Shoulder Injuries In Throwing Athletes
relatively common occurrence in overhead athletes. Shoulder injuries
can be career-changing, or even career-ending events, especially for
overhead athletes such as baseball pitchers, football quarterbacks,
tennis players, and swimmers. Efficient throwing requires a coordinated
effort that progresses from the toes to the fingertips, and this has
been described by Kibler as the kinetic chain concept. The sequence of
body segment motions begins with the lower body and moves to the upper
body and arm. Energy is generated in the legs and trunk and is then
transferred through the shoulder to the arm, which delivers the force
to the ball. Any condition that affects a component of the chain,
especially those located more proximally in the kinetic chain, may
produce changes in later segments, possibly resulting in the
development of pathology.
injury in the thrower’s shoulder, the authors will not attempt to
provide a single unifying theory. Instead, we will provide an overview
clarifying the terminology and describing common pathologic findings,
and presenting the various theories on injury in the throwing shoulder.
The purpose of this chapter is to discuss the biomechanics,
presentation, diagnosis, and treatment of common shoulder injuries in
overhead athletes.
extremity activity in the inherently unstable position of maximal
abduction and external rotation. A thorough understanding of the
biomechanics and joint kinematics of the shoulder is a necessary
prerequisite to diagnose and treat shoulder injuries successfully in
these athletes. Due to the frequency of shoulder injuries in baseball
pitchers, we will review the mechanics of throwing.
exceed 90 miles per hour, and the shoulder of a professional player
will rotate at speeds of up to 7,000 degrees per second, with
distractive forces equal to body weight. These are among the fastest
angular velocities created in all of sport. Throwing has been divided
into six phases (Table 16-1 and Fig. 15-18 in Chapter 15), and the entire throw usually takes
less than 2 seconds. The first three phases occupy 1.5 seconds,
acceleration occupies only 0.05 seconds, and the last two occupy
approximately 0.35 seconds. Also see Chapter 15 for further details on the kinematics of throwing.
|
TABLE 16-1 THE SIX PHASES OF THE BASEBALL PITCH
|
|||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
pitch has been created through a combination of in vitro biomechanical
studies, electromyographic analysis, and clinical observation. Although
football throwing follows the same basic phases, there are slight
differences, imparted by the greater weight of the football, and mainly
resulting in lower angular velocities of approximately 5,000 degrees
per second.
repetitive motion of the shoulder under high loads at the extremes of
motion. Because of these loads, adaptive changes occur in the dominant
extremity of overhead athletes. These changes affect passive
stabilizing structures such as the capsule, ligaments, and bone, as
well as dynamic stabilizers such as the rotator cuff, shoulder girdle,
and chest wall musculature. It is widely believed that repetitive
subfailure loads can lead to acquired laxity of the shoulder, and this
has been demonstrated in cadaveric models.
externally to generate high ball velocities is paramount. Studies have
shown a direct correlation between the amount of external rotation of
the abducted arm and the subsequent speed of the pitched ball. With
repetitive throwing in a developing skeleton, adaptation of the osseous
and ligamentous anatomy occurs, which results in increased humeral
retroversion and acquired ligamentous laxity, allowing increased
external rotation in the throwing arm.
high-level overhead athletes (baseball pitchers and tennis players) has
shown increased external rotation and decreased internal rotation in
the abducted shoulder. It is commonly accepted that the majority of
these changes result from laxity in the anterior inferior glenohumeral
ligament and contracture of the posterior capsule. In the throwing
position, the anterior inferior glenohumeral ligament is the primary
restraint to external rotation. Therefore, it appears likely that this
ligament would be repetitively stressed and could develop laxity,
allowing for increased external rotation. Interestingly, baseball
pitchers commonly have an increased sulcus sign on physical exam, which
may be related to laxity of the coracohumeral ligament, another
restraint to external rotation in both the abducted and adducted arm.
rotation in the throwing arm is acquired retroversion of the humeral
head. Multiple studies have associated this with throwing. This osseous
adaptation has been described in professional handball and baseball
players, especially when intense training was started before skeletal
maturity. An average increase in humeral retroversion of 10 to 20
degrees was observed compared with the nondominant arm.
osseous—range of motion (ROM) is altered. Some authors suggest that
increased humeral retroversion is the predominate cause of this altered
ROM. Others believe that laxity of the anterior inferior glenohumeral
ligament is the main factor and recommend capsular plication as part of
the surgical treatment. Still, other studies suggest that the posterior
capsular contracture is the initiating and primary cause of pathology
and recommend release of the posterior capsule as part of surgical
treatment. Clearly, this area remains in need of additional study.
athletes typically demonstrate muscular asymmetry between the dominant
and nondominant arm as a result of muscle adaptation. It is not
uncommon for athletes to develop hypertrophy of the shoulder girdle
musculature, humeral head, cortex, and arm musculature of the throwing
arm. In chronic shoulder conditions such as suprascapular nerve
dysfunction or rotator cuff pathology, however, subtle atrophy can
sometimes be found, especially in the infraspinatus and supraspinatus
fossa. Overhead athletes, particularly volleyball players, can
demonstrate significant atrophy of the infraspinatus with weakness in
external rotation as a result of suprascapular neuropathy. This
neuropathy is thought to represent a repetitive traction injury, with
constriction occurring at the spinoglenoid notch (often associated with
labral cysts) or more proximally at the scapular notch.
the overhead throwing athlete with varying results and conclusions.
