Slipped Capital Femoral Epiphysis
common adolescent hip disorder and is defined as displacement between
the proximal femoral epiphysis and metaphysis. The displacement occurs
through the hypertrophic zone of the proximal femoral physis. Although
we often conceptualize the epiphysis “slipping” off the femoral neck,
it is the metaphysis that is displaced anterior and proximal with
respect to the epiphysis, resulting in a varus deformity of the hip
because the acetabulum provides a mechanical constraint to prevent
displacement of the epiphysis. Treatment is primarily focused on
preventing further displacement and minimizing the risk of sequelae
such as avascular necrosis of the epiphysis and hip arthrosis.
(mechanical and endocrine) have been proposed but it is likely that the
true etiology is a combination of factors. Evidence supporting a
mechanical etiology includes the incidence of obesity, increased
physeal obliquity, and femoral retroversion seen in children with SCFE.
The result is increased shear stress across the physis. The role of the
endocrine system in the development of SCFE is linked to the male
predominance as well as the increased incidence in children with
hypothyroidism and those with hypogonadism receiving growth hormone
supplementation. Clinically, SCFE is a disease of obese adolescents who
have increased force transmission across an already widened and
possibly weakened physis associated with hormonal changes such as the
adolescent growth spurt.
and may occur any time from age 6 to the time of physeal closure. The
average age at diagnosis is 13.5 years for boys and slightly younger,
at 12 years, for girls. The majority of children are clinically obese.
There is a reported ethnic and geographic variation in prevalence. The
lowest reported incidence has been reported in Japan (0.2 per 100,000),
while one of the highest has been reported in the northeastern United
States (10 per 100,000). It has also been reported that SCFE occurs
more commonly in the summer in seasonal climates north of 40°N latitude.
cases, nearly half of which may be present at the time of initial
presentation. Involvement is usually not symmetric and a high degree of
clinical suspicion should be maintained, not only at the initial
presentation, but throughout the follow-up period. Independent risk
factors for bilateral SCFE include African American heritage and
younger age at diagnosis.
metaphyseal displacement may occur gradually over the course of several
months or as an acute event. The course may also be variable with acute
events superimposed on a gradual slippage. Progressive slipping through
the physis is halted by skeletal maturity or treatment. Despite
deformity, patients with uncomplicated SCFE have a normal acetabulum
and intact articular cartilage, and clinically perform very well for
many years. However, more severe displacement is associated with early
onset degenerative arthritis and may also result in injury to the
posterosuperior epiphyseal vessels causing avascular necrosis of the
femoral head (epiphysis).
|
TABLE 11-1 TRADITIONAL CLASSIFICATION OF SLIPPED CAPITAL FEMORAL EPIPHYSIS
|
|||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||
groin or thigh pain and a limp. The duration of symptoms is corollary
to the different categories in the traditional classification of SCFE
(see Table 11-1). Infrequently the patient
will complain only of medial knee pain (the referral pattern for the
obturator nerve) and a high index of suspicion is needed to make the
diagnosis. All pediatric patients with knee or thigh pain should
undergo hip evaluation.
|
TABLE 11-2 STABILITY CLASSIFICATION OF SLIPPED CAPITAL FEMORAL EPIPHYSIS
|
||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||
-
Externally rotated and slightly flexed hip positioning with patient supine
-
Pain with manipulation of the hip (log roll, flexion, rotation)
-
Pain with straight leg raise
-
External rotation of the thigh with passive hip flexion (asymmetric)
-
Decreased hip flexion
-
Decreased hip internal rotation
-
Decreased hip abduction
-
Limb length discrepancy
-
Antalgic gait (shortened stance phase)
-
Abductor lurch
view best displays the magnitude of the slip and the anterior position
of the metaphysis relative to the epiphysis. The radiographic
appearance of the involved hip is corollary to the different categories
in the traditional classification (see Table 11-1) and severity of disease. The radiographic findings may include:
 |
|
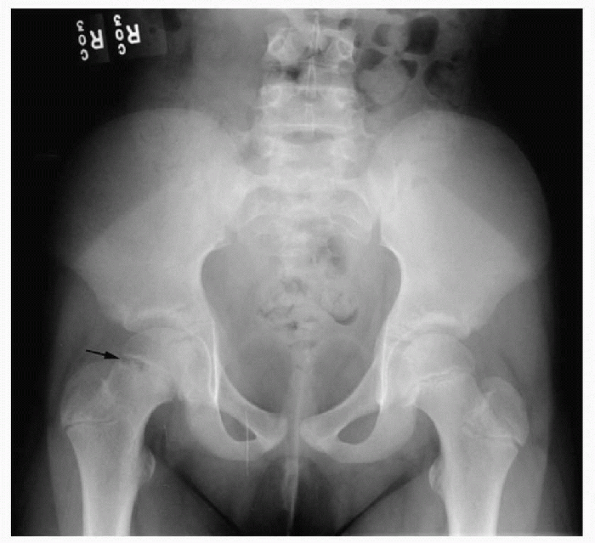
Figure 11-1 Anteroposterior pelvis radiograph showing widening of the right proximal femoral physis.
