Knee
Editors: Morrey, Bernard F.; Morrey, Matthew C.
Title: Master Techniques in Orthopaedic Surgery: Relevant Surgical Exposures, 1st Edition
Copyright ©2008 Lippincott Williams & Wilkins
> Table of Contents > Section II – Lower Extremity > 9 – Knee
9
Knee
Mark W. Pagnano
GENERAL OBSERVATIONS REGARDING SKIN INCISION
Whenever possible an anterior midline incision should be
used for extensive operations that involve the knee joint itself. By
extending the skin incision proximally or distally and developing full
thickness skin flaps it is possible to reach anterior, medial, and
lateral sided structures around the knee. Many patients who require an
open operation on the knee as young adults ultimately come to require
total knee arthroplasty and the utility of the anterior midline
incision should be remembered. If an incision is made medially or
laterally it should be far from the midline such that a substantial
skin bridge (≥7 cm) is present to accommodate a subsequent anterior
midline incision. Rarely today should a surgeon choose to make an
oblique or sharply angled incision around the knee as such incisions
are difficult to accommodate should future surgery, such as total knee
arthroplasty, be required.
used for extensive operations that involve the knee joint itself. By
extending the skin incision proximally or distally and developing full
thickness skin flaps it is possible to reach anterior, medial, and
lateral sided structures around the knee. Many patients who require an
open operation on the knee as young adults ultimately come to require
total knee arthroplasty and the utility of the anterior midline
incision should be remembered. If an incision is made medially or
laterally it should be far from the midline such that a substantial
skin bridge (≥7 cm) is present to accommodate a subsequent anterior
midline incision. Rarely today should a surgeon choose to make an
oblique or sharply angled incision around the knee as such incisions
are difficult to accommodate should future surgery, such as total knee
arthroplasty, be required.
STANDARD MEDIAL PARAPATELLAR ARTHROTOMY
Indications
The medial parapatellar arthrotomy has long been the
standard arthrotomy for total knee arthroplasty. Modifications of this
approach are useful for a variety of procedures including
intramedullary nailing of the tibia and articular cartilage transplant.
standard arthrotomy for total knee arthroplasty. Modifications of this
approach are useful for a variety of procedures including
intramedullary nailing of the tibia and articular cartilage transplant.
Position
Supine.
Technique
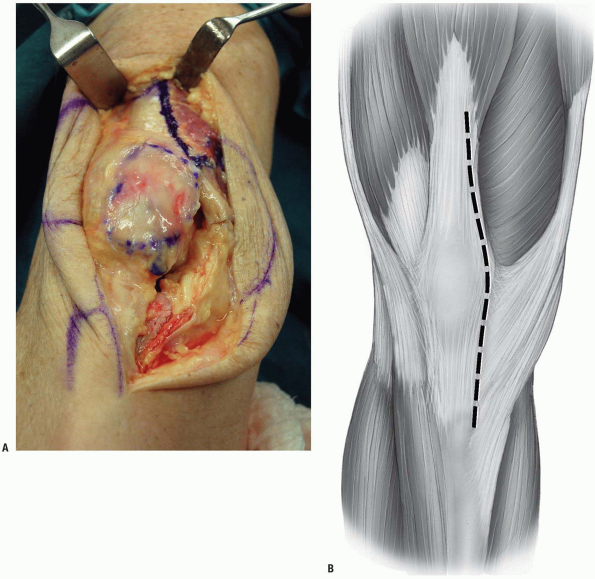
1. Incision: the extensor mechanism is exposed through an anterior midline incision.
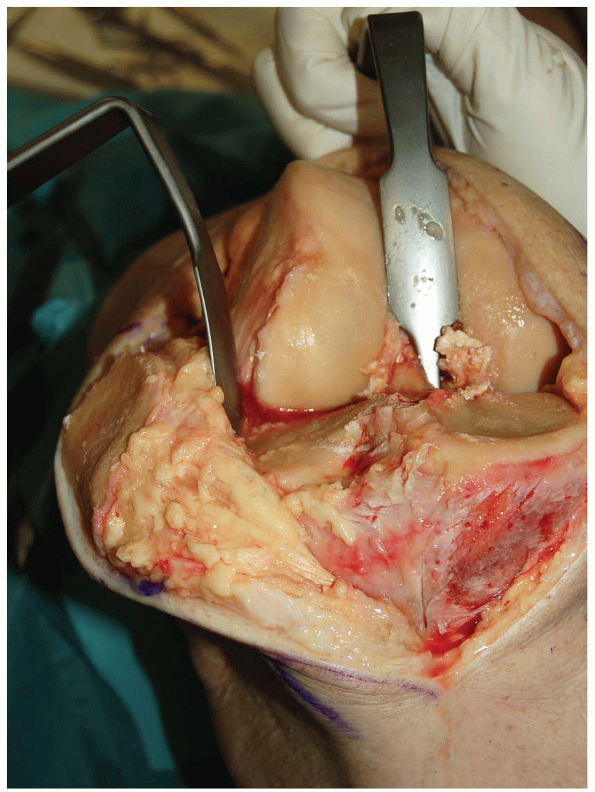
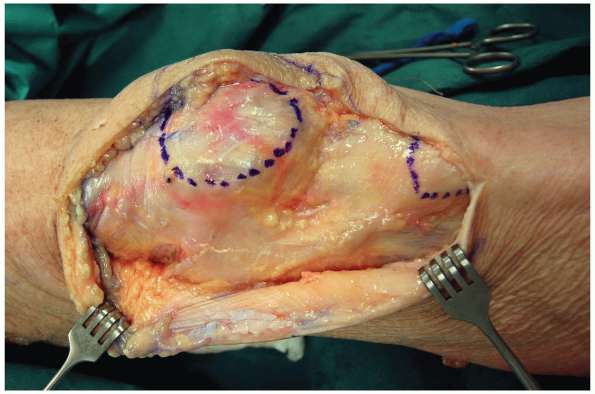
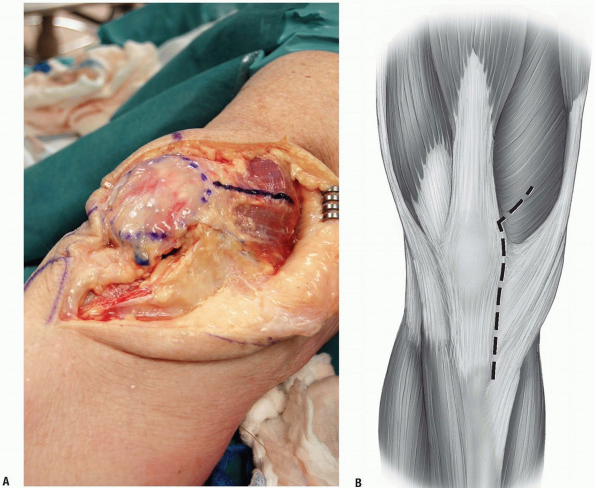
2. The extensor mechanism is exposed both proximally and
distally by developing moderate skin flaps. The arthrotomy parallels
the medial border of the patellar tendon beginning at the insertion of
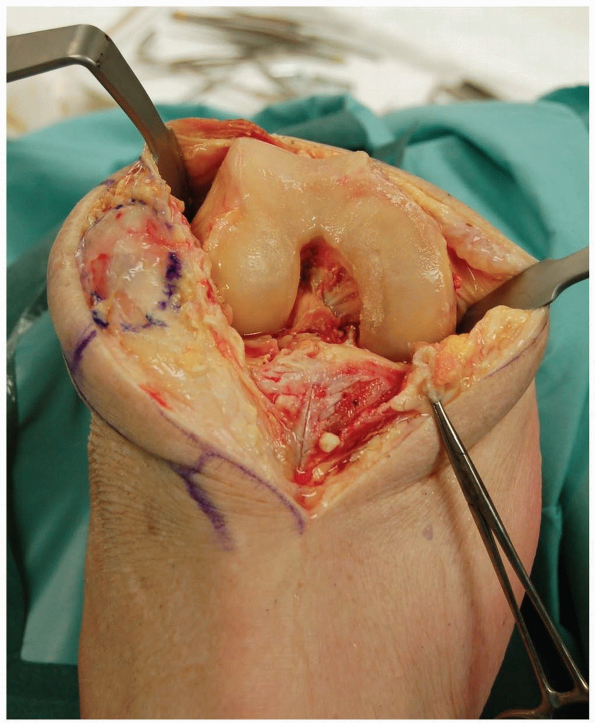
the pes anserine tendons (Fig. 9-1).
distally by developing moderate skin flaps. The arthrotomy parallels
the medial border of the patellar tendon beginning at the insertion of
the pes anserine tendons (Fig. 9-1).
3. The arthrotomy is continued along the medial border
of the patella where most surgeons leave a 1 cm sleeve of soft tissue
attached to the patella in order to facilitate later closure.
of the patella where most surgeons leave a 1 cm sleeve of soft tissue
attached to the patella in order to facilitate later closure.
-
Note: Some surgeons prefer the technique popularized by Insall
where the arthrotomy is carried over the medial edge of the patella
itself as that approach improves visualization of the medial border of
the patella for patellar resurfacing.
