Osteotomies Around the Hip
joint preservation surgery of the hip. This is owing to an enhanced
understanding of the pathogenesis of degenerative hip disease, improved
diagnostic imaging modalities, refined patient selection criteria, and
more sophisticated surgical techniques. Perhaps most important is an
appreciation of the significance of prearthritic and early arthritic
hip symptoms that commonly occur before irreversible joint
deterioration. These early symptoms provide a window of opportunity for
surgical intervention to remedy the underlying hip abnormality and to
improve the prognosis of early hip disease. The goals of joint
preservation surgery are to alleviate hip symptoms, improve the
functional capacity of the hip, and delay or prevent the biologic
cascade of degenerative hip disease. Osteotomy surgery about the hip is
one of the mainstay joint preservation strategies and will continue to
play a major role in the expanding field of hip preservation surgery.
Nevertheless, optimal clinical results of osteotomy surgery are
realized only through careful patient selection, detailed preoperative
planning, accurate surgical procedures, and supervised patient
rehabilitation. The goal of this chapter is to summarize the essential
concepts of hip osteotomy surgery. The fundamentals of patient
evaluation and the basics of osteotomy procedures will be presented for
the most common structural disorders of the hip.
United States as evidenced by the approximately 200,000 total hip
arthroplasties performed annually. The cause of hip osteoarthritis is
complex and multifactorial and continues to be an area in need of
investigation. Patient characteristics including age, gender, genetic
makeup, race, occupation, and activity level have all been identified
as factors that impact the pathophysiology of this disease. Most
relevant to hip joint preservation surgery is the known correlation
between structural hip disorders and secondary osteoarthritis. Harris
emphasized that over 90% of patients with osteoarthritis had an
underlying deformity of the joint that was present at the cessation of
growth. This concept underscores the theory that osteoarthritis of the
hip is very commonly associated with a pre-existing, mechanical
disorder. In the mechanically compromised hip, instability, abnormal
joint loading, and/or impingement can produce abnormal shear forces and
excessive loads per unit area at the articular surface and induce
premature degeneration of the involved articular cartilage. If left
untreated, progressive degenerative articular disease ensues and
secondary osteoarthritis can develop.
common structural deformity associated with secondary osteoarthritis
and serves as a model of this pathophysiologic cascade. The dysplastic
acetabulum is abnormally inclined in the superolateral direction and
does not provide adequate anterolateral femoral head coverage. This
leads to hip instability and anterolateral acetabular rim overload. As
a result of localized overload, labral disease ensues and adjacent
articular cartilage deterioration is initiated. Persistent instability
and localized joint overload accelerate articular cartilage
degeneration and secondary osteoarthritis.
the cause of the problem and establishing whether the hip joint is the
true source of symptoms. Referred pain from other anatomic regions,
most commonly the lumbar spine, needs to be excluded. The interview
should then elicit any history of childhood or adolescent hip disease,
previous hip surgery, hip trauma, risk factors for osteonecrosis, or a
history consistent with inflammatory arthritis. If the patient has
authentic hip symptoms, the duration, character, and location of pain
are determined. The examiner should question about episodes of
snapping, popping, or locking that may suggest soft tissue pathology
about the hip or a mechanical intra-articular component to the disease.
Activities that exacerbate symptoms should be noted. It is important to
delineate whether the patient experiences activity-related hip pain
consistent with abductor fatigue (lateral hip discomfort or tiring) or
instability and associated joint overload
(anterior
or groin discomfort). Alternatively, the symptoms may be more
consistent with anterior impingement disease (anterior or groin
discomfort) and exacerbation with hip flexion activities and prolonged
sitting. The severity of symptoms and functional limitations should
also be discussed as patients with early and less advanced symptoms are
usually better candidates for osteotomy surgery. The social history
should establish the occupation, activity level, and tobacco and
alcohol use habits of the patient. The overall medical condition and
patient capacity to comply with surgical treatment and rehabilitation
are other factors that need to be considered when contemplating
osteotomy surgery. The patient should understand the goals of treatment
and must be willing to actively participate in a relatively involved
postoperative rehabilitation program.
in evaluating a patient for hip osteotomy surgery. The general physical
status, including body height, weight, and apparent conditioning, is
noted. During examination, sitting posture and gait pattern are
observed. The hip is inspected with specific attention to the presence
and position of surgical scars. The Trendelenburg test and side-lying
abduction testing indicate the integrity of hip abductor strength.
