The Foot
well as localized afflictions will be analyzed. To understand
pathologic states and to institute treatment, it is first necessary to
have a firm grasp of growth and development, as well as normal
functional anatomy of the foot. The healthy foot at birth is generally
flexible and well aligned. Having said this, contractures are common,
involving all manner of deformity, but usually they resolve with
exercises, observation, or both. The longitudinal arch is generally
absent at birth but slowly and spontaneously develops (1). Commonly, there is medial deviation of the forefoot that
resolves spontaneously in over 90% of cases. Even in cases with moderate residual deformity (2, 3, 4), there is little long-term disability.
specialized footwear, including shoes and arch supports. Numerous
studies in populations that use shoes suggest that adaptations to
footwear are not generally required. Sim-Fook and Hodgson (5), and Rao and Joseph (6)
found a higher incidence of flatfoot among children who wore shoes than
those who grew up barefoot. Staheli et al. have documented the
progressive development of the longitudinal arch in healthy children as
measured by the ratio of midfoot to hindfoot width (1).
valgus or varus alignment of the leg. In a case where valgus deformity
of the knee is present, there will be increased weight bearing on the
medial side of the foot and the appearance of a flatfoot. Salenius and
Vankka (7) documented the progressive increase
in genu valgum to 4 years of age, followed by spontaneous resolution.
In addition to angular deformity, one should be aware that rotational
deformity of the femoral and tibial shaft will result in apparent foot
deformity as well, with altered push-off (8).
child, but this growth accelerates ahead of the adolescent growth
spurt. Distal epiphyses tend to close first, followed by diminished
growth through the midfoot and cessation of growth 1 to 2 years before
the growth in height ends. Metatarsal growth plates are located
proximally on the first metatarsal and distally on metatarsals 2
through 5. The tuberosity of the calcaneus grows through the calcaneal
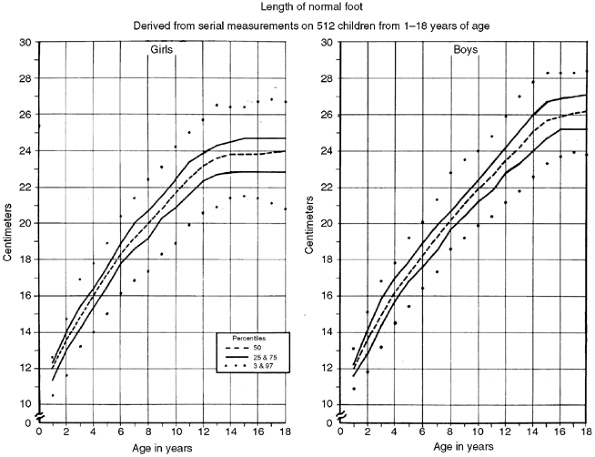
apophysis. A group led by Green (9) documented the growth of the foot with age and produced a chart as shown in Figure 30.1. Foot growth decelerates at 12 to 13 years of age in girls and 14 to 15 years of age in boys.
healthy state to comprehend and treat pathologic structural conditions.
The structure of the foot is based upon its constituent parts,
including proper alignment of seven tarsal bones, five metatarsals, and
five digits. Each tarsal bone has a defined shape with complex
articular surfaces, variable ossification pattern, centripetal growth,
and links to adjacent bones through thick ligaments. The complex
articular surfaces allow only limited gliding transplanar
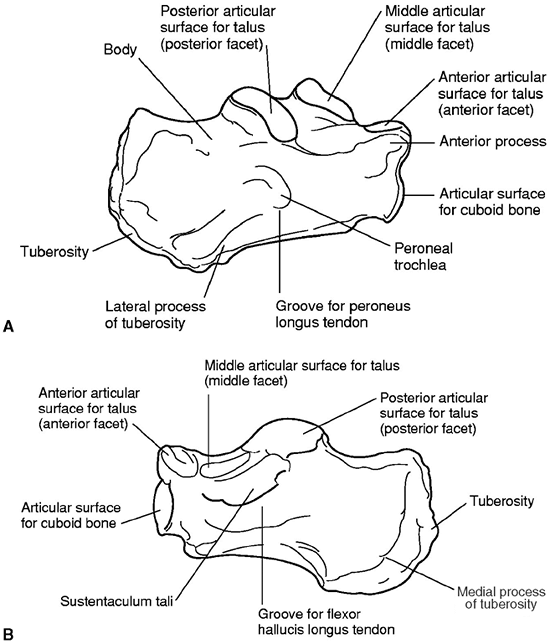
motion. An example of this is the motion of the subtalar joint. Figure 30.2
shows the dorsal surface of the calcaneus with three articular
surfaces—the posterior, middle, and anterior facets. Motion through
this complex joint is best thought of as a gliding, rotational
translation of the calcaneus under a fixed talus. Subtalar motion,
therefore, is not pure inversion or eversion of the calcaneus under the
talus. To understand the foot, rather than thinking of articular motion
about a single axis, one should consider foot motion, whether
inversion, eversion, or pronation and supination, as the sum of the
gliding motion involving multiple joints. Restriction of any joint in
the hindfoot or midfoot will result in restricted motion throughout all
structures. In a cadaver study, Wulker et al. (10)
showed the effect of selective fusion in the hindfoot and midfoot.
Motion of the subtalar joint was not significantly affected by fusion
of the calcaneocuboid joint, but reduced to 25% of its normal range by
fusion of both the talonavicular joint and calcaneocuboid joint.
Talonavicular motion was decreased by subtalar fusion but was not
affected by calcaneocuboid fusion. It was concluded that the
talonavicular joint was the key articulation for hindfoot motion.
 |
|
Figure 30.1
In 1956, a group led by Green documented the growth curves for the foot in boys and in girls. Growth of the foot tends to decelerate before the longitudinal growth of the child. (From Anderson M, Blais MM, Green WT. Lengths of the growing foot. J Bone Joint Surg Am 1956;38-A:998–1000, with permission.) |
as the joints of the foot have no intrinsic stability. Major ligaments
within the foot are the interosseous ligament, the plantar
calcaneonavicular ligament, the plantar calcaneocuboid ligament, and
the bifurcated or internal calcaneocuboid ligament (11).
The interosseous ligament is a condensation of the articular capsules
between the talus and the calcaneus, involving the posterior, middle,
and anterior facets of the subtalar joint. The plantar
calcaneonavicular ligament, or spring ligament, is a broad, thick band
connecting the anterior margin of the sustentaculum talae of the
calcaneus to the plantar surface of the navicular. This ligament
connects the calcaneus to the navicular and supports the head of the
talus. The spring ligament is reinforced by the posterior tibial tendon
on its plantar medial surface. The interosseous ligament forms the axis
of rotation of the subtalar joint, whereas the spring ligament supports
the head of the talus in stance. The calcaneocuboid and the spring
ligaments stabilize the articulation between the hindfoot and midfoot,
known as the Chopart joint. The three cuneiforms and metatarsals are
connected by a series of plantar and dorsal ligaments, which are
strong, flat bands. Metatarsals are stabilized by the intermetatarsal
ligament proximally. Distally, the metatarsals are connected by a
transverse fibrous band between the metatarsal heads, known as the transverse metatarsal ligament.
 |
|
Figure 30.2
The calcaneus has three articular surfaces that compose the subtalar joint. Motion of the calcaneus relative to the talus is a rotational translation, rather than pure inversion or eversion. A: Lateral surface. B: Medial surface. |
combination of all tarsal and metatarsal bones. The structure
distributes weight evenly across the foot in stance, allowing weight
distribution on the calcaneus, as well as across the metatarsal heads.
Little force is required in the tibialis posterior tendon to maintain
position in stance. Basmajian and Stecko (12)
demonstrated that there was almost no electromyographic activity in the
muscles of the foot and ankle when physiologic loads were applied to
the plantigrade foot in stance. They concluded that the bone-ligament
complex determines the height of the longitudinal arch, whereas muscles
maintain balance, accommodate the foot on uneven terrain, protect the
ligaments from stress, and propel the body forward. Mann and Inman (13) confirmed this theory.
ligaments, allowing only flexion and extension across joints. Each of
the joints has a proximal cylindrical surface with a concave distal
surface. Tendons inserting on the mid and distal phalanx, with
intrinsic muscles acting to flex the metatarsal phalangeal (MP) joint,
function well in the healthy state. This alignment, however, creates an
unstable position of the MP joint in dorsiflexion, once the intrinsic
muscles are unable to flex the proximal phalanx, leading to claw toes.
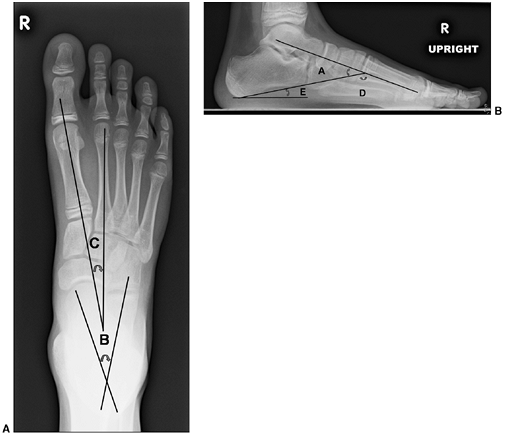
both clinically and radiographically in order to define healthy and
pathologic states. Radiographically, images are always taken in the
standing position, except in the case of infants, for whom position
should be specified. In standing anteroposterior and lateral views of
the foot, the following angles should be determined (Fig. 30.3):
-
The lateral talocalcaneal angle (A)
(lateral view) is measured as the angle subtended by the long axis of
the talus and the plantar surface of the calcaneus. Normally, it is in
the 30 to 45-degree range. It is decreased in the varus foot and
increased in the valgus foot (Fig. 30.3B). -
The anterior talocalcaneal angle (B)
(anteroposterior view) is measured as the angle subtended by the long
axis of the talus and the long axis of the calcaneus. Normally, it is
30 to 45 degrees, decreased in a varus foot and increased in a valgus
hindfoot (Fig. 30.3A). -
Meary angle (lateral view) is the
measurement of the angle subtended by the long axis of the talus and
the long axis of the first metatarsal on a standing lateral view.
Normally, these lines are colinear. In cases where the apex is directed
dorsally, a cavus foot is present. Cases where apex is angled
plantarward are valgus or flatfeet (Fig. 30.3B). -
Intermetatarsal angle (C)
(anteroposterior view) is the measurement of the angle subtended by the
long axis of the first and second metatarsal. This angle is generally
less than 5 degrees but is increased in deformities associated with
bunion formation (Fig. 30.3A). -
The longitudinal arch (D) (Hibb angle,
lateral view) is generally measured as an angle between the plantar
surface of the calcaneus and the first metatarsal. It is decreased in
cavus feet, particularly with a “calcaneus” deformity in which the
longitudinal axis of the calcaneus is increasingly vertical (Fig. 30.3B). -
Calcaneal pitch (E) (lateral view) is
measured as the angle between the horizontal and the plantar surface of
the calcaneus. It is an indicator of the position of the calcaneus in
stance and is particularly important in evaluating a cavus foot or
clubfoot (Fig. 30.3B).
-
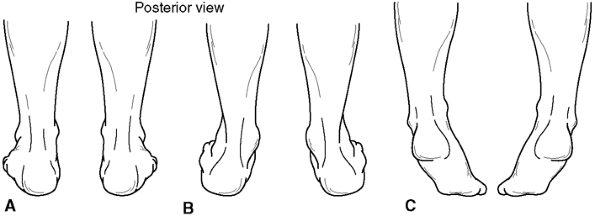
Hindfoot varus and valgus: This position
is measured in stance as the angle between the long axis of the tibia
and the long axis of the hindfoot, either in varus, valgus, or neutral (Fig. 30.4 A and B). -
Normal hindfoot mobility. This is measured by looking for the hindfoot to tip into mild varus as the patient rises on the toes (Fig. 30.4C).
-
Longitudinal arch. Observe the normal
longitudinal arch as the space under the medial side of the foot in
stance. An increase in longitudinal arch in a non-weight-bearing
position as well as when a person rises on the toes in stance is normal. -
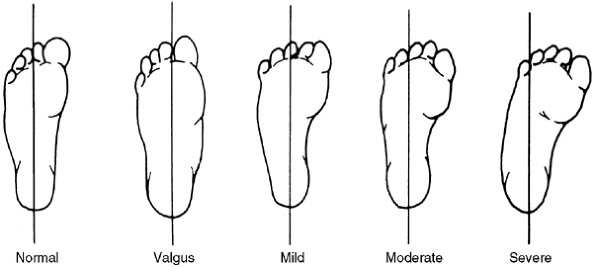
Heel bisector. The long axis of the heel should intersect the second metatarsal head in the normal state (Fig. 30.5).
-
Thigh-foot angle. With the patient in a
prone position, the long axis of the foot, defined by the center of the
heel to second metatarsal head, should be aligned with the long axis of
the thigh. Medial and lateral deviations from this should be recorded
as an angular measurement.
foot that we have defined, one must consider both the intrinsic and the
extrinsic muscles affecting this complex. The extrinsic muscles have
their origin above the ankle and include the anterior tibialis, the
posterior tibialis, the extensor hallucis longus, the extensor
digitorum communis, the flexor hallucis longus, the flexor digitorum
communis, two peroneal muscles, and the gastrocsoleus complex. The
intrinsic muscles of the foot primarily are plantar and can be divided
into four layers. The most superficial layer includes the abductor
hallucis, the flexor digitorum brevis, and the abductor digiti minimi.
The second layer is the quadratus plante and the lumbricals. The third
layer is the flexor hallucis brevis, the adductor hallucis, and the
flexor digiti minimi brevis. The fourth layer includes the interossei.
The intrinsic dorsal musculature is the extensor digitorum brevis
muscle that arises from the distal lateral calcaneus and ligaments of
adjacent joints. The balance among all of these muscles is critical for
proper function as well as avoidance of cavus deformity. The
gastrocsoleus complex acts as a powerful plantar flexor muscle. It is
opposed by the anterior tibialis
muscle
and toe extensors. The anterior tibialis muscle is, however, a
supinator of the forefoot, and unless it is counteracted by the
peroneus longus, the anterior tibialis will create a deformity with
forefoot supination and a dorsal bunion. The posterior tibialis muscle
produces hindfoot varus and medial deviation of the forefoot unless
balanced by the peroneal muscles. The complex symphony of muscle
function produces coordinated, efficient activity in the healthy state.
However, imbalance due to pathologic states results in deformity. Under
standing the static and dynamic healthy state of the foot is necessary
to approach and treat foot pathology.
 |
|
Figure 30.3 The standard radiographs of the foot are taken in the standing position, anteroposterior and lateral views. A: On the anteroposterior view (A), the intermetatarsal angle (C) between the first and second metatarsal and the talocalcaneal angle (B) can be measured. B: On the lateral view of the foot, the lateral talocalcaneal angle, the Meary angle, the Hibb angle (D), and the calcaneal pitch (E) should be determined.
|
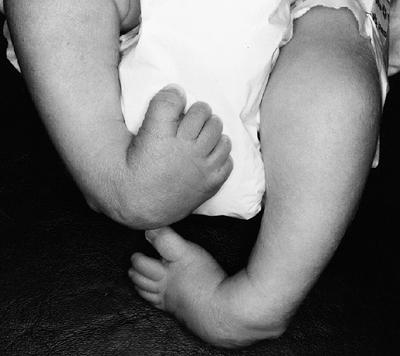
deformity characterized by equinus of the hindfoot and adduction of the
midfoot and forefoot with varus through the subtalar joint complex (Fig. 30.6). There is also a cavus deformity
through the midfoot, which accompanies most clubfeet. In identifying the pathologic tissue in a clubfoot, Irani and Sherman (14) found the talus to be uniformly abnormal, and a group led by Clarke (15)
demonstrated malformation of the calcaneus. In addition, however, those
who have looked at the tissue surrounding the bones have identified
vascular abnormalities, muscle lesions, abnormal muscle insertions, and
retracting fibrosis to be associated pathologic abnormalities in
clubfoot deformity. The pathology clearly is not limited to the osseous
structures. Clubfeet in general are “idiopathic,” occurring in
otherwise healthy children. Some are positional, with rapid correction
and requiring little by way of treatment. On the other extreme of the
spectrum of clubfeet are those associated with syndromes such as
Freeman-Sheldon syndrome and arthrogryposis, in which there is a rigid
clubfoot with fibrotic muscles and little in the way of active muscle
function. Idiopathic clubfoot bridges the spectrum between these two
conditions.
 |
|
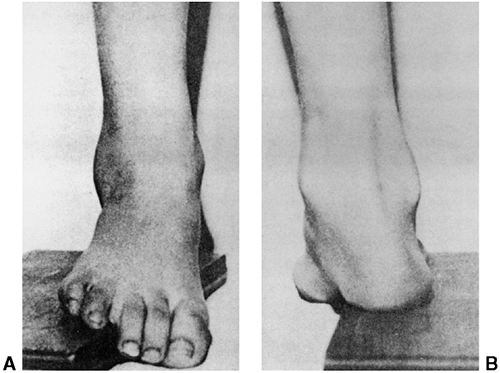
Figure 30.4 A, B:
Hindfoot position is measured as varus or valgus, on the basis of the angle subtended by the longitudinal axis of the tibia and the longitudinal axis of the hindfoot. C: With normal hindfoot mobility as the patient rises on the toes, the calcaneus tips into varus position. |
 |
|
Figure 30.5
The heel bisector method. The severity of metatarsus adductus is determined by the relation between the toes and the distal end of the line bisecting the heel. The severity does not correlate with prognosis. (From Bleck EE. Developmental orthopaedics. III. Toddlers. Dev Med Child Neurol 1982;24:533.) |
Boys are affected more than girls in all studies, varying from a
twofold increased incidence to a high of 4:1, depending on the
population studied. Bilateral involvement is present in approximately
50% of cases (17,21).
 |
|
Figure 30.6 Clubfoot deformity is associated with forefoot supination, deep medial creases, and equinovarus of the hindfoot.
|
determined that the occurrence rate was 17 times higher than in the
normal population for first-degree relatives and six times higher for
second-degree relatives. Unaffected parents with an affected son have a
2.5% chance of another child having the disorder. If the affected child
is a girl, then there is a 6.5% chance of a son having clubfoot and a
2.5% chance of a subsequent daughter being affected. Wynne-Davies
proposed dominant inheritance with reduced penetrance or multifactorial
inheritance to describe this pattern of occurrence.
also identified maternal smoking as a significant factor in etiology.
The joint effect of family history of clubfoot and maternal smoking
during pregnancy was more than additive, suggesting a
genetic-environmental interaction. Rebbeck et al. (24), using a complex mathematical model, concluded that the inheritance of clubfoot could be explained as a single-gene defect.
plantarward on the head of the talus. In severe cases, the navicular
may actually articulate with the medial malleolus. The talus is
shortened, with medial deviation of its head and deformity of the talar
neck, but the long axis is actually laterally deviated in the mortise,
as shown by Carroll and Hertzenberg (25). The
sheath of the posterior tibial tendon and the calcaneonavicular
ligament are shortened and thick, contributing to medial deformity.
Posterolaterally, the calcaneofibular ligament is also shortened and
thickened, causing medial spin of the calcaneus in clubfoot. Deep
posterior and medial skin creases are universally present in a clubfoot
(Fig. 30.7).
 |
|
Figure 30.7 Clubfoot (left) with single heel crease and healthy foot (right) with multiple heel creases.
|
Muscles in clubfoot are smaller than normal and there is an increase in
intracellular connective tissue within the gastrocsoleus and posterior
tibial muscles. A predominance of type I muscle fiber has been seen in
posterior and medial muscle groups. Electron microscopic studies have
shown loss of myofibrils and atrophic fibers, suggesting a regional
neuronal abnormality as well (25).
An electron microscopic study of medial ligaments in clubfoot
identified myofibroblasts, which could be responsible for fibroblastic
contracture in the postoperative clubfoot. Fukuhara et al. (30)
showed myofibroblastlike cells in the deltoid and spring ligaments.
Together, the thickened and shortened ligaments with contractile
fibroblasts may produce a significant component of the clubfoot
pathology. Sano et al. (31) confirmed these
findings, showing that cells of the medial ligamentous structures
contained vimentin uniformly and myofibro-blasts in some cases. More
recently, Khan et al. (32) were unable to show myofibroblastlike cells in clubfeet, and van der Sluijs and Pruys (33) demonstrated normal collagen cross-linking in clubfeet.
showed deficient dorsalis pedis flow in 45% of clubfeet compared to 8%
of normal controls. In the more severely affected feet requiring
surgery, the incidence of dorsalis pedis abnormality was 54%, whereas
those successfully treated with cast therapy had an abnormality in
dorsalis pedis flow in only 20% of cases. This data suggests that the
severity of clubfoot may in some way relate to the vascular abnormality
frequently seen in this condition.
The diagnosis is made in the newborn child based on clinical findings
of equinus of the hindfoot with some degree of varus and medial
deviation. There is little ossification in the bones of the healthy
foot of the newborn, whereas delay in ossification in the clubfoot has
been documented (38). The ossific nucleus of
the talus is not centrally located, further compromising the validity
of x-ray evaluation of clubfoot (39,40).
Ossification of the navicular does not occur until the age of 3 to 4
years in children with clubfoot and may be eccentric. Brennan et al. (41)
documented poor reproducibility of x-ray films in a child with clubfoot
because of problems with positioning, in addition to the unusual shape
of the ossification center as it develops.
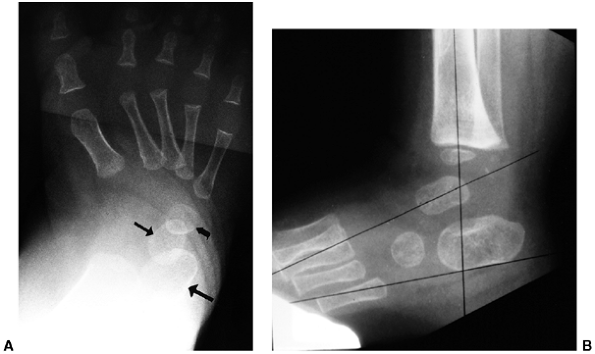
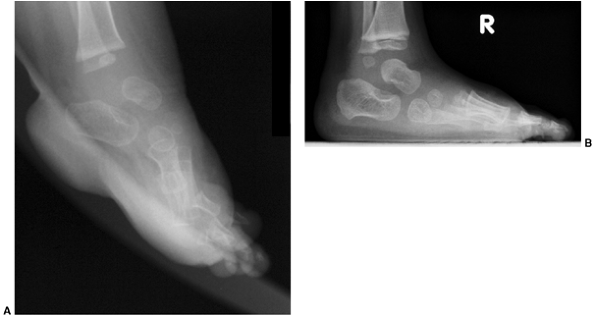
The anterioposterior view is obtained with the foot pressed against a
radiographic plate. In taking this view, the foot is dorsiflexed
maximally and held in a position of external rotation (37,45) (Fig. 30.8).
The talus to first metatarsal angle is measured on both the
anteroposterior and lateral views, with increasing angles indicating
more severe deformity. As the navicular is not ossified, there is no
direct measurement of the position of this bone relative to the long
axis of the talus (46). The axis of the talus
and the calcaneus usually converge, and the axis of the talus and the
first metatarsal form a straight line in the healthy state. The degree
of divergence from this linear alignment represents the intrinsic
deformity of the clubfoot (46). With
dorsiflexion, the long axis of the talus and the calcaneus remain
parallel, and the calcaneus remains plantar-flexed relative to the long
axis of the talus (Fig. 30.8). The alignment of the calcaneus and the cuboid is assessed on the anterioposterior view.
evaluation of the correction of clubfoot deformity. The difficulty in
the intraoperative measurement is in reproducibly holding the foot in
the right position for imaging. Intraoperative radiography remains
controversial in the management of clubfoot deformity.
tomography (CT) scan, magnetic resonance imaging (MRI), and ultrasound.
These different techniques of measurement have demonstrated
conclusively a shortened longitudinal axis with medial deviation of the
talar neck. However, the longitudinal axis of the talus is laterally
rotated within the mortise. The calcaneus is internally rotated with
decreased space between the calcaneus and the fibula posteriorly. The
navicular is dislocated plantarward and medially on the head of the
talus, as shown by ultrasound and MRI evaluation.
include looking for spinal pathology, neurologic abnormality, and any
syndrome or associated condition in which clubfeet is frequently found (Table 30.1).
Clubfoot is associated with a small calf on the ipsilateral side and a
slightly shortened tibia. A minimal tibial length discrepancy is
present at birth, but Spiegel and Loder (47) found it to be greater than
0.5 cm in 32 of 47 patients who were affected at maturity. Along with a
shortened tibia, internal tibial torsion is occasionally associated
with clubfoot deformity.
 |
|
Figure 30.8 A: Simulated weight-bearing anteroposterior radiograph of clubfoot. The talus (small straight arrow) and calcaneus (large straight arrow)
are parallel, rather than divergent. The metatarsals are markedly adducted in relation to the talus. The cuboid ossification center (curved arrow) is medially aligned on the end of the calcaneus, rather than in the normal straight alignment. B: Maximum dorsiflexion lateral radiograph of clubfoot. The talus and calcaneus are somewhat parallel to each other and plantar-flexed in relation to the tibia. |
the initial examination in all patients, as clubfoot has been found to
be associated with absent anterior compartment muscles and lesions
involving the innervation to the anterior and lateral compartment
muscles.
-
The rigidity and degree of the deformity.
-
Depth of skin creases (Fig. 30.7).
-
Tightness and contractility of muscles.
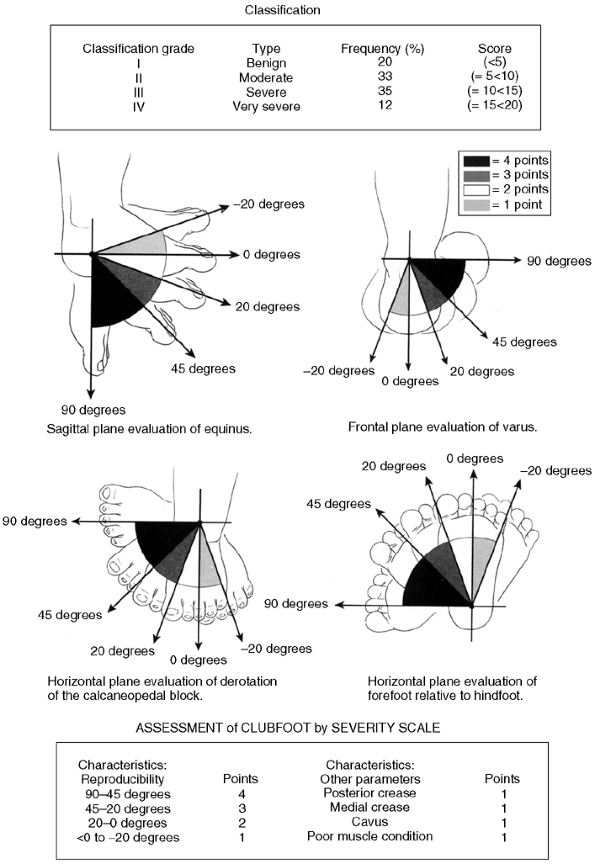
use, the author finds two of them to be of particular value in
attempting to classify clubfeet at the initiation of treatment. One of
these classification systems was defined by Dimeglio et al. (48) and the second by Pirani (49).
