ENDOCRINOLOGY
processes with a common pathologic mechanism. In each situation, a
relative decrease in serum calcium, phosphorus, or a combination of
each, causes abnormalities of normal physeal development and
mineralization in the immature patient. While these abnormalities
affect both the axial and appendicular skeleton, it is the effect on
the extremities that becomes most clinically apparent, and is of most
interest and concern to the pediatric orthopaedic surgeon. Similar
perturbations of serum chemistries may be found in adults, as seen in
association with renal disease, and with some malignancies, but the
classic clinical appearance of rickets is found only in the skeletally
immature.
clinical symptoms and signs. As such, there is no singular disease that
can be termed rickets. Classic (dietary) rickets
is secondary to dietary abnormalities and deficiency of vitamin D,
which in turn lead to abnormalities in calcium uptake and metabolism.
This is relatively infrequent in the Western world, but troubling
reports have appeared recently of an increased incidence of dietary
(vitamin D deficiency) rickets in children who are exclusively
breast-fed.
or activated vitamin D. As such, infants who are exclusively breast-fed
require vitamin D supplementation prior to the introduction of more
advanced foods. This is particularly problematic in those infants with
darker skin color, in whom melatonin competes with vitamin D for the
ultraviolet (UV) radiation in the skin cells, thus increasing the
amount of sun exposure required to activate an appropriate level of
vitamin D. Premature infants, and those of families with particular
religious considerations that require significant coverage of the head
and face, particularly in females, may be at greater risk for rickets
secondary to a lack of activated vitamin D.
especially in fall and winter months in which the opportunity for
natural UV exposure is limited both by the cold and by clothing cover.
Other groups that may develop similar findings include children with
severe milk allergies who do not receive appropriate supplementation,
and children made to follow a strict vegetarian diet, which may be low
in vitamin D content. Overall, rickets secondary to deficiency of
vitamin D is uncommon in modern Western society, but does occur,
particularly in some cultures, and the pediatric orthopaedic surgeon
must remain vigilant.
calcium, phosphate, or vitamin D metabolism. Many of these have an
underlying genetic basis. The most common genetic abnormality is hypophosphatemic rickets
which is usually transmitted in an X-linked dominant pattern, but may
occur secondary to a spontaneous mutation. Females appear to be more
commonly affected than males. Patients with this disorder possess a
defect within the proximal and distal convoluted renal tubules, which
inhibits appropriate resorption of phosphate, thereby leading to
profound hypophosphatemia due to severe phosphate wasting in the urine.
Such abnormal levels of serum phosphate inhibit normal mineralization
and cause development of changes similar to those seen in classic
rickets, despite normal calcium intake and uptake, and normal intake
and ability to activate vitamin D. This type of rickets is often termed
vitamin D resistant, as the levels and
activity of vitamin D are generally normal, and further vitamin D
supplementation without addressing the phosphate issue does not improve
the clinical situation. Medical management of such patients requires
significant oral supplementation with neutral phosphate to maintain
appropriate serum levels in the face of persistent renal loss.
The most problematic of those remaining would be renal osteodystrophy
in patients with chronic renal insufficiency. These patients will have
the well established underlying problem of chronic renal disease, and
the skeletal manifestations should be expected to varying degrees. The
causes described previously make up most cases seen by pediatric
orthopaedic surgeons, and certainly the most common causes of clinical
findings for which the pediatric orthopaedic surgeon would be the
primary diagnostician. More detailed descriptions of these less common
entities are beyond the scope of this review, and one should consult
standard pediatric and endocrinology texts for further information.
-
Generally, patients are of short stature, but often heavier than children of similar chronologic age.
-
Classically, their demeanor has been described as lethargic or irritable.
-
Examination of the appendicular and axial
portions of the skeleton, as well as the bones of the skull, provides
reliable findings.-
□ Frontal bossing, flattening of the
skull due to changes of the growth regions about the cranial suture
lines, and varying levels of dental disease. -
□ Enlargement of the growth centers of
the ribs (costal cartilages) has been described as “rachitic rosary”
because it feels like a string of beads, and pectus carinatum can be
seen occasionally.
