The Wrist and Hand
this chapter: three to the wrist and two each to the flexor tendons and
scaphoid.
is used primarily for exploring the carpal tunnel and its enclosed
structures. The applied anatomy of each approach is considered
separately in this chapter.
is useful in the treatment of phalangeal fractures. A discussion of the
applied anatomy of the finger flexor tendons follows the description of
these two approaches in this chapter.
The methods of drainage used for these conditions are described
together, with an introduction to the general principles of drainage in
the hand. Of all the infections of the hand that require surgery,
paronychia and felons are by far the most common.
surgical approaches. In the hand, however, the majority of wounds
encountered arise from trauma, not from planned incisions. A brief
review of the overall anatomy of the hand is vital to explain the
damage that may be caused by a particular injury. Although clinical
findings are the key to the accurate diagnosis of tissue trauma,
knowledge of the underlying anatomy is crucial in bringing to light all
possibilities and minimizing the risk that a significant injury will be
overlooked. For example, arterial hemorrhage from a digital artery in a
finger nearly always is associated with damage to a digital nerve,
because the nerve lies volar to the severed artery. Arterial hemorrhage
in a finger should alert the surgeon to the possibility of nerve
injury, which often appears clinically as a change in the quality of
sensation rather than as complete anesthesia, and can be overlooked in
a brief examination.
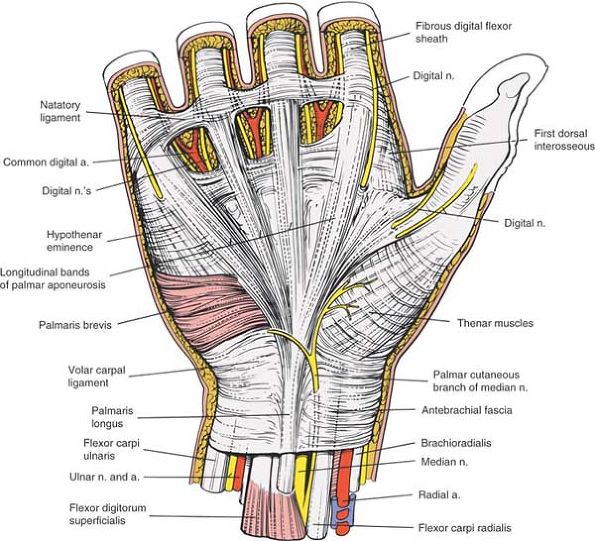
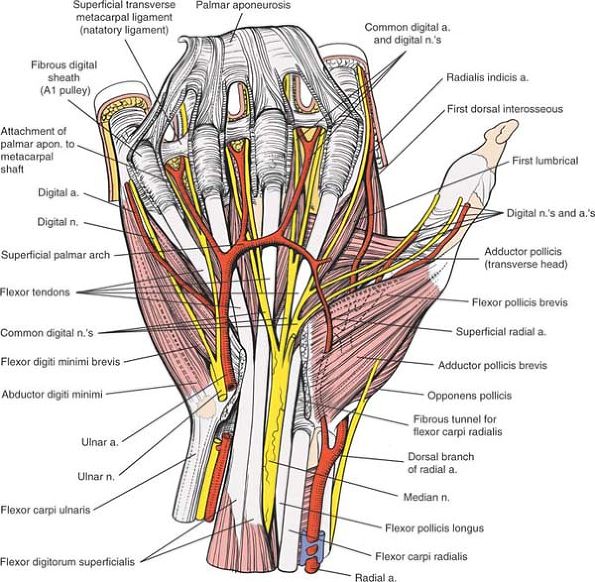
topographic anatomy of the hand. This information is presented in one
section rather than on an approach-by-approach basis to provide a clear
and integrated picture of hand anatomy.
the extensor tendons that pass over the dorsal surface of the wrist. It
also allows access to the dorsal aspect of the wrist itself, the dorsal
aspect of the carpus, and the dorsal surface of the proximal ends of
the middle metacarpals. Its uses include the following:
-
Synovectomy and repair of the extensor tendons in cases of rheumatoid arthritis; dorsal stabilization of the wrist1,2
-
Wrist fusion3
-
Excision of the lower end of the radius for benign or malignant tumors
-
Open reduction and internal fixation of
certain distal radial and carpal fractures and dislocations, including
dorsal metacarpal dislocations, displaced intraarticular dorsal lip
fractures of the radius, and transscaphoid perilunate dislocations.
Plates applied to the dorsal surface of the distal radius frequently
cause irritation to the numerous extensor tendons that pass over their
surface. For this reason, volar approaches are now usually preferred
for plate fixation of fractures of the distal radius. Volar approaches
are particularly suitable for locked internal fixators. -
Proximal row carpectomy4,5
the forearm and put the arm on an arm board. Exsanguinate the limb by
applying a soft rubber bandage, and then inflate a tourniquet (Fig. 5-1).
 |
|
Figure 5-1
Place the patient supine on the operating table. Turn the forearm downward and place the arm on a board, for the dorsal approach to the wrist joint. |
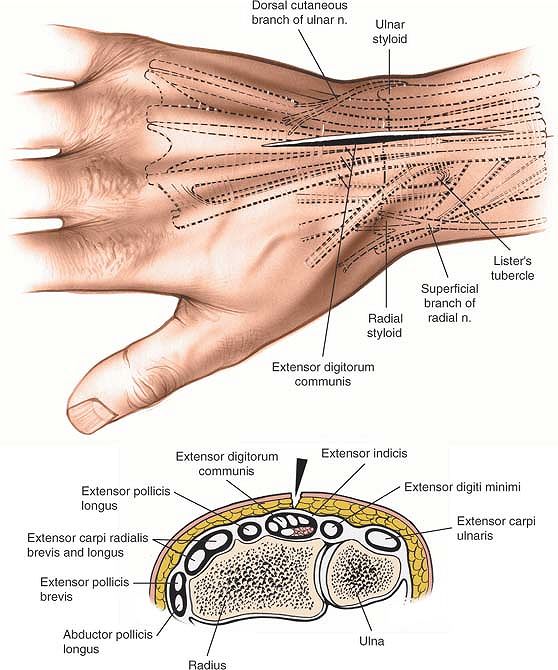
of the wrist, crossing the wrist joint midway between the radial and
ulnar styloids. The incision begins 3 cm proximal to the wrist joint
and ends about 5 cm distal to it. It can be lengthened if necessary (Fig. 5-2).
and redundant, the incision does not cause a contracture of the wrist
joint, even though it crosses a major skin crease at right angles.
extensor carpi radialis longus muscle and the extensor carpi radialis
brevis muscle are supplied by the radial nerve. Because both muscles
receive their nerve supply well proximal to the incision, however, the
intermuscular plane between them can be used safely.
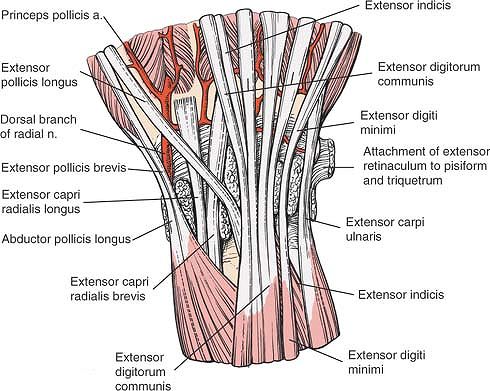
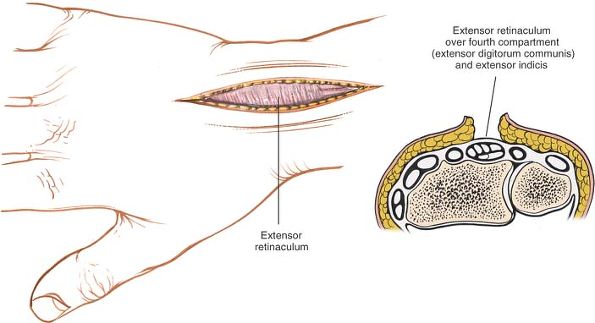
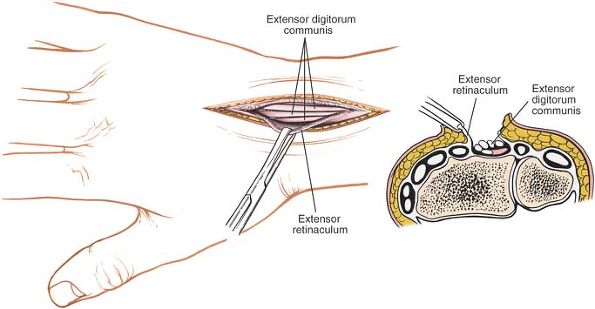
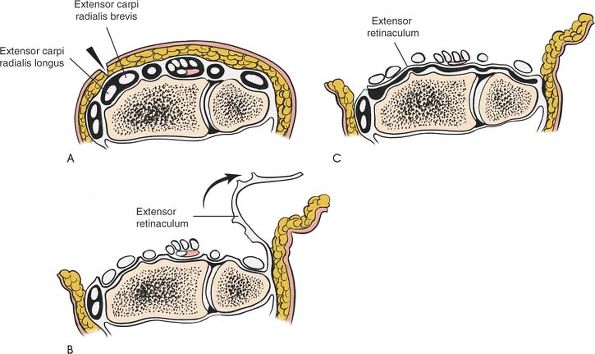
incision to expose the extensor retinaculum that covers the tendons in
the six compartments on the dorsal aspect of the wrist (Fig. 5-3).
radialis longus and brevis muscles in the second compartment of the
wrist. The compartment is on the radial side of Lister’s tubercle. To
expose the other compartments, incise the ulnar edge of the cut
retinaculum by sharp dissection in an ulnar direction to deroof
sequentially the four compartments on the ulnar side. Then, dissect the
radial edge of the cut extensor retinaculum radially to deroof the
first compartment. The extensor retinaculum should be preserved;
during
closure, it can be sutured underneath the extensor tendons to prevent
them from being abraded by the bones, which can be deformed grossly by
rheumatoid arthritis (Fig. 5-8).
 |
|
Figure 5-2 Skin incision for the dorsal approach to the wrist joint. A cross section at the distal portion of the radius is seen.
|
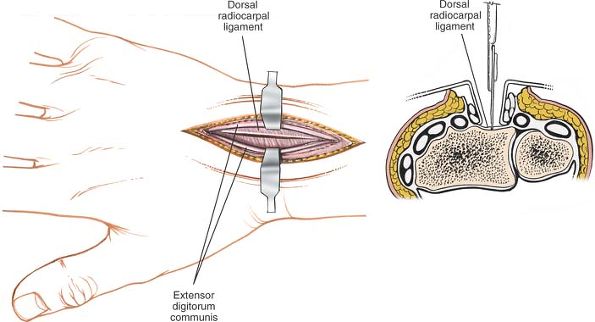
digitorum communis and extensor indicis proprius muscles in the fourth
compartment of the wrist. Mobilize the tendons of the compartment,
lifting them from their bed in an ulnar and radial direction to expose
the underlying radius and joint capsule (Fig. 5-4). Incise the joint capsule longitudinally on the dorsal aspect of the radius and carpus (Fig. 5-5).
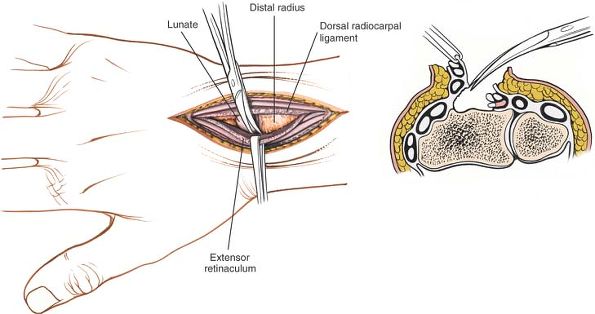
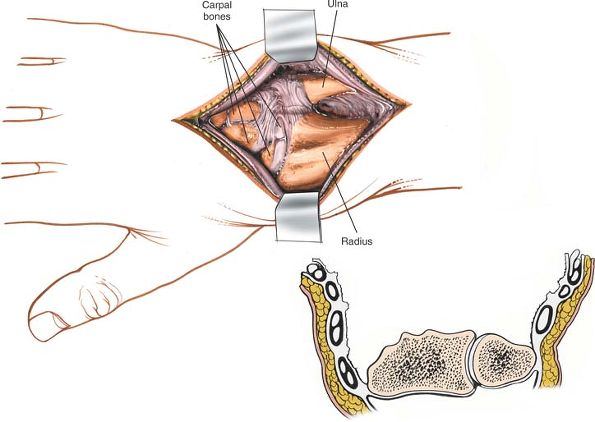
Continue the dissection below the capsule (the dorsal radiocarpal
ligament) toward the radial and ulnar sides of the radius to expose the
entire distal end of the radius and carpal bones (Figs. 5-6 and 5-7).
brevis muscles, which attach to the bases of the second and third
metacarpals and lie in a tunnel on the radial side of Lister’s
tubercle, must be retracted radially to expose fully the dorsal aspect
of the carpus.
 |
|
Figure 5-3
Skin flaps are developed, and the extensor retinaculum is visualized in the deeper portion of the wound. Cross section reveals the approach to the fourth tunnel, which contains the extensor digitorum communis and the extensor indicis proprius. |
 |
|
Figure 5-4 The retinaculum over the fourth compartment has been opened, revealing the communis tendons.
|
 |
|
Figure 5-5
The extensor communis tendons and extensor indicis proprius have been retracted, revealing the dorsal radiocarpal ligament and the joint capsule, which then is incised. |
 |
|
Figure 5-6
The dorsal radiocarpal ligament and the extensor tendons are elevated from the posterior aspect of the radius to expose the entire dorsal end of the bone. |
 |
|
Figure 5-7 The extensor tendons in their compartments have been elevated to expose the distal end of the radius and ulna.
|
 |
|
Figure 5-8 (A) For synovectomy, make an incision over the second compartment. (B)
Open each of the compartments sequentially from radius to ulna by incising the septum that connects the retinaculum to the carpus itself and the joint capsule. (C) Now that the compartments have been deroofed, place the retinaculum between the extensor tendons and the distal ends of the radius and ulna to provide added protection for the tendons. |
 |
|
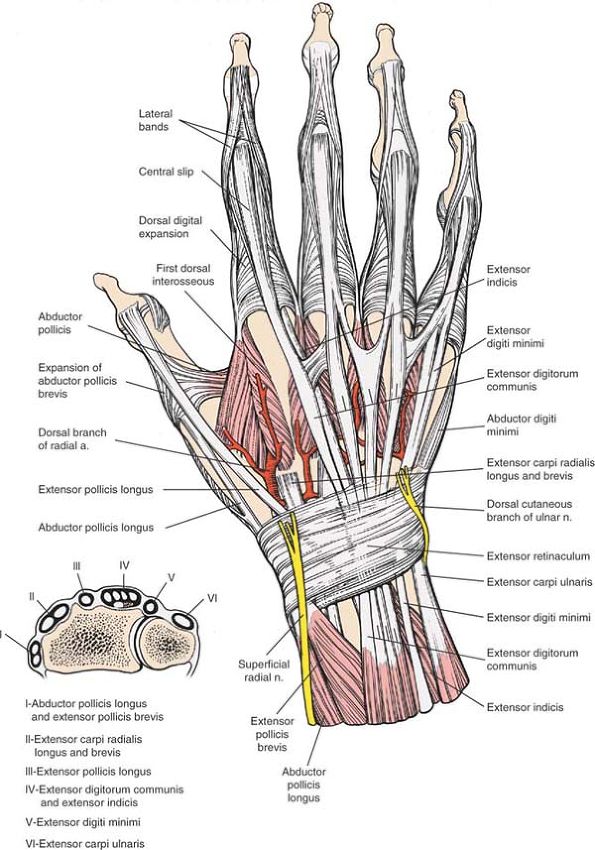
Figure 5-9 The dorsal aspect of the wrist and hand. Cross section of the distal forearm (inset). Note the compartmentalization of tendons into six distinct tunnels at the dorsal aspect of the distal forearm.
|
(superficial radial nerve) emerges from beneath the tendon of the
brachioradialis muscle just above the wrist joint before traveling to
the dorsum of the hand. The skin incision lies between skin that is
supplied by cutaneous branches of the ulnar nerve and skin that is
supplied by cutaneous branches of the radial nerve. Damage to cutaneous
nerves commonly occurs if the dissection of the flaps is begun within
the fat layer. If the skin incision is taken down to the extensor
retinaculum before the ulnar and radial flaps are elevated, the nerves
are protected by the full thickness of the fat. Take care, however, to
identify and preserve any nerve branches that are encountered during
the incision of the subcutaneous tissue (Fig. 5-9).
the wrist joint on its lateral aspect. As long as the dissection at the
level of the wrist joint remains below the periosteum, the artery is
difficult to damage.
the incision cannot be extended proximally to expose the rest of the
radius. It can be extended to expose the distal half of the dorsal
aspect of the radius, however, by retracting the abductor pollicis
longus and extensor pollicis brevis muscles, which cross the operative
field obliquely.
extend the incision distally and retract the extensor tendons. (This
type of extension seldom is required in practice.) The approach
provides excellent exposure of the wrist joint and allows easy access
to all six compartments of the extensor tunnel.
joint and pass beneath the extensor retinaculum, which is a thickening
of the deep fascia of the forearm. The extensor retinaculum prevents
the tendons from “bowstringing.” Fibrous septa pass from the deep
surface of the retinaculum to the bones of the forearm, dividing the
extensor tunnel into six compartments. These septa must be separated
from the retinaculum so that each compartment can be opened in surgery
(see Fig. 5-9).
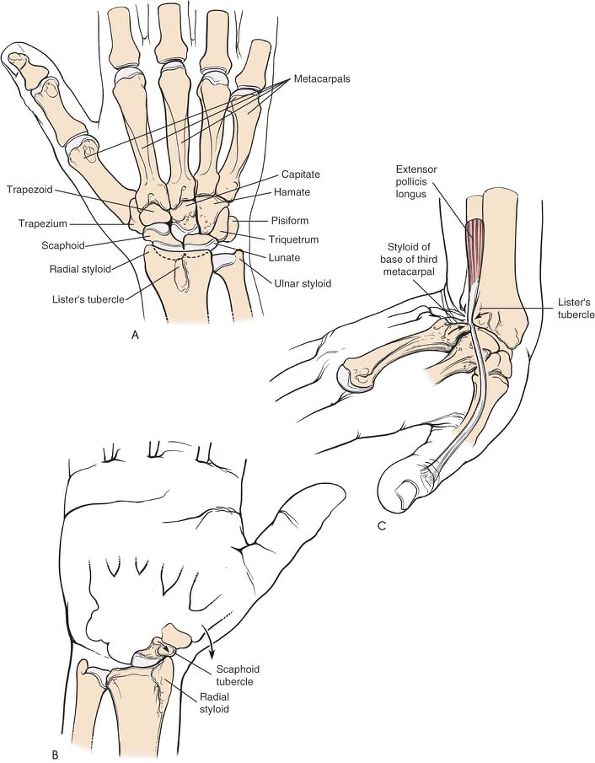
is the distal end of the lateral side of the radius. It also is the
site of attachment of the tendon of the brachioradialis muscle. Its
medial part articulates with the scaphoid bone (Fig. 5-12A).