External rotation strength as a function of the infraspinatus and teres
minor muscles in the dominant shoulder of professional baseball
pitchers has been found to be significantly weaker than the nonthrowing
shoulder. The shoulder abductors, the deltoid, and supraspinatus
muscles usually do not demonstrate marked hypertrophy in throwers, and
some studies have even demonstrated significantly weaker supraspinatus
strength in the throwing arm of pitchers compared with the nondominant
arm.
strength of the internal rotators and adductor muscles. The
subscapularis, latissimus dorsi, pectoralis major, teres major,
coracobrachialis, and the long head of the triceps act in concert to
internally rotate and adduct the arm during the acceleration phase of
throwing.
-
A detailed history is the basis for a successful diagnosis and treatment.
-
Duration, location, and timing of symptoms, as well as associated symptoms, provide essential clues to the diagnosis.
-
Patient age and history of other injuries are also important in creating a differential diagnosis.
-
Patient age is relevant in that certain diagnoses are more common in particular age groups.
-
For example, shoulder pain in young athletes should raise concerns for physeal injury.
-
Younger athletes are also more likely to have problems with laxity.
-
Older players, especially pitchers, are more likely to suffer from rotator cuff pathology.
-
Pitchers in the middle of their careers may experience both laxity and rotator cuff pathology.
-
-
Timing of symptoms during the throwing cycle is important in formulating a differential diagnosis (Table 16-2).
-
Pain during cocking can suggest labral pathology, internal impingement, laxity, and/or instability.
-
Pain during late cocking or the early acceleration phase is seen with anterior instability.
-
Pain after ball release or during deceleration is frequently associated with rotator cuff pathology.
-
Posterior instability typically presents with pain during follow-through.
-
-
Timing of symptoms during a game is also important.
-
Symptoms occurring late in the game or
after repeated pitching starts suggest fatigue, typically of the
rotator cuff. These symptoms may respond well to rest and
rehabilitation.
-
-
History of associated symptoms and/or other nonshoulder injuries should also be obtained.
-
It is important to consider the kinetic
chain concept, as injuries to the lower extremities, spine, and other
areas may alter throwing mechanics and in turn cause shoulder pain.
-
-
A history of numbness, tingling, or discoloration in the fingers should raise concern for a neurologic or vascular problem.
-
Distal paresthesias or “dead arm” may also be associated with shoulder instability.
|
TABLE 16-2 RELATIONSHIP OF PHASE OF THROW WITH DIFFERENTIAL DIAGNOSIS
|
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
-
The majority of injuries seen in the
throwing athlete will present with an insidious onset; therefore, the
examiner must be attuned to the presence of vague complaints and subtle
findings on physical exam, as opposed to gross deformity and overt
distress. -
Inspection of both symptomatic and
asymptomatic throwing athletes at rest will typically reveal some
asymmetry—frequently, hypertrophy of the dominant shoulder and arm. -
Chronic shoulder conditions can present
with very subtle atrophy that can be detected with careful inspection
of the supraspinatus and infraspinatus fossa, in addition to the
scapular stabilizers bilaterally. -
Atrophy within the infraspinatus fossa
can signal the presence of suprascapular neuropathy, which occurs in
overhead and throwing athletes presumably from traction. -
General posture and alignment of the shoulder girdle should also be noted.
-
Many throwing athletes with shoulder pathology will hold the scapula in a depressed and protracted position.
-
Palpation can be helpful in
distinguishing between disorders of the subacromial space or
supraspinatus, the long head of the biceps, and the teres major tendons. -
All bony prominences around the shoulder
should be palpated, especially the acromioclavicular (AC) joint, where
tenderness and swelling can indicate degeneration. -
Acute AC joint disruptions are uncommon unless there has been a history of trauma.
-
Attention should also be directed to the bicipital groove and coracoid process.
-
Tenderness of the bicipital groove is
typical for biceps tendonitis, whereas pain with deep palpation of the
coracoid can indicate an impingement process. -
The exam should always include palpation
of the posterior joint line, where pain from both rotator cuff and
labral pathology can sometimes be elicited. -
Additionally, pain from the presence of
posterior glenoid osteophytes (e.g., Bennett’s lesions) can be
appreciated with deep palpation of the posteroinferior glenohumeral
joint.
-
ROM, both glenohumeral and scapulothoracic, must be evaluated.
-
Scapulothoracic motion should be smooth and symmetrical.
-
Asymmetry or winging of the scapula
should alert the examiner to the presence of periscapular muscle
weakness and overuse or, less commonly, nerve injury or tightness of
the pectoralis minor muscle. -
Painful crepitus with scapulothoracic motion may suggest inflammation of the scapulothoracic bursa.
-
Rotation of the abducted arm in overhead
athletes typically shows loss of internal rotation and increased
external rotation due to posterior capsular tightness and stretching of
the anterior structures. -
Posterior capsular tightness is best
assessed in the prone position, where maximum internal rotation of the
shoulder can result in inferior scapular winging. -
Frequently, there is a net loss in ROM due to a comparatively larger loss of internal rotation than gain of external rotation.