Abductor weakness is a common finding in patients with early hip
disease. Leg-length determination is made with the patient standing,
noting the presence or absence of a balanced pelvis. Functional
leg-length inequality can be measured by noting the height of a block
placed under the short leg necessary to balance the pelvis.
Alternatively, measurement of true leg-length inequality can be made
with the patient supine, measuring from the anterior superior iliac
spine to the medial malleolus and comparing the measurement to the
contralateral side. The neurovascular status of the extremity should
also be determined, especially in patients with a history of previous
hip trauma and/or surgery.
the presence of pain and hip joint irritability during the motion
examination. When assessing hip range of motion it is important to
steady the pelvis with one hand while the examiner’s other hand ranges
the ipsilateral hip. This determines motion end points more accurately
because the examiner better appreciates forced motion of the pelvis
through the hip. With this technique hip flexion, abduction, adduction,
and rotation are recorded. Hip internal and external rotation both in
extension and flexion are measured. Restricted flexion and internal
rotation in flexion should be appreciated as this finding is common in
patients with anterior femoroacetabular impingement. Again, careful
appreciation of motion end points is important to accurately assess
true hip joint motion and to judge the joint suitability for osteotomy
surgery. The surgeon must verify that the hip has adequate range of
motion to accommodate the proposed reconstruction, because a hip with
inadequate motion may respond poorly to an osteotomy procedure. In
general, at least 90 degrees of hip flexion should be present. One
exception is the patient with a severe slipped capital femoral
epiphysis (SCFE) or a posttraumatic deformity in which restricted hip
flexion may be secondary to malalignment rather than degenerative
changes. In contrast, a patient being evaluated for acetabular
reorientation to correct classic acetabular dysplasia must demonstrate
adequate hip flexion (≥105 degrees) to tolerate the osteotomy, because
improved anterior coverage of the femoral head achieved with the
osteotomy will reduce hip flexion motion. Thus, during evaluation the
surgeon must determine that a functional motion (at least 90 degrees of
flexion) will be maintained postoperatively. Similarly, hip abduction
motion will be reduced with a varus-producing proximal femoral
osteotomy. Therefore, preoperative hip abduction motion must be
adequate (>30 degrees) to accommodate the surgical correction and to
maintain adequate clinical abduction postoperatively.
characterizing the underlying hip disease. The impingement test
(combined flexion, adduction, and internal rotation) is performed to
check for groin discomfort that may indicate labral pathology or the
presence of anterior femoroacetabular impingement. This test is also an
excellent screening maneuver for any intra-articular disease process
and can be extremely helpful in distinguishing an intra-articular from
an extra-articular disorder. Additionally, an apprehension test
(extension, adduction, and external rotation) evaluates anterior
stability of the hip. This maneuver elicits hip (groin) pain in the
setting of an unstable dysplastic hip with insufficient anterior
coverage and associated anterior instability. A positive test is common
with moderate to severe acetabular dysplasia, yet hips with mild
acetabular dysplasia may not be sensitive to anterior stability testing.
anatomy of the hip in a comprehensive fashion, determines the severity
of secondary osteoarthritis, and provides information regarding the
effect of osteotomy correction (congruency and joint space alteration).
A thorough radiographic examination of the hip is extremely important
in optimizing patient selection for surgery, preoperative planning, and
accurate surgical technique. To accomplish this, we obtain a full hip
series including a standing anteroposterior pelvis and false profile.
