Radial Head Fractures
of radial head fracture by internal fixation has become increasingly
accepted (6). As the procedure is now well accepted, several fixation devices and strategies may be used (3,4,5,15). The major burden on the surgeon is the proper patient selection as well as meticulous technique.
-
Fracture type. The best indication for open reduction and internal fixation is a Mason type II radial head fracture (4,9,11,14,15).
This includes a fracture of less than 30% of the radial head, or the
classic “slice fracture” that is displaced more than 3 mm. -
Associated injury causing instability (8,11,13,17,19).
These complications include associated elbow dislocation, isolated
medial collateral ligament disruption, and Essex-Lopresti injury. This
topic is dealt with in detail in Chapter 7. -
Age. All type
II radial head fractures may be considered amenable for open reduction
and internal fixation in those under 50 to 55 years of age. Type II
fractures with associated instability should be fixed at virtually any
age (Chapter 7).
This problem is best suited for implant replacement. As improved radial
head implants are being developed and with increased understanding of
“complex instability,” we include the technique for prosthetic implant
replacement later in this chapter.
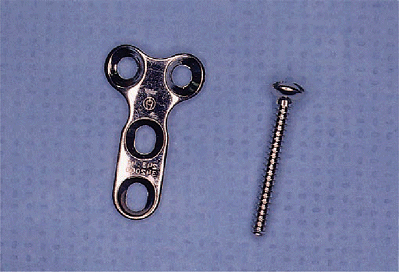
The Herbert screw is available and might be used. It has the advantage
of stabilizing the fracture before insertion of the screw, but it is
expensive. It is not necessary to have both systems available.
injury has occurred. The effect of radial head fixation is usually
adequate in most instances, so direct ligamentous repair is not
necessary. If the elbow remains unstable after radial head fracture
fixation, one might be prepared for the concurrent application of a
distraction device (see Chapter 8).
must be assessed. After the radial head fracture has been treated the
injury at the wrist is managed either by reduction and splinting in
full supination, by cross-pinning of the ulna, or by direct suture of
the triangular fibrocartilage (20).
extremity is prepared and draped with a nonsterile tourniquet. An arm
table may be used. I prefer the position described for other
reconstructive procedures with the patient being in the supine position
and the arm being brought across the chest.
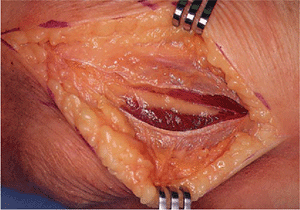
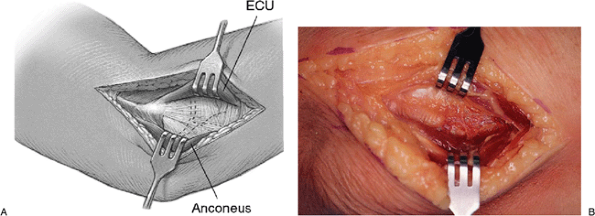
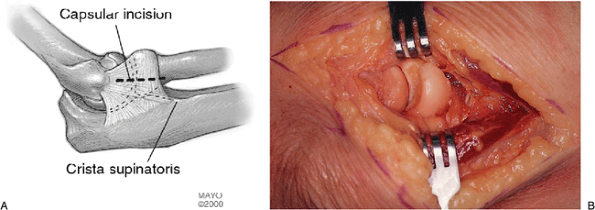
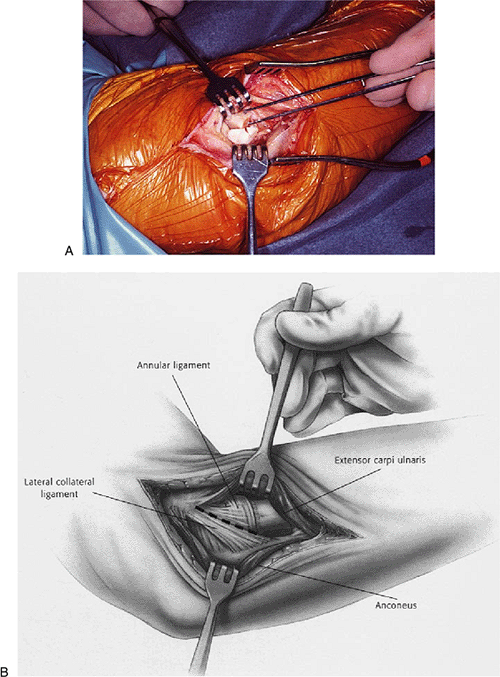
A portion of the extensor carpi ulnaris is elevated sufficiently to
allow exposure of the lateral collateral ligament complex (Fig. 5-5). If it has not been
torn by the injury, an incision is made in the capsule anterior to the lateral complex that attaches to the ulna (Fig. 5-6).
