Pelvic Fractures: Sacral Fixation
injury, most commonly they occur as one component of a pelvic ring
injury. Notoriously difficult to diagnose on plain films, a sacral
injury is often found by a surgeon who displays a high index of
suspicion based on the mechanism of injury and physical examination.
Even nondisplaced or minimally displaced sacral fractures may be
unstable and have the potential to displace prior to healing.
Therefore, the orthopedic surgeon is challenged to identify and treat
sacral fractures knowing that these injuries are at high risk for
displacement. Information such as the pattern of the sacral fracture,
its location, disruption of surrounding bone and soft-tissue
structures, mechanism of injury, and the severity of the anterior
pelvic-ring injury must be considered by the surgeon determining the
inherent stability of a sacral fracture.
their relationship to the sacral foramina. This classification system
correlates with neurologic injury as well. Zone I injuries are lateral
to the sacral foramina and are associated with L5 nerve-root injuries
in 20% to 25% of cases. Fractures through the sacral foramina are zone
II injuries, and injury to the sacral nerve roots occur in up to 50% of
patients with this type of fracture. If the fracture is medial to the
sacral foramina, the injury is in zone III, and neurologic injury with
bowel and/or bladder dysfunction occurs in up to 70% of zone III
patients.
with a short period of bed rest followed by mobilization and protected
weight bearing until healed. Prolonged bed rest or traction is not
recommended in unstable injuries because of the inherent risks of deep
venous thrombosis, pressure ulceration, and aspiration or pneumonia.
Frequent radiographic follow-up is mandatory to identify fractures
that, although initially thought to be stable, subsequently displace
following mobilization. Sacral fractures medial to the L5–S1 facet
joint are more constrained by the disc and facet joint capsule and are
less prone to displacement than alar or transforaminal fractures.
Fractures caused by a lateral
compression mechanism are also less likely to displace than anterior-posterior compression and “vertical shear” injuries.
reduction and fixation. Because instability is often difficult to
ascertain, displacement is more often cited as the indication for
surgical treatment. Displacement of greater than 1 cm in the posterior
pelvic ring is generally accepted as an indication for reduction and
fixation. Complex pelvic-ring injuries that include a sacral fracture
may also benefit by fixation such that patient mobilization is
improved. Reduction and fixation of displaced sacral fractures that are
associated with neurologic injury may help improve the chance for
neurologic recovery. As with any injury, associated traumas, medical
comorbidities, patient age, and preinjury functional level must be
considered in determining appropriate treatment.
evaluation and resuscitation with basic and advanced trauma life
support (ATLS) protocols are essential. The evaluation of patients with
a pelvic ring injury includes a visual examination and palpation of the
back, buttocks, flank, groin, and perineum so the integrity of the skin
and soft tissues can be assessed. The presence of a fluid wave, a local
area of fluctuance, or a well-circumscribed area of cutaneous
anesthesia may identify a Morel-Lavaleé lesion or internal degloving.
To exclude the presence of an occult open fracture or an associated
injury to the rectum or genitourinary tract, the surgeon must conduct
thorough rectal and vaginal examinations and document the neurologic
status of the limbs.
anteroposterior (AP) radiograph of the injured pelvis. Although the
presence of a sacral fracture may be difficult to ascertain on this
film, interruption of the arcuate lines of the sacral neural foramina,
avulsions of the transverse processes of L5 and/or sacrospinous or
sacrotuberous ligamentous avulsions, or asymmetry of the posterior
pelvis should prompt further evaluation. The 40-degree caudad (inlet)
and 40-degree cephalad (outlet) projections as well as a computed
tomography (CT) scan allow the surgeon to evaluate further the
integrity of the anterior and posterior pelvic ring. Occasionally,
obturator and iliac oblique views give further information about a
posterior pelvic injury.
the soft tissues as well as the fracture pattern and stability. If
operative treatment is selected, the status of the posterior
soft-tissue envelope must be critically assessed. If the condition of
the soft tissues is unsatisfactory, then open treatment of the sacral
fracture should be deferred until an exposure can be made safely
through a viable soft-tissue envelope.
to 7 days to allow the patient’s condition to stabilize, to obtain
appropriate imaging studies, and to assemble the operative team.