Frog and cross-table laterals of the hip are taken supine. When
considering an osteotomy, functional radiographs are obtained to check
congruency in a position mimicking the osteotomy. These radiographs are
performed with the surgeon or assistant holding the extremity and are
used to confirm clinical comfort in a position of radiographic
congruency. For example, a flexion-abduction view is obtained to assess
the hip articulation in anticipation of acetabular reorientation for
treatment of classic acetabular dysplasia. This radiograph mimics the
joint congruency and improved anterolateral femoral head coverage to be
achieved by the osteotomy. Similarly, an abduction functional view is
performed to assess the hip for a varus-producing proximal femoral
osteotomy. These functional radiographs should demonstrate joint
congruency without hinging and ideally show an improvement or at least
maintenance of the joint space. If congruency or the optimal joint
reorientation position is questionable with functional radiographs, a
hip exam with fluoroscopy can provide additional information regarding
the joint suitability for osteotomy surgery. With more complicated
deformities, fluoroscopic examination can be
extremely informative regarding congruency of the articulation and for planning an optimal osteotomy correction.
thoroughly evaluate and define the disease pattern of the hip being
considered for surgery. Magnetic resonance arthrogram may be indicated
to assess acetabular labral disease, articular cartilage integrity,
acetabular rim pathology, and femoral head and femoral neck anatomy.
Alternatively, a CAT scan of the hip can be useful for more detailed
characterization of osseous abnormalities and can facilitate
preoperative planning. Sources of bony impingement, femoral head/neck
junction anatomy, version of the acetabulum, and osteonecrotic lesion
size and location are also better defined with CAT scan images.
Clearly, preoperative assessment of all disease components (both
acetabular and femoral) enables the surgeon to develop a comprehensive
treatment plan and optimize the results of the procedure.
It is extremely important to emphasize that several patient-related
variables are considered when selecting patients for surgery and when
devising a specific treatment plan. Osteotomy surgery has distinct
indications, contraindications, and goals when compared with total
joint replacement surgery.
authentic hip symptoms and have an associated structural abnormality
should be considered for osteotomy surgery. Typically, an optimal
surgical candidate is relatively young (physiologically less than 50
years old), well-conditioned, and active. The hip has a correctable
deformity, sufficient range of motion, adequate congruency, and has not
progressed to advanced secondary osteoarthritis. The patient should
have an understanding of the hip problem and the proposed surgical
procedure and should be willing to comply with the postoperative
rehabilitation protocol. Nonoperative measures, including physical
therapy, activity restriction, and nonsteroidal anti-inflammatory
medicines, can be used to minimize symptoms, although a long-term
benefit from these modalities is unlikely. Nonsurgical measures as a
primary treatment are reserved for patients who are marginal or poor
candidates for an osteotomy and for patients not interested in a major
hip surgery.
prearthritic or early arthritic hip symptoms prior to the development
of advanced joint deterioration. In general, prearthritic conditions
predispose the hip to dynamic instability, localized joint overload,
impingement, or a combination of these factors. If these disorders are
diagnosed early, the effects of corrective osteotomy surgery can be
extremely beneficial (Tables 10-2 and 10-3).
The goals of this type of surgery are to correct the underlying
structural abnormality of the hip, relieve the patient’s discomfort,
enhance hip function and activity, and delay or prevent the progression
of hip joint deterioration. Osteotomy correction can improve the
structure and biology of the joint in various ways. Surgical correction
can normalize the structural anatomy of the hip, enhance stability,
relieve or prevent
impingement,
optimize congruency, decrease localized articular surface overload, and
improve the biomechanics of the joint. It is important to emphasize
that joint instability and impingement can be simultaneous problems.
