CHAPTER 69 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
CHAPTER 69 – Posterolateral Corner Reconstruction
Russell F. Warren, MD
Injury to the posterolateral corner of the knee is a rare but often debilitating entity. Posterolateral corner injury is usually associated with additional ligament injury and can be missed on initial physical examination. [2] [3] [6] [7] If it is identified early (within 3 weeks), many authors recommend acute repair of the posterolateral corner. However, recent data suggest that the results of reconstruction may be equivalent to those of acute repair.[11] Reconstruction of the posterolateral corner is indicated for those who present after 3 weeks of injury or who have inadequate soft tissue for successful repair. Biomechanical data have shown that reconstruction of the posterolateral corner must restore function of the lateral collateral ligament and popliteofibular ligament to resist posterior translation, varus opening, and external rotation of the tibia on the femur. [4] [5] [12]
It is essential to obtain a complete history of the injury at the time of the initial evaluation. Injuries to the posterolateral corner of the knee are rarely isolated and are usually associated with significant trauma to the knee. A detailed account of previous treatments, as well as operative reports, if they are available, should be obtained before consideration of additional surgical intervention.
| • | Acute, traumatic knee injury | |
| • | Activity-related instability | |
| • | Previous ligament reconstruction (anterior or posterior cruciate ligament) may have failed |
Examination of the cruciate and collateral ligaments as well as of the neurovascular status of the patient should be well documented. A significant percentage of posterolateral corner injuries occur in the setting of knee dislocation. Examination of the acute injury may be limited by pain.
| • | Tenderness over posterolateral aspect of the knee with ecchymosis ( Fig. 69-1 ) |
|
| • | Positive varus instability at 30 degrees (and 0 degrees with combined injury) | |
| • | Associated ligamentous instability may be present (anterior cruciate ligament, posterior cruciate ligament) | |
| • | Positive result of posterolateral drawer test | |
| • | Positive result of external rotation (dial) test: increased only at 30 degrees, isolated posterolateral corner injury; increased at 30 degrees and 90 degrees, posterior cruciate ligament and posterolateral corner injuries | |
| • | Positive result of external rotation recurvatum test (with combined injury) ( Fig. 69-2 ) |
|
| • | Positive result of reverse pivot shift test | |
| • | Examination findings may be consistent with peroneal nerve injury |
| • | Similar to acute, although a varus thrust during gait may develop | |
| • | Lateral joint line pain |
Magnetic resonance imaging is performed to assess meniscus and ligamentous structures. Magnetic resonance arteriography may be considered, in conjunction with magnetic resonance imaging, for evaluation of acute or subacute posterolateral corner injuries in the setting of suspected knee dislocation.
Electromyelography is performed at 3 weeks if peroneal nerve injury is present.
Indications and Contraindications
Reconstruction of the posterolateral corner of the knee is generally indicated for complete disruptions (grade III) or grade II injuries with symptomatic instability. Associated ligamentous injuries may need to be addressed at the time of posterolateral corner reconstruction. A relative contraindication for posterolateral corner reconstruction is varus knee alignment. High tibial osteotomy, before or in conjunction with the posterolateral corner reconstruction, should be considered in chronic cases.
Significant limb malalignment, chondral injury, or associated ligament injuries may need to be addressed before or in conjunction with the posterolateral corner reconstruction in chronic cases.
Graft selection should be discussed with the patient at the preoperative visit. Graft options include hamstring autograft, Achilles tendon allograft, and anterior tibial tendon allograft tissue.
Reconstruction of the posterolateral corner of the knee can be performed under general, combined spinal and epidural, or regional anesthesia on the basis of the patient’s, anesthesiologist’s, and surgeon’s preferences. The patient is placed supine on a standard operating room table, and a tourniquet is applied to the upper thigh. The knee is flexed 20 to 30 degrees over a bump.
| • | Fibular head | |
| • | Gerdy tubercle | |
| • | Lateral epicondyle of the femur |
Examination Under Anesthesia and Diagnostic Arthroscopy
Examination under anesthesia is performed to test the ligamentous structures of the knee. Diagnostic arthroscopy may be performed to further evaluate the lateral compartment and intraarticular structures. If combined ligamentous reconstruction, cartilage restoration procedures, and tibial osteotomy are to be considered, they may be done under arthroscopic assistance before the posterolateral corner is addressed.
