THORACOLUMBAR FRACTURES: EVALUATION, CLASSIFICATION, AND INITIAL MANAGEMENT
VIII – THE SPINE > Trauma > CHAPTER 141 – THORACOLUMBAR
FRACTURES: EVALUATION, CLASSIFICATION, AND INITIAL MANAGEMENT
must recognize life-threatening injuries and treat them appropriately,
provide initial supportive care at the same time diagnostic studies are
initiated, and protect the neural elements until definitive treatment
can be provided. Whether acting in concert with a team of trauma
specialists or alone in the emergency department, an orderly, stepwise
approach to assessment and management will improve overall outcome and
ensure that serious injuries are not missed.
-
Assess vital functions—airway, bleeding, circulation.
-
Protect the spine while managing initial shock or life-threatening injuries.
-
Initiate a diagnostic workup for suspected spinal injury.
-
Stabilize the spinal column to protect the neural elements during further evaluation and any emergency procedures.
fracture is identified and classified, the surgeon can prepare a
treatment plan based on the fracture pattern, the severity of injury,
and the patient’s overall condition.
the patient’s life. In some cases, the threat to life is evident (e.g.,
from hemorrhage, visceral trauma), but in others it is not.
motor vehicle accidents, involving drivers and passengers of automobiles, riders of motorcycles, and pedestrians (1,7,17,18,20,23,25,29).
Other causes of spine fractures include falls from height, penetrating
trauma, and crush injuries, such as those sustained by a worker caught
beneath a collapsing structure. In these kinds of injuries, polytrauma
is common (Fig. 141.1). In our experience,
patients with unstable thoracolumbar fractures suffer an average of two
other major injuries in addition to their spinal fracture; some
patients may present with as many as six associated injuries (20).
 |
|
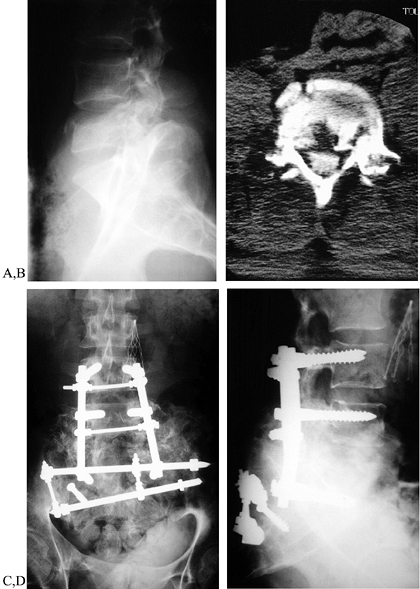
Figure 141.1. Spinal trauma—a high-energy injury. A:
Lateral radiograph of an 18-year-old man crushed under a wall, forced into extreme hyperflexion. He had massive thoracic injuries, a splenic laceration, and a progressive cauda equina injury. Radiograph demonstrates L-5 burst fracture. Pelvic radiographs also demonstrated bilateral sacroiliac fracture–dislocations. B: CT scan shows comminuted lumbar fracture, with retropulsed vertebral body fragment abutting the volar surface of the laminae. C,D: AP and lateral radiographs after emergent stabilization and resuscitation. The patient underwent multiple procedures under the initial anesthetic, including splenectomy, chest tube placement, L-5 vertebrectomy, cauda equina decompression, posterior spinal stabilization L-4 to sacrum, placement of vena caval filter, and posterior stabilization of the pelvic disruption. This aggressive approach provided enough spinal column stability to allow early mobilization and aggressive pulmonary toilet. Four years after this massive injury, the patient was ambulatory with an ankle–foot orthosis, had mild back pain, and had returned to college. |
thoracic fracture reflect the forces of blunt trauma and rapid
decelleration. Intrathoracic injuries include the following:
-
Pneumo- and hemothorax associated with rib fractures or bronchial disruption
-
Myocardial or pulmonary contusion
-
Great vessel injury from blunt trauma or rapid deceleration
-
Hemopericardium and cardiac tampanade
-
Diaphragmatic rupture and acute hiatal hernia
hemo- or pneumothorax or a diaphragmatic rupture, and it may show
widening of the mediastinum associated with a great-vessel injury. If
multiple rib fractures are seen, particularly first rib and clavicle
fractures, consider getting an angiogram to study the aortic arch.