-
Limitations in internal rotation beyond
the normal-butshifted range may place the athlete at risk for the
development of shoulder problems, which will be discussed in more
detail later in the chapter. -
Any discrepancy between active and passive ROM may be a sign of muscle dysfunction or inhibition by pain.
|
TABLE 16-3 SUMMARY OF FUNCTIONAL TESTS
|
||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||
-
Strength testing of the rotator cuff, deltoid, and periscapular muscles should always be performed.
-
Internal (subscapularis and pectoralis
major muscles) and external rotation (infraspinatus and teres minor
muscles) should be evaluated with the arm at the side and in 90 degrees
of abduction. -
The supraspinatus may be evaluated with
resisted abduction with the 90 degrees in the plane of the scapula and
the thumbs pointing to the ground. -
The subscapularis is evaluated with the lift-off test and the belly press test.
-
Any pain elicited during testing will help identify the source of the patient’s symptoms.
-
More subtle muscular dysfunction can frequently be detected by using specific tests (Table 16-3).
-
Glenohumeral joint translation should be evaluated in all directions (anterior, posterior, and inferior).
-
This should be done in multiple positions with the athlete standing, sitting, and lying supine.
-
Although increased laxity in the dominant
arm may not necessarily be the source of pathology, reproduction of
pain with any of these maneuvers is helpful in identifying the presence
and direction of glenohumeral instability.
-
Provocative tests are a very important tool when trying to determine the source of a patient’s shoulder pain.
-
The Neer and Hawkins’ impingement tests are routinely used to evaluate the subacromial space and supraspinatus muscle (Table 16-4).
-
The apprehension and relocation tests are
sensitive tools in diagnosing classic anterior instability if true
apprehension is elicited.-
They are less specific when only pain is produced.
-
-
Placing the arm in abduction and external rotation reproduces the symptoms of pain in many throwing athletes.
-
A positive relocation test—in which
posterior shoulder pain is diminished when a posteriorly directed force
is applied to the maximally abducted and externally rotated arm—may be
a sensitive means of diagnosing occult anterior instability and
internal impingement, which can contribute to rotator cuff disease and
posterior-superior labral pathology.-
Some have speculated that, rather than
testing true instability, the anterior-posterior force used in the
relocation test may represent an “unlocking” of internally impinged
tissues.
-
-
A variety of provocative tests for the superior labral pathology have been described (Table 16-5).
-
Although these tests may be sensitive for
detecting labral tears, none have shown great specificity, and
therefore may also be positive in other pathology.
-
-
We prefer the active compression test.
|
TABLE 16-4 COMMONLY USED TESTS FOR IMPINGEMENT
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||
|
TABLE 16-5 COMMONLY USED TESTS FOR SUPERIOR LABRAL LESIONS
|
||||||||
|---|---|---|---|---|---|---|---|---|
|
-
Examination of the cervical spine is a
necessary part of any shoulder exam due to the high frequency of
referred pain from this location. -
Furthermore, the lower extremities and trunk should also be carefully examined.
-
Imaging should start with plain
radiographs, adding cross-sectional studies such as computed tomography
(CT) or magnetic resonance imaging (MRI) as needed to obtain additional
information about the bony anatomy and condition of soft tissues.
-
Basic radiographs should include a true
anteroposterior, axillary, and outlet views of the shoulder, with
specialized radiographs for the detection of specific lesions added as
needed. -
The Stryker notch view is useful in the
evaluation of posterior humeral lesions and in the diagnosis of a
Bennett’s lesion (exostosis of the posterior glenoid). -
A West Point view can be used to identify
bony Bankart lesions, whereas specialized views are available to
evaluate the AC joint for arthritic or traumatic changes.
-
CT scans have specific but limited applications in the evaluation of the thrower’s shoulder.
-
It is the study of choice for the
evaluation of glenoid abnormalities, such as bony Bankart lesions and,
in conjunction with a contrast arthrogram, it allows for the evaluation
of labral tears.
-
In addition to plain radiographs, MRI is the imaging modality of choice for most conditions of the thrower’s shoulder.
-
Ideally suited for soft-tissue imaging,
MRI is particularly useful in evaluating rotator cuff pathology and
injury to the glenoid labrum. -
MRI, when used in conjunction with
gadolinium arthrography, has reached a sensitivity of 90%, even for the
evaluation of partial thickness rotator cuff tears. -
It also allows for the assessment of
muscle degeneration, an important consideration before surgical
treatment of chronically retracted rotator cuff tears, and the
evaluation of labral cysts. -
To detect intra-articular pathology such
as labral tears, the sensitivity of MRI can be augmented by the
intra-articular injection of gadolinium. It is important to note that
even MRI scans of asymptomatic throwing athletes commonly show
pathologic changes; therefore, the MRI findings should be used
primarily to support a diagnosis suggested by the history and physical
exam findings, rather than as a screening tool.
-
Diagnostic arthroscopy remains the gold standard for the diagnosis of pathology in the thrower’s shoulder.
-
Intra-articular pathology can be clearly
defined, and the integrity of the rotator cuff and biceps-labral anchor
complex can be directly tested. -
By using what some have termed “dynamic-assessment arthroscopy,” the diagnosis of internal impingement can be made.
-
Viewed from the posterior portal with the
shoulder in the ABER (abduction-external rotation) position combined
with extension, contact between the undersurface of the rotator cuff
and the posterior-superior labrum is easily identified, along with any
associated lesions of these and other surrounding structures. -
Diagnostic arthroscopy should be
reserved, however, for the throwing athlete who has failed conservative
management for 3 to 6 months and still continues to have an unclear
diagnosis.
