Miscellaneous Disorders of the Hip Joint
– HIP > Part B – Evaluation and Treatment of Hip Disorders > 7 –
Miscellaneous Disorders of the Hip Joint
hip is lengthy. This section addresses some of the unique and more
troublesome problems. Patients can present with symptoms of pain and
functional loss or may simply present with a radiographic abnormality
discovered incidentally (Table 7-1). Some of
these problems are rare and can be difficult to treat. Some disorders
have characteristic radiographic features that can be diagnostic (Table 7-1).
uncommon disorder characterized by an effusion, thickened hyperplastic
synovium with joint erosions and cysts. It can present with an
insidious onset, and the ultimate diagnosis can be difficult to make as
it may mimic other inflammatory disorders. Patients who present with a
nontraumatic monoarticular effusion should be suspected of having PVNS.
disorder is the result of a true neoplastic process or whether it is
merely a reactive monoarticular arthritis. The fact that it is
monoarticular supports the concept that it is a neoplastic disease.
Although rare, polyarticular disease can occur.
common in the third to fifth decade of life. The incidence of this
disorder is 1.5 per million; it most commonly affects the knee, hip,
ankle, hand, and foot.
is blood tinged and the synovium is thickened, nodular, and stained
reddish brown with yellow nodules. Histologically, there is a
mononuclear stromal cell infiltrate with multinucleated giant cells and
foamy histiocytes and there are areas of macrophages containing
hemosiderin.
arthritis. The classic radiographic changes that are present include
bone erosions in the head and neck of the femur and the acetabulum. The
MRI typically shows an effusion with hypertrophic synovium with areas
of low signal on T1 and bright areas on T2. Because of the hemosiderin
present, there will be other small areas of low signal intensity of T1-
and T2-weighted images.
differential diagnosis may include infection or other inflammatory
arthritis and an aspiration may be appropriate. Histologic changes from
other inflammatory arthritis disorders can often mimic PVNS,
particularly if there have been recurrent hemarthroses; thus this
condition is often overdiagnosed on pathology reports.
Attempts at radionucleotide synovectomy have been disappointing. The
surgical recurrence rate is high, especially with the diffuse form;
therefore, thorough synovectomy, curettage of the cystic lesions, and
bone grafting of cavitary defects must be meticulously performed. To
visualize the joint completely, the hip must be dislocated. Surgical
dislocation of the hip is safe, and the risk of avascular necrosis is
very low if the procedure is done correctly. I prefer a
classic
trochanteric slide osteotomy. Care is taken to avoid dissection of any
of the posterior capsular structures. The anterior hip capsule is
exposed, and an arthrotomy is made in line with the femoral neck. Flaps
are then created at the base of the neck toward the lesser trochanter
anteriorly and posteriorly along the superior aspect of the capsule
just distal to the labrum. A Z-shaped capsular arthrotomy now permits
an anterior dislocation of the hip. The ligamentum teres is avulsed or
transected, and the dislocation is complete. Adequate visualization now
permits a complete synovectomy.
|
TABLE 7-1 Radiographic Diagnoses any Orthopaedic Surgeon Should be able to Make
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
disease, moderate dose radiation therapy can be considered. Older
patients or those with associated substantial degenerative arthritis
are best managed with complete synovectomy and an arthroplasty.
Fortunately, with more choices in implant materials, such as metal on
metal or ceramic on ceramic bearing surfaces, younger patients can
enjoy the reduced recurrence rate and better function that total joint
arthroplasty can offer.
need to be followed radiographically with periodic MRI scans. A
baseline scan is done 6 weeks postsynovectomy. Asymptomatic small local
recurrences can be observed. Patient counseling is very important with
this disease, because there is risk of progressive arthritis and
subsequent need for a total hip arthroplasty. At times this can be a
frustrating, progressive, difficult-to-control disease, and patients
need to understand this at the beginning of treatment.