However, if the fracture is well delineated, the surgeon has all the
necessary resources available, and the patient is clinically stable,
surgery need not be delayed. Indications for early intervention are
control of bleeding, debridement of open fractures, or a patient who
requires emergent surgery for other reasons and has no
contraindications to proceeding with pelvic fixation. In patients with
degloving injuries, debridement of devitalized tissue or drainage of
hematoma may be necessary before definitive fixation.
reduced before fixation of an associated, anterior, pelvic-ring or
acetabular fracture. If only two sites of injury are found in the
pelvic ring, anterior ring reduction and fixation often indirectly
assists the reduction of the sacral fracture. When more than two zones
of injury exist, malreduction of one component of the pelvic ring may
preclude an anatomic reduction of the posterior pelvic ring or
acetabulum.
attempted because if successful, a percutaneous iliosacral-screw
fixation can often be utilized. If the closed reduction is
unsuccessful, however, the surgeon must be prepared to proceed with
open reduction and
internal fixation (ORIF), if the soft tissues allow, rather than accept a posterior pelvic-ring malreduction.
anesthesia in the prone position on a radiolucent table. The thorax is
supported on bolsters, and the face is appropriately positioned and
padded. Pillows are placed beneath the thighs to equal the height of
the bolsters. This prevents loss of lumbar lordosis and a flexed
position of the pelvis, which makes obtaining and interpreting oblique
radiographic projections difficult. The pelvis itself is not directly
supported because bolsters pressing directly against the anterior
superior spines may be a deforming force on the pelvic ring. The knees
are flexed and the tibiae rest on a padded support (Fig. 40.1).
Hip extension and knee flexion relax the sciatic nerve as well as
improve safety when access through the greater sciatic notch is needed.
The surgical field should include the entire pelvis, including the
contralateral posterior–superior iliac spine (PSIS) and the ipsilateral
greater trochanter, for possible placement of distractors or clamps.
The patient is not routinely placed in skeletal traction because it
often rotates the pelvis rather than contributes to the reduction.
Likewise, the use of a perineal post may be a deforming force against
the anterior pelvic ring and may result in difficulty obtaining an
anatomic reduction of the posterior injury.
The subcutaneous tissue is incised down to the fascia of the gluteus
maximus muscle. The gluteus maximus muscle must be reflected laterally
so that its neurologic and vascular supplies are preserved. The gluteus
maximus originates from the posterior iliac crest, the fascia of the
multifidus, and the spinous processes of the sacrum. Failure to release
the maximus from its origin will result in an obligatory
devascularization and denervation of any muscle left behind. Although
fasciocutaneous flaps are generally preferred, elevating the gluteus
fascia off the muscle belly can make repair of the maximus muscle
impossible. The subcutaneous tissue is elevated medially off of the
surface of the maximus fascia to the origin of the muscle, and the
maximus is then elevated subperiosteally from the ilium and sharply off
of the multifidus fascia (Fig. 40.3). The maximus can be elevated as far laterally as needed for
exposure but in most circumstances need not be elevated much beyond the crista gluteae (Fig. 40.4).
 |
|
Figure 40.1.
The patient is positioned prone with the hips extended and the knees flexed on the radiolucent table. The chest and thighs are supported on bolsters leaving the pelvis free for manipulation. |
 |
|
Figure 40.2.
The skin incision is drawn for open reduction of a sacral fracture. The planned incision is vertical and 2 cm lateral to the palpable posterior superior iliac spine. Both hemipelvises are draped into the surgical field while the perineum is excluded. |
 |
|
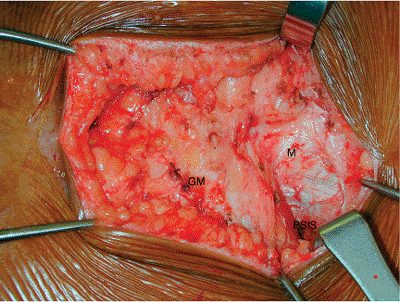
Figure 40.3. The skin and subcutaneous tissues have been elevated off the fascia of the gluteus maximus. The gluteus maximus (GM) is seen at the insertion onto the multifidus fascia (M). The posterior superior iliac spine (PSIS) is exposed in the cranial portion of the wound.
|
 |
|
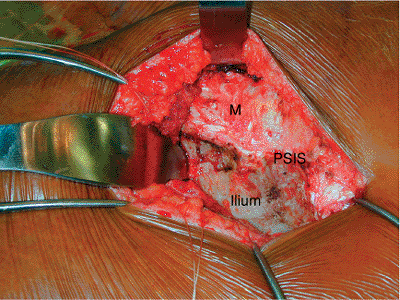
Figure 40.4.