-
With very few exceptions, the treatment
of shoulder injuries, especially in professional athletes, should start
with a conservative program. -
Conservative management is divided into four phases: rest, stretching, strengthening, and a throwing program.
-
The first phase consists of activity
restriction or modification, nonsteroidal anti-inflammatory drugs, ice,
massage, and gentle passive ROM exercises. -
Once the acute pain has diminished, the
program should aim to increase motion with the goal of full motion
before advancing to the next phase.-
Focus is typically on contracted structures, such as the posterior capsule and pectoralis minor muscle in throwers.
-
-
Only after full motion has been restored,
the athlete should begin strengthening, with an emphasis on dynamic
stabilizers at first but also including trunk and lower extremity
musculature in the program.
-
-
The goal is to return to full throwing velocity over the course of 3 months.
-
Lack of significant improvement after 3
months, or the inability to return to competitive play within 6 months,
constitutes failure of conservative management, and should prompt
additional diagnostic tests and consideration of surgical intervention. -
Certain diagnoses such as acute rotator
cuff tears or dislocations may warrant earlier and more aggressive
surgical intervention on a case by case basis.
was thought to be “acquired,” and as such, thought to be a distinct
entity separate from traumatic and atraumatic instability. Neer
theorized that this acquired laxity resulted from repetitive injury and
microtrauma. This concept of acquired laxity gained widespread
acceptance. However, there was no solid evidence to demonstrate whether
laxity represented a failed repair mechanism or a remodeling response.
impingement are probably the most studied but least understood
components of pathology in the thrower’s shoulder. The definitions of
laxity and instability are often blurred in the literature leading to
much confusion. Although the terms are related, they are distinct
entities. Laxity does not equal instability. Laxity is excessive motion
for a particular direction or rotation for a particular joint. It may
represent a normal inherent property of the soft tissues or it may be
an adaptation for a given sport. For many authors, the term
“instability” is generally reserved for the sensation of humeral head
translation in the glenoid, associated with pain and discomfort. Taking
this into account, the nomenclature of “subtle instability” may have
led to some confusion. Others have called this microinstability. Kuhn (2002) recommended that a better description might have been “pathologic laxity.”
compete in high-level overhead sports, excessive laxity may be
responsible for the development of shoulder pathology.
For
example, excessive laxity of the glenohumeral ligaments could
predispose the athlete to injury to the labrum and/or rotator cuff.
However, this athlete may not have a sensation of instability. This
pathologic laxity is the “subtle instability” described by Jobe et al. (1983). It presents as pain with certain motions, but does not result in true apprehension or a feeling of impending dislocation.
or microinstability. Primary instability is the result of generalized
ligamentous laxity, whereas posttraumatic instability is caused by a
distinct traumatic event. Microinstability is the result of repetitive
stresses, especially in shear, during the cocking and acceleration
phases. Initially, the stretching of anterior structures permits
athletes to attain higher degrees of external rotation, thus allowing
them to perform at a higher level. Over time, increasing loads lead to
further stretching and failure of the anterior capsule.
Microinstability develops with increased anteroposterior translation of
the humeral head that can lead to labral fraying, subacromial
impingement, and rotator cuff tears.
deepening the glenoid. It also serves as the attachment site for the
long head of the biceps and the superior and middle glenohumeral
ligaments. Labral tears are common in athletes and can be quite
debilitating, especially tears of the superior labrum affecting the
biceps anchor. Superior labral tears have received increased attention
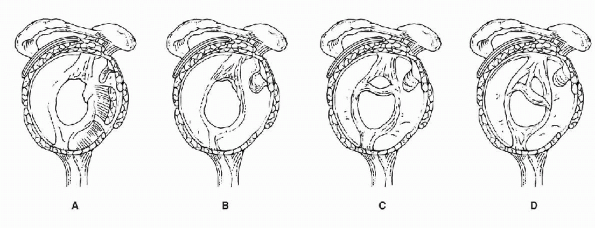
and have been termed superior labrum, anterior-posterior, or SLAP lesions. The original reference describes four types of SLAP lesions (Figs. 16-1, 16-2 and 16-3; Table 16-6).
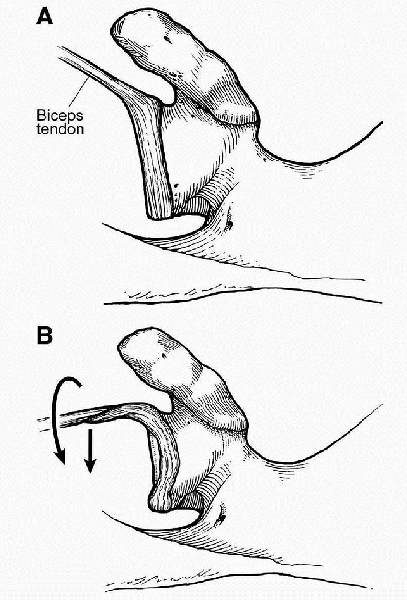
common in throwers, whereas true avulsions of the biceps anchor (type
II SLAP lesions) are less frequent. Several theories exist regarding
their etiology. Classically, SLAP lesions were thought to be the result
of traction or compressive mechanisms, such as sudden pulling on the
arm or falls on the outstretched arm. It was thought that traction on
the biceps was likely responsible for the development of these lesions
during the deceleration phase of throwing, but recent biomechanical
studies and arthroscopic observations have suggested the extreme
external rotation seen in the thrower’s shoulder as the causative
factor. Increased strain at the biceps anchor during the late cocking
phase with the arm in maximum external rotation results in a
“peel-back” effect, which has been suggested as the mechanism behind
the development of SLAP lesions in throwers (see Fig. 16-5).