The classification systems apply a point score to a number of physical
findings, which when totaled leads to a “grade of involvement.” Flynn
et al. (50) have shown a good correspondence between the classification systems of Pirani and Dimeglio. Flynn and MacKenzie (50)
showed a correlation coefficient of 0.9 with the Pirani system and 0.83
with the Dimeglio system when applied by three individuals. The
correlation improved in both systems after the initial 15 feet were
scored. Wainwright et al. (51) compared four
classification systems: Dimeglio, Catteral, Harold and Walker, and
Ponseti and Smoley, determining that the Dimeglio system was the most
reproducible. Both the Dimeglio and the Pirani point systems attempt to
differentiate between mildly affected feet requiring little treatment
and those that are extremely severe. If outcome of treatment is to be
compared, a valid classification system at the onset of therapy must be
developed.
|
TABLE 30.1 SYNDROMES WITH WHICH CLUBFOOT IS COMMONLY ASSOCIATED
|
|
|---|---|
|
practice. One should create a checklist with either of the systems and
attempt to score feet at the initiation of treatment. Either of the
scoring systems can be applied in less than 5 minutes. In the Pirani
system, isolated physical findings such as space between the medial
malleolus and navicular, and space between the calcaneus and the
fibula, are identified and given scores on a 0, 0.5 or 1.0 basis. In
the Dimeglio system (Fig. 30.9), the position
of the foot deviation—whether equinus, varus, or medial—is scored based
on the degree of deformity, as well as muscle function and depth of
skin creases. The author
believes
that the isolated physical findings in the Pirani classification will
correlate directly with the gross foot position data in the Dimeglio
classification, leading to the correlation found by Flynn and others in
applying these systems. Choose one and attempt to grade clubfeet, on
the basis of these clinical criteria.
 |
|
Figure 30.9
Dimeglio’s classification system for clubfoot deformity rates the position of the foot relative to equinus, varus, foot rotation, and forefoot medial deviation. These are scored from 0 to 4 on the basis of severity. Finally, the depth of posterior crease, medial crease, cavus, and muscle condition are each assigned a 0 or 1 point score. Total score ranges from 0 to 20 points, correlating with the severity of the clubfoot deformity. (From Dimeglio A, Bonnet F, Mazeau P, et al. Orthopaedic treatment and passive motion machine: consequences for the surgical treatment of clubfoot. J Pediatr Orthop B 1996;5:173–180, with permission.) |
pregnancy, intrauterine diagnosis of clubfoot has become increasingly
frequent. This has implications, requiring the orthopaedist to be able
to provide informed consultation concerning the long-term outcome of
the deformity, as well as its proposed
treatment.
The orthopaedist must possess knowledge of the accuracy of diagnosis,
its relation to syndromes, and the treatment regimes need in order to
have an informed discussion with the prospective parents. It appears
that the earliest that a clubfoot can be diagnosed by ultrasound with
accuracy is 12 weeks of gestational age. With sequential studies, there
is an increased ability to visualize the deformity, relating either to
the progressive development of a clubfoot deformity or perhaps the
accuracy with which it can be seen. According to Keret et al. (52),
the clubfoot deformity has been detected in routine studies in
approximately 60% of cases, which is indicative of some degree of false
negative assessment. In 86% of cases, the deformity is identified by 23
weeks of gestational age, but still others are recognized up to 33
weeks. The diagnosis is made on ultrasound by the fixed position of the
foot in an equinovarus position, not deviating from this on sequential
observations (Fig. 30.10). Three-dimensional ultrasound may provide a more accurate diagnosis than standard ultrasound studies (53).
Because postnatal studies suggest an occurrence rate at birth between
0.1% and 0.6%, one can assume a rather low false negative rate. The
false-positive rate for diagnosis of clubfoot in utero using ultrasound varies from 30% to 40%, depending on series and criteria (55, 56, 57, 58). A term functional false-positive rate
has been used in cases in which a foot may have the appearance of
remaining in a plantar flexed, varus and medially deviated position but
can passively be corrected to neutral during exam just following birth.
The foot is characterized with a score of 0, 1, or 2, using the
Dimeglio classification system. Such a foot requires only
parent-administered exercise, and no long-term deformity results. With
the advancement of ultrasound and increase in experience, the accuracy
of diagnosis will steadily increase.
The combination of technologic advances and improved expertise in
obtaining and interpreting images will certainly lead to further
progress in recognizing fetal structural abnormalities. This brings one
to the question of the need for amniocentesis and karyotyping if an
isolated clubfoot deformity is found. In 1998 Shipp and Benacerraf (60) and Rijhsinghani et al. (55)
suggested that amniocentesis and karyotyping were necessary to identify
associated syndromes when clubfoot was identified. In 2000, Malone et
al. (61) showed that in 57 cases of isolated
clubfoot deformity out of 27,000 prenatal exams, there were no
unrecognized associated abnormalities. Therefore, the recommendation is
that karyotyping not be done in cases where a diagnosis of isolated
clubfoot deformity was made. This still appears controversial, and a
geneticist should be consulted about the need for amniocentesis if the
question arises.
 |
|
Figure 30.10 The clubfoot is diagnosed by ultrasound in utero when there is persistent medial deviation and equinus of the foot relative to the tibia.
|
intervention once an intrauterine diagnosis of clubfoot is made. The
orthopaedist is only involved in counseling the family and providing
treatment following birth. The author has found that this information
allows for an informed discussion with the pregnant mother and
interested father about the treatment and outcome in clubfoot
deformity. The parents can be comforted by being shown the successful
outcome after treatment of patients with this deformity. Myths about
the crippling effect of clubfoot deformity can be dispelled. Accurate
information about treatment and outcome allow the parents to make a
personal decision concerning pregnancy and allows for an improved
emotional state for the family during the delivery of their child.
significant deformity, with treatment consisting of some form of
positional correction. The most extreme of these, perhaps, used a
Thomas wrench to achieve correction. The viscoelastic properties of
ligaments and tendons were recognized by Atlee as early as 1868,
allowing for the correction of this deformity. In response to the
traumatic methods of management of clubfoot, Kite (62,63),
in 1939, presented his method of cast correction with a plea for
conservative management. In Kite’s method, the forefoot is distracted
and laterally deviated while holding the back of the heel with the
opposite hand. Pressure was placed over the calcaneocuboid joint
laterally to facilitate correction, and the cast was applied. The cast
was applied in two phases: first with a slipper holding the foot to
prevent breech through the midfoot, and second with correction of the
equinus and medial deviation deformity.
period of immobilization, often greater than 1½ to 2 years. Lovell et
al. reported results using the Kite method in 1979 with long-term
follow-up. In 47 patients with 67 affected feet, the average duration
of casting was 20.4 months, while the improvement of 43 feet was rated
to be good, 12 feet were rated fair, and 12 feet were rated poor (64,65). Because of this rather negative experience as well as increasingly popular methods of surgical management, use
of corrective cast treatment was deemphasized through the 1970s, 1980s, and 1990s.
developed and utilized a method for treatment of clubfoot using a
combination of casting, manipulation, heel cord tenotomy, and prolonged
splinting. As this method was begun as early as the 1940s, long-term
follow-up of this technique is available and the results suggest that
there should be new enthusiasm for the use of casts or conservative
management of clubfoot deformity. The basis of Ponseti’s treatment (66,67)
was the knowledge of the pathoanatomy of clubfoot deformity based on
the studies done on affected stillborn infants, as well as extensive
experience. Using weekly manipulations and casting for a period of 5 to
8 weeks, the deformity is corrected. In over 95% of cases, extensive
surgical release can be avoided in the case of idiopathic clubfoot. The
Ponseti method has recently been accepted as the standard for
conservative management of clubfoot in the United States with
increasing enthusiasm for it worldwide.
sequential manipulation and cast application. The foot can be thought
of as having three components of deformity to be corrected
sequentially: cavus, adduction, and varus equinus (2,7,68).
the first ray. One needs to address this in the initial phase of
correction. In order to correct cavus, the inner part of the forefoot
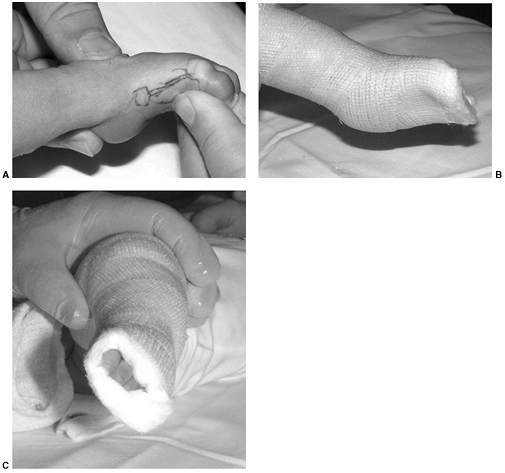
is dorsiflexed, placing the foot in a supinated position (Fig. 30.11).
Erroneously attempting to correct supination of the forefoot initially
results in actually pronating the foot and increasing the cavus
deformity. Whereas Carroll et al., and Carroll in 1988 (69,70),
stated that cavus can only be corrected by plantar fascia release and
intrinsic lengthening, Ponseti has shown the ability to alter this
deformity by his casting technique. In only 6 of
104 feet was there persistent cavus in a series reported by Laaveg and Ponseti (36) in 1980 (Fig. 30.12).
 |
|
Figure 30.11 A: At the time of initial casting of a clubfoot, the cavus deformity is treated with elevation of the first metatarsal head. B, C:
A cast is applied with the foot in equinus and the forefoot supinated with pressure under the first metatarsal head and counterpressure over the head of the talus laterally. |
with counterpressure applied laterally over the head of the talus.
Pressure is placed under the first metatarsal head.
The lateral shift of the navicular and cuboid occurs as the tight joint
capsule and ligaments yield to the pressure of manipulation (65).
Several minutes of manipulation are required at each cast change to
slowly stretch ligaments prior to cast application. A series of casts
is applied on a weekly basis for the next 4 to 6 weeks to achieve
midfoot (primarily talonavicular) correction. Simultaneously with the
correction of the talonavicular joint, the calcaneus rotates under the
talus, and the posterior aspect of the calcaneus moves away from the
fibula with stretching of the calcaneofibular ligament. Care needs to
be taken not to pronate the foot in this process and to maintain the
forefoot in neutral position with respect to pronation and supination.
The equinus is the last component corrected once the forefoot and
midfoot are aligned.
under the talus relative to the axis of the leg. The external rotation
and abduction of the foot is steadily increased up to 70 degrees in the
last cast. This is a very different position from the one generally
used in traditional methods of clubfoot casting. Clearly, the only way
that this position can be achieved is with a long leg cast. There is no role for short leg casts in the correction of clubfoot deformity.
forefoot deformity is addressed and completely resolved. The mechanism
of correction is a combination of upward pressure under the entire foot
while pulling down on the heel with the other hand. One needs to
achieve 15 degrees of dorsiflexion while holding the foot in 70 degrees
of external rotation/abduction. In nearly all cases, a percutaneous
tenotomy of the Achilles tendon is required to achieve this position
without midfoot breech. Following a tenotomy, the foot can be
dorsiflexed to a position well above neutral without midfoot breech.
The heel cord reconstitutes rapidly following its lengthening, as has
been documented both by clinical experience as well as by observation
at the time of revision surgery. The final cast following tenotomy is
left in place for 2 weeks. In this cast, the foot is held in a position
of 15 degrees of dorsiflexion with 70 degrees of external rotation of
the foot relative to the leg. After removal of the final cast, a
Dennis-Brown bar is applied. The Dennis-Brown bar is positioned with
the feet in slight dorsiflexion created by a bend in the mid-part of
the bar, and 70 degrees of abduction or external rotation of the shoes.
Padding over the heel in the shoe can help in providing relief for the
calcaneus so that blistering does not occur, and this padding will also
prevent the foot from rising out of the shoe. Dorsiflexion cannot be
achieved adequately without splinting the foot in a position of severe
external rotation and abduction. The author also supplements the
treatment at this point with physical therapy to stimulate firing of
the peroneal and anterior tibial muscles, and to maintain the range of
motion of the foot.
by night splinting. The night splinting is used until at least 18
months of age. Recurrences can be dealt with by return to corrective
casting in select cases. Surgical therapy may be required in some cases
with failure of this method of management. Ponseti (65) believes that in the absence of a good splinting program, a recurrence rate of 70% may occur. In
such cases, it may be difficult to reinstitute this method of management, and surgical therapy may be required.
 |
|
Figure 30.12 A: This patient had severe cavus deformity as a component of his clubfoot deformity. B:
Following Ponseti management, x-ray films indicate resolution of his cavus deformity with sequential casting and no plantar release. |
acceptance of the need for night splinting and “buying into” this
method of management is critical. With the proper approach and
coaching, and support from the nursing and physical therapy staff as
well as from the treating orthopaedic surgeon, acceptance of this
treatment by the parents and child can be achieved.
clubfoot correction, advocates of semirigid fiberglass have had good
success with this alternative material. Coss and Hennrikus (71)
have shown that semirigid fiberglass is superior to plaster of paris in
durability, convenience, performance, and ease of removal. Parents can
remove semirigid casts without soaking. Molding of the cast is a bit
more difficult with fiberglass than with plaster of paris.
reviewed 45 patients, ranging in age from 25 to 42 years, with 71
clubfeet. Thirty of the patients had tibialis anterior transfers, of
which 25 were rated at 5/5 strength. In the remaining 5 patients, the
strength of the transfer was rated as 4+/5 Only 2 patients in the
entire group had osteoarthritic changes. While the degree of
dorsiflexion, inversion, and eversion were less in the patient with
clubfoot than in the healthy individual, plantar flexion was normal.
Improvement in 62% of clubfeet was excellent, with 16% good, and 22%
poor. Fifty-four percent of the patients participated in sports,
compared to 40% of age-matched controls. Twenty-six percent of patients
could walk unlimited distances. There was a distinct lack of
correlation between radiographs and clinical outcome. Significantly,
the lateral talocalcaneal angle was not a predictor of normal function.
Following the recognition of the results achieved by Ponseti, a number
of individuals have tried to reproduce his results. Hertzenberg et al. (73)
in 2002 compared a group of 27 patients treated with the Ponseti method
to 27 patients treated with traditional casting techniques. One of the
patients in the Ponseti group required posteromedial release, whereas
91% of patients in Hertzenberg’s control group required surgical
therapy. Foot abduction splinting with a Dennis-Brown bar was crucial
to the success of this method of treatment, just as Ponseti had shown.
A percutaneous heel cord lengthening was done in 31 of 34 patients in
Hertzenberg’s series.
their experience with the Ponseti method of management with similar
results. Ninety-two percent of patients had initial success within the
first year of life after using the Ponseti method. Hattori et al. (75)
showed the positive effect of the Dennis-Brown bar in the postcasting
management of clubfoot, particularly if applied in the first months of
life. In evaluating the positive effects of the Ponseti method, Kuhns
et al. (76) used ultrasound to document the
progressive movement of the navicular around the head of the talus as
treatment continued. Pirani et al. (77) has similarly documented the successful correlation of correction of the chondroosseous defects in clubfoot using ultrasound.
positive, similar to that of Lehman and Hertzenberg. The combination of
corrective casting through the specific methods of management of
Ponseti has resulted in excellent reduction of the midfoot deformity,
specifically the talonavicular joint. A midfoot breech is prevented by
liberal use of heel cord lengthening at the time of dorsiflexion. The
necessity of postoperative splinting using a Dennis-Brown bar cannot be
overstated. Much effort must be used in convincing parents of affected
children that the value of splinting far outweighs the inconvenience
endured. As some patients have recurrent deformity postcasting,
splinting must be augmented by return to casting as well as physical
therapy. With long-term follow-up, one can expect some recurrence of
deformity or relapse. Dobbs and Ponseti (78) have documented relapse in
an 8-year-old child who was previously fully corrected. Long-term
follow-up is mandatory in clubfeet managed by the Ponseti method, just
as in any other technique.
This is a dynamic method of management, utilizing exercise for
correction with supplementation by taping and continuous passive motion
(CPM) in some cases.
tight medial structures, including the posterior tibial tendon and
plantar soft tissue. An attempt is also made to strengthen the peroneal
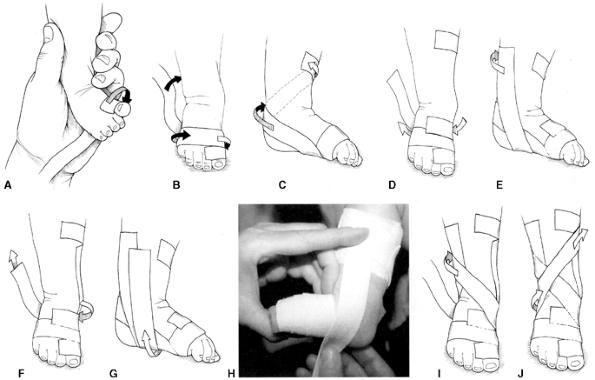
muscles by stimulation. Adhesive taping (Fig. 30.13)
is applied to supplement the exercise and maintain correction that is
gained by stretching. Daily treatments are continued for 2 months. The
treatment frequency in this program is then decreased to 3 sessions per
week until 6 months of age. After that time, the child is continued on
a physical therapy program, and night splinting is used for 2 to 3
years.
of a CPM machine at night was advised, and this resulted in fewer
patients requiring surgical treatment for residual clubfoot deformity.
The CPM machine may be valuable in the first 12 weeks of life,
according to Dimeglio. Using this technique, Bensahel et al. (80)
achieved good results in 48% of 338 patients, as reported in 1990. With
resorting to surgery to complete the treatment in half of the patients,
an overall success rate of 86% in the good and excellent category was
achieved. Dimeglio et al. (42) reported that
74% of patients were successfully treated with exercise and CPM,
without the need for surgical therapy. In 2001, a group led by Richards
and Johnson (83) from the Scottish Rite
Hospital in Texas reported their initial results with this technique.
In their treatment of the first 30 clubfeet, 54% required some surgery
with 18% having a limited posterior release and 28% needing a
traditional posterior medial clubfoot release. Just as Dimeglio saw
improvement with CPM, these investigators found a small, incremental
advantage to the use of CPM at
night.
In the French method, effort is concentrated on gentle stretching of
plantar and medial structures, as well as taping to hold the foot but
allow motion, rather than the rigid nature of clubfoot casting.
Recognizing that peroneal weakness is a significant problem in clubfoot
deformity, effort is made to maintain mobility and strengthening,
rather than immobilization. The author does not have personal
experience with this technique, beyond taping and a gentle exercise
program in mild clubfeet but believes that the results speak for
themselves, and satisfactory outcome can certainly be achieved with
this technique. Dimeglio and Bensahel have clearly documented the value
of this method of management. One disadvantage in the functional
(French) method of management of clubfoot is the added personal input
with physical therapy and taping that is required. Where a cast remains
in place for 1 week following manipulation and application, taping and
exercise tend to require more maintenance and continuous care. The cost
of application of this method is significant, both in dollars expended
and interference with parental work and family functioning. These
issues need to be considered while making a choice of therapy for
clubfoot.
 |
|
Figure 30.13
Taping is used to maintain the passive range of motion achieved during manipulation sessions when clubfeet are managed by the French method. As the tape is applied sequentially in Steps A to J as pictured, the foot can be derotated with correction of the forefoot, midfoot, and hindfoot deformity, including equinus. (From Noonan KJ, Richards BS. Nonsurgical management of idiopathic clubfoot. J Am Acad Orthop Surg 2003;11:392–402, with permission.) |
applying the “functional treatment of clubfoot,” found that 75% of feet
treated in this manner required surgical therapy. A coauthor, Fabry,
felt that there was greater benefit to the treatment of clubfoot with
exercise in the Dimeglio grade 1 and 2 feet, than in the mild and
moderate foot. With a Dimeglio score less than 10, he found consistent
success, whereas in higher grades, surgical treatment was required.
management with physical therapy of clubfoot, one might logically
wonder whether there is still a role for the management of clubfoot
with surgery. Clearly, less extensive clubfoot surgery and fewer
clubfoot surgeries, in absolute numbers, are done now because of
improved conservative methods of clubfoot management as described. In
more severe clubfeet, Dimeglio grades 3 and 4, and in the syndromic or
neuropathic clubfoot, surgical treatment remains necessary in a number
of cases. Fabray achieved success with the physical therapy method of
clubfoot management in only 25% of cases. As documented in a paper by
Cohen-Sobel et al. (85), the long-term
follow-up of clubfeet treated surgically is consistent with an
excellent level of function in most cases despite some anatomical and
radiologic imperfections. Gait studies have documented a weakness in
push-off in general, but reasonable function in most series treated
surgically. The negative results of surgical therapy are due to
persistent deformity, weakness, stiffness, and pain.
deformity, one must look at the indications, timing of procedure,
technique, and postoperative management. The results of the various
procedures should be compared, allowing the surgeon to make an educated
choice of what procedure to use for primary clubfoot release, as there
are a number of procedures with some variation in joints released,
tendons lengthened or transferred, and bones osteotomized.
is failure to correct the deformity by conservative methods within the
first year of life. The author would attempt the Ponseti method in a
child up to 1 year of age with a foot not previously treated or not
optimally treated, as there has been a high rate of success with this
technique, even in older patients. However, in the case of the foot
that has failed to respond to cast correction with good application of
cast technique or exercise, surgical management is certainly indicated.
perform surgery when the child is between 4 and 9 months of age.
Prolonged casting, once a decision that surgical therapy is necessary,
is generally not indicated. The neonatal surgery recommended by Ryoppy
and Sairanen (86) and Pous and Dimeglio (87)
has not met with general enthusiasm and is not consistent with the
general understanding of clubfoot deformity, in which an effort is made
to avoid surgery, recognizing the amount of scarring that relates to
the contractile fibrosis on the medial side of the foot in early
infancy. Ponseti has documented the high cellular nature of medial
ligaments in the infant clubfoot, and Zimny and others (2)
have documented the presence of myofibroblasts that might well be
stimulated by early surgery, leading to a more rigid foot and
unsatisfactory outcome.
recommended the first comprehensive, single-stage surgical therapy for
clubfoot. The emphasis in this procedure was on the correction of the
medial subtalar joint and ankle joint; medial release of the
talonavicular joint was done as well. The deformity at the
posterolateral corner of the foot or calcaneofibular ligament was not
addressed in this procedure. Whereas many feet achieved satisfactory
correction with this technique, one of the major complications that
occurred was hindfoot lateral translation with persistent medial spin
of the foot and valgus hindfoot. Hudson and Catterall (43)
published a paper suggesting that the release of the tissue at the
posterolateral corner or calcaneofibular ligament along with posterior
release could be done without need for extensive medial release,
yielding satisfactory results in clubfoot surgery. Their method,
although not subjected to a common grading system as is true of most
clubfoot surgery, resulted in satisfactory outcome in a vast majority
of cases. Through the 1980s and 1990s, a number of surgical procedures
for correction of clubfoot were recommended, with strong advocates for
each technique. Such surgical procedures were attributed to Simons (90), McKay (91,92), Goldner and Fitch (93), and Carroll (70).
This article will attempt to briefly describe each of these procedures
and identify how each one is unique. When the procedures are actually
compared and commonality is searched for, one finds that there is much
in common in these procedures, yet each has a distinctive feature with
which an individual’s name has been and continues to be associated.
a posterior ankle release is done without opening the subtalar joint.
The extension of the release medially through the deltoid is
significant, focusing on the deltoid as a major pathologic structure
responsible for medial deviation of the talus. Correction involves
lengthening of the deltoid with extensive medial release and
reconstruction of the talonavicular joint medially and laterally,
avoiding the subtalar joint.
His procedure is based upon a concept of achieving proper rotation of
the calcaneus under the talus. The interosseous ligament remains
intact, but a limited release of the subtalar joint as well as ankle
joint, concentrating on the posterolateral corner, is performed. The
plantar fascia is always released as well as intrinsic toe flexors, and
the calcaneocuboid joint is addressed to achieve satisfactory alignment
of the lateral column.
espoused the concept of correction of clubfoot deformity by complete
subtalar release dividing the interosseous ligament. The application of
this extensive procedure has resulted, even in Simons’ own series, in
significant overcorrection in some feet. Most surgeons and authors have
cautioned against division of the interosseous ligament because of
overcorrection and severe deformity because of this procedure. Simons (97)
also described the concept of correction of the calcaneocuboid joint in
clubfoot; this has resulted in recognition of the contribution of
lateral column deformity to the overall unsatisfactory surgical results
in clubfoot correction.
incision around the posterior aspect of the foot several millimeters
above the posterior crease, to a two-incision Carroll approach (70)
with a posterolateral incision and a zigzag medial incision. In cases
in which the wound cannot be closed following clubfoot correction
(Cincinnati), researchers have found that the wound can be left open,
and it closes spontaneously during a period of healing without
negatively affecting outcome (99).
syndromic and severe clubfoot deformity based on Dimeglio
classification. The accepted procedure for clubfoot surgery at this
time might be described as the “a la carte” procedure (44).
In this procedure, pathologic structures leading to deformity are
released in order to properly align the foot. Common features in an “a
la carte” release are heel cord lengthening and posterior release of
the ankle and subtalar joint with extension to the calcaneofibular
ligament. The medial release is a judicious one, with lengthening of
the posterior tibial tendon as needed. In doing the midfoot release,
attention is paid both to the medial and lateral columns to ensure that
the long axis of the talus is properly aligned with the first ray and
the long axis of the calcaneus
is
properly aligned with the fourth and fifth ray. The interosseous
ligament is always left intact. In cases where the heel cord can be
lengthened in a fractional rather than a Z technique, this is done.
Supramalleolar lengthenings of the flexor hallucis longus and flexor
digitorum longus tendons are preferable, if they can be done. Cavus
deformity is corrected with a plantar fascia release if needed.
Finally, the tendons are generally repaired tight to avoid
postoperative weakness. The author prefers repairing the heel cord with
the proximal tendon at half-tension with the foot at neutral.
to casting for a period of time until healing has occurred and
exercises begun. Kirschner-wire (K-wire) stabilization of the foot with
one or two wires following surgery has been generally advocated.
Generally, wire stabilization of the talonavicular joint is done to
prevent talonavicular subluxation. The residual deformity or increasing
postoperative deformity from subluxation of the navicular is severe and
has prompted most surgeons to stabilize the talonavicular joint
following release. A second wire may be placed through the subtalar
joint to prevent lateral translation of the calcaneus, particularly if
the interosseous ligament is divided. Finally a wire may be placed
across the calcaneocuboid joint in cases where marked deformity of the
lateral column is documented and surgical correction required.
little over recent years. Cast immobilization is universal, in
recognition of the need for holding the foot in a corrected position to
allow for ligament and tendon healing as well as bone remodeling.
Attempts to stimulate early motion (91,92)
have not been widely utilized. Postoperative casting is generally done
for 2 to 3 months, followed by a prolonged period of observation,
physical therapy, and postoperative splinting. Generally, special shoes
are not required, but the use of arch supports or simple shoe
modifications may be of benefit in selected cases.
procedures as described in the preceding text, the results in most
reports document 60% to 80% good or excellent results (43,89,90,92,94,95),
with improvement of residual deformity in a number of cases and failure
in approximately 10%. This general distribution of outcome is
reflective of much in the surgical literature. Researchers who have
studied patients with clubfoot deformity, however, find consistent
abnormalities in all feet that have been corrected surgically. The most
prominent of these abnormalities is weakness in the gastrocsoleus and
difficulty with push-off (100). Others have
found some element of foot drop and a tendency to externally rotate
from the hip to compensate for some of the persistent internal rotation
deformity of the foot (101). Despite these
weaknesses, function is generally good and compatible with normal shoe
wear and full activity. There are, however, a group of residual
deformities that are consistent across all methods of management, and
this article will consider each of these.
seen because a clubfoot, with its diffuse spectrum of pathology, is not
rendered healthy by a single operation. The individual problems are not
seen in isolation but in combination. It will, however, be beneficial
to consider each of these deformities or problems separately in order
to understand the diagnosis and management of postoperative clubfoot
deformity.
