Capsular Release for Flexion Contracture: The Column Procedure
has not been badly injured and the loss of motion is limited to
extension due primarily to thickening of the anterior capsule. This
type of stiffness is termed extrinsic and the joint surface is minimally damaged (7).
In this circumstance several options are available. The technique
described later is used in preference to an anterior exposure. The
indications are very similar, and the author has found this technique
to be simple and reliable with a low complication rate (6). This exposure is preferable in the author’s opinion to a formal anterior approach (3, 8,10) and avoids the more aggressive release needed for intrinsic contracture (7,11). Arthroscopic release of the anterior capsule is discussed in Chapter 2 (5).
extension of at least 40 degrees and preservation or minimal changes of
the articular surface. Posttraumatic etiology such as dislocation is an
ideal indication. If limitation of motion includes loss of flexion, an
additional step is needed, but the loss of flexion can usually be
effectively treated by anterior capsular release.
requiring interposition of the joint. Interposition is used if any of
the following three contraindications are present (7):
a significant alteration of the articular contour, loss of joint
cartilage (50%), or pathology that requires release of one or both
collateral ligaments (see Chapter 22).
spasticity, especially involving the flexor muscles and residual
impairment from closed head injury.
 |
|
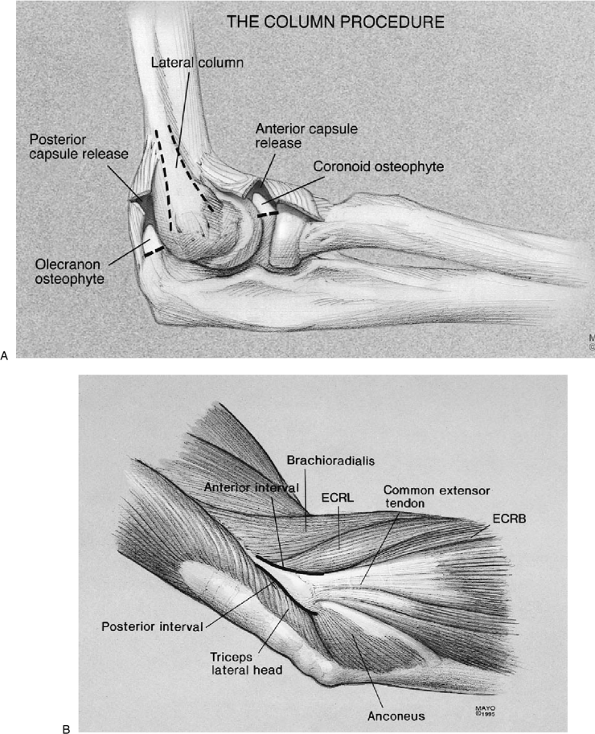
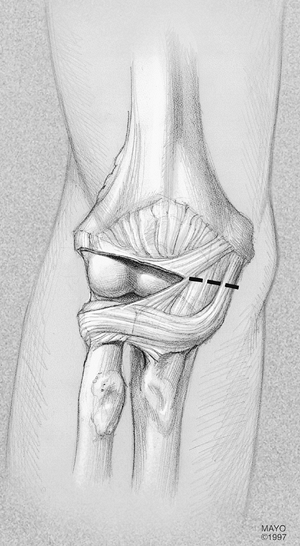
Figure 21-1. A:
The concept of the column procedure. Identify the supracondylar ridge and approach the anterior and posterior aspects of the capsule as necessary. Osteophytes are readily removed from the coronoid process or the olecranon. B: Relevant anatomy of the “column.” The anterior and posterior aspects of the lateral column are identified (solid lines). (Abbreviations: ECRL, extensor carpi radialis longus; ECRB, extensor carpi radialis brevis.) |
pathology (i.e., extrinsic to the joint surface). This is determined in
my practice by a simple lateral radiograph. This is the least expensive
and the most accurate manner of evaluating the joint before surgery.
There is no indication for an MR or a CT scan in treating patients with
capsular contracture or posttraumatic loss of motion.
are both flexion and extension elements to the contracture. If the
patient has normal or near normal flexion, then the dissection may be
limited to the anterior capsule with the simple elevation of the common
extensor tendon and exposure of the anterior capsule. If the patient
has limitation of flexion, then elevation of the triceps and removal of
the posterior capsule are necessary. Although the determination of the
extent of such resection is obviously done at the time of surgery, it
is important to discuss the nature of the surgery preoperatively with
the patient in the context of the anticipated rehabilitation and
ultimate result.
aware of the implications of ulnar nerve irritation before surgery.
