Stress Fracture
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Stress Fracture
Stress Fracture
John H. Wilckens MD
Simon C. Mears MD, PhD
Description
-
A stress (microscopic) fracture occurs when:
-
Repetitive stresses are applied to a bone faster than it is able to remodel to withstand this challenge.
-
As the stressing force continues, the bone gradually fatigues and eventually breaks.
-
Remodeling occurs in response to the stress but does not happen quickly enough to prevent the break.
-
-
Suddenly increased forces are applied to
a normal bone (e.g., a metatarsal stress fracture that occurs in a
military recruit who marches 20 miles without adequate conditioning).
-
-
Related to the stress fractures is the
insufficiency fracture, in which normal forces cause a fracture of
weakened bone (e.g., a femoral neck fracture in an osteopenic elderly
woman). -
Weightbearing bones of the lower extremity are affected, most commonly:
-
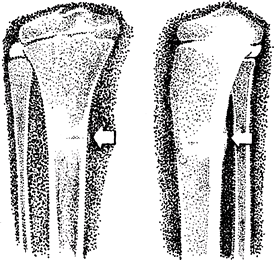
Metatarsus (Fig. 1)
-
Calcaneus
-
Tibia (Fig. 2)
-
Fibula
-
Femoral neck
-
-
Classification/radiographic grading (1):
-
Grade I: Normal radiograph, positive STIR
-
Grade II: Normal radiograph, positive STIR, positive T2-weighted MRI
-
Grade III: Periosteal reaction on radiograph, positive T1- and T2-weighted MRI, STIR without definite cortical break
-
Grade IV: Fracture line or periosteal reaction, fracture line on T1- and T2-weighted MRI
-
-
Synonyms: March fracture; Fatigue fracture
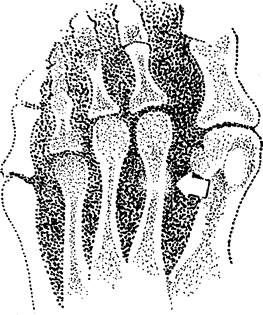 Fig.
Fig.
1. Stress fracture of the foot most commonly involves the metatarsal
shafts. It is signified by sclerosis or a periosteal reaction (arrow).
General Prevention
-
Avoid sudden increases in physical activity levels, especially when involving walking or running.
-
Runners should be educated to reduce mileage and to rest when they have acute, new-onset pain with activity.
Epidemiology
-
Can occur at any age (2):
-
Typically, people ≤60 years old develop stress fractures after sustained or cyclic exertion.
-
Persons >60 years old develop stress fractures from normal stress to a weak bone.
-
Incidence
-
Stress and insufficiency fractures occur more often in females than in males.
-
Commonly occur in:
-
Running and jumping athletes
-
5% of military recruits (3)
-
In a recent study, elite tennis players had a 12% rate of stress fracture (4).
-
Prevalence
Femoral stress fractures occur at a rate of 20 per 100,000 person-years; 1/2 are within the femoral neck (5).
Risk Factors
-
Female triad (eating disorder, amenorrhea, stress fracture [osteoporosis])
-
Rapid change in conditioning program:
-
>10% increase in running mileage per week
-
Military recruit in boot camp
-
-
Skeletal malalignment:
-
Pes cavus, pes planus
-
Excessive external rotation of the hip
-
-
Muscle fatigue: as muscles fatigue, they absorb less shock, which is transmitted to the bone (e.g., marathon running).
-
Low bone density
-
Gender: Female recruits have higher rates of stress fracture than do male recruits (6).
-
Low aerobic fitness is a predictor of stress fracture in recruits (7).
![]() Fig. 2. Stress fracture of the tibia, with sclerosis and periosteal reaction.
Fig. 2. Stress fracture of the tibia, with sclerosis and periosteal reaction.
Etiology
-
Sudden increase in strenuous activity in young people
-
Minimal stress in people with weak or osteopenic bone
Associated Conditions
-
Osteopenia
-
Metabolic bone disease
-
Female triad
Signs and Symptoms
-
The patient initially presents with a 2–3-week history of a vague, dull ache with exertion or impact loading.
-
As the injury progresses, the pain becomes sharper and localized and begins earlier in training.
-
If a stress fracture progresses to complete (macroscopic) fracture, pain occurs at rest.
Physical Exam
-
Antalgic gait may be present.
-
Point tenderness is noted in the affected bone.
-
Observe swelling and thickening of the soft tissues over the affected bone.
-
Pain in the hip with resisted active straight-leg raise (Stinchfield sign).
Tests
Lab
No serum laboratory tests
Imaging
-
Radiography:
-
Plain radiographs (AP and lateral views) typically do not show findings until 2 weeks after the onset of symptoms.
-
What usually is observed is healing, periosteal callus, or sclerosis at the fracture site.
-
-
Bone scan:
-
Very sensitive
-
Findings may be delayed 48–72 hours in elderly patients with insufficiency fractures.
-
-
MRI:
-
Very sensitive
-
Allows for classification and prognosis
-
Can rule out other soft-tissue injuries in the differential diagnosis
-
Differential Diagnosis
-
Infection
-
Fracture
-
Soft-tissue injury
-
Exertion or chronic compartment syndrome
-
Tumor
P.425
General Measures
-
In general, the patient must reduce activity below the threshold of pain.
-
If the patient has pain with walking, crutches should be used.
-
If the patient has pain with motion, or at rest, the injured part should be immobilized in a cast or fracture splint.
-
Activity
-
After initial treatment, activity should be increased gradually.
-
Once the patient is pain free, low-impact training can be started and advanced as tolerated.
-
Once running is resumed, mileage should be increased slowly.
Special Therapy
Physical Therapy
-
Identify training errors that led to the stress fracture.