The inadequate release of the calcaneofibular ligament or the posterior
lateral corner is probably one of the most common causes of valgus
hindfoot. As the foot is dorsiflexed, the posterior lateral tether
draws the calcaneus laterally toward the fibula. As Ponseti (65)
has shown, this ligament is shortened and thickened in the clubfoot in
the absence of treatment. Although it may seem counterintuitive that a
release at the posterior lateral corner will prevent hindfoot valgus, a
surgeon can prove it to him- or herself by doing sequential ligament
release at the time of surgery. Catterall (43) has demonstrated the importance of posterior lateral release.
 |
|
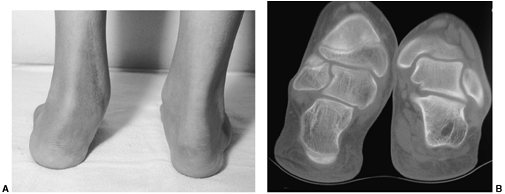
Figure 30.14 A: Valgus deformity of the hindfoot is a complication of clubfoot management resulting in weak push-off and pain. B: Computed tomography (CT) scan is used to evaluate the deformity and the subtalar joint.
|
instability, in which division of the interosseous ligament as well as
release of the subtalar joint may result in lateral translation of the
calcaneus under the talus, as shown by Simons (90).
Although complete subtalar release has been recommended by some,
overcorrection of the hindfoot into a valgus position is one of the
complications that can result from this procedure.
produce hindfoot valgus, in that as a patient bears weight, the
forefoot will rotate into a position in which it is flat on the ground,
forcing the hindfoot into valgus. Therefore, a rigid forefoot and
midfoot malalignment may contribute to hindfoot valgus. Posterior
tibial insufficiency may also lead to valgus hindfoot over time.
that it produces a poor mechanical situation in which the gastrocsoleus
complex is compromised. With the insertion of the gastrocsoleus
displaced laterally relative to the axis of rotation of the ankle
joint, push-off is diminished and a deforming moment is applied to the
hindfoot with activity. This leads to both poor push-off and pain.
Lateral impingement between the calcaneus and fibula may also result
from lateral displacement of the calcaneus. With time, progressive
lateralization of the hindfoot associated with midfoot collapse will
lead to an unsatisfactory result.
for rigid forefoot supination that may drive the hindfoot deformity.
Also evaluate the muscle strength in all groups, including the
posterior tibial muscles. With the patient rising on the toes, look for
evidence of subtalar motion, with normal mechanics representing a
slight tip of the hindfoot into varus with plantar flexion. Standing
anteroposterior and lateral radiographs of the foot underestimate the
deformity of hindfoot valgus in general. A CT scan will allow
evaluation of the subtalar joint as well as the alignment of the
hindfoot deformity. Also, be aware that valgus may result from the
tilting of the distal tibial articular surface.
includes both conservative and surgical measures. An arch support or
University of California Berkeley (UCB) insert may improve hindfoot
position to a point where symptoms are relieved and progressive
deformity does not occur. Physical therapy to strengthen the posterior
tibial muscle may be of value. Mild hindfoot valgus may follow
operative management, but also may be a complication of conservative or
cast treatment for clubfoot.
calcaneal translational osteotomy as well as calcaneal lengthening, and
finally, subtalar arthrodesis. In severe cases, triple arthrodesis may
be necessary. In a calcaneal slide osteotomy, the tuberosity of the
calcaneus is shifted medially, generally from the lateral approach,
with the calcaneal osteotomy just posterior to the posterior facet of
the subtalar joint. In order for the procedure to work, a competent
subtalar joint must be present and is best evaluated using a CT scan (Fig. 30.14B).
The axis of alignment of the foot in weight-bearing may be corrected
with a translational osteotomy, and the pull of the gastrocsoleus
complex may be shifted into proper alignment with the tibial talar
joint. The calcaneal slide osteotomy will not affect the midfoot and
forefoot deformity. It also will not affect the longitudinal arch of
the foot nor the talonavicular relation.
In this procedure, the hindfoot is corrected by distraction of the
calcaneus with a secondary improvement in the talocalcaneal as well as
the talonavicular alignment. The negative effect of calcaneal
lengthening on the foot is forefoot supination, which is a frequent
pathologic state in clubfoot deformity. An intact peroneus longus
muscle may decrease forefoot supination, but one should be aware that
with the calcaneal lengthening osteotomy forefoot supination may be
increased. In cases where significant supination is the result of
calcaneal lengthening, a plantar flexion osteotomy done through the
first and second cuneiform will restore medial column sagittal plane
alignment. The goal of this procedure is to restore proper foot
balance, with the healthy tripod sharing weight bearing between the
first and fifth metatarsal and the tuberosity of the calcaneus. A
preoperative requirement for calcaneal lengthening osteotomy in the
postoperative clubfoot is flexibility of the foot such that the
lengthening osteotomy will produce the desired midfoot effect. In a
rigid clubfoot deformity, translational osteotomy may be of more
benefit.
incompetent subtalar joint as judged by CT scan, subtalar arthrodesis
can be considered. In such a case, the correction of the valgus
malalignment of the hindfoot will require an iliac crest graft in order
to improve the weight-bearing axis through the subtalar joint. Internal
fixation with either screw or staple is required as well. In cases
where the distal articular surface of the tibia is the cause of valgus
deformity, an appropriately timed medial epiphyseodesis may correct the
problem (103,104).
the forefoot, lateral weight bearing in stance, and persistent medial
rotation of the foot. Functionally, the patients tend to push off over
the lateral border of the foot without normal weight-bearing and have
foot pain with recurrent ankle sprains. In general, this is a
persistent foot position that relates to undercorrection of the
clubfoot. Mechanically, it may be better in push-off strength than a
persistent valgus foot deformity. Persistent hindfoot varus deformity
may result from undercorrection after surgical or casting treatment of
clubfoot deformity. A Coleman block
test (Fig. 30.15)
may be used to demonstrate the degree of flexibility of the hindfoot.
In the block test that is commonly used for cavus foot deformity,
hindfoot varus secondary to medial column plantar flexion can be
differentiated from a rigid hindfoot deformity. In the clubfoot, the
rigid hindfoot deformity is generally, but not always, present.
Remember that forefoot pronation or plantar flexion of the first ray
may contribute to hindfoot varus and must be identified by physical
examination in order to properly manage this condition. By motor
testing, one should evaluate the strength or competence of the
peroneals, as well as the strength of all muscle groups within the foot.
 |
|
Figure 30.15
The Coleman block test for determination of hindfoot flexibility. The flexible varus deformity of the hindfoot will correct to valgus when the plantar-flexed first metatarsal is allowed to drop down off the edge of the block of wood. Failure to correct to valgus indicates the need for surgical correction of the hindfoot, in addition to the procedures on the forefoot. (From Coleman SS, Chesnut WJ. A simple test for hindfoot flexibility in the cavovarus foot. Clin Orthop 1977;123:60–62, with permission.) |
upon its cause and the extent of the associated foot deformity. In the
young child with undercorrection of the entire clubfoot after surgical
release, a revision surgery addressing forefoot medial deviation,
cavus, and hindfoot varus may be required. In the older child with
persistent hindfoot varus, a calcaneal osteotomy as a combination of
lateral closing wedge and translation is generally the treatment of
choice.
years of age, with secondary deformity of the bones, may require
osteotomy in addition to capsular release in order to achieve
correction. Use of lateral column wedge osteotomy for shortening,
either through the cuboid or calcaneus should be considered in order to
achieve satisfactory alignment. Calcaneocuboid fusion, as described by
Evans (105), has been used in selected cases in
achieving lateral column alignment. Loss of calcanecuboid motion
produces little effect on subtalar motion (10).
as a combination of sliding of the tuberosity as well as lateral
closing wedge. If the entire deformity is corrected by lateral closing
wedge of the calcaneus, the heel height is significantly decreased,
making shoe fitting with impingement on the lateral malleolus more
difficult. The combination osteotomy using lateral shift as well as
closing wedge gives a better functional result. Stabilization of the
osteotomy is done with screw or threaded K-wire fixation.
This may result from overlengthening of the heel cord and mimic the
foot deformities seen in poliomyelitis and other neurologic conditions.
The moment arm for pull of the gastrocsoleus is decreased, further
compromising push-off that is at first weakened simply by the
overlengthening of the heel cord. Coleman (106) has described an osteotomy of the calcaneus in which the tuberosity is translated posteriorly. The
combined effect of this osteotomy is to decrease the calcaneal pitch
while increasing the moment arm for pull of the gastrocsoleus complex.
Clinically, patients with foot pain and weak push-off may be improved
by this operation. The author has no data on the increased strength of
the gastrocsoleus that is associated with such an osteotomy, but it
does decrease the elevation of the longitudinal arch and does relieve
some of the symptoms associated with the short cavus foot.
 |
|
Figure 30.16 A:
A weak gastrocsoleus complex may result in a “calcaneus” deformity in which the calcaneal pitch is significantly increased and the mechanical advantage of the gastrocsoleus complex significantly decreased. B, C: A calcaneal lengthening osteotomy improves foot alignment and lengthens the gastroc moment arm. |
medial displacement of the navicular on the head of the talus, it is
clear that this deformity represents a postsurgical complication. Kuo
and Jansen (107) have described this navicular
displacement as having an occurrence rate of about 8% in their series
regardless of the type of incision used. The actual deformity is one of
rotation of the navicular on the head of the talus, mimicking dorsal
and lateral translation of the navicular. Once the navicular is
displaced, its shape becomes altered from a bean-shaped bone with a
concave articular surface opposing the talar head to a wedge-shaped
bone that is nearly impossible to replace in its anatomic location and
maintain alignment. Recurrent deformity following attempted reduction
of the talonavicular joint therefore has been somewhat distressing. A
group led by Davidson (108) has recommended
talonavicular fusion as a definitive procedure to treat severe cases of
talonavicular subluxation requiring surgery. While this decreases
midfoot and hindfoot mobility, the trade-off for improvement in
alignment is at times necessary.
compatible with a quite reasonable outcome. The foot tends to be short
with a relatively short plantar flexed medial column compared to the
lateral. Asymptomatic talonavicular subluxation should be managed with
observation and adaptive footwear as needed. The midfoot tends to be a
bit elevated and the foot a bit wider through the midfoot. At times,
arch supports or cushioning of the shoe may relieve pain. If symptoms
continue unabated, attempts to realign the foot surgically as discussed
in the preceding text are required.
treatment of clubfoot, the longitudinal arch is decreased with weight
bearing and the head of the talus is plantar-flexed. This is usually
associated with a valgus hindfoot and probably results from
incompetence of the spring ligament or calcaneonavicular ligament,
posterior tibial muscle insufficiency, or malalignment at the time of
surgery (2,7,68).
anterior facet of the calcaneus provide a stable articulation for the
head of the talus. When the ligament is overly stretched by casting or
divided with overlengthening at the time of surgery, malalignment of
the talonavicular joint will result. Pinning of the medial column
postsurgery is done in an attempt to maintain the proper talonavicular
joint relationship and avoid sagging of the longitudinal arch. The
force of the posterior tibial tendon is always decreased
postlengthening, and this may aggravate midfoot collapse postsurgery.
dorsiflexion against a tight heel cord when casting. The use of a
percutaneous heel cord tenotomy using the Ponseti method of clubfoot
casting will prevent midfoot breech and decrease the incidence of this
problem after conservative management of clubfeet. Pinning of the
talonavicular joint may prevent this deformity at the time of surgery;
finally, overlengthening of the posterior tibial tendon should be
avoided.
support in mild cases associated with mild symptoms. If the decrease in
the longitudinal arch is accompanied by symptoms unrelieved by arch
supports, treatment with surgical reconstruction may be indicated. This
may be best handled with a calcaneal lengthening and medial reefing if
a flexible foot with competent subtalar joint is present (102).
undercorrection of the clubfoot deformity. In the flexible deformity in
which the navicular can be properly aligned on the head of the talus,
peroneal weakness and relative overpull of the posterior tibial muscle
is often present. In the young child, this is managed with exercise,
stimulation of the peroneal muscles, and prolonged night splinting to
maintain position and flexibility of the foot until peroneal strength
increases to a point that the foot will be stabilized. Attempts at
electrical stimulation have been tried with variable benefit. In the
older child, aged 3 or 4 years, addressing persistent lateral weakness
with an anterior tibial tendon transfer, either split or whole, is the
treatment of choice (discussed in the following text regarding forefoot
supination) (109,110).
transfer and muscle strengthening will not be sufficient. Corrective
casting or exercise can be utilized first, in order to achieve
realignment of the foot if possible. In the absence of success with
conservative management, either shortening of the lateral column or
lengthening of the medial column is required. The lateral column may be
shortened either through the cuboid, the calcaneus, or a combination
with calcaneocuboid joint fusion as described by Evans (105).
It has been shown that the calcaneocuboid joint fusion has little
effect on subtalar and hindfoot motion and may be a beneficial
procedure in neglected or recurrent clubfoot deformity. Osteotomies,
however, with maintenance of joint motion, are in general preferable to
fusions if satisfactory alignment can be achieved. In the very young
child less than 12 months of age, a “Lichtblau” (111)
procedure, which is a resection of a portion of the cartilaginous
articular surfaces of the calcaneus, allows correction of lateral
column deformity. This is only used for infants at the time of the
primary clubfoot procedure.
this results from relative overpull of the anterior tibial tendon with
weak peroneus longus or simply from undercorrection of forefoot
supination, as a component of the original clubfoot deformity. In the
initial cast treatment, great care is taken not
to pronate the foot in the Ponseti method of management. Once the cavus
deformity is treated and the talonavicular joint reduction achieved,
the forefoot is placed in neutral, but care is always taken not to
pronate the first ray, as this may increase the underlying cavus foot
deformity. After proper technique of casting or clubfoot release, it is
noted, however, that some cases have persistent supination of the
forefoot with dorsal bunion. Long-term muscle imbalance is probably the
most common cause of a dorsal bunion. The muscle imbalance that
commonly leads to this is a weak gastrocnemius, compensated by
increased overpull of the great toe flexor and weak peroneals countered
by overpull of the anterior tibial tendon. McKay (112)
has suggested that the flexor hallucis brevis is responsible for the
toe flexion deformity of the great toe in a number of cases. The first
treatment for this deformity is exercise, stretching the toe flexor and
increasing the strength of the peroneal muscles. Surgery is required
for persistent deformity, with transfer of the anterior tibial tendon,
either whole or in part, to the second cuneiform or the cuboid (109,110).
Studies suggest that both of these transfers have a positive effect in
balancing the foot. Treatment for the dorsal bunion may involve flexor
transfer to the first metatarsal, as shown by McKay (112).
It appears that results of split transfer and complete transfer are
equivalent. If a split transfer is used, the lateral limb must be
sufficiently tight to hold the foot in a slightly everted position
following insertion.
significant degree of deformity, surgery should be delayed or limited
to osteotomy rather than arthrodesis. Symptomatic, severely deformed
feet may be improved by proper alignment despite the need for
arthrodesis, multiple osteotomies, or Ilizarov correction. Triple
arthrodesis is not generally indicated in patients younger than 10
years, as foot growth will be severely compromised. The stiff, deformed
foot can only be improved by triple arthrodesis if a stiff, plantigrade
foot is achieved. There is no question that a foot with intact subtalar
motion is less symptomatic with vigorous activity than one in which
fusion has occurred (114). Accepting this, the
role for arthrodesis is limited to a rigid foot in which deformity
compromises ability to stand and walk. In the preoperative evaluation,
be sure to look for opportunities to correct a foot by osteotomies, and
always be certain to manage deformities conservatively with arch
supports, pads, and braces prior to embarking on surgical correction.
and knee contributing to the apparent foot deformity prior to surgery.
In general, the techniques of triple arthrodesis applied to varus
deformities are much more successful than those applied to valgus
deformities. Correction with closing lateral wedge osteotomy to correct
a varus deformity is much easier to achieve a plantigrade foot. The
techniques of a Beak triple arthrodesis described by Siffert et al. (115), or Lambrinudi triple arthrodesis as modified by Hall and Calvert (116),
are beneficial and highly successful. In cases of valgus triple
arthrodesis, a bone graft is often required in order to create a
satisfactory hindfoot alignment.
a high patient satisfaction with triple arthrodesis in adults for
correction of deformity and eliminating hindfoot pain. However, the
objective data of their series on patient performance is less positive
than patient perception of improvement. Ilizarov management of the
relapsed clubfoot was popularized by Grill and Franke (118);
in 1990, he reported the use of this apparatus for correcting relapsed
clubfeet to a plantigrade position in which normal shoe wear was
possible. At the time of the report, deformity had recurred in 2 of 13
affected feet operated on in the initial series. Wallander et al. (119), Choi et al. (120), Bradish and Noor (121), and Steinwender et al. (122)
have shown the value of Ilizarov management of severe clubfoot
deformity. Synthesizing the available literature, it appears that a
patient with a severe relapsed clubfoot will generally benefit from a
combination of soft-tissue releases and osteotomies with Ilizarov frame
distraction. Hutchinson has documented the benefit of Ilizarov
management using pedobarography, showing a more normal pressure
distribution of the foot following Ilizarov correction.
rotated, supramalleolar osteotomy may be of value. Internal tibial
torsion is generally associated with clubfoot deformity; however,
internal rotation gait is highly associated with clubfoot deformity and
has been identified in postoperative patients in 8% to 48% of cases.
This may result from either weak peroneal musculature, internal tibial
torsion, persistent medial spin of the foot in the mortise, or
persistent foot deformity with metatarsus adductus. Use of a distal
tibial osteotomy to correct the internal rotation component of the
deformity, which results from internal tibial torsion, has been
recommended by Goldner and Fitch (123). It also
may be used as a compromise in realigning a foot that has internal
rotation deformities from all of the above possible etiologies. The
distal tibial osteotomy may be done without fibular osteotomy. If
rotational correction cannot be achieved without unacceptable
translation, a fibular osteotomy at approximately the same level should
be done. The osteotomy can be held in place by 2 crossed K-wires or a
small plate. In Goldner’s series, 2 of 66 patients required change in
position because of vascular compromise at the time of rotational
correction. In general, rotational osteotomy through the tibia results
in excellent alignment of the foot and improved gait.
infancy and is characterized by medial deviation of the forefoot on the
hindfoot (Fig. 30.17). The deformity in its
mildest form resolves spontaneously, has no rigidity, and is of little
clinical significance. In its more severe form, it may be associated
with pain and difficulty wearing shoes, and hence requires treatment.
incidence of metatarsus adductus to be 1 per 1000 live births, with an
increased incidence with positive family history. This is a significant
variation from the data of Hunziker et al. (124),
who found an overall frequency of metatarsus adductus at 12%, with even
higher incidence in twin births. As there is increased awareness of
this condition and increased reporting, higher frequencies are recorded
(125, 126, 127). Although historically this has been associated with hip dysplasia (128,129), recently no association between hip dysplasia and metatarsus adductus has been found (130,131). Therefore, there is no indication for ultrasound screening of hips in infants when this deformity exists.
have documented an alteration in the medial cuneiform in association
with metatarsus adductus without joint subluxation or tendon
abnormalities. Reimann and Werner (133)
suggested that the primary abnormality in metatarsus adductus was
subluxation of the tarsal metatarsal joints in addition to cuneiform
abnormality (133). The possibility of muscle
contracture, with imbalance between the anterior and posterior tibial
tendons and abnormal insertion of the anterior tibial tendon, has been
suggested (126, 134, 135, 136). An abnormally shaped cuneiform (137) may play a role in persistent metatarsus adductus (Fig. 30.18).
 |
|
Figure 30.17 Metatarsus adductus in an infant. Note convex lateral border and neutral hindfoot alignment.
|
 |
|
Figure 30.18
Metatarsus adductus in an older child with trapezoidal-shaped medial cuneiform. (From Cappello T, Mosca VS. Metatarsus adductus and skewfoot. Foot Ankle Clin 1998:683, with permission.) |
is the hallmark of this condition. There is prominence of the proximal
fifth metatarsal laterally. The hindfoot is generally in neutral and
forefoot slightly supinated. A deep medial crease is usually present.
in which the feet are placed on a photocopy machine and the axis of the
heel is projected through the forefoot or a similar line is drawn on
the plantar surface of the foot. The heel bisector moves laterally
across the toes with increasing severity of the condition. The second
classification (Fig. 30.19) (138)
defines metatarsus adductus based on flexibility. By holding the heel
with a thumb providing a fulcrum over the fifth metatarsal head,
pressure is applied laterally to the forefoot. The degree to which the
lateral border of the foot can be corrected determines the flexibility
of the foot.
developed a classification system for metatarsus adductus and skewfoot
based on radiographs in a small group of children, Cook et al. (141)
found that classification system to have high interobserved and
intraobserver error. Given that the natural history of this condition
is one of spontaneous resolution, simply documenting the clinical
deformity and observing for spontaneous resolution is a generally
accepted routine. Radiographs are indicated for patients with
persistent deformity. A standing or simulated weight-bearing view will
demonstrate a trapezoidal shape to the medial cuneiform
and medial deviation of the metatarsals (Fig. 30.18).
This can be differentiated from skewfoot, in which lateral subluxation
of the navicular is a hallmark on the anteroposterior view. When the
navicular is not ossified, the long axis of the first metatarsal is
translated laterally relative to the talus.
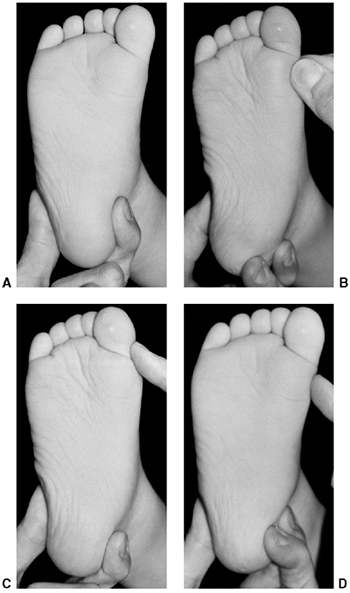 |
|
Figure 30.19 Bleck’s flexibility classification of metatarsus adductus. A: Metatarsus adductus in an infant. B: A flexible foot can be passively overcorrected into abduction with little effort. C: A partly flexible foot can be passively corrected only to the midline. D: An inflexible foot cannot be passively corrected to the midline. (From Bleck EE. Developmental orthopaedics. III. Toddlers. Dev Med Child Neurol 1982;24:533.)
|
in the older child, a contribution of internal tibial torsion and
femoral anteversion in addition to metatarsus adductus should be noted
on physical examination and clearly documented. The natural history of
each of these deformities will then contribute to the spontaneous
resolution or persistence of the intoeing deformity.
Although passive stretching exercises are commonly recommended, their
efficacy has not been clearly demonstrated. Ponseti and Becker (3) noted potential harm in increasing hindfoot deformity by overzealous treatment.
and Ponseti have demonstrated efficacy in manipulation and serial
casting in resolution of metatarsus adductus that is either partially
flexible or inflexible. Best results from corrective casting occur in
patients younger than 1 year at initiation of therapy (3,138,140). In the use of corrective casting, there is some risk of increasing hindfoot valgus or producing an iatrogenic skewfoot (3,126).
One way in which the risk of hindfoot valgus can be decreased in
corrective casting for metatarsus adductus is by plantar-flexing the
foot slightly to lock the subtalar joint. Postcast splinting may be
used to decrease the rate of recurrence, which has been reported as
occurring in between 8% and 37% of cases (126,138,142).
months and 1 year of age. In children younger than 6 months, gentle
exercises are advocated with use of a reverse-last shoe or Bebax shoe
at times to maintain correction.
In select cases in which the deformity has a primary component of
medial deviation of the great toe, release of the abductor hallucis has
been advocated; it should be noted that this may result in the
development of hallux valgus (143). Medial capsulotomies have been reported in treatment of this deformity (144). Heyman et al. (145)
described treatment using forefoot capsulotomy of the tarsometatarsal
joints with release of intermetatarsal ligaments. Long-term studies (146,147),
however, have shown a 41% failure rate, with complications including
skin slough and pain with prominence of the tarsal metatarsal joints.
used as a beneficial extraarticular alternative, avoiding the
complications of capsulotomies (148,149).
The greatest risk in this procedure, however, is growth arrest of the
first metatarsal from physeal injury, noted in a significant number of
patients treated in this manner (148,150,151).
disability from metatarsus adductus, a combination osteotomy including
closing wedge of the cuboid and opening wedge of the first cuneiform
has been advocated (152) (Fig. 30.20).
As the primary deformity in metatarsus adductus is a trapezoid-shaped
first cuneiform in most cases, this procedure is most appealing. It
treats the deformity where the pathology is, and carries no risk of
growth arrest to the first metatarsal. It has been described with
removal of a lateral wedge from the cuboid with insertion into the
first cuneiform. The author has found the wedge from the cuboid to be
of insufficient substance to provide sufficient strength as a spacer in
the opening wedge of the cuneiform; allograft appears to be a
better
choice. In severe cases, the cuboid-closing osteotomy and
cuneiform-opening osteotomy can be combined with osteotomies of the
second, third, and fourth metatarsals at their bases, to provide better
correction (153, 154, 155, 156).
 |
|
Figure 30.20
Correction of symptomatic metatarsus adductus in an older child with an opening-wedge osteotomy of the medial cuneiform and a closing-wedge osteotomy of the cuboid. |
deformity combining medial deviation of the forefoot, lateral
translation of the midfoot, and valgus hindfoot into one condition (Fig. 30.21).
The recognition of the multiplanar abnormalities in this deformity is
critical to its appropriate treatment. In the past, inconsistent
terminology has been applied to this, including congenital metatarsus
varus (136) or serpentine metatarsus adductus (125). Mosca (102,157,158) defined the skewfoot with a significant valgus hindfoot (Fig. 30.22) as a major component of this deformity.
terminology relative to this deformity, not to mention its rarity, the
pathogenesis, natural history, and treatment remain a bit confusing.
