congenital talipes equinovarus. J Pediatr Orthop
2003:23:265-272.
H, Csukonyi Z, Desgrippes Y, et al. Surgery in residual clubfoot:
one-stage medioposterior release “a la carte.” J Pediatr Orthop
1987;7:145-148.
AH, Marxen JL, Osterfeld DL. The Cincinnati incision: a comprehensive
approach for surgical procedures of the foot and ankle in childhood. J
Bone Joint Surg (Am) 1982;64: 1355-1358.
YN, Carroll NC. Analysis of the components of residual deformity in
clubfeet presenting for reoperation. J Pediatr Orthop 1992;12:207-216.
VJ. Resistant congenital clubfoot: one-stage posteromedial release with
internal fixation: a follow-up report of a fifteen-year experience. J
Bone Joint Surg Am 1979:61:805-814.
unknown etiology that was first described by Henken in 1914. Other
synonyms for this deformity include rocker bottom foot, rigid flatfoot,
and convex pes valgus. About half of all CVT cases occur as an isolated
deformity; the remainder have additional pathology. The hallmark of
this condition is the fixed vertical position of the talus that does
not correct with maximum plantarflexion of the foot.
CVT is associated with other abnormalities or is part of genetic or
neuromuscular conditions. Box 4.3-1 lists conditions associated with CVT.
-
CVT is a rare condition.
-
It is bilateral in approximately 50% of cases.
-
There is no definite gender or racial difference.
-
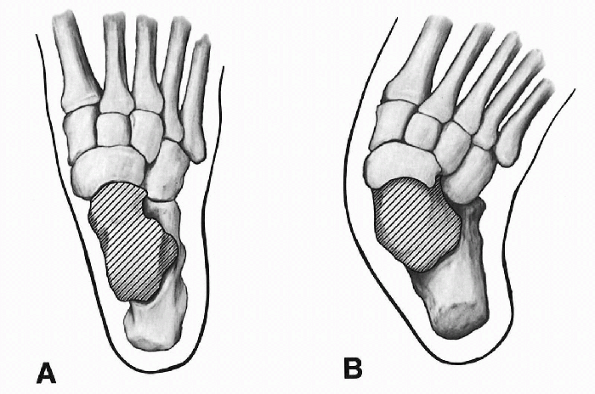
Dorsal dislocation of the talonavicular joint where the navicular lies dorsal to the talus
-
Equinus position of the talus
-
Equinus position of the calcaneus
-
Osseous changes (Figs. 4.3-1 and 4.3-2)
-
□ The talus is plantarflexed and medially deviated. This deformity is rigid.
-
□ The os calcis
is in equinovalgus and is abducted or laterally subluxed underneath the
talus. It is in close contact with the lateral malleolus. -
□ The navicular is dorsally dislocated on the talar neck.
-
□ As a result of these primary changes,
secondary adaptive changes develop. The dislocated navicular adapts to
this new position and becomes wedge-shaped with a hypoplastic plantar
segment. The sustentaculum becomes hypoplastic and offers no support to
the talar head. The calcaneocuboid joint gradually subluxes. -
□ The cuboid becomes displaced laterally and dorsally.
-
-
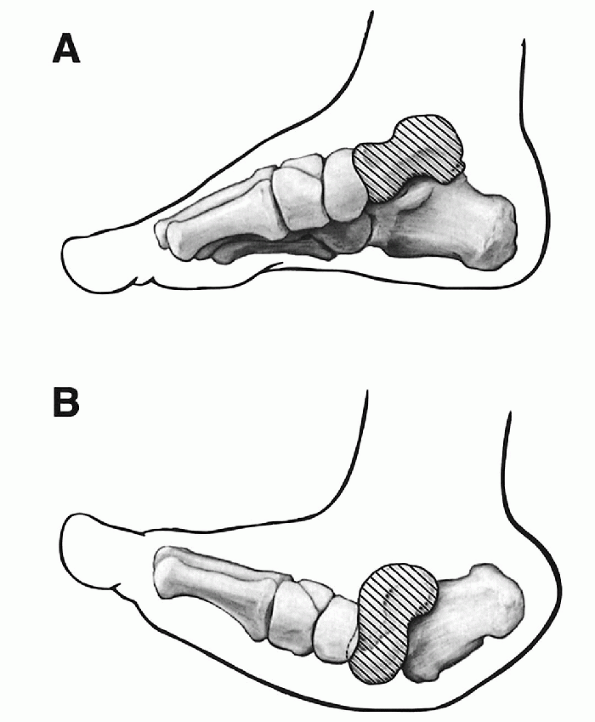
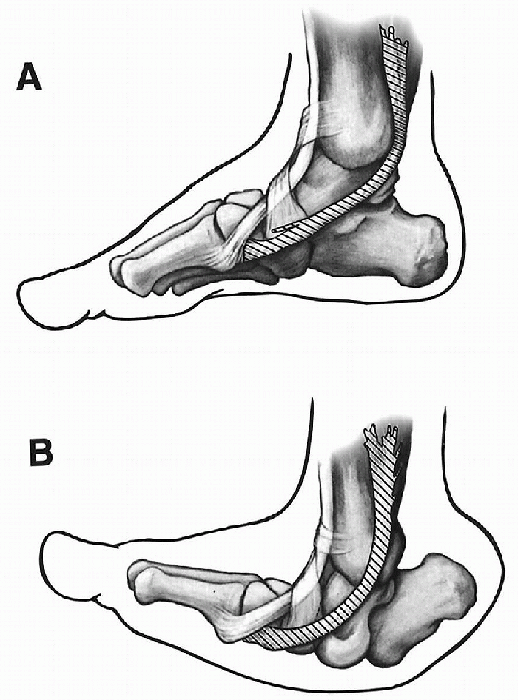
Ligamentous changes (Fig. 4.3-3):
-
□ Stretching of the calcaneonavicular or spring ligament.
-
□ Contractures of the lateral part of the
talonavicular capsule, the calcaneofibular, the interosseous
talocalcaneal ligament, and the posterior capsule of the ankle and
subtalar joints. The dorsolateral part of the calcaneocuboid capsule
may also be contracted.
-
-
□ Muscular and tendinous changes:
-
□ Contractures of:
-
□ Tibialis anterior tendon
-
□ Long extensors of the toes
-
□ Peroneal tendons
-
□ Tendo Achilles
-
-
□ Anterior subluxation of:
-
□ Tibialis posterior tendon (Fig. 4.3-4)
-
□ Peroneal tendons
-
-
-
□ Retinacular changes (Fig. 4.3-5):
-
□ The dorsal extensor retinaculum is thickened and contracted.
-
□ The superior peroneal retinaculum is stretched.