Specific Steps (
Box 69-1
)
An incision is made in the skin from a point just proximal and posterior to the lateral epicondyle and extended in line with the iliotibial band to a point just distal to Gerdy tubercle, midway between Gerdy tubercle and the fibular head. The incision is carried sharply down to the level of the iliotibial band with a scalpel or electrocautery. Anterior and posterior soft tissue flaps are raised to expose the lateral epicondyle, the Gerdy tubercle, and the fibular head.
| Surgical Steps | ||||||||||||||||||||||||
|
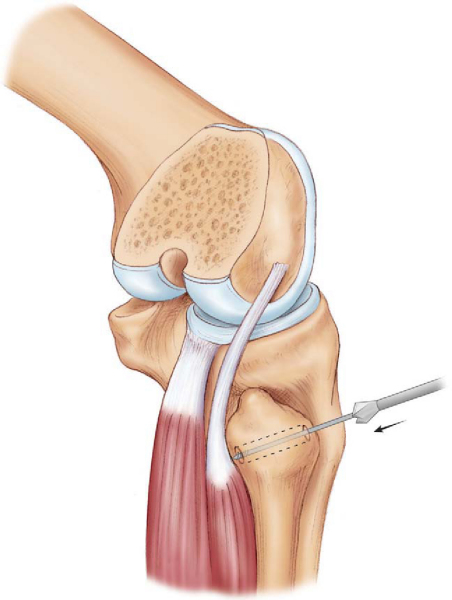
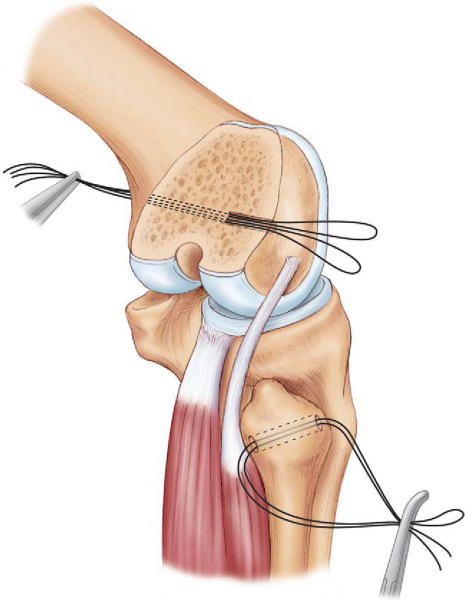
The posterior border of the long head of the biceps femoris is identified and incised sharply. The peroneal nerve is identified at the posterior border of the muscle belly and dissected from proximal to distal as it passes across the fibular head. The fascia overlying the peroneal muscles should be released to allow adequate decompression of the nerve. A vessel loop is placed around the nerve for identification and protection throughout the remainder of the case. After identification and protection of the peroneal nerve, anterior and posterior subperiosteal dissection of the fibular head is performed. A guide wire is placed from anterior to posterior, inclined distally, approximately 2 cm from the tip of the fibula, and overreamed with a 7- to 8-mm acorn reamer (
Fig. 69-3
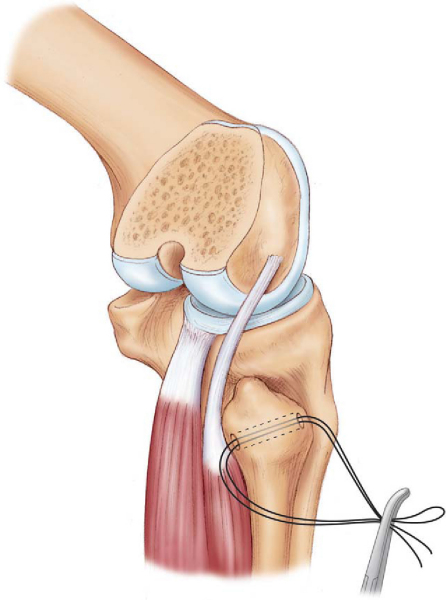
). A No. 5 Ethibond (Ethicon, Inc., Somerville, NJ) suture is placed through the fibular hole and tagged for later graft passage (
Fig. 69-4
).