-
-
The patient may develop an increased
thoracic kyphosis, termed “rachitic catback,” but significant scoliosis
associated with, or attributable to, rickets is uncommon.
common in patients with rickets, and are often the primary reason for
pediatric orthopaedic evaluation.
-
There is generalized shortening of all
long bones, and the joints will appear bulbous and widened, especially
in the face of severe, untreated disease. -
The humeri usually develop varus deformities, while the lower extremities may demonstrate either varus or valgus angulation.
-
Commonly, the younger the patient, the
more likely the lower extremities will present in varus, rather than
valgus, and overall varus deformities of the lower extremities are much
more common than valgus. -
In contrast, skeletal manifestations of
chronic renal disease generally become apparent later in development,
and the lower extremity deformities in these patients tend toward
valgus. -
In addition to the structural
abnormalities, children with rickets may present with significant
ligamentous laxity, which will exacerbate the angular deformities,
particularly in the lower extremities during weightbearing.
or known rickets relies exclusively on the use of standard radiographs.
No special studies using computed tomography, magnetic resonance
imaging, or bone scan are necessary.
-
The histologic abnormalities resulting
from the alterations in physeal development and maturation lead to
standard radiographic changes directly adjacent to the growth plates. -
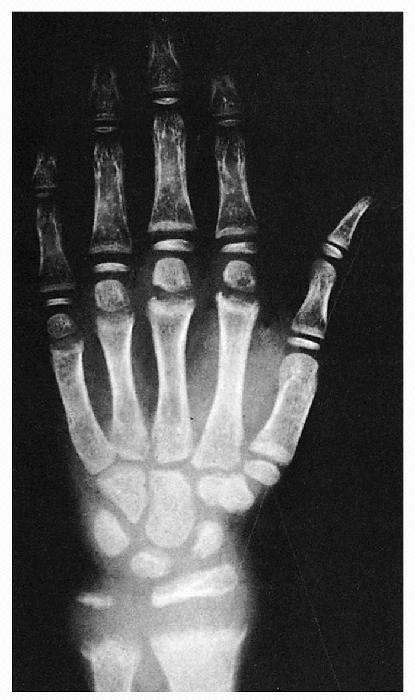
Plain radiographs demonstrate widening,
irregularity, and cupping of the growth plates of all bones that
undergo endochondral ossification (Fig. 25.1-1). -
The zone of provisional calcification is much less distinct than that of an unaffected individual.
-
As a result of these abnormalities, the
metaphyses of the appendicular skeleton appear widened or flared, and
angular deformities will occur over time and may be influenced by
weightbearing. -
Similar changes may be seen in the long
bones of those patients with a number of the metaphyseal dysplasias,
most commonly those of the Schmid or McKusick type.-
□ Assessment of serum chemistries may be
necessary to differentiate patients with certain skeletal dysplasias
from those with changes secondary to rickets.
-
-
Radiographic abnormalities are also evident within the diaphyseal regions of the more tubular bones.
-
Deposits of nonossified osteoid present as transverse radiolucent lines that may resemble fractures.
-
□ These areas are often referred to as
Looser lines, or Milkman pseudofractures, and may be seen in up to 25%
of patients with rickets (Fig. 25.1-2). -
□ These lesions classically occur along
the compressive sides of long bones, including the proximal femur, as
well as the ribs, clavicle, and pelvis. -
□ The etiology of Looser lines is
unclear, but they may be the result of incomplete fractures through
areas weakened by the generalized abnormality of bone maturation and
development.