Strong and sudden radial deviation of the wrist may cause the radial
styloid process to slam into the scaphoid and fracture it (see Fig. 5-12B). Alternatively, such a force may cause a fracture of the radial styloid.
fails to reunite or after arthritic changes in the wrist joint have
affected the radial margin of the radioscaphoid joint.
dorsoradial tubercle) is a small bony prominence on the dorsum of the
radius. The tendon of the extensor pollicis longus muscle angles around
its distal end, changing direction about 45° as it does so. When the
wrist is hyperextended, the base of the third metacarpal comes very
close to Lister’s tubercle, and the two bones can crush the trapped
tendon of the extensor pollicis longus. This probably is the reason the
tendon suffers delayed rupture in some cases of minimal or undisplaced
fractures of the distal radius; the tendon sustains a vascular insult
at the time of the original injury, even though it remains intact (see Fig. 5-12C).4
the skin almost perpendicularly on the dorsum of the wrist can cause
broad scarring. Nevertheless, because the skin on the wrist is so
loose, this is one of those rare occasions when a skin incision can cross a major skin crease at right angles without causing a joint contracture.
that lies obliquely across the dorsal aspect of the wrist. Its radial
side is attached to the anterolateral border of the radius; its ulnar
border is attached to the pisiform and triquetral bones. (Were it
attached to both bones of the forearm instead, pronation and supination
would be impossible, because its fibrous tissue is incapable of
stretching the necessary 30%.)
retinaculum to the bones of the carpus, dividing the extensor tunnel
into six compartments (Fig. 5-10). From the radial (lateral) to the ulnar (medial) aspect, the compartments contain the following:
-
Abductor pollicis longus and extensor pollicis brevis.
These tendons lie over the lateral aspect of the radius. They may
become trapped or inflamed beneath the extensor retinaculum in their
fibroosseous canal, producing de Quervain’s disease (tenosynovitis
stenosans). -
Extensor carpi radialis longus and extensor carpi radialis brevis.
These muscles run on the radial side of Lister’s tubercle before
reaching the dorsum of the hand. The tendon of the extensor carpi
radialis longus is used frequently in tendon transfers. The tendons run
in separate synovial sheaths.![]() Figure 5-10
Figure 5-10
Anatomy of the distal forearm, with the extensor retinaculum excised
and the septa remaining. The retinaculum on the ulnar side inserts into
the triquetrum and pisiform bones. -
Extensor pollicis longus.
This tendon passes into the dorsum of the hand on the ulnar side of
Lister’s tubercle. It may rupture in association with fractures or
rheumatoid arthritis. The oblique passage of this tendon on the dorsal
aspect of the wrist creates significant problems for plate fixation of
fractures of the distal radius. Tendon irritation and even rupture may
occur due to abrasion of the tendon on the surface of the plate.
Similar problems apply to a lesser degree with all the other extensor
tendons.6 -
Extensor digitorum communis and extensor indicis. The indicis tendon is used commonly in tendon transfers.
-
Extensor digiti minimi. This tendon overlies the distal radioulnar joint.
-
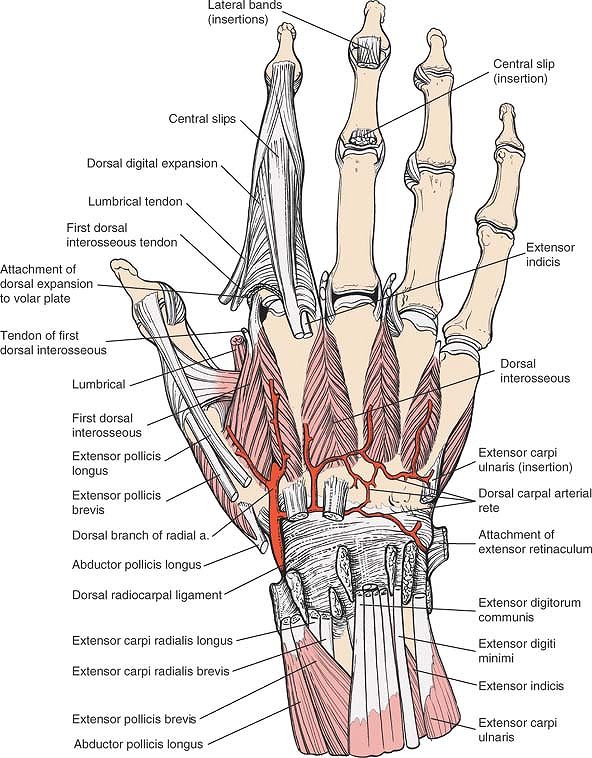
Extensor carpi ulnaris. This tendon passes near the base of the ulnar styloid process. It is used sometimes in tendon transfers (Fig. 5-11; see Fig. 5-10).
 |
|
Figure 5-11
The extensor tendons have been removed, revealing the dorsal radiocarpal ligament. The radial artery is seen piercing the first dorsal interosseous muscle and contributing to the dorsal carpal rete. Note the hood mechanism for the index finger; contributions are made to it by the first dorsal interosseous and the first lumbrical muscles. |
 |
|
Figure 5-12 (A) Dorsal aspect of the bones of the distal forearm, wrist, and proximal hand. (B)
A strong and sudden radial deviation of the wrist may cause the radial styloid process to impinge on the scaphoid tubercle and fracture it. (C) With sudden extreme dorsiflexion of the wrist, as when one falls on an outstretched hand, the extensor pollicis longus tendon may be trapped or crushed between the dorsal radial tubercle (Lister’s tubercle) and the base of the third metacarpal. |
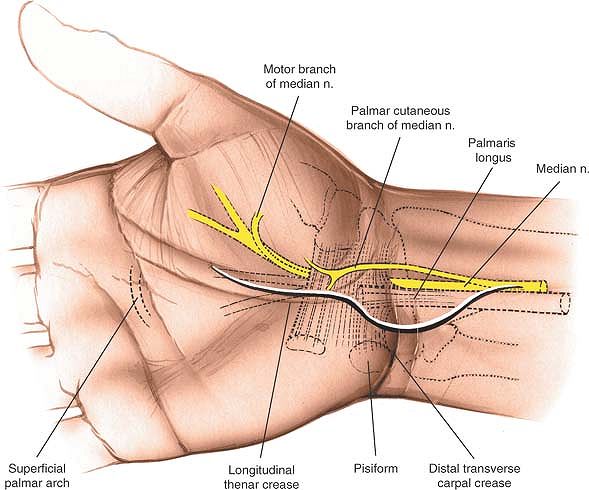
tunnel is one of the most common operations of the hand. Two anatomic
structures, the motor and palmar cutaneous branches of the median
nerve, determine how the tunnel is approached. Both structures vary
considerably in the paths they take; they are so unpredictable that
“blind” procedures, which are acceptable elsewhere, must be avoided.
The tunnel must be decompressed through a full incision and under
direct vision. The uses of the incision include the following:
-
Decompression of the median nerve7,8
-
Synovectomy of the flexor tendons of the wrist
-
Excision of tumors within the carpal tunnel
-
Repair of lacerations of nerves or tendons within the tunnel
-
Drainage of sepsis tracking up from the mid-palmar space
-
Open reduction and internal fixation of
certain fractures and dislocations of the distal radius and carpus,
including volar lip fractures of the radius
forearm on a hand table in the supinated position so that the palm
faces upward. Use an exsanguinating bandage (Fig. 5-13).
 |
|
Figure 5-13 Position of the patient for volar approaches to the wrist and hand.
|
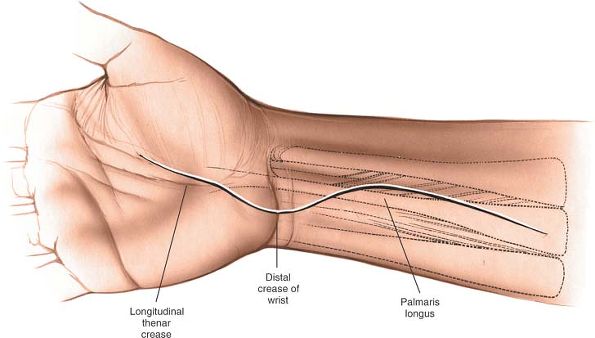
muscle bisects the anterior aspect of the wrist. Its distal end bisects
the anterior surface of the carpal tunnel. It is easy to palpate in the
distal forearm if the patient is instructed to pinch the fingers
together and flex the wrist.
crease, about one third of the way into the hand. Curve it proximally,
remaining just to the ulnar side of the thenar crease, until the
flexion crease of the wrist is almost reached: to avoid problems in
skin healing, do not wander into the thenar crease itself. Then, curve
the incision toward the ulnar side of the forearm so that the flexion
crease is not crossed transversely (Fig. 5-14).
 |
|
Figure 5-14
The incision for the volar approach to the wrist. The incision should be made on the ulnar side of the palmaris longus tendon to protect the palmar cutaneous branch of the median nerve. |
anatomic dissection in which the major nerves are identified, dissected
out, and preserved. No muscles are transected except, on occasion, some
fibers of the abductor pollicis brevis and palmaris brevis that cross
the midline.
palmar cutaneous branch of the median nerve, which usually presents on
the ulnar side of the flexor carpi radialis, has a variable course.
Dissection should be carried out meticulously, with particular
attention paid to the location of the nerve (see Fig. 5-14). After the fat is incised, the fibers of the superficial palmar fascia come into view; section them in line with the incision.
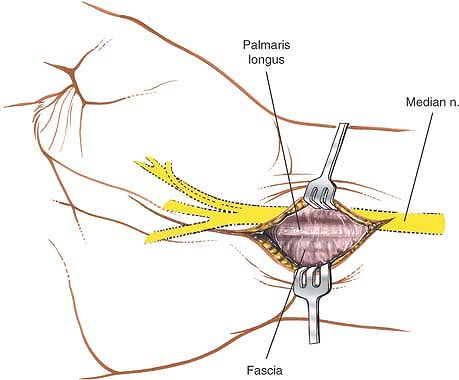
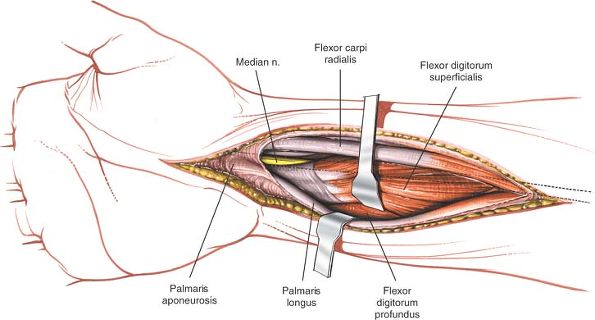
insertion of the palmaris longus muscle into the flexor retinaculum
(the transverse carpal ligament; Fig. 5-15).
Retract the tendon toward the ulna and identify the median nerve
between the tendons of the palmaris longus muscle and the flexor carpi
radialis muscle. The nerve lies closer to the palmaris longus than to
the flexor carpi radialis (Fig. 5-16).
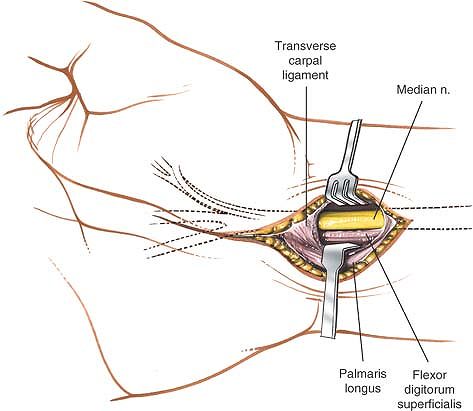
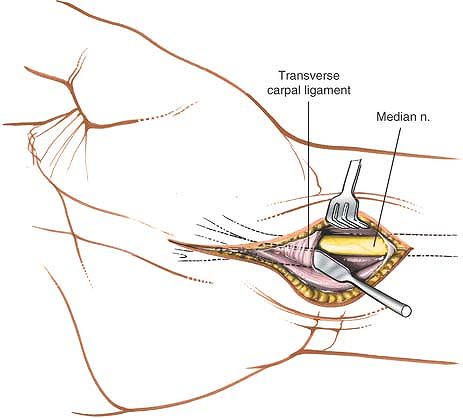
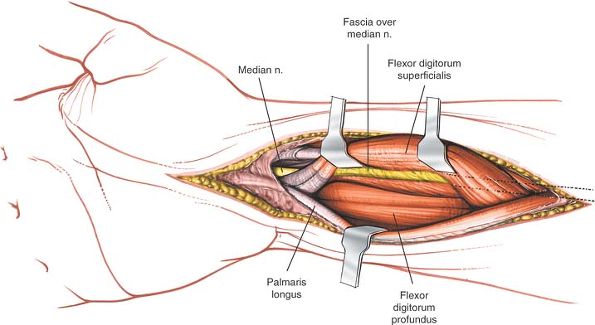
dissector) down the carpal tunnel between the flexor retinaculum and
the median nerve (Fig. 5-17). Carefully incise
the retinaculum, cutting down on the dissector to protect the nerve.
Make the incision on the ulnar side of the nerve to avoid possible
damage to its motor branch to the thenar muscle. Divide the entire
length of the retinaculum (Fig. 5-18).
 |
|
Figure 5-15 The skin is retracted, and the deep fascia and tendon of the palmaris longus are inspected.
|
 |
|
Figure 5-16
The deep fascia is incised. The palmaris longus is retracted toward the ulna, revealing the median nerve as it enters the carpal tunnel. |
 |
|
Figure 5-17 A spatula is placed under the transverse carpal ligament to protect the median nerve as the ligament is incised.
|
 |
|
Figure 5-18
The transverse carpal ligament is released on the ulnar side of the nerve to avoid damage to the motor branch of the thenar muscle. |
usually arises from the anterolateral side of the median nerve just as
the nerve emerges from the carpal tunnel. The motor branch then curves
radially and upward to enter the thenar musculature between the
abductor pollicis brevis and flexor pollicis brevis muscles. Sometimes,
however, the motor branch arises within the tunnel and pierces the
flexor retinaculum to reach the thenar musculature. In these rare
cases, the motor nerve itself may have to be decompressed before the
patient’s symptoms will be relieved fully (see Fig. 5-18).
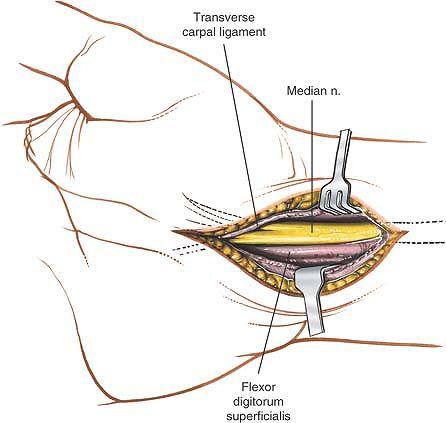
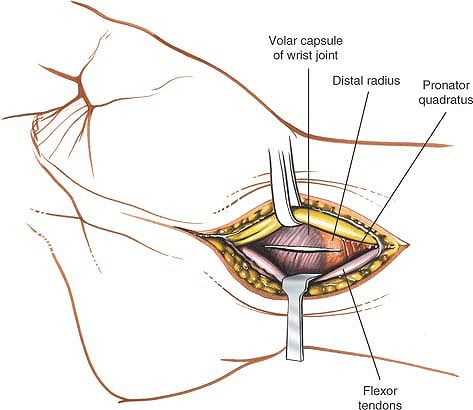
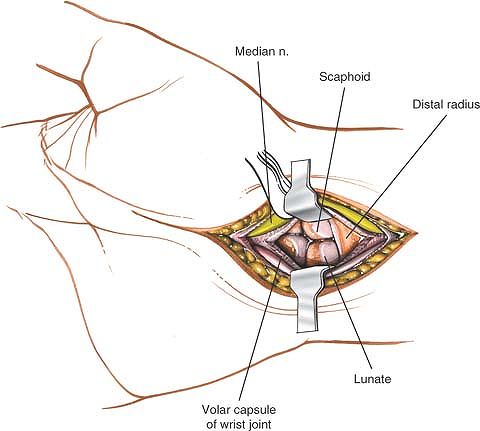
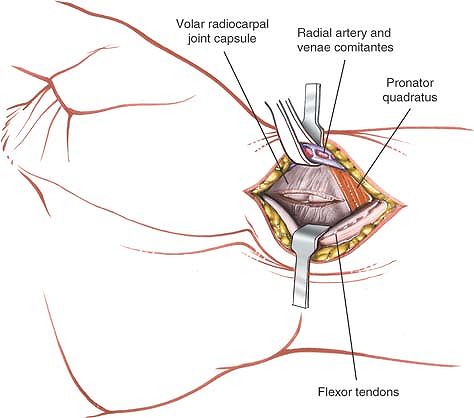
aspect of the wrist joint. If this is required, mobilize the median
nerve in the carpal tunnel and retract it radially to avoid stretching
its motor branch. Next, mobilize and retract the flexor tendons in the
carpal tunnel (Fig. 5-19). Incising the base of
the tunnel longitudinally exposes the volar aspect of the carpus.
Extending the incision proximally provides access to the volar aspect
of the wrist joint and the distal radius (Fig. 5-20).
The most convenient approach for access to the volar aspect of the
distal radius is the distal portion of the anterior approach to the
radius (see Chapter 4).
 |
|
Figure 5-19
The median nerve is retracted radially and the flexor tendons are retracted toward the ulna, revealing the distal radius and joint capsule. An incision then is made into the capsule to expose the carpus. |
arises 5 cm proximal to the wrist joint and runs down along the ulnar
side of the tendon of the flexor carpi radialis muscle before crossing
the flexor retinaculum. The greatest threat to this nerve occurs if the
skin incision is not angled to the ulnar side of the forearm (see Fig. 5-14).
to the thenar muscles exhibits considerable anatomic variation. The
risk to the nerve is minimized if the incision is made into the carpal
tunnel on the ulnar side of the median nerve (see Applied Surgical Anatomy of the Volar Aspect of the Wrist and Fig. 5-32).
crosses the palm at the level of the distal end of the outstretched
thumb. Blind slitting of the flexor retinaculum may damage this
arterial arcade if the instrument passes too far distally. The arch is
in no danger if the flexor retinaculum is cut carefully under direct
observation for its entire length (see Figs. 5-14 and 5-32).
Minimal access approaches to divide the flexor retinaculum rely on
arthroscopic visualization of the anatomical structures to ensure their
preservation.
 |
|
Figure 5-20 Incise the joint capsule to expose the carpus.
|
approach can be extended to expose the median nerve. To accomplish
this, extend the skin incision proximally, running it up the middle of
the anterior surface of the forearm (Fig. 5-21).
Incise the deep fascia of the forearm between the palmaris longus and
flexor carpi radialis muscles. Retract the flexor carpi radialis in a
radial direction and the palmaris longus in an ulnar direction,
exposing the muscle belly of the flexor digitorum superficialis muscle
in the distal two
thirds of the forearm (Fig. 5-22).