cardiac tampanade. Rapid placement of a chest tube will resolve the
pneumo- or hemothorax, with immediate improvement of oxygenation and
cardiac output. Pericardiocentesis will decompress the cardiac
tampanade with rapid improvement in circulatory function. These
injuries are often associated with thoracic fractures and
fracture–dislocations. A quick assessment of bilateral breath sounds
and heart sounds should identify either problem. In a tension
pneumothorax, breath sounds are absent or diminished on the injured
side, and the esophagus and trachea are displaced toward the normal
lung. In cardiac tampanade, there are indistinct heart sounds, and the
neck veins are distended. Cardiac output is impaired in either case,
and the patient manifests signs of shock and cyanosis.
injuries. The association of lap-belt abrasions with the classic
flexion–distraction fracture should alert the physician to a high
likelihood of intra-abdominal injury (12).
Because this fracture occurs as the body is flexed forward over the
lap-belt, visceral injuries are found in 40% to 60% of patients (10,27).
Solid viscera may be injured directly when they are compressed between
the body wall and the lap-belt, or they may be torn from their
attachments when the body is suddenly and rapidly decelerated. Hollow
viscera may be ruptured, perforated, or torn from their mesenteries.
Obtain a general surgical assessment whenever a flexion–distraction
injury is suspected. A rigid abdomen, falling hematocrit, and abdominal
pain or tenderness are clear indications for emergent peritoneal lavage
and laparotomy. In the stable patient with no symptoms of shock, an
abdominal computed tomography (CT) scan may be used to rule out an
abdominal injury. Intra-abdominal injuries are also common in
thoracolumbar injuries.
fractures are high-energy injuries, it is not surprising that they are
commonly associated with additional skeletal injuries:
-
Fractures of the femurs, tibias, and feet are common.
-
Fractures of humeri and forearm bones are less common.
-
Major pelvic fractures are not common and are usually seen only after massive trauma.
-
Hemorrhage from multiple long-bone fractures can be severe, resulting in shock (3).
assessed in the emergency room, and the cervical spine should be
protected throughout the initial evaluation and emergency procedures (19).
Unconscious, obtunded, or intoxicated patients cannot provide a
dependable history or reliably report pain or numbness. These patients
should be protected as though a cervical injury existed (2,24).
Plain radiographs will demonstrate the majority of bony injuries but
may not reveal soft-tissue disruptions; retropharyngeal hematoma
indicates significant soft-tissue injury and mandates a formal cervical
workup (30). Head injuries may be evaluated by
a magnetic resonance imaging (MRI) or CT scan prior to anesthesia if
surgery is needed, or they may be held under observation if otherwise
stable.
hypovolemic shock is the most serious, and it must be recognized and
corrected quickly. Young patients manifest tachycardia and peripheral
vasoconstriction as primary symptoms; hypotension may not be seen until
shock is severe and vascular collapse occurs. Older patients generally
do not compensate well, and tachycardia and hypotension may both appear
early on.
-
Place a Foley catheter to monitor urine output.
-
Rapidly assess common sites of blood
loss—open wounds, intra-abdominal and intrathoracic hemorrhage, and
long-bone and pelvic fractures. -
Institute fluid resuscitation immediately.
tone. Patients present with hypotension and tachycardia although they
have warm, well-perfused skin and peripheral tissues. They may not
respond to fluid bolus, and vasopressors may be needed.
output, including cardiac tampanade, tension pneumothorax, myocardial
injury, or myocardial infarction. In every case, rapid vascular access
and fluid resuscitation are the vital initial treatments for spinal
trauma patients.