If the elbow is stable, sufficient reflection of the common extensor
tendon is necessary to allow adequate exposure of the radial head. A
band is used to reflect the common extensor tendon, and a small rake
retracts the inferior posterior aspect of the capsule.
 |
|
Figure 5-1.
Most fractures are managed with the 2.7-mm miniscrew system, which includes a countersink to lessen the likelihood of screw head prominence. |
 |
|
Figure 5-2.
With the patient in a supine position with the arm brought across the chest, the distal portion of the Kocher incision is made over the radial head and over the lateral epicondyle. |
 |
|
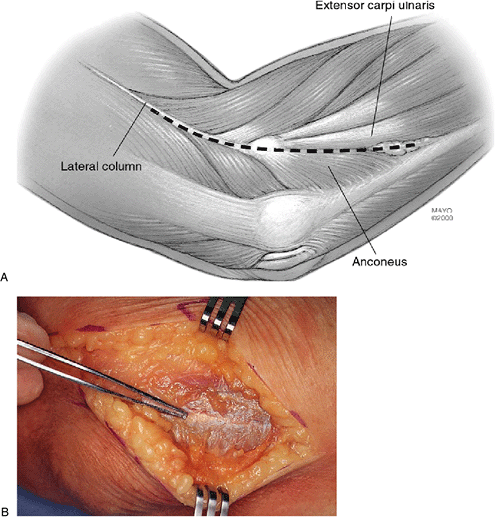
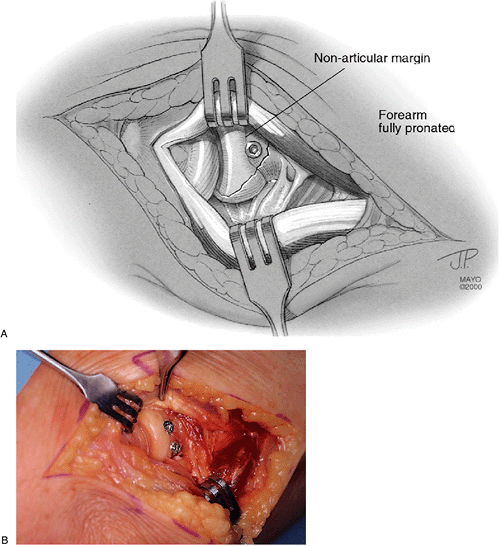
Figure 5-3. A,B: The interval between the anconeus and extensor carpi ulnaris is well visualized here.
|
 |
|
Figure 5-4. This interval is entered and the muscles are retracted.
|
 |
|
Figure 5-5. A,B:
Sharp dissection of the extensor carpi ulnaris and minimal elevation of the anconeus by a periosteal elevator reveals the lateral capsule. |
fragments without soft tissue, they may be removed from the wound and
the surface cleansed with a water pick (Fig. 5-6).