The median nerve adheres to the deep surface of the flexor digitorum
superficialis, held there by fascia. Thus, if the flexor digitorum
superficialis is reflected, the nerve goes with it (Fig. 5-23).
 |
|
Figure 5-21 Extend the wrist incision proximally to expose the distal forearm and median nerve.
|
 |
|
Figure 5-22
Incise the fascia on the forearm between the palmaris longus and the flexor carpi radialis to expose the tendons and muscles on the flexor digitorum superficialis. |
 |
|
Figure 5-23
Reflect the flexor digitorum superficialis and note that the median nerve moves with it, because it is attached to the muscle via the posterior fascia of the muscle. |
incision can be extended into a volar zigzag approach for any of the
fingers, providing complete exposure of all the palmar structures (see Volar Approach to the Flexor Tendons and Fig. 5-38).
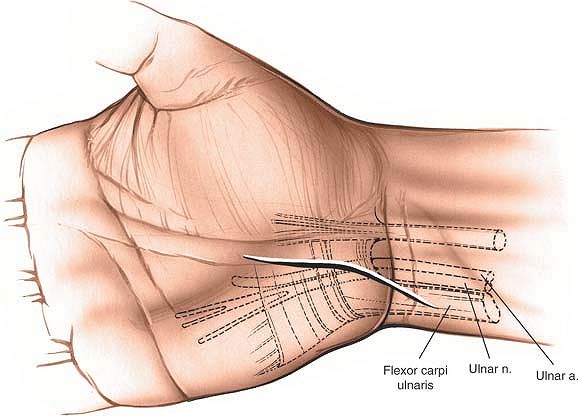
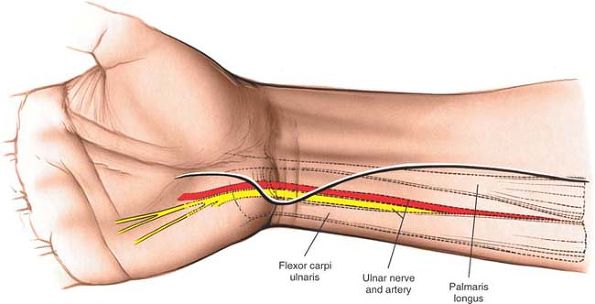
nerve at the wrist. It is used primarily to decompress the canal of
Guyon in cases of ulnar nerve compression. It also permits exploration
of the ulnar nerve in cases of trauma. The approach is freely extensile
proximally, allowing exposure of the nerve all the way up the forearm.
the hand on a hand table in the supinated position, so that the palm
faces upward. Use an exsanguinating soft bandage, then inflate a
tourniquet (see Fig. 5-13).
 |
|
Figure 5-24 Incision for the exposure of the ulnar nerve in the canal of Guyon.
|
the hypothenar eminence and crossing the wrist joint obliquely at about
60°. Extend the incision onto the volar aspect of the distal forearm.
The incision should be about 5 to 6 cm long (Fig. 5-24).
anatomic dissection in which the nerve and vessels are dissected out
and preserved.
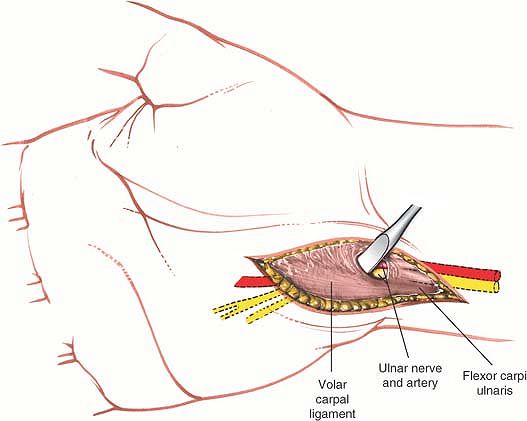
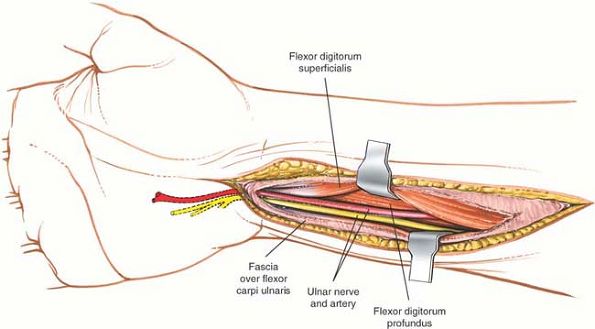
identify the tendon of the flexor carpi ulnaris in the proximal end of
the wound (Fig. 5-25). Mobilize the tendon by
incising the fascia on its radial border, and retract the muscle and
tendon in an ulnar direction to reveal the ulnar nerve and artery (Fig. 5-26).
 |
|
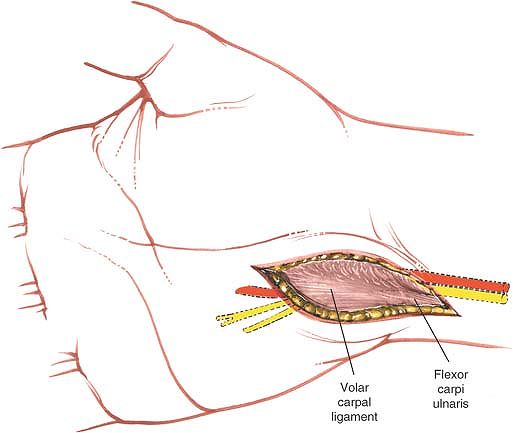
Figure 5-25 The volar carpal ligament is seen as a continuation of the deep palmar fascia and fibers of the flexor carpi ulnaris.
|
 |
|
Figure 5-26 The volar carpal ligament is isolated and the nerve is protected in preparation for sectioning of the volar carpal ligament.
|
 |
|
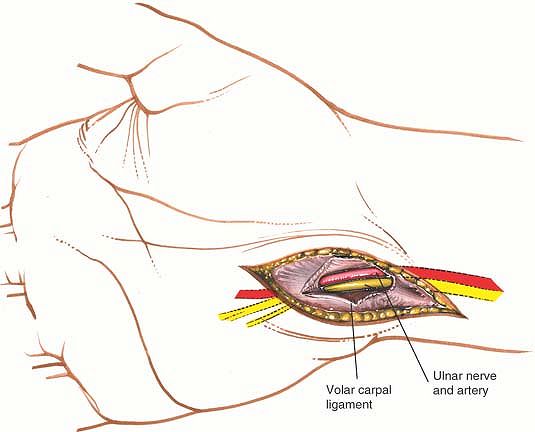
Figure 5-27 The roof of the canal has been incised, revealing the ulnar nerve and artery.
|
fibrous tissue, the volar carpal ligament. During this procedure, take
great care to protect the nerve and vessel. The ulnar nerve now is
exposed across the wrist joint; the canal of Guyon is decompressed (Fig. 5-27).
-
When the fascia on the radial side of the
flexor carpi ulnaris is incised to allow retraction of the muscle,
during superficial surgical dissection -
When the volar carpal ligament is incised, during deep surgical dissection
the skin incision proximally on the anterior aspect of the forearm,
running it longitudinally up the middle of the forearm (Fig. 5-28).
Incise the deep fascia in line with the incision and identify the
radial border of the flexor carpi ulnaris. Develop a plane between the
flexor carpi ulnaris muscle (which is supplied by the ulnar nerve) and
the flexor digitorum superficialis muscle (which is supplied by the
median nerve), retracting the flexor carpi ulnaris toward the ulna to
reveal the ulnar nerve. This incision can expose the ulnar nerve almost
to the level of the elbow joint (Fig. 5-29), where it passes between the two heads of the flexor carpi ulnaris muscle.
 |
|
Figure 5-28 Explore the ulnar nerve proximally in the forearm.
|
 |
|
Figure 5-29
Develop the plane between the flexor carpi ulnaris and the flexor digitorum superficialis. In the depth of the wound, the ulnar nerve is visualized running under the reflected head of the flexor carpi ulnaris. |
surface of the carpus. Its base is formed by the deeply concave surface
of the volar aspect of the carpal bones, and its roof is formed by the
flexor retinaculum (Fig. 5-30). The ulnar nerve
runs over the surface of the flexor retinaculum; it is enclosed in its
own fibro-osseous canal, the canal of Guyon (Fig. 5-31).
 |
|
Figure 5-30
Superficial anatomy of the wrist and palm. Note the course of the cutaneous branch of the median nerve. The longitudinal bands of the palmar aponeurosis are continuations of the palmaris longus tendon. |
-
The pisiform.
This is located on the ulnar border of the wrist. The pisiform is a
mobile sesamoid bone lying within the tendon of the flexor carpi
ulnaris muscle. The bone was sometimes used by artisans to tap nails
into soft wood or leather.
P.207P.208
Stress fractures have been noted in cobblers who use the pisiform for this purpose.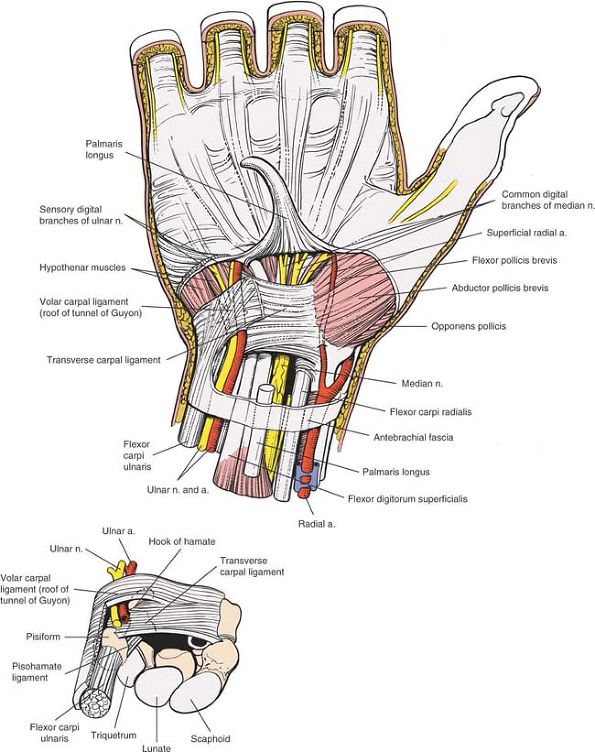 Figure 5-31
Figure 5-31
The palmar aponeurosis and fascia have been elevated to reveal the
transverse carpal ligament. The fascia of the forearm and the
expansions of the flexor carpi ulnaris (volar carpal ligament) are left
intact where they form the roof of the tunnel of Guyon. The canal of
Guyon looking from proximal to distal (inset).
The transverse carpal ligament forms the floor of the tunnel of Guyon;
the roof is formed by the volar carpal ligament, which is a
condensation of the fascia of the forearm and expansions of the flexor
carpi ulnaris tendon. The canal is formed medially by the pisiform bone
and laterally by the hook of the hamate bone. -
The hook of the hamate.
This is slightly distal and radial to the pisiform. To locate it, place
the interphalangeal joint of the thumb on the pisiform, pointing the
tip toward the web space between the thumb and index finger, and rest
the tip of the thumb on the palm. The hook of the hamate lies directly
under the thumb. Because it is buried under layers of soft tissue, one
must press firmly to find its rather shallow contours. The deep branch
of the ulnar nerve lies on the hook, and neurapraxia of the nerve has
been described in cases of fracture. -
The ridge of the trapezium.
The trapezium lies on the radial side of the carpus, where it
articulates with the first metacarpal. To palpate the ridge, identify
the joint between the trapezium and the thumb’s metacarpal bone by
moving the joint passively. The ridge feels like a prominent lump on
the volar aspect of the trapezium (see Fig. 5-36A). -
The tubercle of the scaphoid.
This small protuberance is barely palpable just distal to the distal
end of the radius on the volar aspect of the wrist joint (see Figs. 5-35 and 5-36A).
the groove on the trapezium, converting the groove into a tunnel
through which the tendon of the flexor carpi radialis muscle runs
before it attaches to the base of the second and third metacarpals (see
Figs. 5-35 and 5-36A).
-
Tendon of the palmaris longus.
The palmaris longus is a vestigial muscle of no functional importance.
Its tendon is used frequently for tendon grafting. It is important to
test for the presence of this tendon before surgery, because it is
absent in about 10% of the population. The tendon also is used as an
anatomic landmark for the injection of steroid into the carpal tunnel.
If the patient is asked to flex the wrist against resistance, the
tendon of the palmaris longus (if it is present) is easily palpable
together with the thicker and more radially located tendon of the
flexor carpi radialis. The easily defined gap between the two tendons
is the site where the needle should be inserted for injection of the
carpal tunnel. The needle should be inserted here dorsally and distally
at an angle of almost 45°. Note also that because the carpal tunnel is
a distensible space, if problems are encountered in injecting it, then
the tip of the needle either is still in the flexor retinaculum or is
imbedded in one of the tendons in the tunnel. Correctly positioned
syringes should enter the space without encountering much resistance to
pressure. -
Palmar cutaneous branch of the median nerve. The course of the palmar cutaneous branch of the median nerve may vary in four important ways (see Fig. 5-30):
-
Normally, the nerve branches off 5 cm
proximal to the wrist. It runs along the ulnar side of the tendon of
the flexor carpi radialis before crossing the flexor retinaculum. On
rare occasions, the nerve actually may be enclosed by parts of the
flexor retinaculum and, thus, may run in a tunnel of its own on the
wrist.The nerve divides into two major branches, medial and
lateral, while crossing the flexor retinaculum. The lateral is the
larger branch. Both supply the skin of the thenar eminence. -
Less often, the nerve arises from the median nerve in two distinct branches, which travel separately across the wrist.9
-
The palmar cutaneous branch may arise within the carpal tunnel and penetrate the flexor retinaculum to supply the skin of the thenar eminence.
-
The palmar cutaneous branch may be
absent, replaced by a branch derived from the radial nerve, the
musculocutaneous nerve, or the ulnar nerve.9The skin incision described above avoids cutting the
nerve by angling across the distal forearm in an ulnar direction. One
must be aware, however, that considerable variability exists in the
course of the nerve. Because damage can result in the formation of a
painful neuroma, transverse incisions on the volar aspect of the distal
forearm must be avoided. (Compression lesions of the nerve have been
reported, but these are rare.)10,11
-
-
Ulnar nerve. The ulnar nerve runs down the volar surface of the distal forearm under cover of the flexor carpi ulnaris muscle (see Fig. 5-31).
The ulnar artery lies on its radial side. The tendon of the flexor
carpi ulnaris inserts into the pisiform, which then joins with the
hamate and fifth metacarpal via ligaments. Just proximal to the wrist,
the artery and nerve emerge from under the muscle to pass over the
flexor retinaculum (the transverse carpal ligament) of the wrist (see Fig. 5-31).
the nerve, and, finally, the tendon of the flexor carpi ulnaris (see Fig. 5-31).
damage by lacerations. The grim triad of lacerations of the tendon of
the flexor carpi ulnaris, the ulnar artery, and the ulnar nerve is a
common sequela of falling through a window with the ulnar border of the
wrist flung forward to protect the face.
covered with a tough fibrous tissue that is continuous with the deep
fascia of the forearm, the volar carpal ligament. The tunnel thus
formed, the canal of Guyon, has four boundaries: a floor, the flexor
retinaculum (transverse carpal ligament); a medial wall, the pisiform;
a lateral wall, the hamate; and a roof, the volar carpal ligament
(distal fascia of the forearm; see Fig. 5-31).
 |
|
Figure 5-32
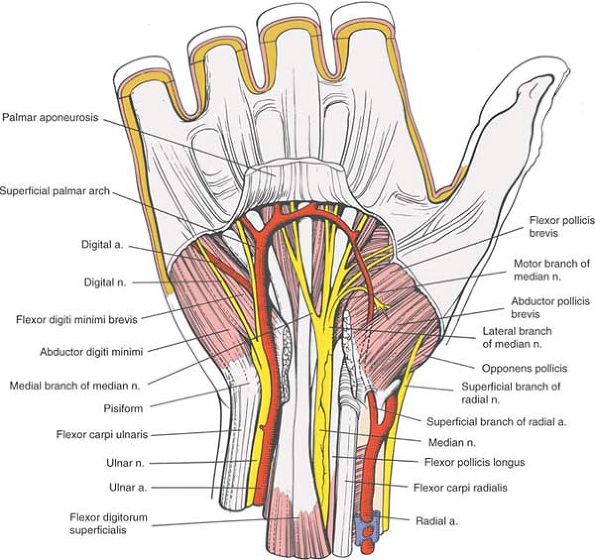
The palmar aponeurosis has been resected further distally to expose the superficial palmar arterial arch. The transverse carpal ligament also has been resected. The median nerve lies superficial to the tendons of the profundus, but at the same level with the superficialis muscle tendons. Note the motor branch of the median nerve to the thenar muscles. The location of its division from the median nerve is quite variable. |
branches. The superficial branch supplies the palmaris brevis muscle
and the skin of the small finger and ulnar half of the ring finger. The
deep branch supplies all the small intrinsic muscles of the hand,
except those of the thenar eminence and the radial two lumbricals (see Figs. 5-32, 5-33, 5-34 and 5-35).
 |
|
Figure 5-33
The palmar aponeurosis has been elevated up to its attachment to the digital flexor sheaths. Its deeper attachments to the carpal plate and bone have been cut. The flexor tendons and digital nerves are shown in continuity, as are the superficial palmar arch and the thenar and hyperthenar muscles. Note that the digital nerves and vessels go deep or dorsal to the natatory ligaments. Flexor Pollicis Brevis. Origin. Flexor retinaculum. Insertion. Radial border of proximal phalanx of thumb. Action. Flexor of metacarpophalangeal joint of thumb. Nerve supply. Median nerve (motor or recurrent branch).
Abductor Pollicis Brevis. Origin. Flexor retinaculum and tubercle of scaphoid. Insertion. Radial side of base of proximal phalanx of thumb. Action. Abduction of thumb at metacarpophalangeal joint and rotation of proximal phalanx of thumb. Nerve supply. Median nerve (motor or recurrent branch).
|
 |
|
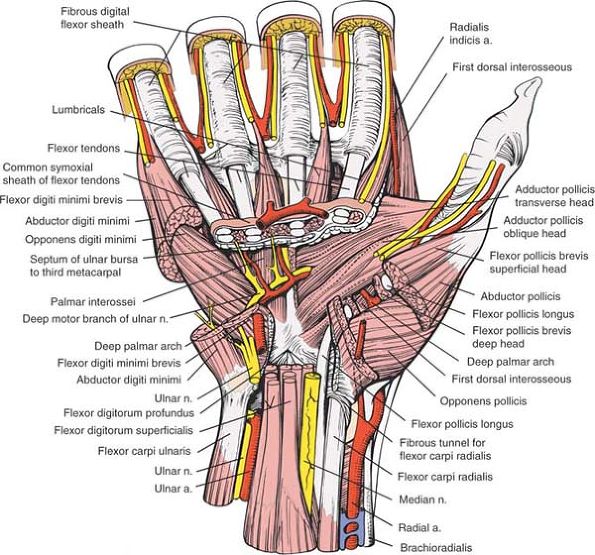
Figure 5-34
Portions of the thenar and hypothenar muscles have been resected to reveal their layering. The ulnar nerve passes between the origin of the abductor digiti minimi and the flexor digiti minimi. In the thenar region, the course of the flexor pollicis longus is seen as it crosses between the two heads of the flexor pollicis brevis. Portions of the long flexors of the fingers have been resected to show their layering. The superficial palmar arch runs superficial to the tendons, whereas the deep palmar arch is immediately deep to the tendons. Note that potential spaces develop on the undersurface of the flexor tendons and their sheaths, and on the deep intrinsic muscles of the hand, the interosseous on the hyperthenar side and the adductor pollicis on the thenar side. A septum that runs from the undersurface of the flexor tendons to the third metacarpal divides the two spaces. More distally, the superficial transverse ligament has been resected, revealing the course of the lumbricals and the digital vessels that run superficial or palmar to the deep transverse metacarpal ligaments. Adductor Pollicis. Origin.