This is supported by laboratory studies that have shown the long head
of the biceps to be an important dynamic restraint to external rotation
of the abducted arm. As part of the “peel-back” theory, the authors
have noted an increased incidence of SLAP lesions in patients with
decreased total arc of motion, such as seen in baseball pitchers who
often have internal rotation deficits greater than the concomitant gain
in external rotation (Fig. 16-4). Burkhart and Morgan (1998)
have developed a theory regarding the association between decreased
glenohumeral internal rotation and the development of pathology in the
shoulder. This model is known as glenohumeral internal rotation deficit
(GIRD) and will be discussed in more detail later in the chapter.
 |
|
Figure 16-1 SLAP types. A: Type 1. B: Type 2. C: Type 3. D: Type 4.
|
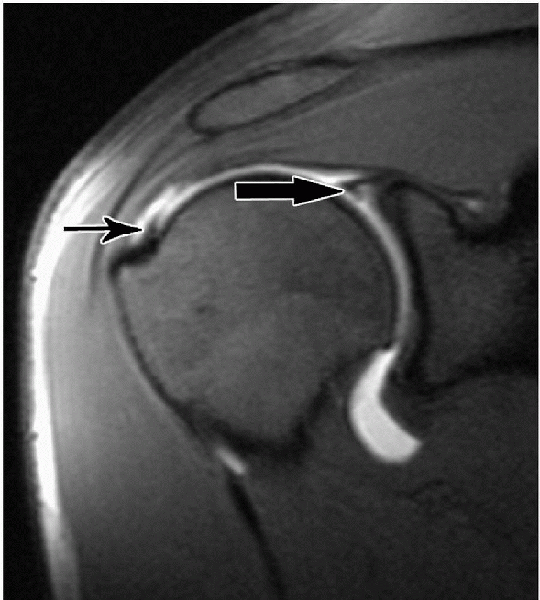 |
|
Figure 16-2 Shoulder MRI demonstrating partial thickness rotator cuff tear (small arrow) and SLAP tear (large arrow).
(From Magee T, Williams D, Mani N. Shoulder MR arthrography: which patient group benefits most? Am J Roentgenol 2004;183:969-974.) |
-
SLAP lesions present with vague pain,
which sometimes localizes to the posterosuperior joint line and can be
exacerbated with overhead activities. -
They can produce symptoms of locking or snapping and, depending on tear size, instability.
-
Throwers frequently report pain in the late cocking phase and loss of velocity.
-
Posterior tightness and positive provocative tests are common physical findings.
-
Radiographic workup should include conventional radiographs and MRI arthrogram to delineate the lesion further.
 |
|
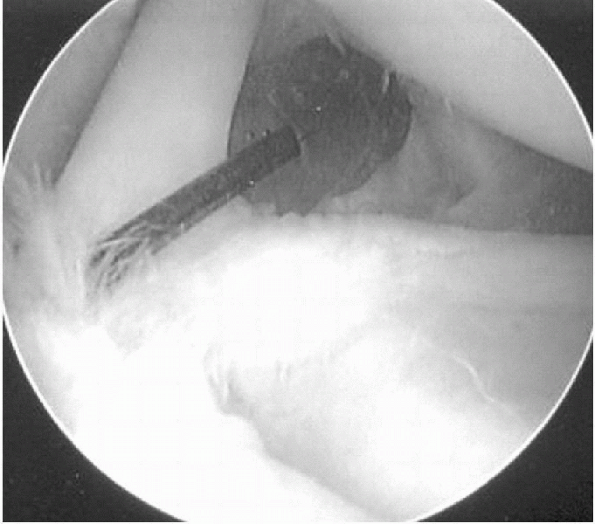
Figure 16-3 Shoulder arthroscopy, view from posterior portal, demonstrating the biceps anchor with a SLAP tear.
|
-
Treatment of SLAP lesions is typically
conservative at first, with many players responding to rest and
rehabilitation in the acute period. -
If the acute inflammation in the shoulder
has subsided, and the player has completed a course of rehabilitation
but is still unable to resume throwing, serious consideration should be
given to surgical intervention. -
Surgical treatment of symptomatic SLAP
lesions consists of shoulder arthroscopy, which frequently demonstrates
a positive “drive-through” sign, a displaceable biceps vertex and, in
up to 60% of cases, associated rotator cuff pathology, mostly
partial-thickness undersurface tears. -
If the biceps-labral anchor is avulsed,
it is partially debrided and secured back to the glenoid with suture
anchors, followed by a postoperative rehabilitation program for
posterior capsular stretching. -
If minor tearing and fraying are present,
but no true avulsion of the biceps anchor, a simple labral debridement
can be performed. -
Although thermal capsulorrhaphy has
fallen into disfavor in most cases, there have been some favorable
results in the throwing athletes with superior labral tears.-
When thermal capsulorrhaphy was combined
with labral repair, better results were seen than with labral repair
alone, and 87% of overhead athletes were able to return to play.
