Sternoclavicular Joint Disloclation
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Sternoclavicular Joint Disloclation
Sternoclavicular Joint Disloclation
Theodore T. Manson MD
John H. Wilckens MD
Description
-
The medial end of the clavicle dislocates from its articulation with the sternum.
-
Dislocations may be anterior or posterior.
-
Posterior dislocations:
-
May cause neurovascular or respiratory compromise.
-
-
Posterior reductions:
-
Must be reduced.
-
-
Anterior dislocations often are unstable, even if reduced, but few functional deficits occur with this instability.
-
Epidemiology
-
Rare injury (1):
-
1% of all joint dislocations
-
3% of all shoulder girdle injuries
-
40% from vehicular trauma
-
21% from sports-related injury
-
63% of dislocations are anterior.
-
Pathophysiology
-
The sternoclavicular joint is a diarthroidal connection between the clavicle and sternum.
-
Strong ligaments bind the 2 bones together.
-
The capsular sternoclavicular ligaments are the primary restraints to AP movement.
-
Assisting the capsular ligaments are the costoclavicular and intra-articular disc ligaments.
-
-
Several vital structures lie immediately posterior to the sternoclavicular joint (Fig. 1).
-
Innominate artery and vein
-
Trachea
-
Esophagus
-
Vagus and phrenic nerves
-
Anterior jugular vein
-
Posterior dislocation can cause compression of these structures.
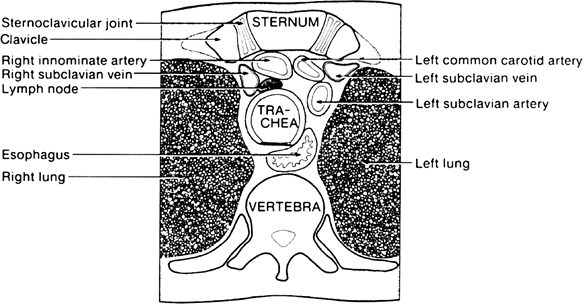 Fig.
Fig.
1. Cross-sectional view of the anatomy of the vital structures
posterior to the sternoclavicular joint. (Reprinted by permission from:
Rockwood CA, Jr. Disorders of the sternoclavicular joint. In: Rockwood
CA, Jr, Matsen FA, III, eds. The Shoulder: Philadelphia: WB Saunders, 1990;477–525.
-
-
The medial clavicular physis is the last physis to fuse, usually at the age of 23–25 years.
-
A presumed sternoclavicular dislocation in a patient <25 years old may be a physeal fracture rather than a dislocation.
-
The prognosis for physeal fractures is better than that for dislocations.
-
Etiology
-
Often a result of motor vehicle collisions or sports
-
2 common mechanisms:
-
Direct blow to medial clavicle:
-
Usually causes posterior dislocation
-
-
Lateral compression of shoulder:
-
Football pile up
-
Side-impact motor vehicle collision
-
-
Associated Conditions
High-energy injuries should have a full ATLS workup (2) to exclude additional thoracic, spinal, and extremity injury.
Signs and Symptoms
-
Patients may report history of direct blow or lateral compression injury.
-
Patients usually report pain with any movement of arm.
-
Worse with compressing shoulders together
-
Patient usually supports arm with the contralateral hand.
-
History
-
Ask about numbness or weakness in arms.
-
Ask about shortness of breath or difficulty with talking.
-
Ask about difficulty with swallowing.
Physical Exam
-
With anterior dislocations, the medial end of the clavicle will be more prominent than the contralateral side.
-
With posterior dislocations, the medial clavicle may no longer be palpable and a sulcus may be present.
-
The affected shoulder appears shortened and thrust forward.
-
Perform a thorough neurologic examination of both arms.
-
Compare pulses between arms.
-
Look for venous congestion in the neck and arms.
Tests
Imaging
-
Radiography:
-
The sternoclavicular joint is difficult to image on plain radiographs.
-
A chest radiograph may give some hint of deformity, and specialized views are difficult to obtain and interpret.
-
-
CT:
-
Provides most information about a sternoclavicular dislocation
-
Shows the bony anatomy of the dislocation
-
Shows what, if any, structures are being compressed in a posterior dislocation
-
Is the study of choice if a sternoclavicular joint dislocation is suspected
-
If a posterior dislocation is suspected, consider using CT angiography.
-
Differential Diagnosis
-
The sternoclavicular joints also can be sprained, for which the treatment is symptomatic sling use.
-
Other thoracic trauma, such as a
pneumothorax, can cause shortness of breath, in which case the ATLS
protocol should be followed.
P.423
Initial Stabilization
-
In general, sternoclavicular dislocations should be reduced.
-
Anterior dislocations often are unstable after reduction, but most orthopaedic surgeons prefer an attempt at reduction.
-
Posterior dislocations always should be reduced and usually are stable thereafter.
General Measures
-
Reduction of a sternoclavicular joint
dislocation often can be performed closed, but general anesthesia or
deep sedation often is necessary secondary to pain and muscle spasm. -
Reduction of an anterior dislocation:
-
Position the patient supine with a 3–4-inch bolster between the scapulae.
-
A common error is to use too small a bolster.
-
Abduct the affected shoulder to 90°.
-
Extend the affected shoulder 15°.
-
Have the assistant apply traction to affected arm.
-
Apply direct posterior pressure to the medial clavicle.
-
Place the affected arm in a figure-8 bandage or sling and swath after reduction.
-
-
-
Reduction of a posterior dislocation:
-
Position the patient supine with a 3–4-inch bolster between the scapulae.