Reconstructive techniques must aim to improve joint function by
optimizing the dynamic balance between joint stability and impingement.
|
TABLE 10-2 Osteotomy Procedures for Specific HIP Disorders
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||
|
TABLE 10-3 Clinical Results of HIP Osteotomy Surgery (Selected Studies)
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
pathophysiologic mechanisms of joint deterioration. Thus, the
techniques of osteotomy reconstruction must be individualized to the
underlying structural abnormality of the hip and to the specific
disease characteristics of each case. The most common conditions
amenable to joint preservation surgery include classic developmental
dysplasia (DDH), Perthes-like deformities, SCFE, osteonecrosis, and
posttraumatic deformities.
preservation osteotomy surgery of the hip. This disease is
characterized by deficient anterolateral femoral head coverage,
superolateral inclination of the acetabular articular surface, a
lateral position of the hip center, and variable version abnormalities
of the acetabulum. On the femoral side, coxa valga, excessive
anteversion, and a nonspherical femoral head are common. This
combination of abnormalities can result in joint instability, localized
anterolateral joint overload, acetabular labral disease, and eventual
secondary arthrosis. In the presence of a congruent joint and in the
absence of advanced secondary osteoarthritis, symptomatic DDH is an
excellent indication for a reconstructive acetabular osteotomy.
been described, the Bernese periacetabular osteotomy (PAO) has gained
worldwide popularity over the past decade. This is our preferred
technique because the osteotomy is performed with an abductor-sparing
approach, uses orthogonal osteotomy cuts, and preserves the posterior
column. It enables major multiplanar corrections, preserves acetabular
fragment blood supply, provides reliable healing, and enables
accelerated rehabilitation. The procedure is most commonly performed
through a modified Smith-Peterson approach, and four periacetabular
cuts are made to enable acetabular mobilization. The first cut is an
infra-acetabular osteotomy that starts just below the inferior lip of
the acetabulum, aims toward the middle of the ischial spine, and
extends to the level of a trajectory bisecting the posterior column
(approximately 1 cm anterior to the posterior cortex of the posterior
column). The inferior osteotomy is followed by the superior pubic ramus
cut, which is made just medial to the iliopectineal eminence and angled
away from the joint. The third cut is made at the anterior superior
iliac spine directly towards the sciatic notch. The fourth and final
osteotomy cut is made with a goal of bisecting the posterior column
between the articular surface anteriorly and the posterior cortex. This
osteotomy meets the first infra-acetabular cut posteroinferior to the
acetabulum. The acetabular fragment is then mobilized and repositioned
with internal rotation, forward tilt, and medial translation. The
internal rotation component of the reduction provides lateral coverage
and maintains anteversion of the acetabulum. The acetabulum is fixed
provisionally with k-wires, the reduction is assessed with
intraoperative radiographs, and definitive fixation is then performed.
Final radiographs are obtained to confirm an osteotomy correction that
improves anterolateral femoral head coverage (lateral center-edge angle
20 to 30 degrees, anterior center-edge angle 15 to 25 degrees), reduces
the superolateral inclination of the acetabular articular surface (0 to
15 degrees), restores a more medial position of the hip joint center
(medial aspect of the femoral head 5 to 10 mm lateral to ilioischial
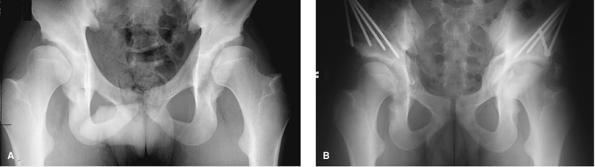
line), and maintains anteversion of the acetabulum (Fig. 10-1A, B).
anterior and posterior lips, and it is important that the acetabulum
not be overreduced or retroverted, as this can result in secondary
anterior femoroacetabular impingement. Slight undercorrection is
preferred over excessive
correction
to avoid creating an femoroacetabular impingement. Additionally, hip
flexion and abduction motion is checked clinically, and it is
imperative that at least 90 degrees of passive hip flexion and 30
degrees of abduction are achieved on the operating room table. After
range of motion evaluation, we perform an arthrotomy to inspect the
integrity of the acetabular labrum and to assess for anterior
femoroacetabular impingement. Large, unstable labral tears are repaired
with suture anchors, whereas stable tears are left untreated. Lack of
femoral head/neck offset can result in anterior femoroacetabular
impingement postoperatively and can be treated with osteoplasty if
found to be a source of impingement. In cases with an associated major
femoral deformity, a proximal femoral osteotomy may be necessary. In
severely dysplastic hips, a valgus proximal femoral deformity may have
to be treated with a varus-producing intertrochanteric osteotomy to
optimize the reconstruction. Long-term clinical results of the Bernese
periacetabular osteotomy, as reported by Siebenrock et al., have
demonstrated good to excellent results in 73% of patients followed for
an average of 11.3 years. These data are derived from the learning
curve experience with this osteotomy. It is likely that with
contemporary patient selection criteria and refined surgical
techniques, the good clinical results of this procedure will be longer
lasting and more predictable.