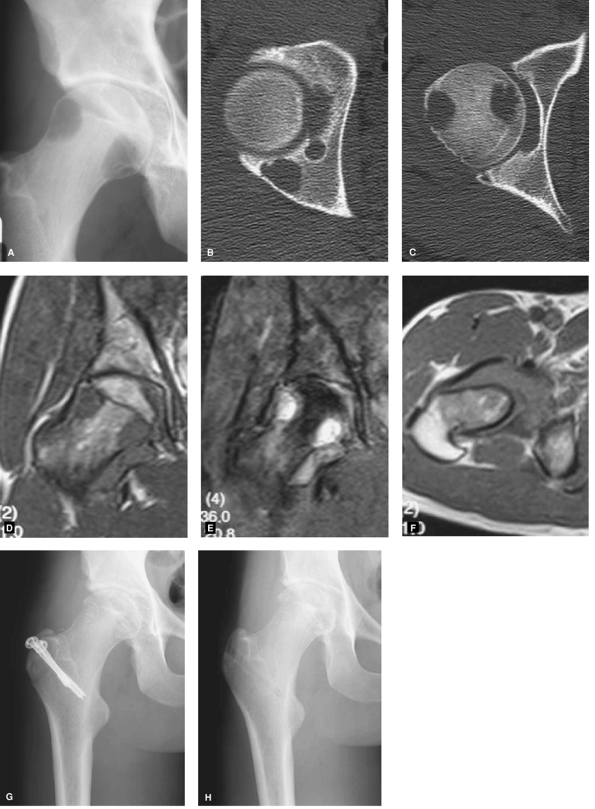
month history of increasing hip pain with episodes of severe hip pain.
His physical examination reveals a limp and a painful restricted range
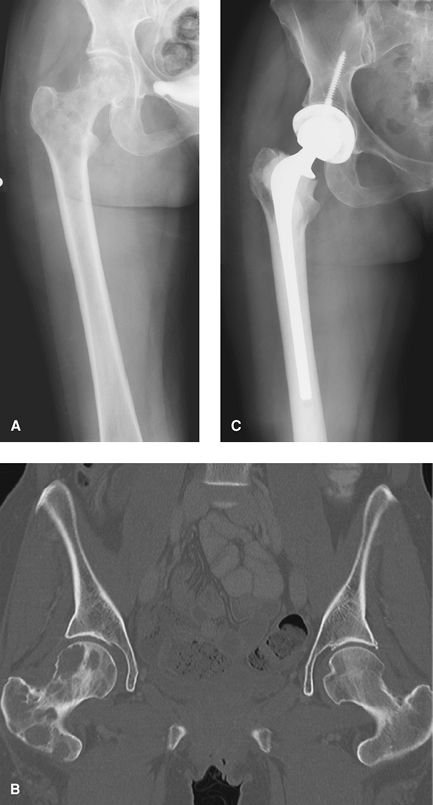
of motion. His plain x-ray films and CT scan (Fig. 7-1A–C)
demonstrate subtle soft tissue swelling and multiple radiolucent
lesions affecting the femoral head and acetabulum. His MRI shows
hypointensity on T1 and increased intensity on T2 with low T1 and T2
areas consistent with hemosiderin deposits (Fig. 7-1D–F).
He was treated with an open arthrotomy with surgical dislocation of the
hip, complete synovectomy, and curettage and bone grafting of the head
and acetabular lesions (Fig. 7-1G). Nine months
later he underwent removal of the screws in the event a total hip was
ever required in the future. Currently 4 years later he remains in
remission and has maintained a normal joint space (Fig. 7-1H).
metaplastic transformation of synovial tissue. The disease can affect
any synovial tissue. The synovium becomes thickened with the formation
of nodules of cartilage. The cartilage nodules can grow and become
fixed nodules or break off and become loose bodies. Bathed in synovial
fluid, they can grow and ossify. The loose fragments can range from
tiny radiolucent pieces of cartilage to large bony masses centimeters
in diameter.
pain, limp, and restricted range of motion. Symptoms of a loose body
with locking and giving way are common. Occasionally patients present
with end-stage osteoarthritis. The disease is monoarticular affecting
the knee, shoulder, elbow, and hip most commonly. Extra-articular
disease can occur anywhere there is synovial tissue.
osteoarthritis with numerous ossified loose bodies. However, the many
loose bodies may be cartilage and unossified, and therefore not visible
on plain radiographs. In the early stages, differentiation between
other causes of an irritable hip can be difficult.
diagnostic. These can demonstrate synovial proliferation with the
presence of nodular disease and numerous loose bodies. Once calcified
and ossified, the loose bodies can be more readily seen. Occasionally a
large synovial extension into the soft tissues can result in an
impressive collection of loose bodies.