Oblique head from bases of second and third metacarpals, trapezoid, and capitate. Transverse head from palmar border of third metacarpal. Insertion. Ulnar side of base of proximal phalanx of thumb via ulnar sesamoid. Action. Adduction of thumb. Opposition of thumb. Nerve supply. Deep branch of ulnar nerve. Opponens Pollicis. Origin. Flexor retinaculum. Insertion. Radial border of thumb metacarpal. Action. Opposition of metacarpal bone of thumb. Nerve supply. Median nerve (motor or recurrent branch).
|
 |
|
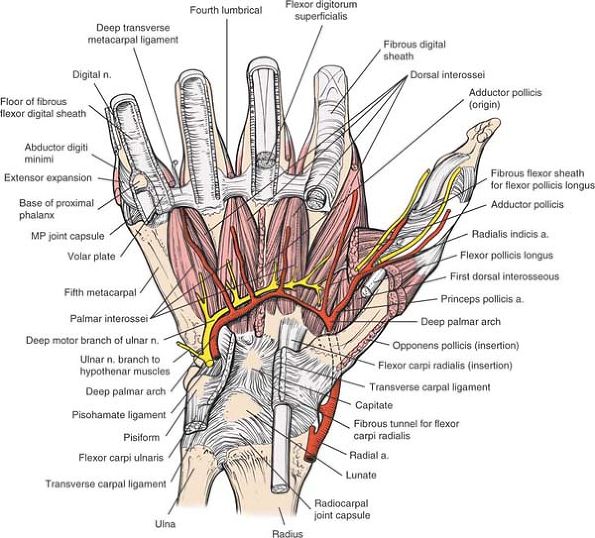
Figure 5-35
The deepest layer of the palm is revealed. The deep palmar arterial arch lies deep to the long flexor tendon and superficial to the interosseous muscles. It crosses the palm with the deep branch (motor branch) of the ulnar nerve. The nerve supplies all the interosseous muscles. More distal, the interosseous muscles are seen running deep (dorsal) to the deep transverse ligament. The deep transverse metacarpal ligaments attach to the palmar plate, which is seen on the fifth metacarpal. The pulleys of the thumb are seen in relationship to the digital nerves. |
forearm deep to the flexor digitorum superficialis muscle. Just above
the wrist, it becomes superficial and lies between the tendons of the
palmaris longus and flexor carpi radialis muscles. It enters the palm
by traversing the carpal tunnel (see Fig. 5-31).
pollicis longus muscles. The superficialis tendons lie toward the ulnar
side of the nerve. At the distal border of the flexor retinaculum, the
nerve divides into two branches (see Figs. 5-32 and 5-33).
-
The medial branch
sends cutaneous branches to the adjacent sides of the ring and middle
fingers, and to the adjacent sides of the middle and index fingers. -
The lateral branch
sends cutaneous branches to the radial side of the index finger and to
both sides of the thumb. The lateral branch usually also sends off the
motor, or recurrent, nerve (see Fig. 5-32), which is the key surgical landmark and major surgical danger in carpal tunnel decompression.
-
The classic course (seen in 50% of
patients). The branch arises from the volar radial aspect of the median
nerve distal to the radial end of the carpal tunnel. The nerve hooks
radially and upward to enter the thenar muscle group between the flexor
pollicis brevis and abductor pollicis brevis muscles.The position of the motor branch can be estimated by
drawing one vertical line from the web space between the middle and
index fingers, drawing another from the radial origin of the first web
space, then connecting to the hook of the hamate (Kaplan’s cardinal
line). The intersection of these two lines marks the origin of the
motor branch (see Fig. 5-36B).12 -
A variation that occurs in about 30% of
patients. The branch arises from the anterior surface of the nerve
within the carpal tunnel. It passes through the tunnel with its parent
nerve and hooks around the distal end of the flexor retinaculum to
enter the thenar group between the flexor pollicis brevis and abductor
pollicis brevis muscles. -
A variation that occurs in about 20% of
patients. The branch arises from the anterior surface of the nerve
within the carpal tunnel. It travels radially to pierce the flexor
retinaculum and enter the thenar group of muscles between the abductor
pollicis brevis and flexor pollicis brevis muscles.13 -
A rare variation. The branch arises from the ulnar side of the median nerve.14
It crosses the median nerve within the tunnel, then hooks around the
distal end of the flexor retinaculum to enter the thenar muscle group.
It also may pass through the flexor retinaculum and lie anterior to it.15 -
Another rare variation. The nerve arises
from the anterior surface of the median nerve within the carpal tunnel.
At the distal end of the flexor retinaculum, the branch hooks radially
over the top of the retinaculum. The nerve crosses the distal part of
the retinaculum almost transversely before entering the thenar group of
muscles. -
A very rare variation (multiple motor branches).16 Double nerves may follow any of the courses described above.
-
A third rare variation (high division of the median nerve).17
The nerve may divide into medial and lateral branches high up in the
forearm. The thenar branch, originating from the lateral branch, may
leave the carpal tunnel either in the conventional manner or by
piercing the flexor retinaculum on its radial side.
is exposed. If the tunnel is opened on the ulnar side of the nerve, the
motor branch will be preserved unless it lies on the same side.
Patients with exceptionally rare variations usually have large palmaris
brevis muscles, which should alert the surgeon to the possibility
during the approach.10
ring fingers are superficial to the tendons of the index and little
fingers. This arrangement dictates correct repair in cases of multiple
tendon laceration (see Fig. 5-31).
to the tendons of the flexor digitorum superficialis. The tendon to the
index finger is separate; the other three still may be attached
partially to each other as they pass through the carpal tunnel (see Fig. 5-31).
that of the flexor carpi radialis and is found on the most radial
aspect of the canal at the same depth as the profundus tendons (see Figs. 5-31 and 5-34).
retinaculum to lie in the groove of the trapezium before it inserts
into the bases of the second and third metacarpals. It does not pass
through the carpal tunnel (see Fig. 5-35).
 |
|
Figure 5-36 (A)
The bones of the wrist and palm and the proximal metacarpals are seen in relationship to the creases of the wrist. The necks of the metacarpals are at the level of the distal palmar crease. The distal wrist crease runs from the proximal portion of the pisiform to the proximal portion of the tubercle of the scaphoid and marks the proximal level of volar carpal ligament. The proximal transverse palmar crease is at the radiocarpal joint. (B) Kaplan’s cardinal line. Used to locate the motor branch of the median nerve to the thenar muscles. |
It also provides excellent exposure of both neurovascular bundles in
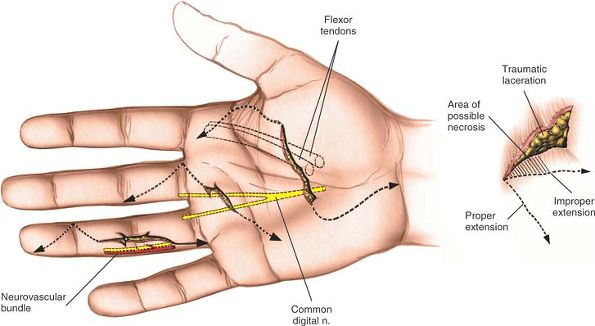
the finger. The skin incision can be extended into the palm, the volar
surface of the wrist, and the anterior surface of the forearm, making
it a suitable approach in cases of trauma, where many levels may have
to be exposed. Its other major advantage is that many skin lacerations
can be incorporated into the skin incision. Its uses include the
following:
-
Exploration and repair of flexor tendons
-
Exploration and repair of digital nerves and vessels
-
Exposure of the fibrous flexor sheath for drainage of pus
-
Excision of tumors within the fibrous flexor sheath
-
Excision of palmar fascia in Dupuytren’s contracture
arm abducted and lying on an arm board. Adjust the height of the table
to make sitting comfortable. Most right-handed surgeons prefer to sit
on the ulnar side of the affected arm. An exsanguinating bandage and
tourniquet, as well as good lighting, are essential (see Fig. 5-13).
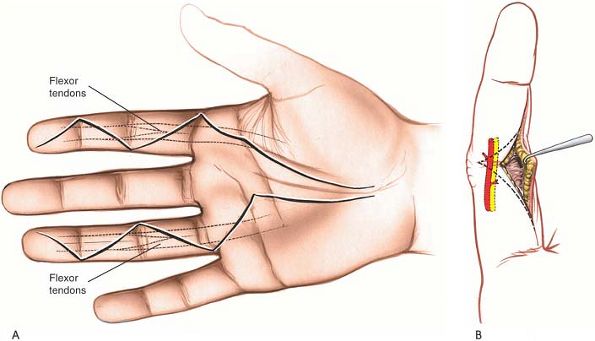
well distal to the metacarpophalangeal joint. The course of the volar
zigzag incision takes these creases into account, running diagonally
across the finger between creases (Fig. 5-37).
 |
|
Figure 5-37 The relationship of the skin creases to the tendons and joints of the wrist and hand is seen.
|
methylene blue to outline the proposed site. The angles of the zigzag
should be about 90° to each other (or to the transverse skin crease);
angles considerably less than 90° to each other may lead to necrosis of
the corners (Fig. 5-38A).
The angles should not be placed too far in a dorsal direction;
otherwise, the neuromuscular bundle may be damaged when the skin flaps
are mobilized (see Fig. 5-38B). Of course, the basic zigzag pattern should be modified to accommodate any preexisting lacerations (Fig. 5-39).
 |
|
Figure 5-38 (A) Basic zigzag incision for exposure of the flexor tendons of the palm and fingers. (B) If an incision is placed too far laterally or medially, the neurovascular bundle may be damaged.
|
 |
|
Figure 5-39
The basic zigzag pattern should be adapted to preexisting lacerations for exploration of the underlying structures. When adapting the skin incisions to previously existing lacerations, attempt to maintain an angle of about 90° to prevent necrosis of the corners of the incision (inset). |
site of the incision is innervated by nerves coming from either side of
the incision, so no areas of anesthesia are created.
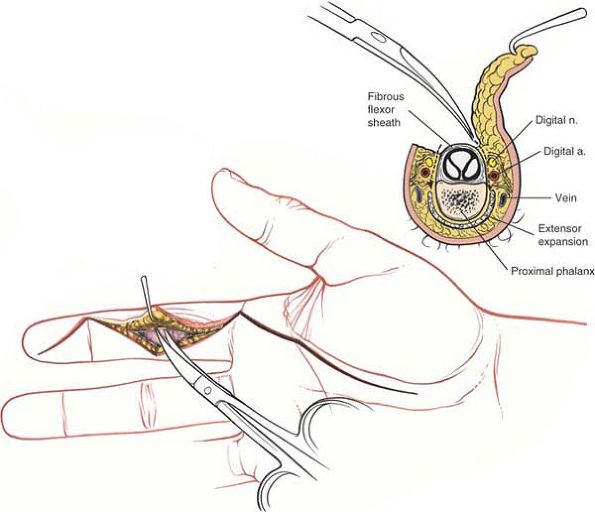
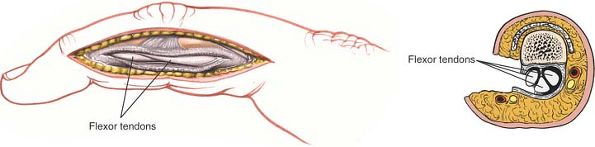
starting at the apex. Elevate the flaps along with some underlying fat.
Do not mobilize the flaps widely until the level of the flexor sheath
is reached, to ensure thick flaps and reduce the risk of skin flap
necrosis (Fig. 5-40).
 |
|
Figure 5-40
Elevate thick skin flaps. Stay as close to the sheath as possible to prevent damage to the laterally placed neurovascular structures. |
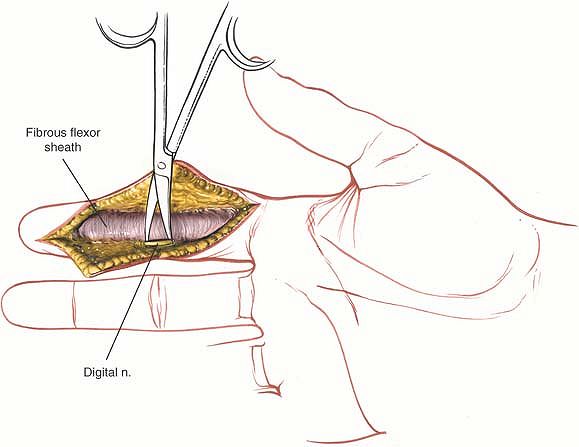
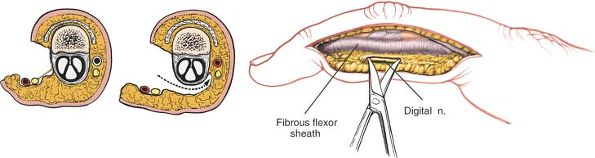
the subcutaneous tissues at the lateral border of the fibrous flexor
sheath. The neurovascular bundle is separated from the volar
subcutaneous flap by a thin layer of fibrous tissue known as Grayson’s
ligament. This layer must be opened for full exposure of the
neurovascular bundle. The easiest way to pry the tissues apart is to
open gently a small pair of closed scissors so that the blades separate
the tissues in a longitudinal plane. The blades actually are working
along the line of the digital nerve, maximizing exposure of the nerve
while minimizing the
chance of accidental laceration (Fig. 5-42; see Fig. 5-40).
 |
|
Figure 5-41
Expose the flexor tendons in a longitudinal fashion. The digital nerves lie lateral to the tendons. Maintain the A2 and A4 pulleys. |
 |
|
Figure 5-42 Identify the neurovascular bundles and preserve them.
|
the fibrous flexor sheath and the digital nerves and vessels. (In
practice, it seldom is necessary to go this deep; surgery on the
osseous structures usually is safer through a midlateral or dorsal
incision [Fig. 5-43].)
 |
|
Figure 5-43 (A)
Incision for the midlateral approach to the finger. The incision lies between the proper digital nerve, which runs toward the palm, and its dorsal branch. The incision also can be made with the finger flexed; connect the dorsal portions of the interphalangeal creases (inset). (B) Lateral view of the anatomy of the finger. Note the division of the proper (common) digital nerve into dorsal and palmar branches, the relationship of the palmar division of the nerve to the flexor tendon sheath, and the insertion of the lumbrical and interossei muscles into the hood mechanism. |
tendons, and incising the periosteum from the volar surface of the bone
lead to adhesions within the fibrous flexor sheath. It is very
important to note that the consequences of this will be the loss of
full function of the finger. Therefore, every effort should be made to
avoid this at all costs.
at too acute an angle, and skin sutures should be meticulous to ensure
closure. Skin flaps should be thick enough to avoid skin necrosis (see Fig. 5-39). The tourniquet should be removed and hemostasis secured before closure is undertaken.
eventually joining the curved incision parallel to the thenar crease
that is used for exposure of the structures of the palm, volar surface
of the wrist, and anterior surface of the forearm. The key to making
these incisions is to avoid crossing flexion creases at 90°, thus
preventing the development of flexion contractures, and to leave skin
flaps with substantial corners (see Fig. 5-39).
flexor tendons and digital nerves in the fingers. It affords access to
the neurovascular bundle on the incised side of the finger; at the same
time, it is difficult to extend into the palm. Its uses include the
following:
-
Open reduction and stabilization of phalangeal fractures
-
Exposure of the fibrous flexor sheath and its contents
-
Exposure of the neurovascular bundle
the arm stretched out on an arm board. Good lighting and a good
exsanguinating bandage and tourniquet are essential (see Fig. 5-13).
are the key to this skin incision. They extend around the medial and
lateral surfaces of the fingers and end slightly nearer the dorsal than
the volar surface of the finger.
or if it is struck in full extension. If so, the surgical landmark for
the skin incision is the junction between the wrinkled dorsal and the
smooth volar skin on the side of the finger (see Fig. 5-43).
the finger, starting at the most dorsal point of the proximal finger
crease. Continue cutting distally to the distal interphalangeal joint,
passing just dorsal to the dorsal end of the flexor skin crease. Extend
the incision farther distally toward the lateral end of the fingernail.
The incision actually is dorsolateral rather than truly lateral (see Fig. 5-43). Alternatively, flex the finger and make an incision connecting dorsal end points of the interphalangeal crease.
intermuscular interval is developed. The nerve supply to the finger
comes mainly from two sources, the dorsal digital nerves and the volar,
or palmar, digital nerves. Because the skin incision marks the division
between these two supplies, it causes no significant areas of
hypoesthesia.
flap in line with the skin incision. The fat over the proximal
interphalangeal joint is quite thin; take care not to incise the joint
itself. Continue the dissection toward the midline of the finger,
angling slightly in a volar direction. The main neuromuscular bundles
lie in the volar flap (Fig. 5-44).
 |
|
Figure 5-44 Develop the skin flap down to the flexor sheath, maintaining the neurovascular bundle in the volar flap.
|
 |
|
Figure 5-45 Incise the flexor sheath longitudinally to reveal the tendons.
|
 |
|
Figure 5-46
By longitudinal dissection, the neurovascular structures are revealed within the volar flap. Careful dissection of the flexor sheath can expose the entire palmar aspect of the bundle. |
in danger if the skin incision and approach drift too far in a volar
direction. This approach always should begin just dorsal to the end of
the interphalangeal creases. If the approach does begin at this site,
the danger to the palmar digital nerve will be diminished (see Fig. 5-43A).
expose the neurovascular bundle on the opposite side. Note that the
exposure gained is not as good as that offered by a zigzag volar
approach.
key to the treatment and prognosis of flexor tendon injuries. Nowhere
else in the body are the links between anatomy, pathology, and
treatment illustrated so clearly. The structure of the tendons, their
blood supply, and their special relationship to other structures all
relate to the pathogenesis of injury and repair.