This aspect is carefully sought and discussed. If present, a posterior
incision is made and the ulnar nerve is explored. If it is injured
before or after capsule release, the nerve is decompressed or
translocated.
involvement or that a release of the collateral ligament is necessary
to obtain adequate exposure, then the surgeon should be prepared to
apply the distraction device protecting the collateral ligament repair
and separating the joint surfaces for approximately 3 weeks after
surgery (see Chapters 8 and 22).
It is uncommon to be faced with this option if the proper determination
of the nature of the contracture and adequate imaging and assessment of
the joint surface have occurred before the surgery as discussed earlier.
understanding of the time commitment that is required after such
surgery. The emphasis on the maintenance of the splinting program for
several weeks or even months following the procedure is quite
important, particularly depending upon the type of occupation and the
expectations that the patient may hold.
column procedure consists of arthrotomy, release of the anterior and
posterior capsule if needed, and excision of osteophytes through a
limited lateral approach (Fig. 21-1).
ipsilateral extremity and the arm draped free and brought across the
chest. The proximal one-half of a Kocher incision, which extends 6 cm
proximal to and 3 cm distal to the epicondyle, is used if there is no
previous incision and if there are no symptoms related to the ulnar
nerve (Fig. 21-2). If there are symptoms
related to the ulnar nerve, a midline posterior incision is made so
that the nerve can be explored. If there is gross evidence of
impingement before or after the capsular release, the nerve is
decompressed as necessary.
minimum disruption of normal tissue, the fleshy origin of the extensor
carpi radialis longus and the distal fibers of the brachioradialis are
identified (Fig. 21-3). Release of the origin of these muscles from the humerus provides direct access to the superolateral aspect of the capsule (Fig. 21-4).
The brachialis is swept from the anterior aspect of the capsule with a
periosteal elevator. The capsule is entered anteriorly at the
radiohumeral joint to allow assessment of the thickness of the capsule (Fig. 21-5A). A modified knee retractor (V. Muller and Co., St. Louis, MO) with a blade-shaft angle of 130 degrees (Fig. 21-5B)
protects the brachialis, the radial nerve, and the brachial artery. The
anterior aspect of the capsule is grasped, and the lateral half is
excised
to
at least the level of the coronoid. The most medial aspect of the
capsule, which can sometimes be difficult to visualize but can be
palpated, is incised to complete the release (Fig. 21-6).
The elbow is extended, and any remnant adhesion is gently lysed. At
this time, if there is full extension or if extension is within 10
degrees of normal and there are no radiographically evident spurs on
the olecranon, no additional release is needed. The capsule is left
open, and the wound is closed.
 |
|
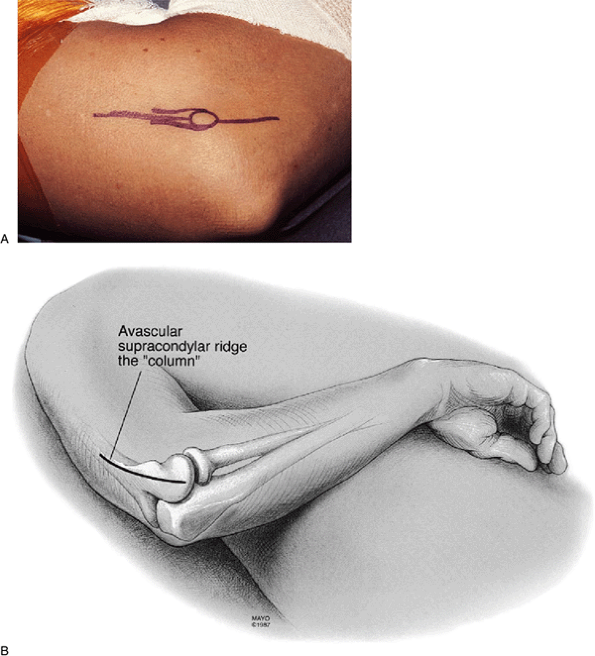
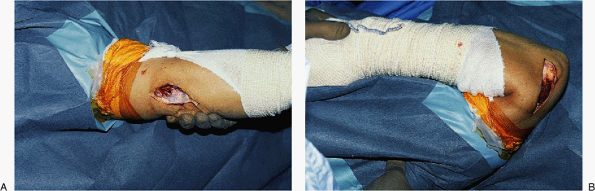
Figure 21-2. A,B:
If a simple “column” release is anticipated a limited incision measuring 6 to 8 cm in length is made over the lateral column, ending 2 cm distal to the lateral epicondyle as shown in this right elbow. |
this is probably the result of extensive scarring and adhesions
involving the posterior aspect of the capsule. If this is the case, the
triceps is elevated from the posterior aspect of the humerus, the
posterior aspect of the capsule is released, and the olecranon fossa is
cleaned of soft tissue. The tip of the olecranon is removed with an
osteotome if there are osteophytes (Fig. 21-7). The amount of flexion
and extension of the elbow is assessed. Typically, full extension is readily attained (Fig. 21-8).