Further lateral dissection of the gluteus maximus off of the ilium has been performed. The greater sciatic notch is exposed and a cobra retractor is in place. The multifidus (M) fascia has not been disturbed. |
the anterior and lateral edge of the sacrum, and the greater sciatic
notch can be cleaned from medial to lateral. The superior-gluteal
neurovascular bundle will be encountered in the lateral portion of the
notch. Curved elevators can be used along with manual techniques to
dissect along the anterior aspect of the sacroiliac joint and as far
medial as the palpable, ventral, sacral-nerve roots. The ventral,
sacral, neural foraminae of S1 thorough S4 should be palpable. The
erector spinae is then elevated off the dorsal surface of the sacrum as
far medially as needed for fracture visualization. The dorsal cutaneous
nerves emanating from the dorsal sacral foramina are visualized but are
often injured, particularly in transforaminal sacral fractures.
Periosteum is cleaned from the dorsal surface of the sacrum while the
surgeon takes particular care to preserve fracture edges that can be
used to help assess the reduction (Fig. 40.5).
of a lamina spreader or a femoral distractor, with pins placed in both
PSIS. The ventral sacral-nerve roots can be visualized in zone II
fractures, and any bony fragments that might impinge on the nerves can
be removed at this time.
the ilium to the spinous process of S3 or S4. The surgeon should make a
careful examination of the preoperative CT scan to identify the
presence of a lower-sacral spina-bifida occulta, which would prevent
safe clamp placement in this location. Varying the location of the
clamp position on the ilium can result in a more posterior or anterior
direction of pull and can help fine-tune the reduction. A second clamp
can be placed more transversely to aid in fracture compression (Fig. 40.6).
To avoid damaging the ventral nerve roots, the reduction of the sacral
fracture must be accurate and the nerve roots free of impinging bony
fragments before significant compression is applied at the fracture
site.
foramina, the surgeon may want to utilize a midline approach and place
the incision directly over the spinous processes. The multifidus may be
elevated subperiosteally, from medial to lateral, off of the sacral
lamina. Reduction clamps may be placed from ilium to ilium or directly
onto the dorsal surface of the sacrum through unicortical drill holes.
Pins placed bilaterally in the PSIS can be used to distract and clean
the fracture as well as assist in the reduction.
 |
|
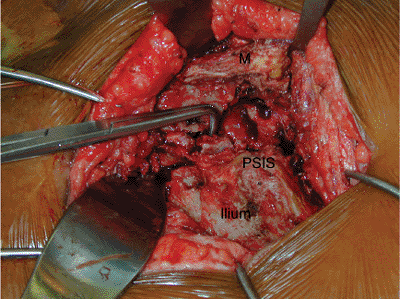
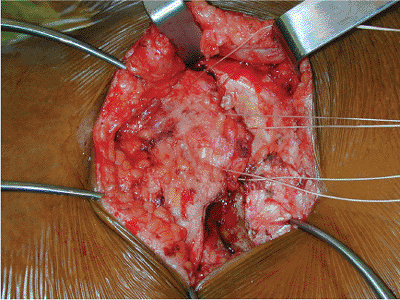
Figure 40.5.
The multifidus and erector spinae have been elevated subperiosteally off of the dorsal surface of the sacrum. The comminuted sacral fracture is exposed. |
 |
|
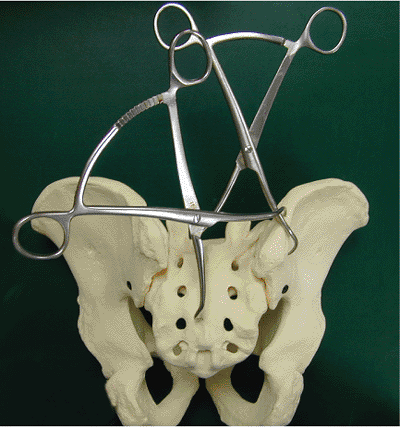
Figure 40.6.
Clamp placement shown on a sawbone model of a transforaminal sacral fracture. One clamp is used to control cranial displacement of the hemipelvis. The more transversely oriented clamp helps compress the fracture. |
sacral fractures. They include the use of iliosacral screws, posterior
iliosacral plating, dorsal sacral plating, and lumbopelvic fixation.
