Cervical Spine
-
Cervical spine injuries usually occur
secondary to high-energy mechanisms, including motor vehicle accident
(45%) and falls from a height (20%). -
Less commonly, cervical spine injuries
occur during athletic participation (15%), most notably during American
football and diving events, and as a result of acts of violence (15%). -
Neurologic injury occurs in 40% of patients with cervical spine fractures.
-
Spinal cord damage is more frequently associated with lower rather than upper cervical spine fractures and dislocations.
-
The atlas is
the first cervical vertebra, which has no body. Its two large lateral
masses provide the only two weight-bearing articulations between the
skull and the vertebral column.-
The tectoral membrane and the alar ligaments are the key to providing normal craniocervical stability.
-
The anterior tubercle is held adjacent to the odontoid process of C2 by the transverse atlantal ligament.
-
Fifty percent of total neck flexion and extension occurs at the occiput-C1 junction.
-
The vertebral artery emerges from the
foramen transversarium and passes between C1 and the occiput,
traversing a depression on the superior aspect of the C1 ring.
Fractures are common in this location.
-
-
The axis is the second cervical vertebra, whose body is the largest of the cervical vertebrae.
-
The transverse atlantal ligament (cruciform ligament) provides primary support for the atlantoaxial joint.
-
The alar ligaments are secondary stabilizers of the atlantoaxial joint.
-
The facet joint capsules at occiput-C1 and C1-C2 provide little support.
-
Fifty percent of total neck rotation occurs at the C1-C2 junction.
-
-
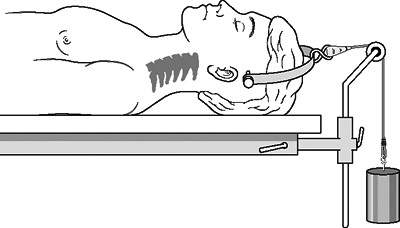
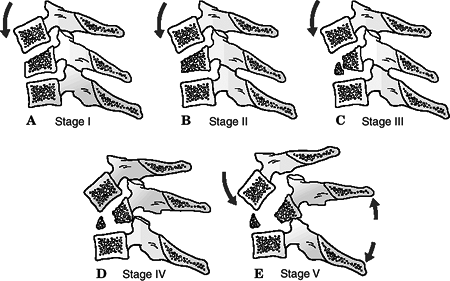
C3-C7 can be conceptualized as a three-column system (Denis) (Fig. 9.1):
-
Anterior column: The anterior vertebral
body and intervertebral disc resist compressive loads, while the
anterior longitudinal ligament and annulus fibrosis are the most
important checkreins to distractive forces (extension). -
Middle column: The posterior vertebral
body and uncovertebral joints resist compression, while the posterior
longitudinal ligament and annulus fibrosis limit distraction. -
Posterior column: The facet joints and
lateral masses resist compressive forces, while the facet joint
capsules, interspinous ligaments, and supraspinous ligaments counteract
distractive forces. -
The vertebral artery bypasses the empty
foramen transversarium of C7 to enter the vertebral foramina of C6-C1.
Injuries to the vertebral arteries are uncommon because of the
redundancy of the vessel.
P.82 -
 |
|
Figure
9.1. The components of the cervical three-column spine. The ligamentous complexes resist distractive forces. The bony structures counteract compression. (From Rockwood CA Jr, Green DP, Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 4th ed, vol. 2. Philadelphia: Lippincott-Raven, 1996:1489.)
|
-
Motor vehicle accidents (primarily in
young patients), falls (primarily in older patients), diving accidents,
and blunt trauma account for the majority of cervical spine injuries. -
Forced flexion or extension resulting
from unrestrained deceleration forces, with or without distraction or
axial compression, is the mechanism for most cervical spine injuries.
-
Patient assessment is indicated: airway, breathing, circulation, disability, and exposure (ABCDE).
-
Initiate resuscitation: Address life-threatening injuries. Maintain rigid cervical immobilization.
-
Tracheal intubation and central line
placement are often performed in the emergency setting. During
intubation, manipulation of the neck can potentially displace unstable
cervical fractures or dislocations. Manual in-line stabilization should
be maintained throughout the intubation process. Alternatively, mask
ventilation can be continued until fiberoptic or nasotracheal
intubation can be safely performed. If an unstable spine is highly
suspected, a cricothyroidotomy may be the safest alternative for airway
control. -
Evaluate the level of consciousness and neurologic impairment: Glasgow Coma Scale (see Chapter 2).
-
Assess head, neck, chest, abdominal, pelvic, extremity injury.
-
Ascertain the patient’s history:
mechanism of injury, witnessed head trauma, movement of
extremities/level of consciousness immediately following trauma, etc. -
Physical examination
-
Neck pain
-
Lacerations and contusions on scalp, face, or neck
-
-
Neurologic examinationP.83
-
Cranial nerves
-
Complete sensory and motor examination
-
Upper and lower extremity reflexes
-
Rectal examination: perianal sensation, rectal tone
-
Bulbocavernosus reflex (see Chapter 8)
-
-
Lateral cervical spine radiograph: This
will detect 85% of cervical spine injuries. One must visualize the
atlantooccipital junction, all seven cervical vertebrae, and the
cervicothoracic junction (as inferior as the superior aspect of T1).
This may necessitate downward traction on both upper extremities or a
swimmer’s view (upper extremity proximal to the x-ray beam abducted 180
degrees, axial traction on the contralateral upper extremity, and the
beam directed 60 degrees caudad). Patients complaining of neck pain
should undergo complete radiographic evaluation of the cervical spine,
including anteroposterior (AP) and odontoid views. On the lateral
cervical spine radiograph, one may appreciate:-
Acute kyphosis or loss of lordosis.