-
 |
|
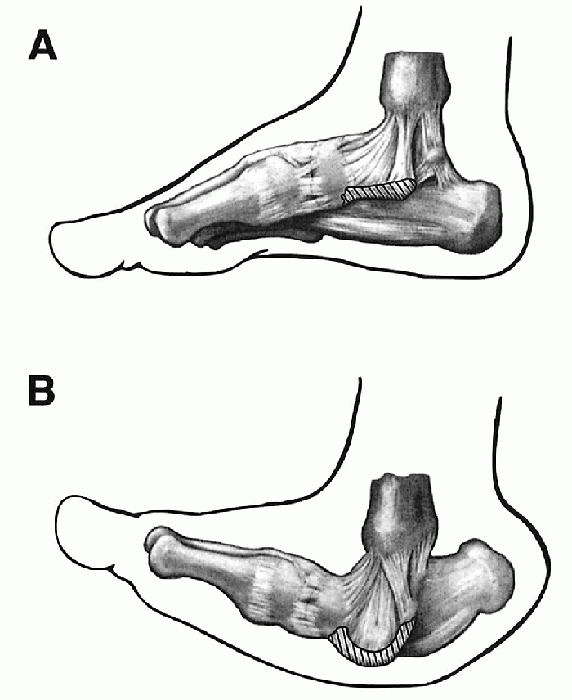
Figure 4.3-1 Osseous changes as viewed from the top. (A) Normal foot. (B)
Foot with vertical talus. (Adapted from Kumar SJ, Cowell HR, Ramsey PL. Foot problems in children. AAOS Instr Course Lect 1982;31:235-251.) |
-
Myelomeningocele
-
Diastematomyelia
-
Hydrocephalus
-
Cerebral palsy
-
Poliomyelitis
-
Trisomies 13, 15, 17, and 18
-
Freeman-Sheldon disorder
-
Nail patella syndrome
-
Marfan syndrome
 |
|
Figure 4.3-2 Osseous anatomy as seen from a medial view. (A) Normal foot. (B)
Elongated talar neck in congenital vertical talus. (Adapted from Kumar SJ, Cowell HR, Ramsey PL. Foot problems in children. AAOS Instr Course Lect 1982;31:235-251.) |
Lichtblau described three types according to etiology: teratogenic,
neurogenic, and acquired. Pouliquen suggested a radiologic
classification based on the talocalcaneal angle and reducibility of the
equinus of the os calcis on the lateral x-ray of the foot. The most
practical classification, however, is the one described by Ogata and
colleagues:
 |
|
Figure 4.3-3
The plantar calcaneonavicular ligament is stretched and attenuated in a foot with vertical talus. Note the contrast between the normal foot (A) and the deformed foot (B). This structure is not clearly visualized during surgery. (Adapted from Kumar SJ, Cowell HR, Ramsey PL. Foot problems in children. AAOS Instr Course Lect 1982;31:235-251.) |
-
Primary isolated form
-
Associated form without neurologic deficit (e.g., dislocated hip, clubfoot, hand anomalies)
-
Associated form, with neurologic deficit
-
Equinusvalgus position of the hindfoot
-
Rocker bottom deformity of the midfoot
(formed by the dislocated head of the talus which can be palpated on
the medial and plantar aspect of the foot) -
Dorsiflexion and abduction of the forefoot
the dislocated head of the talus and this may cause pain. Most of the
weightbearing area of the foot is centered over the dislocated head of
the talus.
 |
|
Figure 4.3-4 Orientation of the anterior and posterior tibial tendons. (A) Normal foot. (B)
Foot with vertical talus, showing contracture of the tibialis anterior tendon and subluxation of the tibialis posterior tendon. (Adapted from Kumar SJ, Cowell HR, Ramsey PL. Foot problems in children. AAOS Instr Course Lect 1982;31:235-251.) |
However, the gait may be awkward and clumsy. Wearing of shoes may cause
problems.
associated with other abnormalities such as dislocation of the hip or
are part of neuromuscular conditions such as arthrogryposis, spinal
dysraphism, and cerebral palsy.
suspected, a complete physical and neurologic examination of the child
should be performed. Magnetic resonance imaging (MRI) of the spine is
recommended.
cartilaginous. The ossification center of the cuboid appears within the
first month of life, while that of the navicular appears
between
2 and 5 years of age. However, a radiologic diagnosis of CVT can still
be made in the neonate by the appearance of the fixed vertical position
of the talus.
 |
|
Figure 4.3-5 Tendons on the lateral and posterior aspect of the foot. (A) Normal foot. (B)
A foot with vertical talus has a contracted tendo Achilles, anterior subluxation of the peroneal tendons, contracture of the dorsal extensor retinaculum, and attenuation of the superior peroneal retinaculum. In addition, the course taken by the peroneus tertius is straighter. (Adapted from Kumar SJ, Cowell HR, Ramsey PL. Foot problems in children. AAOS Instr Course Lect 1982;31:235-251.) |
 |
|
Figure 4.3-6 Clinical appearance of congenital vertical talus.
|
important view, both in neutral and maximal plantar flexion as this
will differentiate between an oblique and a vertical talus. In the
neutral view, both oblique talus and CVT may appear the same. However,
in the maximum plantarflexion view, an oblique talus will reduce and
there is realignment of the long axis of the talus with that of the
first metatarsal, as shown in Figure 4.3-7. This does not occur in cases of CVT, as shown in Figure 4.3-8. Other angles measured in the lateral view include:
 |
|
Figure 4.3-7 Radiologic appearance of oblique talus showing restoration of the normal talo-first metatarsal angle in maximal plantarflexion.
|
 |
|
Figure 4.3-8
Lateral view of congenital vertical talus (A) showing vertical position of the talus that will not correct with maximum plantarflexion (B). |
-
Talocalcaneal angle: either increased or decreased
-
Tibiocalcaneal angle: measures the amount of equinus of the os calcis
-
Talo-first metatarsal angle: increased (normal 0 to 10 degrees).
-
Talocalcaneal angle: increased
-
Talo-first metatarsal angle: increased
-
Calcaneo-fifth metatarsal angle: increased
-
This is the most common differential diagnosis in the neonatal period.
-
There is no equinus of the heel but rather a pure calcaneus deformity.
-
The calcaneovalgus deformity responds
very well to passive manipulation and corrects completely after a few
weeks or months of stretching.
 |
|
Figure 4.3-9 Anteroposterior view showing increased talo-first metatarsal angle.
|
-
Oblique talus usually presents as a
severe flatfoot deformity, either idiopathic flatfoot or associated
with other conditions such as Down syndrome. An oblique talus is
flexible in contrast with CVT, which is a rigid deformity. -
Usually there are no associated neurologic abnormalities.
-
The differentiation between an oblique
and a vertical talus is made on a lateral view of the foot and ankle in
neutral and in maximal plantar flexion as previously mentioned. -
The treatment of oblique talus is
completely different than that of vertical talus. If the deformity is
flexible, usually no surgical treatment is indicated. In cases where
there is contracture of the tendo Achilles, treatment includes
stretching of the tendon and repeated casting or lengthening of the
tendon. Many surgical procedures have been described for the treatment
of oblique talus (the same as for severe flatfoot deformities).
 |
|
Figure 4.3-10 Clinical appearance of a calcaneovalgus foot.
|
-
In these cases, there is very limited
subtalar motion. Radiologic examination reveals the coalition most
commonly in the calcaneonavicular or talocalcaneal joints.
-
This may develop as a complication of clubfoot surgery.
always surgical. Casting is applied usually for stretching of the
anteriorly contracted structures. Surgery is usually indicated before
walking age, around 9 to 12 months of age.
