CHAPTER 63 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
CHAPTER 63 – Central Quadriceps Free Tendon Reconstruction of the Anterior Cruciate Ligament
Central quadriceps tendon was first used for anterior cruciate ligament (ACL) reconstruction by John Marshall in the late 1970s.[7] Marshall incorporated a portion of the retinaculum from the anterior aspect of the patella as part of this graft. Blauth, a German surgeon, then reported use of the central quadriceps tendon with bone from the proximal patella in the 1980s.[2] Hans Uli Stäubli, a Swiss orthopedic surgeon, also used the central quadriceps tendon with bone and has studied the anatomy[10] as well as the mechanical properties of the graft.[11]
In 1995, we reported use of quadriceps tendon–bone graft for ACL reconstruction as a reliable ACL graft alternative.[4] At that time, Walter Shelton was also using the quadriceps tendon with bone for ACL reconstruction. He has subsequently reported his experience.
In 1997, with the advent of improved soft tissue fixation for ACL reconstruction, we first used the central quadriceps as a free tendon graft, without bone, for ACL reconstruction, reporting this new technique in 1999.[3] Craig Morgan also used quadriceps tendon and similarly found it to be highly satisfactory as an alternative to hamstring or bone-tendon-bone reconstruction of the ACL. Peter Jokl, at Yale University, adopted the central quadriceps free tendon graft for ACL reconstruction and has reported consistently good results with it as well. We have not chosen to use any other graft type since that time, as our results have been consistently satisfactory with a very low complication rate and stability results comparable to those obtained with other graft types. We believe that the central quadriceps free tendon provides an important alternative for ACL reconstruction, yielding results similar to those of other autografts but without some of the short- and long-term problems associated with bone-tendon-bone and hamstring reconstruction. Risk of patellar fracture[13] and anterior knee pain[9] noted after bone-tendon-bone reconstruction have been avoided with central quadriceps free tendon.[12] The long-term reports of weakness in flexion[6] and the short-term risks of hamstring spasm, bleeding, and nerve and vein injury are also obviated with use of central quadriceps free tendon.
In short, the central quadriceps free tendon is an important and desirable autograft alternative for ACL reconstruction. It is harvested from a large tendon donor site without neurovascular complication risk and without risk of patellar fracture.
We use central quadriceps tendon for reconstruction in virtually all patients, male and female, competitive athletes and working people. Our criteria for surgery, elicited in the history, include recurrent instability related to ACL deficiency that limits daily function or participation in desired athletic activity and an active athletic lifestyle requiring quick turning, pivoting, and cutting such that problems might be predictable without ACL reconstruction. We establish a loss of ACL function by clinical examination to detect positive Lachman and pivot shift test results. We routinely use magnetic resonance imaging for confirmation.
Contraindications include gross obesity, sedentary lifestyle in which ACL reconstruction may not be necessary, immunosuppressive therapy, and smoking on a regular basis. I find that most smokers are willing to give up smoking during the preoperative and postoperative period to allow graft healing. We have noted that small women (under 5 feet tall) may have a short quadriceps tendon. Even in such patients, an adequate graft can be harvested. No quadriceps tendon rupture has occurred in any of our patients.
The patient is placed on a standard operating room table with a tourniquet applied to the most proximal thigh; the operative leg is marked as appropriate for surgery, and an arthroscopic leg holder is placed over the tourniquet such that the leg is projecting off the end of the table with the lower table dropped (
Fig. 63-1
). The nonoperative leg is placed in a well-padded leg holder.
The leg is elevated and exsanguinated with an Esmarch wrap, and the tourniquet is inflated to a pressure of 250 mm Hg. The arthroscope is introduced in a standard lateral peripatellar approach, and the complete knee arthroscopy is performed before harvesting of the graft in most cases. Meniscal repair, when necessary, is performed before the ACL reconstruction.
On entering the intercondylar notch, care is taken to establish the exact nature of the ACL tear. The remnants of the ACL are probed thoroughly; a small number of patients have an intact strut of ACL plucked off the posterior intercondylar notch that may be amenable to primary repair with anchors. We have found this to be successful in the occasional appropriate patient. In such patients, the femoral attachment site is abraded, two suture anchors are placed there, and suture ends are passed through the proximal ACL stump to secure it to the avulsion site.
