Ultrasound Guided Sciatic Nerve Block
Editors: Chelly, Jacques E.
Title: Peripheral Nerve Blocks: A Color Atlas, 3rd Edition
Copyright ©2009 Lippincott Williams & Wilkins
> Table of Contents > Section IV – Ultrasound > 40 – Ultrasound Guided Sciatic Nerve Block
40
Ultrasound Guided Sciatic Nerve Block
Richard Brull
Vincent Chan
The transducer is positioned axially, midway between the greater
trochanter and ischial spine, immediately inferior to the gluteal
crease (Figs. 40-1, 40-2A).
The ischial tuberosity medially and the greater tuberosity laterally
are seen as curvilinear hyperechoic shadows. The sciatic nerve is seen
as a hyperechoic elliptical structure deep to the gluteus maximus
muscle (Fig. 40-2B).
Sterile prep of the skin. The needle is placed lateral to the probe
nearly perpendicular to the skin along the long axis of the beam (in
plane). Some practitioners prefer to use an out of plane approach. With
this approach, imaging the needle can be difficult, and its position is
often inferred by the movement of the tissue at its tip, or by
injecting small aliquots of local as the needle is advanced toward the
sciatic nerve. Because the needle tip is often difficult to see, nerve
stimulation is especially useful for sciatic block. Some practitioners
prefer to begin with a high current, 1 to 2 mA. Others begin closer to
the threshold of stimulation, 0.5 mA. The needle is advanced until
dorsi or plantar
P.298
flexion of the foot is observed. Injection of local proceeds until the nerve is surrounded by a hypoechoic ring.
 |
|
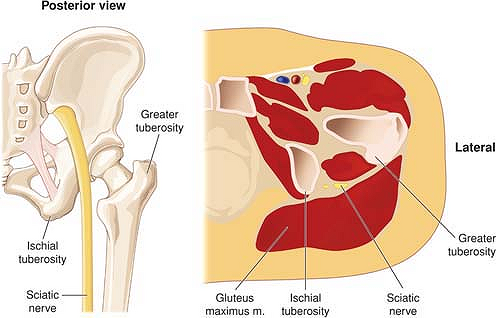
Figure 40-1.
Gross anatomy of the sciatic nerve along with a section or drawing illustrating the position of the nerve in transverse section. |
-
The sciatic nerve is one of the most
difficult ultrasound guided blocks to master because of its depth from
the skin and the lack of easily recognized adjacent vascular structures.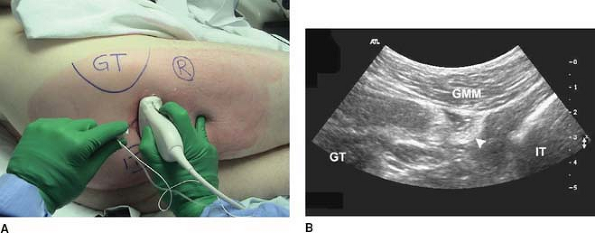 Figure 40-2. Infragluteal sciatic nerve block. A: Patient and probe positioning. B:
Figure 40-2. Infragluteal sciatic nerve block. A: Patient and probe positioning. B:
Transverse sonogram using a 2 to 5 MHz curved array transducer probe
(Philips HDI 5000 system, Bothell, WA). GMM, gluteus maximus muscle;
GT, greater trochanter of the femur; IT, ischial tuberosity; arrowhead, sciatic nerve. -
The infragluteal gluteal approach is the easiest technique because it is the most superficial.
-
Some practitioners may wish to master the gluteal and anterior approaches as well.
P.299
Gluteal Approach
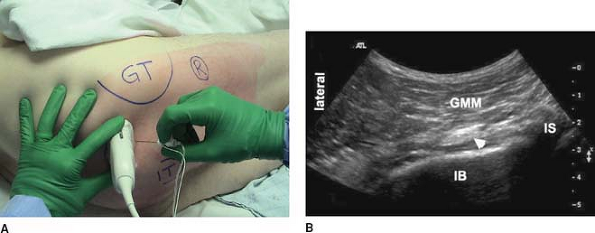
Anatomically, the ultrasound guided gluteal approach to
sciatic nerve block most closely resembles Labat’s classic posterior
technique. The patient is positioned semiprone with the operative side
uppermost. A 2 to 5 MHz curved array probe is placed obliquely at the
level of the ischial spine, midway between the greater trochanter of
the femur and the sacral hiatus (Fig. 40-3A).
In this view, the sciatic nerve is pictured as a thin hyperechoic
elliptical structure deep to the gluteus maximus muscle, superficial to
the linear hyperechoic shadow of the ischial bone, and lateral to the
subtle curvilinear hyperechoic shadow of the ischial spine (Fig. 40-3B).
The round hypoechoic pulsatile pudendal artery and compressible vein,
as well as the inferior gluteal vessels, can often be identified medial
to the sciatic nerve in this view (Fig. 40-3B).
sciatic nerve block most closely resembles Labat’s classic posterior
technique. The patient is positioned semiprone with the operative side
uppermost. A 2 to 5 MHz curved array probe is placed obliquely at the
level of the ischial spine, midway between the greater trochanter of
the femur and the sacral hiatus (Fig. 40-3A).