-
Continuity of radiographic “lines”:
anterior vertebral line, posterior vertebral line, facet joint line, or
spinous process line. -
Widening or narrowing of disc spaces.
-
Increased distance between spinous processes or facet joints.
-
Abnormal retropharyngeal swelling, which depends on the level in question:
-
At C1: >10 mm
-
At C3, C4: >4 mm
-
At C5, C6, C7: >15 mm
-
-
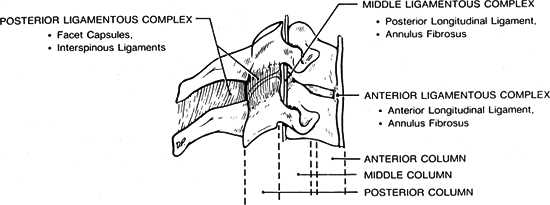
Radiographic markers of cervical spine instability, including the following:
-
Compression fractures with >25% loss of height
-
Angular displacements >11 degrees between adjacent vertebrae (as measured by Cobb angle)
-
Translation >3.5 mm
-
Intervertebral disc space separation >1.7 mm (Figs. 9.2 and 9.3)
-
-
-
Computed tomography (CT) and/or magnetic
resonance imaging (MRI) may be valuable to assess the upper cervical
spine or the cervicothoracic junction, especially if it is inadequately
visualized by plain radiography. -
The proposed advantages of CT over a
lateral cervical film as an initial screening tool are that it is more
sensitive for detecting fractures and more consistently enables
assessment of the occipitocervical and cervicothoracic junctions. A
potential disadvantage of CT as an initial radiographic assessment is
that subtle malalignment, facet joint gapping, or intervertebral
distraction is difficult to assess using axial images alone. -
The most useful applications of MRI are
in detecting traumatic disc herniation, epidural hematoma, spinal cord
edema or compression, and posterior ligamentous disruption. An
additional application of MRI is the ability to visualize vascular
structures.P.84MR arteriograms can be used to assess the patency of the vertebral arteries.![]() Figure
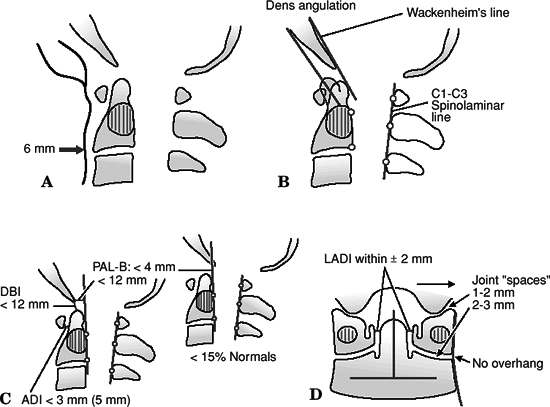
Figure
9.2. (A) Prevertebral soft tissue shadow. In a healthy recumbent adult
without an endotracheal tube, the prevertebral soft tissue shadow
should not exceed 6 mm. (B) Bony screening lines and dens angulation.
The anterior cortex of the odontoid should parallel the posterior
cortex of the anterior ring of the atlas. Any kyphotic or lordotic
deviation should be viewed with suspicion for an odontoid fracture or
transverse atlantal ligament disruption. Wackenheim line is drawn as a
continuation from the clivus caudally. The tip of the odontoid should
be within 1 to 2 mm of this line. The C1-C3 spinolaminar line’s
reference points are drawn from the anterior cortex of the laminae of
the atlas, axis, and C3 segments, which should fall within 2 mm of one
another. Greater deviation should raise suspicion of atlantoaxial
translation or disruption of the neural arches of either segment. (C)
Ligamentous injury reference lines (lateral x-rays). The atlas-dens
interval (ADI) should be less than 3 mm in an adult (5 mm in a child).
The space available for the cord is measured as the distance from the
posterior cortex of the odontoid tip to the anterior cortex of the
posterior arch of the atlas and should amount to more than 13 mm. The
dens-basion interval (DBI) is the distance between the odontoid tip and
the distal end of the basion. It should be less than 12 mm in adults.
The posterior axis line (PAL-B) should not be more than 4 mm anterior
and should be less than 12 mm posterior to the basion. (D) Bony
screening lines (anteroposterior imaging). The left and right lateral
atlas-dens intervals (LADIs) should be symmetric to one another (with
2-mm deviation). The bony components of the atlantooccipital joints
should be symmetric and should not be spaced more than 2 mm apart on
anteroposterior images. (Courtesy of Fred Mann, MD, Professor of
Radiology, University of Washington, Seattle.)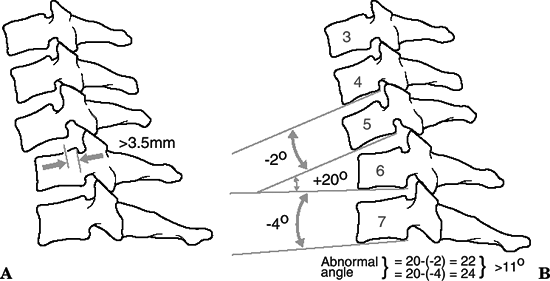 Figure
Figure
9.3. Radiographic indications of instability. Greater than 3.5 mm of
translation (A) or 11 degrees of angulation (B) and widening of the
separation between spinous processes are indications of instability on
the lateral plain film.(Adapted from Bucholz RW. Lower cervical spine injuries. In: Browner BD, Jupiter JB, Levine AM, et al. eds. Skeletal Trauma, vol. 1. Philadelphia: WB Saunders, 1992:707.) -
Stress flexion/extension radiographs
rarely if ever should be performed if instability is suspected; they
should be performed in the awake and alert patient only. In a patient
with neck pain, they are best delayed until spasm has subsided, which
can mask instability. The atlantodens interval (ADI) should be <3 mm
in adults and <5 mm in children. -
Traction x-rays are taken during reductions only.