Researchers have stated that the deformity may result from improper
cast technique applied to metatarsus adductus and/or clubfoot, but
there clearly are a number of idiopathic cases.
of metatarsus adductus with iatrogenic lateral subluxation of the
navicular and creation of valgus hindfoot (3),
its cause generally remains unknown. Most cases occur spontaneously
with a trapezoid-shaped medial cuneiform as seen in metatarsus adductus
(157,159), but the hallmark of the condition is medial deviation of the forefoot with lateral translation of the midfoot.
from skewfoot in the infant, in whom no calcification of the navicular
or first cuneiform is present. However, clinically one may note a
significant valgus deformity in association with metatarsus adductus
and the ability to palpate the head of the talus in the longitudinal
arch. By direct observation (Fig. 30.21), a
deep concavity in the medial aspect of the foot, created by a step-off
between the head of the talus and the base of the first metatarsal, is
palpable. This is seen in association with adduction of the first ray
and valgus hindfoot. The deformity is generally flexible with
respect
to subtalar motion but somewhat rigid with respect to correction of the
forefoot. Callusing may be present under the head of the talus (Fig. 30.23) and at the base of the fifth metatarsal, as seen in severe metatarsus adductus (102,157,159). Tightness of the heel cord may cause symptoms of pain, as it often does in the flatfoot.
 |
|
Figure 30.21
Probable skewfoot in an infant. Apparent metatarsus adductus, but with the head of the talus visible and palpable medially. This indicates coexistent eversion of the subtalar joint with abduction of the navicular on the head of the talus. (From Mosca VS. Flexible flatfoot and skewfoot. In: Drennan JC, ed. The child’s foot and ankle. New York: Raven Press, 1992:355, with permission.) |
 |
|
Figure 30.22 Adolescent skewfoot, that is, valgus deformity of the hindfoot with adductus of the forefoot.
|
midfoot, radiographs taken at birth are difficult to interpret in
differentiating metatarsus adductus from skewfoot. It is, however,
noted that in metatarsus adductus, there is generally medial deviation
of the first ray, but that the proximal portion of the first metatarsal
is aligned with the head of the talus, whereas in the skewfoot (Fig. 30.24),
the first ray is translated relative to the long axis of the talus, and
may actually be parallel to it, and yet appear to be significantly
medially deviated. Attempts by Berg (140) to
radiographically differentiate metatarsus adductus from skewfoot in the
infant have been unrewarding because of poor interobserver and
intraobserver reliability (141).
determine the degree of deformity, both in the anteroposterior and lateral projections.
 |
|
Figure 30.23 Painful callus that developed under the head of the talus in a skewfoot with contracted Achilles tendon.
|
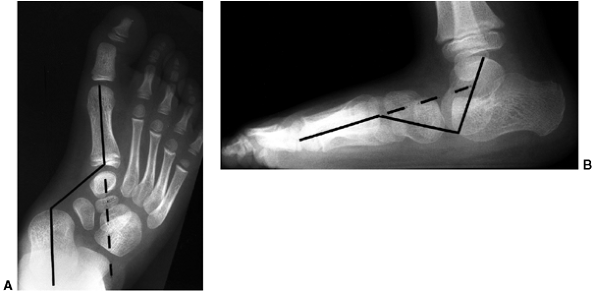 |
|
Figure 30.24 Anteroposterior (A) and lateral (B)
radiographs of a skewfoot demonstrating skew, or zigzag, deformities in both planes. (From Mosca VS. Calcaneal lengthening for valgus deformity of the hindfoot. Results in children who had severe, symptomatic flatfoot and skewfoot. J Bone Joint Surg Am 1995;77:500–512, with permission.) |
that many cases of mild skewfoot undergo spontaneous correction, as
happens with metatarsus adductus (3,4) and flexible flatfoot (1,46).
The long-term disability attributed to this deformity remains difficult
to estimate, but treatment is clearly required in some cases because of
pain and difficulty with wearing shoes at the end of the first decade
of life (102, 125, 126, 127, 136, 157, 158, 159, 160).
is difficult. In applying cast treatment to the forefoot deformity in
skewfoot, the risk is of increasing the valgus deformity in the
hindfoot and the lateral translation of the midfoot. Therefore, when
corrective casting is applied to skewfoot in early childhood, the foot
should be placed in a plantar-flexed position with slight varus to lock
the hindfoot and gentle pressure applied to the forefoot.
Overaggressive casting should not be undertaken (3,125, 126, 127, 138, 140). Dennis-Brown bars are not indicated in this condition.
deformity have pain and callusing under the head of the talus as well
as over the fifth metatarsal and the first metatarsal head medially (102, 157, 158, 159).
Tight heel cord is often associated with painful skewfoot, as is
present in a painful flatfoot. Stretching of the Achilles tendon is
indicated as part of conservative management. A soft orthosis to
support the talar head and the longitudinal arch and decrease the
deformity in the hindfoot may be of value. Use of a rigid orthosis in
this condition may cause increased pain and should be used cautiously.
relieve pain and callosities. Operative management should be directed
at the specific deformity that appears to be associated with symptoms
in a given case; that is, if the lateral translation through the
midfoot and forefoot deformity is most prominent, treatment may include
closing-wedge osteotomy of the cuboid and lengthening of the first
cuneiform (Fig. 30.25), similar to metatarsus adductus. If, however, the deformity has a major component of hindfoot valgus (Fig. 30.26), it must be treated. Historical recommendations have included osteotomies at the base of the
metatarsals (136) and subtalar and triple arthrodesis of the hindfoot (147,148,160).
The use of arthrodesis in this condition should be avoided and attempts
at correction through osteotomy encouraged. Complications of triple
arthrodesis and subtalar arthrodesis are enumerated in the section on
flatfoot in this chapter. Mosca (157) proposed
correction of symptomatic skewfoot by combining individual osteotomies
of the forefoot and hindfoot to result in the correction of this foot
deformity (Fig. 30.26). The combination of a
calcaneal lengthening to correct hindfoot valgus as well as a first
cuneiform lengthening to correct forefoot deformity is warranted. This
is done according to the modified technique of Evans (102,161);
it is always associated with lengthening of the heel cord and generally
associated with medial reefing of the talonavicular joint. In Mosca’s
series (157), 9 of 10 patients with severe skewfoot achieved satisfactory clinical and radiographic corrections of skewfoot deformity.
 |
|
Figure 30.25
In the skewfoot without severe hindfoot valgus deformity, appropriate management may be first cuneiform lengthening with lateral closing wedge of the cuboid, similar to treatment of metatarsus adductus. |
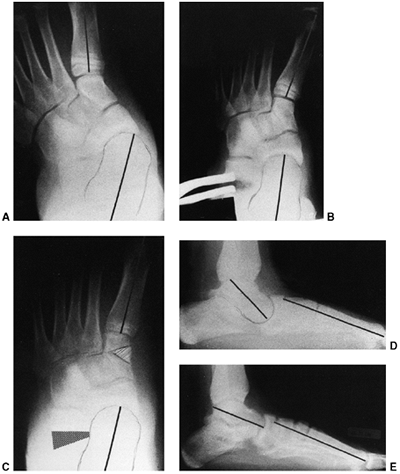 |
|
Figure 30.26 Preoperative, intraoperative, and postoperative radiographs of a painful skewfoot in a 13-year-old adolescent. A: Preoperative anteroposterior view. B: Intraoperative distraction of calcaneal osteotomy. C: Corrected deformity on anteroposterior radiographs with grafts in place. D: Preoperative lateral view. E:
Postoperative correction. Calcaneal lengthening osteotomy, medial cuneiform opening-wedge osteotomy, and Achilles tendon lengthening were used. (From Mosca VS. Flexible flatfoot and skewfoot. In: Drennan JC, ed. The child’s foot and ankle. New York: Raven Press, 1992:355, with permission.) |
condition in which a decrease in the healthy longitudinal arch of the
foot is present in stance, associated with valgus alignment of the
hindfoot. Although this deformity is often referred to as “pronation,”
it should be noted that the actual deformity is a valgus hindfoot
associated with a relative supination of the forefoot. The term
flexibility refers to mobility about the subtalar joint, which
differentiates this from the rigid flatfoot or peroneal spastic
flatfoot indicative of an underlying pathologic state. A “flexible”
flatfoot indicates a variation of a normal, which is occasionally
associated with symptoms in its pathologic state.
flatfoot was present in 23% of 3619 adults. They classified them into
flexible, or hypermobile, flatfoot, which was generally asymptomatic
and accounted for at least two thirds of the flatfeet. In 25% of cases,
the flatfoot was associated with a tight heel cord and was much more
likely to be associated with symptoms (162,163). According to a study by Reimers et al. carried out in Danish schoolchildren (164), the proportion of feet with decreased longitudinal arch declined from 42% in the 3- to 5-year
age group to 6% in the teenagers. They found a strong relation between
short Achilles tendon and persistence of deformity in the teenagers.
alignment in early childhood, with spontaneous resolution in the vast
majority of cases. Although muscle weakness has been proposed as a
possible etiology, Basmajian and Stecko (12)
demonstrated that little or no electromyographic activity of the
muscles of the foot and ankle is present when physiologic loads are
applied to a standing subject with the foot in plantigrade position.
They, therefore, concluded that the bone-ligament complex, and not
muscle contraction, determines the height of the longitudinal arch.
Mann and Inman (13) confirmed this theory. The
effects of extrinsic factors on the shape and development of the
longitudinal arch is suggested by studies from developing countries,
including those of Sim-Fook and Hodgson (5) and Rau and Joseph (6), finding a higher incidence of flatfoot in children wearing shoes than those who did not. Echarri and Forriol (165),
in applying Staheli’s index of arch development, found boys to have a
higher tendency for flatfoot than girls, and wearing of shoes to have
no influence on the height of the longitudinal arch or morphology of
the foot.
longitudinal arch in early infancy and its spontaneous resolution with
growth, one may be hard pressed to call this, in general, a pathologic
condition. However, in a number of cases, spontaneous resolution does
not occur and symptoms become quite significant. The difficulty is in
isolating the pathologic form of flatfoot deformity from the normal
developmental form. The general examination should include assessment
of ligamentous laxity as well as torsional and angular deformities. It
is noted that flatfoot deformity has a higher presence in association
with valgus deformities of the knees and generalized ligamentous
laxity. In the presence of external tibial torsion or external rotatory
deformity of the hip, the push-off in gait is compromised and the
deformity of flatfoot increased. In general, a flexible flatfoot will
revert to a normal position with the presence of a longitudinal arch in
a non-weight-bearing or sitting position. When rising on the toes, the
longitudinal arch will form and the hindfoot tip into the varus with
plantar flexion of the hindfoot and simultaneous development of a
longitudinal arch (Fig. 30.27).
with the patient kneeling on a chair will often demonstrate the
hindfoot to be in neutral with an associated supination deformity of
the forefoot. In stance, the elevation of the great toe (in the Jack
toe-raise test) (Fig. 30.28) will produce an elevation in the longitudinal arch by using the windlass effect of the plantar fascia (159,166).
Dorsiflexion of the foot with knee extended and hindfoot slightly
inverted should be done to test for Achilles tendon tightness, as this
is the common pathologic state associated with painful flatfoot
deformity. Finally, the skin pattern on the plantar aspect of the foot
should be viewed, as callosities over the head of the talus are
associated with symptoms and greater severity of flatfoot deformity.
Sequential footprint measurements can be done in order to determine
severity of the foot deformity. Kanatli et al. (167) have shown an excellent correlation between footprint and radiographic analysis in flexible flatfeet in children. Lin (168)
showed that subjects with flatfoot deformity tended to perform physical
tasks poorly and walked more slowly than controls with healthy feet.
They also found that flatfoot deformity was associated with valgus
knees and generalized ligamentous laxity to some degree. They cautioned
against regarding flatfoot deformity as a static problem and encouraged
analysis of its effect on activity. Cowan et al. (169)
reported a study of prospective Army recruits, indicating that
low-arched individuals had no increase in the risk of injury, whereas
Kaufman et al. (170) reported an increased risk
of overuse injuries in patients with dynamic pes planus, particularly
with restricted ankle dorsiflexion.
 |
|
Figure 30.27
The arch elevates and the heel corrects from valgus to varus in a flexible flatfoot during toe standing, because of the windlass effect of the plantar fascia. (From Mosca VS. Flexible flatfoot and skewfoot. In: Drennan JC, ed. The child’s foot and ankle. New York: Raven Press, 1992:355, with permission.) |
deformity, a complete physical examination must be done, testing muscle
strength of all lower extremity muscles and ruling out spinal pathology
by physical examination. Range of motion and alignment as well as
muscle strength and sensation should be evaluated in the lower
extremities. Tightness of the Achilles tendon and flexibility of the
foot deformity must be emphasized.
needed for routine evaluation. In severe cases, however, a series of
sequential lateral radiographs may be helpful in
determining
the course of the deformity. Radiographs, however, define only a static
position and cannot be used as an indication for treatment (46,171).
 |
|
Figure 30.28
The arch elevates in a flexible flatfoot with the Jack toe-raise test because of the windlass effect of the plantar fascia. (From Mosca VS. Flexible flatfoot and skewfoot. In: Drennan JC, ed. The child’s foot and ankle. New York: Raven Press, 1992:355, with permission.) |
as measured between the long axis of the talus and the first metatarsal
and the calcaneal pitch, which are indicative of the severity of the
flatfoot deformity (Fig. 30.29). One may also
look for localized sag between the navicular and first cuneiform rather
than at the talonavicular joint, as this may have significant
implications for treatment. A tarsal coalition may also be evaluated
radiographically by standing anteroposterior, lateral, and oblique
radiographs. Brown et al. (173) found that the
C-sign on the lateral radiograph was more specific for flatfoot than
for subtalar coalition. Although some have felt that the C-sign (Fig. 30.30) was diagnostic of middle facet talocalcaneal coalition, it appears not to be so.
must be differentiated from a vertical talus. In doing this, a
plantar-flexion lateral view of the foot is obtained in order to show
that the long axis of the first metatarsal becomes colinear with the
long axis of the talus on a lateral view (Fig. 30.30).
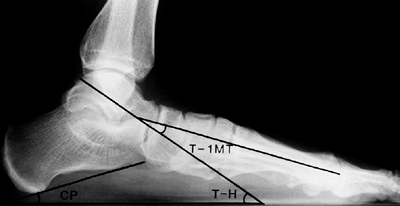 |
|
Figure 30.29 Weight-bearing lateral radiograph. The calcaneal pitch (CP) and the talus-horizontal angle (T-H) are the best measurements to assess valgus deformity of the hindfoot. The talus-first-metatarsal angle (T-1MT)
is known as the Meary angle. A plantar flexed apex is seen in a valgus foot. (From Mosca VS. Calcaneal lengthening for valgus deformity of the hindfoot. Results in children who had severe, symptomatic flatfoot and skewfoot. J Bone Joint Surg Am 1995;77:500–512, with permission.) |
resolve in most cases, as has been shown by Staheli and others. Shoeing
has no effect on the development of the longitudinal arch and may
actually be detrimental to it (165). There
appears to be a wide range of arch height at all ages, but in general,
there is consistent development of a healthy longitudinal arch during
childhood (Fig. 30.31). There are no long-term
prospective studies on the natural history of flatfoot deformity
related to symptoms. It does appear, however, that in select cases,
particularly in association with a tight heel cord, unresolved flatfoot
deformity may be associated with an increase in foot pain and stress
injuries in the lower extremities. Most authorities agree that flexible
flatfoot is an anatomic variant and not a disabling deformity (159,162,171).
Nevertheless, it may be associated with symptoms in its unresolved
state. Uncontrolled studies indicate some efficacy of orthotic devices
and shoe modifications in the development of the longitudinal arch in a
child’s foot (174). More recently, randomized
control studies reveal no benefit from shoe modifications and inserts
compared to normal development (175, 176, 177). In a study by Garcia-Rodriguez et al. (178),
the prevalence of flexible flatfoot was evaluated in school children
between the ages of 4 and 13 years. They found the prevalence of
flatfoot deformity to be 2.6%. However, 14.2% of the children were
receiving orthopaedic treatment, despite the diagnostic criteria for
flatfeet being satisfied in only 2.7% of the children. More
surprisingly, the children meeting the diagnostic criteria for flatfoot
deformity were only being treated in 28.1% of the cases. Overweight
children were found to be at greater risk of flatfoot deformity.
Caution against the rate and expense of overtreatment of a physiologic,
self-limiting deformity was raised.
with flexible flatfoot deformity may have activity-related pain. The
pain is usually diffuse or may be focal over the longitudinal arch. An
exam should be done to evaluate muscle tightness as well as the foot
deformity and flexibility of the flatfoot. If a tight heel cord is
found, a stretching
program should be begun. Mann and Inman (13)
found a higher incidence of intrinsic muscle activity in flatfoot
deformity, which may result in fatigue and pain during prolonged
standing. Over-the-counter or custom-molded shoe inserts have been
shown to relieve or diminish symptoms (179). Although arch supports do seem to provide relief in a number of cases, Miller et al. (180)
were unable to show any change in ground reaction forces relating to
the use of orthotic devices. The data were contrary to the current
hypothesis about the benefits of the use of an orthotic device.
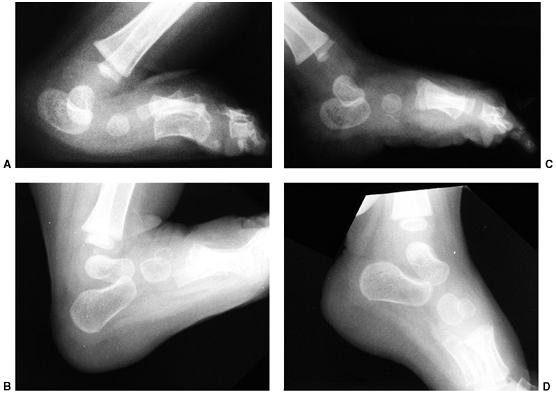 |
|
Figure 30.30 A: Lateral dorsiflexion radiograph of congenital vertical talus, showing persistent plantar flexion of the talus and calcaneus. B: Lateral dorsiflexion radiograph of a healthy foot, showing full dorsiflexion of the talus and calcaneus. C:
Lateral plantar-flexion radiograph of the congenital vertical talus, showing persistent dorsal translation of the forefoot on the hindfoot. D: Lateral plantar-flexion radiograph of a healthy foot, showing good alignment of the forefoot on the hindfoot. |
by an orthotic device, it appears that symptoms can be significantly
decreased. With an external rotation position of the foot in push-off,
stresses over the midfoot are exacerbated. Use of an orthotic device
and/or supportive shoe may be of value in such cases. Surgery is rarely
indicated in flexible flatfoot deformity. However, in select cases,
despite attempts at conservative therapy with an exercise program and
proper arch support, surgery should be considered. Alignment of the
entire lower extremity emphasizing valgus alignment at the knee and
ankle and rotational alignment of the femur and tibia should be
considered. When surgery is to be considered, options include
soft-tissue reconstruction, osteotomy, arthroereisis, and arthrodesis.
Surgery for flexible flatfoot should be an infrequent procedure,
employed in cases of intolerable pain despite maximal conservative
management. Weight loss and correction of angular and rotational
malalignment of the legs, including ankle valgus, should be considered
preoperatively. In an occasional patient with a tight heel cord despite
a vigorous stretching program, judicious heel cord lengthening may have
a role in the management of flexible flatfoot, as an isolated
procedure. Beyond this, soft-tissue reconstruction plays no part in the
management of a persistently painful flexible flatfoot deformity.
Fusion, including localized midtarsal, subtalar, and triple
arthrodesis, has been recommended for the treatment of a flexible
flatfoot deformity over the past 70 years. Localized midtarsal
arthrodeses are all variants of a Hoke navicular cuneiform type fusion (181, 182, 183, 184, 185, 186, 187).
Each of these reconstruction arthrodeses may improve alignment of the
foot, but long-term results indicate poor outcomes in 49% to 70% of
cases. The results were classified as unsatisfactory based on
degenerative arthritis primarily involving the talonavicular joint,
pain, or recurrence of deformity. In response to unsatisfactory results
of limited arthrodeses, some have recommended triple arthrodesis as a
procedure of value to prevent midfoot and hindfoot arthritis. Long-term
results of triple arthrodeses indicate that this
procedure also carries a significant risk of long-term negative consequences based on adjacent degenerative arthritis and pain (188).
Therefore, present recommendations primarily include trying to
reconstruct the foot while maintaining all normal articulations.
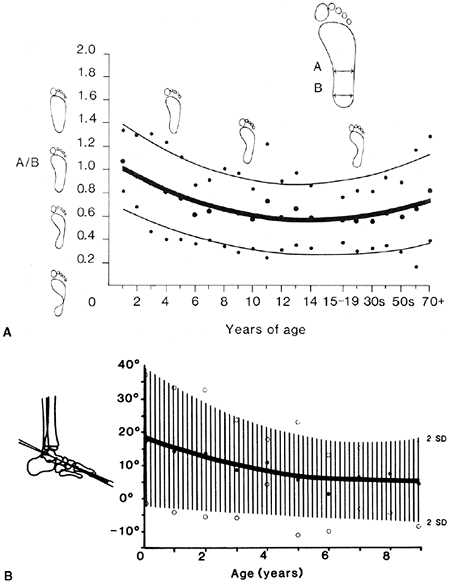 |
|
Figure 30.31 A:
Footprints from individuals of all ages show that children are more flat-footed than adults, that there is a wide range of healthy arch heights, and that the arch generally elevates spontaneously during the first decade of life. B: Radiographs from children of all ages confirm the footprint data. The drawing and graph represent the lateral talus-first-metatarsal angle. (A from Staheli LT, Chew DE, Corbett M. The longitudinal arch. A survey of eight hundred and eighty-two feet in normal children and adults. J Bone Joint Surg Am 1987;69:426–428, with permission; B from Vanderwilde R, Staheli LT, Chew DE, et al. Measurements on radiographs of the foot in normal infants and children. J Bone Joint Surg Am 1988;70:407–415, with permission.) |
be the option of choice for a flexible flatfoot at this time. Such
procedures improve alignment while maintaining mobility. There are two
osteotomies that hold promise for long-term relief of symptoms. Both
are calcaneal procedures, but one translates the calcaneal tuberosity
medially whereas the other lengthens the calcaneus with a positive
effect on hindfoot and forefoot alignment.
will not elevate the plantar-flexed talus, but will realign the
weight-bearing axis of the hindfoot. The isolated hindfoot osteotomy
may be combined with a closing wedge osteotomy of the medial cuneiform
and an opening wedge osteotomy of the cuboid to restore forefoot and
midfoot alignment, as described by Rathjen and Mubarak (190),
with good results. In cases in which the talus is not exceedingly
plantar-flexed and the navicular is not dorsolaterally translated, this
appears to be a valuable procedure, perhaps even the procedure of
choice. If there is a tight heel cord, one should consider a fascial
lengthening in association with this osteotomy.
appears to offer the best opportunity to correct the flexible flatfoot
deformity, maintaining joint mobility while reconstructing bony
alignment. In this procedure, an opening-wedge osteotomy is performed
through the neck of the calcaneus between the anterior and middle facet
(Fig. 30.32), inserting a trapezoidal graft
(generally allograft) to maintain length. The effect of this osteotomy
in lengthening the calcaneus is correction of the eversion of the
subtalar joint. The osteotomy improves the valgus alignment of the
calcaneus, reduces the dorsolateral translation of the navicular into
proper alignment with the long axis of the talus, and improves the
talocalcaneal relation.
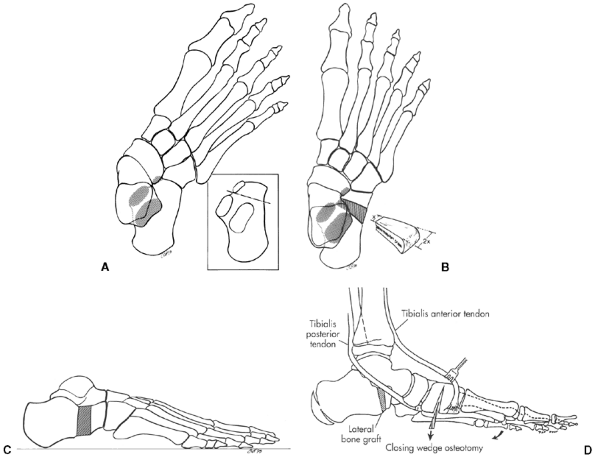 |
|
Figure 30.32 A:
Calcaneal lengthening osteotomy. Dashed line indicates the position of the oblique osteotomy between the anterior and middle facets of the calcaneus. B, C: Insertion of the trapezoid-shaped tricortical iliac crest bone graft corrects all components of the valgus deformity of the hindfoot. D: A plantar-based closing wedge osteotomy of the medial cuneiform corrects the supination deformity of the forefoot. Lengthening of the gastrocnemius or the Achilles tendon is almost always necessary. (A, B, and C from Mosca VS. Calcaneal lengthening for valgus deformity of the hindfoot. Results in children who had severe, symptomatic flatfoot and skewfoot. J Bone Joint Surg Am 1995;77:500–512; D from Anderson AF, Fowler SB. Anterior calcaneal osteotomy for symptomatic juvenile pes planus. Foot Ankle 1984;4:274–283, with permission.) |
the talus as seen on the lateral view (Meary angle) is likewise
improved by this procedure (102, 161, 191, 192, 193).
Although the effects of this procedure on a flexible flatfoot are
primarily positive, it may supinate the forefoot elevating the first
ray. If this occurs, a plantar-flexion osteotomy through the first
cuneiform is mandatory in order to restore the tripod of the foot and
prevent an exacerbation of forefoot supination deformity (Fig. 30.32).
The effect of elevating the first ray is counteracted by an intact
peroneus longus that should be maintained while doing this lengthening
osteotomy. Heel cord lengthening and peroneus brevis lengthening are
always done as a part of this procedure.
procedure, a block of material is placed in the subtalar joint in order
to eliminate motion in the flexible flatfoot (194,195).
The block may be sylastic or high-molecular-weight polyethylene, but in
either case there is a significant incidence of loosening,
displacement, and synovitis related to this procedure. Black et al. (196) and Verheyden et al. (197)
both recommended abandonment of this procedure because of a high rate
of negative outcomes. This is in contrast to the work of Grady (198)
who reported consistently excellent results in 234 children. Although
the author has no experience personally with this procedure, the use of
a nonbiologic implant in young children for what is generally a
self-limited condition seems illogical. Osteotomies seem to be of
benefit in the occasional patient to correct deformity and relieve
symptoms. Treating the asymptomatic flatfoot in children with a
surgical reconstructive procedure appears to be generally unwise and
unnecessary. In the face of neurologic conditions and pathologic
degrees of ligamentous laxity, however, some method of management of
the flexible flatfoot deformity may include such procedures, as
described by Smith and Millar (195).
dislocated dorsolaterally on the head of the talus. Associated with
this in varying degrees are hindfoot equinus, dorsal cuboid
dislocation, and anterior soft-tissue contracture including toe
extensors, peroneals, and anterior tibial tendons (199). Taken together, these describe the deformity in congenital vertical talus.
neuromuscular diseases. Case reports have indicated autosomal dominant
transmission with incomplete penetrance (203,206)
in some cases. Congenital vertical talus is associated with
myelomeningocele, sacral agenesis, diastematomyelia, and
arthrogryposis. In Sharrard and Grosfield’s series of patients with
myelomeningocele (207), 10% of patients had
vertical talus associated with spinal dysraphism. Given the frequency
with which this deformity is associated with neuromuscular disorders, a
thorough evaluation of the neuroaxis with MRI is indicated in patients
with vertical talus.
surface, with a hindfoot resting in equinus and a hypoplastic,
laterally deviated forefoot (Fig. 30.33). Lloyd-Roberts and Spence (208)
described the appearance as “a prominence in the sole of the foot from
which the heel and forefoot rise in a gentle curve.” The Achilles
tendon is always contracted with a fixed equinovalgus position. The
head of the talus is palpable in the medial aspect of the midfoot. Upon
plantar-flexing the foot, a gap can be felt anterior and medially to
the medial malleolus as a space where the normal neck of the talus
should be, when the navicular plantar flexes over the head of the
talus. In contrast to a flexible flatfoot or a positional
calcaneovalgus foot, the talonavicular joint cannot be reduced by
manipulation. Some authors have differentiated a vertical talus from an
oblique talus (175,209).