protect the patient’s spine so that a more formal evaluation and workup
can be carried out without injuring the spinal cord. This is
particularly important in the polytrauma patient who may be
unconscious, may require anesthesia and surgical care, and must be
moved repeatedly to manage other life-threatening injuries. Plain
radiographs of the cervical spine are mandatory before intubating the
patient, and if injury is seen or suspected, a fiberoptic nasotrachial
intubation is the safest.
slide board, and it should always be done with sufficient personnel to
make the transfer smoothly and without struggling. When log-rolling the
patient, the team must coordinate efforts to see that the shoulders and
pelvis move together as a unit. If the patient is hemodynamically
stable and does not require emergency procedures, he may be transferred
to a firm mattress and maintained under strict spinal precautions until
the workup is completed. Precautions include strict supine positioning,
log-rolling side to side every 2 hours for skin care, and periodic
reexamination of neurologic status. Head-injured and combative patients
may need to be sedated and intubated to avoid self-inflicted spinal
cord injury.
stabilized, return to the spinal injury assessment. Obtain a complete
history, paying close attention to reports of transient paresthesias,
acute back or neck pain, or temporary weakness or paralysis at the time
of injury. Record the location and radiation of pain symptoms, as well
as any radicular symptoms. Any history of previous injury, fracture, or
pain symptoms should be noted. A global examination of motor and
sensory function should rapidly focus on any areas of deficit. If the
patient cannot cooperate with the exam, carefully observe and note
spontaneous movements and withdrawal responses. Carry out a rectal exam
to assess rectal tone, voluntary rectal control, and the bulbocavanosus
reflex. If the patient is neurologically normal, log-roll him to one
side so that the spine can be palpated for step-offs, tenderness, or
kyphosis. Note the condition of the skin over the symptomatic area. If
a neurologic deficit exists, obtain radiographs of the symptomatic
level before moving the patient.
Steroids have been shown to improve spinal cord recovery relative to
placebo and naloxone therapy, and they are thought to combat abnormal
biochemical processes brought on by thromboxanes and prostaglandins
released at the site of injury. Steroids must be given within 8 hours
of injury to have any beneficial effect. Patients treated with
high-dose steroids may be exposed to an increased infection rate and
risk of gastrointestinal hemorrhage.
possible until the patient has been stabilized hemodynamically and has
recovered from initial resuscitation. When the patient is alert and
cooperative, a formal motor, sensory, and reflex examination should be
repeated, and a detailed history of the accident obtained.
injury; presence or absence of neurologic symptoms, and past history of
spinal trauma, surgery, or symptoms. In high-energy injuries, it is
often difficult to determine exactly what forces acted on the spine to
produce fracture, but knowledge of the injury mechanism can help
identify associated injuries and provide clues to the level of
instability to be expected. A lap-belted patient in a motor vehicle
accident may present with a straightforward flexion–distraction injury,
for instance, whereas a patient ejected from the vehicle or from a
motorcycle frequently will present with a more complex fracture pattern
consistent with the combination of torsional and axial loading forces
experienced when striking the ground. If the forces involved in the
fracture were rather low, an underlying pathologic process must be
considered. If the forces involved were very high, and multiple
injuries were sustained, the risk of prolonged recumbency to the
patient’s life must be considered in timing a surgical procedure.
elicit any history of transient paresthesias or paralysis from the time
of injury. Even if the patient’s symptoms resolved quickly, they
suggest that some level of root or cord injury occurred at the time of
the injury; therefore, assume that the spinal fracture is unstable. If
the patient cannot give the details of the event, careful scrutiny of
field notes can provide important clues to whether the patient had
abnormal findings at the accident site. These notes are often gross
evaluations only, however, and a patient with a severe cauda equina
injury can still “move all four extremities.”
important to understanding the current injury. Lower extremity weakness
due to old injury or spinal disease can confuse the diagnostic picture
after an acute injury, and a preexisting deformity—compression
fracture, spondylolisthesis, or kyphosis—can be difficult to
differentiate from a new injury. Furthermore, the surgical approach to
the multiply operated back will be more demanding and may require
different instrumentation than for an ordinary fracture.