-
Reduction of the talonavicular dislocation
-
Restoration of normal weightbearing area of the foot
-
Obtain a plantigrade and braceable foot in cases where braces are indicated.
subluxation and the second stage (6 weeks later) is directed at
correcting the equinus deformity of the heel. The main disadvantage of
this technique is the high incidence of avascular necrosis (AVN) of the
talus.
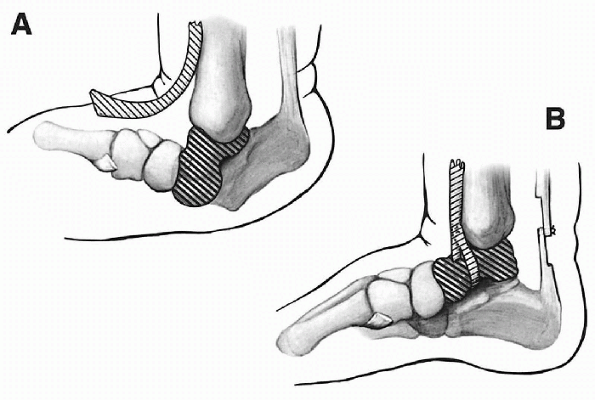
surgery. Details of this procedure are well described by Drennan,
Tachdjian, and Kumar (Fig. 4.3-11). A single
Cincinnati skin incision or a combination of two or three incisions can
be used. Releases are performed posteriorly, laterally, and medially:
-
Posterior approach:
-
□ Achilles tendon is lengthened.
-
□ Ankle and subtalar joints are released.
-
□ Talofibular and calcaneofibular ligaments are incised.
-
-
Lateral approach (centered over the sinus tarsi):P.30
-
□ Extensor digitorum brevis muscle is reflected.
-
□ Sinus tarsi is cleaned.
-
□ Calcaneocuboid joint is opened.
-
□ Interosseous talocalcaneal ligament is incised.
-
□ Peroneal tendons are lengthened.
-
-
Medial approach:
-
□ Complete capsulotomy of the talonavicular joint is performed.
-
□ Capsule is incised near the navicular to avoid AVN of the talus.
-
□ Tibialis posterior tendon is dissected and incised.
-
-
The following tendons are lengthened:
-
□ Tibialis anterior
-
□ Extensor hallucis longus
-
□ Extensor digitorum longus
-
-
Reduction of the talonavicular dislocation:
-
□ Kirschner wire (K-wire) is inserted in
the posterior aspect of the talus and used as a lever to reduce the
talonavicular joint. -
□ Equinus position of the calcaneus is
corrected with a K-wire and the calcaneocuboid joint reduced if
necessary and held in place with a K-wire. -
□ Capsulorrhaphy of the talonavicular joint is performed.
-
□ The tibialis posterior tendon is transferred to the plantar aspect of the navicular to support the head of the talus.
-
□ Transfer of the tibialis anterior to the neck of the talus through a drill hole in the neck of the talus may be performed (Fig. 4.3-12).
-
-
Other bony procedures described in the treatment of CVT include:
-
□ Excision of the navicular
-
□ Talectomy
-
□ Grice procedure
-
□ Triple arthrodesis.
-
 |
|
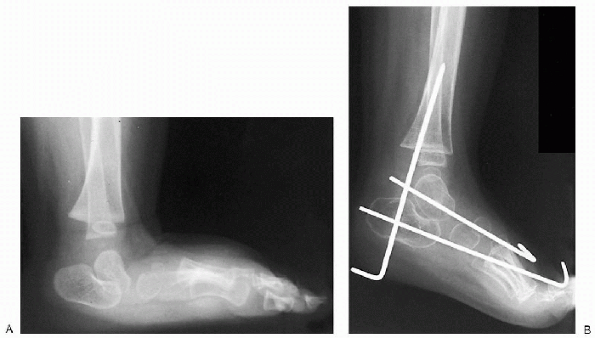
Figure 4.3-11 Preoperative (A) and postoperative (B) x-rays.
|
 |
|
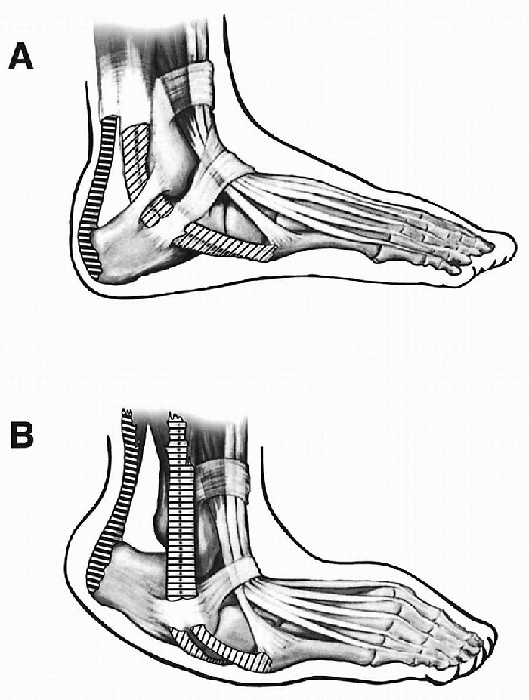
Figure 4.3-12 (A)
Isolation of the anterior tibial tendon and placement of the drill hole in the talar neck. Depending on the size of the tendon, either the whole tendon or, preferably, only two-thirds of it is detached. (B) Tendon threaded through the drill hole and sutured onto itself. (Adapted from Kumar SJ, Cowell HR, Ramsey PL. Foot problems in children. AAOS Instr Course Lect 1982;31:235-251.) |
recurrent cases in which a standard soft tissue release as previously
described fails to correct the deformity.
-
The pins are removed after 2 months.
-
Total period of cast immobilization is 3 to 4 months.
-
Complications are common and include skin
necrosis, infection, AVN of the talus, and, most important, recurrence
of the talonavicular dislocation.
However, the numerous surgical procedures reported, as well as the wide
range of rigidity and severity of the deformity, make it very difficult
to compare the results of published series.
-
Poor cosmetic appearance
-
Ankle plus subtalar motion loss
-
Prominent talar head
-
Loss of medial longitudinal arch
-
Hindfoot valgus
-
Abnormal shoe wear
-
Abnormal appearance
-
Hindfoot equinus
-
Talometatarsal axis
-
Talonavicular subluxation
Congenital convex pes valgus: results of an early comprehensive
release. Foot Ankle 1980;1:62-73.
-
Whenever a diagnosis of CVT is made,
other associated conditions should be sought and a complete neurologic
examination performed. MRI of the spine is recommended. -
Radiologic examination of the foot and
ankle in maximal plantarflexion on the lateral view is part of the
diagnosis and should always be performed. -
Congenital vertical talus usually does not respond to casting and surgery is nearly always recommended.
-
Recurrence rate is high. This should be explained to the child’s parents.
correction and parents should be made aware of this complication. The
prognosis for very rigid feet, especially when associated with
neuromuscular or other conditions, should be guarded.
RS, Williams RM, Gould JS. Congenital convex pes valgus: results of an
early comprehensive release. Foot Ankle 1980;1: 62-73.