-
Identify and correct mechanics and muscle imbalance.
-
Core strengthening
Medication
NSAIDs can be given, but they have an inhibitory effect on bone healing, making them a controversial intervention.
First Line
Acetaminophen
Surgery
-
For high-risk stress fractures:
-
Fractures whose displacement would cause catastrophic complications:
-
Femoral neck fractures require emergent
internal fixation because a complete, displaced femoral neck fracture
is associated with a high incidence of AVN (8).
-
-
Fractures associated with a high rate of delayed union or nonunion (8): Patella, tarsal navicular, talus
-
Disposition
Issues for Referral
High-risk fractures (see what has been determined previously)
Prognosis
-
Stress fractures in young people have a good prognosis.
-
Older patients or those with metabolic bone disease typically continue to develop insufficiency fractures in other bones.
-
Time to return to full activity (1):
-
Grade I: 3+ weeks
-
Grade II: 5+ weeks
-
Grade III: 11+ weeks
-
Grade IV: 14+ weeks
-
Complications
-
Completion of fracture, the most common
complication of stress fractures, substantially prolongs healing and
may require internal fixation. -
Continued pain even after fracture healing may occur.
Patient Monitoring
Radiographs are obtained every 4–6 weeks to monitor progress to healing.
References
1. Arendt
E, Agel J, Heikes C, et al. Stress injuries to bone in college
athletes: a retrospective review of experience at a single institution.
Am J Sports Med 2003;31:959–968.
E, Agel J, Heikes C, et al. Stress injuries to bone in college
athletes: a retrospective review of experience at a single institution.
Am J Sports Med 2003;31:959–968.
2. Bennell
K, Grimston S. Risk factors for developing stress fractures. In: Burr
DB, Milgrom C, eds. Musculoskeletal Fatigue and Stress Fractures. Boca
Raton: CRC Press, 2001:35–54.
K, Grimston S. Risk factors for developing stress fractures. In: Burr
DB, Milgrom C, eds. Musculoskeletal Fatigue and Stress Fractures. Boca
Raton: CRC Press, 2001:35–54.
3. Armstrong DW, III, Rue JPH, Wilckens JH, et al. Stress fracture injury in young military male and females. Bone 2004;35:806–816.
4. Maquirriain J, Ghisi JP. The incidence and distribution of stress fractures in elite tennis players. Br J Sports Med 2006;40:454–459.
5. Niva MH, Kiuru MJ, Haataja R, et al. Fatigue injuries of the femur. J Bone Joint Surg 2005;87B: 1385–1390.
6. Gam
A, Goldstein L, Karmon Y, et al. Comparison of stress fractures of male
and female recruits during basic training in the Israeli anti-aircraft
forces. Mil Med 2005;170:710–712.
A, Goldstein L, Karmon Y, et al. Comparison of stress fractures of male
and female recruits during basic training in the Israeli anti-aircraft
forces. Mil Med 2005;170:710–712.
7. Shaffer RA, Rauh MJ, Brodine SK, et al. Predictors of stress fracture susceptibility in young female recruits. Am J Sports Med 2006;34:108–115.
8. Boden BP, Osbahr DC. High-risk stress fractures: Evaluation and treatment. J Am Acad Orthop Surg 2000;8:344–353.
Additional Reading
Brukner PD, Bennell KL. Stress fractures. In: O’Connor FG, Wilder RP, eds. Textbook of Running Medicine. New York: McGraw-Hill, 2001:227–256.
Codes
ICD9-CM
733.11 Stress fracture
Patient Teaching
Gradual increase in training intensity (e.g., <10% in running mileage per week)
Prevention
-
Patient education:
-
With new-onset pain with activity, the patient should rest and reduce training.
-
The patient should try to identify and correct any training errors.
-
FAQ
Q: Do all high-risk stress fractures require surgery?
A:
No. These fractures can be treated with prolonged nonweightbearing and
immobilization. However, they are associated with a high risk of
nonunion. Surgical fixation allows earlier weightbearing, less
immobilization, improved predictable healing, and earlier return to
activity.
No. These fractures can be treated with prolonged nonweightbearing and
immobilization. However, they are associated with a high risk of
nonunion. Surgical fixation allows earlier weightbearing, less
immobilization, improved predictable healing, and earlier return to
activity.
Q: Can you get a stress fracture in nonweightbearing bone?
A:
Any bone subjected to an increased mechanical load (including
repetitive muscle use) can develop stress fractures. For example,
overhead athletes, such as pitchers, can develop stress fractures in
the humerus and olecranon, and rowers can develop stress fractures of
the ribs.
Any bone subjected to an increased mechanical load (including
repetitive muscle use) can develop stress fractures. For example,
overhead athletes, such as pitchers, can develop stress fractures in
the humerus and olecranon, and rowers can develop stress fractures of
the ribs.
Q: When can an athlete return to activity?
A:
Athletes with stress fractures can participate in “active rest,”
decreasing their activity below the threshold of pain. If an athlete
has a stress fracture in a weightbearing bone, then core strengthening
and balancing exercises and aquatic (or hydroaerobic) exercises can be
done. Once pain-free, an athlete can begin low-impact aerobics, such as
stationary cycling or elliptical training. If the athlete is pain free
with these activities, jogging and sports-specific activities can be
begun.
Athletes with stress fractures can participate in “active rest,”
decreasing their activity below the threshold of pain. If an athlete
has a stress fracture in a weightbearing bone, then core strengthening
and balancing exercises and aquatic (or hydroaerobic) exercises can be
done. Once pain-free, an athlete can begin low-impact aerobics, such as
stationary cycling or elliptical training. If the athlete is pain free
with these activities, jogging and sports-specific activities can be
begun.