The use of iliosacral screws is the most common method of fixation of
sacral fractures. If the fracture can be reduced by closed means,
insertion of percutaneous iliosacral screws can be done with the
patient in either the supine or prone position.
bilateral sacral fractures in zones I or II. Fractures in zone III are
also amenable to this technique, but great care must be used in screw
placement so that iatrogenic nerve injury is avoided. A thorough
understanding of the direction of fracture displacement improves the
surgeon’s chances of reducing the fracture by closed means. A closed
reduction is attempted by traction to correct axial displacement.
Percutaneously inserted Schantz screws, pointed pelvic-reduction
clamps, a femoral distractor placed in the posterior iliac spines, or a
spiked pusher to close gaps or disimpact fractures are useful
instruments for adjunctive techniques of fracture reduction. Once a
reduction has been obtained and confirmed fluoroscopically, provisional
fixation with clamps, Kirschner (K) wires, or external fixation is
useful to hold the fracture prior to definitive iliosacral-screw
fixation. If a satisfactory reduction cannot be accomplished by closed
means, the surgeon should proceed to open reduction.
verified with the image intensifier. Only then can internal fixation be
safely done. The height of the sacral ala should be compared
bilaterally on the cephalad projection (outlet view), and the sacral
neural foramina should appear bilaterally symmetric. On the caudad
projection (inlet view), the contour
of
the posterior pelvis should appear bilaterally symmetric, and the
reduction can be checked by restoration of the sacral alar line. The
most common means of internal fixation for sacral fractures are
iliosacral screws. Because the ideal direction of these screws should
be perpendicular to the sacral fracture, the screws are inserted
through a separate, small, lateral incision. Two partially threaded,
large-fragment lag screws are generally placed in the first sacral
segment. The length of these screws should be sufficient that the
threads of the lag screw lie within the body of S1. As this bone is
more dense than the alar bone, longer screws, although they may improve
resistance to shear, may not have the pullout strength and
interfragmental compression of screws with threads that lie within the
body of S1. When closed reduction and percutaneous screws are used,
some surgeons favor fully threaded screws to avoid overcompression of
the fracture and impingement on the sacral nerve roots. When open
reduction is performed, the reduction is directly visualized and this
is less of a concern. In any case, interfragmentary compression is
recommended to improve the initial fracture stability.
significantly displaced sacral fractures that are not adequately
stabilized by iliosacral screws alone. On occasion, when iliosacral
screws are tightened, gapping occurs at the caudal portion of the
fracture. In our experience, this is a good indication to supplement
the iliosacral screw construct with a posterior tension-band plate. The
plate may also provide limited interfragmentary compression to the
fracture. Although it may be utilized as a stand-alone implant, the
resultant force applied when the tension band plate is secured to the
bone may result in an external rotation deformity through one or both
sides of the pelvis, particularly if the fracture is not already
secured with iliosacral screw fixation.
on the contralateral side of the pelvis, and a limited portion of the
gluteus maximus is reflected off the erector spinae fascia. A straight
10- or 12-hole, 3.5- or 4.5-mm reconstruction plate is used. The
optimal position of the dorsal tension band plate is just below the
PSIS. This decreases plate prominence and ensures that the screws in
the ilium are anchored in the strong bone of
the
sciatic buttress. The plate is typically inserted from the side of the
open reduction and tunneled through to the contralateral surgical site.
A 1/2-inch osteotome is passed from one incision, ventral to the
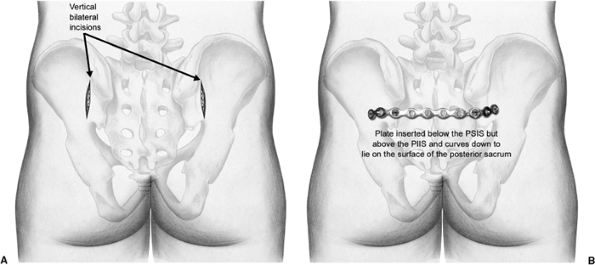
erector spinae fascia, osteotomizing the sacral spinous process of S2 (Fig. 40.7). The unbent straight pelvic reconstruction plate is then passed along the same track until visualized in the second incision (Fig. 40.8).