K, Schoenecker PL, Sheridan J. Congenital vertical talus and its
familial occurrence: an analysis of 36 patients. Clin Orthop
1979;139:128-132.
or bony connection between bones of the hindfoot or midfoot. It is
frequently congenital (but may occasionally be acquired), and is
usually between the calcaneus and talus or navicular. Coalitions may
cause pain and stiffness and a flatfoot in adolescence, and may be
responsible for recurrent ankle sprains. Younger children with
coalitions are often asymptomatic. Adults may also have asymptomatic
coalitions.
computed tomography (CT) or magnetic resonance imaging (MRI) may be
required. Initial treatment should be nonoperative. However, many will
require an operation. Surgery may involve resection of the fusion (with
or without interposition of material to stop recurrence) or
arthrodesis. Results of these operations are good, at least in the
short to medium term.
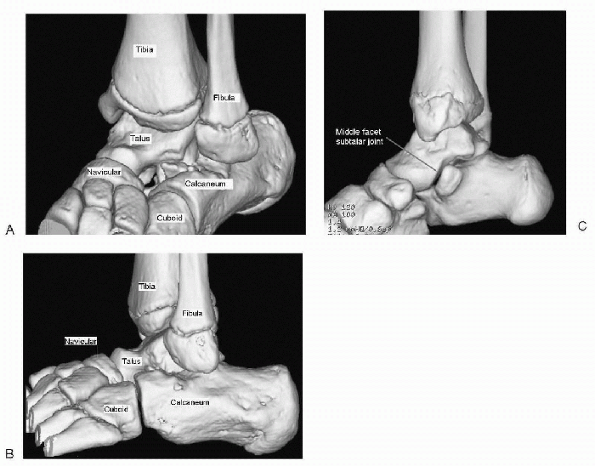
of the hindfoot is complicated. The two bones below the ankle joint lie
on top of each other—the talus above and the calcaneus below. They meet
at the subtalar joint, which has three facets—posterior, middle, and
anterior. Distal to this are two bones that lie side by side: the
navicular on the medial side and the cuboid on the lateral side. The
anterior calcaneus articulates with the cuboid, and the anterior talus
articulates with the navicular.
 |
|
Figure 4.4-1
Normal osseous anatomy of the hindfoot taken from a threedimensional computed tomography reconstruction as seen from the dorsolateral side of the left foot (A), the lateral side of the left foot (B), and the medial side of the right foot (C). |
and calcaneus (i.e., bridging the middle facet) and between the
calcaneus and the navicular (which do not normally form an
articulation).
-
Failure of segmentation of the mesenchymal anlage
-
Bone malformation in the hindfoot
-
Coalitions frequently associated with congenital deficiencies
-
Untreated clubfoot
-
Inflammatory arthritis
-
Intraarticular fractures
-
Osteonecrosis
-
Coalitions alter normal motion that acts as a shock absorber and torque converter:P.33
-
□ Subtalar joint (rotatory, gliding)
-
□ Transverse tarsal joint (“socket” navicular around “ball” of the talar head)
-
□ Ankle joint (talar dome flexing and extending within mortise)
-
-
Coalitions lead to abnormal stresses on adjacent joints resulting in painful symptoms or compensatory adaptations:
-
□ Ball-and-socket ankle joint (abnormal inversion and eversion)
-
□ Traction on talonavicular dorsal capsule (talar beaking)
-
□ Loss of subtalar motion with variable hindfoot valgus
-
-
Incidence: 0.03% to 2% of general population (not all coalitions are symptomatic)
-
□ Calcaneonavicular: 53%
-
□ Talocalcaneal: 37%
-
-
No racial predilection
-
40% to 68% are bilateral
-
Multiple coalitions occur in the same foot in up to 20% of cases
-
Genetics: 39% of first-degree relatives
of an affected individual have a coalition, suggesting unifactorial
autosomal dominant trait
-
Calcaneonavicular (CNC)
-
Talocalcaneal (TCC):
-
□ Middle facet—most common
-
□ Posterior facet
-
□ Anterior facet
-
-
Other:
-
□ Talonavicular (TNC)
-
□ Calcaneocuboid
-
□ Naviculocuneiform
-
□ Cubonavicular
-
-
Type 1: Osseous
-
Type 2: Cartilaginous
-
Type 3: Fibrous
-
Pain initially with activities
-
Repetitive sprains
-
Onset based on ossification:
-
□ CNC: 8 to 12 years
-
□ TNC: 3 to 5 years
-
□ TCC: 12 to 16 years
-
-
Progress: Becomes during symptomatic during teenage years
-
Location:
-
□ Anterolateral or lateral: sinus tarsi
-
□ Peroneal muscles (spasm)
-
 |
|
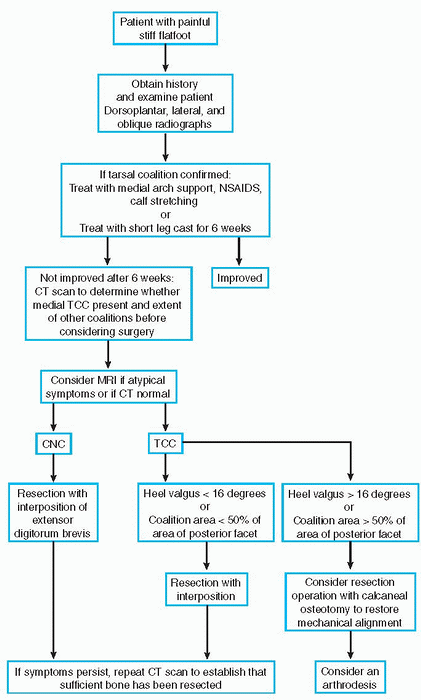
Algorithm 4.4-1 Algorithm for the diagnostic workup of tarsal coalitions.
|
-
Limited or no subtalar motion (easier to identify if coalition is unilateral)
-
No correction of heel valgus or reformation of longitudinal arch on tiptoe
-
Pes planus
-
Hindfoot valgus
-
Flat medial longitudinal arch
-
Midfoot pronation
-
Antalgic gait
-
Peroneal muscle spasm (spastic flatfoot)
-
Rheumatoid arthritis
-
Osteoid osteoma
-
Injury
-
Anteroposterior (dorsoplantar) weightbearing:
-
□ Coalition seen between talus and navicular (TNC)
-
□ Ball-and-socket ankle
-
-
Lateral weightbearing (Fig. 4.4-2):
-
□ Anteater nose (CNC)
-
□ Talar beaking (not degenerative sign) (TCC)
-
□ C sign (of Lateur): Initially thought to be a reliable indicator for middle facet TCC but is actually specific for flatfoot, not coalition)
-
□ Rounding/flattening talar lateral process
-
□ Concave plantar surface: talar neck
-
□ Narrowing of the posterior subtalar facet (TCC)
-
□ Failure to visualize middle subtalar facet (TCC)
-
-
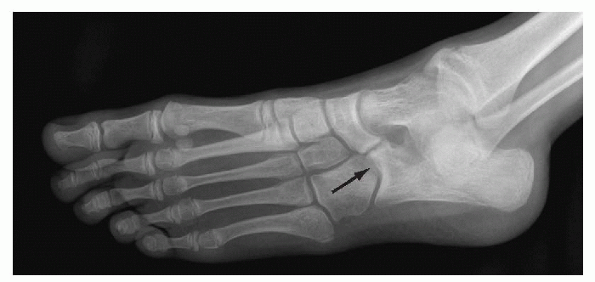
Internal oblique (45-degree angle, Sloman view) (Fig. 4.4-3):
-
□ No gap between calcaneum and navicular (CNC)
-
□ Asymmetry of the anterior subtalar joints (TCC)
-
-
Axial (Harris-Beath view):
-
□ Middle facet TCC
-
 |
|
Figure 4.4-2 Lateral weightbearing view of the hindfoot in a patient with a stiff flatfoot caused by a calcaneonavicular coalition.