-
As with other transitional regions of the
spine, the craniocervical junction is highly susceptible to injury.
This region’s vulnerability to injury is particularly high because of
the large lever-arm induced cranially by the skull and the relative
freedom of movement of the craniocervical junction, which relies
disproportionately on ligamentous structures rather than on intrinsic
bony stability.
-
These are frequently associated with C1 fractures as well as cranial nerve palsies.
-
The mechanism of injury involves
compression and lateral bending; this causes either compression
fracture of the condyle as it presses against the superior facet of C1
or avulsion of the alar ligament with extremes of atlantooccipital
rotation. -
CT is frequently necessary for diagnosis.
 |
|
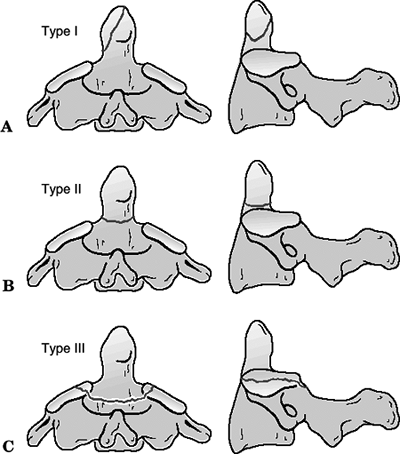
Figure
9.4. Anderson and Montesano classification of occipital condyle fractures. (A) Type I injuries are comminuted, usually stable, impaction fractures caused by axial loading. (B) Type II injuries are impaction or shear fractures extending into the base of the skull, and are usually stable. (C) Type III injuries are alar ligament avulsion fractures and are likely to be unstable distraction injuries of the craniocervical junction. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
| Type I: | Impaction of condyle; usually stable |
| Type II: | Shear injury associated with basilar or skull fractures; potentially unstable |
| Type III: | Condylar avulsion; unstable |
-
Treatment includes rigid cervical collar
immobilization for 8 weeks for stable injuries and halo immobilization
or occipital-cervical fusion for unstable injuries. -
Craniocervical dissociation should be considered with any occipital condyle fracture.
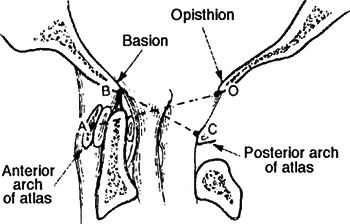 Figure 9.5. Powers ratio.(From Browner BD, Jupiter JB, Levine AM, et al. eds. Skeletal Trauma, vol. 1. Philadelphia: WB Saunders, 1992:668.)
Figure 9.5. Powers ratio.(From Browner BD, Jupiter JB, Levine AM, et al. eds. Skeletal Trauma, vol. 1. Philadelphia: WB Saunders, 1992:668.)
-
This is almost always fatal, with
postmortem studies showing it to be the leading cause of death in motor
vehicle accidents; rare survivors have severe neurologic deficits
ranging from complete C1 flaccid quadriplegia to mixed incomplete
syndromes such as Brown-Séquard. -
This is twice as common in children, owing to the inclination of the condyles.
-
It is associated with submental lacerations, mandibular fractures, and posterior pharyngeal wall lacerations.
-
It is associated with injury to the
cranial nerves (the abducens and hypoglossal nerves are most commonly
affected by craniocervical injuries), the first three cervical nerves,
and the vertebral arteries. -
The cervicomedullary syndromes, which
include cruciate paralysis as described by Bell and hemiplegia cruciata
initially described by Wallenberg, represent the more unusual forms of
incomplete spinal cord injury and are a result of the specific anatomy
of the spinal tracts at the junction of the brainstem and spinal cord.
Cruciate paralysis can be similar to a central cord syndrome, although
it normally affects proximal more than distal upper extremity function.
Hemiplegia cruciata is associated with ipsilateral arm and
contralateral leg weakness. -
Mechanism is a high-energy injury
resulting from a combination of hyperextension, distraction, and
rotation at the craniocervical junction. -
The diagnosis is often missed, but it may be made on the basis of the lateral cervical spine radiograph:
-
The tip of odontoid should be in line with the basion.
-
The odontoid-basion distance is 4 to 5 mm in adults and up to l0 mm in children.
-
Translation of the odontoid on the basion is never greater than 1 mm in flexion/extension views.
-
Powers ratio (BC/OA) should be <1 (Fig. 9.5).
-
In adults, widening of the prevertebral
soft tissue mass in the upper neck is an important warning sign of
significant underlying trauma and may be the only sign of this injury. -
Fine-cut CT scans with slices no more
than 2 mm wide are helpful to understand articular incongruities or
complex fracture patterns more clearly. MRI of the craniovertebral
junction is indicated for patients with spinal cord injury and can be
helpful to assess upper cervical spine ligamentous injuries as well as
subarachnoid and prevertebral hemorrhage.
P.88 -
-
Classification based on the position of the occiput in relation to C1 is as follows:
Type I: Occipital condyles anterior to the atlas; most common Type II: Condyles longitudinally dissociated from atlas without translation; result of pure distraction Type III: Occipital condyles posterior to the atlas -
The Harborview classification attempts to
quantify stability of craniocervical junction. Surgical stabilization
is reserved for type II and III injuries.Type I: Stable with displacement <2 mm Type II: Unstable with displacement <2 mm Type III: Gross instability with displacement >2 mm -
Immediate treatment includes halo vest
application with strict avoidance of traction. Reduction maneuvers are
controversial and should ideally be undertaken with fluoroscopic
visualization. -
Long-term stabilization involves fusion between the occiput and the upper cervical spine.
-
These are rarely associated with neurologic injury.