-
-
After formal repair of the biceps-labral
complex, throwers undergo a brief period of immobilization, followed by
a rehabilitation program that focuses on throwing mechanics. -
Return to play is typically 4 to 6 months postoperatively, although return to elite throwing may take closer to 1 year.
-
Patients with a stable biceps anchor at
the time of surgery who have undergone only limited labral debridement
are not immobilized after surgery and can typically resume play after 4
to 6 weeks of rehabilitation.-
Authors have reported on the outcome of
this type of program, with return to preinjury performance levels in
more than 80% of pitchers.
-
|
TABLE 16-6 SLAP LESIONS
|
||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||
 |
|
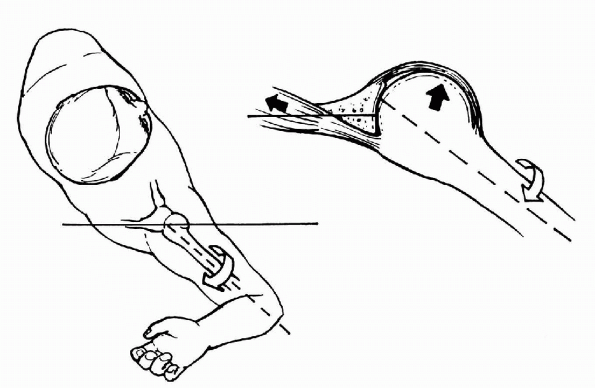
Figure 16-4 Peel-back effect. A: Superior view of the biceps and labral complex of a left shoulder in a resting position. B:
Superior view of the biceps and labral complex of a left shoulder in the abducted, externally rotated position, showing peel-back mechanism as the biceps vector shifts posteriorly. (From Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology. Part I: pathoanatomy and biomechanics. Arthroscopy 2003;19:404-420; with permission from the Arthroscopy Association of North America.) |
-
Most rotator cuff tears in this population are partial-thickness, articular-sided tears.
-
Some result from acute tensile overload
but more commonly the cause is repetitive microtrauma and eccentric
failure of the fibers. -
Whereas cuff tears may occur in the
setting of impingement, in this population they are more commonly the
result of subtle instability. -
Subacromial decompression alone has not
been effective in the athletic population, with return to previous
activity levels in only half the patients. -
Similarly, simple debridement of partial
tears, a largely effective procedure in lower-demand patients, produces
less consistent results especially in the overhead athlete. -
Full-thickness rotator cuff tears are a
rare event in the overhead athlete but have a very poor prognosis even
when repaired, with only half of all players able to return to play. -
Several types of impingement have been described in the literature:
-
“Classic” subacromial or outlet impingement
-
“Secondary” or nonoutlet impingement
-
Subcoracoid impingement
-
Internal impingement
-
-
The “classic” form of impingement as described by Neer (1983) is the result of compression of the rotator cuff between the coracoacromial arch and the humeral head.
-
Anatomical variants such as a hooked
acromion, acromioclavicular joint arthritis with osteophyte formation,
and a laterally sloping acromion have been proposed as predisposing
factors. -
Subacromial impingement is typically diagnosed in the older throwing athlete who has a stable shoulder.
-
These overhand athletes will often have
loss of internal rotation without concomitant increase in external
rotation as seen in many younger throwers. -
Adaptive bony changes may also play a role in this loss of internal rotation.
-
Subacromial impingement can be further
exacerbated by weakness of the rotator cuff from fatigue or improper
technique, leading to superior migration of the humeral head. -
These patients have a painful arc, positive impingement maneuvers, and will typically respond well to subacromial injections.
-
Radiographs in older throwers usually
show varying degrees of an acquired, or congenitally prominent anterior
acromion that predisposes to outlet stenosis. -
Many patients improve with
anti-inflammatory medications combined with a well-supervised physical
therapy program focusing on rotator cuff rehabilitation and scapular
dynamics. -
Arthroscopy with subacromial decompression is reserved for those who fail conservative management.
-
Unlike the subacromial space of a younger
thrower, which is typically smooth and white in appearance, the older
thrower can demonstrate an irritated and thickened bursa with fraying,
matched excoriation and hypertrophy of the coracoacromial ligament. -
If a significant bursal-sided partial or
full-thickness rotator cuff tear is present, consideration for repair
is recommended, either through a “mini-open” or arthroscopic approach. -
It is imperative to inform patients
before surgery, however, that a return to the same premorbid level of
competition is unlikely. -
External impingement as the sole source
of pain appears to be relatively uncommon in throwing athletes, with
the exception of the older thrower.-
This may help explain why a high failure
rate of almost 80% was seen in early reports for throwing athletes
being treated with subacromial decompression for apparent impingement.
-
-
Secondary, or nonoutlet, impingement is a
dynamic process in which a normal subacromial arch is present but there
is abnormal proximity between the arch and the underlying rotator cuff. -
There is a strong association between scapulothoracic dyskinesia and impingement symptoms.
-
Weakness in the scapular stabilizers leads to lack of proper rotation of the scapula during humeral elevation.
-
As a result, the space available for the rotator cuff is acutely narrowed and thus causes impingement symptoms.