An oblique talus is one in which there is dorsal subluxation of the
navicular, but some flexibility of the foot exists such that a rigid
dislocation of the navicular is not present; however, the foot is
significantly more rigid than a common flexible flatfoot. This term may
be confusing, but it is helpful if one considers it as describing a
foot that appears on physical examination to be nearly like a vertical
talus but that nearly reduces fully on a plantar-flexion view
radiograph. In such a foot, an oblique talus can be improved by
conservative management with casting and arch support, whereas surgery
is always required in a true congenital vertical talus.
should be taken in a neutral position, as in any pediatric foot
disorder. Standing radiographs are taken in a child able to stand;
however, in the infant, these radiographs are taken in a neutral
position. The diagnostic x-ray film of a vertical talus is a forced
plantar-flexion view (Fig. 30.30) in which
persistent malalignment of the long axis of the talus and the first
metatarsal are confirmed. Because the navicular and first cuneiform are
not ossified in infancy, the dislocation is implied by virtue of the
lack of colinear alignment of the first metatarsal with the long axis
of the talus. In a lateral x-ray film of a healthy, unstressed foot,
the first metatarsal is aligned with a long axis of the talus. The
position of the cuboid relative to the calcaneus should be determined,
as this is indicative of the severity of a vertical
talus. In the most severe form, there is a dorsal dislocation of the cuboid on the calcaneus.
 |
|
Figure 30.33 Congenital vertical talus in an infant. A: Medial. B: Lateral.
|
Most have found contractures of the tibialis anterior, extensor
hallucis longus, extensor hallucis brevis, peroneus tertius, peroneus
longus, peroneus brevis, and the Achilles tendon. The peroneus longus
and peroneus brevis may be anteriorly subluxed over the lateral
malleolus, and the posterior tibial tendon may be subluxed anteriorly
over the medial malleolus. The head of the talus is generally
protruding below the posterior tibial tendon and the calcaneonavicular,
or spring ligament, is markedly attenuated. The calcaneus is severely
externally rotated and everted, with its posterolateral border in
proximity to the fibula. Sustentaculum talae and anterior facet of the
subtalar joint are exceedingly hypoplastic or absent in the most severe
cases. The dorsal capsule of the talonavicular joint is thickened and
contracted.
significant disability, with poor push-off, difficult shoe fitting, and
a gait that is similar to one seen in a patient who has had a Symme
amputation. The forefoot becomes atrophic over time, with thick plantar
callosity forming over the head of the talus. No weight bearing occurs
either on the true heel pad over the calcaneus nor under the forefoot.
Eventually, push off becomes impossible.
method has markedly decreased the role of surgical management in this
deformity, cast treatment of vertical talus has been rather ineffective
beyond providing stretching of the dorsolateral soft tissues. In
general, the foot is placed in a series of corrective casts in order to
stretch the dorsal structures, hoping that surgical treatment will be
rendered less complex. Casting is considered important by nearly all
who have studied this problem (202,203,212,214).
Following a series of corrective casts, an exercise program and,
perhaps, a bivalve cast or splint is used until the time of surgery.
Surgical options include one-stage or two-stage releases, talectomies,
naviculectomy, subtalar arthrodesis, and triple arthrodesis. Consensus
has lead to a single-stage procedure in most cases at this point.
but was soon abandoned. It was destructive and resulted in unacceptable
outcome, not addressing the underlying pathology. It also left no
options for future reconstruction and has been thoroughly abandoned.
The primary choices for operative management of congenital vertical
talus in a child younger than 2 years are one-stage versus two-stage
reconstruction involving release of tight tendons and ligaments and
realignment of osseous structures. If a two-stage procedure is chosen,
the first stage consists of lengthening the contracted dorsolateral
tendons and release of the contracted dorsolateral joint capsule with
reduction of the midfoot on the hindfoot. The second stage consists of
a posterolateral release of the contracted Achilles tendon, peroneal
tendons, and posterior capsule. Ogata et al. (203) and Mazzocca et al. (215)
found increased complications in the two-stage release. Included in the
complications described by Ogata was avascular necrosis of the talus.
Mazzocca and Romness compared the dorsal to the posterior approach for
one-stage correction of congenital vertical talus. The dorsal approach
was found to be associated with shorter operative time and better
clinical score with fewer complications than the posterior approach.
Several authors have reported the addition of a full or split transfer
of the tibialis anterior to the head or neck of the talus (214,216,217,222,223).
Although the transfer adds little time to the procedure, it would seem
that a dynamic stabilizer of the talus would be unlikely to be
particularly effective in maintaining talonavicular alignment, and that
this procedure, although brief, may complicate an already somewhat
difficult procedure. The author would not recommend the addition of the
anterior tibialis transfer. The peroneus longus, is a plantar flexor of
the first ray, is particularly strong, and complete transfer of the
anterior tibial tendon may lead to an unopposed plantar flexion force,
providing another reason not to alter the anterior tibial insertion.
reconstructive approach is. There is disproportionate growth between
the medial and lateral borders of the foot in an unreduced vertical
talus and marked atrophy of forefoot and midfoot. The abnormality of
the middle and anterior facet of the subtalar joint become
progressively more severe in the unreduced state. Until the age of 2 or
3 years, there may be stimulus toward further growth of cartilage and
improvement of the talonavicular joint following reduction. Beyond
this, shortening of the medial column and lengthening of the lateral
column are approaches to management that may be required. Some authors
have recommended naviculectomy (224,225)
as a primary salvage procedure in congenital vertical talus. It may be
an effective procedure to shorten the medial column and allow
improvement of the position of the foot in the older child.
Posterolateral release has been combined with naviculectomy for full
deformity correction in a group of older children (Fig. 30.34). Coleman (106)
has recommended subtalar arthrodesis in children older than 3 years;
another alternative for this deformity is lengthening of the lateral
column, which may be done in association with peroneal lengthening in
select cases. Early diagnosis and treatment should eliminate the need
for surgical options in the older child. Nevertheless, occasional cases
requiring subtalar (222,223)
and triple arthrodesis have been reported. If triple arthrodesis is
indicated in this procedure, bone grafting will necessarily be used to
supplement
the
correction of the foot and restore proper alignment. The literature
clearly shows, however, that arthrodesis does result in a significant
rate of degenerative arthritis at the ankle and midtarsal joints in the
long term (188, 226, 227, 228, 229, 230, 231, 232). Napiontek (233)
reported overcorrection of the valgus foot in half the patients who
underwent peritalar reduction combined with subtalar arthrodesis.
Arthrodesis of the joints of the hindfoot, therefore, should be
reserved for salvage procedures in adolescents and those with recurrent
deformity or painful degenerative arthritis.
 |
|
Figure 30.34 Radiographs before (A, B) and after (C, D) naviculectomy for congenital vertical talus in an older child. Arrow indicates the navicular.
|
in which the foot is hyperdorsiflexed, often with the dorsal surface of
the forefoot resting on the anterior surface of the lower leg. It is
thought to be primarily a positional deformity.
the term is used. Wynne-Davies et al. (234) reported the incidence to be 1 per 1000 live births, whereas Wetzenstein (235)
noted a 30% to 50% incidence in the newborn, as well as a significant
correlation to flexible flatfoot in older children. It is more common
in girls and firstborn children.
 |
|
Figure 30.35 Positional calcaneovalgus foot deformity.
|
malpositioning, rather than a truly congenital deformation. Contracture
without congenital deformity or dislocation is the hallmark of this
condition.
differentiating it from pathologic states requiring orthopaedic
intervention, is mandatory. The calcaneovalgus foot deformity should be
differentiated from the following conditions:
-
Paralytic calcaneus foot deformity seen in myelodyplasia and other conditions with absent gastrocsoleus.
-
Posteromedial bow of the tibia (Fig. 30.36).
-
Congenital vertical talus (Fig. 30.33).
calcaneovalgus foot is always present but is associated with a bowed,
shortened tibia. The anterior compartment muscles appear to be somewhat
hypoplastic over the concavity of the bow at the distal tibia. The bow (Fig. 30.36C)
is benign and progressive straightening of the tibia occurs, but
leg-length discrepancy is always present. A vertical talus has a fixed
dislocation of the navicular on the talar head, as described in this
chapter. There is far less flexibility in a vertical talus than in a
calcaneovalgus foot deformity. A motor exam can differentiate the
paralytic calcaneovalgus foot deformity from the true positional
abnormality. If the foot is sufficiently flexible for the examiner to
be confident of the diagnosis of positional calcaneovalgus foot
deformity, no x-ray films are taken. In cases in which there is
confusion between a calcaneovalgus foot deformity and a true vertical
talus, a plantar-flexion lateral radiograph is indicated (Fig. 30.30).
Anteroposterior and lateral x-ray films are taken with which a
calcaneovalgus foot can be differentiated from a vertical talus. In
most cases, x-ray films are not required.
casting is indicated. Exercises to stretch the tightened anterior
soft-tissue structures may be beneficial in speeding the resolution of
this positional deformity. Larson et al. (8)
found no difference between cases managed with exercise versus
observation of this deformity at follow-up of 3 to 11 years. Severity
of the initial deformity bears no relation to final outcome.
Wetzenstein (235) found correlation between a
calcaneovalgus foot and flexible flatfoot deformity in the long term.
Corrective casting is rarely judged to be of benefit if the foot cannot
be plantar-flexed below neutral, and particularly if there are
associated tight peroneal muscles and lateral deviation of the forefoot
with external tibial torsion.
linked the two conditions. A “peroneal spastic flatfoot” is a rigid
flatfoot deformity in which subtalar motion is exceedingly limited. The
rigid foot deformity is accompanied by spasm of the extensor digitorum
communis and the peroneal muscles in many cases. Harris and Beath (238)
further associated the findings of talocalcaneal coalition with
peroneal spastic flatfoot. Interestingly, tarsal coalition has also
been linked with an infrequently occurring tibialis posterior spastic
varus deformity (239,240).
and Nievegert-Pearlman syndrome. Such coalitions have also been seen in
lower-limb congenital abnormalities. Tarsal coalitions have been found
in monozygotic twins (244).
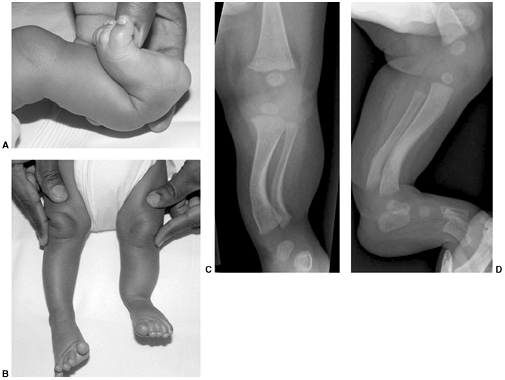 |
|
Figure 30.36 A, B: This patient has a calcaneovalgus foot but with an apparent bow to the tibia with shortening. C, D:
A calcaneovalgus foot should be differentiated from that associated with posteromedial bow of the tibia, as seen on radiographs. |
by Harris and Beath in 1948 to be 2%, on the basis of routine physical
examination of Canadian Army enlistees (238).
On the basis of a cadaveric study by Phitzner in 1896, the rate of
calcaneal navicular synostosis was found to be 2.9%, and if
talocalcaneal coalitions are included as well, its incidence might
reach 6% (245,246). More recently, a study by Lysack and Fenton (247)
documented a general prevalence of calcaneal navicular coalition of
5.6% in a radiographic study, which was significantly greater than
previously reported. The most common sites of tarsal coalition include
the middle facet of the talocalcaneal joint and the calcaneonavicular
coalition (238). Together these account for 90% of all coalitions (248). Tarsal coalitions are bilateral in 50% to 60% of cases. Clarke (249)
documented multiple coalitions in 6 of 30 patients on review
examination of CT scans, raising the question of what the true
percentage of feet with multiple coalitions may be. Also reported are
talonavicular coalitions, calcaneal cuboid coalitions, and navicular
cuneiform coalitions, although all of these are uncommon (248,250) (Fig. 30.37).
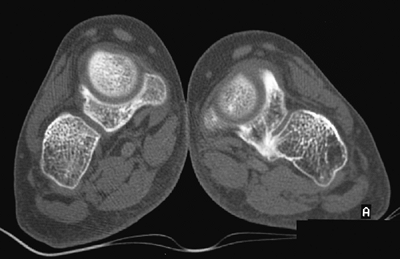 |
|
Figure 30.37 This computed tomography (CT) scan of the midfoot demonstrates a rare cubonavicular coalition.
|
finding in the general population, with symptoms developing in late
childhood and adolescence. The possible etiologies of the painful
tarsal coalition associated with rigid flatfoot are (i) stress fracture
at a time when progressive ossification is occurring or (ii) limited
motion with altered hindfoot mobility causing increased stress across
involved joints. In either case, bone scan often shows increased uptake
in the area of the tarsal coalition. Children with syndromes such as
Apert syndrome have multiple coalitions and generally decreased
activity to a level where symptoms of the coalitions are limited.
limited subtalar motion is the hallmark of tarsal coalition and
peroneal spastic flatfoot. Frequently, an insidious onset of aching
pain over the medial aspect of the foot in the talocalcaneal coalition,
and the sinus tarsi in the calcaneonavicular coalition, is present.
Pain is generally aggravated by activity and relieved by rest. Ankle
spraining associated with this is common. The flatfoot deformity
present is often severe and progressive in a child who has previously
had an intact longitudinal arch. Rigidity is because of restriction of
subtalar motion, so that the foot cannot be inverted as in the normal
physical examination. When the patient rises on tiptoes, the hindfoot
does not invert into its normal varus position (253) (Fig. 30.38).
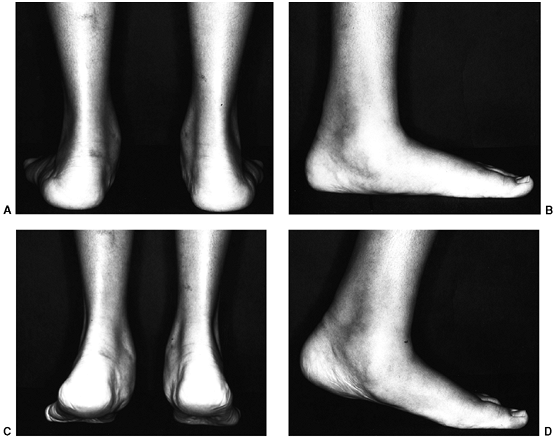 |
|
Figure 30.38 A, B: Rigid flatfoot. C, D:
The arch will not elevate, and the hindfoot valgus will not correct to varus during toe standing, because of immobility of the subtalar joint. (From Mosca VS. Flexible flatfoot and tarsal coalition. In: Richards B, ed. Orthopaedic knowledge update: pediatrics, Rosemont, IL: American Academy of Orthopaedic Surgeons, 1996:211, with permission.) |
flatfoot, can also be seen with juvenile rheumatoid arthritis, bone
lesions of the talus, calcaneus or midfoot, and trauma. Ruling out
arthritis and the other causes of rigid flatfoot deformity is mandatory.
of the foot. The failure of segmentation of the tarsal bones in their
cartilaginous state results in a cartilaginous bridge, which
progressively ossifies forming a synostosis with age. On a standing
lateral view, an elongated process of the calcaneus to navicular can be
seen as the “anteater’s nose” (254) (Fig. 30.39B). Radiographic findings of talocalcaneal coalition include the C-sign (Fig. 30.40) as a line formed from the outline
of the talar dome extending around the inferior margin of the
sustentaculum tali. This has been thought to be a reliable indicator of
talocalcaneal coalition; however, Taniguchi et al. (255)
found the C-sign to have low sensitivity, meaning that the diagnosis of
tarsal coalition is not negated by the absence of a C-sign. Brown et
al. (173) found the C-sign to be specific for a
flatfoot deformity but neither sensitive nor specific for the diagnosis
of subtalar coalition. Liu et al. (256) found
that the absent middle facet was a more accurate sign in the diagnosis
of a subtalar coalition than either talar beaking or the C-sign (Fig. 30.40).
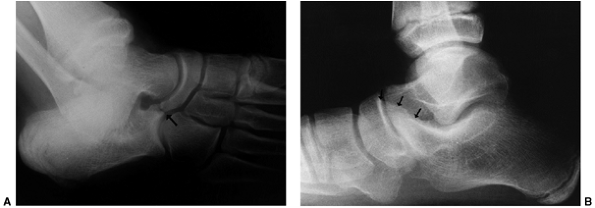 |
|
Figure 30.39 A: A calcaneonavicular coalition (arrow) is best seen on an oblique radiograph of the foot. B: Lateral radiograph demonstrating the anteater nose sign (arrows), indicating a calcaneonavicular coalition.
|
anterior and posterior radiograph of the ankle should be obtained. A
ball-and-socket ankle may be seen in cases of long-standing tarsal
coalition (257,258).
showed that MRI was nearly as good as the “gold standard” CT imaging
for subtalar coalition. In cases where diagnoses such as bone lesions
of the hindfoot or midfoot are considered in the differential
diagnosis, an MRI is indicated rather than a CT scan. While MRI should
not be the first-line study, it can also identify possible fibrous
coalitions (262). Bone scan can also help in identifying the cause of foot pain with an atypical history or pain pattern (260).
Because a rigid flatfoot deformity can result from infection or other
inflammatory disease as well as bone lesions, a laboratory work-up
including a complete blood count (CBC) with differential, sedimentation
rate, C-reactive protein, ANA, and rheumatoid factor may be warranted.
Rheumatologic evaluation in difficult cases with adjacent joint space
narrowing may be helpful as well.
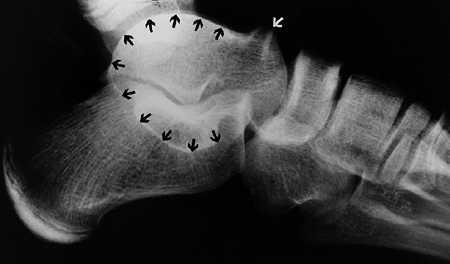 |
|
Figure 30.40 A dorsal talar beak (white arrow) in a foot with a talocalcaneal coalition. This represents a traction spur, not degenerative arthritis. The C-sign of Lefleur (black arrows) is a nonspecific indication of a talocalcaneal coalition.
|
 |
|
Figure 30.41
Talocalcaneal coalitions are best seen on computed tomography (CT) scans taken in the coronal plane. The middle facet is narrow, irregular, and down-sloping. (From Mosca VS. Flexible flatfoot and tarsal coalition. In: Richards B, ed. Orthopaedic knowledge update: pediatrics, Rosemont, IL: American Academy of Orthopaedic Surgeons, 1996:211, with permission.) |
of the foot are separate in infancy in 99% of individuals. Lack of
segmentation of the cartilaginous anlage occurs in some cases, and it
is possible that a fibrous connection between bones undergoes
metaplasia to cartilage (syndesmosis to synchondrosis) and finally to
synostosis (238,263,264).
A coalition alters the normal movement of the subtalar complex in gait.
When rotation and gliding are eliminated by the tarsal coalition,
increased force is concentrated across the talonavicular,
calcaneocuboid, and subtalar joints (265). The
altered motion may lead to degenerative changes in joints over time as
the stresses on cartilage may exceed tolerable limits. Another possible
etiology for symptoms is a stress fracture through the tarsal
coalition. This would account for the large number of individuals who
become symptomatic in adolescence when size and ossification
concentrate stress in the coalition. It is possible that this relates
to ligament sprain, peroneal muscle spasm, irritation of the sinus
tarsi, and irritation of adjacent joints in addition to the arthritis
and stress fracture previously mentioned (236). In general, however, the cause of the pain remains unknown (238,248).
about 25% of individuals with tarsal coalitions become symptomatic. The
onset of pain coincides with the progression of the fusion of the
coalition. This generally occurs between 8 and 12 years of age for
calcaneonavicular coalitions and between 12 and 16 years of age for
talocalcaneal coalitions. As the feet become symptomatic, progressive
valgus deformity of the hindfoot, flattening of the longitudinal arch,
and restriction of subtalar motion occur (251, 253, 254, 257, 258, 259, 260, 262, 263, 266).
restoration of motion. The specific goal of reestablishment of the
longitudinal arch is less clear. Treatment is indicated only for
symptomatic tarsal coalitions (238,257,267). It is not clear that an asymptomatic tarsal coalition with mild restriction would benefit from a surgical excision.
diagnosis of tarsal coalition, attempts should be made to relieve
symptoms by nonoperative means including activity modification,
nonsteroidal antiinflammatory drugs, shoe inserts, and cast
immobilization in a below-knee walking cast. Pain may be eliminated
rapidly following cast application, and as many as 30% of patients
remain pain-free after cast removal following 6 weeks of immobilization
(263). However, Saxena et al. (268)
found that patients who underwent tarsal coalition excision reached
levels of activity beyond the level reached by a matched group of
patients forgoing surgical excision, questioning the wisdom of a
nonoperative approach in the marginally symptomatic patient.
disabling symptoms include resection of the coalition, osteotomy, and
arthrodesis. This chapter will first consider these options applied to
the calcaneonavicular coalition first described by Badgley (269)
in 1927. In this procedure, the coalition is excised and an
interposition material inserted to prevent refusion between the
calcaneus and the navicular. The extensor digitorum brevis as an
interposition material improved outcome, preventing recurrence of the
fusion and providing relief from long-term pain (270, 271, 272).
The presence of a talar beak is not indicative of degenerative
arthrosis and is not by itself a contraindication to resection (273, 274, 275, 276).
Prior to resection of a calcaneonavicular coalition, one should ensure
that a second coalition is not present by analysis of a CT scan of the
hindfoot. The absence of degenerative changes in the talonavicular
joint and calcaneocuboid joint should be ensured. Significant
degenerative arthritis is a contraindication to surgical excision.
Cooperman et al. (277) demonstrated significant
variation in the extent of the fusion of the anterior aspect of the
calcaneus with the navicular. In his analysis of 30 specimens, the
anterior facet of the subtalar joint was totally spared in 8. The
anterior facet was partially replaced in 7 of 30 specimens and
completely replaced in 15. This variation in the anterior portion of
the subtalar joint, related to calcaneonavicular coalitions, may result
in some variation in outcome and certainly relates to the extent and
depth of the resection required to adequately treat this problem.
Failure to resolve symptoms with excision is often related to
inadequate resection at the time of the primary procedure with respect
to depth and breadth of this osseous fusion. A CT scan analysis of the
relation of the anterior facet of the subtalar joint to the calcaneal
navicular coalition will assist in surgical planning.
coalitions are a bit less clear and more complicated. The coalition is
located on the medial side, or tension side, of the valgus foot
deformity, and resection of a portion of the subtalar joint may lead to
further collapse into the valgus. It is stated that resection should
not be done if more than 50% of the subtalar joint surface is involved
with the coalition (273). Wilde et al. (276)
reported unsatisfactory results of resection in feet with a ratio of
the surface area of the coalition to the surface area of the posterior
facet greater than 50%, on the basis of CT scan evaluation. Luhmann and
Schoenecker (278) reported that there were good
postoperative results in feet with valgus deformities of less than 21
degrees but with posterior facet involvement of more than 50%. However,
valgus abnormality in excess of 21 degrees required postoperative
bracing and had compromised results. Many feet with poor outcomes have
narrow posterior facet or impingement of the lateral process of the
talus on the calcaneus. The resection of the talocalcaneal coalitions
therefore remains more controversial, and further study is required for
redefining the indications for resection.
a contraindication to resection, but this diagnosis may be difficult to
make. Talar beaking (Fig. 30.40) is not a sign of degenerative arthritis and not a contraindication to resection (273, 274, 275, 276). Successful resection and interposition in talocalcaneal coalition and calcaneonavicular coalitions have been
found to occur in up to 90% of cases at 10-year follow-up. Interposition materials in the talocalcaneal coalitions include fat (273,279) or a split portion of the flexor hallucis longus tendon (280).
Documented degenerative arthrosis with persistent and recurring pain
after coalition, particularly in adults, represents an indication for
arthrodesis (236). This may be either a triple arthrodesis or a subtalar arthrodesis (281),
depending on the joint and extent of involvement. Osteotomies to
improve realignment remain an alternative to arthrodesis, and the
medial closing wedge osteotomy of the calcaneus or sliding osteotomy to
treat severe valgus deformity should be considered (279,282).
Another surgical procedure that should be considered in feet with some
mobility is the calcaneal lengthening procedure described by Evans; it
can be used following resection of an osseous coalition of the middle
facet in select cases. Although long-term studies are not documented
for this procedure, recognized problems with long-term outcome of
triple arthrodesis are well recognized and alternatives should be
sought (188,226,227,232).
characterized by lateral deviation of the great toe with prominence of
the first metatarsal head medially. The apex of the deformity is at the
first metartarsal phalangeal joint and it is often associated with a
flatfoot, more commonly in women.
unknown. It is more common in girls than in boys, with girls accounting
for more than 80% of cases. Usually there is a strong family history,
with most patients inheriting the deformity from their mothers (283, 284, 285, 286, 287). Coughlin and Roger (288)
found a positive family history of bunion deformity in nearly three
fourths of patients reported in his series. No inheritance was present
in 70% of cases (288,289).
The Mendellian inherence pattern of juvenile hallux valgus has been
proposed to be X-linked dominant or autosomal dominant with very
variable penetrance (290,292).
As in many cases where complex inheritance patterns are present, it has
been described as a polygeneic or multifactorial inheritance pattern as
well. The cause of hallux valgus deformity is both extrinsic and
intrinsic. Studies of hallux valgus in children who wear shoes compared
to those who do not show an increased risk with footwear (152,292).
However, most evidence leads to the conclusion that juvenile hallux
valgus is a deformity negatively influenced by constricting footwear
but usually secondary to a structural abnormality of the foot (288,289,293).
factor for the development of hallux valgus, as well as its recurrence
following surgical correction, by a number of authors (284,294,295).
However, others feel that flatfoot deformity does not predispose to the
occurrence of juvenile hallux valgus deformity. Coughlin and Roger (288), Kilmartin and Wallace (296), and Canale et al. (285)
found no correlation between pes planus and the rate of success with
surgical correction. The relation between the length of the first
metatarsal and the development of hallux valgus has been studied as
well. Excessively long first metatarsal (284,288,297) and a short metatarsal (298) have been implicated in the incidence and severity of juvenile hallux valgus. However, Coughlin and Roger (288)
have shown that the lengths of the first and second metatarsal in
children with adolescent bunions are similar to those in a healthy
population.
which is defined as an intermetatarsal angle between the first and
second rays of greater than 10 degrees, and juvenile hallux valgus. The
cause of the varus deformity of the first metatarsal may lie in an
abnormal cuneiform–first-metatarsal articulation. The distal articular
surface of the first cuneiform is normally transverse; however, an
oblique orientation of this joint may predispose to a varus deformity
of the first metatarsal (295). The second angle
that is important in quantifying the hallux valgus deformity is the
hallux valgus angle defined by Hardy and Clapham (289). This angle is measured by the intersections of the longitudinal axis of the proximal phalanx and the first metatarsal (Fig. 30.42). The normal hallux valgus angle is less than 16 degrees (299).
the quantification of the juvenile hallux valgus deformity is the
lateral deviation of the articular surface of the first metatarsal. The
distal metatarsal articular angle (DMAA) quantifies this alignment (Fig. 30.43) (288,290,300,301). The higher the DMAA, the greater the valgus deformity of the distal metatarsal articulation. Coughlin and Roger (288)
reported a 48% incidence of juveniles with hallux valgus having an
increased DMAA and a congruous first metatarsal phalangeal joint,
significantly greater than in adults (300). He noted that the DMAA was significantly higher in patients with positive family histories and early onset of hallux valgus.
tendons and sesamoids sublux laterally; the adductor of the great toe
inserting on the proximal phalanx increases the deformity, and finally,
once the hallux valgus deformity is present, the abductor hallucis with
its plantar insertion on the proximal phalanx has no ability to abduct
the great toe.
and the mild pressure present over the metatarsal head medially can be
relieved by proper shoe fitting. When pain is present, it is generally
directly over the medial prominence of the first metatarsal head, as
well as overlapping of the second toe over the laterally deviated great
toe. Intraarticular pain and arthritis are rare in juvenile hallux
valgus. Restriction of motion at the metatarsal phalangeal joint is
also rare.