If the soft tissue remains on any of the loose fragments, great care is
taken to maintain this as a source of blood supply to the fragment. If
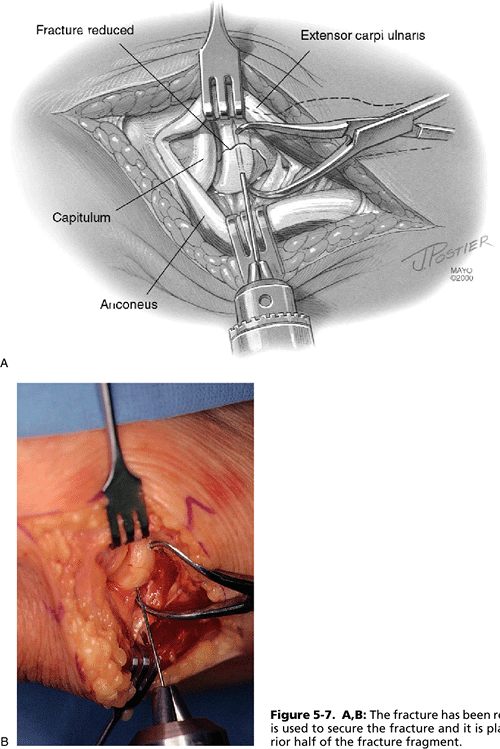
there is a single slice fracture, it is readily fixed to the remaining
portion of the radial head. The articular surface is reduced
anatomically and held with a tenaculum (Fig. 5-7).
The cortical elements are likewise reduced anatomically. It should be
noted that as with tibial plafond fractures, there may be a plastic
deformation of the articular surface such that the articular surface
and the cortical margins may not simultaneously appear to be
anatomically reduced. In this instance, preference is, of course, given
to the anatomic reduction of the articular surface. The reduced
fracture fragment
is stabilized with a single 0.425 K-wire. This is placed through the anterior half of the fragment (Fig. 5-7).
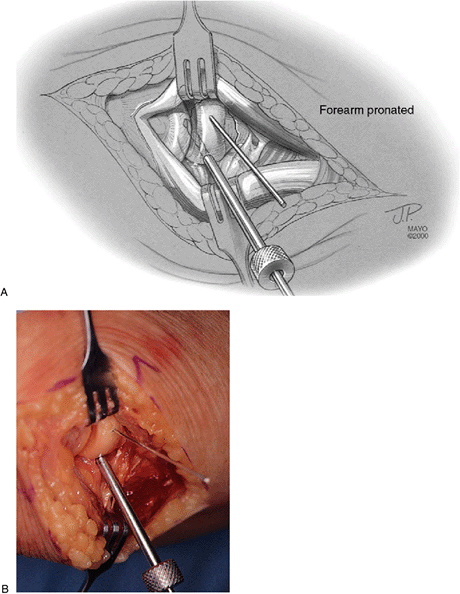
The forearm is then rotated to expose the remainder of the fractured
segment. A 2.0-mm hole is first drilled using a tissue protector (Fig. 5-8).
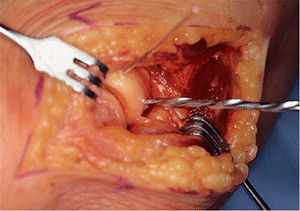
The precise depth of the screw hole is determined with the depth gauge,
and the fracture fragment is then overdrilled with a 2.7-mm drill (Fig. 5-9). The hole is tapped (Fig. 5-10) and countersunk with a hand-held instrument (Fig. 5-11) and the appropriate-length screw is inserted (Fig. 5-12).
The forearm is slightly supinated, the K-wire is removed, and an
identical technique is used to insert a second screw parallel to the
first in the region of the K-wire.
 |
|
Figure 5-6. The lateral capsule is opened just anterior to the lateral complex, which originates at the humerus and attaches to the ulna (A). The fracture has been identified and the hematoma cleaned with a water pick (B).
|
 |
|
Figure 5-7. A,B:
The fracture has been reduced. A K-wire is used to secure the fracture and it is placed in the anterior half of the fracture fragment. |
 |
|
Figure 5-8. A,B:
The forearm is slightly pronated, exposing the posterior half of the fracture fragment. A drill sleeve is used and a 2.0-mm drill bit is employed. |
 |
|
Figure 5-9.