|
|
|
|
Figure 69-3 (Redrawn with modification from Verma NN, Mithofer K, Battaglia M, MacGillivray J. The docking technique for posterolateral corner reconstruction. Arthroscopy 2005;21:238-242.) |
|
|
|
|
Figure 69-4 (Redrawn with modification from Verma NN, Mithofer K, Battaglia M, MacGillivray J. The docking technique for posterolateral corner reconstruction. Arthroscopy 2005;21:238-242.) |
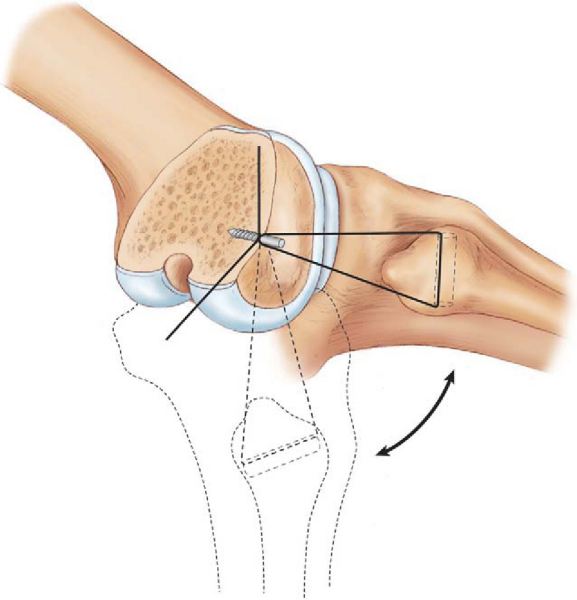
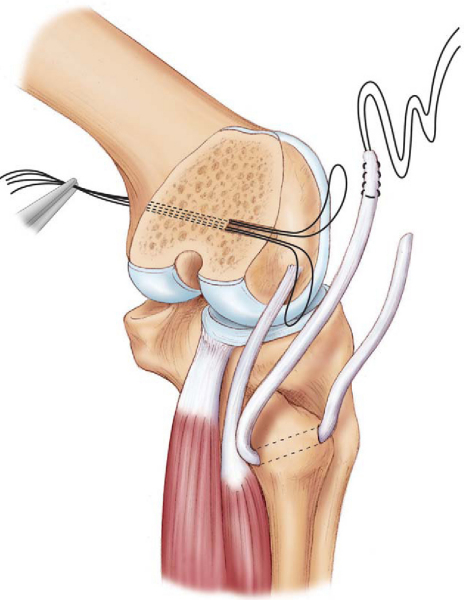
Attention is turned to the lateral epicondyle of the femur, which is easily palpated. A 3- to 4-cm incision is made in the iliotibial band at the level of the lateral epicondyle and extended distally. Blunt dissection is performed deep to the iliotibial band, and the lateral collateral ligament remnant and popliteus insertion are visualized. The isometric point on the femur is generally located midway between the lateral collateral ligament origin and the popliteus insertion. The most isometric point on the femur is determined by placing a suture from the fibular head to a pin on the lateral epicondyle at the center of rotation and cycling the knee from flexion to extension (
Fig. 69-5
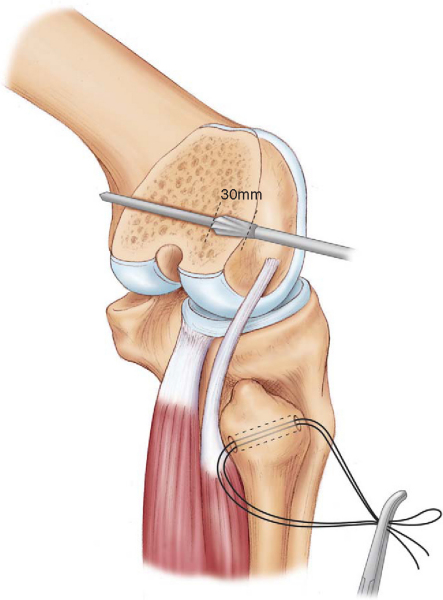
). The isometric point on the femur should not allow more than 2 mm of excursion of the suture when the knee is taken through a full range of motion. Subperiosteal dissection is performed at the isometric point, and a slotted guide pin is drilled across the femur (
Fig. 69-6
). Placement of the guide pin is made parallel to the joint line and may be confirmed with fluoroscopy. The guide pin is overdrilled with an 8-mm reamer to a depth of 30 mm. Two No. 2 FiberWire (Arthrex, Naples, Fla) sutures are placed in the slot of the guide pin, and the free ends are brought out the medial side of the knee (
Fig. 69-7
).