-
-
Posterior capsular tightness can also
create a vector imbalance resulting in posterior-superior migration of
the humeral head with secondary rotator cuff symptoms. -
Malunion from displaced fractures of the
greater humeral tuberosity, and massive rotator cuff tears with loss of
the humeral head depressors, can also result in secondary impingement. -
Treatment recommendations are based on the primary pathology.
-
If the secondary impingement is
associated with a partial-thickness rotator cuff tear affecting more
than half the cuff thickness, the recommended treatment includes a
formal open, mini-open, or arthroscopic cuff repair. -
When scapular dyskinesia is the cause of
secondary impingement, rehabilitation of the periscapular musculature
is typically successful. -
When impingement is caused by tightness
involving the capsule, as in adhesive capsulitis, or by adhesions in
the subacromial space, as seen in trauma or postsurgical cases,
surgical correction with lysis of adhesions is recommended.
P.209 -
-
Coracoid impingement occurs when the subscapularis tendon is compressed between the lesser tuberosity and the coracoid tip.
-
Possible causes include postoperative
changes (e.g., Bristow procedure), previous trauma, anterior
instability, and idiopathic impingement. -
Coracoid impingement is typically a diagnosis of exclusion.
-
Patients present with localized anterior shoulder pain, which can mimic or occur in combination with subacromial impingement.
-
The test most often cited in the
literature is pain localized to the coracoid when the shoulder is
passively forward flexed, adducted, and internally rotated.-
This test differs from O’Brien’s test, because the latter requires active resistance in this position.
-
-
-
Injections in the subcoracoid space have been recommended to aid in the diagnosis and treatment of the condition.
-
A shortened coracohumeral distance, the
distance between the coracoid and the lesser tuberosity with the arm in
maximum internal rotation (average 11 mm in normal vs. 5.5 mm in
symptomatic shoulders) has been described in association with
subcoracoid impingement. This, however, is not specific to this problem. -
If conservative measures fail, a coracoidplasty is the next appropriate step in treatment.
-
This has been described both open and
arthroscopically, with the goal being to debride the tip of the
prominent coracoid to increase the space between the coracoid and the
lesser tuberosity.
-
described internal impingement as a physiologic phenomenon in which the
undersurface of the rotator cuff contacts the posterior-superior labrum
when the arm is placed in maximum external rotation and abduction (Fig. 16-5). Halbrecht et al. (1999)
demonstrated this phenomenon in college baseball players and showed
that internal impingement can occur even in the absence of symptoms.
This is thought to result from recurrent microtrauma, which can
ultimately lead to rotator cuff tearing and destabilization of the
biceps-labral complex. Internal impingement presents as a spectrum of
pathologies with significant overlap that typically involves SLAP
lesions, partial thickness rotator cuff tears, hyperlaxity of the
anterior glenohumeral ligaments, and posterior capsular contractures.
 |
|
Figure 16-5
Internal impingement of the undersurface of the rotator cuff against the posterior labrum in maximum external rotation/abduction. (From Meister K. Injuries to the shoulder in the throwing athlete. Part I: biomechanics/pathophysiology/classification of injury. Am J Sports Med 2000;28:265-275.) |
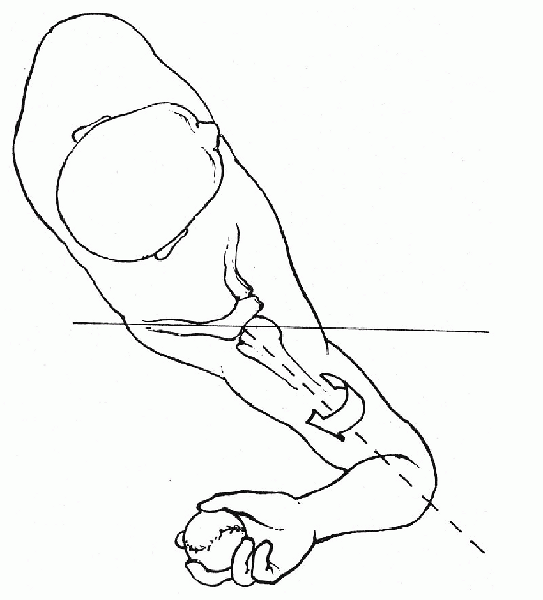
impingement is most likely caused by shoulder girdle muscle fatigue
resulting from a lack of conditioning or overthrowing and/or anterior
capsular stretch resulting in anterior capsular insufficiency. The
authors believe that, during the acceleration phase of throwing, the
humerus should be aligned in the plane of the scapula and that with
fatigue of the shoulder girdle muscles the humerus drifts out of the
scapular plane. This has been termed “hyperangulation” and is called
“opening up” by many pitching coaches. This hyperangulation of the
humerus in turn stresses the anterior capsule (Fig. 16-6).
Loss of anterior capsular integrity compromises the normal posterior
rollback of the humeral head, leading to anterior translation,
therefore causing the undersurface of the rotator cuff to abut against
the margin of the glenoid and labrum. Reducing the laxity in the
anterior inferior glenohumeral ligament seems to improve outcome
significantly in the throwers with internal impingement.