and a complete synovectomy. This can be accomplished arthroscopically
in some cases, but an open synovectomy allows a more thorough
debridement. Arthroscopy has the
advantage
of lower morbidity with less subsequent scarring. Repeat arthroscopy
also is more easily performed forrecurrent disease. If an adequate
debridement and synovectomy cannot be performed with a scope, an open
synovectomy with dislocation of the hip as described above should be
performed. This disease has a high chance of local recurrence.
 |
|
Figure 7-1 A–C:
Plain radiograph and CT scan demonstrating radiolucent lesions in both the femoral head and acetabulum with a normal joint space. D–F; MRI appearance, low signal on T1, bright on T2, marked proliferative synovitis, and small areas of dark signal on both T1 and T2 from hemosiderin. G–H: Immediate postoperative and 4-year follow-up films showing cavitary lesions following curettage and grafting. |
 |
|
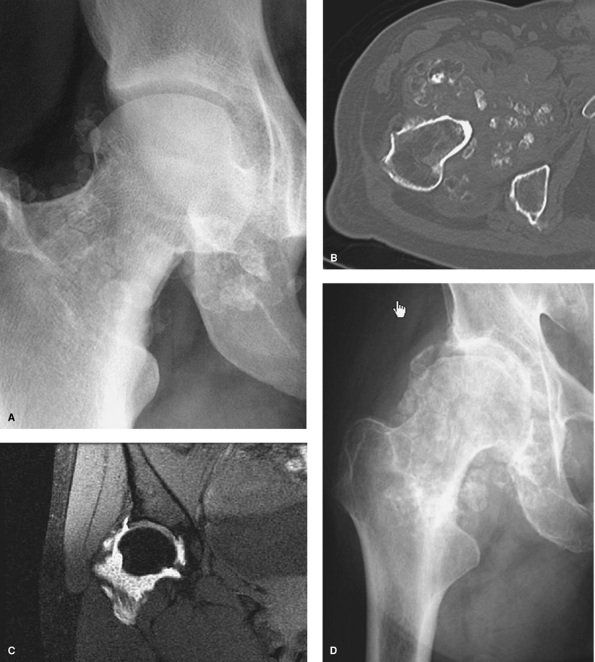
Figure 7-2 A: Plain radiograph demonstrating numerous ossified loose bodies. B: CT scan showing marked synovial proliferation and ossified loose bodies C: MRI T2-weighted image revealing numerous nonossified, noncalcified cartilaginous loose bodies. D: Progression of chondromatosis to advanced secondary degenerative arthritis 4 years later. (Photos A, B, and D courtesy of John Hunter, MD.)
|
3-year history of increasing pain, a limp and diminished range of
motion of his right hip. He has had numerous episodes of locking and
giving way of his leg, but these events were short lived and are
occurring less frequently
now.
His physical examination reveals a limp and a markedly reduced painful
range of motion. His plain radiographs, CT, and MRI scan demonstrated
minimal osteoarthritis with numerous ossified loose bodies (Fig.7-2A–C).
The radiographic features are diagnostic of synovial chondromatosis.
Four years later the patient developed progressive osteoarthritis. (Fig. 7-2D). Treatment at this stage consisted of a total hip arthroplasty with synovectomy and removal of the loose bodies.
affecting bone. It can be solitary (monostotic) or multiple
(polyostotic) and can have a wide variation in severity. It can
sometimes be associated with other medical conditions. This
developmental abnormality results in the failure of primitive bone
remodeling. The immature bone is imbedded in dysplastic fibrous tissue
and is poorly mineralized; it therefore contains the normal
constituents of bone but in a very disorganized form, resulting in
marked reduction in mechanical strength. The bone is therefore prone to
slowly developing deformities and pathologic fractures.
postfertilization somatic cell line gene mutation. The severity of the
disease is dependent on when and where the mutation occurs during
embryogenesis.
present at any age and is nonhereditary. The most common sites of
involvement are the long bones, pelvis, ribs, and craniofacial bones.
finding, pain, deformity, or fracture. The pain can be owing to the
mechanical insufficiency caused by the abnormal tissue or the lesion
itself. The degree of deformity depends on the severity and location of
the bone involved. The proximal femur is a common location, and the
mechanical weakness can result in severe angular deformities with
limb-length inequality. This is especially so in polyostotic fibrous
dysplasia as it tends to progress in adult life. The classic deformity
of the proximal femur is the so-called “shepherd’s crook” deformity, a
pronounced varus deformity with bowing of the femur and shortening of
the limb.
radiograph is usually diagnostic, and the x-ray film characteristics
are so distinctive that a diagnosis can be made with confidence. The
lesion is usually well demarcated and consists of fairly homogenous
fibro-osseous calcified material that has a ground-glass appearance.