|
|
|
|
Figure 69-5 (Redrawn with modification from Verma NN, Mithofer K, Battaglia M, MacGillivray J. The docking technique for posterolateral corner reconstruction. Arthroscopy 2005;21:238-242.) |
|
|
|
|
Figure 69-6 (Redrawn with modification from Verma NN, Mithofer K, Battaglia M, MacGillivray J. The docking technique for posterolateral corner reconstruction. Arthroscopy 2005;21:238-242.) |
|
|
|
|
Figure 69-7 (Redrawn with modification from Verma NN, Mithofer K, Battaglia M, MacGillivray J. The docking technique for posterolateral corner reconstruction. Arthroscopy 2005;21:238-242.) |
The selected graft is subsequently prepared. A No. 2 FiberWire suture is placed in one end of the graft in a Krakow-type fashion; the other end is left free for future measurement and division.
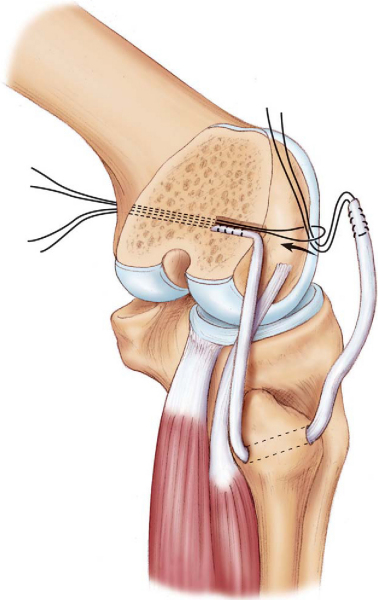
The graft is brought through the fibular tunnel by the previously placed No. 5 Ethibond passing suture (
Fig. 69-8
). Dissection under the iliotibial band is performed with a large clamp, and both ends of the graft are passed beneath it. The end of the graft with the Krakow suture is docked into the femoral tunnel by use of one of the passing sutures and manual traction applied from the medial aspect of the knee (
Fig. 69-9
). The knee is subsequently reduced and taken through a full range of motion with the tibia held in internal rotation and a valgus stress applied. The free end of the graft is tensioned and brought to the aperture of the femoral tunnel for measurement. A No. 2 FiberWire suture is placed in a Krakow-type fashion from the point marked at the femoral tunnel and extended 20 mm distally. The free end of the graft is then divided immediately distal to the Krakow-type stitch. The suture ends in the graft are then shuttled into the tunnel and brought out the medial side of the knee with the remaining passing suture.
|
|
|
|
Figure 69-8 (Redrawn with modification from Verma NN, Mithofer K, Battaglia M, MacGillivray J. The docking technique for posterolateral corner reconstruction. Arthroscopy 2005;21:238-242.) |
|
|
|
|
Figure 69-9 (Redrawn with modification from Verma NN, Mithofer K, Battaglia M, MacGillivray J. The docking technique for posterolateral corner reconstruction. Arthroscopy 2005;21:238-242.) |
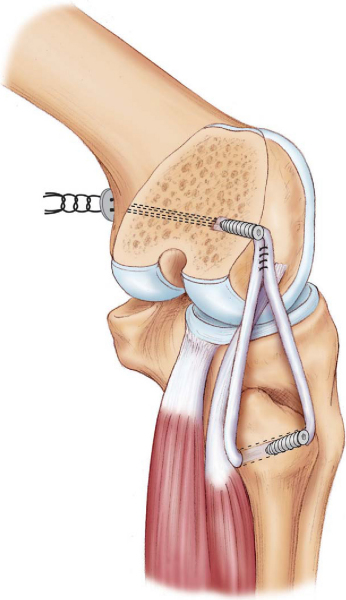
A soft tissue interference screw is placed from anterior to posterior in the fibular tunnel to secure the graft distally. The ends of the graft are firmly docked into the femoral tunnel, and the knee is again taken through a gentle range of motion to eliminate creep within the graft and to confirm isometry. The knee is brought to 20 degrees of flexion, and the tibia is maintained in internal rotation with a valgus stress. The graft ends are secured within the femoral tunnel with an interference screw. In the setting of osteoporotic bone or poor primary fixation, supplemental fixation with a soft tissue button may be performed on the medial cortex of the femur through a separate small incision (
Fig. 69-10
).
|
|
|
|
Figure 69-10 (Redrawn with modification from Verma NN, Mithofer K, Battaglia M, MacGillivray J. The docking technique for posterolateral corner reconstruction. Arthroscopy 2005;21:238-242.) |
The anterior and lateral compartments of the leg are released distally with a long-handled Metzenbaum scissors before wound closure.