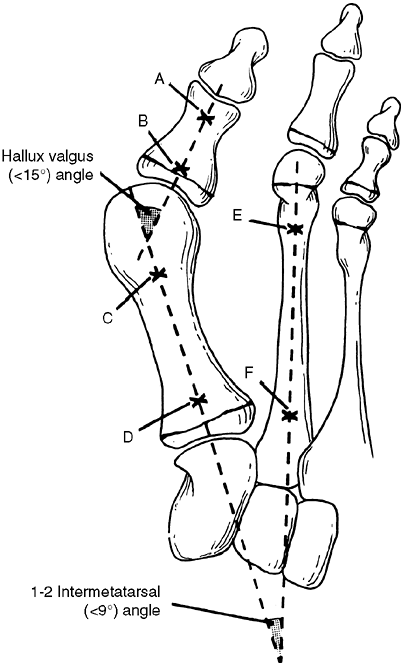 |
|
Figure 30.42 Hallux valgus and first-second intermetatarsal angle. A-B axis of proximal phalanx; C-D axis of first metatarsal; E-F axis of second metatarsal. (From Coughlin M. Juvenile hallux valgus. In: Coughlin M, Mann R, eds. Surgery of the foot and ankle, 7th ed. St. Louis, MO: Mosby, 1999:270, with permission.)
|
bilaterally in women with positive family history. In cases of
unilateral deformity in a woman with a negative family history, be
aware of other causes of muscle imbalance that might lead to a bunion
deformity. Examples of these are central nervous system lesions such as
cerebral palsy, spinal dysraphism, or other spinal cord abnormality,
and peripheral nerve lesions.
deformity, particularly with tight Achilles tendon. Also look for other
causes of pain surrounding the metatarsal phalangeal joint such as
arthritis, inflammation, or lesions of local soft tissue or bone.
foot are necessary in order to evaluate hallux valgus. First, the
overall alignment of the foot should be documented on standing views,
measuring calcaneal pitch and the first metatarsal to long axis of the
talus (Meary angle) on the lateral view. With respect to the bunion
deformity, the hallux valgus angle, the intermetatarsal angle and the
DMAA should be measured. Look for metatarsal phalangeal joint congruity
and relative lengths of the first and second metatarsal. An abnormality
of the proximal phalanx with trapezoidal shape or an abnormal
interphalangeal joint may be present with hallux valgus. Cadaver study
by Vittetoe et al. showed that the intraobserver reliability of DMAA
measurement was high, and interobserver reliability was poor (302).
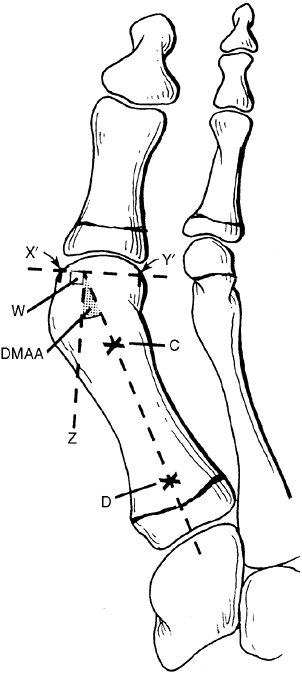 |
|
Figure 30.43
The distal metatarsal articular angle (DMAA) quantifies the angular relation between the articular surface and the shaft of the metatarsal. The DMAA is the angle between the metatarsal shaft (C-D) and the line (W-Z) that is perpendicular to the articular surface (X’-Y’). (From Coughlin M. Juvenile hallux valgus. In: Coughlin M, Mann R, eds. Surgery of the foot and ankle, 7th ed. St. Louis, MO: Mosby, 1999:270, with permission.) |
believed that congruous joints with juvenile hallux valgus were stable
and less likely to progress than those with subluxations. Congruous,
laterally deviated metatarsal phalangeal articulation is much more
common in children than in adults. A congruous first metatarsal
phalangeal joint is found in 9% of adults (300) but in 47% of juvenile patients with bunions (288).
complain of deformity, or pain, or both. There is an assumption on the
part of many patients and parents that prompt treatment of
the
deformity will resolve and cure this problem. This approach—early
correction of the deformity to alleviate the potential for long-term
difficulty—has no role in management of hallux valgus deformity. In
pediatric orthopaedics, we often try to correct deformities early, in
order to keep them from becoming significant problems in the future;
not so for bunions. This “hands off” approach is counterintuitive, both
to patients and their parents. Pain is the primary indication for
treatment of hallux valgus deformity rather than malalignment, because
of the significant recurrence rate. Perhaps there is a role for early
conservative management with night splinting to prevent progressive
bunion deformity. This opinion is based on the work of Groiso (286),
who reported a 50% success rate in night splinting, using an orthoplast
precut splint, holding the great toe in an abducted position at night.
His series included 56 children with 2- to 6-year follow-up. Half the
children showed significant improvements in the metatarsal phalangeal
angle and the intermetatarsal angle. A contrary view was expressed by
Kilmartin et al. (303), who found that hallux
valgus deformity increased more in patients who used splints than those
who did not. The pillar of conservative management is finding shoes
that fit appropriately and have a widened toe box. The upper portion of
the shoe should be soft, and an arch support can be used to decrease
the tendency for pronation of the foot.
alteration of footwear, and a significant change in activity is
required in a child. The age of the patient at the time of surgery is a
significant consideration. Poor results with high complication rates
have been reported consistently in 30% to 60% of young children who
have had hallux valgus surgery (273, 304, 305, 306, 307). The results have been attributed to a number of factors, including further epiphyseal growth causing progressive deformity (283),
growth arrest of the proximal first metatarsal and proximal phalanx,
and return of the proximal phalanx to its position of congruent
articulation. The return of the great toe to a position of congruent
articulation with increasing bunion deformity is a particularly
significant problem in patients with an elevated DMAA. Coughlin and
Roger (288) and others (307)
have, however, performed successful surgical reconstructions with low
complication rates in adolescents with open growth plates. The authors
stress that if possible, surgery should be delayed until the end of
growth.
distal soft tissue realignment (McBride procedure), metatarsal
osteotomy (either proximal or distal), and attention to the DMAA.
valgus should not be aggressive, because a large protuberant medial
eminence is rarely seen in children.
isolation because recurrent deformity will uniformly result. In the
face of a subluxed metatarsal phalangeal joint, soft tissue realignment
may be valuable. In addressing soft tissue abnormalities, medial soft
tissue realignment generally involves a VY reconstruction of the medial
capsule, as well as a lateral release of the adductor tendon. With soft
tissue realignment as an isolated procedure without osteotomy, there is
a 50% to 75% recurrence rate in adolescents (284,288). Hallux varus has also been reported following this procedure (308,309). Therefore, soft tissue repair alone has been abandoned.
hallux valgus deformity. The osteotomies may be the distal first
metatarsal as used in a chevron or Mitchell type osteotomy, the
proximal first metatarsal, or the medial cuneiform. In order to make
the decision of where to do the procedure, radiologic evaluation is
required. For the congruous metatarsal phalangeal joint, a distal
osteotomy may be used to correct the DMAA, whereas a proximal
metatarsal osteotomy or medial cuneiform osteotomy is used to correct
the metatarsus primus varus (290,310) (Fig. 30.44).
In some cases, an additional osteotomy at the base of the proximal
phalanx is required. If the intermetatarsal angle is less than 15
degrees, a simple distal osteotomy, either Mitchell or chevron, can be
used. Standard uniplanar chevron or Mitchell osteotomies do not correct
the DMAA. Translating the metatarsal head laterally and correcting the
angular deformity can be done with effort, using internal fixation with
K-wires to maintain angular correction of the distal fragment and
correction of the DMAA (283, 285, 290, 304,306, 311, 312, 313, 314).
Minimal lateral soft tissue release should be combined with distal
metatarsal osteotomy because of the risk of avascular necrosis (315).
reported 31% of patients in their series with a fair or poor outcome;
the less than satisfactory results related primarily to poor position
of the displaced distal fragment, resulting in recurrent deformity, or
plantar angulation resulting in transfer lesions to the second
metatarsal head. Such problems can be decreased with appropriate use of
internal fixation.
osteotomy, have been reported, with positive outcomes ranging from 81%
to 95% (66,283,311,316).
Positive outcome from this osteotomy related to preserving the length
of the first metatarsal and never dorsiflexing the metatarsal head
while stabilizing the osteotomy with a screw or K-wire.
effective in managing a bunion deformity with an intermetatarsal angle
of less than 15 degrees is the chevron osteotomy. The chevron (314)
osteotomy is a transverse osteotomy through the distal portion of the
metatarsal with a chevron shape. The apex of the chevron osteotomy is
at the midportion of the metatarsal head, and the angular limbs
transverse the cortex of the metatarsal, proximal to the capsular
insertion (317). Good results from this osteotomy have been reported by Zimmer et al. (314)
in 85% of adolescents despite a recurrence rate of 20%. The
intrinsically stable osteotomy avoids the problem of metatarsal
shortening. The DMAA can be corrected by angulating the distal
articular surface.
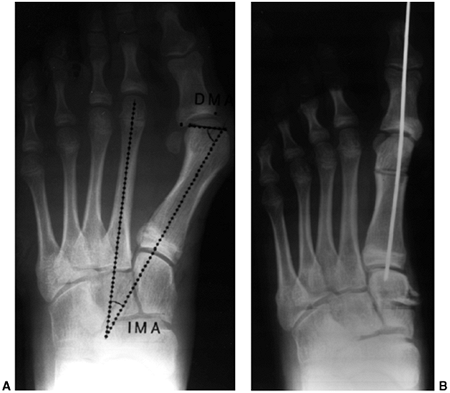 |
|
Figure 30.44 A: Preoperative radiographs of juvenile hallux valgus. IMA, intermetatarsal angle. B: Radiograph after medial cuneiform opening wedge osteo-tomy and distal first metatarsal closing wedge osteotomy. (A from Mosca VS. Ankle and foot: pediatric aspects. In: Beaty J, ed. Orthopaedic knowledge update 6. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1999:583.)
|
If the medial cuneiform distal surface is angulated, an opening wedge
osteotomy through the cuneiform can be done. Peterson and Newman (310)
described a two-level osteotomy for adolescent bunions doing a closing
distal medially based osteotomy with an opening proximal-based
metatarsal osteotomy in which the length of the metatarsal is
preserved, the varus deformity corrected, and the DMAA properly aligned.
the management of bunion deformity in children. Occasionally, an Akin
osteotomy, which is a medial closing wedge of the proximal phalanx (318),
may be used to improve the alignment of a toe in which the metatarsal
alignment is proper and the DMAA appears satisfactory. Hallux valgus,
therefore, should be corrected where the deformity lies. In the
presence of cerebral palsy, bunion deformities are quite common, both
dorsal bunions and hallux valgus. Because of exceedingly high
recurrence rates, fusion of the first metatarsal phalangeal joint is
the procedure of choice (319, 320, 321).
conservative treatment with night splinting and observation.
Appropriate footwear should always be encouraged. Surgical treatment
should be delayed until the end of growth if possible, and the
procedure chosen should treat the deformity present in a given case.
There is no indication for isolated soft tissue repair in the juvenile
bunion deformity.
present at birth, in which the fifth toe is adducted, dorsiflexed, and
medially deviated, generally lying over the metatarsal phalangeal joint
of the fourth toe (Fig. 30.45).
mild forms of the disorder are present in an asymptomatic state, below
the threshold for treatment. There is no sex predilection. In 20% to
30% of cases, bilateral involvement is present (322, 323, 324).
to some degree the fourth toe and fourth metatarsal phalangeal joint.
The interphalangeal joints are normal. The skin tends to be contracted
a bit dorsally and medially, but there is no stress or abnormality on
the skin.
to determine whether or not the metatarsal phalangeal joint is subluxed
or dislocated prior to surgical treatment.
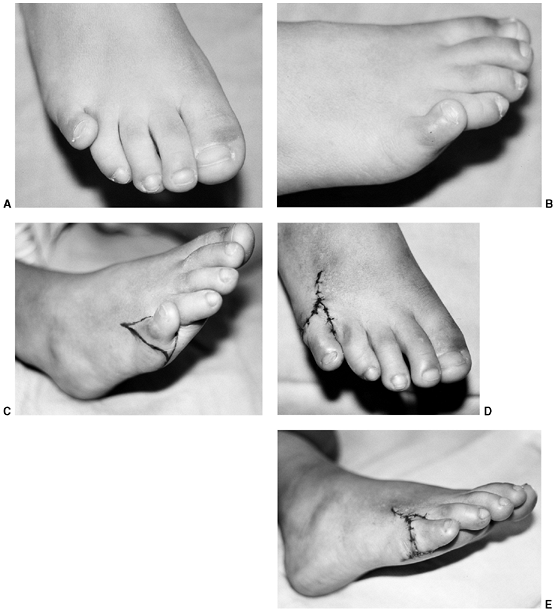 |
|
Figure 30.45 A, B: Congenital overriding fifth toe. C–E: The Butler procedure for congenital overriding fifth toe. Double racket-handle incision with dorsal Y-to-V advancement.
|
fifth metatarsal phalangeal joint, but the toe is not a clawed toe.
Flexion deformity of the interphalangeal joint does not occur.
Shortening of the extensor tendons of the fifth toe is generally
present and must relate to the dorsal position of the toe. The entire
toe is translated proximally and medially.
uncertain, but it has been stated that approximately half of affected
individuals will experience symptoms from this deformity, generally
from shoe wear (323).
taping of the toe, it may be of benefit to patients in whom the
deformity is somewhat mild. Education about the reasonably good
prognosis of the untreated state is worth pursuing; however, in the
case of a committed family with a patient having mild deformity, taping
may be of value. In taping, a loop of standard adhesive tape is brought
around the toe and it provides a plantar tether to the toe.
overlie the metatarsal phalangeal joint just at the point where the shoe fold will lie.
this, including partial or complete excision of the proximal phalanx
and syndactylization to the fourth toe (325). Only fair results have been reported with this approach, and secondary deformities persist in many cases (325). Amputation is only a salvage procedure. The Butler procedure (322,324) originally reported by Cockin (323)
is a very successful approach for the management of this condition. A
racket-handle incision is made to release the contracted soft tissues
dorsally and medially, mobilize the neurovascular bundles, and free the
toe for translation. The toe is then translated plantarlaterally.
Although there is a risk of neurovascular compromise, this is very
infrequent. Plantar skin reconstruction with a VY advancement resolves
the problem of the soft tissue tether. If the toe spontaneously
subluxes, further release of the dorsal capsule and dorsal soft tissues
should be done, and the toe can be pinned in position across the
metatarsal phalangeal joint at the time of the soft-tissue
reconstruction.
more of the toes are flexed and have a varus deformity, generally with
lateral rotation through the interphalangeal joints, causing the toe to
curl and lie under the adjacent or more medial toe (Fig. 30.46).
incidence is not known. It is very frequently bilateral and symmetric,
with high familial incidence (326,327).
 |
|
Figure 30.46
The curly toe deformity generally results from a tight toe flexor as seen in the third toe in this patient. Another possible etiology is an abnormally shaped phalanx that may result in fixed deformity and require osteotomy or fusion for correction of persistent deformity. |
The distal phalanx or the distal and middle phalanges are pulled under
the adjacent medial toe with flexion, varus, and external rotation of
the distal and proximal phalanges. The nail plate of the affected toe
often faces laterally. If the deformity is magnified when dorsiflexion
of the foot and the MP joint tighten the flexor tendon of the toe, the
primary pathologic structure causing the deformity is probably the toe
flexor. This can be confirmed by showing that the deformity can be
decreased by plantar-flexing the foot and ankle, thereby relaxing the
toe flexor.
Joint capsules are generally not affected. Occasionally this deformity
results from a trapezoidal deformity of the bone, and the curly toe
deformity is unrelated to flexor tendon but secondary to structural
abnormality of the toe.
They may become symptomatic in older children, adolescents, or adults,
because of exaggerated pressure on the skin and nails of malaligned
toes. The nail of the underlying toe often cuts the plantar surface of
the overlying toe, causing symptoms.
but may work in mild cases. The family may be educated that, in
general, symptoms are rare and long-term disability is unlikely. Some
patients do experience continued pain and problems from curly toe
deformity. If associated with a tight toe flexor, stretching exercises
might be of benefit. Prior to embarking on surgical treatment, an
attempt at correction of a tight tendon may be of value. Surgery is
indicated if there are callosities and cutting of one toe into the
other, secondary to this deformity. Another indication is an
unacceptable problem with nail deformity.
A double-blind, randomized prospective study comparing simple tenotomy
of the long toe flexor to Girdlestone-Taylor transfer showed no
difference in outcome (329). In this study, 19
patients with bilateral deformity involving the third and fourth toes
were operated on, using a flexor tenotomy release on one side and a
flexor tenotomy with flexon transfer procedure on
the
other. At 4-year follow-up, it appeared that there was no difference
between the two procedures and that simple tenotomy of the flexor
tendon is sufficient treatment for the symptomatic curly toe.
medial enlargement of the tarsal navicular beyond its normal size. A
separate bone, either in the posterior tibial tendon (such as sesamoid
bone) or with a true articulation with the navicular, is within the
breadth of this diagnosis. Other terms that have been used to describe
the separate ossicle are the os tibiale externum, the navicular
secundum, or the prehallux (Fig. 30.47).
accessory bone in the foot, occurring in between 4% and 14% of the
population (162,330,331). It is frequently bilateral and occurs more commonly in women. Geist (331) recognized a higher incidence of accessory naviculars in young patients evaluated radiologically than in cadaver studies.
suggested that three possible situations accounted for the accessory
navicular: (i) bone within the substance of the posterior tibial tendon
as a sesamoid bone, (ii) bone with a true articulation (synovial-joint)
with the navicular and (iii) a synchondrosis.
 |
|
Figure 30.47 Accessory navicular. A: Type I. B: Type II. C: Type III.
|
adolescents. There is a firm prominence distal to the talar head on the
plantar medial aspect of the midfoot. This may be associated with
flexible flatfoot (333, 334, 335, 336).
The accessory navicular, however, is a primary abnormality in the
navicular and posterior tibial tendon relationship and is not related
to flexible flatfoot (337). The prominence of
the navicular is associated with point tenderness; it can be
differentiated from the prominence of the talar head in a flatfoot
deformity by inverting and everting through the subtalar joint with a
thumb over the bony prominence.
should have standing anteroposterior and lateral radiographs in order
to define the abnormality of the navicular. Bilateral films may be
indicated, as there is a high incidence of symmetrical abnormalities.
to foot pain, or perhaps an associated abnormality not related to the
clinical disorder with which the patient presents for evaluation.
Therefore, careful examination differentiating other causes of foot
pain is mandatory. Patients with accessory navicular may present with
complex pain patterns requiring very careful examination prior to
treatment (338). They may even have a peroneal spastic flat foot.
radiographs of the foot are diagnostic of accessory navicular. There
are three types of accessory navicular (339) (Fig. 30.47). In type I accessory navicular, which is rarely symptomatic, a small sesamoid bone is located in the posterior
tibialis tendon. Type II accessory navicular is the most frequently
symptomatic type, which is a bullet-shaped ossicle joined to the
tuberosity of the navicular by a synchondrosis. Type III is a large
horn-shaped navicular, which most likely is the result of fusion of a
type II accessory navicular with the progress of age.
with growth of fibrocartilage and evidence of bone turnover, in the
tissue between the ossicle and the main body of the navicular in the
painful type II accessory navicular (339).
These histologic findings are consistent with healing microfracture or
a chronic stress fracture, substantiating the opinion that repetitive
stress leads to this injury. There is a possibility of finding
inflammatory cells at some stage in the healing process, but the
primary pathology is associated with healing microfracture rather than
chronic inflammation.
If symptoms do occur, a period of protection from stress and injury
generally returns the patient to the asymptomatic state (335).
relieves symptoms. Pain is related to a state similar to that seen in
stress fracture or Osgood-Schlatter disease. The decrease in direct
pressure over the accessory navicular, as well as decreasing stress
from the posterior tibial tendon insertion, may result in relief of
symptoms. This can be done with an orthotic device or arch support or a
soft shoe and a pad placed around the navicular to decrease direct
pressure over it. Finally, the patient can be given a short leg cast to
decrease symptoms by decreasing stress from the posterior tibial tendon
insertion.
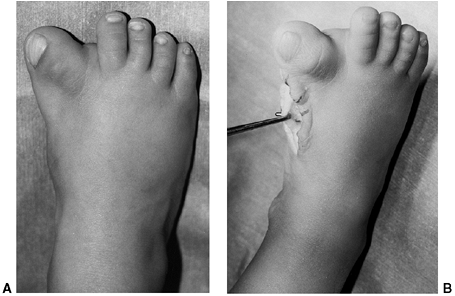 |
|
Figure 30.48 A: Clinical appearance of congenital hallux varus. B: Fibrous band between the hallux and the cartilaginous duplicate tarsal anlage.
|
immobilization, surgery is indicated. There are two possible operations
for treating the accessory navicular. The first is simple excision of
the ossicle and the expanded portion of the navicular through a
tendon-splitting approach (331, 332, 333, 344).
In this procedure, the skin incision should be made dorsal to the
prominence of the accessory navicular. The bone is removed to a point
where the medial foot has no bony prominence over the navicular,
between the head of the talus and the first cuneiform. This generally
requires removing the accessory navicular as well as a prominent
portion of the navicular. Symptoms are relieved in 90% of cases by this
procedure.
in which the posterior tibial tendon is advanced along the medial side
of the foot with the hope of supporting the longitudinal arch. In this
procedure, the ossicle and the prominent medial aspect of the navicular
are excised, just as in the simple excision procedure, but the
posterior tibial tendon is advanced. There appears to be no benefit to
the advancement of the posterior tibial tendon relative to the simple
excision procedure (12,340).
great toe on the first metatarsal, present at birth. It occurs as an
isolated deformity but is often associated with other malformations of
the foot, particularly, short first metatarsal; bracket epiphysis of
the first metatarsal, both pre- and postaxial polydactyly; and a
fibrous band that acts as a tether along the medial side of the great
toe, extending to the base of the first metatarsal (Fig. 30.48) (345,346).
associated with a first metatarsal that is short and rounded, leading
to a very abnormal metatarsal-phalangeal articulation and medial
deviation of the great toe with an enlarged web space between the first
and second digit. Healthy growth of the first metatarsal is generally
compromised, and the medial tether leads to recurrence.
This should be differentiated from the medial deviation of the great
toe, which is a flexible and very common deformity seen in association
with metatarsus adductus. The hallmarks of the congenital deformity are
the fibrous band along the medial side of the foot, the widened web
space between the first and second digit, and the abnormality of the
first metatarsal. Duplication of the great toe with preaxial
polydactyly is quite common, and this may be associated with a complex
syndactyly, as seen in Apert syndrome (243).
be done to assess the varus alignment of the great toe. The deformity
of the first metatarsal can be partially delineated on initial x-ray
films. However, the longitudinal physeal bracket, which may not be
easily seen on initial films, is suggested by a D-shape to the
metatarsal, with no cortical differentiation along the convex medial
border of the epiphysis (347) (Fig. 30.49A).
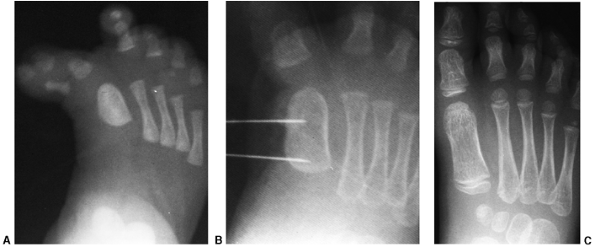 |
|
Figure 30.49 A: Radiographic appearance of congenital hallux varus with a metatarsal longitudinal epiphyseal bracket. B: Pins mark the extent of the resection of the longitudinal epiphyseal bracket. C:
Radiographic appearance 5 years after resection and fat grafting of the longitudinal epiphyseal bracket. The metatarsal has grown normally. |
the origin of the deformity is related to preaxial polydactyly or
duplication of the great toe. The more medial extra digit degenerates
into a fibrous band, rather than fully forming a digit with a
corresponding metatarsal. The rudimentary medial structure then forms a
fibrous band that acts as a bowstring, pulling the hallux into a varus
position (348) (Fig. 30.48B).
growth disorder leading to progressive relative shortening of the first
metatarsal occurs, unless addressed.
Mild forms of hallux varus with a flexible deformity generally resolve
spontaneously, but that condition should be differentiated from
congenital hallux varus.
deformity. Surgical management is indicated with the specific
procedures to be done depending upon the anatomy in the individual
case. The issues to be considered are correction of polydactyly if
present; correction of the soft tissue tether on the medial side of the
foot and the enlarged web space between the great and second toe;
correction of metatarsal-phalangeal joint incongruity; and correction
of metatarsal or bracket epiphyseal deformity (349).
because of shortness of the first metatarsal and growth disorder. In
the soft tissue reconstruction of this deformity, which is part of any
surgical procedure, lengthening the medial tether is mandatory. This
requires resection of the fibrous band as well as Z-plasties in the
skin to increase the length along the medial side of the foot. The
abductor hallucis must be released and the tether on the capsule must
also be released.
toe is resected and the medial reefing of the capsule done if possible.
The incongruity of the metatarsal phalangeal joint may need to be dealt
with by using a K-wire to hold the great toe in position while
remodeling occurs following surgical reconstruction.
demonstrated that resection and interposition grafting of a
longitudinal epiphyseal bracket is an effective technique to treat
growth disorders resulting from this epiphyseal deformity (Fig. 30.49 B and C).
When the longitudinal portion of the bracket is excised, interposition
material with fat or methylmethacrylate can be used, as with any
physeal bridge resection. This procedure is always combined with a soft
tissue reconstruction and resection of duplication of the digits. An
opening wedge osteotomy may be combined in some cases in which the
extra bone from the toe can be used as part of an opening wedge
osteotomy.
Alternative treatments for pain with residual shortening and deformity
include metatarsal lengthening and amputation. Amputation is a
particularly valuable alternative in the management of severe
congenital hallux varus deformity in Apert syndrome (243).
extra digits are present, with or without duplication of the
corresponding metatarsal. Preaxial polydactyly refers to the medial
side of the foot and postaxial polydactyly to the lateral side of the
foot. Simple syndactyly refers to a failure of separation of otherwise
healthy digits with skin connection only. Complex syndactyly refers to
fusion of bone in the digit or metatarsals in adjacent rays.
is failure of differentiation in the apical ectodermal ridge (AER)
during the first trimester of pregnancy, leading to polydactyly and
polysyndactyly (353). Experimentally, polydactyly can be produced by radiation, cytotoxins, and folic acid deprivation.
classified polydactyly as preaxial if the great toe is duplicated and
postaxial if the duplication involved the lateral side of the foot. The
term “central” may be applied to a duplication of the second, third, or
fourth toe, if this can be differentiated. Phelps and Grogan (353)
in a review of 194 supernumerary toes showed 79% to be postaxial,
whereas 15% were preaxial and 6% central. Considerable variation exists
and more than one type may be present in a single foot (Fig. 30.50).
Syndactyly may accompany the extra digit, and toenails may be fused or
separated. Central and postaxial polydactyly tend to be well aligned,
whereas the preaxial polydactyly may be associated with congenital
hallux varus, short first metatarsal, and longitudinal bracket
epiphysis (347,349).