If there is at least 130 degrees of flexion, nothing more needs to be
done posteriorly. If flexion is limited, the coronoid is inspected and
any osteophytes are removed.
 |
|
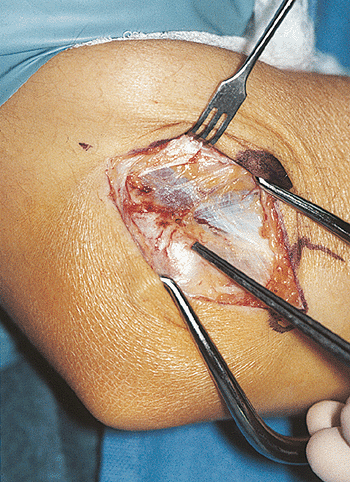
Figure 21-3.
The proximal most muscular attachment to the common extensor tendon defines the origin of the extensor carpi radialis longus. The forceps are on the lateral epicondyle. |
 |
|
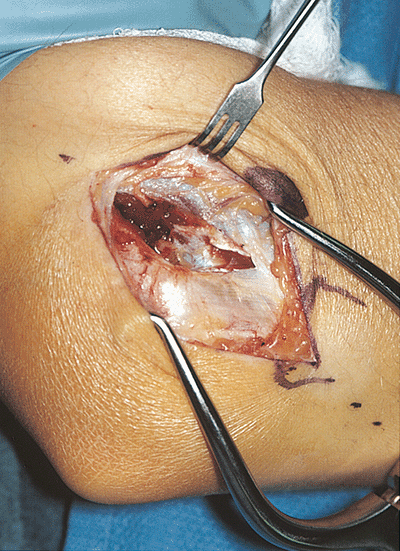
Figure 21-4.
With the elbow at 90 degrees of flexion, the fibers of the extensor carpi radialis longus are followed down to the capsule. The brachialis is elevated from the anterior capsule. |
 |
|
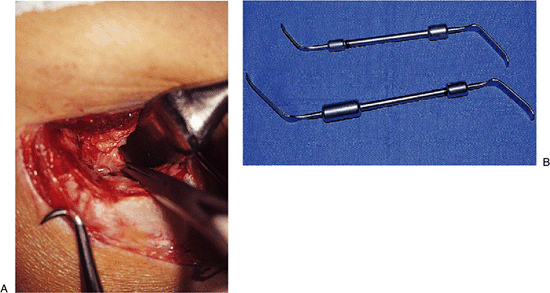
Figure 21-5. A:
Elevation of the extensor carpi radialis longus (ECRL) and the distal fibers of the brachioradialis. The anterior aspect of the capsule is isolated from the brachialis and is identified with an arthrotomy at the anterior aspect of the radiohumeral joint. B: Special retractors (available from Müeller, in two sizes) facilitate exposure and protection of the anterior structures. |
 |
|
Figure 21-6.
The lateral half of the anterior aspect of the capsule is excised as widely as possible, and the remaining medial half is incised (dotted line). |
 |
|
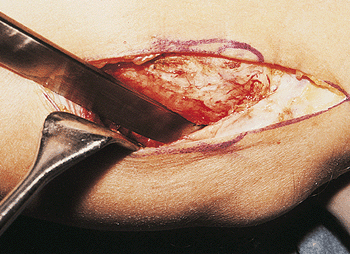
Figure 21-7.