-
A thoracic surgeon should be involved
when reducing a posterior dislocation because a clavicle pulled from a
punctured subclavian vessel or lung can lead to a catastrophic
intrathoracic hemorrhage or pneumothorax. -
2 common techniques of closed reduction:
-
Abduction traction technique; apply
traction to the abducted, extended arm; apply downward pressure to the
shoulder over the glenohumeral joint; grasp the medial clavicle with
fingers and attempt to pull the clavicle anteriorly; if closed
manipulation fails, prepare the skin and use a sharp towel clamp to
grasp the medial clavicle and pull it anteriorly; the clavicle usually
reduces with an audible and palpable pop. -
Adduction traction technique:
-
Adduct the arm; apply lateral traction to
the adducted arm; push down on the shoulder over the glenohumeral
joint; if needed, grasp the medial clavicle with fingers or a sterile
towel clamp; after reduction, place the arm in a sling and swathe or
figure-8 dressing.
-
-
-
Activity
-
The affected arm should be immobilized for 4–6 weeks after reduction.
-
Patients may benefit from sleeping upright (i.e., in a recliner) for pain relief and comfort.
Nursing
-
Patients should have parenteral access and adequate pain relief.
-
Patients may be more comfortable sitting upright with a sling until definitive treatment is rendered.
Special Therapy
Physical Therapy
-
Hand and wrist exercises and elbow ROM exercises can begin immediately.
-
Shoulder exercises usually should wait 4–6 weeks.
Medication
-
Medications for pain control are appropriate.
-
Parenteral and oral narcotics in the acute setting
-
-
NSAIDs in the acute and chronic settings
Surgery
-
Posterior dislocations for which closed reduction has failed should undergo open reduction in the operating room.
-
A thoracic surgeon should be present.
-
After open reduction, the stability of the joint is assessed (often, it is stable).
-
Unstable joints may be stabilized with one of many suture techniques and a graft reconstruction.
-
Kirschner wire or Steinmann pin fixation
are contraindicated secondary to the disastrous sequelae of implant
migration into the mediastinum.
-
-
Posterior dislocations untreated for >7–10 days after injury often require open reduction because of retrosternal adhesions.
-
In most cases, anterior dislocations with instability or residual deformity may be treated nonoperatively.
-
Residual anterior subluxation or dislocation usually causes few functional problems.
-
Symptomatic patients may be treated using open reduction and stabilization, much like patients with a posterior dislocation.
-
-
A patient with a sternoclavicular joint dislocation should be referred to an orthopaedic surgeon for follow-up.
-
Shoulder ROM exercises usually can be started at 4–6 weeks.
-
In stable reductions, a sling and swathe or figure-8 dressing usually is worn for 4–6 weeks.
-
Unstable anterior dislocations can be treated symptomatically with a sling until symptoms resolve.
Prognosis
-
Posterior dislocations usually are stable after reduction.
-
Anterior dislocations often are unstable, but the instability causes few functional deficits.
-
An unstable anterior dislocation usually remains prominent with a cosmetic deformity.
-
Complications
-
The most disastrous complications occur with posterior sternoclavicular dislocations (3).
-
Compression or laceration of great vessels
-
Compression of trachea, resulting in respiratory compromise
-
Compression of esophagus, causing swallowing difficulties
-
Brachial plexopathy
-
TOS
-
-
Anterior dislocations can have sequelae as well, but they are much more benign.
-
Cosmetic deformity (less than a surgical scar)
-
Degenerative changes
-
Recurrent instability and pain with activity
-
Patient Monitoring
Patients should be followed until pain resolves and motion and function are restored.
References
1. Wirth
MA, Rockwood CA, Jr. Injuries to the sternoclavicular joint. In:
Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults,
5th ed. Philadelphia: Lippincott Williams & Wilkins, 2001:1245–1294.
MA, Rockwood CA, Jr. Injuries to the sternoclavicular joint. In:
Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults,
5th ed. Philadelphia: Lippincott Williams & Wilkins, 2001:1245–1294.
2. American
College of Surgeons Committee on Trauma. Advanced Trauma Life Support
Program for Doctors, 6th ed. Chicago: American College of Surgeons,
1997.
College of Surgeons Committee on Trauma. Advanced Trauma Life Support
Program for Doctors, 6th ed. Chicago: American College of Surgeons,
1997.
3. Gove N, Ebraheim NA, Glass E. Posterior sternoclavicular dislocations: A review of management and complications. Am J Orthop 2006;35:132–136.
Additional Reading
Bicos J, Nicholson GP. Treatment and results of sternoclavicular joint injuries. Clin Sports Med 2003;22:359–370.
Rudzki JR, Matava MJ, Paletta GA, Jr. Complications of treatment of AC and sternoclavicular joint injuries. Clin Sports Med 2003;22:387–405.
Wirth MA, Rockwood CA, Jr. Acute and chronic traumatic injuries of the sternoclavicular joint. J Am Acad Orthop Surg 1996;4:268–278.
Codes
ICD9-CM
839.61,839.71 Dislocation, sternoclavicular joint
FAQ
Q:
If a patient has a posterior sternoclavicular joint dislocation and
difficulty with swallowing, shortness of breath, difficulty with
talking, or neck venous distention, how urgent is the condition?
If a patient has a posterior sternoclavicular joint dislocation and
difficulty with swallowing, shortness of breath, difficulty with
talking, or neck venous distention, how urgent is the condition?
A:
In this scenario, the patient should be emergently transferred to a
facility with a CT scanner and a thoracic or trauma surgeon. The medial
clavicle has injured or compressed 1 of several important mediastinal
structures: The trachea, esophagus, and/or the subclavian vessels.
In this scenario, the patient should be emergently transferred to a
facility with a CT scanner and a thoracic or trauma surgeon. The medial
clavicle has injured or compressed 1 of several important mediastinal
structures: The trachea, esophagus, and/or the subclavian vessels.