|
-
To identify associated unseen coalitions (useful for cases preoperatively)
-
If there is clinical suspicion despite normal x-rays
-
If secondary radiologic signs are present
-
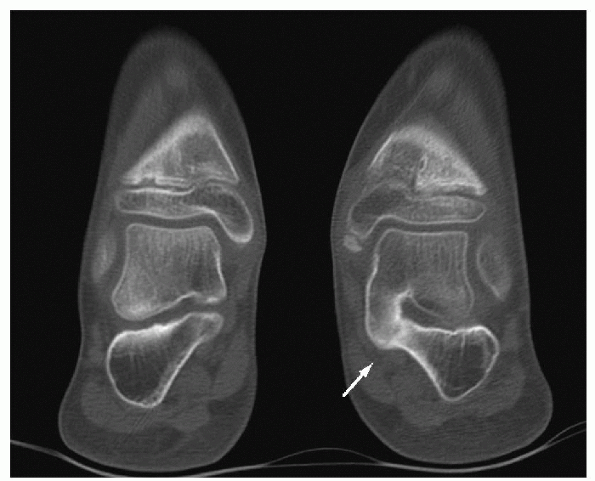
If there is middle facet TCC (Fig. 4.4-4)
-
To differentiate between fibrous, cartilaginous, and osseous.
-
If clinical suggestion is apparent, but CT is normal
-
To differentiate between fibrous and cartilaginous
-
To help detect differential pathology.
-
A screening procedure
-
Useful for localization of pathology
 |
|
Figure 4.4-3
Internal oblique view (45-degree angle, Sloman view) of a stiff flatfoot showing signs of a fibrous calcaneonavicular coalition. |
 |
|
Figure 4.4-4
Coronal computed tomography through both hindfeet showing a middle facet talocalcaneal osseous coalition compared with a normal middle facet on the contralateral foot. |
-
Initial management for all symptomatic coalitions
-
Success rate:
-
□ Less than 33% sustained long-term relief
-
□ Less success for weightbearing coalitions
-
-
Decrease stress
-
Support/correct valgus hindfoot, pronated midfoot
-
Reduce inflammation in mobile joints
-
Decrease peroneal spasm
-
Short leg non-weightbearing/weightbearing casts
-
Shoe inserts (UCBL)
-
Calf muscle stretching
-
Failed nonoperative treatment prior to degenerative changes
-
CN coalitions
-
Joint degenerative
-
Relieve symptoms
-
Improve range of motion
-
Realign foot
-
Excision of coalition with or without interposition
-
Make Ollier incision (oblique over sinus tarsi). Be careful not to injure superficial peroneal nerve.
-
Mobilize extensor digitorum brevis (proximolateral to distomedial).
-
Define bone to avoid injury to talonavicular joint.
-
Perform bone resection parallel in all planes. Beware of tendency to converge toward sole.
-
Interpose extensor digitorum brevis into resection using pull-through suture.
-
Confirm complete resection with intraoperative radiograph.
-
Examine range of motion to confirm increase.
-
Make medial curved incision (part of Cincinnati incision)
-
Identify medial (posterior tibial) neurovascular bundle
-
Find the subtalar joint:
-
□ Open sheaths of tibialis posterior and flexor digitorum longus
-
□ Find posterior subtalar joint through flexor hallucis longus sheath
-
□ Find anterior subtalar joint by
following sustentaculum tali anteriorly then laterally around the
corner to anterior process of calcaneum -
□ Excise bar with burr and rongeurs
-
□ Interpose sheath of flexor hallucis longus, fat, or Gelfoam material
-
□ If heel in valgus, use calcaneal osteotomy
-
-
Make curved incision on lateral foot over subtalar joint
-
Place calcaneum in neutral position (i.e., below talus)
-
Insert cancellous bone graft in sinus tarsi
-
Place cannulated screw through talar neck, across sinus tarsi, into posterolateral calcaneum
-
Surgical fusion:
-
□ Talocalcaneal joint
-
□ Calcaneocuboid joint
-
□ Talonavicular joint
-
-
For severe planovalgus foot or degeneration:
-
□ Make curved incision over sinus tarsi
-
□ Expose and resect the three joints with removal of enough bone to fuse joints in corrected position
-
-
Fix with staples or screws
-
Add cancellous bone graft as necessary
-
Following resection operations: 1-2 weeks partial weightbearing in below-knee cast
-
Following arthrodesis: 12 weeks in a non-weightbearing cast
-
Natural history of untreated peroneal spastic foot at 21 years after diagnosis:
-
□ Only 10% have severe disability
-
□ Average duration of symptoms with bars is 18 months
-
□ Severe tarsal arthritis is unusual
-
-
Results of a survey of 3,600 Canadian male army recruits:
-
□ 74 (2%) had peroneal spastic flatfoot; caused disability
-
□ 217 (6%) had flexible flatfeet; no symptoms or disability
-
-
Results of surgery reported to be good (Table 4.4-1)
|
TABLE 4.4-1 RESULTS OF SURGERY
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
-
Of those who had surgery, failures were attributed to:
-
□ Preexisting talonavicular or subtalar arthritis
-
□ Incomplete excision
-
□ Recurrence of coalition
-
-
Gait analysis 2 to 16 years after TCC resection showed gait abnormality (despite good clinical results)
keep in mind that this condition is very common and is usually
asymptomatic. Approximately 20% of adults have flatfeet, and in 65% of
these adults the condition causes no disability.
flexible flatfoot forms an arch when the patient stands on the tip of
his or her toes. There are two forms of flexible flatfeet: those with
and those without a tight or short Achilles tendon. Though a plain
flatfoot is a benign condition, the flexible flatfoot with a short
Achilles tendon is somewhat more likely to cause pain and disability.
In the patient with a short Achilles tendon, the subtalar and midtarsal
joints pronate to bypass the tight heel cord and get the heel down to
the ground.
position. They generally present during adolescence. Rigid flatfeet are
more likely to be painful. They are usually caused by tarsal coalitions
but may also be the result of the following vertical talus, talipes
calcaneovalgus, compensated metatarsus adductus or skewfoot deformity,
trauma, infections, arthritides, polio, cerebral palsy,
myelodysplasias, or neoplasms.
 |
|
Figure 4.5-1 A normally presenting low arch without pain or biomechanical problems: pes planus.
|
noting any problems at birth and the age at which the onset of
ambulation began. Clinically, one should evaluate rotation of the hips,
tibial/malleolar torsion, foot deformities (i.e., metatarsus adductus),
joint laxity, limb lengths (a flat, pronated foot may indicate a
compensatory mechanism to lower or shorten a longer limb), tightness of
Achilles tendon, Hubscher maneuver (discussed later), foot callosities,
shoe wear patterns, patellar position, and forefoot to hindfoot
relationships.
performed in two ways. The first is the bench exam while the child is
sitting. The other includes a dynamic exam with the child standing and
walking. First, determine whether the flatfoot is flexible or rigid.