If the ACL tear is not repairable, all remnants of the torn ligament are resected. A limited notchplasty is performed, primarily for visualization, and thermal cautery is used to optimize the soft tissue notchplasty, to resect some ACL remnants as needed, and to improve visualization by removal of a limited amount of fat pad in some cases.
Specific Steps (
Box 63-1
)
A short incision is made over the center of the quadriceps tendon insertion into the patella at the midpoint of the proximal pole of the patella, and this incision is extended proximally (
Fig. 63-2
). In most cases, a 3- to 4-cm incision is optimal (the graft has been harvested through smaller incisions on occasion when cosmetic concerns are paramount). After opening of the fascia of the quadriceps tendon, the vastus medialis is identified and the medial border of the quadriceps free tendon autograft is established approximately 5 mm from the insertion of the vastus medialis distally. This is because the thickest portion of the quadriceps tendon is medial. Because of the convergence of the quadriceps tendon proximally, it is important to be not immediately at the medialis insertion but just slightly lateral of it. One may wish to establish medial and lateral borders of the graft by visualizing the apex of the quadriceps tendon with use of an Army-Navy retractor, then centering the graft proximally at the quadriceps tendon apex.
A standard No. 10 scalpel is used to incise the quadriceps tendon for a depth of only 7 mm. This is slightly less than the breadth of a No. 10 scalpel blade. This depth is incised from the proximal pole of the patella to the apex of the quadriceps tendon, which is visualized by retraction. A second incision is then made from the proximal pole of the patella 10 to 11 mm lateral to the first incision and precisely parallel to it. This incision is also made to a depth of 7 mm. The length of the incision proximally is generally 8 to 9 cm from the top of the patella.
At this point, a hemostat is placed between the two incisions to elevate the desired autograft portion of the quadriceps at a depth of 7 mm. This is generally just anterior to the suprapatellar pouch, leaving a few fibers (about 1 to 2 mm) of quadriceps tendon posterior to the desired autograft. The depth and amount of graft for harvest can be adjusted as desired by the surgeon.
Once it is clear that the desired amount of tendon is established by the hemostat, the hemostat is spread widely to release the posterior border of the quadriceps from the autograft.
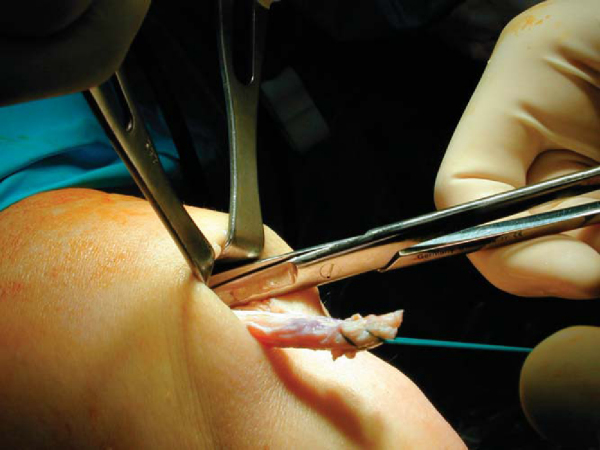
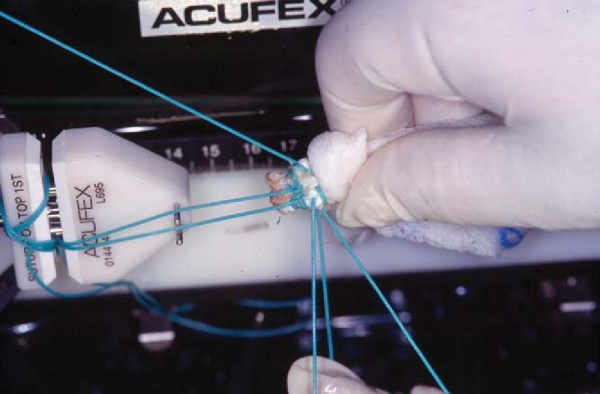
At this point, a uterine T clamp is placed on the distal end of the quadriceps autograft, and No. 5 whipstitches are placed at the distal end of the graft. Only two or three whipstitches on each side of the graft are necessary. A second set of whipstitches is placed at 180 degrees to the first set so that four strands of No. 5 suture (or No. 2 FiberWire) extend from the free tendon end.