A screw is inserted bilaterally between the tables of the ilium into
the sciatic buttress. Tightening these screws adds tension to the plate
over the dorsum of the sacrum and causes compression of the sacral
fracture. The ends of the plate are then bent to the iliac wing in situ
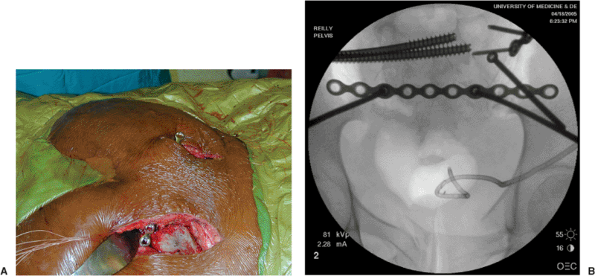
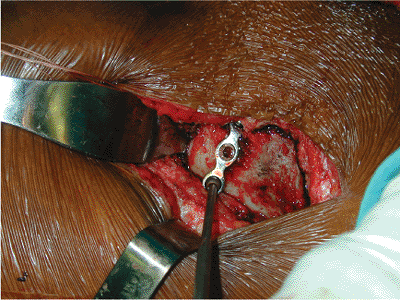
and secured with a single screw at each end of the plate (Figs. 40.9 and 40.10).
 |
|
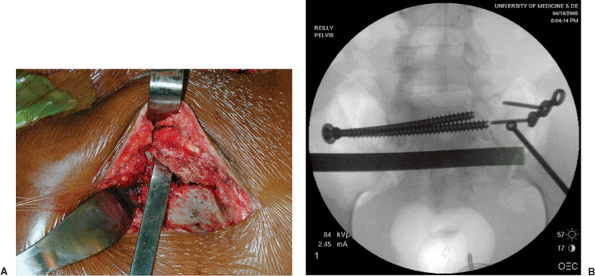
Figure 40.7. A. The osteotome is introduced ventral to the multifidus and utilized to osteotomize the spinous process of S2. B. Fluoroscopic image of in-place osteotome.
|
 |
|
Figure 40.8. A. The osteotome has been exchanged for the straight pelvic-reconstruction plate. B.
The plate has been secured to each posterior superior iliac spine by means of a 4.5-mm screw placed parallel to the greater sciatic notch between the tables of the iliac wings. |
 |
|
Figure 40.9.
The plate is bent to the iliac wing in situ. It will then be fixed with a bicortical screw directed toward the anterior aspect of the sacroiliac joint. |
 |
|
Figure 40.10. Schematic drawings of the bilateral skin incisions (A) and the final plate placement on the sacrum and iliac wings (B).
|
bilateral sacral fractures. Because the body of S1 may not
simultaneously accommodate the presence of multiple bilateral screws,
the number of screws or the lengths of those screws may need to be
compromised. In this circumstance, the plate may be utilized to augment
the iliosacral screw fixation. In pelvic malunion or nonunion
reconstruction, this can be a useful technique to supplement iliosacral
screw fixation and improve the strength of the initial fixation
construct.
 |
|
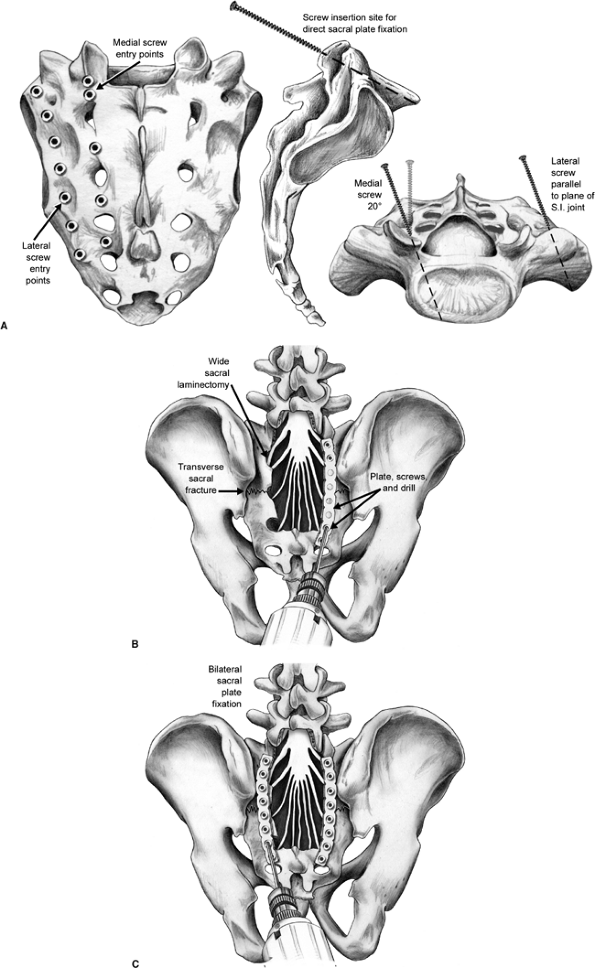
Figure 40.11. A.