In those instances in which there is also loss of flexion, the triceps is elevated from the posterolateral column and the posterior capsule is also excised. If an osteophyte is present, it is removed with an osteotome. |
 |
|
Figure 21-8.
As the joint tends to “rebound” about 15 to 20 degrees from the amount of extension gained at surgery, full extension at the time of surgery is considered a must with this type of procedure. |
which is defined as a subjective alteration in sensation without
objective sensory or motor changes or atrophy, a posterior incision is
used to allow assessment of the lateral and medial aspects of the elbow
through the same skin incision. The ulnar nerve is inspected, and
occasionally it is translocated, but more often it is simply
decompressed in situ.
reveals normal findings, a catheter is inserted percutaneously for a
brachial plexus block, which is maintained with a continuous pump (2). The arm is elevated as much as possible, and continuous passive motion is begun on the day of the operation (1,9).
The machine is adjusted to provide as much motion as pain or the
machine itself allows. The block is discontinued 2 days
postoperatively, and continuous passive motion is discontinued 3 days
postoperatively, at which time the patient is dismissed.
therapy with adjustable splints, which depends on the motion before and
after the procedure, is prescribed. The splints include a
hyperextension or hyperflexion brace, or both. The splint program
usually begins with 20 hours/day for 3 weeks (see Chapter 9).
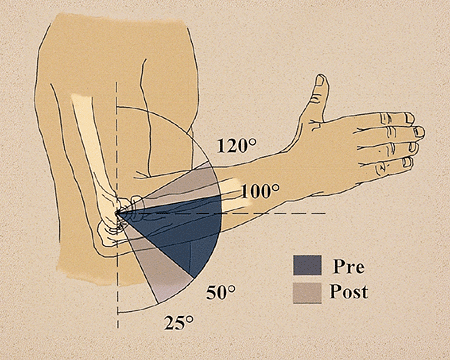
52 to 101 degrees) improved postoperatively to a mean arc of 94 degrees
(from 27 to 121 degrees) (Fig. 21-9). The mean
total gain in the arc of flexion-extension was 45 degrees. Overall, 31
elbows (82%) had a satisfactory result. Greater improvement was
obtained in elbows that had had the more severe stiffness. Others have
reported similar results with the more limited exposure and release (4,12).
 |
|
Figure 21-9. The overall gain in extension and flexion from 52–101 to 27–121 degrees.
|
technique described. To date no patients have permanent neurologic
deficiency, but two have ulnar nerve irritation. Infection, ectopic
bone, or increased pain, although a possibility, have not been recorded.
was treated in a cast for 3 weeks and developed a contracture from 70
to 100 degrees (Fig. 21-10). After release the arc improved
from 20 to 125 degrees (Fig. 21-11). There was no pain and the patient was pleased with the outcome.
 |
|
Figure 21-10. Marked contracture developed after 3 weeks immobilization for “simple” dislocation. The joint is intact.
|
 |
|
Figure 21-11. A,B: Near normal motion of 0 to 135 degrees was obtained at the time of surgery after anterior/posterior capsular release.
|
HS III, Sullivan FL, Urbaniak JR. Anterior capsulotomy and continuous
passive motion in the treatment of post-traumatic flexion contracture
of the elbow: a prospective study. J Bone Joint Surg 1992;74A:1229–1234.
RR, Beaton D, Bechard M. Restoration of elbow motion by anterior
capsular release of post-traumatic flexion contractures. J Bone Joint Surg 1991;73B(Suppl II):107.
RB, Hamilton HW, Wedge JH, et al. Clinical application of basic
research on continuous passive motion for disorders of injuries of
synovial joints. J Orthop Res 1984;1:325.
JR, Hansen PE, Beissinger SF, et al. Correction of post-traumatic
flexion contracture of the elbow by anterior capsulotomy. J Bone Joint Surg 1985;67A:1160–1164.
K, Mizueki T. Debridement arthroplasty for advanced primary
osteoarthritis of the elbow: results of a new technique used for 29
elbows. J Bone Joint Surg 1994;76B:641–646.