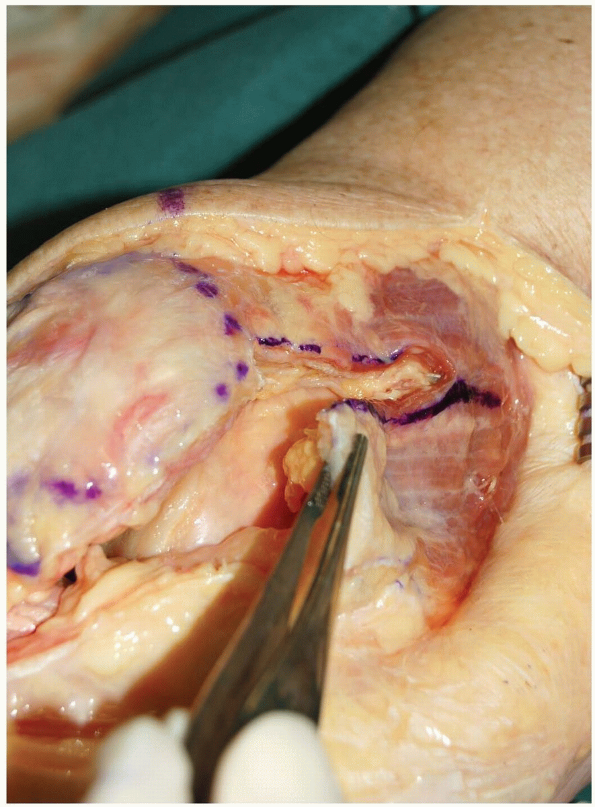
The quadriceps tendon is divided for a distance of 8 cm above the superior pole of the patella (Fig. 9-2).
P.192
 |
|
FIGURE 9-1
|
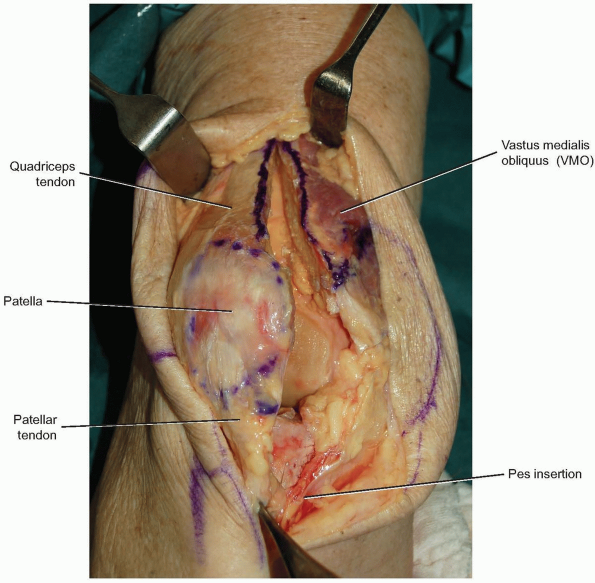
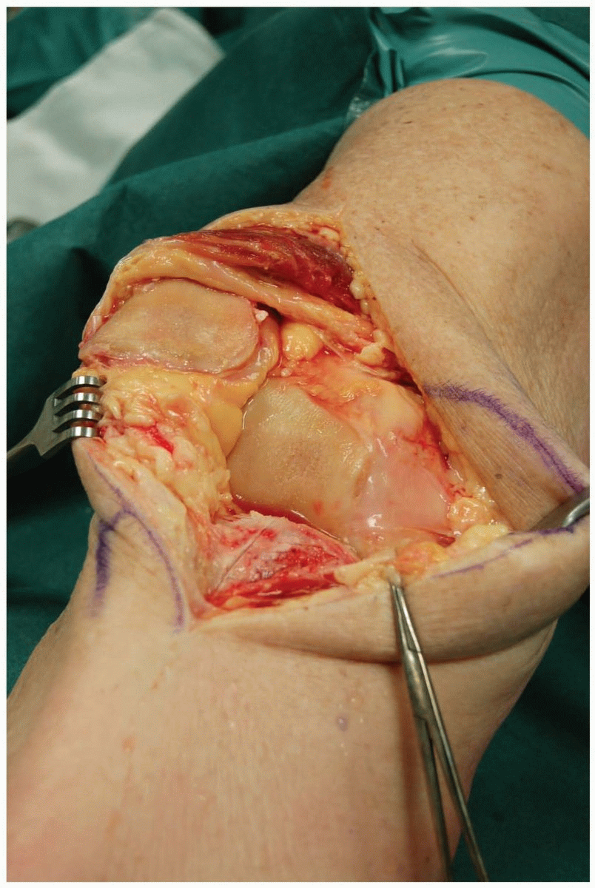
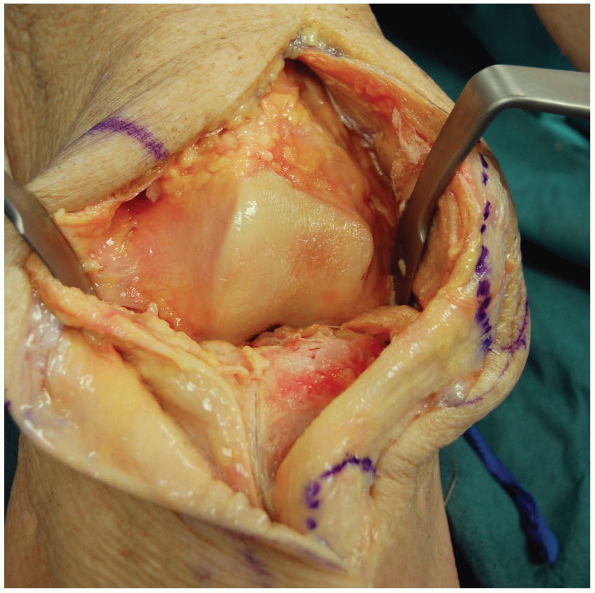
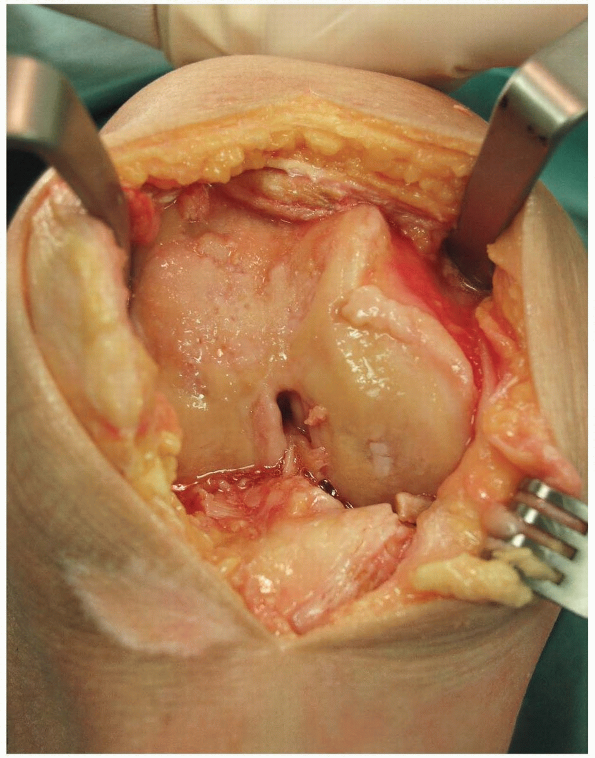
4. Most surgeons leave a small cuff of tendon medially
(1 to 2 cm) with the vastus medialis and the great preponderance of the
tendon in continuity laterally with the rectus femoris and the vastus
lateralis. The retropatellar fat pad is split, the patella is everted,
and the knee can be flexed (Fig. 9-3).
(1 to 2 cm) with the vastus medialis and the great preponderance of the
tendon in continuity laterally with the rectus femoris and the vastus
lateralis. The retropatellar fat pad is split, the patella is everted,
and the knee can be flexed (Fig. 9-3).
-
Note: An
everted patella puts the patellar tendon at risk for avulsion as the
tendon is apt to peel from its attachment to the tubercle. If excessive
tension is noted in the tendon, the patella should just be subluxed and
not everted or the exposure converted to a quadriceps snip.