-
Instability invariably equates to the
presence of transverse alar ligament insufficiency, which can be
diagnosed either by direct means, such as by identifying bony avulsion
on CT scan or ligament rupture on MRI, or indirectly by identifying
widening of the lateral masses. -
Fifty percent of these injuries are
associated with other cervical spine fractures, especially odontoid
fractures and spondylolisthesis of the axis. -
Cranial nerve lesions of VI to XII and neurapraxia of the suboccipital and greater occipital nerves may be associated.
-
Vertebral artery injuries may cause symptoms of basilar insufficiency such as vertigo, blurred vision, and nystagmus.
-
Patients may present with neck pain and a subjective feeling of “instability.”
-
The mechanism of injury is axial
compression with elements of hyperextension and asymmetric loading of
condyles causing variable fracture patterns. -
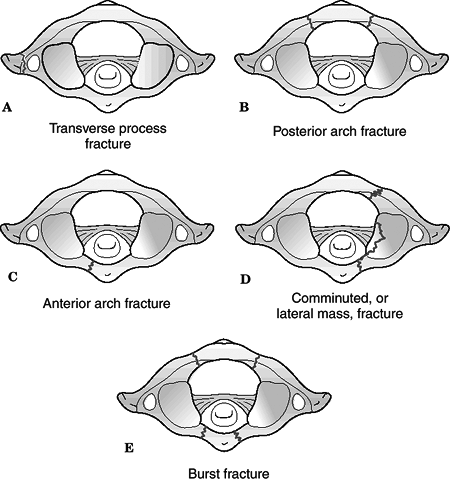
Classification (Levine) (Fig. 9.6)
-
Isolated bony apophysis fracture
-
Isolated posterior arch fracture
-
Isolated anterior arch fracture
-
Comminuted lateral mass fracture
-
Burst fracture
-
-
Treatment
![]() Figure
Figure
9.6. Classification of atlas fractures (according to Levine). (A)
Isolated bony apophysis fracture. (B) Isolated posterior arch fracture.
(C) Isolated anterior arch fracture. Comminuted lateral mass fracture
(D) and burst fracture (E), three or more fragments.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)-
Initial treatment includes halo traction/immobilization.
-
Stable fractures (posterior arch or
nondisplaced fractures involving the anterior and posterior portions of
the ring) may be treated with a rigid cervical orthosis. -
Less stable configurations (asymmetric
lateral mass fracture with “floating” lateral mass, burst fractures)
may require prolonged halo immobilization. -
C1-C2 fusion may be necessary to alleviate chronic instability and/or pain.
-
-
This rare, usually fatal injury, is seen mostly in older age groups (50s to 60s).
-
The mechanism of injury is forced flexion.
-
The clinical picture ranges from severe neck pain to complete neurologic compromise.
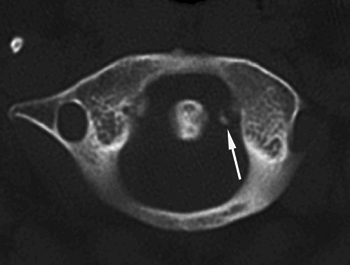 Figure 9.7. Axial CT image demonstrating transverse ligament rupture with atlanto-axial subluxation(Reproduced with permission from Bucholz RW, Heckman JD, Court-Brown C, et al. eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams Wilkins, 2006.)
Figure 9.7. Axial CT image demonstrating transverse ligament rupture with atlanto-axial subluxation(Reproduced with permission from Bucholz RW, Heckman JD, Court-Brown C, et al. eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams Wilkins, 2006.) -
Rupture of the transverse ligament may be determined by:
-
Visualizing the avulsed lateral mass fragment on CT scan.
-
Atlantoaxial offset >6.9 mm on an odontoid radiograph.
-
ADI >3 mm in adults. An ADI >5 mm in adults also implies rupture of the alar ligaments.
-
Direct visualization of the rupture on MRI.
-
-
Treatment
-
Initial treatment includes halo traction/immobilization.
-
In the cases of avulsion, halo immobilization is continued until osseous healing is documented.
-
C1-C2 fusion is indicated for tears of the transverse ligament without bony avulsion, chronic instability, or pain (Fig. 9.7)
-
-
In this rare injury, patients present
with confusing complaints of neck pain, occipital neuralgia, and,
occasionally, symptoms of vertebrobasilar insufficiency. In chronic
cases, the patient may present with torticollis. -
It is infrequently associated with neurologic injury.
-
The mechanism of injury is
flexion/extension with a rotational component, although in some cases
it can occur spontaneously with no reported history of trauma. -
Odontoid radiographs may show asymmetry
of C1 lateral masses with unilateral facet joint narrowing or overlap
(wink sign). The C2 spinous process may be rotated from the midline on
an AP view. -
The subluxation may be documented on
dynamic CT scans; failure of C1 to reposition on a dynamic CT scan
indicates fixed deformity. -
Classification (Fielding)
Type I: Odontoid as a pivot point; no neurologic injury; ADI <3 mm; transverse ligament intact (47%) Type II: Opposite facet as a pivot; ADI <5 mm; transverse ligament insufficient (30%) Type III: Both joints anteriorly subluxed; ADI >5 mm; transverse and alar ligaments incompetent Type IV: Rare; both joints posteriorly subluxed Type V: Levine and Edwards: frank dislocation; extremely rare -
Treatment
-
Cervical halter traction in the supine
position and active range-of-motion exercises for 24 to 48 hours
initially are followed by ambulatory orthotic immobilization with
active range-of-motion exercises until free motion returns. -
Rarely, fixed rotation with continued symptoms and lack of motion indicates a C1-C2 posterior fusion
-
-
A high association exists with other cervical spine fractures.
-
There is a 5% to10% incidence of
neurologic involvement with presentation ranging from Brown-Séquard
syndrome to hemiparesis, cruciate paralysis, and quadriparesis. -
Vascular supply arrives through the apex of the odontoid and through its base with a watershed area in the neck of the odontoid.