|
-
Osteopenia of the hemipelvis and proximal femur
-
Widening of the physis (Fig. 11-1)
-
Irregularity of the physis
-
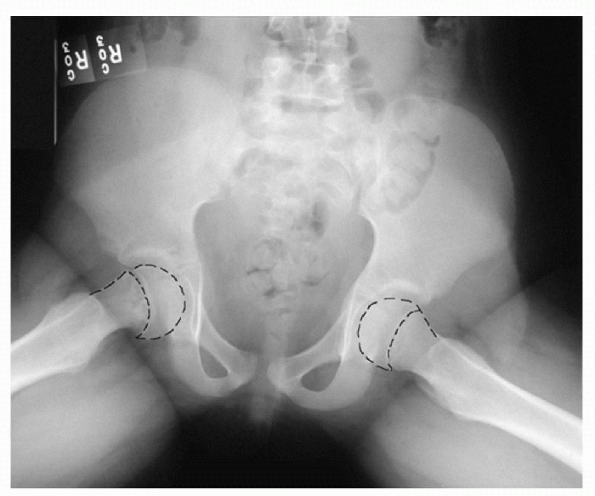
Subtle displacement of the metaphyseal/epiphyseal relationship (Fig. 11-2)
-
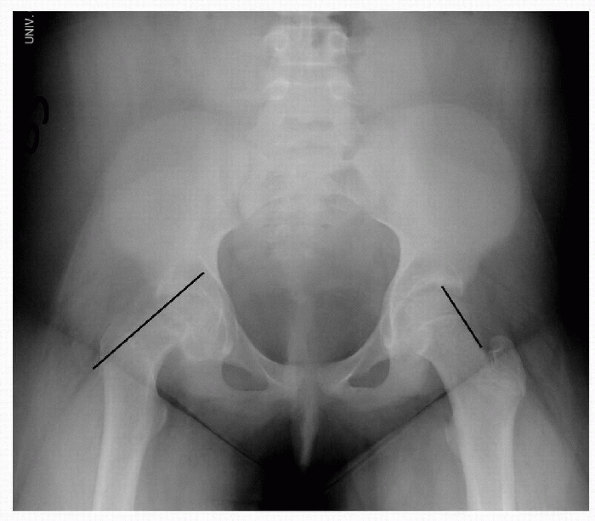
Asymmetry of Klein’s line, most pronounced on AP projection (Fig. 11-3)
-
Metaphyseal blanch sign (overlap of metaphysis on epiphysis)
-
Wide displacement of the metaphyseal/epiphyseal relationship
-
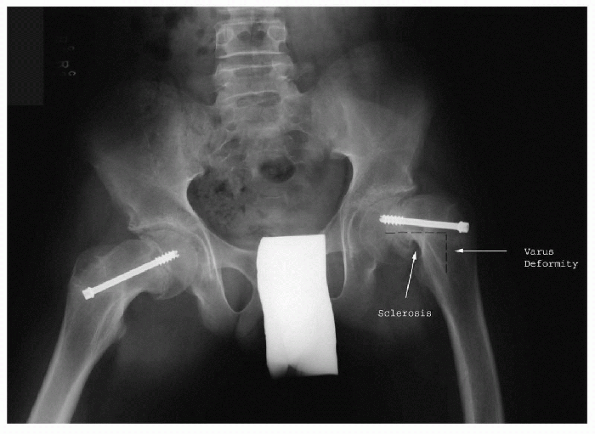
Metaphyseal remodeling (Fig. 11-4)
-
Resorption of superior and anterior proximal metaphysis (see Fig. 11-4)
-
Sclerosis of posterior and inferior proximal metaphysis (see Fig. 11-4)
-
Varus deformity (see Fig. 11-4)
 |
|
Figure 11-2 Frog-leg radiograph showing mild epiphysical displacement on the right side.