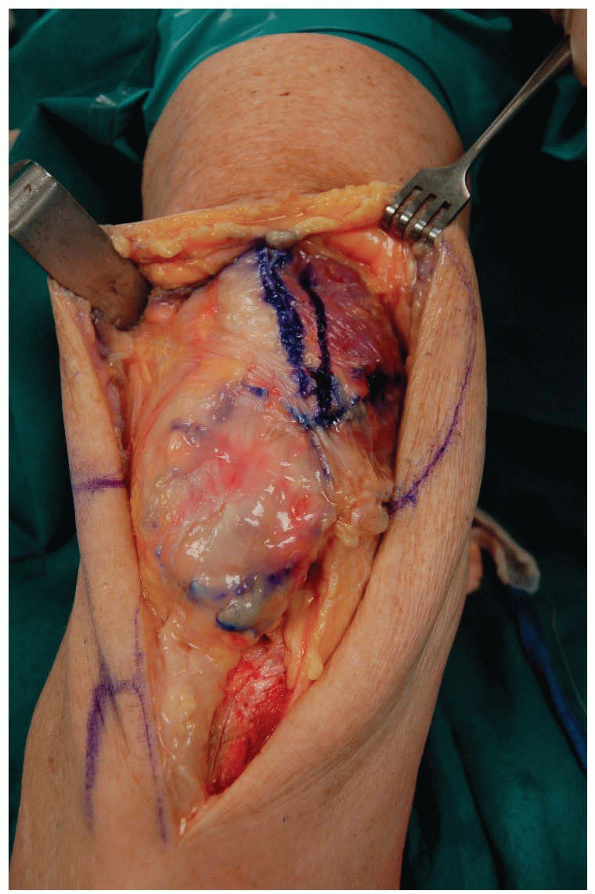
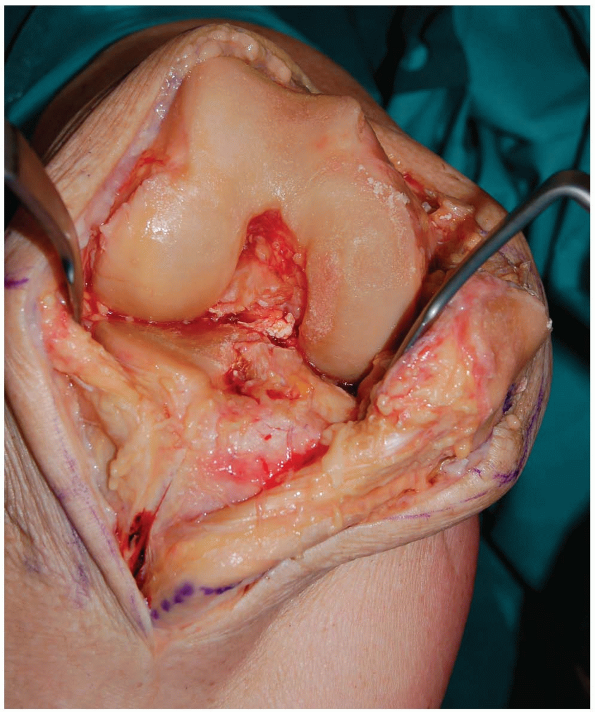
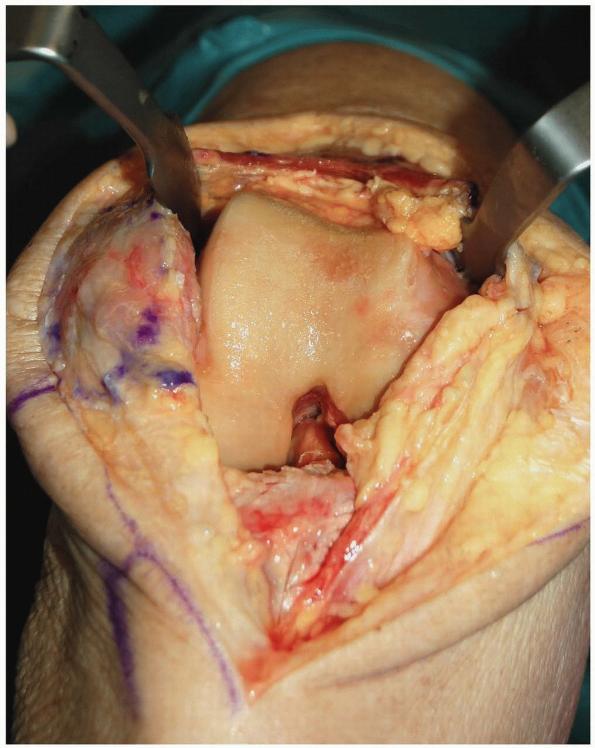
5. During total knee arthroplasty, a subperiosteal
release of the deep portion of the medial collateral ligament can be
carried out. As the knee is progressively flexed the tibia can be
rotated externally, the anterior cruciate ligament can be excised, and
the posteromedial corner of the tibia can be subluxed anterior to the
femur (Fig. 9-4).
release of the deep portion of the medial collateral ligament can be
carried out. As the knee is progressively flexed the tibia can be
rotated externally, the anterior cruciate ligament can be excised, and
the posteromedial corner of the tibia can be subluxed anterior to the
femur (Fig. 9-4).
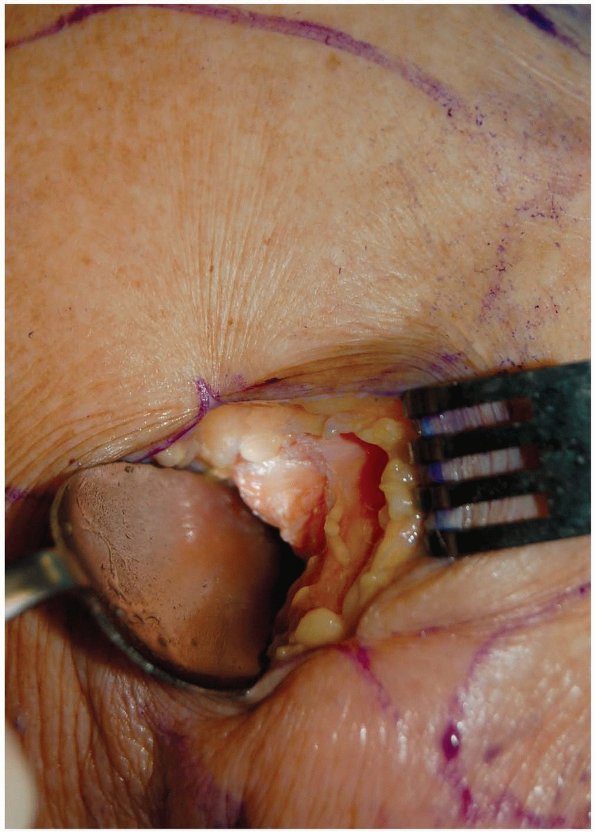
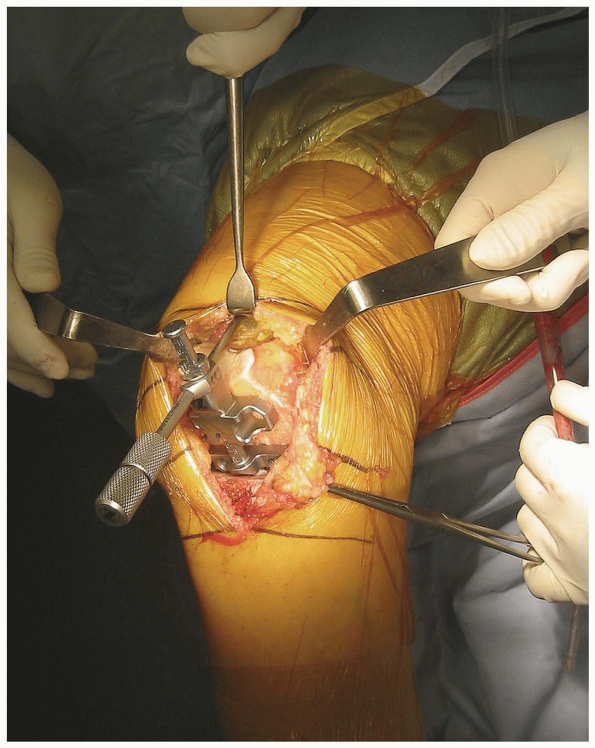
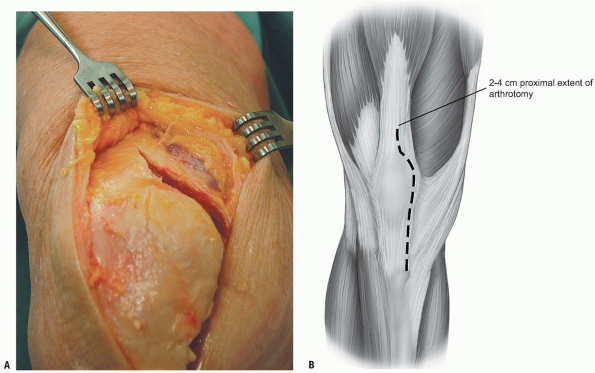
6. A retractor positioned around the tibial attachment
of the posterior cruciate ligament can lever the tibia forward and
improve visualization during resection of the proximal tibia (Fig. 9-5).
of the posterior cruciate ligament can lever the tibia forward and
improve visualization during resection of the proximal tibia (Fig. 9-5).
P.193
 |
|
FIGURE 9-2
|
 |
|
FIGURE 9-3
|
 |
|
FIGURE 9-4
|
 |
|
FIGURE 9-5
|
P.194
The Quadriceps Snip
In cases where there is excessive tension on the
patellar tendon when subluxing or everting the patella, it is useful to
perform a proximal quadriceps snip. This approach was introduced by Insall and is particularly useful in knees that are stiff from prior surgery.
patellar tendon when subluxing or everting the patella, it is useful to
perform a proximal quadriceps snip. This approach was introduced by Insall and is particularly useful in knees that are stiff from prior surgery.