Screw insertion sites for direct sacral-plate fixation. Lateral entry points are adjacent to the dorsal sacroiliac-ligament insertion, while medial entry points are midway between adjacent dorsal foramina. Lateral screws are directed parallel to the plane of the sacroiliac joint, while medial screws are directed perpendicularly to the dorsal sacral lamina. B,C. Plate fixation of a transverse sacral fracture is shown. This was performed in conjunction with a wide sacral laminectomy for nerve root decompression. |
the sacrum may be used in the fixation of zone III and selected zone II
sacral fractures. However, the plate is most commonly employed in the
treatment of transverse sacral fractures. Plates may be contoured to
sit lateral to the sacral foramina, and bicortical screw fixation is
achieved in the ala or body of each sacral segment (Fig. 40.11).
To prevent injuring the exiting ventral sacral-nerve roots, the surgeon
must have a thorough understanding of the intraosseous anatomy.
spared. Through a midline or lateral incision, the multifidus and
erector spinae muscles are elevated to expose the sacrum. During the
subperiosteal dissection, the surgeon must avoid entering the sacral
canal, which is at particular risk if the lamina is fractured. Once the
sacrum has been exposed, decompression of the sacral nerve roots is
performed, if indicated, and the fracture is reduced. Well-contoured
small-fragment plates are used to stabilize the fracture. To avoid
iatrogenic injury to the important adjacent-neurovascular structures,
particularly the L5 nerve root, the surgeon must have a thorough
understanding of the osseous, neural, and vascular anatomy.
with a short spanning plate with screws placed in each alar region.
Usually two plates are required and should be placed over the S1 and S3
regions. Intraoperative fluoroscopy is used to avoid foraminal or
central-canal hardware placement. If a displaced and/or unstable
anterior-pelvic injury exists, anterior stabilization should be
performed. Direct sacral plating is critical to neutralize the stress
on these small, relatively weak plates.
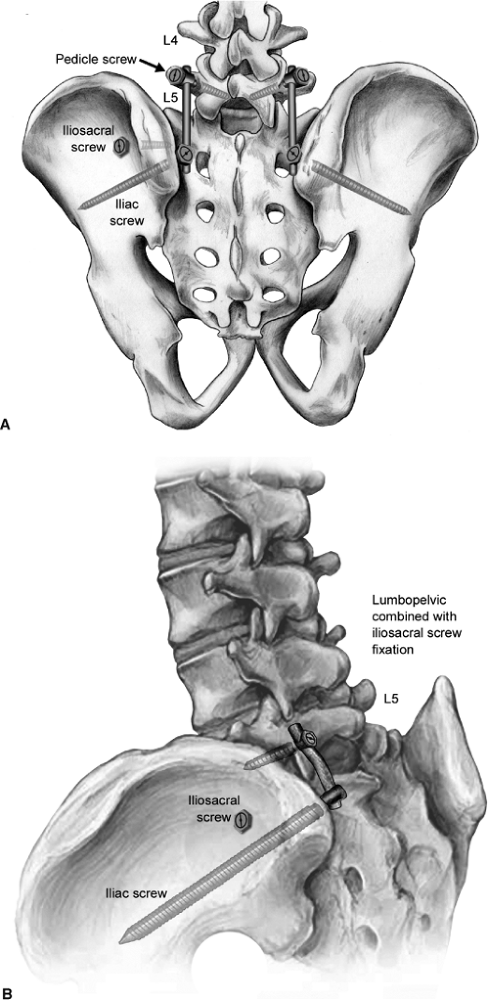
dissociation. Some H-type and U-type fractures result in the body of S1
(and sometimes S2) remaining attached to the spine while the sacral ala
remain attached to the pelvis. Although iliosacral screw fixation may
be successful in maintaining the reduction of the pelvis to the spine,
the most common deformity is kyphosis at the transverse portion of the
sacral fracture, which is caused when the pelvis flexes in relation to
the spine. Because this deformity is characterized by rotation around
the long axis of the iliosacral screw, the ability of screw fixation
alone to resist displacement is poor. In this circumstance, lumbopelvic
fixation has been shown to result in a stronger fixation construct. In
typical cases, pedicle screw fixation in L5 and/or L4 can be connected
to 1 or 2 screws placed between the tables of the ilia above the
greater sciatic notch (Fig. 40.12). Screws
should be placed within the sciatic buttress. They should be long
enough to pass over the greater sciatic notch to prevent flexion of the
pelvis on the lumbar spine (Fig. 40.13).