A 2.7-mm drill bit is then used to overdrill the fracture fragment to receive the 2.7-mm screw. Care should be taken not to split small slice fracture fragments with the overdrilling process. |
 |
|
Figure 5-10. The screw hole is tapped to receive the 2.7-mm screw.
|
 |
|
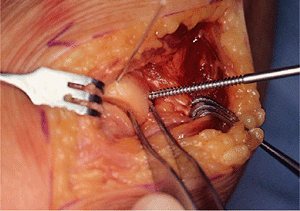
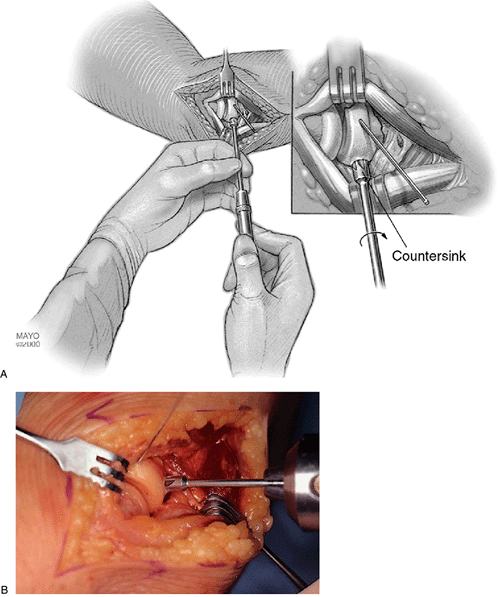
Figure 5-11. A,B: A hand-held countersink instrument is used so that the screw head fits flush with the surface of the fracture fragment.
|
 |
|
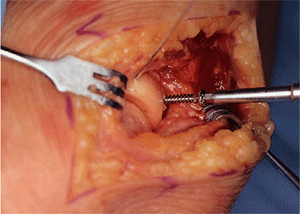
Figure 5-12.
A 2.7-mm screw is then inserted across the fracture fragment, preferably perpendicular to the fracture surface. The errors in screw length should be with the screw slightly short rather than slightly long. Anticipation of the slightly increased depth of insertion after the countersink should also be taken into consideration. |
fragments are first reduced and stabilized by reduction to the larger
fragment. This may then be stabilized with a small K-wire or a
bone-holding clamp. A sharp towel clip may also be used. The mini-AO
screws are used to compress the fracture fragments to the stable
column. Particular care is taken to avoid the screw extending past the
cortex on the opposite side.
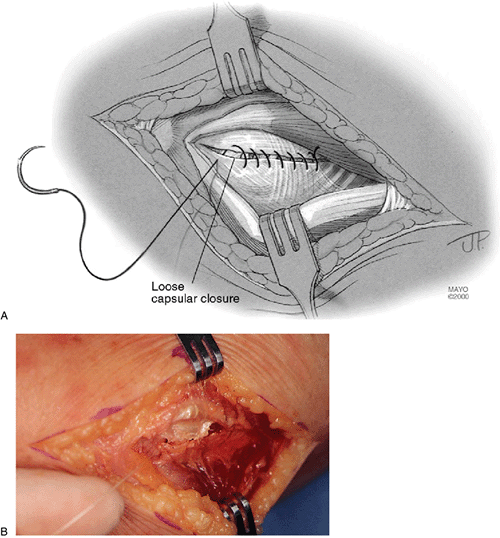
in the lateral capsule. The lateral ulnar collateral ligament (LUCL)
complex must be assessed to assure competency. Incisions anterior to
the LUCL protect this structure if it was not torn at the time of
radial head fracture. The final closure should not be so tight as to
cause restriction of pronation and supination. This should be tested
after closure of the capsule to ensure there is not excessive friction
or compression with the radial head (Fig. 5-13).
An intraarticular drain is placed and absorbable sutures are used to
close the Kocher’s interval. Subcutaneous tissue and skin are closed in
a routine fashion.
 |
|
Figure 5-13. A,B:
The annular ligament is only loosely closed. Great care should be taken not to overlap this structure, as it may be a source of irritation with subsequent pronation and supination. |
 |
|
Figure 5-14.