-
A standard medial parapatellar arthrotomy is done.
-
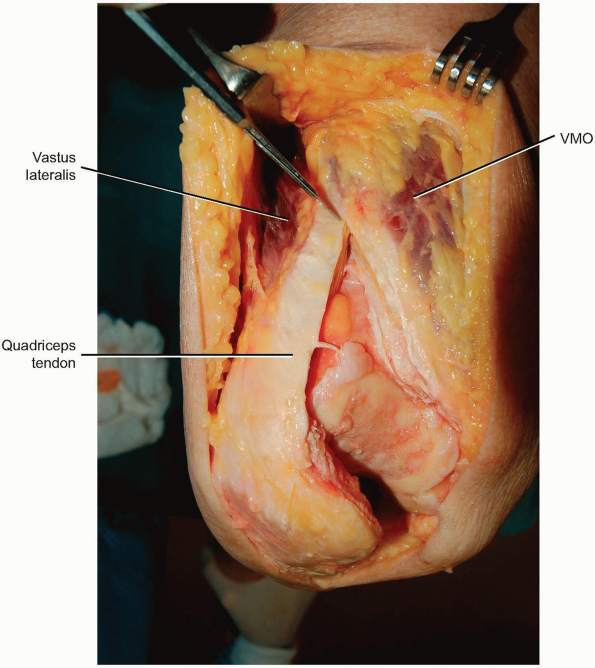
At the proximal portion of the split in
the quadriceps the arthrotomy is then extended proximally and laterally
across the remaining extensor mechanism and up into the muscle fibers
of the vastus lateralis (Fig. 9-6). -
The angle of the cut is the same as the
angle of insertion of the vastus lateralis fibers (60 degrees) such
that the quadriceps snip can extend itself further into the vastus
lateralis if needed (Fig. 9-7).-
Note: The
quadriceps snip is quite versatile. The vast majority of difficult
total knees and revision total knees can be done with a quadriceps snip
coupled with adequate debridement of scar tissue from the lateral
gutter and around the patella.
-
-
The arthrotomy can be closed with
multiple interrupted sutures and there is no need to alter the
patient’s weight-bearing status after using the quadriceps snip
exposure.
 |
|
FIGURE 9-6
|
P.195
 |
|
FIGURE 9-7
|
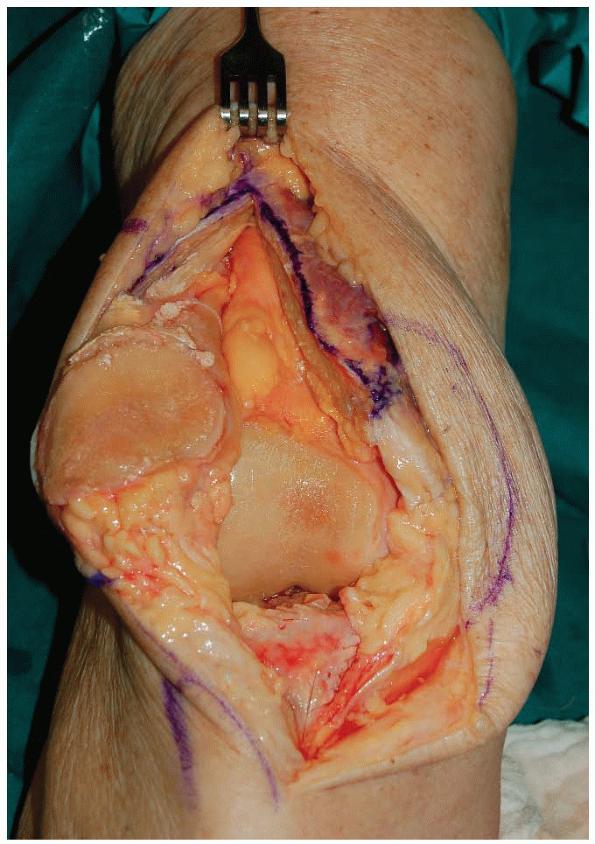
SUBVASTUS APPROACH
Indications
This approach can be used for routine total knee arthroplasty and medial unicompartmental knee arthroplasty.
Because it preserves the entire extensor mechanism’s
attachment on the patella, the subvastus approach has an anatomic edge
on other arthrotomies of the knee joint. Recent anatomic studies at the
Mayo Clinic have confirmed that the tendon of the vastus medialis
extends all the way to the midpole of the patella. Thus any arthrotomy
that extends proximal to the midpole disrupts part of the extensor
mechanism.
attachment on the patella, the subvastus approach has an anatomic edge
on other arthrotomies of the knee joint. Recent anatomic studies at the
Mayo Clinic have confirmed that the tendon of the vastus medialis
extends all the way to the midpole of the patella. Thus any arthrotomy
that extends proximal to the midpole disrupts part of the extensor
mechanism.
Technique
-
Incision: the standard subvastus approach is done through a midline incision.
-
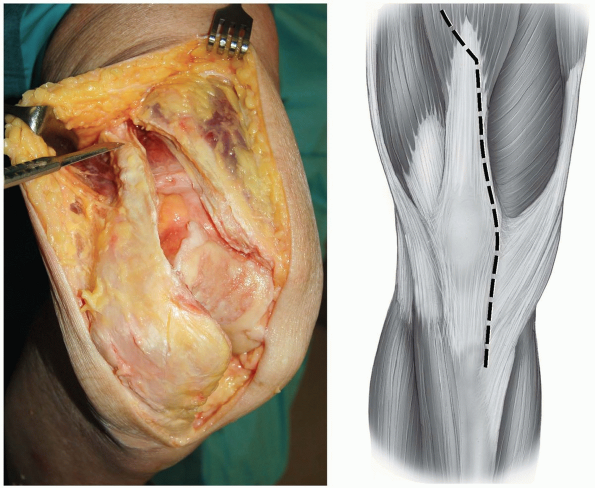
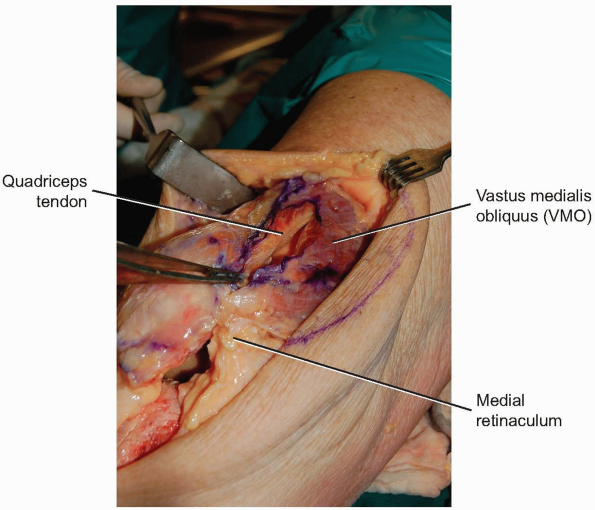
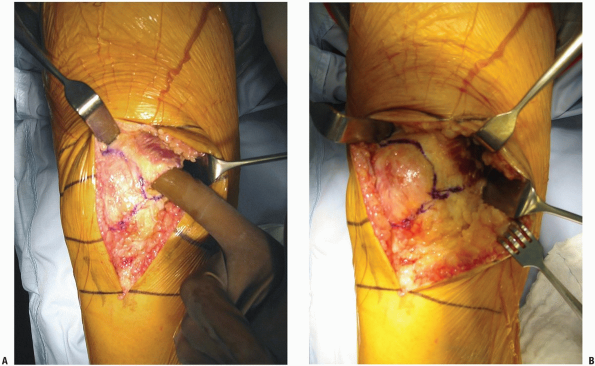
Care is taken to develop a medial skin flap to truly define the inferior border of the vastus medialis obliquus (VMO) (Fig. 9-8).
-
Note: The
VMO attaches to the patella at a 50 degree angle and always extends
more distally and more medially than the surgeon is inclined to think.
The subvastus arthrotomy is made by incising the retinaculum and joint
capsule at the VMO muscle edge from proximal to distal at the same 50
degree angle as the VMO itself. Care should be taken to extend the
arthrotomy to the midpole of the patella and not to cheat the
arthrotomy up toward the superior pole of the patella.
-
-
At the midpole of the patella the arthrotomy is turned distally and parallels the medial border of the patellar tendon (Fig. 9-9).