fracture, meticulous handling of the soft tissues is critical. The
wound should be copiously irrigated and complete hemostasis obtained.
In most cases, we favor the use of a suction drain deep to the fascia
to prevent hematoma formation. Anatomic closure of the gluteus and
thoracolumbar fascia should be accomplished (Fig. 40.14).
If the gluteus maximus is not correctly repaired, the soft-tissue
coverage over the sacrum may be compromised and the gluteal folds may
be asymmetric.
24 to 48 hours. In patients with considerable soft-tissue damage, a
longer duration of antibiotics may be indicated. We strongly recommend
deep venous thromboembolic prophylaxis in all patients unless specific
contraindications clearly prohibit such a precaution.
fracture, mobilization and protected weight bearing on the
contralateral side is continued for 8 weeks. Patients with bilateral
sacral fractures are mobilized from bed to chair, but weight bearing is
precluded for 8 weeks. If spino-pelvic fixation has been utilized,
patients are allowed protected weight bearing with crutches or a walker
and progressed to full weight bearing as tolerated.
the wound is healed, a rehabilitation program that emphasizes
range-of-motion exercises, as well as progressive resistance and
strengthening exercises, is begun. Radiographs are typically taken
postoperatively at 6 and 12 weeks. At 6 months, the patient is
critically assessed regarding pain, mobility, and general health
status. The three pelvic views are obtained and fracture union is
assessed. CT scans can be used to evaluate sacral fractures
postoperatively, but they are
not
as sensitive as plain radiographs at demonstrating residual cranial
displacement. Patients are reviewed at 6 months, 1 year, and yearly
thereafter. The patient may need up to 2 years to achieve maximal
medical and functional recovery.
 |
|
Figure 40.12. A,B. Lumbopelvic fixation is shown with pedicle screws in L5 and iliac screws placed into the sciatic buttress.
|
 |
|
Figure 40.13.
Lateral view of the sacrum showing unilateral lumbopelvic fixation augmenting iliosacral screw fixation of a comminuted sacral fracture. The iliac screw is seen to lie just cranial to the greater sciatic notch. (Courtesy of Sean Nork, MD.) |
 |
|
Figure 40.14.
The gluteus maximus is repaired to the multifidus fascia caudally and to the lumbodorsal fascia cranially. By preserving the gluteus maximus fascia, the surgeon can soundly repair the gluteus to cover the dorsum of the sacrum and restore the contour of the posterior soft tissues of the buttock. |
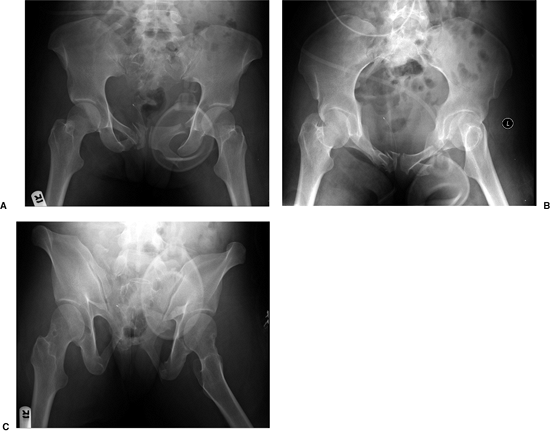
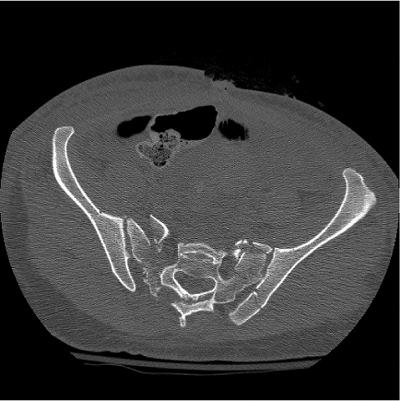
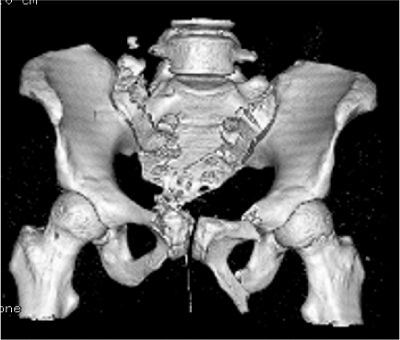
injury after being in a motor vehicle accident. She underwent emergent
laparotomy and repair of an intestinal injury. Her abdomen was packed
open. The AP, caudad, and cephalad views of the pelvis demonstrate
bilateral zone II sacral fractures as well as bilateral, superior and
inferior, ramus fractures; the right-sided fracture extends into the
pubic body (Fig. 40.15). Cranial displacement
of the right hemipelvis is found as is an adduction deformity of the
left hemipelvis. An axial CT scan demonstrates comminution of the
sacral fractures as well as a fracture of the PSIS that extends into
the sacroiliac joint on the left (Fig. 40.16). A three-dimensional CT reconstruction was also used to evaluate the patient’s condition (Fig. 40.17).