 |
|
Figure 10-1 Standard periacetabular osteotomy (PAO) for developmental dysplasia of the hip (DDH). Preoperative (A) and postoperative (B)
anteroposterior pelvic radiographs in a 19-year-old male collegiate athlete with hip pain and instability symptoms. He was treated with staged bilateral periacetabular osteotomies. Note the enhanced lateral coverage, decreased superolateral inclination of the acetabular articular surface, maintained anteversion, and medial translation of the hip center achieved with the osteotomy. The patient returned to full sport activities without restrictions and an excellent clinical outcome. |
is usually on the acetabular side of the joint, and currently, most
surgeons prefer to address the disease with acetabular reorientation.
Uncommonly, the acetabular deformity is very mild and the most profound
deformity is femoral-based. It consists of coxa valga with lateral
joint overload. In these occasional cases a varus-producing proximal
femoral osteotomy can be considered. Perhaps more commonly, a
varus-producing proximal femoral osteotomy is indicated to augment the
acetabular procedure in severe cases. The varus correction can be
combined with extension (apex anterior correction) to enhance hip
stability by containing the femoral head anterolaterally and can
decrease the load per unit surface area along the anterolateral
acetabularrim.
technique to obtain correction and minimize the distortion of the
proximal femur (Figs. 10-2, 10-3).
A varus-producing realignment is performed with a transverse osteotomy
at the superior aspect of the lesser trochanter and a 90-degree blade
plate for reduction and fixation of the osteotomy fragments. The angle
of the chisel and blade insertion dictates the amount of varus
correction obtained. For example, if the blade is inserted at a
110-degree angle to the femoral shaft in the frontal plane, a 20-degree
correction will be obtained when the 90-degree blade plate is inserted
and the osteotomy is reduced. The blade length is estimated with
templates and the blade plate offset (10, 15, or 20 mm) is determined
to maintain the horizontal offset between the center of the femoral
head and the longitudinal axis of the femoral shaft. Specifically,
offset is maintained by medial displacement of the femoral shaft for
varus osteotomies and lateral displacement for valgus osteotomies. A
varus osteotomy shortens the extremity, and the preoperative plan
determines the amount of shortening to be produced. For
valgus-producing osteotomies, an angled blade plate (110, 120, or 130
degrees) is used. The amount of valgus correction is determined by the
angle of insertion and the blade plate angle. For example, a 20-degree
correction is obtained by inserting a 110-degree blade plate at a
90-degree angle to the femoral shaft in the frontal plane. With
reduction of the osteotomy and fixation of the plate, a 20-degree
correction is obtained. Valgus osteotomies lengthen the extremity, and
resection of bone may be required to maintain equal leg lengths.
approach to the proximal femur is performed. The Watson-Jones interval
can be used for access to the anterior hip joint, acetabular labrum,
femoral head, and femoral neck if
necessary.
K-wires are placed to guide the osteotomy cut and the blade insertion.