Having examined the musculoskeletal system in the emergency department,
carefully reexamine the extremities for tenderness and pain, and
examine the back again to determine the level of discomfort and the
presence of step-offs or gaps between the spinous processes, and to
assess the skin over the area of injury.
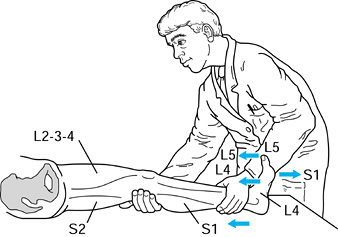
each motor group for the lumbar and sacral plexuses independently and
compare to the contralateral group (Fig. 141.2). Motor strength is recorded on six-point scale:
 |
|
Figure 141.2. Motor testing.
|
|
assessment as to whether the patient is clinically weak or limited in
effort by pain. Also determine whether the pattern of weakness is
consistent with a cord lesion, a root lesion, or a peripheral nerve
injury.
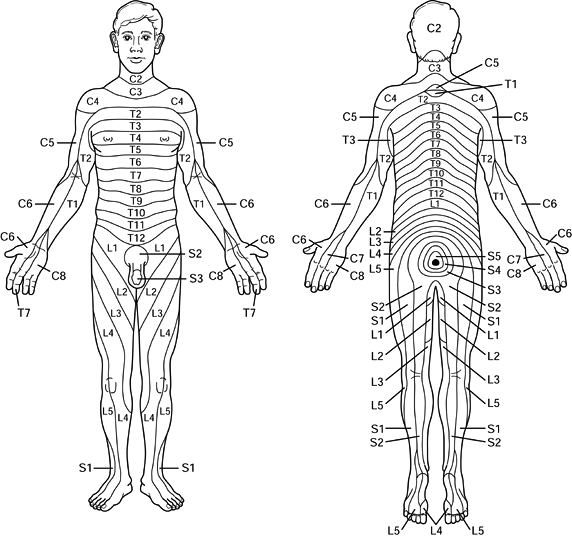
seeks a level of anesthesia, root by root, down to the sacrum. Patients
with thoracic cord injuries will have an anesthetic level at or just
below their fracture. If the anesthetic level and the recognized
fracture do not coincide, obtain an MRI to determine the actual cause
of the cord impairment. Sensation in the lower extremities follows a
dermatomal pattern; test each dermatome for light-touch and pin-prick
sensation (Fig. 141.3).
 |
|
Figure 141.3. Dermatomal patterns.
|
bulbocavernosus reflex, an involuntary contraction of the rectal
sphincter, can be triggered either by gently squeezing the glans penis
or glans clitoris or by gently tugging on the Foley catheter. If this
reflex is absent, the patient either is in spinal shock or has suffered
an injury to the caudal segments of the conus medullaris. Hyperactive
reflexes suggest disinhibition due to a cord-level injury. Absent
reflexes in an isolated distribution suggest an incomplete injury or
root lesion. Complete absence of reflexes may be due to either spinal
cord shock or a complete cauda equina injury. Spinal cord shock occurs
at the time of injury and may persist for 72 hours. While the patient
is in spinal cord shock, the neurologic examination remains
unreliable—an incomplete injury may appear complete due to the
overriding effects of cord shock. Once shock resolves and caudal
reflexes return, the examination provides clear prognostic information:
Incomplete injuries have potential for improvement, complete injuries
have almost none. The bulbocavernosus reflex is the most reliable level
for testing reflex return because it tests the most caudal segment of
the spinal cord.
most caudal motor and sensory unit in the body is the rectum, the
function of which is crucial to independent social activity. Carry out
an independent examination of rectal tone, sensation, and reflex
activity. Do not rely on emergency department records if there is any
concern of neurologic injury. Explain the purpose of the examination to
the patient, who may be anxious over repeated exams. Document resting
tone, voluntary contraction, perianal sensation, and bulbocavernosus
reflex.