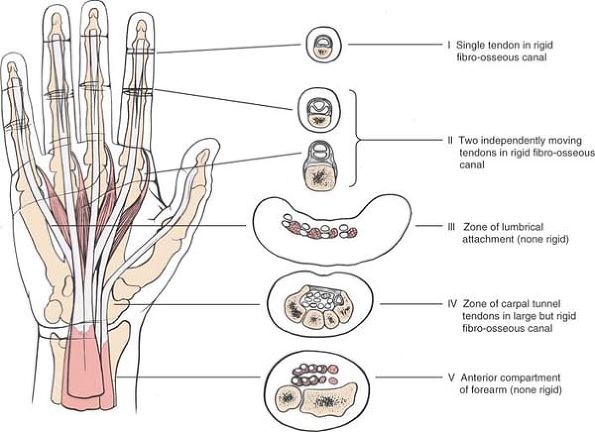
five zones, each of which is separated from the others by anatomic
landmarks. The zones all must be treated differently in cases of tendon
laceration. We shall consider the anatomy from the proximal to the
distal aspect, from zone 5 to zone 1, as devised by Milford (Fig. 5-47).19
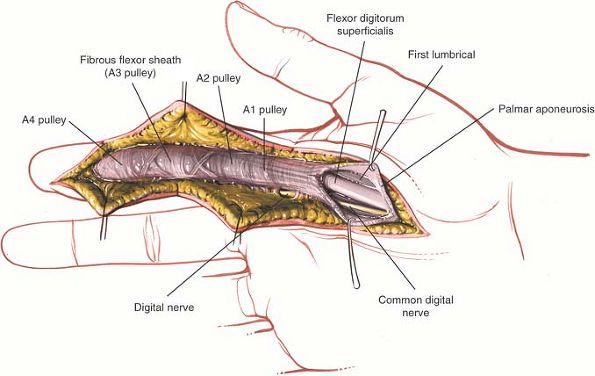
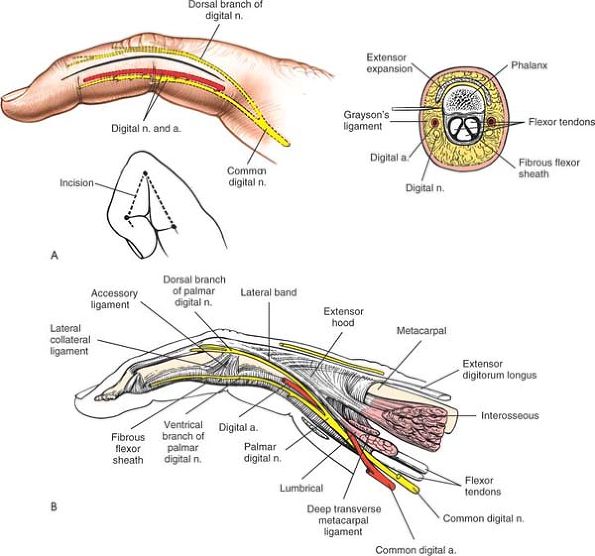
At that point, nine distinct tendons run into the hand toward the
digits. Each finger has two tendons, one each from the flexor digitorum
superficialis muscle and the flexor digitorum profundus muscle. The
thumb has one long flexor, the flexor pollicis longus.
but are surrounded by a synovial sheath in the distal part of the
forearm. Tendon repairs carried out in this area generally are
successful, and independent finger flexion usually returns.
carpal tunnel. All the tendons remain in a common synovial sheath
throughout the carpal tunnel.
prognosis, but not as good as the prognosis of those carried out in
zone 5, because the tendons are enclosed in a fibro-osseous tunnel. The
tunnel must be opened for repairs, and adhesions may form after surgery.
flexor digitorum profundus tendons traverse the palm, a lumbrical
muscle arises from each tendon. The radial two lumbricals arise from a
single head, from the radial side of the profundus tendons to the index
and middle fingers. The ulnar two lumbricals arise from two heads, from
the adjacent sides of the profundus tendons between which they lie. The
tendons of the lumbricals pass along the radial sides of the
metacarpophalangeal joints before they insert into the dorsal
expansion. They pass volar to the axes of the metacarpophalangeal
joints; thus, they act as flexors of those joints, even as they extend
the interphalangeal joints (see Fig. 5-34).
to the lumbrical muscles. Most surgeons do not recommend repairing the
lumbricals; the increased tension on the muscles caused by the repair
produces fixed flexion at the metacarpophalangeal joints and limited
flexion at the interphalangeal joints, resulting in an intrinsic plus
hand.
tendons for each finger run together in a common fibro-osseous sheath.
 |
|
Figure 5-47 The five zones of the wrist and hand (according to Milford).
|
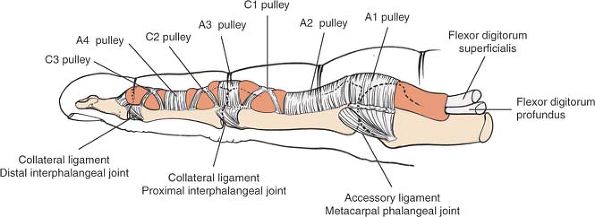
(the distal palmar crease) to the distal phalanges. They are attached
to the underlying bone and prevent the tendons from bowstringing.
They act as pulleys, directing the sliding movement of the tendons.
There are two types: annular and cruciate. Annular pulleys are composed
of a single fibrous band (ring); cruciate pulleys have two crossing
fibrous strands (cross). Annular pulleys act much like the rings on a
fishing rod. Without the ring, the fishing line would pull away from
the rod as it bends. This effect is known as bow-stringing; in human
terms, it results in the loss of range of movement and power in the
affected finger. Annular pulleys include the following:
-
The A1 pulley, which overlies the metacarpophalangeal joint. It is incised during trigger finger release.
-
The A2 pulley, which overlies the
proximal end of the proximal phalanx. It must be preserved (if at all
possible) to prevent bowstringing. -
The A3 pulley, which lies over the proximal interphalangeal joint.
-
The A4 pulley, which is located about the middle of the middle phalanx. It must be preserved to prevent bowstringing.
-
The C1 pulley, which is located over the middle of the proximal phalanx
-
The C2 pulley, which is located over the proximal end of the middle phalanx
-
The C3 pulley, which is located over the distal end of the middle phalanx
superficialis tendon on top of the profundus tendon. Over the proximal
phalanx, the superficialis
tendon
divides into halves, which spiral around the profundus tendon, meeting
on its deep surface and forming a partial decussation (chiasma). The
two then run as one tendon underneath the profundus tendon before
attaching to the base of the middle phalanx. Thus, the superficialis
tendon actually provides part of the bed on which the profundus tendon
runs. Distal to the attachment of the superficialis tendon, the
profundus tendon inserts into the base of the terminal phalanx (see Fig. 5-64).
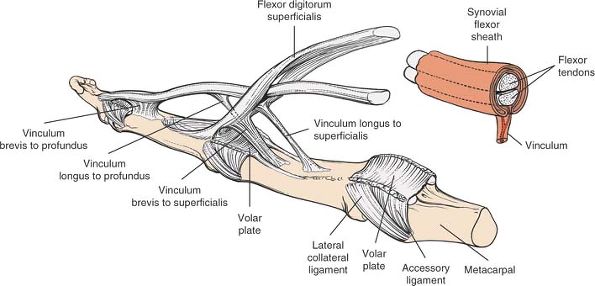
Within the fibro-osseous sheath, the nutrition of the flexor tendons is
provided for by blood vessels that enter the tendons from synovial
folds called vincula (Fig. 5-49).
 |
|
Figure 5-48
The annular and cruciate ligaments of the flexor tendon sheath, lateral view. Note the relationship of the pulleys to the skin creases and joint lines. |
 |
|
Figure 5-49
The vincula longa and brevia are main blood supplies to the flexor tendons. Note the relationship of the vincula to the flexor tendon synovial sheath (inset). |
after lacerations in zone 2, mainly because the flexor tendons are
enclosed within a nondistensible fibro-osseous canal, and also because,
for full function, the tendons must run over each other. It is
important to remember that any adhesion between the two can cause
malfunction of the involved finger.
superficialis tendon. Although the profundus tendon still is enclosed
tightly within a fibro-osseous sheath here, it runs alone. Therefore,
the prognosis for the repair of lacerations in this zone is better than
that for zone 2, although not as good as that for zones 3, 4, and 5.
Each tendon receives its blood supply from arteries that arise from the
palmar surface of the phalanges. These vessels are encased in the
vinculum (mesotenon). Two vincula supply each tendon, as follows:
-
Profundus tendon.
-
The short vinculum runs to the tendon close to its insertion onto the distal phalanx.
-
The long vinculum passes to the tendon from between the halves of the superficialis tendon at the level of the proximal phalanx.
-
-
Superficialis tendon.
-
The short vinculum runs to the tendon near its attachment onto the middle phalanx.
-
The long vinculum is a double vinculum, passing to each half of the tendon from the palmar surface of the proximal phalanx.
-
that this classic arrangement does not always hold true. The long
vincula to both tendons may be absent in the long or ring fingers. When
they are present, the long vinculum to the superficialis tendon may
attach to either or both of its slips, and the long vinculum to the
profundus tendon may arise at the level of the insertion of the
superficialis tendon.22
tendons are explored within their sheaths. The vincula should be
preserved, if possible, to preserve the blood supply to the tendon.
aspects of the flexor tendons are largely avascular; their nutrition
may be derived from synovial fluid. Therefore, sutures placed in the
volar aspects of the tendons do not interfere materially with the blood
supply to the tendons themselves.23
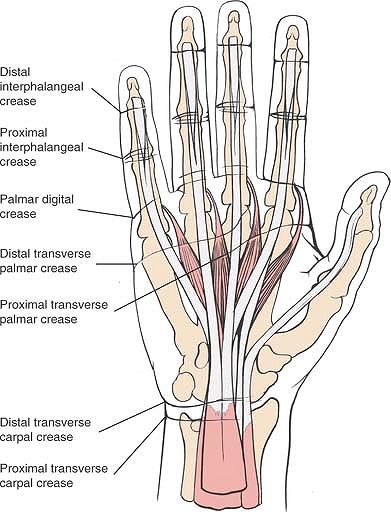
creases, all of which are situated where the fascia attaches to the
skin. There are four major creases: the distal palmar crease
corresponds roughly to the palmar location of the metacarpophalangeal
joints and the location of the proximal (A1) pulley, the palmar digital
crease marks the palmar location of the A2 pulley, the proximal
interphalangeal crease marks the proximal interphalangeal joint, and
the thenar crease outlines the thenar eminence (see Figs. 5-37, 5-47, and 5-48).
two sources: the volar aspect is supplied by the volar digital nerves,
and the dorsal aspect is innervated by the dorsal nerves of the radial
and ulnar nerves, as well as by the dorsal contribution from the volar
digital nerves for the distal 1½ phalanges of the index, long, and ring
fingers. The dorsa of the thumb and small finger are served exclusively
by the radial and ulnar nerves, respectively. Because of this anatomic
arrangement, the midlateral approach to the flexor sheath does not
cause skin denervation (see Fig. 5-43).
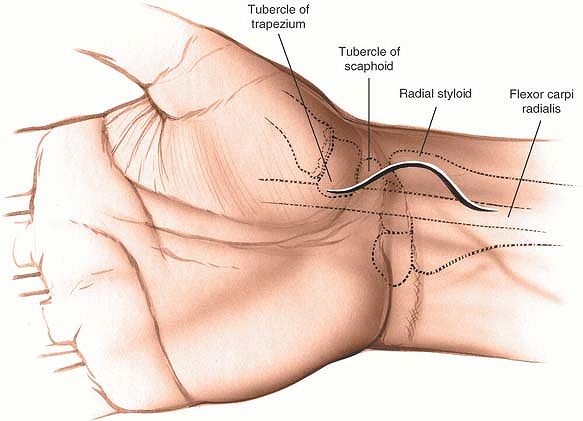
It also avoids damaging the dorsal blood supply to the bone’s proximal
half, as well as the superficial branch of the radial nerve. It does
pose a threat to the radial artery, however, which is close to the
operative field. It leaves a more cosmetic scar than does the dorsal
approach, and its uses include the following:
-
Bone grafting for nonunion of the scaphoid
-
Excision of the proximal third of the scaphoid
-
Excision of the radial styloid, either alone or combined with one of the above procedures
-
Open reduction and internal fixation of
fractures of the scaphoid. In such cases this approach frequently is
combined with the dorsolateral approach to the scaphoid.
muscle lies radial to the palmaris longus muscle at the level of the
wrist. It crosses the scaphoid before inserting into the base of the
second and third metacarpal just on the ulnar side of the radial pulse.
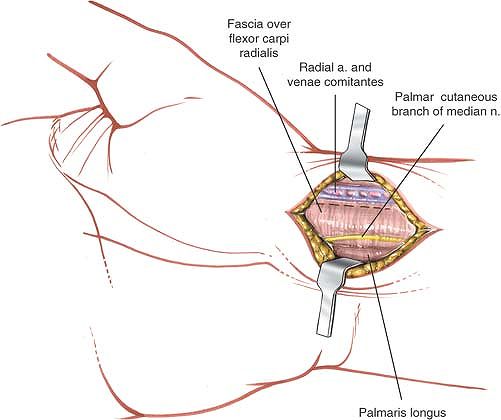
aspect of the wrist, about 2 to 3 cm long. Base it on the tuberosity of
the scaphoid and extend it proximally between the tendon of the flexor
carpi radialis muscle and the radial artery (Fig. 5-50).
 |
|
Figure 5-50
Incision for the volar approach to the scaphoid. Base the incision on the tuberosity of the scaphoid and extend it proximally and distally. The proximal extension is between the tendon of the flexor carpi radialis and the radial artery. |
mobilized is the flexor carpi radialis (which is supplied by the median
nerve).
Retract the radial artery and lateral skin flap to the lateral side.
Identify the tendon of the flexor carpi radialis muscle and trace it
distally, incising that portion of the flexor retinaculum that lies
superficial to it. After the tendon has been freed from its tunnel in
the flexor retinaculum, retract it medially to expose the volar aspect
of the radial side of the wrist joint (Fig. 5-52).
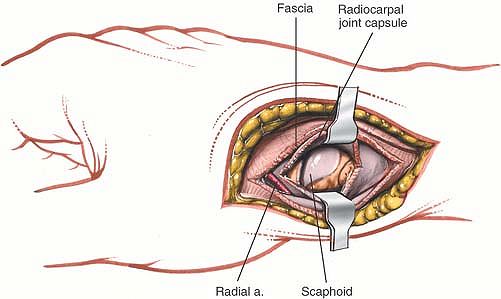
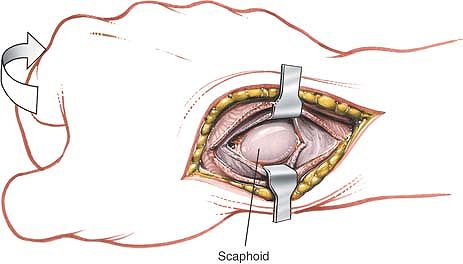
anterior area of bone is nonarticular. To gain the best view of the
proximal third of the bone, place the wrist in marked dorsiflexion (Fig. 5-53).
 |
|
Figure 5-51 Incise the deep fascia between the radial artery and the flexor carpi radialis.
|
 |
|
Figure 5-52
Retract the radial artery and skin flap laterally and the flexor carpi radialis medially to expose the volar aspect of the radial side of the wrist joint capsule. |
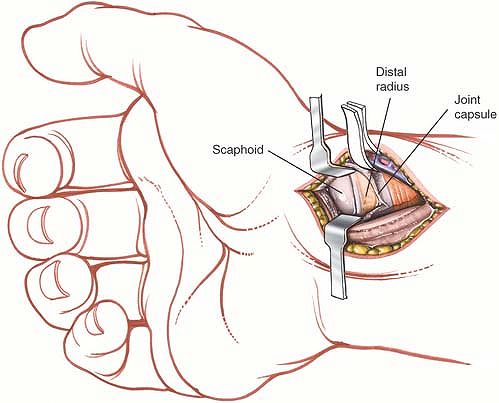 |
|
Figure 5-53 Incise the joint capsule. Dorsiflex the wrist to gain exposure of the proximal articular third of the bone.
|
to the lateral border of the wound and can be incised accidentally at
any time during the dissection. Therefore, it must be identified early
in the procedure.
extent. Proximally, extend the skin incision along the line of the
flexor carpi radialis muscle. Identify the distal border of the
pronator quadratus muscle and elevate it gently from the underlying
bone. This will create adequate exposure of the distal end of the
radius, allowing a bone graft to be taken from this site. Adequate
exposure also will be obtained to allow excision of the radial styloid,
if this is indicated.
dorsiflexion of the wrist. This will expose the proximal pole of the
scaphoid, which is the site of most cases of nonunion. If the location
of the fracture is not completely clear, place a small, radiopaque mark
at the operative site and carry out a radiographic examination on the
operating table. Bone grafting can be carried out adequately with this
exposure, but the insertion of a screw may require a combined dorsal
and volar approach to the scaphoid.25
exposure of the scaphoid bone. Its major drawback is that it endangers
the superficial branch of the radial nerve, and it also may interfere
with the dorsal blood supply of the scaphoid.26 Its uses include the following:
-
Bone grafting for nonunion
-
Excision of the proximal fragment of a nonunited scaphoid
-
Excision of the radial styloid in combination with either of the two above procedures
-
Open reduction and internal fixation of
fractures of the scaphoid. When this approach is used for this
indication, it is frequently combined with a volar approach to the
scaphoid.25
the arm extended on an arm board. Pronate the forearm to expose the
dorsoradial aspect of the wrist, and apply an exsanguinating bandage
and tourniquet (see Fig. 5-1).
 |
|
Figure 5-54
Incision for dorsolateral exposure of the scaphoid. Make a gently curved S-shaped incision centered over the snuff-box. The superficial branch of the radial nerve crosses directly beneath the incision. |
is truly lateral when the hand is in the anatomic position. Palpate it
in this position and then pronate the arm, keeping a finger on the
styloid process.
small depression that is located immediately distal and slightly dorsal
to the radial styloid process. The scaphoid lies in the floor of the
snuff-box. Ulnar deviation of the wrist causes the scaphoid to slide
out from under the radial styloid process, and it becomes palpable. The
radial pulse is palpable in the floor of the snuffbox, just on top of
the scaphoid.
the snuff-box. The cut should extend from the base of the first
metacarpal to a point about 3 cm above the snuff-box (Fig. 5-54).
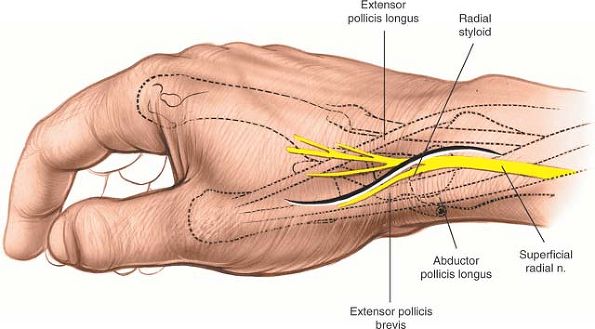
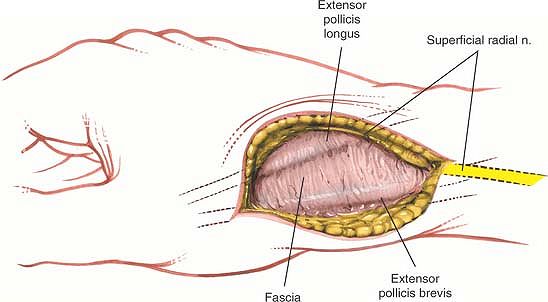
of dissection falls between the tendons of the extensor pollicis longus
and extensor pollicis brevis muscles, both of which are supplied by the
posterior interosseous nerve. Because both muscles receive their nerve
supply well proximal to this dissection, using this plane does not
cause denervation.