To place the blade centrally in the femoral neck, it must be inserted
in the anterior half of the lateral greater trochanter owing to the
posterior overhang. The insertion site should provide a 1.5- to 2.0-cm
bony bridge of lateral femur cortex between the blade entry point and
the osteotomy site. This minimizes the risk of fracture in this
location. In general, varus and flexion/extension osteotomies are
performed with a 90-degree blade plate whereas valgus corrections are
obtained with blade plates ranging from 110 to 130 degrees, depending
on the magnitude of correction. The chisel is advanced with a K-wire
guiding the direction of insertion in the frontal plane and centrally
in the femoral neck. If flexion (apex posterior) or extension (apex
anterior) of the osteotomy is desired, this is incorporated by
adjusting the anterior/posterior angulation of the chisel with respect
to the femoral shaft. Rotation of the femur is then marked and the
transverse osteotomy is made with an oscillating saw at the upper level
of the lesser trochanter. The blade chisel is removed from the proximal
fragment and the blade plate inserted along the prepared track. The
blade plate is further secured to the proximal fragment with a 4.5-mm
cortical screw. The proximal and distal osteotomy fragments are then
mobilized, and the osteotomy is reduced by approximation of the lateral
femur to the plate. The rotation line is used to facilitate the
reduction, and care should be taken to align the two fragments without
a major step-off in the anteroposterior plane. Final reduction and
fixation of the osteotomy is assessed with radiographs or fluoroscopy
in the anteroposterior and lateral planes, and hip range of motion
(flexion and rotation) is checked by clinical examination.
 |
|
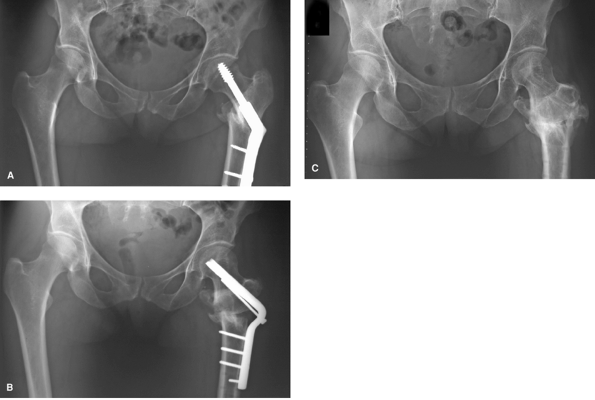
Figure 10-2
Periacetabular osteotomy/proximal femoral osteotomy (PAO/PFO) for Perthes/no wedge technique. Preoperative anteroposterior pelvic radiograph (A) of a 21-year-old male with a history of Perthe disease in childhood, leg-length discrepancy and a 2-year history of progressive lateral hip pain. A Perthe deformity of the proximal femur is noted, and secondary acetabular dysplasia is present. This patient was treated with a combined periacetabular osteotomy and a valgus proximal femoral osteotomy (B). The femoral osteotomy lengthened the extremity, enhanced the congruency of the joint, improved clinical abduction, and improved abductor function. This patient had an excellent clinical result 4 years later (C). |
 |
|
Figure 10-3 Proximal femoral osteotomy (PFO) for posttraumatic malunion. Standing anteroposterior pelvis (A)
of the left hip in a 39-year-old female referred for evaluation of persistent hip pain after treatment of an intertrochanteric femoral fracture. Prior to fracture, the patient was an active recreational runner. She presented complaining of lateral hip pain, leg-length discrepancy, and lack of internal rotation of the left hip. On examination she had a severe limp, profound abductor weakness, a 2-cm leg-length discrepancy, and malrotation with <10 degrees of internal rotation. This proximal femoral malunion was treated with a valgus-derotation femoral osteotomy (B). She had an excellent clinical result and was asymptomatic at 5-year follow-up (C). |
the development of the femoral head and acetabulum, resulting in
residual deformities that can be associated with hip symptoms in
adulthood and can lead to secondary osteoarthritis. Perthes
abnormalities are most remarkable on the femoral side (coxa magna, coxa
plana, coxa breva, and relative trochanteric overgrowth), but can also
encompass a secondary acetabular dysplasia. Generally, these
abnormalities are very complex and must be evaluated carefully to
optimize the surgical treatment plan. Labral disease, instability and
joint overload, joint incongruence, abductor fatigue, and
femoroacetabular impingement can all contribute variably to patient
symptoms and should be considered.
enhance joint stability, decrease localized joint surface overload, and
relieve intra-articular impingement. Additional treatment goals may
include equalization of leg lengths and repositioning of the greater
trochanter. The specific characteristics of the deformity dictate the
type of osteotomy correction. Hips with a femoral deformity and an
associated secondary acetabular dysplasia (the most common scenario for
patients who present with a prearthritic or early arthritic
Perthes-like deformity) are most reliably treated with a combined
acetabular reorientation and proximal femoral valgus osteotomy (Fig. 10-2A–C).