and lateral views of the thoracic spine and/or the lumbosacral spine,
depending on the symptomatic level (16). On
occasion, standard thoracic films will cut off T12–L1, and lumbosacral
films will start at L-1, giving an inadequate view of the most
frequently injured level. If fracture of the thoracolumbar junction is
suspected, repeat AP and lateral radiographs, centered at the T-12
level. In stable fractures (compression fractures, mild burst
fractures, and mild flexion–distraction injuries), plain radiographs
are sufficient to allow definitive treatment, and no further diagnostic
studies are needed. In unstable spine fractures, however, additional
imaging studies are often indicated.
dislocations, significant flexion–distraction injuries, and any
fracture with a neurologic deficit) require further study to assess the
extent of bony disruption, spinal cord impingement, canal compromise,
and/or cord injury. A CT scan provides the most definitive information
on bony characteristics, such as fracture pattern and comminution (8,11,15).
The axial cuts of the CT scan can completely miss flexion–distraction
injuries, however. An MRI is superior for soft-tissue details such as
cord injury, cord compression, disc herniation, and ligamentous
disruption (28). The MRI has the added benefit of scanning the entire thoracolumbar spine, and it can pick up noncontiguous
fractures, cord injury, and epidural hematoma at levels other than that
of the primary fracture. Longitudinal MRI cuts show the soft-tissue
disruption and bony separation of flexion–distraction injuries well.
compromise just a decade ago, is now replaced by the MRI in all but a
few cases. When an MRI is contraindicated (e.g., intraocular fragments,
cardiac valves), CT myelography is an appropriate but more invasive
alternative.
-
Any patient with a progressive neurologic deficit needs emergent imaging.
-
Any patient whose neurologic level does
not coincide with the recognized injury needs further evaluation for an
unrecognized fracture or disc disruption.
cervicothoracic junction when a CT scan cannot be obtained immediately.
Flexion–extension studies or nuclear medicine scans have little role in
acute trauma. There is no role for electrodiagnostic testing in the
acute management of spine trauma patients.
can usually be classified according to one of a number of schemes.
Holdsworth first characterized spinal fractures according to a
two-column—anterior and posterior—model of the spinal column (13,14).
This model has since given way to the three-column model of Denis,
which considers the vertebral body, anulus, and posterior longitudinal
ligament to be the middle column, a discrete unit separate from the
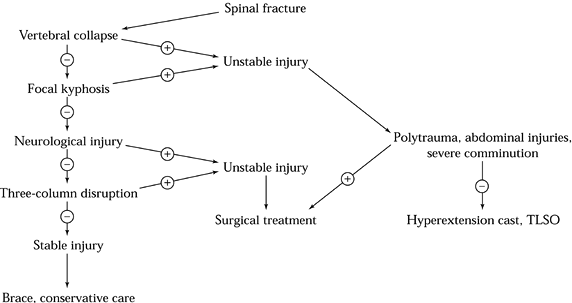
anterior and posterior stabilizers (5,6,22) (Fig. 141.4).
 |
|
Figure 141.4. Three-column model of Denis. A: Anterior column. B: Middle column. C: Posterior column.
|
injury as stable or unstable. Unstable injuries include all those with any of the following:
-
Three-column disruption
-
Greater than 50% collapse of anterior cortex
-
Greater than 25° of focal kyphosis
-
Any extent of neurologic deficit
nonoperatively, not all unstable injuries need to be treated
operatively. A simple algorithm for treatment is indicated in Fig. 141.5.
 |
|
Figure 141.5. Treatment algorithm for thoracolumbar fractures.
|
fracture according to fracture type and severity. The Denis fracture
classification (Table 141.1) depends on
information about the fracture pattern, the mechanism of injury, and
the deforming forces that caused the fracture. The differences between
severe burst fractures and rotational fracture–dislocations, and severe
seat-belt injuries and flexion–distraction fracture–dislocations are
subtle, and of limited importance: These severe injuries are all
clearly unstable, and all require operative treatment.
 |
|
Table 141.1. Denis Fracture Classification
|
with moderate trauma in young patients and minimal to no trauma in
elderly, osteoporotic patients. The anterior column collapses under an
axial or flexion load, with fracture of one or both endplates, but the
middle and posterior columns are undamaged. These stable injuries are
appropriately treated with a removable brace and symptomatic care.