Occasionally the plain radiographs can be nonspecific owing to cystic
degeneration, multiple fractures, or deformity. Patients with a
nonspecific radiographic appearance require further investigation and
sometimes a biopsy.
view of the bone, and a diagnosis can often be made at this point. If
the radiographic appearance is atypical, an MRI study and a biopsy may
be needed.
T1-weighted image and a T2 signal of higher intensity. The signal
intensity is determined by the relative composition of fibrous tissue
and mineralized immature bone. There may also be areas of cystic
degeneration with a high T2 signal.
is not a neoplastic condition but rather to deal with the mechanical
consequences of a relatively weak and deformed bone. Treatment of the
deformed bone is difficult because of its poor mechanical strength, and
eradication of the fibrous dysplasia usually is not possible.
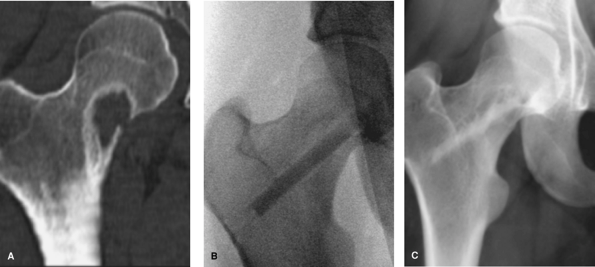
increasing activity-related pain affecting the right groin and thigh.
She has mild pain at rest and moderate pain at night. Her physical
examination is essentially normal. Her CT scan shows a lesion in the
femoral neck, largely radiolucent with a deficiency in the medial
aspect of the cortex (Fig. 7-3A). There is a
well-defined reactive rim with increased bone density. The radiographic
differential is large, favors a benign process, and includes
nonossifying fibroma, fibrous dysplasia, unicameral bone cyst, and
eosinophilic granuloma, and so on. Owing to her symptoms, the location
of the lesion, and the cortical defect, the patient underwent an open
biopsy via a transtrochanteric window under fluoroscopic guidance.
Frozen section was consistent with fibrous dysplasia. The lesion was
then curetted, and a fibular strut graft was passed up through the neck
along the medial cortex of the neck (Fig. 7-3B).
A cortical fibular allograft strut was selected for the reconstruction
to reduce the risk of dysplastic bone remodeling of the graft. Her
follow-up radiograph 4 years later demonstrated a healed graft without
replacement by fibrous dysplasia (Fig. 7-3C).
 |
|
Figure 7-3 A:
Coronal CT scan demonstrating relatively nonspecific lesion with a pronounced rim of reactive bone surrounding a radiolucent lesion with a defect in the femoral neck. B: Intraoperative image following biopsy and curettage of fibrous dysplasia with insertion of an allograft fibular strut. C: Four-year follow-up radiograph showing healing of the graft and no evidence of graft erosion by fibrous dysplasia. |
 |
|
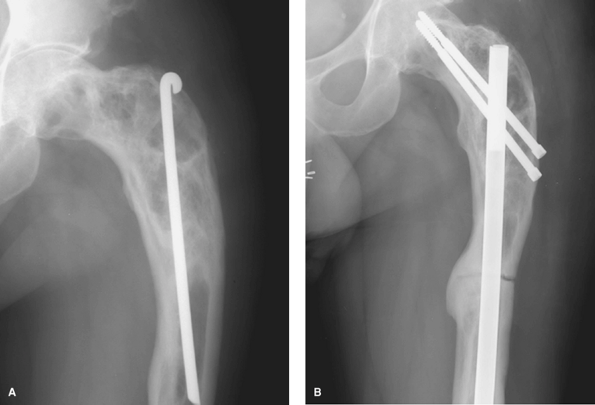
Figure 7-4 A:
Plain radiograph of previously treated fibrous dysplasias. Some areas of radiolucency with a ground glass appearance. Previous Rush rod and surgical changes. Note the varus deformity. B: Follow-up radiograph 2 years following corrective osteotomy and reconstruction nail fixation. |
episodes of his right hip and thigh pain. He has had episodes of severe
pain sometimes requiring crutches. As a child he underwent a surgical
procedure because of recurrent pain. His physical examination revealed
a 1.5-cm. limb-length discrepancy with shortening in the femur. He had
a nearly full range of motion of his hip with minimal pain at the
extremes. His radiographs demonstrate mild osteoarthritis, a varus
deformity of the femoral neck and proximal femur, evidence of previous
surgery, and a mixed radiolucent/radiodense lesion. On close
inspection, the bone has a ground-glass appearance (Fig. 7-4A.)His
previous surgical records included a pathology report describing
fibrous dysplasia. Given his symptoms and the varus deformity, a
corrective osteotomy with intramedullary fixation was performed (Fig. 7-4B). The patient has since enjoyed a marked reduction in his symptoms.