To confirm their identity, pull on the tendons and observe their action
on the thumb. Open the fascia between the two tendons, taking care not
to cut the sensory branch of the superficial radial nerve, which lies
superficial to the tendon of the extensor pollicis longus muscle. The
radial nerve usually has divided into two or more branches at this
level. Both branches cross the interval between the tendons of the
extensor pollicis brevis and the extensor pollicis longus, lying
superficial to the tendons. Their course is variable, and they must be
sought and preserved during superficial dissection (see Figs. 5-54 and 5-55).
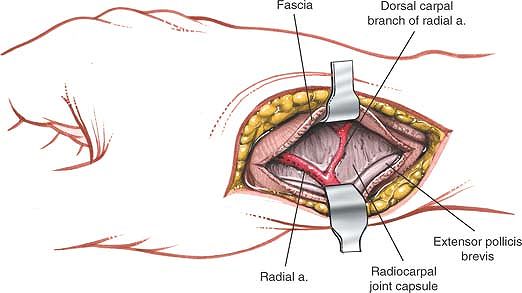
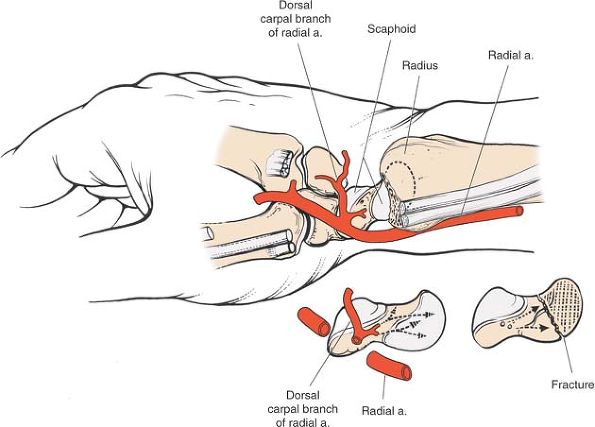
pollicis longus dorsally and toward the ulna, and the extensor pollicis
brevis ventrally. Identify the radial artery as it traverses the
inferior margin of the wound, lying on the bone (Fig. 5-56).
Find the tendon of the extensor carpi radialis longus muscle as it lies
on the dorsal aspect of the wrist joint. Mobilize it and retract it in
a dorsal and ulnar direction, together with the tendon of the extensor
pollicis longus muscle, to expose the dorsoradial aspect of the wrist
joint.
 |
|
Figure 5-55
Identify the superficial branch of the radial nerve and retract it with the dorsal skin flap. Identify the tendons of the extensor pollicis longus dorsally and the extensor pollicis brevis ventrally. Incise the fascia between the tendons. |
Reflect the capsule dorsally and in a volar direction to expose the
articulation between the distal end of the radius and the proximal end
of the scaphoid. The radial artery retracts radially and in a volar
direction with the joint capsule.
Try to preserve as much soft-tissue attachments to the bone as
possible. Modern aiming guides have substantially reduced the need for
radial dissection in open reduction and internal fixation of scaphoid
fractures.
is at risk during this exposure. Because it lies directly over the
tendon of the extensor pollicis longus muscle, it is extremely easy to
cut as the tendon is mobilized. Incising the nerve may produce a
troublesome neuroma, as well as an awkward (although not handicapping)
area of hypoesthesia on the dorsal aspect of the hand.
 |
|
Figure 5-56
Retract the extensor pollicis longus dorsally and the extensor pollicis brevis ventrally. Identify the radial artery and its dorsal carpal branch, taking care to preserve the arterial branch. |
 |
|
Figure 5-57 Incise the joint capsule. The scaphoid is exposed.
|
 |
|
Figure 5-58 Place the wrist in ulnar deviation to expose the proximal third of the scaphoid in its entirety.
|
 |
|
Figure 5-59
Blood supply to the scaphoid. Most branches enter the scaphoid from the dorsal aspect. These branches must be preserved to prevent necrosis of its proximal fragment. |
morbidity. They cause an enormous loss of time from work and can
produce permanent deficits in hand function. Until recently, the
availability of more prompt medical care and the administration of
antibiotics had caused a dramatic decrease in the incidence of major
hand infections; however, the intravenous and subcutaneous use of
narcotics among drug addicts has increased, reintroducing serious hand
infections to the field of surgery.
-
Accurate localization of the infection.
Each particular infection has characteristic physical signs, according
to the anatomy of the particular compartment that is infected. -
Timing of the operation.
The timing of surgical drainage is critical to the outcome of surgical
treatment. If an infection is incised too early, the surgeon may incise
an area of cellulitis and actually cause the infection to spread. In
contrast, if pus is left in the hand too long, particularly around the
tendon, it may induce irreversible changes in the structures it
surrounds.
difficult to determine. In the body, the cardinal physical sign of an
abscess is the presence of a fluctuant mass within an area of
inflammation; however, because there often is only a small amount of
pus present in the hand, an abscess there can be hard to find. In
addition, pus frequently is found in tissues that contain fat. At body
temperature, fat itself is fluctuant, further complicating the physical
diagnosis of an abscess. Nevertheless, some guidelines for the
detection of pus do exist:
-
Pus may be seen subcutaneously.
-
The longer an infection has been present,
the more likely it is that pus will be present. Infections of less than
24 hours’ duration are unlikely to have developed pus. -
Classically, if the patient cannot sleep at night because of pain in the hand, pus probably has formed.
-
If slight passive extension of the finger
produces pain along the finger and in the palm, the tendon sheath is
likely to be infected; it should be explored to drain the pus.
one of the four cardinal signs of acute suppurative tenosynovitis
described by Kanavel.27 The other three follow below:
-
Swelling around the tendon sheath
-
Tenderness to palpation
-
Flexion deformity of the affected finger
determine whether there is pus in the hand. If doubt exists, elevate
the arm and treat the patient with intravenous antibiotics and warm
soaks, reexamining him or her at frequent intervals. If signs of
inflammation diminish rapidly, avoid surgery.
-
Use a general anesthetic or a distal
nerve block. Injecting a local anesthetic at the site of infection is
ineffective and actually may spread the infection within fascial planes. -
Use a tourniquet. The arm should not be
exsanguinated with a bandage, to avoid spreading the infection by
mechanical compression. The arm should be elevated for 3 minutes before
the tourniquet is applied. -
Perfect lighting is critical for all
explorations of pus in the hand. All relevant neurovascular bundles
must be identified to ensure their preservation. -
Draining abscesses of the hand is not
like draining abscesses anywhere else in the body. Boldly incising an
abscess space without approaching it carefully is to be condemned. -
Leave all wounds open after incision.
-
Immobilize the hand in the functional
position after surgery by applying a dorsal or volar splint, or both,
with the metacarpophalangeal joints at 80° of flexion and the proximal
and distal interphalangeal joints at 10° of flexion. At this position,
the collateral ligaments of the metacarpophalangeal, proximal
interphalangeal, and distal interphalangeal joints are at their maximum
length and will not develop contractures during immobilization. -
Elevate the arm postoperatively. Continue
administering intravenous antibiotics until signs of inflammation begin
to diminish. Mobilize the affected part as soon as signs of
inflammation subside. Begin extensive rehabilitation, which may last
several months.
-
Paronychia
-
Pulp space (felon)
-
Web space
-
Tendon sheath
-
Deep palmar area
-
Lateral space (thenar space)
-
Medial space (midpalmar space)
-
-
Radial bursa
-
Ulnar bursa
Hairdressers often are affected because hair from their clients may
become embedded between the cuticle and the bony nail. Tearing the
cuticle to remove a “hangnail” probably is the most common cause of
this infection.
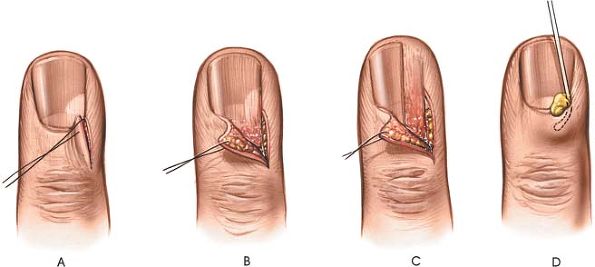
cuticle. The paronychia may occur on either side or it may lift the
whole of the cuticle upward. It even may extend underneath the nail.
supply of the skin in this region is derived from cutaneous nerves that
overlap one another considerably. No area of skin becomes denervated.
cuticle and the nail. If pus extends under the nail, excise either one
corner of the base of the nail or half of the nail itself, depending on
how it has been undermined and lifted off the nail bed (see Fig. 5-60B,C). Occasionally, a nick into the soft-tissue cuticle parallel with the nail will release the pus (see Fig. 5-60D).
 |
|
Figure 5-60 (A through D:) Incisions for the evacuation of pus at the base of the nail (paronychia).
|
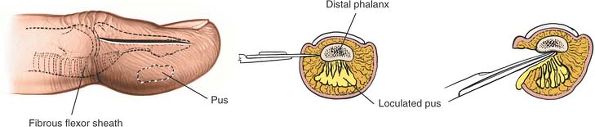
infections that most often require surgical drainage. Infection is
usually caused by a penetrating injury to the pulp, an injury that may
be quite trivial in itself. Superficial infections cause skin necrosis
and point early, usually on the volar aspect of the pulp. Deeper
infections are more likely to cause osteomyelitis of the underlying
distal phalanx, a condition that is known as a felon or whitlow.
-
If the abscess is pointing in a volar
direction in the distal pulp of the finger, as it commonly is, make a
small incision on the lateral side of the volar surface and enter the
abscess cavity obliquely. Midline incisions may produce painful scars. -
If the abscess is deep, the surgery described below may be necessary.
terminal phalanx of the finger, extending to the tip of the finger
close to the nail. The incision should not extend proximally to the
distal interphalangeal joint; more proximal incisions may damage the
digital nerve, causing a painful neuroma, or they may contaminate the
joint with purulent material.
It should not extend distally beyond the distal corner of the nail.
Avoid the ulnar aspect of the thumb and the radial aspect of the index
and long fingers to avoid creating a scar that interferes with pinch.
skin incision lies between skin that is supplied by the dorsal
cutaneous nerve and skin that is supplied by branches of the volar
digital nerves.
 |
|
Figure 5-61 Incision for drainage of pulp space infection (felon). The septa must be cut to ensure appropriate drainage.
|
fibrous septa that connect the distal phalanx with the volar skin,
creating loculi. The infection easily can invade several of these
loculi. To ensure that all pockets of infection are drained, deepen the
skin incision transversely across the pulp of the finger, remaining on
the volar aspect of the terminal phalanx, until the skin of the
opposite side of the finger is reached. Do not penetrate this skin (see
Fig. 5-61). Now, bring the scalpel blade
distally, detaching the origins of the fibrous septa from the bone.
Proximally, take care not to extend the dissection beyond a point 1 cm
distal to the distal interphalangeal crease; otherwise, the flexor
tendon sheath may be damaged and infection introduced into it.
damaged if the skin incision drifts too far proximally. Painful
neuromas can result without an appreciable area of hyperesthesia on the
finger.
skin make this an ideal site for loculation of pus. Take care to open
all the loculi so that adequate drainage takes place. Unsuccessful
treatment of a deep abscess may result in osteomyelitis of the distal
phalanx.
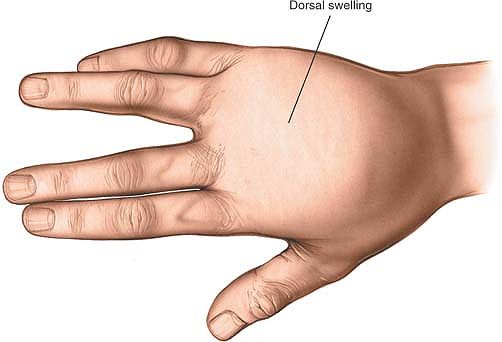
four webs of the palm, are quite common. The abscess usually points
dorsally, because the skin on the dorsal surface of the web is thinner
than the skin on the palmar surface. Characteristically, a large amount
of edema appears on the dorsum of the hand, and the two fingers of the
affected web are spread farther apart than normal (Fig. 5-62).
lumbrical muscles into the palm; therefore, a neglected web space
infection can cause a more extensive infection by spreading up the
lumbrical canal and into the palm.
the arm on an arm board. Use a general anesthetic or an axillary or
brachial block, then raise the arm for 3 minutes before inflating an
arm tourniquet (see Fig. 5-13).
the palm, following the contour of the web space about 5 mm proximal to
it (Fig. 5-63).
 |
|
Figure 5-62
Web space infection. A large amount of edema usually appears on the dorsum of the hand, and the two fingers of the affected web space are spread farther apart than normal. |
The digital nerves and vessels lie immediately under the incision and
may be damaged if the cut is too deep, mainly because the dissection is
being carried out in a transverse rather than a longitudinal plane. The
abscess cavity usually is located just below the skin; it can be
entered with very little additional dissection.
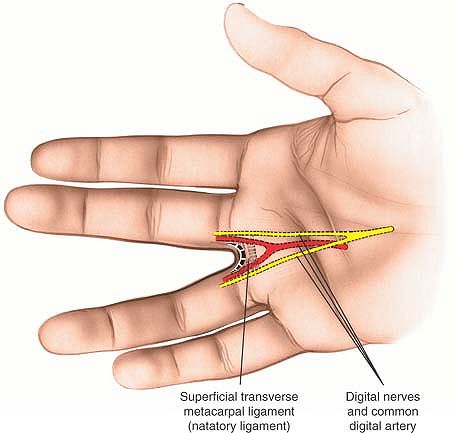 |
|
Figure 5-63 Make a curved transverse incision in the volar skin of the palm, following the contour of the web space.
|
this transverse skin incision. Make sure that an effective tourniquet,
proper lighting, and fine instruments are used in the operation. As
long as the skin is incised with care, the nerves should not be damaged.
to the neurovascular bundle, but scarring during the healing process
may reduce significantly the ability of the two fingers of the web
space to separate. That is why a transverse skin incision is
recommended.
recommend a second, dorsal, skin incision over the pointing area to
improve drainage without appreciably increasing the morbidity of the
procedure.
spaces are surprisingly long (about 2 cm), extending from the edge of
the skin to the metacarpophalangeal joints. They contain both the
superficial and the deep transverse ligaments of the palm, the digital
nerves and vessels, and the tendons of the interossei and lumbricals.
Between these various structures lies loose, fibrous, fatty tissue,
tissue that can be displaced easily by infection and the formation of
abscesses (Fig. 5-64; see Fig. 5-33).
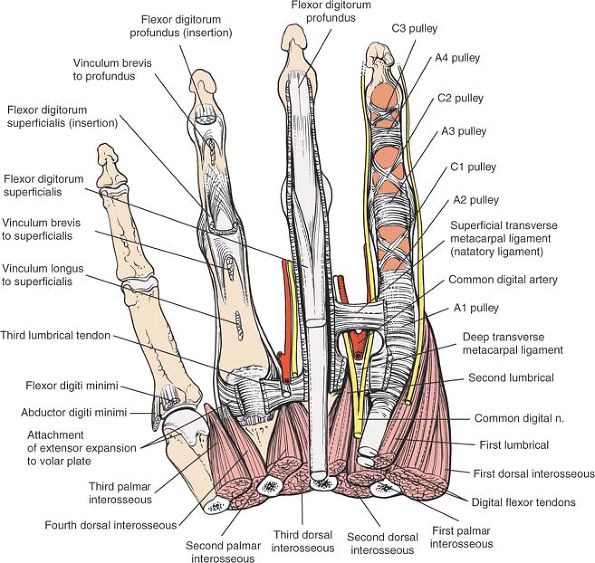 |
|
Figure 5-64
Anatomy of the web space. The neurovascular bundle runs deep to or dorsal to the superficial transverse ligament (natatory ligament) and palmar to the deep transverse metacarpal ligament. The lumbrical muscle runs along with the neurovascular bundle palmar to the deep transverse ligament, whereas the interossei pass dorsal to the deep transverse metacarpal ligament. |
-
Superficial transverse ligament of the palm (natatory ligament).
This ligament lies immediately beneath the palmar skin and supports the
free margins of the webs. The ligament runs superficial (palmar) to the
digital nerves and vessels, and attaches to the palmar aponeurosis. -
Digital nerves and vessels.
These structures lie immediately deep to the superficial transverse
ligament of the palm, with the nerves on the palmar side of the
arteries. -
Tendons of the lumbricals.
These muscles arise from the four tendons of the flexor digitorum
profundus muscle in the middle of the palm. Each lumbrical tendon
passes along the radial side of its metacarpophalangeal joint before
inserting into the extensor expansion on the dorsum of the proximal
phalanx. Infection in the web space can spread proximally along the
lumbrical tendon and enter the palm (see Fig. 5-66). -
Deep transverse ligament of the palm.
This strong ligament connects the volar plates (palmar ligaments) of
the metacarpophalangeal joints. It is 3 to 4 cm proximal to the
superficial transverse ligaments. The lumbrical tendons are volar or
palmar to it, as is the neurovascular bundle (see Fig. 5-64). -
Interosseous tendons.
These muscles, which arise from the metacarpals, insert into the dorsal
expansion over the proximal phalanges. Their tendons pass dorsal to the
deep transverse ligament, in contrast to the lumbrical tendons, which
pass on the ligament’s volar side (see Fig. 5-64).
fingers. Its increased mobility is reflected in the unique anatomy of
its web space: both the superficial and the deep transverse ligaments
are absent and the bulk of the web is filled with two muscles, the
transverse head of the adductor pollicis and the first dorsal
interosseous (see Figs. 5-33, 5-34 and 5-35).
interossei. It arises from the adjacent borders of the first and second
metacarpals, runs deep to the adductor pollicis, and inserts into the
fibrous extensor expansion on the dorsum of the index finger. The
muscle bulk provides most of the substance of the thumb’s web space;
wasting is easy to detect clinically by gently pinching the web while
the patient pinch-grips. The pinch also forms the basis for one test of
an ulnar nerve lesion, because the muscle is supplied by the ulnar
nerve (see Fig. 5-9).
and the princeps pollicis, emerge from between the two muscles of the
thumb web. The radialis indicis artery runs to the radial border of the
index finger, and the princeps pollicis goes to the thumb, where it
divides into two palmar digital arteries. Approaches made in the center
of the web space avoid damage to either artery (see Fig. 5-35).
tendons is one of the most serious of all hand infections. Prompt
surgical drainage is critical, for a long-standing infection almost
always results in fibrosis within the tendon sheath and subsequent
tethering of the tendon itself. Sheath infections are caused by spread
from a pulp infection or by puncture wounds, particularly at the flexor
creases.
flexed position is grossly swollen and tender. The slightest active or
passive extension of the digit produces severe pain, which is the
cardinal physical symptom on which the diagnosis is based.
a result of earlier diagnosis and treatment of superficial finger
infections. Nevertheless, they still occur and offer a true orthopaedic
emergency.
the arm extended on an arm board. A tourniquet is essential, but the
arm should not be exsanguinated as it is with general anesthesia or a
proximal local block (either brachial or axillary). Good lighting and
fine instruments minimize the risk of damaging the vital structures
within the hand (see Fig. 5-13).
roughly marks the palmar site of the metacarpophalangeal joints and the
proximal border of the fibrous flexor sheath of the flexor tendons.