With this comprehensive approach, the acetabular and femoral
deformities can be addressed to optimize the hip reconstruction. This
treatment strategy has been reported by Beck and Mast with good to
excellent clinical results in 85% of cases at an average 3.4-year
follow-up. At surgery, we now perform an arthrotomy to inspect the
integrity of the acetabular labrum and to assess anterior
femoroacetabular impingement from the large, nonspherical femoral head.
Osteoplasty of the prominent anterior femoral head in the setting of
coxa magna can minimize femoroacetabular impingement after acetabular
reorientation.
valgus osteotomy can be effective in improving congruency, relieving
intra-articular impingement, lengthening the extremity, improving
abductor function, and enhancing clinical hip abduction. Osteoplasty of
the femoral head/neck junction may also be indicated in conjunction
with the femoral osteotomy to completely address impingement disease.
For Perthes hips with a less severe femoral deformity and a primary
impingement problem, a femoral head/neck junction osteoplasty alone may
be considered.
and premature osteoarthritis in adulthood, is a residual deformity from
a SCFE. The SCFE deformity most commonly involves posteromedial
displacement of the epiphysis, resulting in an extension and
retroversion deformity of the proximal femur. An apparent varus
deformity is also present. These patients most commonly complain of
restricted hip flexion and symptoms from anterior femoroacetabular
impingement combined with an external rotation deformity of the
involved lower extremity. Direct correction of this deformity can be
performed at the level of the femoral neck, although the risk of
osteonecrosis makes this technique less attractive. Alternatively, a
transverse intertrochanteric osteotomy can adequately address the
deformity with less risk of osteonecrosis. A flexion and derotation
osteotomy can correct the deformity and markedly improve clinical
symptoms. The flexion correction should aim to place the femoral shaft
perpendicular to the epiphysis in the sagittal plane. Slight valgus can
be incorporated into the osteotomy but is frequently obtained with the
flexion correction alone. An anterior capsulotomy should also be
performed to ensure unrestricted postoperative hip extension and to
inspect for residual femoroacetabular impingement. If present, the
prominent anterolateral femoral head/neck junction should be resected.
Severe SCFE deformities can require major deformity corrections (>50
degrees). In these cases it is particularly important to align the
proximal and distal fragments by combining anterior translation and
flexion of the distal fragment. This preserved alignment facilitates
future total hip arthroplasty surgery.
treatment of SCFE deformities support continued use of these
procedures. One recent follow-up study of the Imhauser osteotomy
demonstrated good to excellent results in 77% of patients followed for
an average of 23.4 years. This osteotomy provides a multiplanar
correction
consisting
of flexion, internal rotation, and valgus that is dictated by resection
of a three-dimensional intertrochanteric bone wedge. A similar
multiplanar realignment can also be achieved with the no-wedge
osteotomy technique discussed previously.
head is a controversial topic, and there are many acceptable treatment
options depending on patient characteristics, stage, size, and location
of the lesion. The literature does support the intertrochanteric
osteotomy as an effective strategy for the treatment of very specific
disease patterns. It is imperative that these patients are carefully
selected, and various factors must be considered when contemplating an
intertrochanteric osteotomy for the diagnosis of osteonecrosis.
Patients with a subchondral fracture and/or femoral head collapse
without significant joint space narrowing can be evaluated as potential
candidates for osteotomy surgery. The ideal candidate is a compliant,
healthy patient not on corticosteroids who has a lesion with a combined
osteonecrotic angle on the anteroposterior and lateral radiographs of
<200 degrees. Such patients represent a relatively small subgroup of
the patient population with osteonecrosis. In general, anterolateral
lesions that can be delivered away from the weight-bearing surface of
the femoral head are treated with a flexion-valgus osteotomy. This
repositions the healthier posteromedial femoral head articular
cartilage and subchondral bone into the weight-bearing zone.