-
 |
|
Figure 25.1-1
The changes in the epiphyseal plates of the wrist and hand are clearly seen in this radiography of an 8-year-old child with florid rickets. The distal radial and ulnar epiphyseal lines are markedly increased in axial height and show cupping; the zone of provisional calcification is absent. The changes in the slower-growing physes of the more distally placed bones are less marked, emphasizing the fact that rickets is a disease of the growing skeleton (in contrast to osteomalacia), and, if the physeal regions grow slowly, the findings are less prominent. (From Zaleske DJ. Metabolic and endocrine abnormalities. In: Morrissey RT, Weinstein SL, eds. Lovell and Winter’s pediatric orthopaedics, 4th ed. Vol 1. Philadelphia: Lippincott Williams & Wilkins, 2001:189.) |
 |
|
Figure 25.1-2
Looser lines seen in the rib cage of a child with florid rickets. These linear transverse radiolucent lines, which resemble incomplete fractures, are localized accumulations of osteoid of unknown cause. They are pathognomic for rickets and osteomalacia. (From Zaleske DJ. Metabolic and endocrine abnormalities. In: Morrissey RT, Weinstein SL, eds. Lovell and Winter’s pediatric orthopaedics, 4th ed. Vol 1. Philadelphia: Lippincott Williams & Wilkins, 2001:190.) |
|
TABLE 25.1-1 SERUM LEVELS IN RICKETS
|
||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
the diagnosis of rickets, and is the basis of the differential
diagnosis process, particularly since the radiographic findings are
fairly consistent within multiple etiologies. Information regarding the
differences in laboratory values between the various causes of rickets
of interest to the pediatric orthopaedic surgeon is presented in Table 25.1-1.
exact cause of the bone changes, thereby allowing initiation of
appropriate medical care. It cannot be stressed too highly that medical therapy directed toward correction of the underlying biochemical abnormality must be the initial step.
Any surgical intervention in the face of untreated or active rickets is
doomed to fail and presents significant risk to the patient. Because of
this, coordination between health care professionals providing
medical/endocrinologic care and those providing orthopaedic management
is essential.
improvement is documented through biochemical data and radiographic
evidence of stabilization or improvement of the growth plates, it is
then appropriate to contemplate surgical management. Bracing of the
lower extremities may be instituted during the period of attempted
medical treatment; however, there is controversy in the literature
regarding
benefit. Some very young patients with dietary (or vitamin D sensitive)
rickets demonstrate spontaneous improvement of their limb deformities
after the metabolic issues are stabilized and do not require any
surgical or orthotic intervention.
-
Surgical management of angular
deformities associated with rickets involves realignment osteotomies,
and such procedures are required most frequently for distal femoral and
proximal tibial deformities.-
□ Traditionally, corrections have been
performed acutely within the metaphyseal regions of the involved bones,
and have been stabilized with transfixing pins, compression plating, or
casts. -
□ Modern methods of angular correction
using external fixation (monolateral or circular frames) have greatly
enhanced the process through more precise correction and improved
stability of fixation, thereby eliminating the need for additional cast
immobilization. -
□ Compartment syndromes, delayed unions
and malunions, and superficial and deep infections are reported risks
of realignment procedures, particularly of the tibia.
-
-
Either acute or gradual correction may be
obtained using external fixation techniques, and both allow greater
patient mobility and activity in the postoperative period than those
methods requiring supplemental cast treatment. -
Immobility is a particular problem in
this patient population as it may cause significant shifts in serum
calcium levels, exposing the patient to the inherent risks posed by
such changes. -
Regardless of the type of procedure or
fixation system, there is a significant risk of recurrence for any
skeletally immature patient in whom medical or dietary management of
the underlying process is not maintained. -
This is more of a problem for those
patients with rickets secondary to genetic abnormalities of mineral
absorption or excretion, or vitamin D metabolism. -
Because of heightened awareness and
greater vigilance regarding appropriate intake and the need for
adequate UV light exposure, dietary rickets rarely recurs.
JS, Price CT. Unilateral external fixation for corrective osteotomies
in patients with hypophosphatemic rickets. J Pediatr Orthop
1995;15:232-235.
DY, Choi IH, Lee, CK, et al. Acquired vitamin D-resistant rickets
caused by aggressive osteoblastoma in the pelvis: a case report with
ten years’ follow-up and review of the literature. J Pediatr Orthop
1994;14:793-798.
JL, Weiner DS. Complications in proximal tibial osteotomies in children
with presentation of technique. J Pediatr Orthop 1995;15:307-312.