Note the screw going through the nonarticular portion of the margin of the radial head with the broader portion that articulates with the lesser sigmoid notch appearing below (A). Both screws have been inserted and are flush with the surface, and they are not a source of irritation (B). |
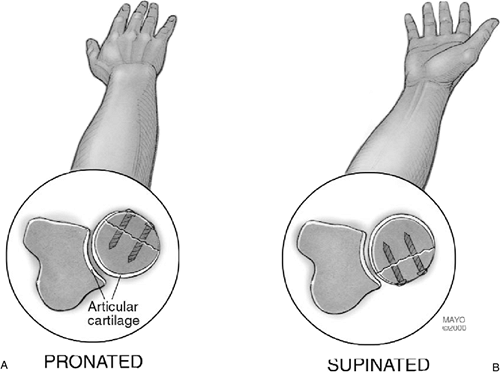
occurs with the forearm partially pronated. The slice thus occurs
through the part of the radial head that does not articulate with the
lesser sigmoid notch. The screw heads are off the articular surface (Fig. 5-14) and do not articulate with the ulna (Fig. 5-15).
 |
|
Figure 5-15.
The fixation can be applied through a margin of the radial head that does not articulate with the ulna either in full pronation (A) or in full supination (B). |
device, a posterior splint is applied for 3 days and a portable
continuous passive motion (CPM) machine may be used for approximately 2
to 3 weeks. Patients are cautioned to avoid active motion, since this
causes increased pressure on the radiohumeral joint. Radiographs are
taken at 3 weeks. If the fracture is stable, then gentle-active and
active assisted motion are allowed, and passive pronation and
supination is encouraged, avoiding flexion in pronation, as this causes
increased stress on the fracture (10).
Radiographs are taken again at 6 weeks. It is anticipated that early
osseous healing should have begun by this time. A period of 3 months is
typically required for complete fracture healing. Motion recovery may
be delayed for 6 to 12 months from injury.
Success ranges from that comparable to the slice fracture to as low as
30% to 33%. A recent study in our laboratory demonstrated improved
functional result with strength approaching normal in the uncomplicated
fracture (2). The strength of the open
reduction with internal fixation (ORIF) group was superior to both
those having resection and those treated without surgery.
failure of fixation and forearm motion loss. This is seen particularly
in those fractures with comminution or with collateral ligament
insufficiency causing increased stresses on or scarring to the repaired
fracture fragments. The treatment for displacement is delayed radial
head excision (1). Resection should not occur
in the first 5 to 7 days after the initial injury, but if displacement
occurs resection should be deferred for approximately 3 to 4 weeks.
only procedure, or fixation followed attempts at manipulation or
debridement, ectopic bone may occur. Little treatment is available in
the acute stage. Typically, the process must mature and then may be
excised at a later date. This does complicate and compromise the
ultimate result of the procedure, and prevention is far more desirable
than the treatment after ectopic bone has formed.
the elbow, disrupting the medial collateral ligament and causing a
compression fracture of the neck of the radius (Fig. 5-16).
The technique described earlier was employed to insert a miniplate at
the margin of the radial head after the fracture was reduced (Fig. 5-17). At 1 year the fracture has healed (Fig. 5-18)
and the patient has a range of motion of 10 to 145 degrees, flexion of
70 degrees, and supination of 80 degrees. There is no pain.
 |
|
Figure 5-16. A radial/head neck fracture dislocation in a 38-year-old physician.
|
 |
|
Figure 5-17. At reduction, the radial head was intact, and a miniplate was used employing the 1.0-AO cortical screws.
|
 |
|
Figure 5-18.
One year after treatment the patient’s fracture has healed with minimal depression and the patient has a near-normal arc of motion. |
for a new modular radial head replacement. Although the technique is
specifically that of the rHead prosthesis by Avanta (San Diego, CA),
the principles are, in general, valid for other designs (7).
-
Acute trauma (6).
-
Comminuted radial head fracture requiring resection associated with ligament injury.