The foot may appear to have an arch when non-weightbearing (Fig. 4.5-2A) and present with a lowering or collapsing of the arch when weightbearing (see Fig. 4.5-2B)
indicating flexible flatfoot. This is easily differentiated from the
rigid flatfoot, which will have no arch in both non-weightbearing and
weightbearing circumstances.
flatfoot flexibility. This test is performed with the patient in a
weightbearing position and involves dorsiflexion of the hallux. If a
flexible deformity exists, you should see the first ray plantarflex,
the plantar fascia shorten and tighten, the medial arch rise, the
calcaneus invert, and the leg externally rotate. This movement is a
good sign that the flatfoot is flexible and the patient should respond well to orthotics.
 |
|
Figure 4.5-2 (A) Normal arch appearing when non-weightbearing takes place. (B) Arch collapses with weightbearing, indicating a flexible flatfoot.
|
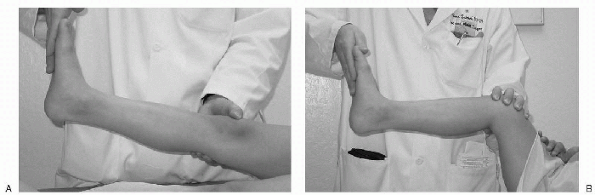
Silverskiöld test. This test is used to determine a gastrocnemius
equinus versus a soleus equinus. With the leg extended (Fig 4.5-3)
the foot is dorsiflexed. If the examiner is unable to acquire 10 to 15
degrees of dorsiflexion with the subtalar joint (STJ) in neutral
position, the knee is then flexed to eliminate the activity of the
gastrocnemius. The foot is again dorsiflexed. If 10 to 15 degrees of
dorsiflexion is still unattainable, a gastrosoleus equinus exists. If
dorsiflexion is available, a gastrocnemius equinus exists.
twisting or bent position of the back (compensating for any scoliosis),
patellar position in the frontal plane, rotation of the leg, heel
strike, toe walking, and foot position. A limp may indicate a leg
length discrepancy with a pronating foot as a compensatory mechanism.
Pronating the foot helps to shorten the longer leg. The normal heel
position at heel strike should be central-lateral. Overpronation
results in a more medial heel strike which results in excessive wear of
shoes. Some hindfoot and midfoot pronation during gait is normal and
allows adaptation to uneven terrain.
 |
|
Figure 4.5-3 (A) Silverskiöld test. Leg is straight and foot is dorsiflexed. Foot acquires less than neutral dorsiflexion. (B) Gastrocnemius is eliminated by flexing the knee. Foot dorsiflexes to approximately neutral. Gastrocsoleus equinus exists.
|
however, a painful or rigid flatfoot may benefit from imaging,
particularly in order to look for tarsal coalitions. The flatfoot on
x-ray can be evaluated by using many different angles and measurements.
Note that in growing children, bones may not be fully ossified;
therefore, certain angles and measurements may not be able to be
determined.
(AP), lateral, oblique, and calcaneal axial (Harris-Beath view), in a
weightbearing position if possible. This gives the truest
representation of the structural relationships of the foot. The AP view
shows transverse plane deformities, particularly the talocalcaneal
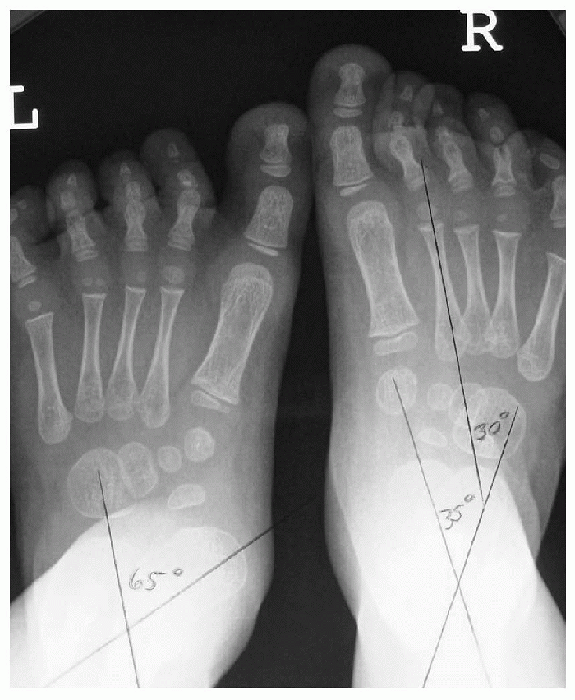
angle (Fig 4.5-4) formed by the bisection of
the calcaneus and talus. As the calcaneus everts and the talus
plantarflexes and adducts with pronation, this angle increases. Normal
pediatric values range from 35 to 50 degrees at birth to 5 years of age
and decrease to 15 to 35 degrees in children more than 5 years of age.
Normal adult values are around 18 degrees. The relationship between the
talus and navicular can also be evaluated. The navicular normally
overlaps the talus approximately 75%. In the abducted, pronated
flatfoot, as the talus begins to plantarflex and
adduct, the navicular covers it less, depending on the severity of the deformity.
 |
|
Figure 4.5-4 Sixty-five-degree talocalcaneal angle on left foot. This angle increases with pronation.
|
This is formed by a line drawn tangential from the medial tubercle of
the calcaneus along the anterior process bisecting a line drawn along
the weightbearing portion of the foot along the fifth metatarsal head
and calcaneus. While this angle can decrease in severe forms of
flatfoot, it is a structural angle, meaning that it could be large in
cases of a cavus foot that has a pronated STJ and midtarsal joint.
Normal values are around 21 degrees.
 |
|
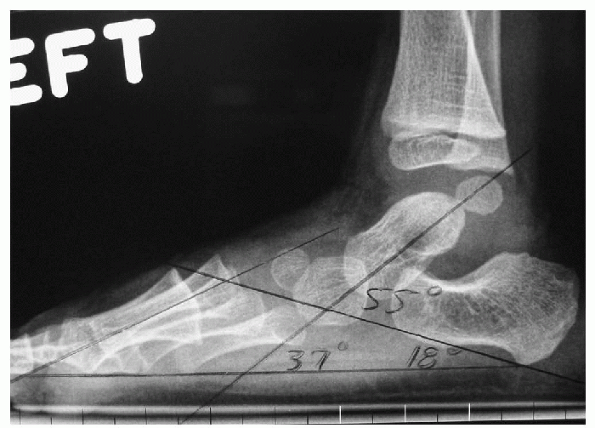
Figure 4.5-5 Calcaneal inclination angle: 18 degrees. Talardeclination angle: 37 degrees. Talocalcaneal angle: 55 degrees.
|
intersecting of a line bisecting the talus and a line drawn along the
weightbearing plane in reference to the fifth metatarsal as previously
described. This angle usually increases with pronation and normally
runs about 21 degrees. If you combine this angle with that of the
calcaneal inclination angle, you get the lateral talocalcaneal angle
formed by bisecting the talus and intersecting it with a line
tangential to the medial tubercle and anterior process of the
calcaneus. This angle also increases with pronation and is about 45
degrees. Calcaneonavicular coalitions may be seen on the 45-degree
oblique view and talocalcaneal coalitions are sometimes seen on the
Harris-Beath view.