proximal femur and acetabulum. The role of the orthopaedic surgeon in
the management of a patient with metastatic disease is to establish the
diagnosis, identify those patients at risk for fracture, and
reconstruct bone defects following fracture (Table 7-2).
different compared with a traumatic fracture in normal bone. Every
effort must be directed to the restoration of the patient’s function
and relief of pain as quickly as possible. Fixation choices should
include those options that permit immediate full weight bearing, with
the assumption that the fracture itself will never heal. The surgeon
must recognize that further local progression of the metastatic lesion
may occur.
retention of the femoral head. Curettage, cementation, and screw
fixation of femoral neck lesions is rarely performed. Reduction and
fixation of femoral neck fractures should not be performed. These
lesions are best managed with either a total hip arthroplasty or
hemiarthroplasty. Consideration should be given to using a long
cemented stem. This permits predictable immediate fixation, allows for
postoperative radiation therapy, and extends the scope of the
reconstruction to prophylactically strengthen the remaining femur. The
management of an impending femoral neck fracture is the same as for a
completed fracture. However, palliative radiotherapy may be offered
first as some patients may have a very good response and thus avoid
surgery.
|
TABLE 7-2 Metastatic Bone Disease Basic Surgical Principles
|
||||||
|---|---|---|---|---|---|---|
|
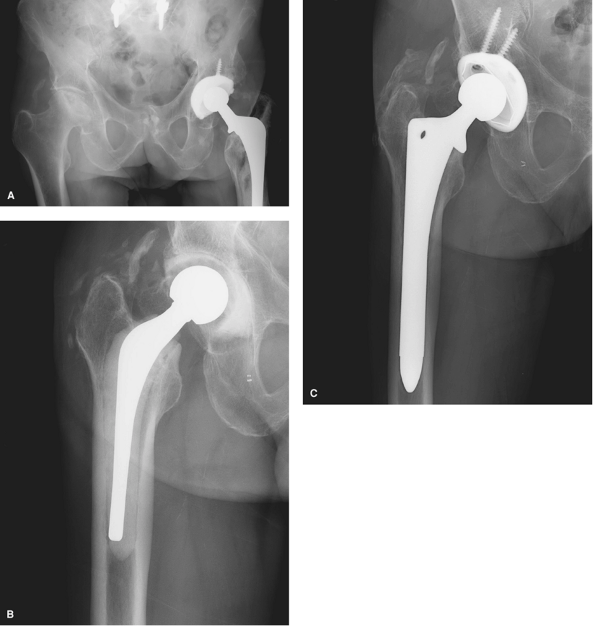
breast cancer. She has had increasing right hip pain for the past
month. The pain was initially present only with weight bearing, but it
is now present at rest and she is using crutches and a wheelchair. She
has had radiation therapy to that area 4 weeks ago. Her physical exam
demonstrated an otherwise healthy-appearing female, but her hip
examination revealed a painful range of motion. Her plain radiographs
and CT scan show widespread disease affecting the head, neck, and
proximal femur. The patient has failed radiation therapy and is at risk
of fracture. The intent of treatment is to fix the problem predictably,
permit immediate return to function, and avoid future problems related
to progression of the disease. Consequently, an arthroplasty was
chosen. In this case, a total hip arthroplasty was performed; a
hemiarthroplasty would work as well, but a total hip avoids the
possibility of a painful hemiarthroplasty in a young patient. A long
cemented stem was chosen to permit predictable immediate fixation,
antibiotic delivery, and prophylactic stabilization of as much of the
femur as possible (Fig. 7-5A–C).
characteristic presentation. The lesion is typically ≤1 cm in diameter.