-
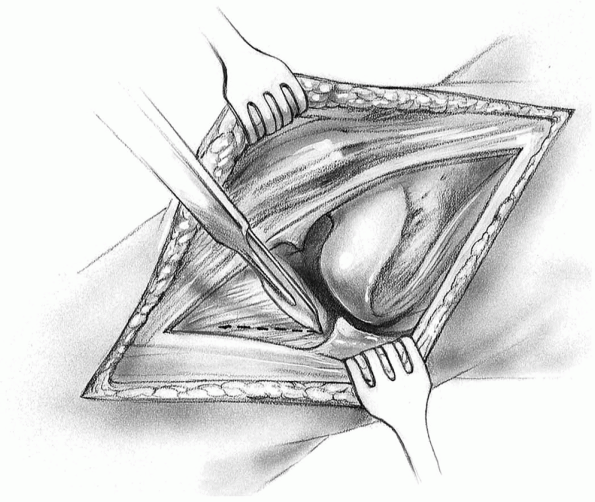
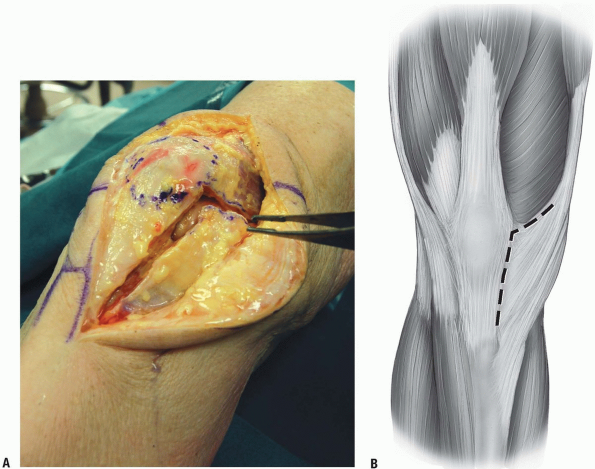
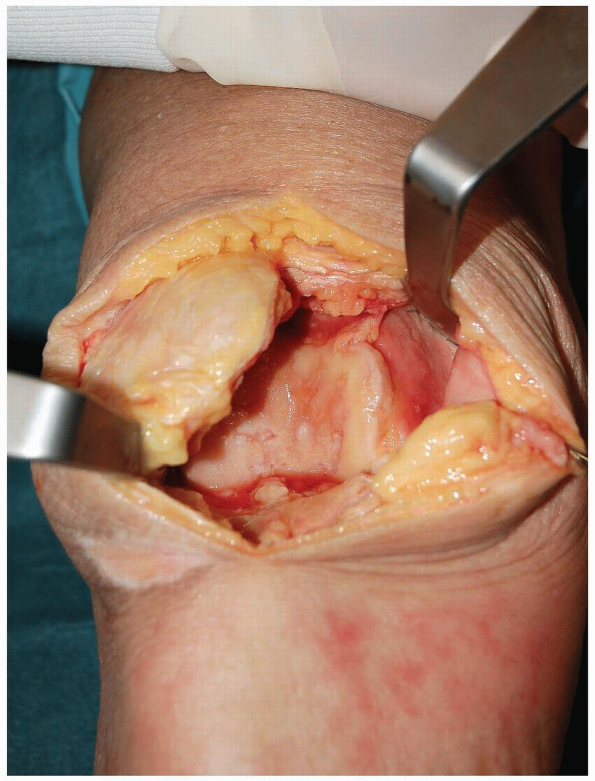
The fat pad is split and the patella can
be subluxed into the lateral gutter of the knee. In cases where the
patella is difficult to sublux laterally, the surgeon will usually find
a tight band of tissue proximal-medially (the medial patellofemoral
ligament) that must be released. Once the medial patellofemoral
ligament is released the patella will sublux laterally with relatively
little force (Fig. 9-10). -
If desired the patella can be everted at this stage and the knee flexed (Fig. 9-11).
-
Note:
Everting the patella is difficult in heavily muscled patients and
markedly obese patients. In those patients the patella should just be
subluxed into the lateral gutter. In patients with substantial patella
baja the subvastus approach is not recommended.
-
-
When closing the subvastus arthrotomy it
is useful to tension and tie the capsular sutures with the knee in 90
degrees of flexion to avoid overtightening the medial capsule.
P.196
 |
|
FIGURE 9-8
|
 |
|
FIGURE 9-9
|
P.197
 |
|
FIGURE 9-10
|
 |
|
FIGURE 9-11
|
P.198
 |
|
FIGURE 9-12
|
 |
|
FIGURE 9-13
|
TRIVECTOR RETAINING APPROACH
The trivector approach can be used for total knee and medial unicompartmental knee arthroplasty.
Technique
-
Incision: an anterior midline incision is made and the vastus medialis muscle and tendon are identified.
-
The knee is flexed to 90 degrees and,
beginning three finger-breadths proximal to the patella, the arthrotomy
is made from proximal to distal 2 cm medial to the quadriceps tendon (Fig. 9-12). -
This means the arthrotomy involves transection vastus medialis muscle fibers proximal and medial to the patella (Fig. 9-13).
-
The arthrotomy is extended distally along
the medial border of the patella and the medial edge of the patellar
tendon. The fat pad is split, the patella is everted with the knee in
extension, and then the knee can again be flexed. -
At the time of closure the surgeon will
see that the edge of the quadriceps tendon actually extends medially
under the cut muscle fibers of the vastus medialis. Thus there is
reasonable tissue through which to place sutures and close the joint
itself.
P.199
 |
|
FIGURE 9-14
|
 |
|
FIGURE 9-15
|
 |
|
FIGURE 9-16
|
LATERAL APPROACH FOR TOTAL KNEE ARTHROPLASTY IN THE VALGUS KNEE
Indications
For patients with substantial valgus deformity who require total knee arthroplasty some surgeons use an anterolateral approach.
Technique
-
Incision: an anterior midline incision is made and a skin flap is developed on the lateral side (Fig. 9-14).
-
The quadriceps tendon is divided
beginning 6 to 8 cm above the superior pole of the patella. Most
surgeons leave a small cuff of quadriceps tendon laterally (1 to 2 cm)
with the vastus lateralis and the great preponderance of the tendon in
continuity medially with the rectus femoris and the vastus medialis. -
The arthrotomy is continued along the
lateral border of the patella leaving a 1 cm sleeve of soft tissue
attached to the patella in order to facilitate later closure (Fig. 9-15). -
Distally the arthrotomy parallels the
patellar tendon. The patella can be subluxed medially or everted
medially and the knee flexed, but each of those maneuvers is more
difficult than with a standard medial parapatellar arthrotomy (Fig. 9-16).
P.200
 |
|
FIGURE 9-17
|
 |
|
FIGURE 9-18
|
LIMITED MEDIAL APPROACH TO THE KNEE FOR ARTHROSCOPIC MENISCAL REPAIR
Indications
Exposure of the posteromedial corner of the knee is needed for arthroscopic inside-out suture repair of medial meniscal tears.
Technique
-
Insertion: the knee is flexed 90 degrees
and the arthroscope can be advanced to light the posteromedial corner
of the knee just posterior to the medial collateral ligament. If the
operating room lights are dimmed, it is possible to transilluminate the
skin at the level where the incision should be made. -
A short (3 to 4 cm) vertical incision is made (Fig. 9-17). Care is taken to avoid damage to the saphenous nerve and vein.
-
The fascia along the superior border of
the sartorius is divided and blunt finger dissection is carried out to
expose the posteromedial joint capsule itself. -
A simple retractor made from a tablespoon
with its handle bent 120 degrees can be placed against the
posteromedial corner of the knee to catch and deflect the flexible
needles used to carry out the inside-out meniscal repair (Fig. 9-18).
P.201
LIMITED LATERAL APPROACH TO THE KNEE FOR ARTHROSCOPIC MENISCAL REPAIR
Indications
Exposure of the posterolateral corner of the knee is needed for arthroscopic inside-out suture repair of lateral meniscal tears.
Technique
-
Insertion: the knee is flexed 90 degrees
and the arthroscope can be advanced to light the posterolateral corner
of the knee just posterior to the lateral collateral ligament and
anterior to the popliteus tendon. -
If the operating room lights are dimmed
it is possible to transilluminate the skin at the level where the
incision should be made. -
A short (3 to 4 cm) vertical incision is made (Fig. 9-19). The fibular collateral ligament is identified and the posterolateral capsule and arcuate ligament complex lie just posterior.
-
A simple retractor made from a tablespoon
with its handle bent 120 degrees can be placed against the
posterolateral corner of the knee to catch and deflect the flexible
needles used to carry out the inside-out meniscal repair (Fig. 9-20).
 |
|
FIGURE 9-19
|
 |
|
FIGURE 9-20
|
P.202
MINIMALLY INVASIVE APPROACHES FOR TOTAL KNEE ARTHROPLASTY
There has been considerable interest among patients and
surgeons alike in minimally invasive approaches for total knee
arthroplasty. The exact definition of minimally invasive total knee
arthroplasty continues to be debated but most would agree that it
involves a short skin incision, avoiding eversion of the patella, and
limiting the amount of surgical dissection in the suprapatellar pouch.
Alteration of the surgical approach alone however is not enough for
intraoperative success and, thus, manufacturers have introduced
modified or new instruments for minimally invasive total knee
arthroplasty. Patients who have had prior open knee surgery, who have
patella baja, who have a very stiff knee, or who have poor skin quality
are not good candidates for a minimally invasive total knee
arthroplasty approach. Most surgeons would be well served to pursue
specialized cadaver training before using minimally invasive total knee
arthroplasty approaches in clinical practice.
surgeons alike in minimally invasive approaches for total knee
arthroplasty. The exact definition of minimally invasive total knee
arthroplasty continues to be debated but most would agree that it
involves a short skin incision, avoiding eversion of the patella, and
limiting the amount of surgical dissection in the suprapatellar pouch.