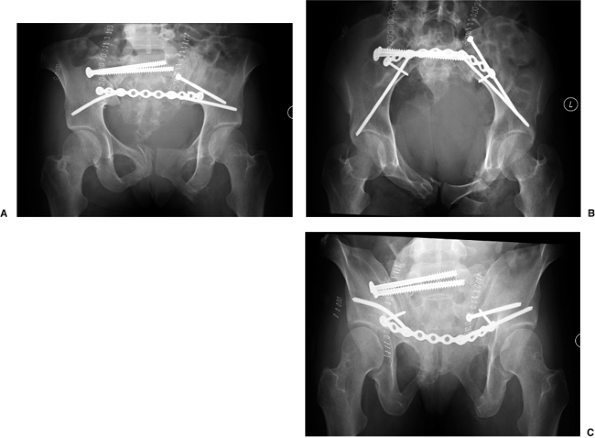
postoperative radiographs taken after open reduction and iliosacral
screw fixation of the right sacral fracture and lag screw fixation of
the left PSIS fracture. Because of the bilateral posterior pelvic-ring
injuries, dorsal tension-band plating
of
the sacrum was chosen to augment the screw fixation. The patient’s
abdomen was left open for an extended period because she experienced an
abdominal compartment syndrome. The anterior pelvic-ring injuries were
not operatively addressed and were allowed to heal without fixation.
 |
|
Figure 40.15.
Initial radiographs demonstrate the comminuted right-sacral fracture, left sacroiliac fracture-dislocation, and comminuted, bilateral, ramus fractures. A drain is seen superimposed due to the patient’s open abdomen. |
 |
|
Figure 40.16. Axial CT scan demonstrating comminuted zone II sacral fractures as well as a PSIS fracture-dislocation component on the left.
|
 |
|
Figure 40.17.
Three-dimensional CT scan helps to clarify the comminution of the sacral fractures as well as demonstrates the multiple sites of pelvic deformity. |
 |
|
Figure 40.18.
Postoperative radiographs after posterior pelvic-ring fixation. The fracture of the mammillary process of the right sacral ala may be mistaken for persistent gross cranial translation of the fracture. However, the heights of the iliac wings and the restoration of the sacral foramina seen on the cephalad view demonstrate that much of the displacement has been corrected. Persistent incongruity is seen in the left sacroiliac joint because of the comminution and impaction of the sacral side of the joint. The symphyseal fragment remains rotated. |
J, Varga E, Woodside T, et al. The strength of iliosacral lag screws
and transiliac bars in the fixation of vertically unstable pelvic
injuries with sacral fractures. Injury 1996;27: 561–564.
C, Simonian P, Agnew, SG, et al. Radiographic recognition of the sacral
alar slope for optimal placement of iliosacral screws: a cadaveric and
clinical study. J Orthop Trauma 1996;10(8):171.
T, Ledoux W, Chapman J, et al. Triangular osteosynthesis and iliosacral
screw fixation for unstable sacral fractures: a cadaveric and
biomechanical evaluation under cyclic loads. J Orthop Trauma 2003;17(1):22–31.