It is characterized by a radiolucent nidus with surrounding reactive
bone formation. The diagnosis is easy to make histologically.
children and young adults, with a male predilection of two to one; it
can occur in any bone. The lesion produces prostaglandins, which
mediate pain and produce new bone formation. Aspirin and other
anti-inflammatories block the production of prostaglandin, hence
controlling the symptoms.
throbbing pain, typically worse at night. The pain is particularly
responsive to aspirin, something patients often stumble on by
themselves. Patients may medicate themselves to the
point
of developing tinnitus. If the tumor is present in the neck or head of
the femur, it can present with typical pain as well as an irritable hip.
 |
|
Figure 7-5 A: Multiple radiolucent destructive lesions affecting the femoral head and neck B: CT scan demonstrating diffuse disease from metastatic breast carcinoma C: Pose operative radiograph, long stemmed cemented total hip arthroplasty.
|
classically demonstrating a radiolucent nidus with a surrounding area
of reactive bone produced by prostaglandin production. Technetium bone
scanning typically shows a hot spot. A bone scan is helpful when the
lesion is not readily apparent on plain radiographs. Computed
tomography is often diagnostic and is helpful in locating the lesion in
difficult anatomic locations. Dynamic enhanced (gadolinium angiography)
magnetic resonance imaging is helpful in differentiating an osteoid
osteoma from other similar-appearing lesions. The nidus of an osteoid
osteoma will show a bright blush from the gadolinium.
dramatic appearance on magnetic imaging with edema involving the bone
and surrounding soft tissues. A prominent and florid synovial reaction
can occur if the lesion is intra-articular, on the surface of the
femoral neck, or near the synovium. This can mimic other synovial
proliferative disorders both clinically and radiographically.
is not acceptable is radiofrequency ablation. With the precise guidance
of computed tomographic fluoroscopy under general anaesthesia, a
radiofrequency needle is placed within the center of the nidus and
heated to 90°C for 6 minutes. The morbidity is low, the failure rate is
low, and typically the patient is painfree the next day. A biopsy is
done at the time of needle insertion, but because of the small size of
the needle used, representative tissue is seen only 40% of the time.
More than 95% of patients can be expected to be cured with a single
treatment. The risk of relapse is low. The patient may resume full
unrestricted activity immediately following treatment.
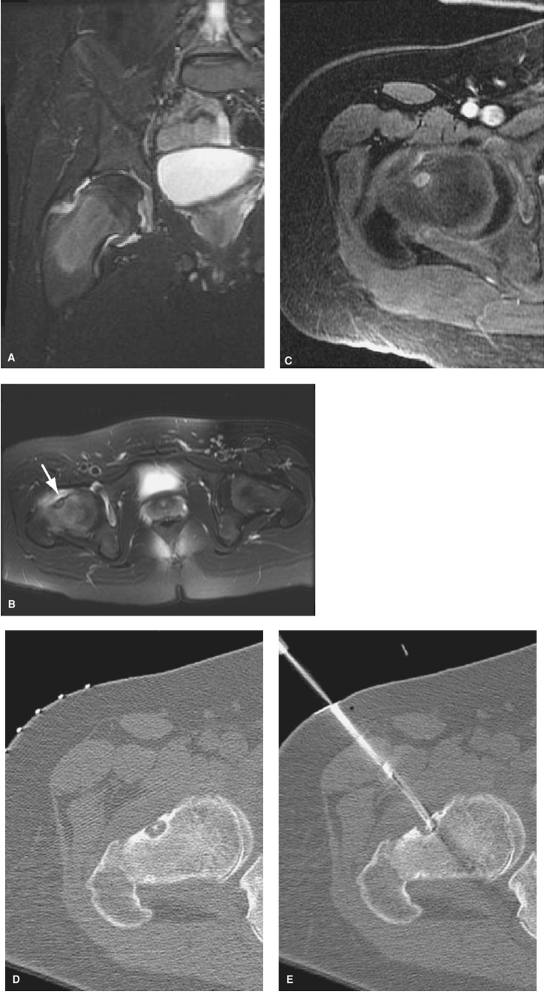
of intermittent hip pain. It has been increasing over the last 2 months
and is particularly worse at night. The patient has been taking
ibuprofen with moderate pain relief. Physical examination reveals a
marked restriction in range of motion of the hip and muscular atrophy.