-
High-energy mechanisms of injury include
motor vehicle accident or falls with avulsion of the apex of the dens
by the alar ligament or lateral/oblique forces that cause fracture
through the body and base of the dens. -
Classification: (Anderson and D’Alonzo) (Fig. 9.8).
Type I: Oblique avulsion fracture of the apex (5%) Type II: Fracture at the junction of the body and the neck; high nonunion rate, which can lead to myelopathy (60%) Type IIA: Highly unstable comminuted injury extending from the waist of the odontoid into the body of the axis Type III: Fracture extending into the cancellous body of C2 and possibly involving the lateral facets (30%) -
Treatment
Type I: If it is an isolated injury, stability of the fracture pattern allows for immobilization in a cervical orthosis. Type II: This is controversial, because
the lack of periosteum and cancellous bone and the presence in
watershed area result in a high incidence of nonunion (36%). Risk
factors include age >50 years, >5 mm displacement, and posterior
displacement. It may require screw fixation of the odontoid or C1-C2
posterior fusion for adequate treatment. Nonoperative treatment is halo
immobilization.Type III: There is a high likelihood of union with halo immobilization owing to the cancellous bed of the fracture site.
 |
|
Figure
9.8. The odontoid fracture classification of Anderson and D’Alonzo. (A) Type I fractures of the odontoid tip represent alar ligament avulsions. (B) Type II fractures occur at the odontoid waist, above the C2 lateral masses. (C) Type III fractures extend below the odontoid waist to involve the body and lateral masses of C2. Hadley has added the type IIA fracture with segmental comminution at the base of the odontoid (not shown) (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
Patients often present with neck pain, limited range of motion, and no neurologic injury.
-
The mechanisms of injury are axial compression and lateral bending.
-
CT is helpful for diagnosis.
-
A depression fracture of the C2 articular surface is common.
-
Treatment ranges from collar immobilization to late fusion for chronic pain.
-
This is associated with a 30% incidence
of concomitant cervical spine fractures. It may be associated with
cranial nerve, vertebral artery, and craniofacial injuries. -
The incidence of spinal cord injury is low with types I and II and high with type III injuries.
-
The mechanism of injury includes motor
vehicle accidents and falls with flexion, extension, and axial loads.
This may be associated with varying degrees of intervertebral disc
disruption. Hanging mechanisms involve hyperextension and distraction
P.93
injury,
in which the patient may experience bilateral pedicle fractures and
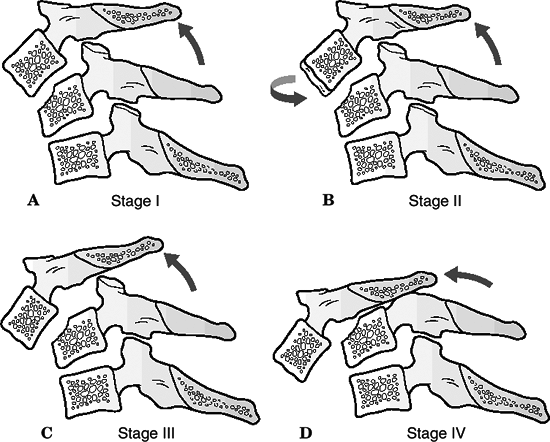
complete disruption of disc and ligaments between C2 and C3.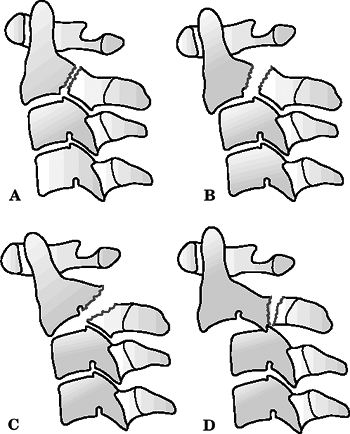 Figure
Figure
9.9. Classification of traumatic spondylolisthesis of the axis
(hangman’s fracture) (according to Effendi, modified by Levine). (A)
Type I, nondisplaced fracture of the pars interarticularis. (B) Type
II, displaced fracture of the pars interarticularis. (C) Type IIa,
displaced fracture of the pars interarticularis with disruption of the
C2-C3 discoligamentous complex. (D) Type III, dislocation of C2-C3
facets joints with fractured pars interarticularis(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Classification (Levine and Edwards; Effendi) (Fig. 9.9)
Type I: Nondisplaced, no angulation; translation <3 mm; C2-C3 disc intact (29%); relatively stable Type Ia: Atypical unstable lateral
bending fractures that are obliquely displaced and usually involve only
one pars interarticularis, extending anterior to the pars and into the
body on the contralateral sideType II: Significant angulation at
C2-C3; translation >3 mm; most common injury pattern; unstable;
C2-C3 disc disrupted (56%); subclassified into flexion, extension, and
listhetic typesType IIA: Avulsion of entire C2-C3
intervertebral disc in flexion with injury to posterior longitudinal
ligament, leaving the anterior longitudinal ligament intact; results in
severe angulation; no translation; unstable; probably caused by
flexion-distraction injury (6%); traction contraindicatedType III: Rare; results from initial
anterior facet dislocation of C2 on C3 followed by extension injury
fracturing the neural arch; results in severe angulation and
translation with unilateral or bilateral facet dislocation of C2-C3;
unstable (9%); type III injuries most commonly associated with spinal
cord injury -
Treatment
Type I: This usually requires rigid cervical orthosis for up to 6 weeks. Type II: This is determined by
stability; it usually requires halo traction/immobilization with serial
radiographic confirmation of reduction for at least 6 weeks.Type IIA: Traction may exacerbate the condition; therefore, only immobilization may be indicated. Type III: Initial halo traction is followed by open reduction and posterior fusion of C2-C3, with possible anterior fusion.