The classification system is based primarily on metatarsal
abnormalities. The metatarsals are present on radiographic views at
birth, but generally radiographic evaluation is delayed in order to
allow full ossification of the phalanges for surgical planning.
with proper alignment of the digit may remain in place unless the foot
is significantly widened. However, a malaligned toe, particularly
preaxial polydactyly, requires surgical treatment. Lateral or postaxial
polydactyly is generally treated with excision, with the assumption
that this is a relatively simple procedure in infancy and the wide foot
will become a problem with shoe fitting in the future.
 |
|
Figure 30.50 Preaxial and postaxial bilateral polydactyly.
|
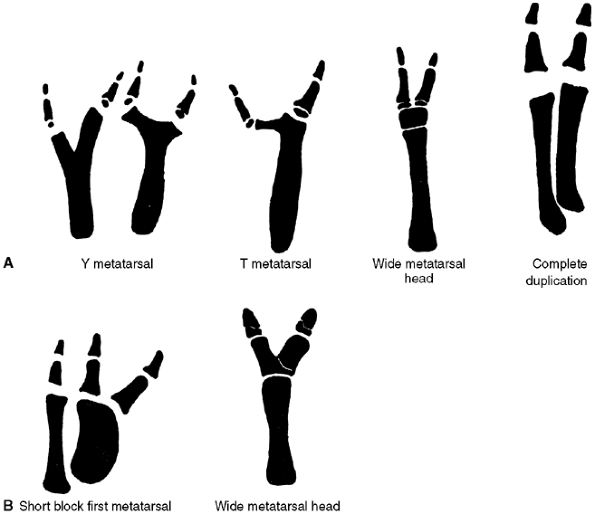 |
|
Figure 30.51 Venn-Watson classification of polydactyly. A: Postaxial. B: Preaxial. (From Venn-Watson EA. Problems in polydactyly of the foot. Orthop Clin North Am 1976;7:909–927, with permission.)
|
Division of a synchondrosis at the base of the proximal phalanx is
quite safe, and growth arrest is highly unlikely. Likewise, an enlarged
metatarsal head may be reduced in size by performing a transphyseal
longitudinal osteotomy (353). In a case with a
duplicated metatarsal or Y-shaped metatarsal, the corresponding
metatarsal abnormality should always be removed at the time of
resection of the extra digit.
phalanges and associated toenail generally are removed through a
racket-type incision (353,356).
The nail fold should be recreated to prevent problems with chronic
ingrown toenail. As polydactyly is often associated with syndactyly, a
decision must be made about reconstruction of both the extra digit and
the syndactyly. In general, the skin bridge between the toes is left in
place and the lateral border digit removed, if surgery is chosen (356).
Postaxial polydactyly generally results in satisfactory outcome with
excellent results. Preaxial polydactyly, on the other hand, is more
likely to result in residual varus deformity, short metatarsal, and
unsatisfactory outcome. Attention to the longitudinal epiphyseal
bracket (347) may result in improved length of
the first ray and should be considered in cases when this deformity is
present with preaxial polydactyly.
involving soft tissue (simple syndactyly), or soft tissue and bone
(complex syndactyly). The most common fused digits are the second and
third, which may be either complete or incomplete (Fig. 30.52).
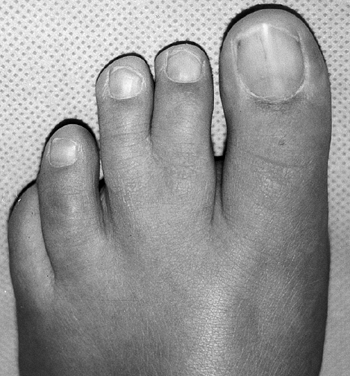 |
|
Figure 30.52 Clinically benign zygosyndactyly.
|
angular abnormality of the digit that causes problems. Occasionally,
differential length of the toes may result in a flexion deformity of
the longer toe and a callus over the proximal interphalangeal (PIP)
joint. Rarely, this may become a problem with pain.
surgical management is planned, in order to differentiate simple from
complex syndactyly.
asymptomatic throughout life, and surgical treatment and adaptive shoe
wear are generally not needed.
syndactyly as comfort and function are not impaired. Given presently
available footwear, which often includes a strap between the first and
second toes, a case can be made for surgical management in select
cases. Caution must be exercised, as the surgical scars may be less
cosmetically pleasing than the condition itself and lead to angular
deviation of digits from contracture, where satisfactory alignment was
present in the preoperative state. Unlike fingers, discriminatory
function of individual digits is not required in the toes, and toe
syndactyly is rarely surgically managed. If toe deformity is occurring
because of differential growth, a case for surgical reconstruction may
be made.
 |
|
Figure 30.53 A: Macrodactyly most commonly involves the second ray; in this case, the first and third are involved to some degree. B: Radiographic appearance demonstrates enlargement of bone as well as soft tissue.
|
both hands and feet. It may involve single digits or the entire hand or
foot. Macrodactyly may occur as part of a syndrome such as Proteus
syndrome (357) or Klippel-Trenaunay-Weber
syndrome (venous lymphatic malformation). Some have described the
condition of macrodactyly as congenital lipofibromatosis. Another term
similarly applied to it is macrodystrophia lipomatosa. Finally, the
findings of macrodactyly may be present in a lymphatic malformation or
in patients with lymphedema. CT scan, MRI, and physical examination
will help to differentiate the above conditions.
large series of patients with macrodactyly, in which they documented
the low incidence of this condition, as well as a male predilection. It
was also determined that the second digit is most commonly involved,
and multiple digit involvement is present in approximately 50% of cases
(Fig. 30.53).
as “macrodactyly.” Features of Klippel-Trenaunay-Webber and
neurofibromatosis should be checked for. In neurofibromatosis, café au
lait spots are frequently apparent. In Proteus syndrome, a cerebriform
skin pattern on the plantar surface of the foot as well as asymmetries
of growth and nevi are present. Surprisingly, in
Klippel-Trenaunay-Webber, a syndrome of venous lymphatic malformation,
ipsilateral macrodactyly is frequently present with a vascular
component, and contralateral macrodactyly is present as a fibro-fatty
disorder. Fifty percent of patients with foot involvement in
macrodactyly have a dorsally angled digit with weak toe flexors (360).
foot are useful for monitoring growth rates of digits and for surgical
planning. MRI (361) is of value in macrodactyly
in order to differentiate cases of vascular malformation in association
with macrodactyly from true fibro-fatty disorders or lymphedema.
tissues in the foot. In general, there is an overabundance of
fibro-fatty tissue, often in a neural distribution. The cause of the
overgrowth remains unknown.
growth throughout the life of the child. It may, however, be
progressive with disproportionate overgrowth compared to healthy digits
(362). The type with progressive overgrowth is more likely (358). It may be disabling, with respect to shoe fitting and the possibility of wearing commercially available shoes.
 |
|
Figure 30.54
Macrodactyly of the foot is most effectively managed by a second ray resection in general. The width of the foot can be reduced by resecting the entire second metatarsal. |
to be individualized and must be recognized to be a long-term
commitment to that child and family. Treatment involves several options
including soft tissue debulking, amputation, and epiphyseodesis. In
general, ray resection of the toe and corresponding metatarsal are the
most satisfactory procedures to use in dealing with this condition of
the foot (363). Toe amputation alone has not
been cosmetically satisfactory, nor has it resulted in significant
improvement of the foot deformity. In mild cases, epiphyseodesis of the
proximal phalanx (364) and of the distal metatarsal, as well as surgical debulking, may be of some value (358, 359, 364, 365, 366, 367).
Ray resection combined with debulking of soft tissue has the best
outcome and lowest risk of recurrent deformity, achieving the goal of
shoe fitting with commercially available footwear in some cases (358,359,367) (Fig. 30.54).
In selecting the timing for epiphyseodesis of the foot, the author
generally uses an x-ray film of the affected child’s parent’s foot in
order to predict the approximate rate of growth of the healthy foot and
therefore timing of epiphyseodesis. Growth charts for the size of the
foot were developed by Green (Fig. 30.1);
however, it is preferable to use the size of the parent’s foot and the
size of the contralateral foot for timing of epiphyseodesis. A
successful ray resection should remove the entire metatarsal. If the
proximal metatarsal is left in place, the space between the first and
second metatarsal remains wide and an unsatisfactory outcome will
result.
necessary in the management of macrodactyly, and the parents should
understand this at the outset of the procedure. The author has found
that debulking procedures in the presence of lymphedema are less
successful than in cases of fibro-fatty type macrodactyly or vascular
malformation.
The much less common form of this condition has an incidence of
approximately 1 per 150,000 live births, in which there is a
spontaneous mutation and no evidence of a familial condition.
Approximately 10% of cleft feet are of this pattern (372). Boys are affected more frequently than girls.
such a defect might be caused by genetic or toxic influence, leading to
an error in differentiation. Such irregularities may lead to
polydactyly or syndactyly or the much more rare central defect of cleft
foot. Watson and Bonde (374) proposed that a
specific region in the AER localized to the second or third ray, which
is the typical area for deficiency in a cleft foot. They further
proposed that the extent of damage to the AER would relate to both the
width and depth of the cleft defect of the foot.
interdigital space to a central ray deficiency or even a monodactylous
foot (375). Associated abnormalities include
cleft hand, cleft lip and palate, deafness, urinary tract
abnormalities, triphalangeal thumbs, and tibial hemimelia.
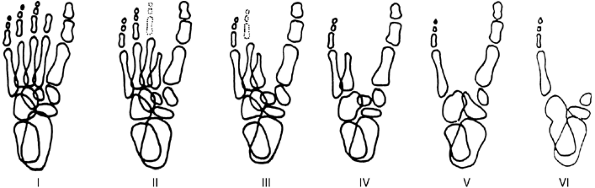 |
|
Figure 30.55
Cleft foot classification according to Blauth and Borisch. (From Blauth W, Borisch NC. Cleft feet. Proposals for a new classification based on roentgenographic morphology. Clin Orthop 1990; 258:41–48, with permission.) |
The classification system is based on the extent of bony deficiency of
the central rays, culminating in a foot with a nearly absent medial ray.
foot: the monodactylous foot with a single ray, and a tibial diastasis
with central ray deficiency of the foot. Other variations include cross
bones and synostosis (Fig. 30.56). Radiographs
of the foot should be taken at presentation in order to classify the
deformity appropriately. Other diagnostic studies include renal
ultrasonography as indicated to rule out renal abnormalities as they
are frequently associated with cleft foot.
Often a hallux valgus results from the pull of a conjoined flexor and
extensor, resulting in an abductor as a component of this deformity.
regular shoes without pain or compromise of function. For such
individuals, no surgical treatment may be required. However, in many
cases of cleft feet there is a marked increase in width (Fig. 30.57),
which prevents normal shoe fitting. Painful callosities develop over
the medial and lateral metatarsal heads. A severe hallux valgus is
frequently present, secondary to a conjoined flexor extensor tendon.
the ability to wear a standard shoe without pain and with good
function. A secondary goal is reconstructing the foot to a socially
acceptable appearance. Surgical repair is recommended for feet in which
a significant improvement can be
made
in the shape of the foot, facilitating shoe wear and improving
function. In recommending surgical repair, it should be remembered that
most cleft feet can function quite well without repair. Bony
prominences, medially and laterally, cause pain because of direct
pressure from footwear, rather than pain from walking. Wood et al. (376)
recommended surgical therapy for closure of a cleft foot, in which soft
tissue is reconstructed by a series of rectangular flaps. The flaps are
approximated and metatarsal osteotomies performed. Their reported
experience was of 42 operations in 15 affected feet that were felt to
warrant surgical repair, and their recommended age of patients was
between 6 and 12 months. The author has resorted to reconstruction,
creating a web space using a Barsky flap from one of the border digits
to define the depth of the new web space, and closure of the cleft
using a zigzag skin repair. In addition to the skin repair, the
underlying tendon reconstruction and metatarsal osteotomies are
important in this reconstruction (Fig. 30.58).
There frequently is a conjoined flexor and extensor tendon to the great
toe functioning as an adductor and causing a severe hallux valgus. The
recognition of this with centralization of both the extensor and flexor
tendon and division of the conjoined tendon as an adductor is
important. Metatarsal osteotomies and midtarsal osteotomies are used to
narrow the foot and reconstruct the cleft, in addition to soft tissue
repair. Complex plastic surgical procedures to create the appearance of
toes have been described, but they do not produce functional benefit (377).
 |
|
Figure 30.56 A: This patient had a mild cleft foot with a transverse metatarsal bridging the cleft and widening the foot. B: With repair of the cleft and removal of the transverse metatarsal, a healthy foot resulted.
|
 |
|
Figure 30.57 Father and son with cleft feet.
|
arch. The high arch may be secondary to plantar-flexion deformity of
the forefoot (forefoot equinus) or dorsiflexion of the calcaneus (378).
The hindfoot is generally in varus, but may be laterally oriented or in
valgus at times. The forefoot is generally pronated with a
plantar-flexed first ray.
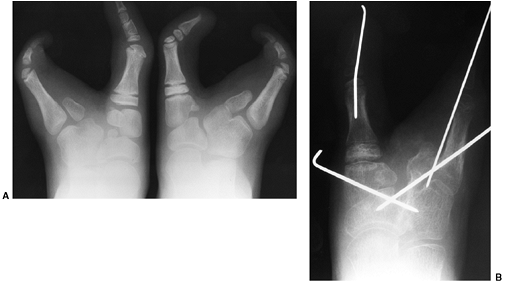 |
|
Figure 30.58 Preoperative (A) and postoperative (B) radiographs of symptomatic cleft foot treated with osteotomies.
|
opposing extrinsic or intrinsic muscle groups. A very high proportion,
greater than two thirds, of patients with a cavus foot have an
underlying neurologic disorder (379). The
number of cases termed “idiopathic” cavus foot continues to decrease as
diagnostic methods improve. The diagnosis of hereditary sensory motor
neuropathy (HSMN), which includes the types I and II
Charcot-Marie-Tooth (CMT) (380), is the most
common neurologic disorder resulting in this deformity. On physical
examination, in addition to considering the array of systemic diseases
resulting in cavus foot, one should also explore the structural
abnormality and muscle imbalance that leads to this disorder. Forefoot
plantar flexion involving primarily the first ray is the most common
structural problem leading to a cavus foot. In this state, the first
ray plantar flexion compromises the normal tripod structure of the
foot, shifting weight bearing laterally and driving the hindfoot into
varus. This may result from weak anterior tibial muscle relative to
peroneus longus muscle (7), overpull of the extensor hallucis longus compensating for a weak anterior tibial muscle (68), or intrinsic muscle contracture of the foot with weakness (2).
With time, the plantar fascia contracts and the varus hindfoot
deformity becomes fixed. The second major group of cavus feet are those
with a dorsiflexion deformity of the calcaneus; this generally is the
result of weakness in the gastrocsoleus complex (Fig. 30.59) and a
compensatory push-off augmented by toe flexors. Any abnormality in the
neuromuscular axis may affect muscle balance in the foot, contributing
to a cavus deformity. Bilateral involvement suggests a systemic
condition, whereas unilateral cavus deformities suggest a more
localized differential diagnosis (Table 30.2).
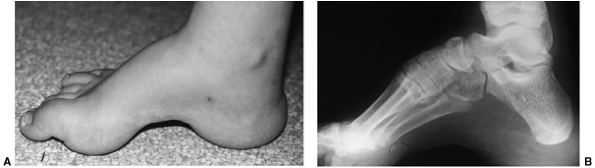 |
|
Figure 30.59 Calcaneocavus deformity in a child with myelomeningocele. A: Transtarsal cavus with thick callosities under the calcaneus and the metatarsal heads. B: Radiograph of the calcaneocavus “pistol-grip” deformity.
|
neurologic condition. That is, the frequency of CMT or Freidrich ataxia
in a given population will define the frequency of the cavus foot that
is secondary to these deformities.
generally related to either instability or pain. Instability may be
secondary to muscle weakness, sensory loss, or deformity (381).
The pain is generally related to prominence of the metatarsal heads,
callosities over the toes, or malalignment increasing the stresses of
weight bearing. Muscle contraction is not required to maintain erect
posture with a healthy, balanced foot. With excessive plantar flexion
of the first ray, the normal tripod (first metatarsal, fifth
metatarsal, and calcaneus) is lost, leading to an abnormal force
distribution. In the malaligned state, not only are stresses increased
across joints and pressures increased on bony prominences, but also
muscle strength is required to maintain posture. The combination of
these leads to pain, fatigue, and instability.
|
TABLE 30.2 CAUSES OF CAVUS FOOT DEFORMITY
|
|
|---|---|
|
frequently reported symptom is a recurrent spraining of the ankle with
a feeling of giving out. Ligament injuries as well as the malalignment
lead to pain. Blistering and calluses result over bony prominences.
This is particularly true over the dorsal aspects of the
interphalangeal (IP) and PIP joints, as well as the plantar aspect
under the metatarsal head and lateral border of the fifth metatarsal.
Muscle weakness related to the underlying condition leads to giving out
with loss of the dynamic stabilizers of the ankle, particularly the
peroneal muscles. Finally, sensory loss, particularly position and
vibratory, disrupts the normal feedback loop that provides dynamic
stabilization of the ankle.
neuromuscular abnormality, symptoms at presentation may reflect the
underlying condition. A history of change in foot shape or change in
foot size is important. Family history is critical; if possible,
examination of other members of the family, rather than simply asking
for history of underlying medical conditions, can often be revealing
because a subtle cavus foot may be present. Further medical, birth, and
developmental histories, as well as a review of systems, are mandatory
in searching for underlying causes of cavus foot.
and gait first. In a sitting position, the foot can appear to have a
high arch but be completely flat in stance. In the swing phase of gait,
the foot dorsiflexion may be the result of isolated extensor hallicus
longus (EHL) contraction, rather than a coordinated activity of
anterior tibial as well as EHL and toe extensors. Look at foot position
at heel strike, as weight may immediately shift to the lateral border
of the foot. Does heel strike occur or is forefoot equinus preventing
heel strike and there is no contact of the calcaneus with the ground?
Are there any compensatory features of gait present such as knee
hyperextension or Trendelenburg compensation at the hip? The spine
should be evaluated for evidence of scoliosis, cutaneous defects over
the spine typical in diastomatomyelia, or fatty deposits seen in
lipomeningoceles.
and reflexes must be done in all cases. Sensory examination should
include light touch, pain, and vibratory sense. Stocking and glove
sensory loss may be reflective of underlying peripheral neuropathy.
Despite varied patterns of muscle imbalance, the cavus deformity with a
plantar-flexed first ray is rather constant (382, 383, 384).
localization of the deformity to the forefoot or hindfoot. A tight
plantar fascia is palpable as a subcutaneous band along the
longitudinal arch with stretching of the forefoot. The
hindfoot is evaluated using the Coleman block test (Fig. 30.15) (385).
In this test, a 1-inch block is placed under the lateral border of the
foot allowing the first ray to plantar-flex without driving the
hindfoot into varus. In the common case where the plantar-flexed first
ray is the primary problem in cavus foot, the hindfoot will shift
beyond neutral into a position of slight valgus, as stance is assumed (Fig. 30.61).
The hindfoot should also be examined with the patient in prone position
or kneeling in order to evaluate the isolated position of the hindfoot
and eliminate forefoot deformity. The degree of hindfoot flexibility is
vital for surgical planning.
 |
|
Figure 30.60 Cavovarus deformity in this individual with Charcot-Marie-Tooth disease. A: The arch is elevated only along the medial border of the foot. B: Varus and adduction can be appreciated.
|
whereas varus and calcaneus deformity are seen quite frequently.
Flexibility or rigidity must be determined, as treatment implications
are critical. With the flexible state, tendon-balancing procedures are
effective, whereas rigidity of deformity requires osteotomy and at
times arthrodesis. Toe deformity with MP hyperextension and PIP flexion
are important to identify and treat. With the foot dorsiflexed, the toe
flexion deformity is accentuated by tightening the flexor hallucis
longus and the flexor digitorum communis. With plantar flexion, the
extrinsic toe flexors are relaxed and the deformity of the PIP and MP
joints can be determined. Tender callosities over joints must be
documented.
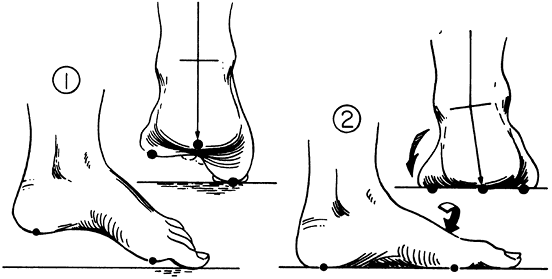 |
|
Figure 30.61
The tripod effect. The hindfoot must assume a varus position when weight bearing if the first metatarsal is fixed in plantar flexion (1). Initial contact of plantar-flexed first metatarsal (2). Fifth metatarsal makes contact through supination of the forefoot (arrow), which also drives the hindfoot into varus. (From Paulos L, Coleman SS, Samuelson KM. Pes cavovarus. Review of a surgical approach using selective soft-tissue procedures. J Bone Joint Surg Am 1980;62:942–953, with permission.) |
foot are obtained in all cases as part of the initial evaluation. Even
in mild cases, knowing the radiologic appearance of the foot
establishes a baseline on which future evaluation of progression can be
judged. The standing lateral film is most important for evaluation. The
long axis of the talus should be collinear with the long axis of the
first metatarsal. Deviation from this with the dorsal apex is seen in
cavus foot deformity. This has been termed the Meary angle.
The angle between the first metatarsal and the long axis of the
calcaneus is the Hibb angle, and this is a gauge of the elevation of
the longitudinal arch. In the normal state it is greater than 150
degrees but it steadily decreases as cavus foot worsens (Fig. 30.62).
Finally, the calcaneal pitch is the angle between the calcaneus and the
horizontal and is a measure of hindfoot sagittal plane deformity.
Cock-up toe deformity and MP dorsal subluxations should be observed as
well. In the anteroposterior view, there is normally an angle of
approximately 30 degrees between the talus and calcaneus. With
increased varus deformity of the hindfoot, this angle lessens and the
talus and calcaneus become increasingly parallel. Further diagnostic
studies generally involve anteroposterior and lateral views of the
spine and sacrum, looking for underlying deformity that may relate to
etiology. Beyond this, MRI of the neuroaxis may be indicated, as well
as complete neurologic evaluation, electromyography (EMG), and nerve
conduction velocities in order to complete the search for etiology.
nonoperative treatment of the cavus foot, the author believes this
should be reconsidered. This is a frequently progressive
deformity
that must be monitored. Tightness in the heel cord should be managed
with a stretching program, and weakness in dorsiflexion and peroneals
may be countered by an exercise program to improve strength and a
lightweight brace or angle foot orthoses (AFO) to prevent recurrent
spraining or injury. Although a specific program to stretch the
longitudinal arch or plantar fascia may not be effective in altering
the natural history of this condition, preventing equinus deformity is
valuable, and attempts to improve or maintain muscle balance should be
pursued. Plantar callosities are often bothersome and painful to
patients. These symptoms may be ameliorated with an appropriate arch
support with metatarsal pad. A properly made orthotic may significantly
improve symptoms and delay or prevent the need for surgical
reconstruction (386).
Management rather than cure of the cavus foot is the concept to
remember. As cavus deformity is usually secondary to neuromuscular
disease, continued problems and further treatment should be anticipated
(188,226,227,378,386,387).
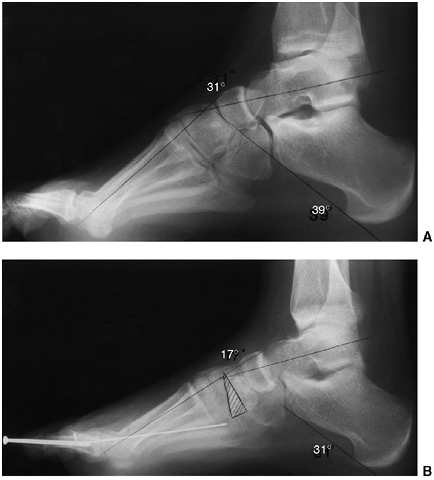 |
|
Figure 30.62 Lateral radiograph of a cavovarus foot deformity before (A) and after (B)
a medial cuneiform plantar-based opening wedge osteotomy. The axis lines of the first metatarsal and the talus cross each other in the body of the medial cuneiform, indicating that as the site of deformity. (From Mosca VS. Ankle and foot: pediatric aspects. In: Beaty J, ed. Orthopaedic knowledge update 6. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1999:583.) |
the deformity present, determined by physical exam and radiographic
evaluation. The elevation of the longitudinal arch (Hibb angle)
universally requires a plantar fascia release. A plantar-flexed first
ray that is flexible may be balanced by tendon transfer, whereas a
rigid deformity requires an osteotomy in order to correct the
plantar-flexion deformity. The hindfoot may have fixed varus deformity
(Coleman block test) (385) and require an
osteotomy for correction, or it may be flexible and assume normal
posture simply with correction of the first ray or forefoot deformity.
On the other hand, the entire forefoot may be involved in such a way
that midfoot osteotomy is required in order to achieve correction.
Finally, toe deformity must be corrected. No single prescription for
surgical correction of cavus foot can be found, but a group of
operations applied to specific deformities for individual patients
allow satisfactory management of the cavus foot deformity.
In this procedure, the plantar fascia and the origin of the abductor
hallucis is released. The neurovascular bundle is identified under the
fascia of the abductor hallucis and followed distally into the plantar
aspect of the foot. In doing this, the plantar fascia can be safely
released. Open rather than percutaneous release should be done, as
tight plantar structures need to be released in addition to simply
dividing the superficial fascia. Steindler (388)
described a procedure in which the intrinsic muscles of the foot were
released extraperiosteally with correction of the deformity. Release of
the calcaneonavicular ligament may facilitate correction of a severe
elevation of the longitudinal arch when combined with corrective
casting. Plantar midfoot and hindfoot release when combined with
corrective casting has been shown to be of some value by Paulos,
Coleman, and Samuelson (383) as well as by Sherman and Westin, who (389) noted that in up to 85% of patients, significant correction of residual cavus deformity in clubfoot could be treated
with extensive plantar release and corrective casting. Corrective
casting has no role in a calcaneal cavus foot with increased calcaneal
pitch. Further stretching of the hindfoot and weakening of the
gastrocsoleus will result without significant correction of the
longitudinal arch. In poliomyelitis, or conditions in which the
deformity is secondary to weak gastrocsoleus and a pistol-grip
calcaneus deformity is present, there is no role for corrective casting.
shows the effect of two pairs of opposing muscle forces on the first
ray. These opposing force couples are the anterior tibial muscle versus
the peroneus longus, and the extensor hallucis longus versus the flexor
hallicus longus and intrinsics. In the face of a weak anterior tibial
muscle, the peroneus longus plantar flexes the first ray. The EHL
overpulls with dorsiflexion of the great toe, plantar flexing the
metatarsal head as the toe flexor produces an IP flexion deformity as
well. Two muscle-balancing procedures providing benefit to the first
ray in a cavus foot are the peroneus longus to brevis transfer and the
Jones transfer, or EHL, to first metatarsal head, accompanied by IP
fusion. In the peroneus longus to brevis transfer, the two tendons are
sewn together just distal to the fibula, and the distal portion of the
peroneus longus tendon is divided. In the EHL transfer (Jones
procedure), the tendon is divided at the MP joint and the proximal
tendon is placed through the metatarsal. The distal stump of the EHL
tendon is transferred to the extensor brevis, and an IP fusion of the
great toe is done to prevent subsequent flexion deformity of the great
toe. Tynan and Klenerman (390) showed that this
transfer was highly effective in treating clawing of the hallux and
plantar-flexion deformity of the first ray in 90% of cases; it was,
however, unreliable in curing pain under the first metatarsal head,
helping only in 43% of patients at follow-up. Breusch et al. (391)
showed that the overall rate of patient satisfaction was 86%, but that
the problems of catching of the big toe when walking barefoot and
transfer lesion to the second metatarsal head occurred. They also noted
that transfer of the peroneus longus to peroneus brevis was a
significant risk factor for elevation of the first metatarsal. In cases
with significant peroneal weakness it should not routinely be used as
in many cases of cavus foot, the lesser toes are involved with clawing,
with plantar flexion of the lesser metatarsal heads as well, resulting
in pain and deformity. The balancing procedures for the lesser toes
involve transfer of the extensors to the metatarsal heads with IP
fusion, with or without flexor tenotomy. Another alternative in a case
with a weak anterior tibial tendon is transfer of the entire group of
extensor tendons to the cuneiforms in an effort to augment weak
dorsiflexion, as described by Cole (392). Mulier, Dereymaeker, and Fabry (393)
found an association between metatarsalgia and long, clawed toes. With
transfer of the extensor digitorum longus tendons to the metatarsal
necks, symptoms were relieved in 25 of 33 affected feet. Although
symptoms were improved in the remainder, residual deformity remained.