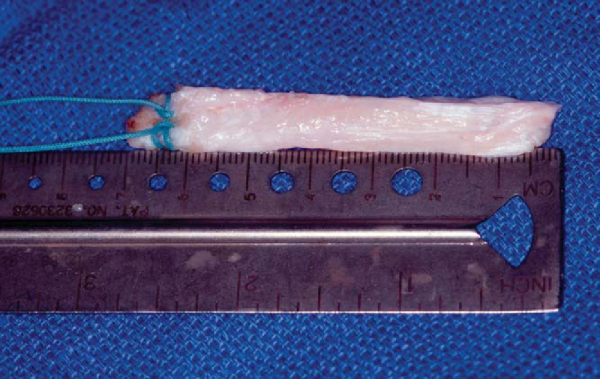
By use of blunt dissection and limited Metzenbaum scissors release proximally, the extent of the quadriceps free tendon (central quadriceps free tendon) graft is estab lished, and the free tendon graft is released at 7 to 9 cm from the top of the patella (
Fig. 63-3
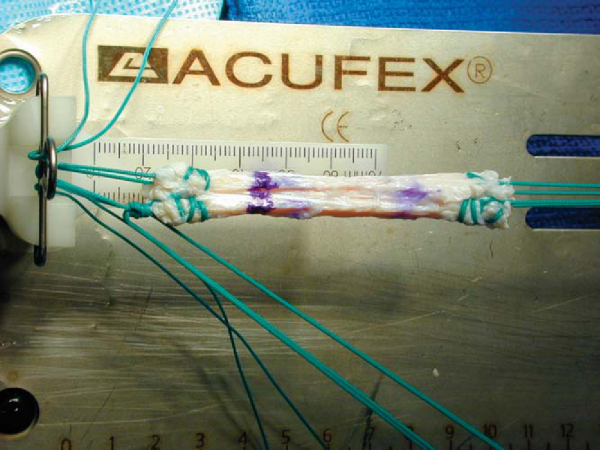
). The graft is then taken to a back table, where No. 5 whipstitches are placed in the other end of the graft (Figs. 63-4 and 63-5 [4] [5]), the graft length is confirmed, and the size of the graft is established for tibial and femoral tunnels (
Fig. 63-6
). The goal is to establish a tunnel size that will allow a snug fit of the autograft. In most cases, an 8-mm tunnel on each end is appropriate.
Principles of central quadriceps free tendon reconstruction of the ACL are the same as those of other free tendon reconstructions of the ACL.
A tibial guide is placed through a low medial, slightly enlarged arthroscopy portal, and the angle of the guide is placed at 55 degrees. The guide pin is placed through a small incision midway between the tibial tubercle and the medial collateral ligament. The guide pin is placed to exit at the midpoint of the ACL stump, generally about 8 to 9 mm anterior to the posterior cruciate ligament and at a level just posterior to the anterior horn of the lateral meniscus in most cases. The knee is taken through a full range of motion to be certain that the tunnel is free of impingement in all planes. The tibial pin is generally placed at the center of the tibial ACL insertion halfway up the intercondylar spine. It is particularly important that it not be too far lateral. A pin at the top of the tibial spine is too lateral.
The tibial tunnel is then drilled with a fully threaded drill of an appropriate size, determined by measuring the graft size with cannulas. The tibial tunnel must always be the same size as or slightly larger than the appropriate femoral tunnel size. A débridement is done after drilling of the tibial tunnel to remove ligament remnants and bone fragments that may be in the joint. A thorough irrigation is also done.
We establish the femoral tunnel with use of a guide in most cases. The goal is to be at a point consistent with the conjunction of the anteromedial and posterolateral bands of the native ACL. It is particularly important that it not be too anterior (to avoid undue tightness and stretching of the graft in flexion). Our preference, if there is any question, is to be more posterior rather than too anterior. Having said this, we establish the point for the femoral socket 6 to 7 mm anterior to the over-the-top point as determined by the blade of the guide. The guide is then rotated slightly to permit the pin to pass into the posterolateral notch at a 10:30- (right knee) or 1:30- o’clock (left knee) orientation, based on the perceived “clock face” within the notch, from the top of the notch to the articular surface of the lateral condyle. The femoral socket orientation is established with the knee at 90 degrees of flexion in all cases. Orientation of the pin is examined with a hook probe after the pin is drilled out the lateral cortex through the skin. If the orientation is thought to be appropriate and consistent with the anteromedial-posterolateral band junction, it is then drilled with an acorn-type reamer to a depth of 35 to 40 mm. Margins of the tunnel are then rasped gently. A hemostat is kept on the proximal end of the pin where it exits laterally. After this, an EndoButton drill is used to drill through the lateral cortex, and a No. 5 suture, doubled over with the loop left distally, is drawn up through tibial and femoral tunnels with a hemostat on either end.