In this view, the sciatic nerve is pictured as a thin hyperechoic
elliptical structure deep to the gluteus maximus muscle, superficial to
the linear hyperechoic shadow of the ischial bone, and lateral to the
subtle curvilinear hyperechoic shadow of the ischial spine (Fig. 40-3B).
The round hypoechoic pulsatile pudendal artery and compressible vein,
as well as the inferior gluteal vessels, can often be identified medial
to the sciatic nerve in this view (Fig. 40-3B).
Anterior Approach
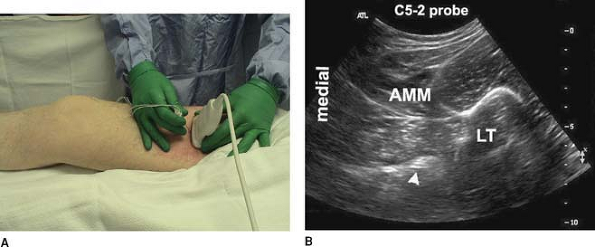
Anatomically, the ultrasound guided anterior approach to
sciatic nerve block most closely resembles the anterior technique
described by Beck and Chelly and Delaunay. This approach is especially
useful in patients who cannot be positioned semiprone (e.g., trauma).
The patient rests supine with the operative leg externally rotated to
facilitate needle passage posterior to the lesser trochanter of the
femur. A 2 to 5 MHz curved array probe is placed obliquely
approximately 8 cm distal to the inguinal crease at the medial border
of the rectus femoris muscle (Fig. 40-4A).
In this view, the sciatic nerve is pictured as a hyperechoic semilunar
structure deep to the adductor magnus muscle and immediately
posteromedial to the curvilinear bony shadow of the lesser trochanter
of the femur (Fig. 40-3B).
The round hypoechoic pulsatile femoral artery and compressible vein are
identified much more superficial and lateral to the sciatic nerve (Fig. 40-4B).
sciatic nerve block most closely resembles the anterior technique
described by Beck and Chelly and Delaunay. This approach is especially
useful in patients who cannot be positioned semiprone (e.g., trauma).
The patient rests supine with the operative leg externally rotated to
facilitate needle passage posterior to the lesser trochanter of the
femur. A 2 to 5 MHz curved array probe is placed obliquely
approximately 8 cm distal to the inguinal crease at the medial border
of the rectus femoris muscle (Fig. 40-4A).
In this view, the sciatic nerve is pictured as a hyperechoic semilunar
structure deep to the adductor magnus muscle and immediately
posteromedial to the curvilinear bony shadow of the lesser trochanter
of the femur (Fig. 40-3B).
The round hypoechoic pulsatile femoral artery and compressible vein are
identified much more superficial and lateral to the sciatic nerve (Fig. 40-4B).
 |
|
Figure 40-3. Gluteal sciatic nerve block. A: Patient and probe positioning. B:
Transverse sonogram using a 2 to 5 MHz curved array transducer probe (Philips HDI 5000 system, Bothell, WA). GMM, gluteus maximus muscle; IB, ischial bone; IS, ischial spine; arrowhead, sciatic nerve. |
P.300
 |
|
Figure 40-4. Anterior sciatic nerve block. A: Patient and probe positioning. B:
Transverse sonogram using a 2 to 5 MHz curved array transducer probe (Philips HDI 5000 system, Bothell, WA). AMM, adductor magnus muscle; LT, lesser trochanter of the femur; arrowhead, sciatic nerve. |
Suggested Readings
Chan
VW, Nova H, Abbas S, McCartney CJ, Perlas A, Quan XD. Ultrasound
examination and localization of the sciatic nerve: a volunteer study. Anesthesiology 2006;104:309–314.
VW, Nova H, Abbas S, McCartney CJ, Perlas A, Quan XD. Ultrasound
examination and localization of the sciatic nerve: a volunteer study. Anesthesiology 2006;104:309–314.
Chelly JE, Delaunay L. A new anterior approach to the sciatic nerve block. Anesthesiology 1999;91:1655–1660.
Gray AT, Collins AB, Schafhalter-Zoppoth I. Sciatic nerve block in a child: a sonographic approach. Anesth Analg 2003;97:1300–1302.
Grechenig W, Clement HG, Peicha G, Klein A, Weiglein A. [Ultrasound anatomy of the sciatic nerve of the thigh]. Biomed Tech (Berl) 2000;45:298–303.
Marhofer
P, Schrogendorfer K, Wallner T, Koinig H, Mayer N, Kapral S.
Ultrasonographic guidance reduces the amount of local anesthetic for
3-in-1 blocks. Reg Anesth Pain Med 1998;23:584–588.
P, Schrogendorfer K, Wallner T, Koinig H, Mayer N, Kapral S.
Ultrasonographic guidance reduces the amount of local anesthetic for
3-in-1 blocks. Reg Anesth Pain Med 1998;23:584–588.
Peer
S, Kovacs P, Harpf C, Bodner G. High-resolution sonography of lower
extremity peripheral nerves: anatomic correlation and spectrum of
disease. J Ultrasound Med 2002;21:315–322.
S, Kovacs P, Harpf C, Bodner G. High-resolution sonography of lower
extremity peripheral nerves: anatomic correlation and spectrum of
disease. J Ultrasound Med 2002;21:315–322.