Observe patients with advanced osteoporosis for progressive collapse;
severe compression fractures may warrant a CT examination to rule out a
burst component.
to higher axial or flexural loads at a high loading rate. These
fractures are commonly the result of motor vehicle accidents, falls
from height, or crush injuries. The anterior cortex fails in
compression, and either one or both endplates are fractured. The middle
column is also fractured, and a portion of the posterior vertebral body
is retropulsed backward into the canal. Depending on the severity of
the fracture, the posterior elements may be fractured as well.
Determine the need for surgical treatment by the extent of vertebral
comminution, the extent of canal compromise, and the status of the
posterior column structures (21). Burst fractures may be subdivided by fracture pattern:
-
Type A fractures occur with axial loading, with fractures of both upper and lower endplates.
-
Type B fractures are the most common (50%), with fracture of only the upper endplate.
-
Type C fractures, with disruption of the lower endplate, are uncommon.
-
Type D fractures have a rotational displacement of one body relative to the other on AP radiographs.
-
Type E fractures are lateral compression injuries, with traumatic scoliosis (Fig. 141.6).
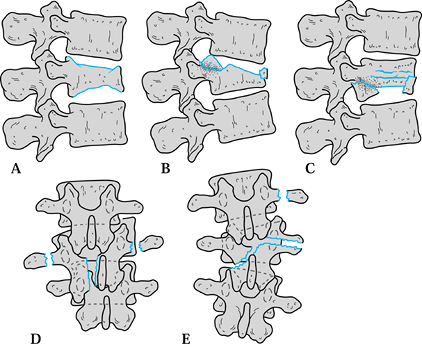 Figure 141.6. Burst fracture patterns.
Figure 141.6. Burst fracture patterns.
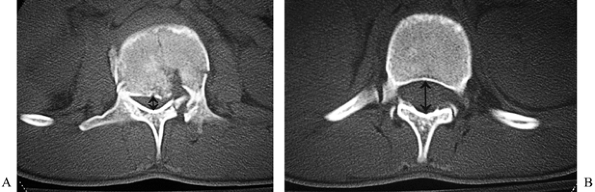
scan, by comparing the AP diameter of the normal spinal canal at an
adjacent level to the reduced diameter at the level of the retropulsed
fragment (26). The ratio of the injured to the intact diameters provides the percent compromise (Fig. 141.7).
The greatest compromise occurs at the level of the pedicles and upper
vertebral body. In type A and B burst fractures, the central portion of
the posterior cortex and body is driven back into the canal between the
two pedicles, which then prevent the fragment from reducing. Because of
the differing volumes of neural tissue in the canal at different
levels, compromise of greater than 50% may produce symptoms at the
thoracolumbar junction, whereas compromise of 85% or more may be well
tolerated at the lumbosacral junction (9). A CT scan will also demonstrate the presence and extent of posterior element disruptions (Fig. 141.8). Three-column injuries are
inherently more unstable than two-column injuries, and the inability to
load the posterior facet joints in a hyperextension cast may exclude
nonoperative care for some patients.
 |
|
Figure 141.7. Canal dimension at injured level (A) is compared to adjacent normal level (B) to determine percent canal compromise.