After thorough irrigation of the joint again, the EndoButton depth gauge is used to establish distance from the lateral cortex edge to the intercondylar notch entrance of the femoral tunnel. This then determines the length of the sutures from the desired quadriceps autograft femoral intercondylar notch point to the EndoButton itself.
Sutures of the quadriceps autograft are threaded through the EndoButton on a Graft Master, and we prefer to place one of each suture through one central eye of the EndoButton and then back down through the other central eye of the EndoButton such that there are two No. 5 strands going in and out through the other central eye. These are then tied to the other ends of the No. 5 sutures immediately adjacent to the quadriceps tendon graft. After a secure knot is tied with at least four throws, the suture ends are cut. The distance from the EndoButton to a point marked at approximately 2 cm from the tip of the quadriceps graft should be exactly the same as the distance measured with the EndoButton depth gauge from the lateral cortex to the femoral socket entry point.
After this, a No. 5 suture is placed through one side of the EndoButton, a No. 2 suture through the other, and the graft is drawn up through the tibia into the femoral socket. The EndoButton is flipped after it is through the proximal femoral cortex hole.
Interference screw fixation with poly-l-lactic acid (PLLA) screws has been a successful alternative,[14] giving the option of an anchor such as an EndoPearl (Linvatec, Largo, Fla) or a bone disk[15] (
Fig. 63-7
) on the femoral side. We prefer EndoButton fixation alone on the femoral side.
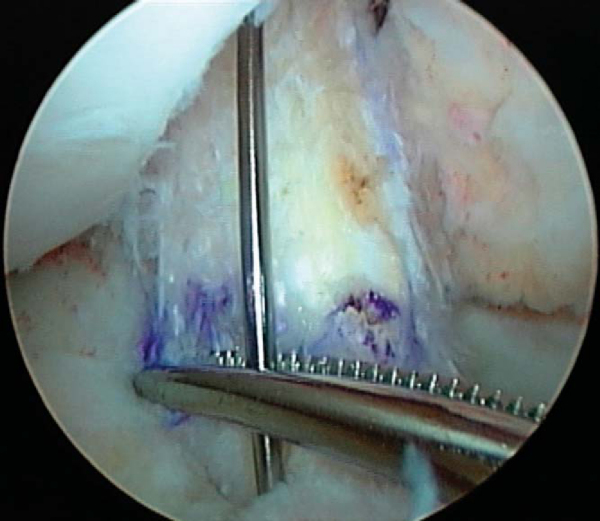
For tibial side fixation, I prefer a polylactate bioabsorbable screw, 5 to 10 mm from the joint space (near but not at the tunnel opening into the joint). On the basis of studies by Nagarkatti,[8] we use a PLLA screw one size larger than the tibial tunnel size and place it carefully through the tibial tunnel, over a guide pin (
Fig. 63-8
), while holding the knee at 20 degrees of flexion and at tension equivalent to a 30- to 40-pound pull after thoroughly cycling the graft after femoral fixation. We are sure to insert the screw by turning (not pushing) the screw so that there is no risk of pushing the graft back. We prefer two sets of No. 5 whipstitches (FiberWire is a desirable alternative) coming off the tibial end of the graft (four strands). Although it is not necessary to achieve a stable knee, these suture ends may be tied over a button at the tunnel entrance for added security.
| PEARLS AND PITFALLS | ||||||||||||||||||
|
Patients are placed in a knee immobilizer after surgery but encouraged to bear full weight and to start immediate range of motion. A home program of closed-chain exercises has worked well, and loss of range of motion is extremely uncommon. Most patients achieve motion quickly as pain is less than with other autografts. Closed-chain physical therapy may be started after 10 days to 2 weeks (we generally use subcuticular closure). Most patients are off crutches with supportive quadriceps function by 2 weeks from the time of surgery. Patients do closed-chain exercises for 3 months and then progress to running. Most patients return to competitive sports at 6 months. The cosmetic results have been excellent (
Fig. 63-9
).