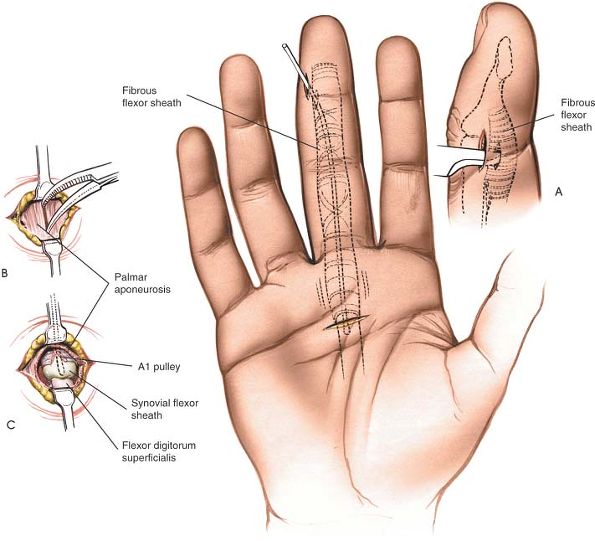 |
|
Figure 5-65
Incision for infection of the flexor digital sheath. Make a small transverse incision just proximal to the distal palmar crease, over the infected flexor tendon. (A) A second incision may be necessary, and this should be made over the distal end of the middle phalanx in the midlateral position. (B) Separate the longitudinally running fibers of the palmar aponeurosis. (C) Incise the A1 pulley to reveal the underlying synovial sheath, which then should be opened. |
is the surface marking of the distal interphalangeal joint and lies
just proximal to the distal end of the fibrous flexor sheath.
distal palmar crease and over the infected flexor tendon. The incision
should be 1.5 to 2.0 cm long (Fig. 5-65).
midlateral approach is roughly in the line of demarcation between skin
that is supplied by the digital nerves and skin that is supplied by the
dorsal cutaneous nerves.
aponeurosis by blunt dissection, by opening a closed hemostat so that
the dissection is carried out parallel to, rather than across, the main
neurovascular bundles of the palm (see Fig. 5-65B).
Proceed deeper onto the proximal end of the fibrous flexor sheath. At
this level, the proximal (A1) pulley is visible. Incise the pulley
longitudinally to reveal turbid fluid or, more rarely, frank pus (see Fig. 5-65C).
If turbid fluid is found, make the second skin incision and deepen it,
coming down dorsal to the digital nerves and vessels. Incise the
fibrous flexor sheath at the distal end of the middle phalanx.
incisions. If the skin incision in the finger is made too far in a
volar direction, it may threaten the neurovascular bundle. The bundle
is safe as long as the skin incision remains just dorsal to the dorsal
end of the proximal and distal interphalangeal creases (see Fig. 5-65 and Midlateral Approach to the Flexor Sheaths).
neurovascular bundles at right angles, and because the bundles lie
immediately deep to the palmar aponeurosis, the bundles may be damaged
by overzealous incision of the skin. Separating the fibers of the
palmar aponeurosis by blunt dissection in the line of the fibers avoids
damage to the nerves.
lead to diminished hand function. The infected area usually lies deep
to the flexor tendons and lumbricals, but superficial to the
metacarpals and their muscles, the adductor pollicis and the interossei.
septum of fascia that arises from the fascia surrounding the flexor
tendons of the middle finger and attaches to the third metacarpal. The
area on the lateral side of the septum sometimes is called the thenar
space, and the area on the medial side is called the midpalmar space.
In this text, the terms lateral space and medial space are used, because the term thenar space can be confusing, as this area has nothing to do with the space that is occupied by the thenar muscles of the thenar eminence (Fig. 5-66; see Fig. 5-34).
tenderness, and swelling of the palm. The middle and ring fingers lose
their ability to move actively, and moving them passively produces
severe pain. The hand is grossly swollen, resembling an inflated rubber
glove.
signs similar to those of infections of the medial space, but the index
finger and thumb are the digits that lose the ability to move.
in hand surgery. These deep infections are being seen more frequently
now, however, primarily because of the increase in drug addiction. More
than any other infection in the hand, they can cause systemic illness
associated with high fevers.
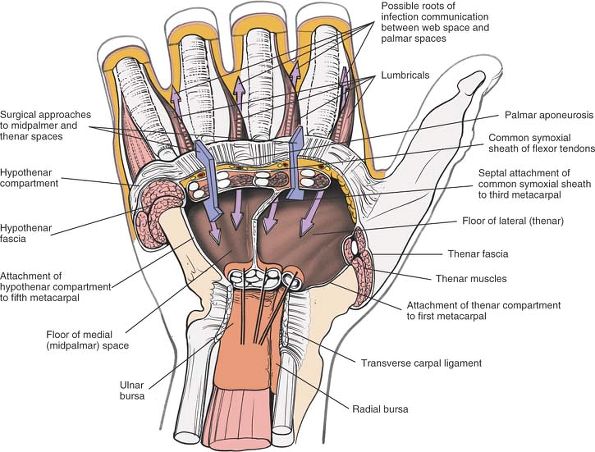 |
|
Figure 5-66
Within the central compartment of the palm, a potential deep space exists between the undersurface of the flexor tendons and the upper surfaces of the interossei and adductor pollicis muscles. This deep palmar space is subdivided into medial midpalmar and lateral thenar spaces by the oblique septum that arises from the connective tissue surrounding the middle finger flexor tendons and runs to the palmar surface of the middle metacarpal. Infections involving the web space may travel along the lumbrical muscle to enter these two potential spaces. |
proximal to the distal palmar crease and over the swelling. The length
of the incision should be determined by the size of the abscess to be
drained (Fig. 5-67).
crosses the paths of the digital nerves. Open the palmar fascia by
blunt dissection at the distal end of the wound and identify the long
flexor tendon to the ring finger. Enter the medial midpalmar space by
blunt dissection on the radial border of this tendon (Figs. 5-68, 5-69 and 5-70).
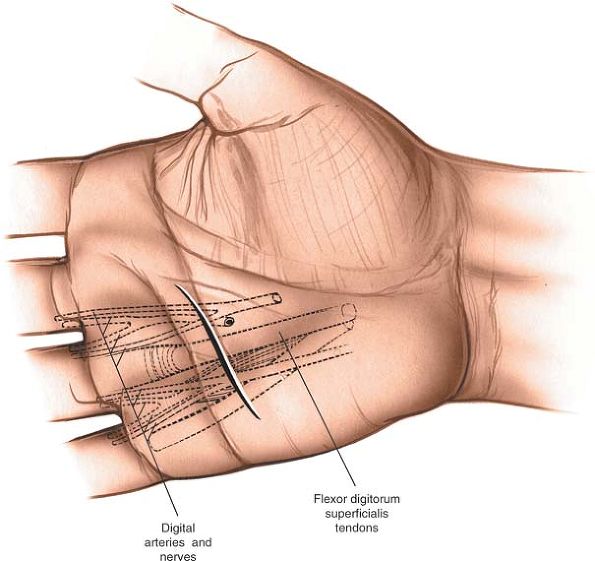 |
|
Figure 5-67 Incision for drainage of the medial space (midpalmar space).
|
little and ring fingers run immediately under the palmar aponeurosis
and cross the line of the skin incision. No part of the palmar
aponeurosis should be incised transversely until these nerves have been
dissected out fully (see Fig. 5-69).
with the digital nerves and also may be in danger. For this reason, the
digital arteries should be identified before the palmar aponeurosis is
incised.
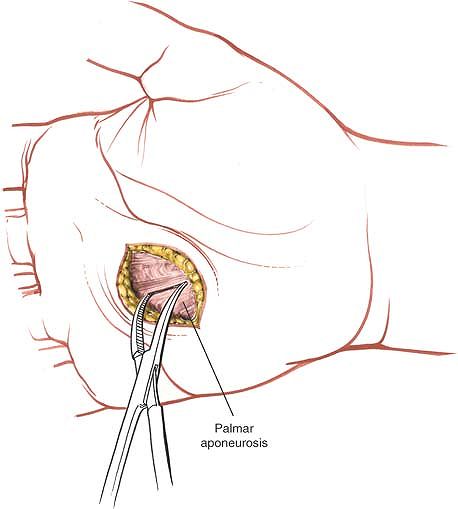 |
|
Figure 5-68 Open the palmar fascia by blunt dissection at the distal end of the wound.
|
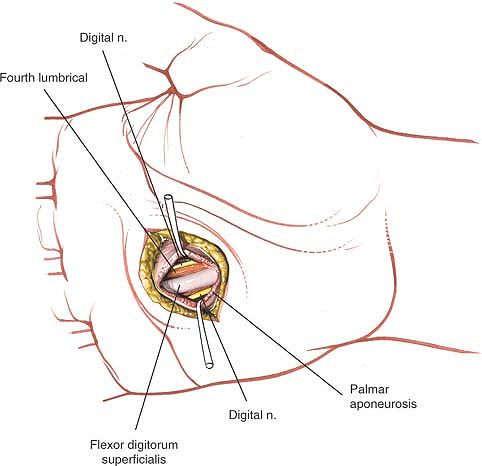 |
|
Figure 5-69
The long flexor tendon to the ring finger is identified. The neurovascular structures run parallel to it on each side, and the lumbrical is visible on its radial side. |
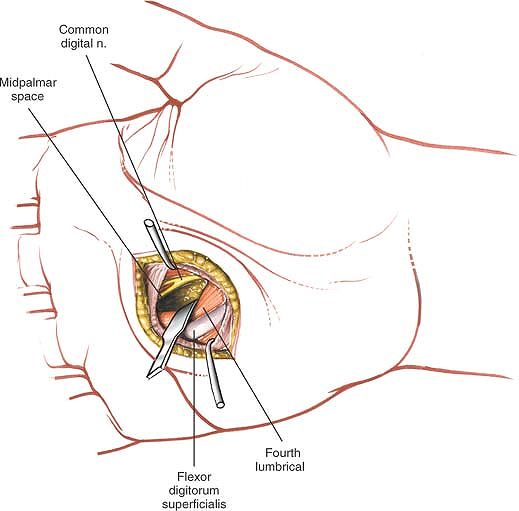 |
|
Figure 5-70 The deep palmar space is entered by retracting the lumbrical and its tendon medially.
|
taking care to identify and preserve the digital nerves to the index
finger. Identify the long flexor tendon to the index finger (Figs. 5-72 and 5-73). Deep to these tendons is the lateral space; enter it by blunt dissection (Fig. 5-74).
index finger are directly in line with the skin incision. Take care not
to damage them during incision of the palmar aponeurosis.
emerges from the deep surface of the median nerve as the median nerve
leaves the carpal tunnel. Note, however, that the location of its
division from the median nerve is quite variable. This nerve hooks
around the distal end of the flexor retinaculum to supply the muscles.
Make sure to identify the branch at the proximal end of the incision so
as to avoid damaging it (see Fig. 5-32).
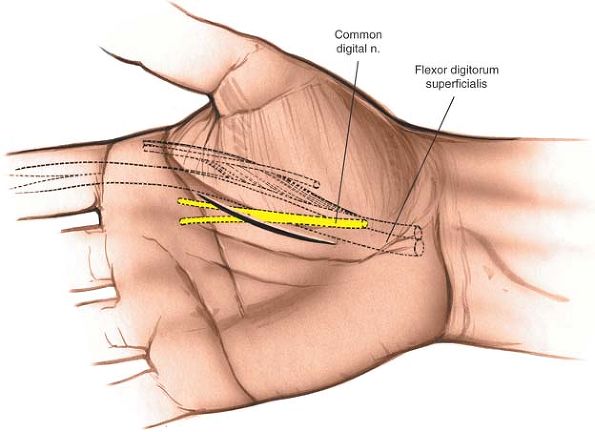 |
|
Figure 5-71 Incision for drainage of the lateral space (thenar space). The incision is made just to the ulnar side of the thenar crease.
|
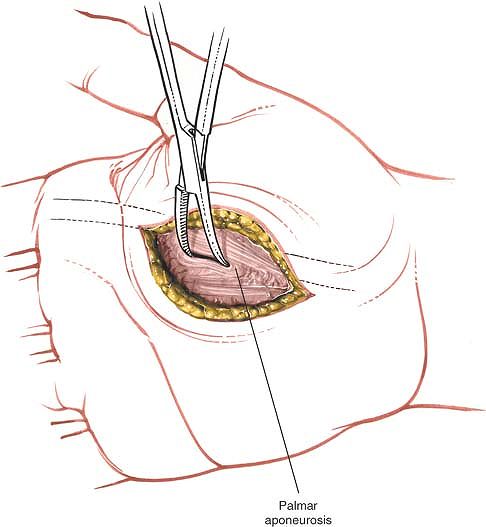 |
|
Figure 5-72 Identify the palmar fascia and spread it in line with its fibers over the flexor tendon to the index finger.
|
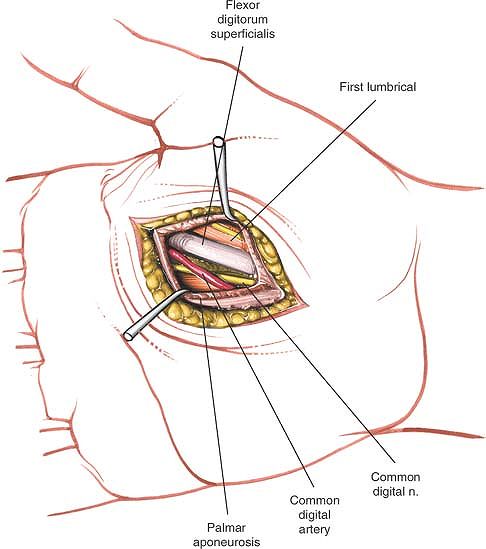 |
|
Figure 5-73
Identify the flexor tendon to the index finger. The neurovascular bundles lie to each side. The lumbrical is seen on the radial side. |
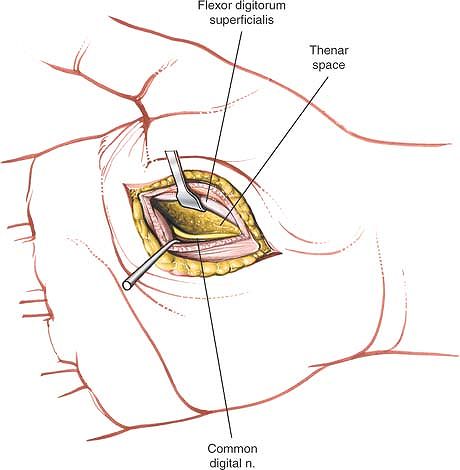 |
|
Figure 5-74 Retract the tendon and lumbrical radially, and enter the space beneath them by blunt dissection.
|
pass through it before attaching to the metacarpals. There are two
major septa: the thenar septum originates
from the palmar aponeurosis and inserts into the first metacarpal,
separating the three muscles of the thenar eminence from the central
palmar structures; and the hypothenar septum
originates on the ulnar side of the palmar aponeurosis and inserts into
the fifth metacarpal, separating the three muscles of the hypothenar
eminence from the central palmar structures (see Figs. 5-34 and 5-66).
to the fingers and the adductor pollicis muscle, as well as the digital
nerves and vessels and the superficial and deep palmar arches.
exists between the undersurface of the flexor tendons and the upper
surface of the interosseous and adductor pollicis muscles. This deep
palmar space is divided into medial (midpalmar) and lateral (thenar)
spaces by the oblique septum that arises
from the connective tissue surrounding the middle finger flexor tendons
and runs to the palmar surface of the middle metacarpal.28 This septum is the anatomic basis for the clinical division of deep palmar infection into two distinct, separate spaces.27
muscle, which runs with the long flexor tendon to the index finger.
Infections in the first web space may track down into the lateral space
along the lumbrical muscle, although this is rare. Although lateral
space infections may be drained through the first web space, such an
incision drains less thoroughly than does the procedure described in
the previous section (see Figs. 5-71, 5-72, 5-73 and 5-74).
A second potential space exists behind that muscle and in front of the
interossei. Infection of this “posterior adductor space” is very rare.29
middle, ring, and little fingers, which run from the long flexor
tendons of the middle, ring, and little fingers (the volar boundary of
the space). The deep boundary is formed by the interossei and
metacarpals of the third and fourth spaces. Thus, infection in the web
spaces between the middle and ring fingers, and between the ring and
little fingers, in theory, may spread to the medial space (see Fig. 5-66).
The medial space may be drained through an incision in these webs, but
the result is not as good as that obtained with direct drainage (see Figs. 5-67, 5-68, 5-69 and 5-70).
synovial sheath that extends from the tendon’s insertion into the
distal phalanx through the palm and carpal tunnel to the forearm just
proximal to the proximal end of the flexor retinaculum. The proximal
end of this sheath is known as the radial bursa (Fig. 5-75).
clinical grounds as are infections of the synovial sheaths of the other
fingers: fusiform swelling of the thumb, with extreme pain on active or
passive extension of the digit.
the arm on an arm board. A general anesthetic or an axillary or
brachial block is essential. Use a nonexsanguinating tourniquet and
have an excellent light source available (see Fig. 5-12).
is the surface marking for the interphalangeal joint of the thumb. It
lies just proximal to the distal end of the fibrous flexor sheath of
the thumb.
make a small longitudinal incision on the lateral side of the proximal
phalanx of the thumb, just dorsal
to the dorsal termination of the interphalangeal crease (Fig. 5-76).
Then, make a second incision over the medial aspect of the thenar
eminence (beware of the motor branch) or on the volar aspect of the
wrist (the proximal end of the radial bursa).