|
 |
|
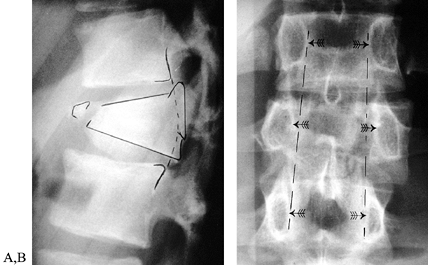
Figure 141.8. Radiographic characteristics of burst fractures. A:
Lateral view demonstrates fracture of anterior cortex and superior endplate, with resulting focal kyphosis. The posterosuperior portion of the vertebral body can be seen retropulsed into the spinal canal, with loss of normal concave contour of the posterior vertebral body. B: AP radiograph demonstrates the increased intrapedicular distance associated with a burst fracture; the distance between the L-1 pedicles is significantly greater than for the levels either above or below, indicating a complete disruption of anterior, middle, and posterior columns. |
The classic one-level injury is the Chance fracture. The mechanism of
injury involves the patient being thrown forward across an intact
lap-belt, resulting in a hyperflexion force acting around a center of
rotation anterior to the spinal column—at
the belt itself. This results in distraction forces at all three
columns of the spine: (a) The posterior elements are torn apart through
either the facet joints or the bone itself, (b) the middle column is
torn apart through either the posterior disc or the posterior vertebral
body, and (c) the anterior column is either disrupted (in severe
injuries) or left as a hinge that cannot resist either flexion or
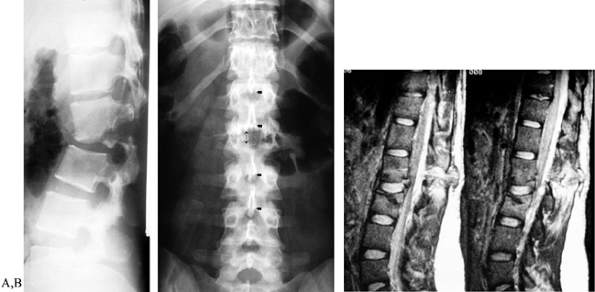
rotational displacement. Plain radiographs demonstrate the gap between
the spinous processes and the disruption of the pedicle in most cases (Fig. 141.9)
but may show minimal displacement when the patient is supine because
the fracture tends to reduce in this position. An MRI shows the injury
clearly.
 |
|
Figure 141.9. Radiographic characteristics of seat-belt fractures. A:
Lateral radiograph of severe flexion–distraction injury, taken in sitting position. The patient was admitted following a head-on motor vehicle accident and treated for abdominal contusions, splenic rupture, and rupture of the colon. Injury was not apparent on supine radiographs. B: AP radiograph shows wide spacing between spinous processes at the level of injury. C: MRI confirms extensive soft-tissue disruption including rupture of the lumbodorsal fascia. |
column and lap belt can rupture hollow viscera, lacerate solid viscera
(liver and spleen), and avulse major vascular pedicles. Unrecognized,
any of these injuries can prove rapidly fatal; it is therefore
necessary that any patient with a seat-belt injury be carefully
assessed by a general surgeon for acute or occult intra-abdominal
injury.
ligamentous structures and the underlying disc at the same level, or
through the posterior lamina, pedicle, and vertebral body in the same
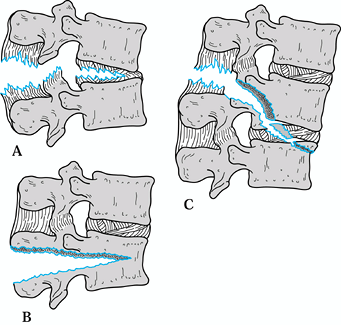
transverse plane (Fig. 141.10). These injuries
disrupt only a single motion segment. Two-level injuries begin
posteriorly at one level of lamina or facet joint, then proceed
anteriorly in an oblique fashion so that the injury passes out of the
vertebral body into an adjacent disc or through the disc into an
adjacent body. In these injuries, two adjacent motion segments are
disrupted, and stabilization requires addressing both levels of injury.
 |
|
Figure 141.10. Seat belt-fractures. A: Injury to soft-tissues only. B: Bony chance fracture. C: Mixed injury.
|
injuries. They are highly unstable, usually associated with neurologic
injury, and often associated with other musculoskeletal and visceral
injuries. The neurologically intact
patient
must be carefully protected during any necessary testing or emergent
operative procedures, and the spine must be stabilized at the first
reasonable opportunity to allow mobilization and prevent paralysis. In
the patient with neurologic deficit, postural reduction may improve
alignment and reduce neural compression, and longitudinal traction may
allow manual reduction of a displaced fracture–dislocation. Neither
will reduce neural compression by retropulsed vertebral fragments,
however, and direct decompression is indicated for those patients with
an incomplete injury and hopes of improvement.
are caused by hyperflexion and rotation forces such as seen when a
patient is ejected from a vehicle at high speed. When the vertebral
body is fractured, this injury may be indistinguishable from a severe
type D burst fracture. Shear fractures are more uncommon injuries and
occur in the absence of axial loading or flexion–extension forces.