-
Vertebral bodies have a superior cortical
surface that is concave in the coronal plane and convex in the sagittal
plane, allowing for flexion, extension, and lateral tilt by the gliding
motion of the facets. -
The uncinate process projects superiorly
from the lateral aspect of the vertebral body. With degenerative
changes, these may articulate with the superior vertebra, resulting in
an uncovertebral joint (of Luschka). -
The mechanism of injury includes motor vehicle accidents, falls, diving accidents, and blunt trauma.
-
Radiographic evaluation consists of AP,
lateral, and odontoid views of the cervical spine, as described earlier
in the section on radiographic evaluation of cervical spine
instability).-
If cervical spine instability is
suspected, flexion/extension views may be obtained in a willing,
conscious, and cooperative patient without neurologic compromise. A
“stretch” test (Panjabi and White) may be performed with longitudinal
cervical traction. An abnormal test is indicated by a greater than
1.7-mm interspace separation or a >7.5-degree change between
vertebrae. -
CT scans with reconstructions may be obtained to characterize fracture pattern and degree of canal compromise more clearly.
-
MRI may be undertaken to delineate spinal cord, disc, and canal abnormalities further.
-
The amount of normal cervical motion at
each level has been extensively described, and this knowledge can be
important in assessing spinal stability after treatment.
Flexion-extension motion is greatest at the C4-5 and C5-6 segments,
averaging about 20 degrees. Axial rotation ranges from 2 to 7 degrees
at each of the subaxial motion segments; the majority (45% to 50%) of
rotation occurs at the C1-C2 articulation. Lateral flexion is 10 to 11
degrees per level in the upper segments (C2-5). Lateral motion
decreases caudally, with only 2 degrees observed at the cervicothoracic
junction.
-
 |
|
Figure 9.10. (A–E) The five stages of compression flexion injuries.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
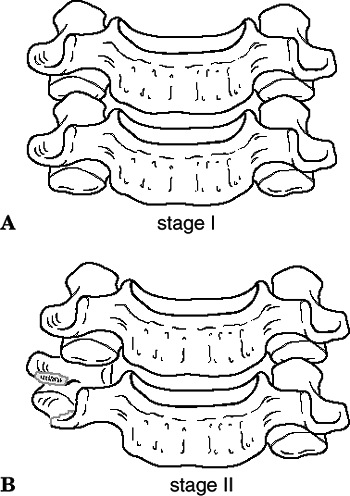
Compressive flexion (shear mechanism resulting in “teardrop” fractures)
Stage I: Blunting of anterior body; posterior elements intact Stage II: “Beaking” of the anterior body; loss of anterior vertebral height Stage III: Fracture line passing from anterior body through the inferior subchondral plate Stage IV: Inferoposterior margin displaced <3 mm into the neural canal Stage V: “Teardrop” fracture;
inferoposterior margin >3 mm into the neural canal; failure of the
posterior ligaments and the posterior longitudinal ligament -
Vertical compression (burst fractures) (Fig. 9.11)
Stage I: Fracture through the superior or inferior endplate with no displacement Stage II: Fracture through both endplates with minimal displacement Stage III: Burst fracture; displacement of fragments peripherally and into the neural canal -
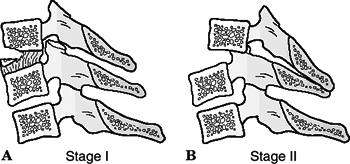
Distractive flexion (dislocations) (Fig. 9.12)
Stage I: Failure of the posterior ligaments, divergence of the spinous processes, and facet subluxation Stage II: Unilateral facet dislocation; translation always <50% Stage III: Bilateral facet dislocation; translation of 50% and “perched” facets Stage IV: Bilateral facet dislocation with 100% translation -
Compressive extension (Fig. 9.13)
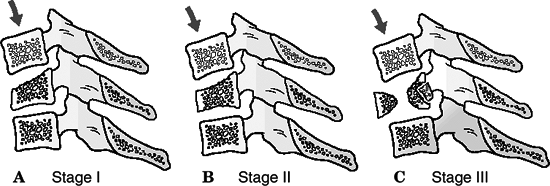 Figure 9.11. (A–C) The three stages of vertical compression injuries.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 9.11. (A–C) The three stages of vertical compression injuries.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)Stage I: Unilateral vertebral arch fracture Stage II: Bilateral laminar fracture without other tissue failure Stages III, IV: Theoretic continuum between stages II and V Stage V: Bilateral vertebral arch
fracture with full vertebral body displacement anteriorly; ligamentous
failure at the posterosuperior and anteroinferior margins![]() Figure 9.12. (A–D) The four stages of distraction flexion injuries.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 9.12. (A–D) The four stages of distraction flexion injuries.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Distractive extension (Fig. 9.14)
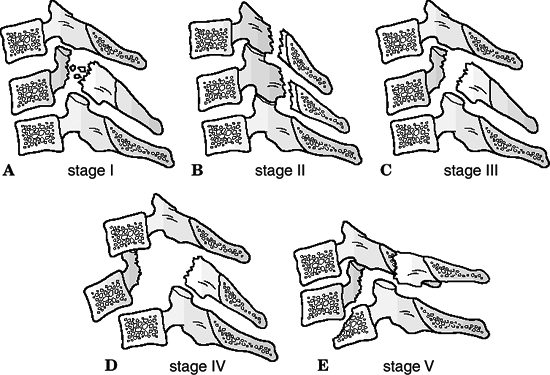 Figure 9.13. (A–E) The five stages of compression extension injuries.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 9.13. (A–E) The five stages of compression extension injuries.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)Stage I: Failure of anterior
ligamentous complex or transverse fracture of the body; widening of the
disc space and no posterior displacementStage II: Failure of posterior ligament complex and superior displacement of the body into the canal ![]() Figure 9.14. (A and B) The two stages of distraction extension injuries.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 9.14. (A and B) The two stages of distraction extension injuries.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Lateral flexion (Fig. 9.15)
Stage I: Asymmetric, unilateral
compression fracture of the vertebral body plus a vertebral arch
fracture on the ipsilateral side without displacementStage II: Displacement of the arch on the AP view or failure of the ligaments on the contralateral side with articular process separation -
Miscellaneous cervical spine fractures
 Figure
Figure
9.15. Lateral flexion injuries. Blunt trauma from the side places the