Flexible flatfeet that ache may be managed with orthoses. Orthoses are
contraindicated in flexible flatfeet with a tight Achilles tendon, as
raising the arch exacerbates the underlying problem. Treatment in this
case is stretching the Achilles tendon through physical therapy or
casting. Rigid flatfeet may respond temporarily to orthoses but are
more likely to require surgical treatment to correct the underlying
defect or deformity. Various osteotomies of the hindfoot and midfoot
have been described to correct bony deformity. Arthrodesis is rarely
indicated in children and is used primarily as a salvage procedure in
cases of severe subtalar joint arthrosis.
AS, Downey MS, Martin DE, et al, eds. McGlamry’s comprehensive textbook
of foot and ankle surgery, 3rd ed. Philadelphia: Lippincott Williams
& Wilkins, 2001.
LT. Evaluation of planovalgus foot deformities with special reference
to the natural history. J Am Podiatr Med Assoc 1987;77: 2-6.
usually familial disorders. They are often associated with other
anomalies or syndromes.
bilateral in one-third of cases. It is classified as either primary or
secondary. Primary congenital hallux varus is a supernumerary cartilaginous toe anlage presenting on the medial aspect of the foot (Fig. 4.6-1). It is not associated with any other anomalies.
is associated with other anomalies especially polydactyly, true
metatarsus varus, and dysplasia of bone such as dystrophic dwarfism and
Apert syndrome. In secondary congenital hallux, the first metatarsal is
broad and shortened. It is often associated with bracket epiphysis.
needs of the individual deformity. In both types, it is important that
sufficient skin be maintained medially to ensure complete correction.
Sometimes it is necessary to develop a flap to lengthen the shortened
medial side. All the structures medially, including a metatarsal
phalangeal joint capsule and the abductor halluces must be released to
obtain complete correction. If associated with bony deformities of the
distal phalanx (Fig. 4.6-2), an osteotomy is required to prevent recurrence of the deformity.
 |
|
Figure 4.6-1 Primary congenital hallux varus.
|
 |
|
Figure 4.6-2 Joint deformity in residual secondary congenital hallux varus.
|
the result of deformity of the distal phalanx of the great toe, is
deviated laterally toward the second toe at the interphalangeal joint (Fig. 4.6-3). It is
associated with syndromes and is also seen in neurologic conditions
such as cerebral palsy. Treatment is indicated with severe deformities
that result in callus and nail problems. In the younger individual, a
wedge resection of the proximal phalanx is done to realign the toe. In
the older child, an interphalangeal joint fusion is required because of
the adaptive changes that occur at the interphalangeal joint.
 |
|
Figure 4.6-3 Congenital hallux valgus—deformity at interphalangeal joint.
|
distal interphalangeal joint and usually involves a single toe. It is
usually asymptomatic in young children, but can become painful in
adolescence with shoe wear leading to corns as the toe strikes the sole
of the shoe. In infancy treatment consists of stretching and adhesive
strapping to the adjacent toes. Sectioning of the long flexor can treat
more severe deformities, especially on the second or third toe if the
deformity is still flexible. A fusion of the distal interphalangeal
joint is required in the mature foot with a rigid deformity.
proximal interphalangeal joint. Hammertoe deformity is congenital in
origin and often familial. It will often become symptomatic by causing
pressure on the dorsum of the toe by the shoe. Treatment in the infant
consists of stretching exercises in conjunction with adhesive strapping
in corrected position. Flexor tendon transfer can be done in a flexible
deformity in the preadolescent and adolescent. Any fixed deformity
requires fusion of the interphalangeal joint. A flexor tenotomy is also
required in the rigid deformity.
The distal and proximal interphalangeal joints are hyperflexed and the
metatarsophalangeal joint is hyperextended and often dorsally
subluxated. All toes are usually involved in contrast to a mallet toe.
Claw toes are associated with cavus feet seen in neurologic conditions
such as Charcot-Marie-Tooth disease, cerebral palsy, and polio; or as
residuals of compartment syndrome. The condition is listed as
idiopathic only after a thorough search for known etiologies.
the metatarsal heads. Surgical treatment requires correction of any
hindfoot deformity before proceeding with correction of the forefoot.
Flexor tendon transfer to the dorsum of the toe (Girdlestone-Taylor
procedure) along with extensor tenotomies and metatarsophalangeal joint
capsulotomy are used in flexible deformities. In fixed deformities, a
resection of the distal proximal phalanx with extensive dorsal
capsulotomies is preferred. The proximal interphalangeal joint is fixed
with a Kirschner wire for 6 weeks to maintain alignment while soft
tissue healing occurs and stabilizes the digit. In the great toe, the
Jones procedure and arthrodesis of the interphalangeal joint and a
transfer of the extensor hallucis longus to the first metatarsal is
used to align the toe.
such as neurofibromatosis, hemangiomatosis, lipomatosis, and
arteriovenous fistula. It can be part of the Proteus syndrome and
Klippel-Trenaunay-Weber syndrome. Localized gigantism most frequently
involves the second and third toes and the accompanying metatarsal. The
soft tissue is enlarged with tissue of the primary disease. Magnetic
resonance imaging can be used to distinguish localized macrodystrophia
lipomatosis from other conditions causing local gigantism. In
lipomatosis there is an increase in fibrofatty tissue, bony
hypertrophy, and fatty infiltration of muscle. In neurofibromatosis
there is fibrofatty infiltration of neural fascicles.
as well as the systemic disease associated with it. The major objective
of surgery is to reduce the size of the foot to improve function and
cosmesis. For a single toe, early epiphysiodesis can be used to control
some of the growth. Epiphysiodesis is unpredictable and resection of
middle or distal phalanx is often indicated to shorten the digit.
Amputation or ray resection is indicated for severe enlargement,
multiple previous failed procedures, and in the insensate toe.
Amputation of a toe should be exercised with care in localized
gigantism as secondary deformities have been described. Amputation of
the second toe may lead to development of hallux valgus. In some cases,
partial toe amputation can help with shoe wear. Complications such as
skin necrosis, infection, and recurrence are common.
It is usually bilateral and has a high familial incidence. It commonly
involves the lateral three toes. The toe is deviated medially under the
adjacent medial toe. It is considered to be secondary to a hypoplasia
of the intrinsic muscles. Curly toe is usually asymptomatic. In the
infant, strapping has been found ineffective. Severe deformities can be
treated either by a tenotomy of the flexion digitorum longus and flexus
digitorum brevis or a Girdlestone-Taylor tendon transfer. Contracted
deformity will often require an osteotomy of the phalanx. In contrast
to congenital overlapping toe, surgery is less frequent, but still
requires special attention to the available skin.
There is dorsiflexion of the metatarsus phalangeal joint with abduction external rotation of the digit (Fig. 4.6-5).