MR imaging reveals a lesion on the neck of the femur with an effusion,
synovitis, and surrounding edema (Fig. 7-6A).
The image was initially suggestive of either infection or Ewing
sarcoma. The clinical and radiographic features were more consistent
with osteoid osteoma with a brisk inflammatory reactive response (Fig. 7-6B–D). The patient was treated with a CT-guided radiofrequency thermal ablation (Fig. 7-6E). The patient had an excellent response and remains symptomfree 2 years later.
that classically arises in the epiphysis and accounts for <1% of all
primary bone tumors. Most tumors arise in patients with active
epiphyses, and the most common location is the proximal humerus,
followed by the knee and hip.
an incidental finding. Symptoms include pain, swelling, and a painful
range of motion.
defined reactive rim. The lesion may show subtle areas of calcification
within it, and its location is usually indicative of the diagnosis. The
lesion is hot on bone scan, and generalized uptake around the affected
joint is not uncommon.
 |
|
Figure 7-6 A: T2-weighted MR image demonstrating marrow signal changes in the proximal femur with a large effusion. B: Axial MR image demonstrating the nidus. C: Dynamic enhanced MRI showing characteristic blush from gadolinium. D–E: CT images demonstrating the nidus and placement of the radiofrequency probe.
|
intralesional calcification and better defines the plain radiographic
appearance. Magnetic resonance imaging demonstrates a homogenous
hypointense appearance on T1-weighted imaging and variable to
hyperintense signal on T2-weighted images. A secondary aneurysmal bone
cyst component is not uncommon with chondroblastoma. This is evident by
an area of high signal on T2 suggestive of blood and fluid levels on
both MRI and CT scans. A large amount of reactive edema in the bone and
synovitis in the joint is often seen as well and explains the symptoms
of pain and joint irritability seen with often relatively small
lesions. Giant cell tumor and clear cell chondrosarcoma are in the
differential, but these tend to occur in older patients. Clear cell
chondrosarcoma can have a similar MRI appearance to chondroblastoma but
is usually in an older age group, is larger, and extends beyond the
epiphysis.
recurrence rate of 5% to 15%, largely depending on the thoroughness of
resection. Chondroblastoma of the femoral head presents a challenge in
all aspects of its management. In patients in whom the diagnosis is
unlikely to be a clear cell chondrosarcoma, treatment can consist of
open biopsy, frozen section, and immediate curettage and bone grafting.
The surgical approach can include arthrotomy, surgical dislocation, and
approaching the lesion from a window in the neck below the articular
cartilage or a transtrochanteric tunnel through the neck of the femur.
Open arthrotomy has a higher morbidity but would most likely allow for
a more complete curettage. A transtrochanteric approach has a lower
morbidity but a higher chance of local recurrence. The older patient
with a radiolucent epiphyseal tumor is a more difficult problem. The
differential diagnosis would include a clear cell chondrosarcoma. A
biopsy has the potential to contaminate either the joint or the
intertrochanteric region depending on the approach. If the index of
suspicion is very high or if the femoral head is so involved and the
joint is not contaminated, an excisional biopsy and total hip
arthroplasty can be considered on very rare occasions.
presents with a 4-month history of left hip pain. Activity related, it
is increasing in severity and is present at rest and at night. Physical
examination reveals a limp and a generally diminished range of motion
of her hip with severe pain at the extreme of motion. Plain radiographs
demonstrate a radiolucent lesion arising solely in the epiphysis of the
proximal femur (Fig. 7-7A). MRI demonstrates a well-defined lesion with a modest amount of edema (Fig. 7-7B, C).
The clinical and radiographic features strongly favored a
chondroblastoma. The patient was treated by an intralesional curettage
and bone grafting. This was done via a transtrochanteric approach with
fluoroscopic guidance. A core of bone was removed with a 16-mm
trephine. The bone was reserved, and the curettage was guided by
fluoroscopy with direct visualization using a laparoscope through the
tunnel. Once completed, the core was reinserted into the defect and the
lateral deficiency was grafted with morselized allograft. The
postoperative MRI at 18 months shows the transtrochanteric approach and
the resolution of the lesion with healing of the graft. (Fig. 7-7D–E).