ipsilateral spine in distraction while compressing the contralateral
spine. (A) Stage I injury, asymmetric centrum fracture with a
unilateral arch fracture. (B) Stage II injury, with displacement of the
body and contralateral ligamentous failure.(Adapted from Rizzolo SJ, Cotler JM. Unstable cervical spine injuries: specific treatment approaches. J Am Acad Orthop Surg 1993;1:57–66.)-
“Clay shoveler’s” fracture: This is an
avulsion of the spinous processes of the lower cervical and upper
thoracic vertebrae. Historically, this resulted from muscular avulsion
during shoveling in unyielding clay with force transmission through the
contracted shoulder girdle. Treatment includes restricted motion and
symptomatic treatment until clinical improvement or radiographic
healing of the spinous process occurs. -
Sentinel fracture: This fracture occurs
through the lamina on either side of the spinous process. A loose
posterior element may impinge on the cord. Symptomatic treatment only
is indicated unless spinal cord compromise exists. -
Ankylosing spondylitis: This may result
in calcification and ossification of the ligamentous structures of the
spine, producing “chalk stick” fractures after trivial injuries. These
fractures are notoriously unstable because they tend to occur through
brittle ligamentous structures. Treatment includes traction with
minimal weight in flexion, with aggressive immobilization with either
halo vest or open stabilization. -
Gunshot injuries: Missile impact against
bony elements may cause high-velocity fragmentation frequently
associated with gross instability and complete spinal cord injury.
Surgical extraction of missile fragments is rarely indicated in the
absence of canal compromise. Missiles that traverse the esophagus or
pharynx should be removed, with
P.99
aggressive
exposure and debridement of the missile tract. These injuries carry
high incidences of abscess formation, osteomyelitis, and mediastinitis.
-
-
Immobilization with a cervical orthosis
(for stable fractures) or Gardner-Wells tong traction (for unstable
injuries) should be maintained in the emergency setting before CT for
evaluation of spinal and other system injuries. -
Vasopressor support is indicated for suspected neurogenic shock and emergency assessment for potential intracranial trauma.
-
Patients with neurologic injuries should
be considered for intravenous methylprednisolone per the NASCIS II and
III protocol (30 mg/kg loading dose and then 5.4 mg/kg for 24 hours if
started within 3 hours, for 48 hours if started within 8 hours.
Steroids have no benefit if they are started more than 8 hours after
injury). -
The majority of cervical spine fractures
can be treated nonoperatively. The most common method of nonoperative
treatment is immobilization in a cervical orthosis. In reality,
orthoses decrease motion rather than effect true immobilization. Motion
at the occipital-cervical junction is slightly increased by most
cervical collars.-
Soft cervical orthosis: This produces no significant immobilization and is a supportive treatment for minor injuries.
-
Rigid cervical orthosis (Philadelphia
collar): This is effective in controlling flexion and extension;
however, it provides little rotational or lateral bending stability. -
Poster braces: These are effective in controlling midcervical flexion, with fair control in other planes of motion.
-
Cervicothoracic orthoses: These are
effective in flexion and extension and rotational control, with limited
control of lateral bending. -
Halo device: This provides the most rigid immobilization (of external devices) in all planes.
-
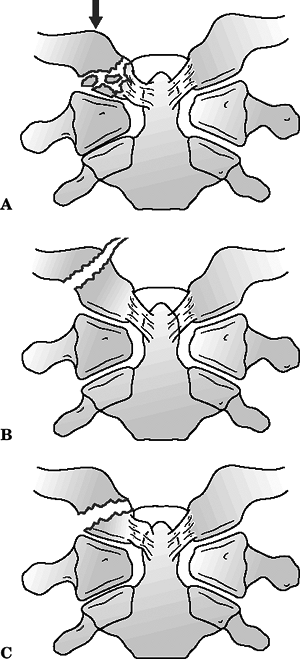
For traction, Gardner-Wells tongs are
applied one finger’s width above the pinna of the ear in line with the
external auditory canal. Slight anterior displacement will apply an
extension force, whereas posterior displacement will apply a flexion
force, useful when reducing facet dislocations (Fig. 9.16). -
Numerous complications are associated
with use of cervical collars. Skin breakdown at bony prominences, in
particular the occiput, mandible, and sternum can occur. Up to 38
percent of patients with severe closed head injuries can develop skin
complications with prolonged use.
-
-
Patients with neural deficits from
burst-type injuries: Traction is used to stabilize and indirectly
decompress the canal via ligamentotaxis. -
Patients with unilateral or bilateral
facet dislocations and complete neural deficits: Gardner-Wells tong
traction and reduction by sequentially increasing the amount of
traction are indicated. -
Traction is contraindicated in distractive cervical spine injuries and type IIA spondylolisthesis injuries of C2.
-
Patients with incomplete neural deficits
or who are neurologically intact with unilateral and bilateral facet
dislocations require MRI before reduction via traction to evaluate for
a herniated disc, especially if a patient is not awake and alert and
able to cooperate with serial examinations during reduction maneuvers.![]() Figure
Figure
9.16. Closed reduction technique. Diagram of cranial tong technique for
maintaining alignment and stability of the spine. Weight is increased
gradually with a maximum of 45 to 50 lb (10 lb for the head and 5 lb
for each successive interspace). Patients with an unrevealing
examination may require a magnetic resonance imaging scan before
reduction to rule out a space-occupying lesion in the vertebral canal.