The condition is usually bilateral and is also familial. In contrast to
congenital curly toe, this condition is symptomatic and can cause
problems with shoe wear. Early treatment requires stretching of the
medial ligaments and structures and the dorsal medial capsule. Taping
is done in the correct position. Surgery, however, is the definitive
treatment. Lengthening of the extensor tendons and dorsal and plantar
capsulotomies are often required. The skin incision must be carefully
planned as it is also contracted. Amputation is not recommended because
it results in pain and pressure on the metatarsal head.
 |
|
Figure 4.6-4 Congenital curly toe (fourth toe).
|
supernumerary digits of the foot. Postaxial (fibular) polydactyly is
transmitted as an autosomal dominant trait and may be associated with
polydactyly of the hand. It is more common in African Americans,
occurring at a rate as high as 1 in 100. Preaxial polydactyly occurs on
the tibial side and is more common among Caucasians. Morphologically,
polydactyly may present as:
 |
|
Figure 4.6-5 Congenital overlapping fifth toe.
|
-
A redundant soft tissue mass that is devoid of bone and cartilage
-
A duplication of the digit or part of the digit that articulates with a hypotrophic metatarsal or bifid metatarsal
-
A complete duplication of the digit with its own metatarsal
fitting and wearing shoes. The optimum age for surgery is 9 to 12
months, when the child is beginning to walk. Two principles are
important in performing any surgery on a multidigited foot:
-
Maintenance of the normal contour of the foot
-
Restoration of normal muscle ligament and tendon insertions. The most lateral and medial digit is usually ablated
accompanying metatarsal can be narrowed if the head is too large or
duplicated.
be removed. Polydactyly of the first ray is often accompanied by
congenital hallux varus and a bracket epiphysis. Excision of the medial
ray, lengthening of the abductor, and plication of the adductor into
the metatarsophalangeal capsule of the first ray is recommended. If
there is significant accompanying varus of the first ray,
syndactylization of the first and second toes may be necessary.
a functional problem. It is most common between the second and third
toes. It is ten times more common in whites than blacks and may be
associated with polydactyly, brachydactyly, phalangeal fusion, and
annular bands. It can be seen as an isolated anomaly or as part of a
syndrome. Surgery is rarely indicated, but when it is necessary, the
same principles and techniques for surgical separation of syndactyly of
the hand apply.
-
Zygodactyly—complete or partial webbing to the nail base
-
Synpolydactyly—syndactyly of latter two toes and polydactyly of the fifth within the syndactyly
-
Syndactyly with metatarsal fusion
syndrome, Apert syndrome, and other forms of acrocephalosyndactyly. It
is an occasional feature in chromosomal abnormalities such as Down
syndrome, trisomy 18, and Cri-du-Chat syndrome. Syndactyly is also seen
in Möbius, Silver, Cornelia de Lange, and Prader-Willi syndromes.
problem and peers often ridicule children with webbed feet. In the
foot, treatment is indicated in syndactyly associated with polydactyly
and fusion of the metatarsals. Treatment is aimed at reconstruction of
the commissure and reconstruction of the digits. The incision is never
linear and consists of a series of flaps with use of skin graft where
necessary.
due to hypertrophy of the nail folds, hypertrophy of the nail bed, and
hypertrophy of the distal pulp. Hypertrophy of the lateral nail folds
results in tissue overgrowth over the nail and occludes the nail
groove. In resistant cases, a resection of 50% of the nail and
resection of lateral nail wall usually solves the problem. In severe
cases wedge resections of the lateral nail fold can open up the nail
groove. In the infant, the nail can be so sharp that it can grow
directly into a hypertrophied distal pulp. Massaging the bulbous tip
underneath the nail is sometimes useful and its recurrence can be
prevented by the use of appropriate size shoes and socks. Some genetic
disorders with nail changes are the nail-patella syndrome
characterized by lunula, and atrophy of the nail. A dislocating
hypoplastic patella, iliac horns, hypermobility, and dislocated radial
heads also characterize this autosomal dominant condition. Darier disease
is an autosomal dominant condition with distal subungual wedge-shaped
keratosis, red and white longitudinal striations, and thinning of the
nail bed. Pachyonychia congenita is
characterized by massive hypertrophy of the nail plates with a brown
and yellowish discoloration. It is also an autosomal dominant
condition. Dyskeratosis congenita is an
Xlinked recessive or autosomal dominant condition with atrophy of the
nail plate and ridges and fusion of the proximal nail fold. Deafness, onycho-osteodystrophy, mental retardation (DOOR) syndrome is an autosomal recessive disorder with anonychia or atrophied nails.
is not uncommon. It is usually bilateral and more common in females.
When more than one metatarsal is involved, it is known as
brachymetapodia. The etiology is thought to be a premature close of the
physis. It has been found in association with Down syndrome, Albright
disease, pseudohypoparathyroidism, and multiple epiphyseal dysplasias.
The fourth metatarsal is most commonly involved. When affecting the
first metatarsal, the condition is known as metatarsus primus atavicus,
and is often associated with congenital hallux varus. Congenital
shortening of the third and fourth metatarsal usually requires no
treatment. Metatarsal lengthening is difficult, has many complications,
and is not recommended for cosmesis. Lengthening of the first
metatarsal should not exceed 36% of the original length.
is a deformity in which the central three rays are dysplastic or absent
and the phalanges of the remaining toes are deviated to the center of
the foot. The hindfoot is normal. This rare condition is usually
bilateral and inherited as an autosomal dominant trait. The gene has
been mapped to the long arm of chromosome 7. It can occur as an
isolated deformity, but more typically is associated with other
anomalies such as cleft hand, cleft lip, syndactyly, and triphalangeal
thumb. Surgery to realign the divergent toes and metatarsals and narrow
the foot is indicated to facilitate shoe wear. Abraham’s classification
is simple and his results in 32 feet in 16 patients were satisfactory.
Treatment is as follows:
-
Type 1, central partial forefoot is treated by syndactylism and partial hallux valgus correction, if needed.
-
Type 2, a complete forefoot cleft to the
tarsus requires syndactylism, and first ray osteotomy is performed
before age 5. If after age 5, first ray amputation is advised. -
Type 3, complete absence of the first through fourth ray, does not need forefoot surgery.
to be secondary to a rupture of the amnion and results in bands of
tissue that wrap around the fetus’ extremities in utero. Four types of constriction band deformities are described:
-
A simple ring around the limb or digit
-
A deeper ring often associated with abnormalities of the distal limb and lymphedema
-
Fenestrated syndactyly or acrosyndactyly
-
Intrauterine amputations
interference with circulation. If the ring is circumferential, a staged
procedure relaxing half the band at a time is preferred. The ring is
excised down to normal tissue and multiple Z-plasties are performed to
ensure adequate skin coverage. Acrosyndactyly should be treated early
because all the digits are fused at the tip and can result in
deformities if left untreated.
JT, Peterson HA. Brachymetatarsia of the first metatarsal treated by
surgical lengthening. J Pediatr Orthop 1992;12: 780-785.
TA, Ganel A, Grogan DP. Effect of proximal phalangeal epiphysiodesis in
the treatment of macrodactyly. Foot Ankle Int 1997;18;500-503.