MT, Tylkowski C, Kriss VM, et al. The effect of osteotomy on bowing and
height in children with X-linked hypophosphatemia. J Pediatr Orthop
1999;19:114-118.
M, Glorieux FH, Cruess RL, et al. Principles and results of lower limb
osteotomies for patients with vitamin D-resistant hypophosphatemic
rickets. Clin Orthop 1988;237:264-270.
BC, Valanis B, Hertzber V. Sunshine exposure and serum
25-hydroxyvitamin D concentrations in exclusively breast-fed infants. J
Pediatr 1985;107:372-376.
DJ. Metabolic and endocrine abnormalities. In: Morrissey RT, Weinstein
SL, eds. Lovell and Winter’s pediatric orthopaedics, 4th ed. Vol 1.
Philadelphia: Lippincott Williams & Wilkins, 2001:177-241.
name given to describe the constellation of pathologic bony entities
that can occur in the patient with underlying renal disease.
-
Damage to the glomerular tubules of the
kidney leads to phosphate retention and decreased production of the
active form of vitamin D (1,25-dihydroxy vitamin D). -
This leads to the inability of the gut to absorb calcium.
-
The resulting hypocalcemia leads to
secondary hyperparathyroidism and bone resorption, in the body’s
attempt to maintain normal serum calcium levels.
-
Rickets or osteomalacia—decreased mineralization of osteoid.
-
Osteitis fibrosis cystica—severe lytic lesions of bone caused by increased levels of parathyroid hormone.
-
Osteosclerosis—due to increased numbers of bony trabeculae, not increased mineralization of bone. This occurs in 20% of patients, and is most evident in the long bones and spine.
-
Ectopic calcification—a by-product of the
hypophosphatemia of renal patients. They are typically acidotic, which
allows for increased serum solubility of calcium salts. However, if the
level of serum calcium increases to
P.293near
normal, either spontaneously or secondary to diet or dialysis, calcium
salts will precipitate out of the bloodstream into the corneas,
conjunctivae, skin, arteriolar walls, and periarticular soft tissues.
-
Short stature
-
Developmental delay
-
Delay in appearance of secondary growth characteristics
-
All of the clinical findings associated with any form of rickets
-
Infections and pathologic fractures: frequently the side effects of treatment with either steroids or dialysis
-
Bony tenderness
-
Soft tissue itching and irritation: secondary to ectopic calcification
-
Joint pain and decreased range of motion: secondary to ectopic calcification
-
Gait disturbances
-
Slipped epiphyses: due to severe hyperparathyroidism, which causes resorption of metaphyseal bone and leads to epiphyseal lysis
-
□ Most commonly proximal femur, but can be proximal humerus, distal femur, or distal tibia
-
□ Slipping of the distal radius and ulna occurs in older children; can lead to significant deformity
-
-
Findings typical of rickets
-
Lesions typical of osteitis fibrosis cystica:
-
□ “Salt and pepper” skull
-
□ Absence of the cortical outline of the distal centimeter of the clavicles
-
□ Subperiosteal resorption of the ulnae, phalangeal distal tufts, and medial proximal tibiae
-
-
Brown tumors—large, lytic lesions with
indistinct borders, often in the pelvis or long bones, characteristic
of hyperparathyroidism
-
Usually multidisciplinary, involving a nephrologist and endocrinologist as well as an orthopaedist.
-
Management of the underlying primary renal disorder, using steroids, dialysis, or renal transplantation.
-
Control of calcium and phosphate levels using drug regimens.
-
Parathyroidectomy is sometimes necessary to control hyperparathyroidism.
-
Vitamin D must be used carefully to avoid the complication of ectopic calcification.
-
Pinning of epiphyseal slips.
-
Osteotomies for limb deformity are sometimes necessary.
DJ. Metabolic and endocrine abnormalities. In: Morrissey RT, Weinstein
SL, eds. Lovell and Winter’s pediatric orthopaedics, 4th ed. Vol 1.
Philadelphia: Lippincott Williams & Wilkins, 2001:177-241.