-
Elbow dislocation (2).
-
Distal radioulnar joint injury (Essex-Lopresti injury) (20).
-
-
Comminuted radial head fracture requiring resection with associated fracture(s).
-
Coronoid type II or III fracture (comminuted or noncomminuted) (16).
-
Olecranon type III fracture (displaced or comminuted and unstable) (13).
-
-
After radial head excision with evidence of medial collateral ligament insufficiency (11) or ulnohumeral instability.
-
-
Reconstruction.
-
With interposition arthroplasty if the radial head is excised and residual elbow instability persists (12).
-
For stabilization of the forearm and elbow after an Essex-Lopresti injury (6,13).
-
Failed silicone radial head implantation if required for stability.
-
-
Acute trauma.
-
Older patient with a comminuted radial
head fracture requiring radial head excision without evidence of elbow
instability or other associated injury (greater than age 65). -
Open fracture of the radial head, olecranon or associated elbow dislocation with high risk for sepsis.
-
Mason type I or II radial head fractures.
-
Mason type III radial head fracture not associated with elbow or forearm instability (2,14).
-
-
Reconstruction (6,14).
-
In reconstructions if the proximal radius is malaligned with the capitellum.
-
Proximal radial shaft fractures associated with comminuted radial head fracture.
-
Disease of or injury to the capitellum (e.g., osteochondrosis).
-
-
Prior sepsis or concern regarding wound contamination.
-
Known sensitivity constituents.
-
Skeletal immaturity.
-
Insufficient soft tissues to provide for lateral or medial elbow stability.
-
For reconstruction if the resected radius is malaligned with the capitellum.
earlier for internal fixation. The lateral capsule is entered slightly
anteriorly to the collateral ligament, and the annular ligament and
capsule are reflected anteriorly and posteriorly to expose the radial
head. A portion of the lateral collateral ligament and anterior capsule
can be reflected from the lateral epicondyle and anterior humerus to
expose the capitellum if necessary. Efforts are made not to detach the
lateral ulnohumeral ligament, but if greater exposure is required, the
ligament is reflected from its humeral origin. If the ligament has been
disrupted, then the exposure progresses through the site of disruption
to expose the radiohumeral joint. The common extensor tendon and
anterior capsule are retracted as needed for adequate exposure (Fig. 5-19).
The device is inserted over the capitellum with the axis alignment rod
being oriented over the ulnar styloid (Fig. 5-20).
This alignment replicates the anatomic axis of forearm rotation. Test
forearm rotation with the axis guide in place to ensure proper
alignment. The proximal flange of the axis guide is placed against the
articular surface of the capitellum, and the cutting guide is then
adjusted proximally or distally for the desired extent of radial head
resection.
pronated and supinated to create a resection perpendicular to the axis
of rotation as defined by the resection guide (Fig. 5-21).
This includes sufficient resection to allow the device to articulate
with the ulna at the lesser sigmoid notch. The distal extent of
resection is the minimal amount that is consistent with the restoration
of function as dictated by the fracture line or previous radial head
resection but still compatible with implant insertion.
of the medullary canal, especially if the elbow is unstable. If the
stability does not allow exposure of the proximal radius, careful
reflection of the origin of the collateral ligament from the lateral
epicondyle may be necessary to permit adequate exposure to the
medullary canal. The canal is entered with a starter awl using a
twisting motion. With the forearm in midrotation, the curved broach is
introduced down the canal (Fig. 5-22).
down the canal with the tip oriented opposite of the radial tuberosity (Fig. 5-23). The appropriate-sized head is then applied (Fig. 5-24).