Occasionally, severe joint destruction can occur, most often when the
diagnosis is delayed. This problem usually is managed with a resection
arthroplasty and a delayed total hip arthroplasty.
States. The incidence is increased in immunocompromised and elderly
patients with comorbidities. Forty-five percent of patients are older
than 65 years of age. The morbidity and mortality rate is dependent on
the organism.
 |
|
Figure 7-7 A: Plain radiograph showing a subtle radiolucent epiphyseal lesion. B–C: MR image demonstrating marrow edema involving the head and neck. D:
Two-year postoperative MRI. The track made by the trephine to obtain access to the lesion is seen on this image. The bone graft is evident in the cavity. E: The corresponding plain radiograph showing the grafted lesion. |
subtle joint irritability to fulminant systemic sepsis. Typically, the
presentation is monarticular and is usually acute in onset. Patients
with pre-existing joint disease report a sudden increase in their joint
symptoms.
and external rotation and any motion of the joint is extremely painful.
With severely immunocompromised patients, the signs may be less
obvious, and in patients with severe sepsis, the diagnosis of
polyarticular sepsis may be difficult to make. Ninety percent of cases
are monarticular.
helpful in demonstrating an effusion with reactive edema. Patients with
pre-existing hip pathology can present more of a challenge
radiographically, as the underlying arthritic problem can be the source
of pain.
 |
|
Figure 7-8 A: Plain radiograph showing advanced avascular necrosis and soft tissue swelling around the right hip joint. B: Interval antibiotic spacer prosthesis. The patient was allowed full weight bearing on this device. C: Subsequent definitive reconstruction with a cementless implant.
|
analysis is the test of choice. Treatment is based on the clinical
findings and the preliminary joint fluid analysis. If the suspected
diagnosis is sepsis, the treatment is arthrotomy, debridement, and
antibiotic therapy.
anterolateral approach, excision of the anterior capsule of the hip,
and a synovectomy without dislocating the hip. In patients who have
pre-existing end-stage hip disease or those patients with persistent
infection with a destroyed hip joint, I resect the femoral head and
insert a primary functionalantibiotic-impregnated spacer total hip
prosthesis. Various spacers are now available. I prefer to use a
therapeutic dosage of antibiotics in the bone cement, typically 4.8 g
of gentamicin and 2.0 g of vancomycin per 40-g package of cement. The
patient receives 6 weeks of parenteral antibiotics followed by a
definitive arthroplasty, usually a minimum of 8 weeks later. The second
stage can be deferred indefinitely in patients who are elderly and
frail and have other significant comorbidities.
of a low-grade gastrointestinal (GI) lymphoma and has been receiving
chemotherapy. He has had right hip pain for the past 5 months. It began
suddenly and has been getting worse. Over the past 3 days the pain has
become severe, and he has been unable to get out of bed for the past 24
hours. On physical examination he appears unwell and his temperature
was 39.5°C. His hip is extremely painful to any motion, and he has
marked tenderness in his right groin. His hip was aspirated, revealing
a white count of 65,000 cells with 80% nucleated polymorphonuclear
cells. A Gram stain revealed Gram-positive cocci. His plain radiograph
showed stage four avascular necroses (Fig. 7-8A).
The patient was treated with surgical debridement and a two-stage total
hip replacement, first using a functional antibiotic-impregnated spacer
prosthesis (Fig. 7-8B). He was treated with 6
weeks of intravenous vancomycin and oral rifampin for
methicillin-resistant staph aureus. He continued his chemotherapy, and
initially it was planned to leave the temporary device in indefinitely.
He did well with his lymphoma, was allowed to be as active as possible,
and finally a year later his hip was replaced with a definitive
prosthesis (Fig. 7-8C).
R, Gill TJ, Gautier E, et al. Surgical dislocation of the adult hip: a
technique with full access to the femoral head and acetabulum without
the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124.
BA, Duncan CP, Beauchamp CP. Long-term elution of antibiotics from
bone-cement: an in vivo study using the prosthesis of antibiotic-loaded
acrylic cement (PROSTALAC) system. J Arthroplasty. 1998;13(3):331–338.