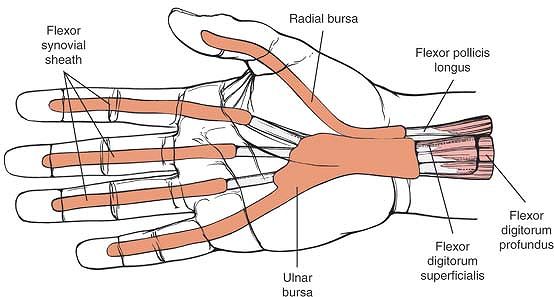 |
|
Figure 5-75 Anatomy of the synovial sheaths of the fingers and the radial and ulnar bursae.
|
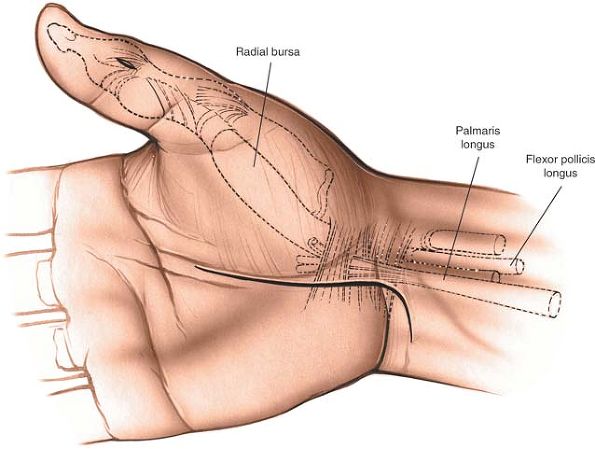 |
|
Figure 5-76
Incision for drainage of the radial bursa. Two incisions are required for complete drainage. Distally, make a small longitudinal incision on the lateral side of the proximal phalanx of the thumb, just dorsal to the interphalangeal crease. Make a second incision over the medial aspect of the thenar eminence on the volar aspect of the wrist, and carry the incision proximally to the end of the radial bursa. Care must be taken to protect the median nerve and its motor branch to the thenar muscles. |
skin incision in the finger lies between skin that is supplied by the
dorsal digital nerves and skin that is supplied by the volar digital
nerves.
remaining dorsal to the radial neurovascular bundle of the thumb.
Identify the fibrous flexor sheath covering the flexor pollicis longus
tendon and incise it longitudinally, just proximal to the tendon’s
insertion into the distal phalanx. Incise the synovium within the
sheath to drain the pus.
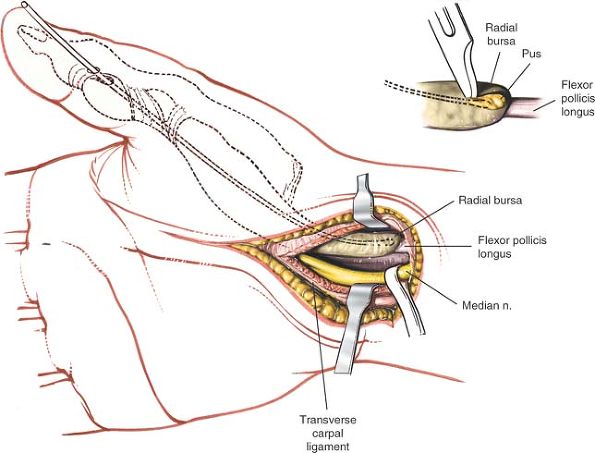 |
|
Figure 5-77
Identify the fibrous flexor sheath covering the flexor pollicis longus tendon and incise it longitudinally just proximal to the tendon’s insertion into the distal phalanx. Incise the synovium in the sheath to drain the pus and then pass a probe proximally along the flexor sheath. Make a small longitudinal incision over the probe at the level of the wrist to ensure complete drainage. |
until the point of the probe can be felt on the volar aspect of the
wrist. Make a small longitudinal skin incision over this point and
dissect carefully down to the probe. The tip of the probe may be
proximal to the proximal end of the flexor retinaculum, or it may be
actually in the carpal tunnel itself. If it is in the carpal tunnel,
then formally incise the flexor retinaculum, taking great care not to
damage the underlying median nerve with its motor branch to the thenar
eminence. This is the only situation in which the median nerve is
approached necessarily from its radial aspect in the carpal tunnel.
infections, a small catheter may be left in the distal end of the
flexor sheath to irrigate the flexor tendon (Fig. 5-77).
in a volar direction, its radial neurovascular bundle may be incised
accidentally.
wrist; the median nerve, the motor branch of the median nerve, or the
palmar cutaneous branch of the median nerve may be cut (see Applied Surgical Anatomy of the Volar Aspect of the Wrist).
the little finger extends from the insertion of the profundus tendon on
the distal phalanx of the little finger to the volar aspect of the
wrist, just proximal to the proximal end of the flexor retinaculum. The
flexor tendons to the index, middle, and ring fingers also are invested
by this layer of synovium as they pass through the carpal tunnel. The
distal extension of the synovial compartment ends at the origin of the
lumbrical muscle from the tendons to the ring, middle, and index
fingers. It is known as the ulnar bursa (see Fig. 5-75).
may lead to infection of the ulnar bursa. The physical signs include a
tenosynovitis affecting the little finger, with active or passive
extension producing extreme pain. In addition, pain may be referred to
the palm when the other fingers are extended.
the arm extended on an arm board. Use a nonexsanguinating tourniquet
and either a general anesthetic or a proximal local block (an axillary
or brachial block).
is the surface marking for the distal interphalangeal joint. It lies
just proximal to the distal end of the fibrous sheath of the little
finger.
The incision should be just dorsal to the line connecting the dorsal
termination of the proximal and distal interphalangeal creases. Make a
second longitudinal incision on the lateral aspect of the hypothenar
eminence at the level of the wrist.
lies between skin that is supplied by the dorsal digital nerves and
skin that is supplied by the volar digital nerves.
to the dorsal side of the neurovascular bundle. Identify the fibrous
flexor sheath and incise it longitudinally. Next, incise the synovium
to allow drainage of the pus. Pass a probe gently along the tendon
until it can be felt on the volar aspect of the wrist, just proximal to
the proximal end of the flexor retinaculum.
and dissect down to it layer by layer. The probe should be just
proximal to the proximal end of the flexor retinaculum. It may be in
the carpal tunnel, however, in which case, the flexor retinaculum will
have to be incised meticulously, taking care to avoid damage to the
underlying median nerve. If the probe is lying in the forearm, then
take great care not to damage the ulnar nerve and artery, which are
very close to the flexor digitorum superficialis tendon to the little
finger (see Fig. 5-78).
infections, a small catheter may be inserted in the distal wound to
allow continuous or intermittent irrigation of the tendon sheath.
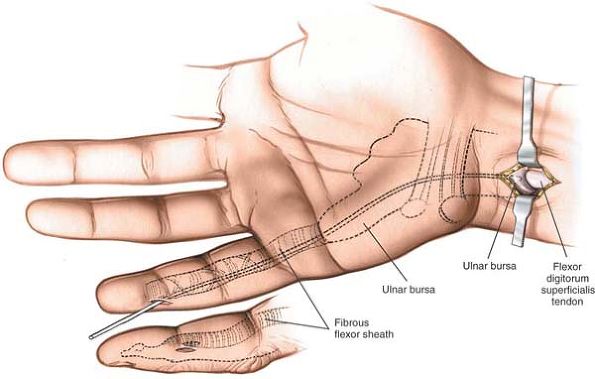 |
|
Figure 5-78
Drainage of the ulnar bursa. Make a short midline incision on the ulnar side of the little finger over the distal end of the middle phalanx. Make a second longitudinal incision over the lateral aspect of the hyperthenar eminence at the level of the wrist. Pass a probe from the distal aspect to the proximal aspect, and cut down onto the probe at its proximal end, a point that marks the proximal end of the ulnar bursa. |
is in danger if the skin incision on the finger is made too far in a
volar direction. The distal vessels run with the nerves.
-
The hand has a natural resting position.
At rest, both the metacarpophalangeal and the interphalangeal joints
normally hold a position of slight flexion. The fingers all adopt a
slightly different degree of rotation, such that the volar surfaces of
the terminal phalanges face progressively more toward the thumb as one
moves from the index finger to the little finger. It is critical to
appreciate the different degrees of rotation in the finger when
assessing displacement in phalangeal or metacarpal fractures. The
degree of flexion increases as one passes from the index finger to the
little finger. This configuration is a result of muscle balance; if one
element is deficient or absent, the resting position of the hand
changes. In cases
P.252
of
acute trauma, a cut flexor tendon may leave a finger extended. An
abnormal resting position often is indicative of tendon damage. -
The concept of muscle balance
also can be applied to chronic conditions of the hand. In patients with
long-standing ulnar nerve lesions, in which the intrinsic muscles of
the hand are paralyzed, the hand develops an abnormal attitude because
of muscle imbalance. The intrinsic muscles normally flex the fingers at
the metacarpophalangeal joints and extend them at the proximal and
distal interphalangeal joints. The absence of intrinsic function leads
to extension of the metacarpophalangeal joints and flexion of the
proximal and distal interphalangeal joints of the affected fingers,
resulting in an ulnar clawhand.
fingers is a tough structure, characterized by flexure creases in the
palm and fingerprints in the fingers. The skin has very little laxity
because of the series of tough fibrous bands that tie it to the palmar
aponeurosis. These bands divide the subcutaneous fat into small loculi,
which are capable of withstanding considerable pressure. The skin’s
lack of mobility means that it is difficult to close even small defects
in it without resorting to plastic procedures such as V-Y advancement flaps or skin grafting.
and even long, distally based flaps may survive. In an elective
incision, however, the angle at the apex of a triangular flap should be
more than 60°, and distally based flaps should be avoided, if possible.
should not be crossed at 90°. Cutting within a flexure crease itself
avoids this problem, but the wound created is difficult to close
without inverting the skin edges. That is the reason that many
incisions parallel natural flexure creases.
It is continuous with the tendon of the palmaris longus muscle,
spreading distally from the distal border of the flexor retinaculum to
cover the central area of the palm between the thenar and hypothenar
eminences. At the bases of the fingers, it divides into four bands, one
for each finger. At the level of the distal palmar crease, these bands
divide into two and run into the fingers to insert into the bases of
the proximal phalanges and the fibrous flexor sheaths (see Fig. 5-30).
to the palmar aponeurosis and actually are in contact with its deep
surface. In patients with Dupuytren’s contracture, the palmar fascia
thickens; contracted and fibrous tissue grows all around the digital
nerves and vessels to enclose them.30
thinner than that over the central palm because of the greater mobility
required from the first and fifth digits.
and fifth metacarpals at its lateral and medial borders, dividing the
hand into three major compartments: the thenar, hypothenar, and palmar
spaces. There also are deep connections between the palmar aponeurosis
and the metacarpals in the distal part of the hand (see Fig. 5-33).
abductor pollicis brevis, the flexor pollicis brevis, and the opponens
pollicis (see Figs. 5-33 and 5-34).
All three are supplied by the median nerve via its motor branch, which
enters the eminence between the short abductor and the flexor.
from the ulnar nerve to its deep head. This dual nerve supply explains
the clinical observation that a complete median nerve palsy does not
necessarily produce complete flattening of the thenar eminence, because
the bulky deep head of the flexor pollicis brevis does not atrophy.
The superficial layer consists of the short abductor and the short
flexor, with the abductor lying on the radial side of the flexor. The
deep layer consists of the opponens pollicis, which produces rotation
of the thumb metacarpal at its saddle-shaped joint with the trapezium.
The ability to oppose the thumb and the other fingers is one of the
major structural advantages that the human hand has over the ape hand.
It is a complex movement requiring several muscles. The abductor
pollicis brevis abducts the thumb, rotation is achieved by the opponens
pollicis, and the movement is completed by the thumb flexors. The
abductor pollicis brevis is the most important muscle in this group.
Median nerve paralysis destroys opposition; the resultant hand often is
known as a simian (apelike) hand.
abductor digiti minimi, the flexor digiti minimi, and the opponens
digiti minimi. These muscles (all of which are supplied by the ulnar
nerve) are arranged in the same layering as are those of the thenar
eminence. The superficial layer consists of the abductor and flexor,
with the abductor lying on the ulnar side;
the
deep layer consists of the opponens digiti minimi. Together, these
muscles help deepen the cup of the palm of the hand. Very little
genuine opposition of the fifth finger is possible compared with that
of the thumb (see Figs. 5-33 and 5-34).
eminence is the palmaris brevis muscle, the only muscle that is
supplied by the superficial branch of the ulnar nerve.
is an arterial arcade that is formed largely by the ulnar artery. The
arcade is completed by the superficial palmar branch of the radial
artery, but this branch often is missing. When it is, the arch remains
incomplete. Four palmar digital arteries
arise from the arcade and pass distally. The most ulnar of the arteries
supplies the ulnar border of the little fingers; the other three common
digital arteries divide in the web space into two vessels that supply
adjacent fingers.
nerves in the palm, an arrangement that is opposite of that of the
finger, and that the thumb and the radial side of the index finger are
not supplied by its branches.
immediately deep to the superficial palmar arch. The ulnar nerve
divides into a superficial and a deep branch at the distal border of
the flexor retinaculum. The superficial branch supplies the ulnar 1½
fingers with sensation. The median nerve divides into two sensory
branches after giving off its motor branch to the thenar muscles. The
medial branch supplies the radial side of the ring finger, the middle
finger, and the ulnar side of the index finger. The lateral branch
supplies the radial side of the index finger and the whole of the thumb.
the long flexor tendons. The tendons of the flexor digitorum
superficialis muscle overlie those of the flexor digitorum profundus
muscle. Each flexor profundus tendon gives rise to a lumbrical muscle,
which passes along the radial side of the metacarpophalangeal joint
before inserting into the extensor expansion from the dorsum of the
proximal phalanx. Lumbricals that arise by two heads from adjacent
profundus tendons (usually the ulnar two) are supplied by the ulnar
nerve; lumbricals that arise from one tendon (usually the radial two)
are supplied by the median nerve.
deep to the long flexor tendons and forms a fourth layer in the palm
(see Figs. 5-34 and 5-35).
The arterial arch consists of the terminal branch of the radial artery,
which enters the palm by passing between the oblique and transverse
heads of the adductor pollicis muscle, and the deep branch of the ulnar
artery. Running with the ulnar artery is the deep branch of the ulnar
nerve, which supplies all the interossei with muscular branches at this
level.
and palmar. The dorsal interossei arise by two heads from adjacent
sides of the metacarpals and insert into the proximal phalanges so that
they abduct the fingers away from the line drawn through the center of
the third finger.
arises from only one metacarpal and inserts into the base of the
proximal phalanx, adducting the finger toward the middle finger.
ulnar nerve. (The function of the interossei can be remembered by the
mnemonics “PAD” and “DAB”: the palmar interossei adduct, and the dorsal interossei abduct.)31
nerve and the radial artery, have courses that do not follow the
layering concept. The way in which they run through the wrist and hand
ties the rest of the anatomy together.
the volar aspect of the distal radius. It reaches the dorsum of the
hand under the tendons of the abductor pollicis longus muscle and the
extensor pollicis brevis muscle, lying on the scaphoid bone in the
anatomic snuffbox. To return to the volar aspect of the palm, it
pierces the deepest layer of the palmar structures, passing between the
two heads of the first dorsal interosseous muscle. At that point, it
gives off two branches, the radialis indicis artery and the princeps
pollicis artery, which supply the index finger and thumb, respectively.
The main arterial trunk then passes between the two heads of the
adductor pollicis and lies superficial to the deepest muscles as it
forms the deep palmar arch.
hand superficial to the flexor retinaculum within the canal of Guyon.
There, it divides into superficial and deep branches (see Fig. 5-31).
The superficial branch gives off digital nerves and lies in the same
plane as the superficial arterial arcade. The deep branch descends
through the layers of the palm, passing between the heads of origin of
the opponens digiti minimi to lie on the
interossei
in the same plane as the radial artery. There, it supplies all the
interossei, the two ulnar lumbrical muscles, both heads of the adductor
pollicis muscle, the three hypothenar muscles, and the deep head of the
flexor pollicis brevis muscle (see Figs. 5-34 and 5-35).
is thinner than the palmar skin and is more mobile to allow for finger
flexion. The subcutaneous tissue contains very little fat, but a large
number of veins. Venous return runs via the dorsum of the hand because
the pressure of gripping otherwise would impede it. The blood supply of
the dorsal skin is not as good as that of the palmar skin, and distally
based skin flaps are less likely to survive.
terminal branches of the superficial radial nerve as far as the middle
of the middle phalanx. The ends of these fingers are supplied by
branches of the median nerve that are derived from the volar digital
nerves.
by the ulnar nerve, the proximal 1½ phalanges are supplied by dorsal
branches of the ulnar nerve, and the distal 1½ phalanges are supplied
by branches of the ulnar nerve (the volar digital nerves).
terminal phalanx, including the nail bed, can be anesthetized by an
injection of local anesthetic around the volar digital nerves.
the long extensors. Just proximal to the metacarpophalangeal joint,
these tendons are united by three oblique bands, which limit retraction
of the tendon if it is cut. As each long extensor tendon passes over
its metacarpophalangeal joint, its deepest part becomes continuous with
the dorsal capsule of that joint. The tendon becomes much broader
before dividing into three slips over the dorsal surface of the
proximal phalanx. The central slip inserts into the base of the middle
phalanx and the two marginal slips receive attachments from interossei
and lumbrical tendons to form a broad extensor expansion, or hood,
which overlies the metacarpal head and the proximal part of the
proximal phalanx. The hood is anchored firmly on each side to the volar
plate of the metacarpophalangeal joint. Each hood receives some of the
insertion of each of two interossei, with the rest going to the
proximal phalanx itself. The amount varies considerably from finger to
finger. The entire insertion of the lumbrical tendon attaches to the
extensor hood (see Fig. 5-9).
tendons are joined to each other by transversely running fibers (the
triangular ligament). Initially, the two marginal slips of the long
extensor tendon pass outward from the midline to insert into the base
of the distal phalanx. By inserting into this extensor expansion from
the palmar side, the lumbrical and interosseous muscles not only can
abduct and adduct the fingers at the metacarpophalangeal joint, but
also can flex the metacarpophalangeal joint while extending the distal
and proximal interphalangeal joints. In this way, each extended finger
can be flexed independently.
and the triangular ligament may produce a flexion deformity at the
proximal interphalangeal joint. The two marginal slips then pass volar
to the joint and act as flexors of that joint, and the joint
“buttonholes” between these two slips. This deformity is known as a
boutonniere deformity or, as the French put it, “le buttonhole.”
I, Vainik K: Posterior (dorsal) synovectomy for rheumatoid involvement
of the hand and wrist: a follow up study of sixty-six procedures. J
Bone Joint Surg [Am] 48:1035, 1966
RG, Defiore JC, Straub LR et al: Long term results of dorsal
stabilization in the rheumatoid wrist. J Hand Surg [Am] 6:272, 1981
D, Jupiter JB, Brennwald J et al: Prospective multicenter trial of a
plate for dorsal fixation of distal radius fractures. J Hand Surg [Am]
22(5):777, 1997
GS, Gardner WJ, Lalonde AA: Neuropathy of the median nerve due to
compression beneath the transverse carpal ligament. J Bone Joint Surg
[Am] 32:109, 1950
EK, Shrewsbury MM: Anatomical course of the thenar branch of the median
nerve—usually in a separate tunnel through the transverse carpal
ligament. J Bone Joint Surg [Am] 52:269, 1970
N, Matsui T, Miyaji N et al: Vascular anatomy of flexor tendon, I:
vincular system and blood supply of the profundus tendon in the digital
sheath. J Hand Surg [Am] 4:321, 1979
G, Myrhage R, Rydevik B: The vascularization of human flexor tendons
within the digital synovial sheath region: structural and functional
aspects. J Hand Surg [Am] 2:417, 1977
AB: Infections of the hand: a guide to the surgical treatment of acute
and chronic suppurative processes in the fingers, hands, and forearm,
7th ed. Philadelphia, Lea & Febiger, 1939