Fabry believed that the transfer of the long extensor tendons to their
respective metatarsal necks with IP joint fusion was an excellent
procedure for patients with metatarsalgia and pes cavus deformity.
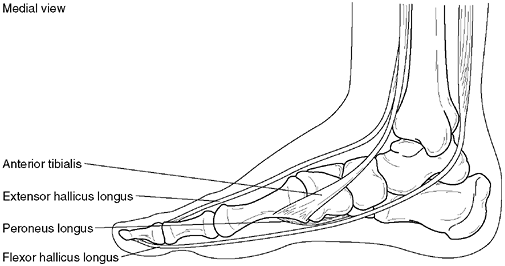 |
|
Figure 30.63
Opposing muscles, anterior tibial versus peroneus longus and extensor hallucis longus versus flexor hallucis longus and intrinsics, create deformity if unbalanced. |
osteotomy prior to or in association with tendon transfer. Following
plantar fascia release, one must make a decision about the
correctibility of the first ray deformity or flexibility of the foot.
If one has any question about the persistence of a plantar-flexion
first ray deformity, osteotomy is required. The osteotomy may be a
plantar opening wedge of the first cuneiform (Fig. 30.62);
this is a stable osteotomy in which bone graft can be used to maintain
the corrected position of the osteotomy. Cuneiform osteotomy avoids the
risk of growth arrest in the proximal first metatarsal in a growing
child. Frequently, the center of rotation in a cavus foot is in the
midfoot or cuneiform, making this osteotomy preferable to metatarsal
procedures. For more severe deformities of the midfoot, a first
cuneiform osteotomy will not be sufficient. Midfoot osteotomies, as
described by Cole (392), Japas (394), Jahss (395), and Wilcox and Weiner (396)
may be used to correct the forefoot and midfoot component of the cavus
deformity. These procedures sacrifice midfoot joints and mobility but
correct forefoot deformity. The talonavicular joint and calcaneal
cuboid joints are preserved in midfoot
osteotomies.
The amount of correction achievable with midfoot osteotomy is dependent
upon the shortening of the foot and the size of the wedge that is
removed. They are accompanied by plantar release. Maximal correction
for midfoot osteotomies is in the range of 20 to 25 degrees. Excessive
correction through the midfoot may lead to a rocker-bottom deformity of
the foot and should be avoided. In select cases, metatarsal osteotomies
may be of value in correction of forefoot deformity. This is
particularly true if residual medial deviation of the forefoot remains
after soft tissue release. A greenstick dorsal closing wedge of the
metatarsals has been described by Swanson et al. (397) and Gould (398). Watanabe (399) found 84% good or excellent results in individuals treated in this manner.
discussion of cavus foot, one must ensure that varus deformity is
corrected. Rarely is calcaneal pitch decreased with equinus coming
primarily from the hindfoot in cavus foot deformity. In reviewing a
large number of patients with CMT, Atkas and Sussman (400)
found the hindfoot always to be in slight dorsiflexion, with equinus
deformity resulting primarily from forefoot and midfoot alteration in
anatomy. Rigid hindfoot varus is best addressed by a modified Dwyer
osteotomy. In this osteotomy, closing lateral wedge of the calcaneus is
combined with a slide or translation of the calcaneal tuberosity to
achieve improved correction. Sammarco and Taylor (401)
reported on a series of combined calcaneus and metatarsal osteotomies
for cavus foot in 15 patients with excellent results, both clinically
and radiologically. Symptoms of metatarsalgia as well as instability
were corrected by this procedure. A pain-free, plantigrade foot was
achieved without sacrificing motion as would be required with
arthrodesis. Occasionally, deformity is sufficiently severe and rigid
that there is no alternative to triple arthrodesis. Although it was
generally thought that a triple arthrodesis would provide long-term
plantigrade foot, Schwend and Drennan (402)
have shown that progressive deterioration over time, secondary to
muscle imbalance, occurs even after triple arthrodesis. Balancing
procedures, therefore, are recommended in association with this
hindfoot fusion. The two types of triple arthrodeses that are indicated
in severe deformities are the Beak triple arthrodesis as described by
Siffert et al. (115) and the Lambrinudi triple arthrodesis as modified by Hall and Calvert (116).
In these operations, the wedges of bone removed allow correction to a
plantigrade foot. In the Beak triple arthrodesis, a portion of the
talus and navicular is removed to achieve satisfactory alignment of the
foot. In the Lambrinudi procedure, a wedge of talus is removed with a
cut perpendicular to the long axis of the tibia, allowing correction of
equinus deformity through bony cuts of the triple arthrodesis.
Similarly, varus deformity is corrected in this manner and internal
fixation achieved with staples or screws.
which had a very low long-term success rate after triple arthrodesis.
Patients in Adelaar’s group were primarily affected with poliomyelitis,
whereas patients in Schwend and Drennan’s group had neuromuscular
disease with progressive muscle weakness and therefore progressive
imbalance. Triple arthrodesis should be reserved for patients where
other procedures will not provide sufficient correction of deformity to
achieve a plantigrade foot. In equivocal cases, patients should be
aware of the need to attempt correction through osteotomies and soft
tissue releases, withholding arthrodesis for severe, recurrent, or
residual deformities in which no alternative is present. Finally,
Ilizarov management has been used in a number of cases of severe foot
deformity with reasonable improvement. A combination of distraction
osteotomy and joint correction is used in order to achieve satisfactory
alignment. This may represent a valuable alternative to triple
arthrodesis, but more data is required in this area. Kucukkaya et al. (403)
have recommended a V osteotomy using the Ilizarov frame and method for
management of foot deformity in poliomyelitis and CMT. In a series of
patients treated in this manner, they documented nearly uniform
achievement of a painless plantigrade foot. It appears that there is a
role for a combination of soft tissue stretching and osteotomy in the
correction of severe deformity using an Ilizarov frame (403).
in young children in whom radiographic findings of the foot showed
characteristic flattening, sclerosis, and irregular ossification
pattern (404). This is a self-limiting condition, with restitution of healthy bony architecture in all cases.
Tsirikos et al. have reported bilateral Kohler disease in identical
twins, suggesting a genetic predilection for this relatively rare
condition (408).
condition is characterized by disordered enchondral ossification
including both osteogenesis and chondrogenesis, presumably related to
mechanical stress at the time of early ossification. Karp (409)
found that ossification of the navicular occurs earlier in girls than
in boys. Half of the girls studied had a navicular that was ossified by
the age of 2 years, and one third of the boys were more than 3½ years
of age by the time ossification occurred. Karp’s feeling was that the
delay in ossification predisposed boys to mechanical injury at the time
of early ossification of the cartilaginous navicular.
time of ossification, avascular necrosis appears to play a role in the
development of Kohler disease. The blood supply to the navi-cular bone
is significant, with a network of perichondrial
vessels.
However, at the time of early ossification, arteries penetrate the
cartilaginous navicular without their mature anastomotic network,
predisposing them to vascular injury. Vascular theories are supported
by biopsy studies showing areas of necrosis in the navicular (404).
presenting with an antalgic gait, tending to walk on the lateral border
of the foot. There is often dorsal medial swelling and tenderness, at
times with redness and warmth, which might suggest infection or
arthritis. Range of motion is generally intact.
foot demonstrate characteristic findings of sclerosis, fragmentation,
and flattening of the navicular bone (Fig. 30.64).
The navicular is the last bone in the foot to ossify. The ossific
nucleus is first seen in girls between 18 and 24 months of age and in
boys 30 to 36 months of age (409). Irregularity in ossification is common, with coalescence of early ossification centers (409).
Kohler disease is a clinical diagnosis, rather than a radiologic one;
that is, a patient with irregular ossification pattern does not have
Kohler disease in the absence of symptoms.
infection, and an evaluation including CBC, sedimentation rate, and
C-reactive protein is beneficial. Occasionally an MRI is helpful in
differentiating these conditions. Stress fractures to the tarsal
navicular exist, generally in adults, and avascular necrosis of the
tarsal navicular has been associated with diabetes, but again in
adults, not in young children.
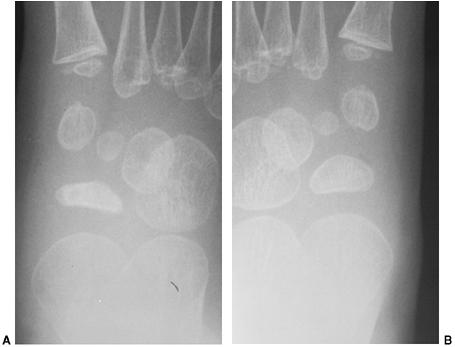 |
|
Figure 30.64 A: Kohler disease manifested as sclerotic and flattened right tarsal navicular. B: Healthy left navicular.
|
of blood supply to the navicular. The most common pattern was a diffuse
network of five or six perichondrial vessels. The most common pattern
was a single dorsal or plantar artery. The single vessels at the time
of ossification predispose to mechanical injury and secondary avascular
necrosis. Histologic examination of affected bones demonstrates
necrosis, resorption of dead bone, and formation of new bone consistent
with remodeling after vascular injury.
childhood. The navicular reconstitutes itself somewhere between 4
months and 4 years of age and is normal at skeletal maturity (405, 406, 407). There is no residual deformity or disability in adults.
support may relieve mild symptoms. For persistent or intense pain, a
short leg cast has been shown to be beneficial. Borges et al. (407), Ippolito et al. (405), and Williams et al. (406)
found that treatment with a below-knee cast for a minimum of 8 weeks
reduced the duration of symptoms. Use of a walking cast was found to be
as effective as use of
a
nonwalking cast. As symptoms were routinely relieved by a short leg
cast in this self-limiting condition, failure to follow the expected
course might be an indication for biopsy. There is, however, no role
for biopsy or surgery in typical cases of Kohler disease.
of the os calcis leading to heel pain in a growing child, which he
thought was an inflammatory disorder. The advent of radiologic imaging
in the early 20th century led Kohler, Freiberg, and many others to the
identification of clinical conditions characterized by similar
radiographic findings called “osteochondroses.”
The average age at presentation is 11.5 years; it is two to three times
more common in boys than in girls, and 60% of patients have bilateral
involvement (412). As girls become more athletically active, the author suspects that there will be no sexual predilection for this condition.
12-year-old athletically inclined boy. The patient has pain secondary
to impact as well as repetitive pull of the gastrocsoleus on the
apophysis. The pain is limited to the heel. It may be associated with
warmth, swelling, and even redness. The characteristic finding is pain
with medial lateral compression over the tuberosity of the calcaneus.
pain, which include cystic lesions of the calcaneus and osteomyelitis.
Frequently, children with calcaneal apophysitis have a tight Achilles
tendon.
because there is no diagnostic radiographic finding. In a review of
radiographs of children with and without Sever apophysitis, sclerosis
appears with equal frequency in the healthy and diseased state.
Fragmentation of the apophysis (414), however, is the radiologic finding seen with increasing frequency in Sever disease (Fig. 30.65).
localizing pathology but is generally not needed. An MRI will be
helpful in making the differentiation between disease states involving
the body of the calcaneus and apophysitis. Such conditions include
stress fracture, lytic lesion, or osteomyelitis.
 |
|
Figure 30.65 Lateral radiograph showing the normal irregularities of ossification of the apophysis of the os calcis in the growing child.
|
forces from the plantar fascia and the Achilles tendon during weight
bearing (413,415,416).
It is also subjected to impact with heel strike in gait. The
combination of direct impact and tension forces from the plantar fascia
and the pull of the gastrocsoleus complex lead to a stress fracture
from repeated microtrauma. Liberson et al. (415)
reviewed the pathology of the apophysis of the os calcis in children.
Their data supported the hypothesis of a stress fracture as a cause of
this injury.
general, patients respond to activity restriction and use of a heel pad
in the shoe, making them comfortable. Stretching exercises of the
Achilles tendon may be helpful in decreasing symptoms, and certainly in
decreasing recurrent episodes of Sever apophysitis. Nonsteroidal
antiinflammatory medicines may be of some value. For persistent
symptoms, a short leg cast will relieve pain. With the use of a short
leg cast for patients with symptoms, the average time for relief and
return to activity is 2 months, with the range of time being from 1 to
6 months (412). The recurrence of symptoms is
relatively common in adolescents. There may be some benefit in the
long-term use of heel pads and a heel cord stretching program in the
prevention of recurrence of this condition.
painful condition of the second metatarsal head, characterized by
flattening of the articular surface of bone with both lucency and
sclerosis in the metatarsal head. The term “infraction” implied a
traumatic origin, whereas “infarction” would imply an ischemic origin.
occurs most commonly in adolescent girls and is, surprisingly, the only
“osteochondrosis” with a predilection for the female sex. The second
metatarsal head is most commonly affected, followed by the third. Less
commonly, the first, fourth, and fifth metatarsals are involved. Less
than 10% of individuals have bilateral involvement.
classified under an osteochondrosis that is characterized by disordered
enchondral ossification. It has been classified by Siffert (413)
as primarily an articular osteochondrosis that may or may not disrupt
the associated epiphysis. Proposed theories for etiology include
trauma, repetitive stress, vascular abnormalities, or high heeled shoes
(418,419).
weight-bearing activities or athletics. There is soft tissue swelling
about the metatarsal head and tenderness with restriction of motion on
examination. The differential diagnosis includes arthritis as well as a
metatarsal stress fracture.
 |
|
Figure 30.66 A: Freiberg infraction of the second metatarsal head. Early stage with crescent sign. B: Later stage with collapse of the metatarsal head. The patient, a young woman, was asymptomatic.
|
is one of increased sclerosis, flattening of the articular surface, and
lucency. It has an appearance somewhat like Perthes disease of the
metatarsal head. The prognosis cannot be accurately determined by the
extent of involvement seen radiographically. Classification systems for
this disease based on radiographic appearance exist (419, 420, 421) but have not been particularly useful in clinical management.
Stage 1 is associated with swelling and pain in the absence of
radiologic changes. In stage 2, the cells of the chondrocytes in the
epiphysis die secondary to loss of nutrition by diffusion from joint
fluid or loss of oxygen from blood flow. In stage 3, repair takes place
with gradual replacement of necrotic bone and healing. Intraarticular
loose bodies may complicate the clinical course of Freiberg infraction.
stages as listed in the preceding text, with reconstitution of a
satisfactory articular surface and relief of pain. The long-term
results depend on the severity of the damage to the articular surface
and whether loose bodies result.
and allow healing of this condition in most cases. Treatments include
avoidance of activity, use of shoe inserts with a metatarsal pad, and
the use of well-padded shoes. Avoiding high-heeled shoes that place
more pressure on the metatarsal heads is advised. Surgery for this
condition generally includes joint debridement and removal of loose
bodies (417,420,423), elevation of a collapsed articular surface with bone grafting (421), excision of a metatarsal head and shortening of a metatarsal (424), and metatarsal dorsiflexion osteotomy (419,420,423).
Debridement of periarticular osteophytes or prominent bone impinging on
metatarsal phalangeal joint motion is a procedure that usually gives
satisfactory symptomatic relief (417,420,423) if required. The distal metatarsal dorsiflexion osteotomy has been reported to relieve symptoms (419,420,425).
In any procedure, it is important to avoid damage to the blood supply
of the metatarsal head at the time of surgery, limiting soft tissue
dissection (419).
LT, Chew DE, Corbett M. The longitudinal arch. A survey of eight
hundred and eighty-two feet in normal children and adults. J Bone Joint Surg Am 1987;69:426–428.
P, Weinstein SL, Ponseti IV. The long-term functional and radiographic
outcomes of untreated and non-operatively treated metatarsus adductus. J Bone Joint Surg Am 1994;76:257–265.
B, Reimann I, Becker-Andersen H. Congenital calcaneovalgus. With
special reference to treatment and its relation to other congenital
foot deformities. Acta Orthop Scand 1974;45:145–151.
N, Stukenborg C, Savory KM, et al. Hindfoot motion after isolated and
combined arthrodeses: measurements in anatomic specimens. Foot Ankle Int 2000;21:921–927.
R. Family studies and the cause of congenital club foot. Talipes
equinovarus, talipes calcaneo-valgus and metatarsus varus. J Bone Joint Surg Br 1964;46:445–463.
AC, Holt VL, Mosca VS, et al. Talipes equinovarus and maternal smoking:
a population-based case-control study in Washington state. Teratology 2002;66:91–100.
MA, Paulozzi LJ, Moore CA. Family history, maternal smoking, and
clubfoot: an indication of a gene-environment interaction. Am J Epidemiol 2000;152:658–665.
H, Handelsman JE, Badenhorst M, et al. The muscles in club foot—a
histological, histochemical and electron microscopic study. J Bone Joint Surg Br 1977;59-B:465–472.
ML, Willig SJ, Roberts JM, et al. An electron microscopic study of the
fascia from the medial and lateral sides of clubfoot. J Pediatr Orthop 1985;5:577–581.
K, Schollmeier G, Uhthoff HK. The pathogenesis of club foot. A
histomorphometric and immunohistochemical study of fetuses. J Bone Joint Surg Br 1994;76:450–457.
R, Davidson R, Dormans J, et al. Radiographs of the infant foot: a
study of reproducibility of measurement and positioning. Orthop Trans 1994;18:996.
A, Bonnet F, Mazeau P, et al. Orthopaedic treatment and passive motion
machine: consequences for the surgical treatment of clubfoot. J Pediatr Orthop B 1996;5:173–180.
S, Sairam S, Homfray T, et al. Outcome of antenatally diagnosed talipes
equinovarus in an unselected obstetric population. Ultrasound Obstet Gynecol 2002;20:226–229.
A, Yankowitz J, Kanis AB, et al. Antenatal sonographic diagnosis of
club foot with particular attention to the implications and outcomes of
isolated club foot. Ultrasound Obstet Gynecol 1998;12:103–106.
N, Tran T, Umstad M, et al. Mid-trimester ultrasound diagnosis of
isolated talipes equinovarus: accuracy and outcome for infants. Aust N Z J Obstet Gynaecol 1998;38:301–305.
KD, Raffel C, Breckle RJ, et al. Chronology of neurological
manifestations of prenatally diagnosed open neural tube defects. J Matern Fetal Neonatal Med 2002;11:89–92.
WB, Mohaideen A, Madan S, et al. A method for the early evaluation of
the Ponseti (Iowa) technique for the treatment of idiopathic clubfoot. J Pediatr Orthop B 2003; 12:133–140.
BS, Wilson H, Johnston CE, et al. Nonoperative clubfoot treatment using
the French method: comparing clinical outcome with radiographs. Pediatric Orthopaedic Society of North America 2001 annual meeting. Rosemont, IL: Pediatric Orthopaedic Society of North America, 2001:142.
Campenhout A, Molenaers G, Moens P, et al. Does functional treatment of
idiopathic clubfoot reduce the indication for surgery? Call for a
widely accepted rating system. J Pediatr Orthop B 2001;10:315–318.
VJ. Surgical correction of the resistant club foot. One-stage
posteromedial release with internal fixation: a preliminary report. J Bone Joint Surg Am 1971;53:477–497.
VJ. Resistant congenital club foot—one-stage posteromedial release with
internal fixation. A follow-up report of a fifteen-year experience. J Bone Joint Surg Am 1979;61:805–814.
AH, Marxen JL, Osterfeld DL. The Cincinnati incision: a comprehensive
approach for surgical procedures of the foot and ankle in childhood. J Bone Joint Surg Am 1982;64: 1355–1358.
VS. Calcaneal lengthening for valgus deformity of the hindfoot. Results
in children who had severe, symptomatic flatfoot and skewfoot. J Bone Joint Surg Am 1995;77:500–512.
JR, Valadie AL, Ferguson RL, et al. Surgical management of ankle valgus
in children: use of a transphyseal medial malleolar screw. J Pediatr Orthop 1997;17:3–8.
SY, Sullivan RJ, Davidson RS. Talo-navicular arthrodesis for residual
midfoot deformities of a previously corrected clubfoot. Foot Ankle Int 2000;21:482–485.
E, Hayek S, Gilai AN, et al. Tibialis anterior tendon transfer for
residual dynamic supination deformity in treated club feet. J Pediatr Orthop B 2000;9:207–211.
H, Hansson G, Tjernstrom B. Correction of persistent clubfoot
deformities with the Ilizarov external fixator. Experience in 10
previously operated feet followed for 2-5 years. Acta Orthop Scand 1996;67:283–287.
IH, Yang MS, Chung CY, et al. The treatment of recurrent arthrogrypotic
club foot in children by the Ilizarov method. A preliminary report. J Bone Joint Surg Br 2001;83:731–737.
UA, Largo RH, Duc G. Neonatal metatarsus adductus, joint mobility,
axis, and rotation of the lower extremity in preterm and term children
0-5 years of age. Eur J Pediatr 1988; 148:19–23.
CE, Betz RR, Clancy M, et al. Relationship of congenital hip and foot
deformities: a national Shriner’s Hospital survey. Orthop Trans 1991:96.
DA, Breed AL, Cook T, et al. Observer variability in the radiographic
measurement and classification of metatarsus adductus. J Pediatr Orthop 1992;12:86–89.
R, Stevens PM. Idiopathic forefoot-adduction deformity: medial
capsulotomy and abductor hallucis lengthening for resistant and severe
deformities. J Pediatr Orthop 1997;17: 496–500.
CH, Herndon CH, Strong JM. Mobilization of the tarsometatarsal and
intermetatarsal joints for the correction of resistant adduction of the
fore part of the foot in congenital club-foot or congenital metatarsus
varus. J Bone Joint Surg Am 1958;40-A:299–309; discussion 291–309.
RE, Sharma NK, Hassler WL, et al. Tarsometatarsal mobilization for
resistant adduction of the fore part of the foot. A follow-up study. J Bone Joint Surg Am 1970;52:61–70.
JC, Van der Walt ID. Correction of resistant adduction of the forefoot
in congenital club-foot and congenital metatarsus varus by metatarsal
osteotomy. Br J Surg 1966;53:558–560.
DA, Schoenecker PL, Blair VPI. Combined lateral column shortening and
medial column lengthening in the treatment of severe forefoot adductus.
Orthop Trans 1991;15:768.
KA, Lenhart MK. Treatment of residual clubfoot deformity—the
“bean-shaped” foot—by opening wedge medial cuneiform osteotomy and
closing wedge cuboid osteotomy. Clinical review and cadaver
correlations. J Pediatr Orthop 1991; 11:374–381.
VS. Skewfoot deformity in children: correction by calcaneal neck
lengthening and medial cuneiform opening wedge osteotomies. J Pediatr Orthop 1993;13:807.
J, Pedersen B, Brodersen A. Foot deformity and the length of the
triceps surae in Danish children between 3 and 17 years old. J Pediatr Orthop B 1995;4:71–73.
JJ, Forriol F. The development in footprint morphology in 1851
Congolese children from urban and rural areas, and the relationship
between this and wearing shoes. J Pediatr Orthop B 2003;12:141–146.
KR, Brodine SK, Shaffer RA, et al. The effect of foot structure and
range of motion on musculoskeletal overuse injuries. Am J Sports Med 1999;27:585–593.
SD, Millar EA. Arthrorisis by means of a subtalar poly- ethylene peg
implant for correction of hindfoot pronation in children. Clin Orthop 1983;15–23.
LD, Ashley RK, Gilbert RJ. Treatment of the congenital vertical talus:
a retrospective review of 36 feet with long-term follow-up. Foot Ankle 1987;7:326–332.
WR, Fitz DA, Smith WS. The pathologic anatomy of congenital convex pes
valgus. Post mortem study of a newborn infant with bilateral
involvement. J Bone Joint Surg Am 1968; 50: 458–466.
AD, Thomson JD, Deluca PA, et al. Comparison of the posterior approach
versus the dorsal approach in the treatment of congenital vertical
talus. J Pediatr Orthop 2001;21: 212–217.
R, Littlejohn A, Gormley J. Aetiology and interrelationship of some
common skeletal deformities. (Talipes equinovarus and calcaneovalgus,
metatarsus varus, congenital dislocation of the hip, and infantile
idiopathic scoliosis). J Med Genet 1982;19:321–328.
H. The significance of congenital pes calcaneo-valgus in the origin of
pes plano-valgus in childhood. Preliminary report. Acta Orthop Scand 1960;30:64–72.
RD, Bennett JT. Tarsal coalition presenting as a pes cavo-varus
deformity: report of three cases and review of the literature. Foot Ankle 1993;14:540–544.
DP, Holt GR, Ogden JA. Talocalcaneal coalition in patients who have
fibular hemimelia or proximal femoral focal deficiency. A comparison of
the radiographic and pathological findings. J Bone Joint Surg Am 1994;76:1363–1370.
AE, Mize WA, Crawford AH, et al. The “anteater nose”: a direct sign of
calcaneonavicular coalition on the lateral radiograph. J Pediatr Orthop 1987;7:709–711.
JE, Goldner JL, Martinez S, et al. Computerized tomography of
talocalcaneal tarsal coalition: a clinical and anatomic study. Foot Ankle 1986;6:273–288.
LM, Van Hoe LR, Van Ghillewe KV, et al. Subtalar coalition: diagnosis
with the C sign on lateral radiographs of the ankle. Radiology 1994;193:847–851.
P, Kumar SJ. Calcaneonavicular coalition treated by resection and
interposition of the extensor digitorum brevis muscle. J Bone Joint Surg Am 1990;72:71–77.
PB, Aronsson DD, Lamont RL, et al. The Mitchell procedure for the
treatment of adolescent hallux valgus. A long-term study. J Bone Joint Surg Am 1993;75:1610–1618.
HA, Newman SR. Adolescent bunion deformity treated with double
osteotomy and longitudinal pin fixation of the first ray. J Pediatr Orthop 1993;13:80–84.
KJ, Feiwell LA, Freedman EL, et al. The effect of chevron osteotomy
with lateral capsular release on the blood supply to the first
metatarsal head. J Bone Joint Surg Am 1995;77:197–204.
DW, Leventen EO. A new osteotomy for hallux valgus: a horizontally
directed “V” displacement osteotomy of the metatarsal head for hallux
valgus and primus varus. Clin Orthop 1981;157:25–30.
GB, Grogan DP, Bobechko WP. Butler arthroplasty for correction of the
adducted fifth toe: a retrospective study of 36 operations between 1968
and 1982. J Pediatr Orthop 1985;5: 439–441.
MH, Gonzalez S, Breck LW, et al. Lateral transfer of the posterior
tibial tendon in certain selected cases of pes plano valgus (kidner
operation). Clin Orthop 1965;40:139–144.
LG, Happle R, Mulliken JB, et al. Proteus syndrome: diagnostic
criteria, differential diagnosis, and patient evaluation. Am J Med Genet 1999;84:389–395.
AG, Bonde RK. Congenital malformations of the flipper in three West
Indian manatees, Trichechus manatus, and a proposed mechanism for
development of ectrodactyly and cleft hand in mammals. Clin Orthop 1986;202:294–301.