Alteration of the surgical approach alone however is not enough for
intraoperative success and, thus, manufacturers have introduced
modified or new instruments for minimally invasive total knee
arthroplasty. Patients who have had prior open knee surgery, who have
patella baja, who have a very stiff knee, or who have poor skin quality
are not good candidates for a minimally invasive total knee
arthroplasty approach. Most surgeons would be well served to pursue
specialized cadaver training before using minimally invasive total knee
arthroplasty approaches in clinical practice.
Mini Subvastus Approach
Indications
The minimally invasive subvastus approach provides good
exposure of both condyles, preserves the entire extensor insertion on
the patella, is made easier by avoiding patellar eversion, and allows
rapid and reliable knee joint closure.
exposure of both condyles, preserves the entire extensor insertion on
the patella, is made easier by avoiding patellar eversion, and allows
rapid and reliable knee joint closure.
-
Comment: As
in all minimally invasive techniques, retractor placement and leg
position are important in facilitating visualization throughout the
procedure. Surgeons can learn this technique in a step-wise fashion by
making a standard incision using the subvastus exposure without
everting the patella and then gradually decreasing incision size over
time.
Technique
-
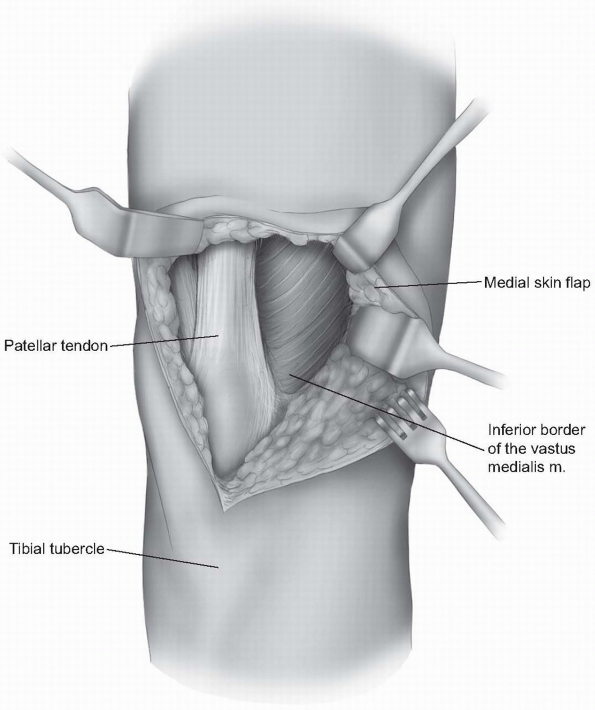
Incision: an anterior midline incision is made from the superior pole of the patella to the top of the tibial tubercle (Fig. 9-21).
-
A medial skin flap is raised and the inferior border of the vastus medialis muscle is identified (Fig. 9-22).
-
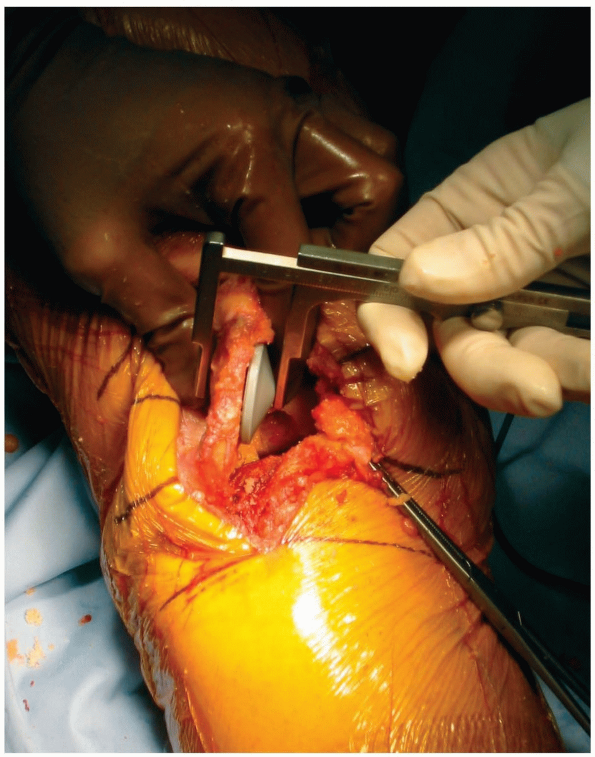
Beginning 5 to 8 cm medial to the patella
border, the fascia is incised at the inferior border of the vastus
medialis and the arthrotomy is continued over to the midpole of the
patella at a 50 degree angle paralleling the angle of insertion of the
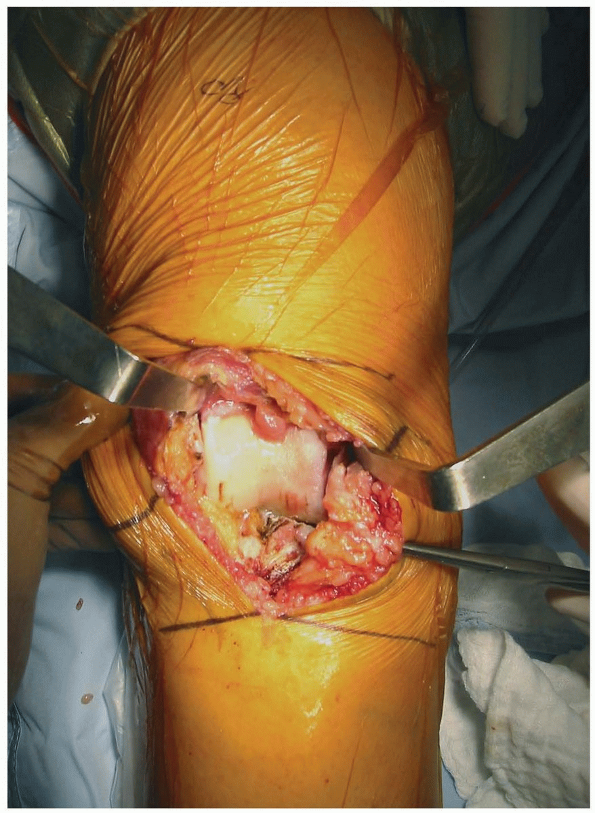
vastus medialis muscle fibers (Fig. 9-23). -
Care must be taken to preserve the
triangle of tendon that inserts down to the midpole of the patella as
this is where the retractor will rest. If the tendon is not preserved,
the retractor will slide proximally and macerate the vastus medialis
obliquus muscle itself. The distal portion of the arthrotomy parallels
the patellar tendon. -
A 90 degree bent Homan retractor is
placed into the lateral gutter of the knee and the patella and distal
portion of the extensor mechanism are retracted with relatively little
tension on the vastus muscle itself (Fig. 9-24). -
The patella is not everted. Another bent
Homan retractor is placed medially and the knee can be flexed to expose
both femoral condyles simultaneously and the distal femur is cut. -
The proximal tibia is exposed with
subperiosteal elevation of the deep medial collateral ligament and then
bent Homans are placed medially and laterally against the tibia and a
pickle-fork retractor is placed posteriorly around the posterior
cruciate ligament (PCL) attachment levering the tibia forward (Fig. 9-25). -
The tibia is cut and that then provides
more working room for sizing and rotating the femur (typically the most
difficult part of any minimally invasive total knee procedure) (Fig. 9-26). -
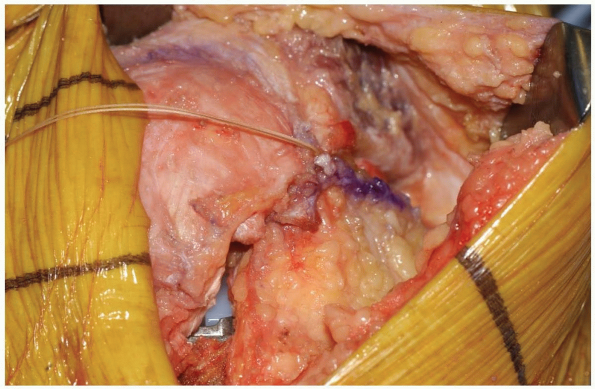
After the femoral cuts are made, a
laminar spreader is placed in the flexion space and the notch
osteophytes, cruciate ligament(s), medial and lateral menisci, and
posterior osteophytes can be excised under direct vision. The trial
components can be assembled and the knee reduced. -
The patella is then turned up 90 degrees but not everted and cut from medial to lateral for patellar resurfacing (Fig. 9-27).