Failure of reduction may also necessitate such a scan.(Adapted from Bucholz RW. Lower cervical spine injuries. In: Browner BD, Jupiter JB, Levine AM, et al., eds. Skeletal Trauma, vol. 1. Philadelphia: WB Saunders, 1992:638.) -
A halo has been recommended for patients
with isolated occipital condyle fractures, unstable atlas ring
fractures, odontoid fractures, and displaced neural arch fractures of
the axis. -
The halo vest relies on a tight fit of
the vest around the torso and is poorly tolerated by elderly patients
and patients with pulmonary compromise or thoracic deformities, such as
those with ankylosing spondylitis. -
The halo ring should be applied 1 cm
above the ears. Anterior pin sites should be placed below the equator
of the skull above the supraorbital ridge, anterior to the temporalis
muscle, and over the lateral two-thirds of the orbit. Posterior sites
are variable and are placed to maintain horizontal orientation of the
halo. Pin pressure should be 6 to 8 lb in the adult and should be
tightened at 48 hours and monthly thereafter. Pin care is essential. -
Prolonged recumbence carries an increased
morbidity and mortality risk, and consideration should be given to the
use of a RotoRest bed and mechanical as well as pharmacologic
thromboprophylaxis. -
Because of the normally wide spinal canal
diameter, decompression of neural elements in upper cervical spine
fractures is not commonly required for traumatic conditions. -
The optimal time to perform surgery,
particularly in patients with neurologic deficits, remains unclear. The
two most commonly proposed benefits of earlier versus later surgery are
improved rates of neurologic recovery and improved ability to mobilize
the patient without concern of spinal displacement. To date, little
human clinical evidence supports the view that early surgical
decompression and stabilization improve neurologic recovery rates.
However, clinical series have demonstrated that surgery performed as
soon as 8 hours after injury does not appear to increase the rate of
complications or lead to neurologic decline.
-
The mainstay of operative treatment of
upper cervical fractures and dislocations remains fusion with
instrumentation, most commonly performed from the posterior approach.
In order of frequency, the most common upper cervical fusion procedures
are atlantoaxial fusion, occipitocervical fusion, and least commonly,
C1-C3 fusion. -
Fusion of the occiput-C1 limits 50% of flexion and extension.
-
Fusion of C1-C2 limits 50% of rotation.
-
Screw fixation of a type II odontoid fracture
-
Anterior interbody fusion and plating of the C2-3 interspace for a type IIA or III hangman’s fracture
-
Anterior arthrodesis of the atlantoaxial
articulations as a rare salvage procedure for failed posterior
atlantoaxial fusion at-tempts
-
Modified Brooks or Gallie arthrodesis uses sublaminar wires and a bone graft between the arches of C1 and C2.
-
Flexion control is obtained via the
wires, extension via the bone blocks, and rotation via friction between
the bone blocks and the posterior arches.
-
-
Transarticular screws are effective, especially if the posterior elements of C1 and C2 are fractured.
-
The two indications for direct fracture
repair in the upper cervical spine involve the treatment of type II
odontoid fractures or type II traumatic spondylolistheses of C2 with
interfragmentary screw fixation. -
This is not indicated for fixation of anteriorly displaced odontoid fractures.
-
Fifty percent of flexion/extension and 50% of rotation are evenly divided between each of the facet articulations.
-
Fusion of each level reduces motion by a proportionate amount.
-
Posterior decompression and fusion:
-
The posterior approach to the cervical
spine is a midline, extensile approach that can be used to access as
many spinal levels as necessary, with a variety of instrumentation
techniques in use. -
In the majority of acute, traumatic,
subaxial spinal injuries, posterior decompression via laminectomy is
not necessary. Canal compromise is most frequently caused by
dislocation, translation, or retropulsed vertebral body fragments. In
rare cases of anteriorly displaced posterior arch fragments,
laminectomy would be indicated to directly remove the offending
compressive elements. This is not true, however, in cases of acute
spinal cord injury associated with multilevel spondylotic stenosis or
ossification of the posterior longitudinal ligament, in which a
posterior decompressive procedure may be considered the procedure of
choice if cervical lordosis has been maintained. -
Open reduction of dislocated facet joints is typically performed using a posterior approach.
-
-
Bilateral lateral mass plating
-
This can be utilized for a variety of
fractures including facet fractures, facet dislocations, and “teardrop”
(compressive flexion stage V) fractures. -
Single-level fusions are sufficient for dislocations, although multilevel fusions may be required for more unstable patterns.
-
This can stop fusion at levels with
fractured spinous processes or laminae, thus avoiding the fusion of
extra levels with consequent loss of motion.
-
-
Anterior decompression and fusion
-
These are used for vertebral body burst fractures with spinal cord injury and persistent anterior cord compression.
-
The anterior approach to the subaxial
spine utilizes the interval plane between the sternocleidomastoid
(lateral) and anterior strap (medial) muscles. Deeper, the interval of
dissection is between the carotid sheath laterally and the
trachea/esophagus medially. -
MRI, myelography, and CT are valuable in preoperative assessment of bony and soft tissue impingement on the spinal cord.
-
A simple discectomy or corpectomy in
which osseous fragments are removed from the canal and a tricortical
iliac or fibular graft placed between the vertebral bodies by a variety
of techniques can be performed. -
In the presence of a herniated cervical
disc associated with dislocated facet joints, one may elect to perform
an anterior discectomy and decompression before facet reduction. -
Anterior plating or halo vest immobilization adds stability during healing.
-