|
 |
|
Figure 11-3 Anteroposterior radiograph of a mild slip of the right femoral epiphysis and correspondingasymmetry of Klein’s line.
|
 |
|
Figure 11-4
Frog-leg radiograph of bilateral chronic slips, after pinning, demonstrating varus deformity and metaphyseal remodeling and sclerosis. |
 |
|
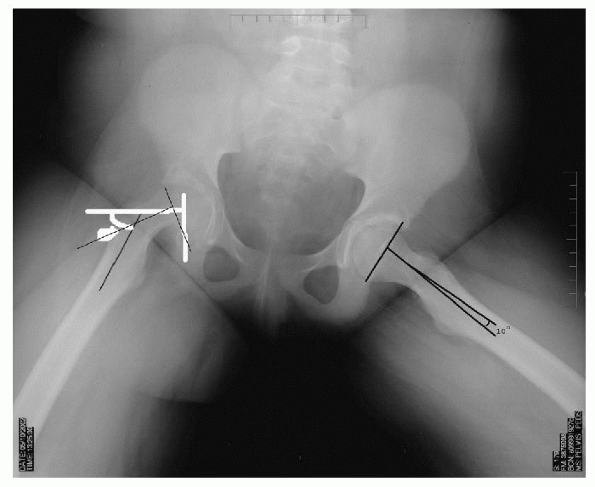
Figure 11-5 Frog-leg projection showing moderate slip of the right femoral epiphysis with corresponding increased Southwick angle.
|
-
AP view displacement of the epiphysis on the metaphysis
-
□ mild: less than one third
-
□ moderate: one third to one half
-
□ severe: greater than one half the width of the femoral neck
-
-
Frog-leg view Southwick angle (epiphyseal shaft angle) (Fig. 11-5)
-
□ mild: less than 30 degrees
-
□ moderate: 30 to 50 degrees
-
□ severe: greater than 50 degrees.
-
preslip SCFE and may aid in early diagnosis when radiographs are
normal. Ultrasound may detect hip joint effusion and metaphyseal
remodeling but is usually not needed for diagnosis. The presence of an
effusion is thought to correlate with an acute event. Magnetic
resonance imaging may be useful in the early detection of avascular
necrosis but is not useful in the diagnosis of SCFE.
|
TABLE 11-3 DIFFERENTIAL DIAGNOSIS OF SLIPPED CAPITAL FEMORAL EPIPHYSIS
|
||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||
-
Idiopathic (most common)
-
Endocrinopathy
-
□ Hypothyroidism (most common)
-
□ Hypopituitarism
-
□ Growth hormone deficiency
-
□ Hypogonadism
-
□ Craniopharyngiomas
-
-
Osteodystrophy
-
Radiation
than the fiftieth percentile for weight (negative age/weight test) can
routinely be considered to have idiopathic SCFE (Table 11-4).
Children who fall outside these boundaries (positive age/weight test)
and children less than the tenth percentile for height on a standard
Tanner growth chart are significantly more likely to have an underlying
endocrine disorder. Preliminary endocrine screening should include
thyroid-stimulating hormone and free thyroxine serum levels.
of disease, provide pain relief, have few complications, be easy for
the patient and family to tolerate, and be technically simple. The gold
standard of treatment is immediate bed rest and in situ
stabilization with single or multiple pins or screws. Postoperatively,
the patient is allowed flatfoot weightbearing with crutches. The
following section is divided into treatment options for stable and
unstable SCFE.
preventing further progression and also treating or preventing
bilateral SCFE. However, progression of slip occurs in up to 10% of
cases and spica casting has also been shown to have an unacceptable
rate of chondrolysis. Articular cartilage nutrition occurs primarily
through diffusion from the synovial fluid and this mechanism is
severely hampered by
immobilization. Treatment in a hip spica cast is not recommended and is of historical value only.