-
Cementing is done first on the tibial
tray, then femur, insertion of the tibial polyethylene, and finally the
patella. The tourniquet is let down and the subvastus space is
specifically examined to ensure there are no bleeders. -
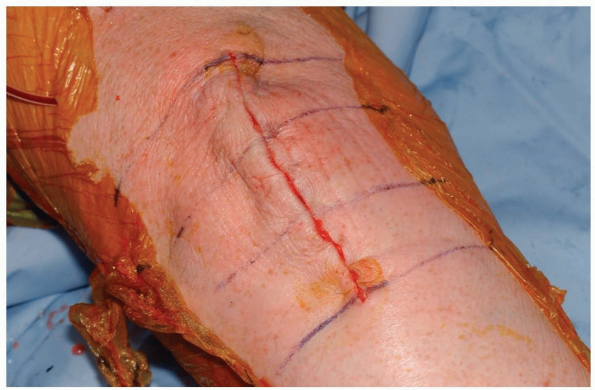
The arthrotomy is closed with multiple
interrupted sutures and it is useful to tension and tie these sutures
with the knee in 90 degrees of flexion to avoid overtightening the
medial capsule (Fig. 9-28). The wound is closed in layers (Fig. 9-29).
P.203
 |
|
FIGURE 9-21
|
 |
|
FIGURE 9-22
|
P.204
 |
|
FIGURE 9-23
|
 |
|
FIGURE 9-24
|
 |
|
FIGURE 9-25
|
P.205
 |
|
FIGURE 9-26
|
 |
|
FIGURE 9-27
|
 |
|
FIGURE 9-28
|
 |
|
FIGURE 9-29
|
P.206
Mini Midvastus Approach
Technique
-
Incision: a midline incision is made from the superior pole of the patella to the midpoint of the tibial tubercle distally.
-
A medial arthrotomy is begun distally 5
mm medial to the tibial tubercle and extended proximally just medial to
the patellar border (Fig. 9-30). -
At the superomedial corner of the patella
the arthrotomy is turned proximal-medially and a 2 cm split is made
between the muscle fibers of the vastus medialis (Fig. 9-31). -
The patella is retracted laterally with a
bent Homan but not everted, the fat pad is excised, and the anterior
horns of the medial and lateral menisci are incised (Fig. 9-32). -
The distal femur is prepared with the leg
in 70 to 90 degrees of flexion. The anteroposterior axis of the knee as
described by Whitesides is used to assess femoral rotation. -
The distal cutting guide is placed and
the cut made. The femur is then sized, with variations in knee flexion
angle needed to accommodate the guide, and the finishing cuts are made. -
The tibia is exposed with bent Homan
retractors placed medially and laterally at the tibial margins and a
posterior retractor is used to lever anteriorly. -
A tibial cutting guide specifically
modified for small incision surgery is of great assistance here. The
lateral portion of the tibia is the most difficult to cut safely and a
narrow saw blade is useful in maneuvering around the patellar tendon. -
After removing the proximal tibial
fragment a laminar spreader can be placed in the flexion space and the
osteophytes, cruciate ligaments, and posterior menisci removed under
direct vision. -
The trial components are assembled and the knee reduced.
-
The patella is prepared last. Cementing is done first on the tibia followed by the femur and then the patella.
P.207
 |
|
FIGURE 9-30
|
 |
|
FIGURE 9-31
|
 |
|
FIGURE 9-32
|
P.208
Mini Medial Parapatellar Approach
Indications
The mini medial parapatellar approach has the advantage
that it can be quickly converted to a standard medial parapateller
approach at any time. The indications are similar to the other
mini-incision approaches for total knee arthroplasty.
that it can be quickly converted to a standard medial parapateller
approach at any time. The indications are similar to the other
mini-incision approaches for total knee arthroplasty.
Technique
-
Incision: a midline or slightly medially
biased incision is made from the just above the superior pole of the
patella to the top of the tibial tubercle. -
The medial parapatellar arthrotomy is
done similar to the standard parapatellar approach except that the
proximal extent of the quadriceps tendon incision is only 2 to 4 cm
(versus the 8 to 10 cm in the standard approach) (Fig. 9-33).-
Note: If there is difficulty subluxing the patella laterally then the arthrotomy is extended more proximally.
-
-
Modified instruments are used to make the
bone cuts according to the surgeon’s normal sequence. Some prefer to
cut the tibia first and that can be done with this approach. -
There is adequate exposure to safely cut
the tibia with bent Homan retractors placed medially and laterally to
protect the collateral ligaments and a pickle-fork retractor placed
posteriorly. -
Cutting the tibia first provides more working room in both flexion and extension for the remainder of the procedure.
-
The exposure exists to reference the anteroposterior axis and the posterior condyles for rotational positioning of the femur (Fig. 9-34).
-
The epicondylar axis can be identified
after appropriate retractor placement. Appropriate soft tissue
balancing is done and the trial components are assembled. -
The patella can be prepared by turning
the patella up 90 degrees and cutting from medial to lateral or by
everting the patella with the knee in full extension after the trial
components have been removed. -
Typically the tibia is cemented first followed by the femur and patella.
-
Note: In
all of the mini total knee approaches the surgeon should specifically
look for retained cement laterally around both the femoral and tibial
components before closing. That area often is obscured when the patella
is subluxed and not everted.
-
P.209
 |
|
FIGURE 9-33
|
 |
|
FIGURE 9-34
|
P.210
Alternative
-
An even more limited medial parapatellar
exposure has been used by some surgeons with the arthrotomy stopping at
the superior pole of the patella (Fig. 9-35).
That approach has been given the trademarked term quad-sparing because
it does involve the detachment of the vastus medialis obliquus tendon
which inserts along the medial patella from the superior pole to the
midpole. -
That approach affords the poorest visualization of any of the minimally invasive approaches for total knee arthroplasty (Fig. 9-36).
-
Note:
Because of that limited visualization the procedure must be carried out
with instruments that cut from medial to lateral and demands partial
cuts through resection guides followed by free-hand finishing cuts. In
addition, the patella must be cut first with this approach raising the
possibility of inadvertent damage to the cut patellar surface from
poorly placed retractors.
-
 |
|
FIGURE 9-35
|
 |
|
FIGURE 9-36
|
P.211
Mini Lateral Approach
Technique
-
Incision: an 8 to 10 cm incision is made from just below Gerdy’s tubercle and extends proximally to the lateral epicondyle.
-
The iliotibial band is split in line with
the skin incision and then elevated from Gerdy’s tubercle to allow
exposure of the proximal tibia. The fat pad and the anterior horn of
the lateral meniscus are excised. -
A retractor is placed across the knee
joint to retract the patellar tendon anteromedially and allow the
anterior horn of the medial meniscus to be excised. -
The synovium overlying the distal
anterior femur is removed and the patella is mobilized medially.
Specialized cutting guides are required to allow cutting in a lateral
to medial direction. -
The distal femur is resected first.
-
The tibia is cut next and that is done
with a partial cut through the resection guide followed by a free-hand
finishing cut. The femur is then sized and the femoral finishing guide
is rotated relative to the anteroposterior axis. The notch osteophytes,
anterior cruciate ligament, meniscal remnants, and posterior
osteophytes are excised and the trial components inserted. -
The patella is turned up 90 degrees and cut from lateral to medial.
-
Cementing of the tibia is done first
followed by the femur and patella. Care is taken to look for excess
cement medially after this approach.
EXTENSILE LATERAL APPROACH TO THE KNEE FOR POSTEROLATERAL CORNER RECONSTRUCTION
Indications
Wider exposure of the posterolateral corner of the knee
is required for repair or reconstruction of the stabilizing ligamentous
and capsular structures of the posterolateral corner.
is required for repair or reconstruction of the stabilizing ligamentous
and capsular structures of the posterolateral corner.