Tracking, both in flexion and extension and in forearm rotation, should
be carefully assessed. Malalignment of the radial osteotomy cut will
cause abnormal tracking during flexion/extension and/or forearm
pronation and supination.
 |
|
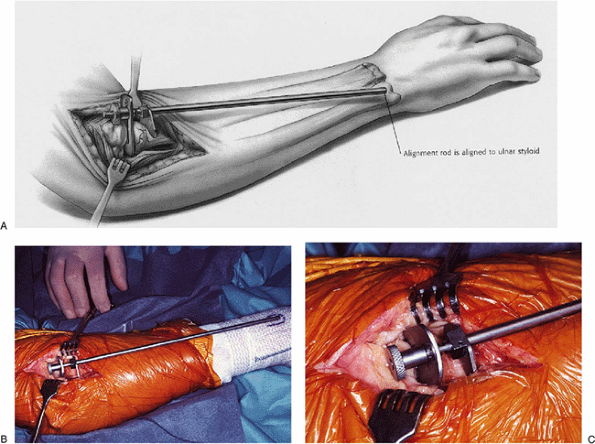
Figure 5-19. A,B:
After a type III radial head fracture the right elbow joint is exposed through Kocher’s interval and the fracture is identified. If the collateral ligament is intact, reflection from the humeral attachment to a variable extent may be necessary to insert the implant. |
 |
|
Figure 5-20. The alignment device is inserted in the joint. The distal portion is placed over the ulnar styloid (A,B) and the proximal portion rests against the capitellum (C).
|
 |
|
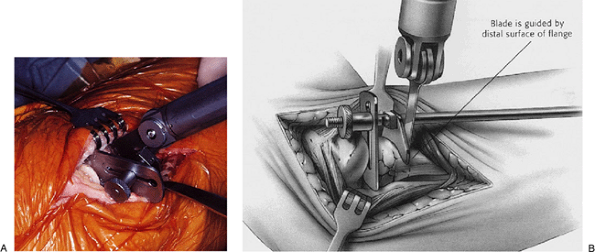
Figure 5-21. A,B:
An oscillating saw is used to resect the neck perpendicular to the axis of rotation by using the resection guide and rotating the forearm during resection. |
 |
|
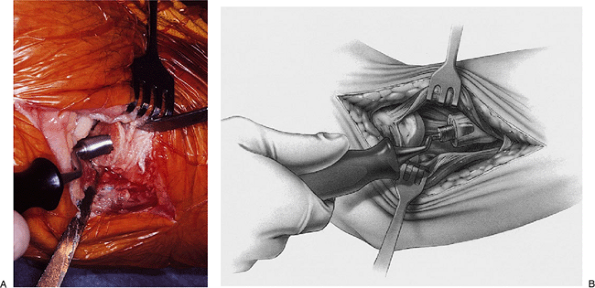
Figure 5-22. A,B: Insertion of the broach down the canal is facilitated by the curvature, which matches the stem of the implant.
|
 |
|
Figure 5-23. A,B: The curved trial stem of the implant is readily inserted down the canal.
|
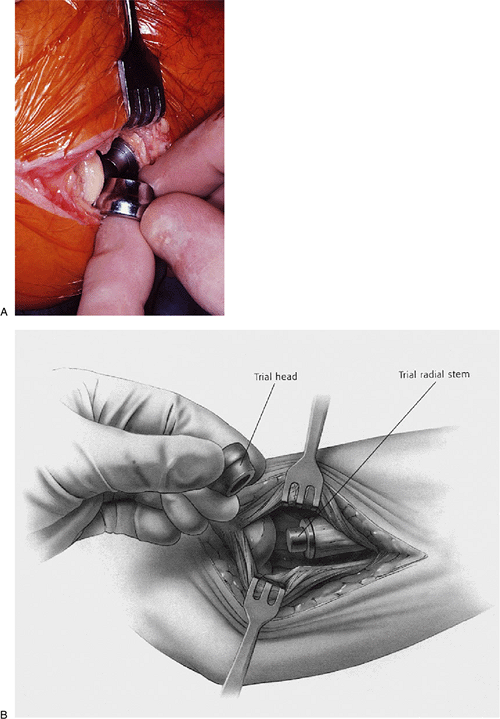 |
|
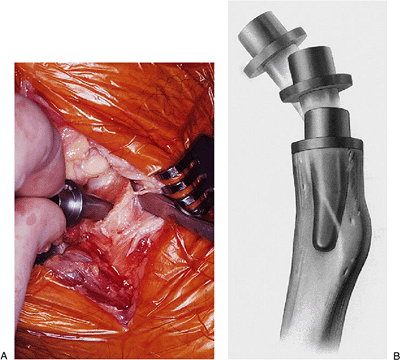
Figure 5-24. A,B: The appropriately sized head is applied.