The incisions are closed in layers, and a drain is placed within the wound. Care should be taken to ensure that the peroneal nerve is not under tension during the closure.
Tibial Osteotomy and Posterolateral Corner Reconstruction
Combined Cruciate Ligament and Posterolateral Corner Reconstruction
Posterior and anterior cruciate ligaments should be secured within the tibial and femoral tunnels, respectively, before completion of posterolateral corner reconstruction. The knee is held in a reduced position during subsequent fixation of the posterolateral corner. The final posterior or anterior cruciate ligament fixation should be performed after completion of the posterolateral corner reconstruction.
| • | At 7 to 10 days for suture removal and postoperative radiographs |
| • | Peroneal nerve injury | |
| • | Infection | |
| • | Arthrofibrosis | |
| • | Recurrent instability |
After posterolateral corner reconstruction, good to excellent results can be expected in 85% to 90% of cases (
Table 69-1
). Patients will generally have resolution of instability but may continue to have some degree of pain, depending on the cartilage injury at the time of the initial trauma. Recent data suggest that results of anatomic reconstructions may be better than those of procedures that do not attempt to restore the normal anatomy.[13]
| Author | Followup | Outcome |
|---|---|---|
| Noyes et al[9] (1996) | 42 months | 16/21 (76%) good–excellent |
| Albright and Brown[1] (1998) | 4 years | 26/30 (87%) clinical improvement |
| Latimer et al[8] (1998) | 28 months | 10/10 (100%) resolution of subjective instability |
| Stannard et al[11] (2005) | 2 years | 20/22 (91%) successful |
| Yoon et al[13] (2006) | Minimum 1 year | Anatomic reconstruction: 20/21 (95%) good–excellent |
| Posterolateral corner sling: 21/25 (84%) good–excellent |
1.
Albright JP, Brown AW: Management of chronic posterolateral rotatory instability of the knee: surgical technique for the posterolateral corner sling procedure.
Instr Course Lect 1998; 47:369-378.
2.
Baker Jr CL, Norwood LA, Hughston JC: Acute posterolateral rotatory instability of the knee.
J Bone Joint Surg Am 1983; 65:614-618.
3.
DeLee JC, Riley MB, Rockwood Jr CA: Acute posterolateral rotatory instability of the knee.
Am J Sports Med 1983; 11:199-207.
4.
Gollehon DL, Torzilli PA, Warren RF: The role of the posterolateral and cruciate ligaments in the stability of the human knee: a biomechanical study.
J Bone Joint Surg Am 1987; 69:233-242.
5.
Grood ES, Stowers SF, Noyes FR: Limits of movement in the human knee: effect of sectioning the posterior cruciate ligament and posterolateral structures.
J Bone Joint Surg Am 1988; 70:88-97.
6.
Hughston JC, Andrews JR, Cross MJ, Moschi A: Classification of knee ligament instabilities. Part II. The lateral compartment.
J Bone Joint Surg Am 1976; 58:173-179.
7.
Hughston JC, Jacobson KE: Chronic posterolateral rotatory instability of the knee.
J Bone Joint Surg Am 1985; 67:351-359.
8.
Latimer HA, Tibone JE, ElAttrache NS, McMahon PJ: Reconstruction of the lateral collateral ligament of the knee with patellar tendon allograft: report of a new technique in combined ligament injuries.
Am J Sports Med 1998; 26:656-662.
9.
Noyes FR, Barber-Westin SD: Surgical restoration to treat chronic deficiency of the posterolateral complex and cruciate ligaments of the knee joint.
Am J Sports Med 1996; 24:415-426.
10.
Noyes FR, Stowers SF, Grood ES, et al: Posterior subluxations of the medial and lateral tibiofemoral compartments: an in vitro ligament sectioning study in cadaveric knees.
Am J Sports Med 1993; 21:407-414.
11.
Stannard JP, Brown SL, Farris RC, et al: The posterolateral corner of the knee: repair versus reconstruction.
Am J Sports Med 2005; 33:881-888.
12.
Veltri DM, Warren RF: Anatomy, biomechanics, and physical findings in posterolateral knee instability.
Clin Sports Med 1994; 13:599-614.
13.
Yoon KH, Bae DK, Ha JH, Park SW: Anatomic reconstructive surgery for posterolateral instability of the knee.
Arthroscopy 2006; 22:159-165.