Technique
-
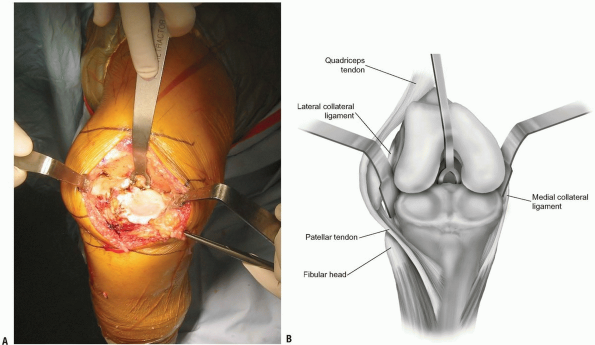
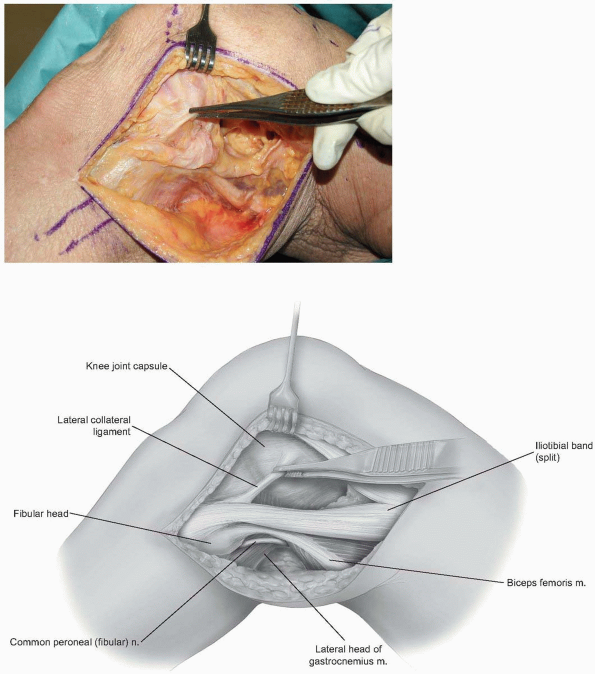
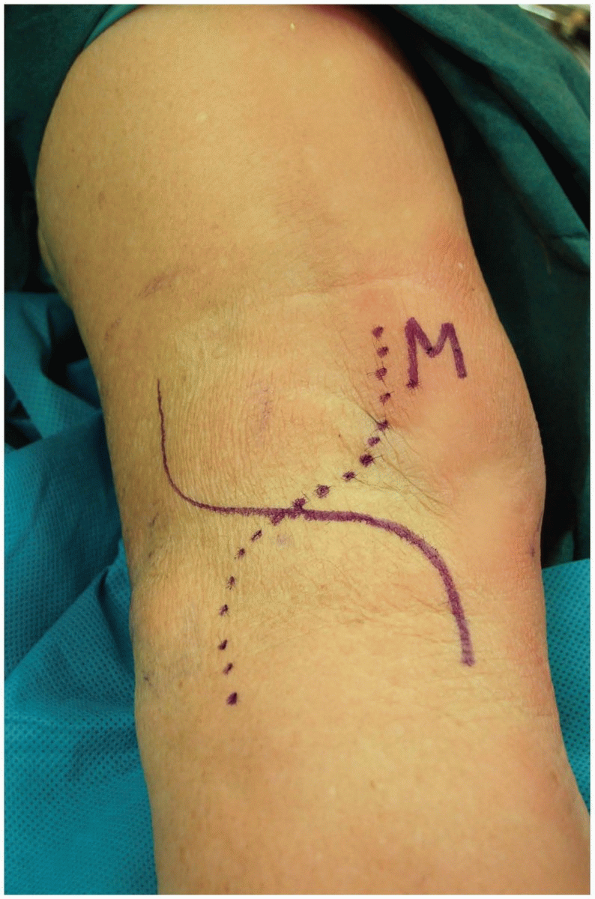
Incision: the skin incision follows the
posterior 10% of the iliotibial band proximally and extends between the
fibular head and Gerdy’s tubercle distally (Fig. 9-37). -
The iliotibial band is split
longitudinally to allow access to the lateral collateral and popliteus
insertion sites at the lateral epicondyle (Fig. 9-38). -
The biceps tendon is identified as is the
peroneal nerve which runs just posterior to that tendon. The posterior
corner of the knee is readily assessed.
P.212
 |
|
FIGURE 9-37
|
 |
|
FIGURE 9-38
|
P.213
POSTERIOR APPROACH TO THE POPLITEAL FOSSA AND POSTERIOR CRUCIATE LIGAMENT ORIGIN
Indications
The posterior approach allows access to the
neurovascular structures of the popliteal fossa and direct
visualization of the posterior cruciate ligament’s tibial attachment
site.
neurovascular structures of the popliteal fossa and direct
visualization of the posterior cruciate ligament’s tibial attachment
site.
Technique
-
Incision: an S-shaped incision is used to cross the flexion crease (Fig. 9-39).
-
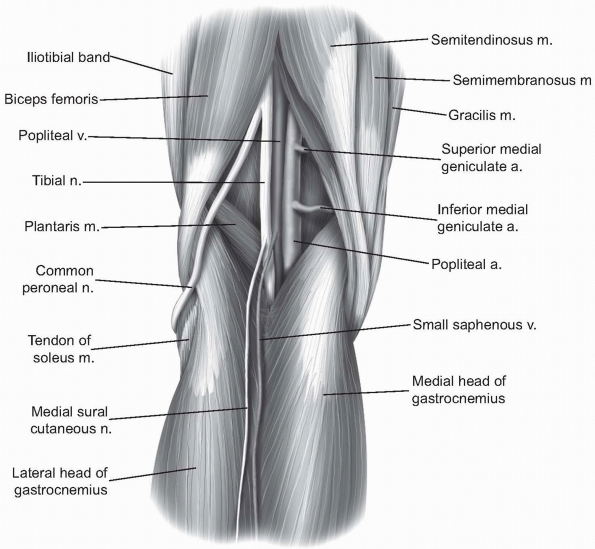
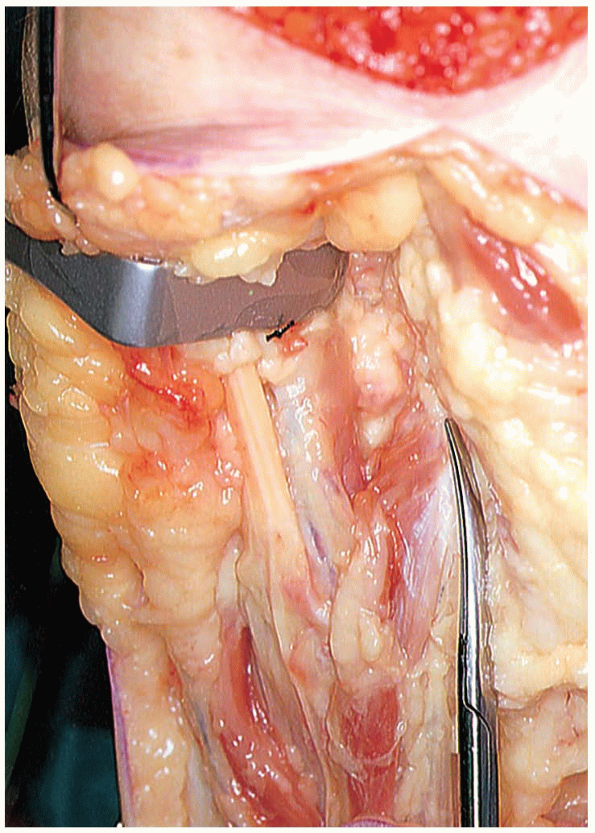
The fascia overlying the popliteal fossa is incised, exposing the neurovascular bundle (Fig. 9-40).
-
In the midline is the small saphenous
vein which is often found in association with the medial sural
cutaneous nerve which can be followed back to the tibial nerve. The
popliteal artery and vein will lie deep to the tibial nerve. The
scissors mark the medial head of the gracilis medius (Fig. 9-41). -
The neurovascular structures can be retracted laterally to allow direct access to the posterior aspect of the knee (Fig. 9-42).
-
Alternatively, when approaching the
tibial attachment of the posterior cruciate ligament, the dissection
can begin medial to the medial head of the gastrocnemius muscle. -
The medial gastrocnemius is then
retracted laterally past the midline allowing exposure of the tibial
attachment of the posterior cruciate while also protecting the
neurovascular structures.
 |
|
FIGURE 9-39
|
 |
|
FIGURE 9-40
|
P.214
 |
|
FIGURE 9-41
|
 |
|
FIGURE 9-42
|
RECOMMENDED READING
Bezwada
HP, Mont MA, Bonutti PM, et al. Minimally invasive lateral approach to
total knee arthroplasty. In: Berger RA, Scuderi GR, Tria AJ, eds. MIS Techniques in Orthopedics. New York: Springer, 2006.
HP, Mont MA, Bonutti PM, et al. Minimally invasive lateral approach to
total knee arthroplasty. In: Berger RA, Scuderi GR, Tria AJ, eds. MIS Techniques in Orthopedics. New York: Springer, 2006.
Boerger TO, Aglietti P, Mondanelli N, et al. Mini-subvastus versus medial parapatellar approach in total knee arthroplasty. Clin Orthop Relat Res 2005;440:82-87.
Buechel FF. Lateral approach. In: Lotke PA, ed. Master Techniques in Orthopedic Surgery: Knee Arthroplasty. New York: Raven Press, 1995.
Hoffman AA, Plaster RI, Murdock LE. Subvastus approach for primary total knee arthroplasty. Clin Orthop 1991;269:70.
Fisher DA, Trimble SM, Breedlove K. The medial trivector approach in total knee arthroplasty. Orthopedics 1998;21(1):53-56.
Garvin KL, Scuderi GR, Insall JN. Evolution of the quadriceps snip. Clin Orthop Relat Res 1995;321:131-137.
Insall JN. A midline approach to the knee. J Bone Joint Surg 1971;53-A;1584-1586.
Jacob RP. The arthroscopic meniscal repair: Techniques and clinical experience. Am J Sports Med 1991;16:137-141.
Laskin
RS, Beksac B, Phongjunakorn A, et al. Minimally invasive total knee
replacement through a mini-midvastus incision: an outcome study. Clin Orthop 2004;428:74-81.
RS, Beksac B, Phongjunakorn A, et al. Minimally invasive total knee
replacement through a mini-midvastus incision: an outcome study. Clin Orthop 2004;428:74-81.
Roysam GS, Oakley MJ. Subvastus approach for total knee arthroplasty: a prospective randomized and observer blinded trial. J Arthroplasty 2001;16:454-457.
Scuderi GR, Tenholder M, Capeci C. Surgical approaches in mini-incision total knee arthroplasty. Clin Orthop Relat Res 2004;428:61-67.