|
TABLE 11-4 ATYPICAL RESULTS IN SCREENING FOR SLIPPED CAPITAL FEMORAL EPIPHYSIS
|
||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||
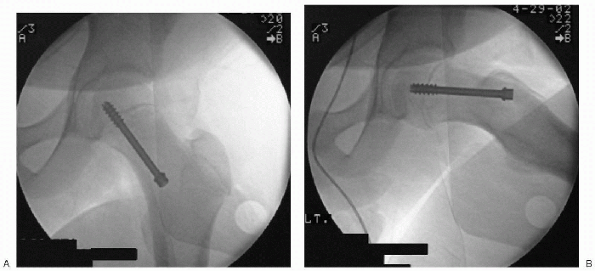
reduction can be accomplished with a single cannulated screw or pin and
is considered the gold standard. The screw or pin should enter the
anterior aspect of the proximal femur, cross the physis at 90 degrees,
and enter the center of the epiphysis with the tip below subchondral
bone. A screw placed in this orientation accommodates the deformity,
and has maximal stability with minimal risk of complications (Fig. 11-6).
Postoperatively, partial weightbearing with crutches is advanced as
tolerated. In stable slips, an additional second screw creates only a
minimal increase in stability and theoretically can negatively impact
femoral epiphyseal circulation.
 |
|
Figure 11-6 Operative anteroposterior (A) and frog-leg (B) radiographs showing single screw fixation.
|
multiple pin fixation is associated with an unacceptable rate of
avascular necrosis (AVN) and is not recommended.
the lesser trochanter and fixation with a compression hip screw can
stabilize SCFE and reduce deformity. The result is an improved range of
motion at the expense of a more involved procedure that may exacerbate
any leg length discrepancy. Osteotomy may be indicated in stable
chronic SCFE with a Southwick angle greater than 60 degrees or as a
later reconstructive option.
with an intertrochanteric osteotomy. The procedure is not routinely
performed.
outcome may be poor. Unstable SCFE may be associated with AVN despite
adequate treatment because unstable slips tend to be severe and
potentially involve injury to the posterosuperior epiphyseal vessels.
It has been argued, but not clearly proven, that early decompression of
the hip joint (aspiration or open capsulotomy), gentle reduction of
deformity, and internal fixation may decrease the incidence of AVN.
Frequently, when the patient is anesthetized, a spontaneous partial
reduction will occur. In patients with a severe slip angle there is
little epiphyseal-metaphyseal overlap and multiple screw fixation may
be impossible. Partial reduction often allows two-screw fixation and
improved rotational stability in these difficult cases.
be placed on bed rest until open or percutaneous pinning performed.
Flatfoot weightbearing may begin on the first postoperative day and
progress to weightbearing as tolerated once radiographic evidence of
early callus is seen.
collapse of the femoral head with resultant pain, stiffness, limp, and
degenerative changes. Radiographs confirm the diagnosis. Risk factors
include:
-
Unstable slip
-
Severe slip angle
-
Acute slip
-
Reduction attempt of chronic slip deformity
-
Screw placement in superolateral quadrant of the epiphysis
-
Femoral neck osteotomy
articular cartilage of unknown etiology. Patients present with pain,
stiffness, limp, and contracture. Joint space may be narrowed on
radiographs and arthrogram. Risk factors include:
-
Severe slip
-
Prolonged symptoms without treatment
-
Cast immobilization
-
Unrecognized pin/screw penetration into joint
SR, Alman B, Wright JG. short stature as a screening test for
endocrinopathy in slipped capital femoral epiphysis. J Bone Joint Surg
(Br) 2001;83B:263-268.
MB, Weinstein SL. natural history and long-term outcomes of slipped
capital femoral epiphysis. Instr Course Lect 2001;50: 571-575.
RT, Greenfield MVH. Clinical characteristics of children with atypical
and idiopathic slipped capital femoral epiphysis: description of the
age-weight test and implications for further diagnostic investigation.
J Pediatr Orthoped 2001;21:4:481-487.
T, Piehl F, Wright JG. Acute slipped capital femoral epiphysis: review
of outcomes and rates of avascular necrosis. J Bone Joint Surg (Am)
1996;78:398-402.
PJ, Sullivan CM, Phillips WA, et al. Slipped capital femoral epiphysis:
prediction of contralateral involvement. J Bone Joint Surg (Am)
1996;78:1149-1155.