In a long-term followup study (all patients more than 2 years after surgery; average, 66 months) of the central quadriceps free tendon for ACL reconstruction (DeAngelis, Cote, and Fulkerson, unpublished), the median International Knee Documentation Committee score at followup was 90, the average side-to-side KT-1000 difference (20-pound pull) was 1.2 mm, and the single-leg hop quotient was 0.96. There were five graft failures in the group of 124 patients. Most important, no patient had anterior knee pain or loss of knee range of motion.
Short-term pain has been less than with alternative autografts, and satisfaction of patients has been consistently high. In a short-term followup study by Joseph,[5] patients undergoing central quadriceps free tendon ACL reconstruction reported pain medication use for 6 days, versus 19 days in a matched group of patients receiving hamstring autografts and 22 days in a comparable group of patients with bone-tendon-bone ACL reconstruction. The patients undergoing central quadriceps free tendon reconstruction also reached rehabilitation landmarks sooner.
Finally, Adams et al[1] have demonstrated by mechanical testing that the quadriceps tendon is stronger, in general, after graft harvest than the patellar tendon is before a bone-tendon-bone graft is harvested.
1.
Adams D, Mazzocca A, Fulkerson J: Residual strength of the quadriceps versus patellar tendon after harvesting a central free tendon graft.
Arthroscopy 2006; 22:76-79.
2.
Blauth W: Die zweizugelige Ersatzplastik des Vorderen Kreuzband der Quadricepssehne.
Unfallheilkunde 1984; 87:45-51.
3.
Fulkerson J: Central quadriceps free tendon for anterior cruciate ligament reconstruction.
Oper Tech Sports Med 1999; 7:195-200.
4.
Fulkerson JP, Langeland R: An alternative cruciate reconstruction graft: the central quadriceps tendon.
Arthroscopy 1995; 11:252-254.
5.
Joseph M, Fulkerson J, Nissen C, Sheehan TJ: Short-term recovery after anterior cruciate ligament reconstruction: a prospective comparison of three autografts.
Orthopedics 2006; 29:243-248.
6.
Marder RA, Raskind JR, Carroll M: Prospective evaluation of arthroscopically assisted anterior cruciate ligament reconstruction. Patellar tendon versus semitendinosus and gracilis tendons.
Am J Sports Med 1991; 19:478-484.
7.
Marshall JL, Warren RF, Wickiewicz TL, Reider B: The anterior cruciate ligament: a technique of repair and reconstruction.
Clin Orthop 1979; 143:97-106.
8.
Nagarkatti DG, McKeon BP, Donahue BS, Fulkerson JP: Mechanical evaluation of a soft tissue interference screw in free tendon anterior cruciate ligament graft fixation.
Am J Sports Med 2001; 29:67-71.
9.
Sachs RA, Daniel DM, Stone ML, Garfein RF: Patellofemoral problems after anterior cruciate ligament reconstruction.
Am J Sports Med 1989; 17:760-765.
10.
Stäubli HU, Schatzmann L, Brunner P, et al: Quadriceps tendon and patellar ligament: cryosectional anatomy and structural properties in young adults.
Knee Surg Sports Traumatol Arthrosc 1996; 4:100-110.
11.
Stäubli HU, Schatzmann L, Brunner P, et al: Mechanical tensile properties of the quadriceps tendon and patellar ligament in young adults.
Am J Sports Med 1999; 27:27-34.
12.
Theut P, Fulkerson J. Anterior cruciate ligament reconstruction utilizing central quadriceps free tendon: a retrospective functional outcome study. Presented at the annual meeting of the American Academy of Orthopaedic Surgeons, San Francisco, 2001.
13.
Viola R, Vianello R: Three cases of patella fracture in 1,320 anterior cruciate ligament reconstructions with bone–patellar tendon–bone autograft.
Arthroscopy 1999; 15:93-97.
14.
Weiler A, Hoffmann RF, Bail HJ, et al: Tendon healing in a bone tunnel. Histological analysis after biodegradable interference fit fixation in a model of anterior cruciate ligament reconstruction in sheep.
Arthroscopy 2002; 18:124-135.
15.
Weiler A, Richter M, Schmidmaier G, et al: The EndoPearl device increases fixation strength and eliminates construct slippage of hamstring tendon grafts with interference screw fixation.
Arthroscopy 2001; 17:353-359.