Translational forces occurring when the subject is struck squarely from
the side, front, or back act to shift one vertebral body relative to
the next by shearing through bony articulations and ligamentous
structures. Flexion–distraction fracture–dislocations occur when all
three columns fail in hyperflexion. These injuries are often not
distinguishable from severe seat-belt injuries.
 |
|
Figure 141.11. Fracture dislocations. A: Flexion-rotation. B: Shear. C: Flexion-distraction.
|
Instrumentation systems that depend on distraction forces to secure
hook purchase cannot be safely applied in these injuries, and any
system incorrectly applied may overdistract the fracture and stretch
the neurologic elements, precipitating or worsening the neurologic
injury.
comprehensive initial evaluation. The key to success is, as always, to
look at the whole patient—never allowing a single, dramatic injury to
distract attention from more subtle, and potentially more dangerous,
injuries. Once the patient is hemodynamically stable, and the fracture
is recognized and classified, prepare a treatment plan based on the
fracture pattern, the severity of injury, and the patient’s overall
condition. The options for nonoperative and operative treatment are
extensive, and the correct choice for any patient must be determined by
weighing all the above considerations, as well as the surgeon’s
experience, against the potential risks of treatment.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
DR, Burkus JK, Montesano PX, et al. Unstable Thoracolumbar and Lumbar
Burst Fractures Treated with the AO Fixateur Interne. J Spinal Disord 1992;5:335.
MB, Shepard MJ, Collins WF, et al. A Randomized, Controlled Trial of
Methylprednisolone or Naloxone in the Treatment of Acute Spinal Cord
Injury. Results of the Second National Acute Spinal Cord Injury Study. N Engl J Med 1990;322:1405.
JH, Harrington PR, Erwin WD. Results of Reduction and Stabilization of
the Severely Fractured Thoracic and Lumbar Spine. J Bone Joint Surg Am 1978;60:799.
GY, Kathol MH, Daniel WW. Imaging of Acute Injuries of the Cervical
Spine: Value of Plain Radiography, CT, and MR Imaging. AJR Am J Roentgenol 1995;164:43.
SD, Court-Brown CM. Rationale for the Management of Flexion Distraction
Injuries of the Thoracolumbar Spine Based on a New Classification. J Spinal Disord 1989;2:176.
C, Firooznia H, Rafii M, et al. Computed Tomography of Thoracic and
Lumbar Spine Fractures That Have Been Treated with Harrington
Instrumentation. Radiology 1984;151:731.
JS, Goletz TH, Lilleas F, et al. Diagnosis of Vertebral Fractures: A
Comparison of Conventional Radiography, Conventional Tomography, and
Computed Axial Tomography. J Bone Joint Surg Am 1982;64:586.
RF, Benson DR. Missed Cervical Dissociation—Recognizing and Avoiding
Potential Disaster. J Emergency Medicine, In Press, 1998.
MM, Oxland TR, Kifune M, et al. Validity of the Three-column Theory of
Thoracolumbar Fractures. A Biomechanic Investigation. Spine 1995;20:1122.
HM, Donaldson DH, Brown CW, Stringer EA. Stabilization of Thoracic
Spine Fractures Resulting in Complete Paraplegia. A Long-term
Retrospective Analysis. Spine 1994;19:1726.
WP, Rogas JV, Sickler ME, et al. Thoracolumbar Burst Fractures: CT
Dimensions of the Spinal Canal Relative to Postsurgical Improvement. AJR Am J Roentgenol 1985;145:337.
RM. Radiology of the Cervical Spine in Trauma Patients: Practice,
Pitfalls, and Recommendations for Improving Efficiency and
Communication. AJR Am J Roentgenol 1990;155:465.