Anteromedial lesions that cannot be delivered away from the
weight-bearing zone with a valgus osteotomy are managed with a varus
flexion osteotomy to use the healthy posterolateral femoral head as the
primary weight-bearing surface. In well-selected candidates treated
with sound surgical technique, proximal femoral osteotomy can be very
effective. Mont et al. reviewed 37 varus osteotomies (26 with a
combined flexion or extension component) in the treatment of Ficat
stage II and III disease. At 11.5 year follow-up, they noted 76% good
or excellent clinical results.
can be excellent indications for osteotomy surgery. For example,
nonunions of the femoral neck are associated with profound clinical
symptoms and can be effectively managed with a valgus-producing
proximal femoral osteotomy in appropriate patients. With the Pawuel
technique, a laterally based closing wedge osteotomy at the
intertrochanteric level achieves valgus correction. This converts the
tension and shear forces across the nonunion (secondary to varus
displacement) to a compressive force that facilitates healing. Marti et
al. reviewed 50 cases of femoral neck nonunion treated with the Pawuel
valgus-producing osteotomy at an average 7.1-year follow-up. They
observed 86% of the nonunions to be healed, whereas 14% had been
converted to total hip replacements.
of hip dysfunction, especially in active young patients. Such
deformities must be carefully characterized, and the corrective
osteotomy is planned to address the specific malunion pattern of each
case. In the intertrochanteric region, a transverse osteotomy at the
superior aspect of the lesser trochanter and the no-wedge technique can
be used to correct multiplanar deformities and obtain predictable
healing (Fig. 10-3).
proximal femoral osteotomy are mobilized on the first or second
postoperative day. For the first 6 weeks, patients bear 30 pounds
partial weight and perform isometric exercises only. At 6 weeks, active
strengthening exercises are initiated with an emphasis on abductor
strengthening, and weight-bearing status is advanced to 5% for an
additional 4 weeks. Ten to 12 weeks postoperatively patients advance to
full weight bearing depending on the details of the case and
radiographic signs of healing. Aggressive hip strengthening is then
permitted at this phase of rehabilitation. Unrestricted activity is
allowed when radiographic healing of the osteotomy is evident. In
general, we recommend hardware removal 1 to 2 years after the osteotomy
to facilitate future conversion to total hip arthroplasty if required.
Removal of proximal femoral blade plates also reduces the risk of
trochanteric bursitis symptoms associated with the retained hardware.
infection, nonunion, fixation failure, neurovascular injury,
thromboembolic disease, and perioperative medical problems. A learning
curve is known to contribute to the incidence of complications for most
surgeons. Unique to acetabular osteotomy surgery are the potential
complications of intra-articular fracture and overcorrection.
Intra-articular fracture has a poor prognosis and usually leads to
rapid joint deterioration. Overcorrection can cause secondary
impingement disease and must be kept in mind when planning and
performing acetabular reorientation. Persistent hip symptoms and
progression of secondary osteoarthritis are additional problems that
can occur; they underscore the limitations of joint preservation
surgery in the setting of major degenerative changes and emphasize the
importance of careful patient selection.
R, Klaue K, Vinh TS, et al. A new periacetabular osteotomy for the
treatment of hip dysplasias. Technique and preliminary results. Clin Orthop. 1988;232:26–36.
K, Cordier W, Katthagen BD. Long-term follow-up study after corrective
Imhauser osteotomy for severe slipped capital femoral epiphysis. J Pediatr Orthop. 2000;20:749–756.
RT, Ekkernkamp A, Ganz R, et al. Periacetabular and intertrochanteric
osteotomy for the treatment of osteoarthrosis in dysplastic hips. J Bone Joint Surg Am. 1995;77(1):73–85.