|
implant have been determined, the prosthetic radial stem is inserted
with a rotational motion down the medullary canal and tapped in place
with the impactor. Bone cement (PMMA) may occasionally be used if
secure press-fit fixation is absent. The modular head is next placed
over the taper using longitudinal distraction and/or varus stress to
distract the radiocapitellar interface sufficiently
to permit the radial head to be inserted. The radial head implant is secured using the impactor. Alignment is again assessed (Fig. 5-25).
again, reconstitution of the LUCL is essential. If this appears
inadequate, it should be reinforced with a No. 5 nonabsorbable Bunnell
or Krachow stitch.
day, assuming the elbow is considered stable. The goal of radial head
replacement and soft-tissue repair is to achieve elbow stability. Both
flexion/extension and pronation/supination arcs are allowed without
restriction. Active motion can begin by day 5.
prosthetic replacement. If the implant is asymptomatic and tracks well,
routine removal is not necessary at this time.
radial head and elbow dislocation. The effort to fix the radial head
was unsuccessful and the medial ulnar collateral ligament did not heal (Fig. 5-26).
Reconstruction with the radial head implant and tendon graft
reconstruction of the MCL were successful and the patient has minimal
discomfort or evidence of instability (Fig. 5-27).
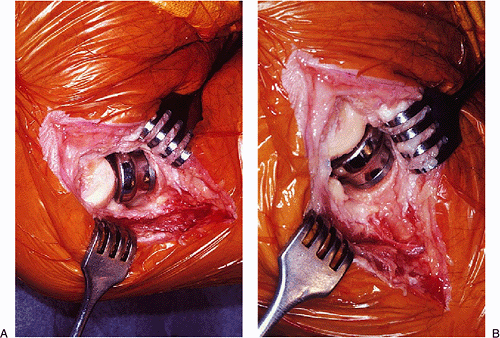 |
|
Figure 5-25. Proper tracking is assessed during flexion (A) and extension (B).
|
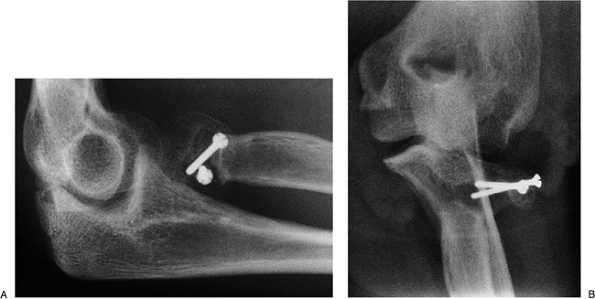 |
|
Figure 5-26.
A 30-year-old physician underwent reduction and fixation of type III radial head fracture with concurrent elbow dislocation. The fracture went to a nonunion (A) and the medial collateral ligament failed to heal (B). |
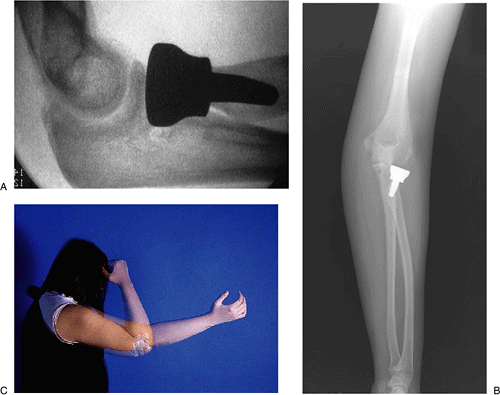 |
|
Figure 5-27. Treatment with implant and MCL reconstruction. The implant is well positioned and the elbow is stable (A,B). At 4 weeks the patient has excellent motion and stability (C).
|