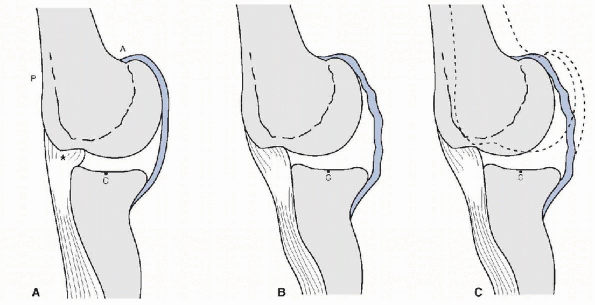
recently questioned whether or not internal impingement actually
occurs. They described their own model (GIRD) as the primary cause
behind the pathologic changes seen in the “internal impingement”
patient. The Morgan-Burkhart model is based on the frequency of
posterior capsular contractures in throwers. Combined with the
possibility of acquired humeral retroversion, the tight posterior
capsule shifts the center of rotation of the humerus in the
posterior-superior direction. This permits greater clearance of the
greater tuberosity. Because of
the diminished “cam” effect, the anterior capsule becomes functionally lengthened (Fig. 16-7).
With a functionally lengthened anterior capsule allowing clearance of
the greater tuberosity, excessive external rotation is achieved. As a
result, the biceps anchor is “peeled back” under tension, causing
injury to the posterior-superior structures, most notably to the
posterosuperior labrum. The progression of the “peel-back” mechanism
allows further “pseudolaxity” of the anterior capsule to occur. The
pathologic cycle culminates in torsional failure of the rotator cuff,
not compressional failure as in the internal impingement model. The end
results are articular-sided partial rotator cuff tears and SLAP lesions
typically seen in the throwing shoulder.
 |
|
Figure 16-6 Hyperangulation of the humerus.
|
 |
|
Figure 16-7 Cam effect. A:
With the arm in a position of abduction and external rotation, the humeral head and the proximal humeral calcar produce a significant cam effect of the anteroinferior capsule, tensioning the capsule by virtue of the space-occupying effect. B: With a posterosuperior shift of the glenohumeral contact point, the space-occupying effect of the proximal humerus on the anteroinferior capsule is reduced (reduction of cam effect). This creates a relative redundancy in the anteroinferior capsule that has probably been misinterpreted in the past as microinstability. C: Superimposed neutral position (dotted line) shows the magnitude of the capsular redundancy that occurs as a result of the shift in the glenohumeral contact point. (After Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology. Part I: pathoanatomy and biomechanics. Arthroscopy 2003;19:404-420.) |
rotation deficit to identify those players at risk for pathology.
Defined as a greater than 25-degree loss of internal rotation of the
dominant shoulder, compared with the contralateral side, GIRD is a
common phenomenon in throwing athletes. Some studies have found average
deficits of up to 50 degrees when compared with the contralateral side,
with concomitant increases in external rotation on the order of 30
degrees. Shoulders with a total arc of motion less than 180 degrees and
an internal rotation deficit of greater than 25 degrees seem to be at
risk for developing SLAP lesions as a result of increased
posterosuperior “peel-back” forces.
first recognizing the relationship of GIRD with the development of
shoulder dysfunction. By following 39 professional pitchers over a
single season, he demonstrated that the development of shoulder
problems occurred in more than half of the players with GIRD greater
than 35 degrees.
high-level tennis players were divided in two groups and prospectively
followed for 2 years. One group performed daily posteroinferior
capsular stretching to minimize GIRD, whereas the control group
continued their routine exercise program. Over the course of the study
period, those in the stretching group
had a 38% decrease in the incidence of shoulder problems compared with controls.
physical therapy program focused on stretching of the tight posterior
capsule, with a concomitant decrease in shoulder-related problems. The
remaining 10%, frequently older elite players, who are unresponsive to
conservative treatment can be treated by selective arthroscopic
posteroinferior capsulotomy in the zone of the posterior band of the
inferior glenohumeral ligament.
humeral retroversion, its contribution to throwing, and its relevance
to internal impingement. Increased humeral retroversion allows for
increased external rotation with an obligate loss of internal rotation.
Interestingly, Riand et al. (1998) reported that a loss of normal
humeral retroversion (normally 25 to 35 degrees) to less than 10
degrees total humeral retroversion will increase the risk of contact
between the greater tuberosity and the posterior-superior glenoid
labrum (e.g., internal impingement). In patients with a loss of humeral
retroversion (as opposed to throwing athletes who typically have
increased retroversion), the subsequent internal impingement was
corrected with humeral osteotomy.
added greatly to our understanding of scapular dynamics and its role in
preventing injuries in the throwing athletes. The scapula functions to
provide a stable platform for the humeral head during rotation and
elevation, while transferring kinetic energy from the legs and trunk to
the upper extremity. It has been estimated that only half of the
kinetic energy imparted to the ball results from arm and shoulder
action. The remaining half is generated by leg and trunk rotation, and
is transferred to the upper limb through the scapulothoracic joint,
making it an important, but frequently overlooked part of the kinetic
chain.
periscapular musculature secondary to fatigue, direct trauma, or nerve
injury (e.g., the long thoracic nerve). It can negatively impact
shoulder function in several ways. To reach the extremes of motion
needed in overhead athletics, elevation of the acromion is required or
else impingement results. Normal function of the serratus anterior,
trapezius, and rhomboid muscles is required to achieve the necessary
scapular positioning. Loss of function from nerve injury, weakness,
and/or fatigue leads to scapular hyperangulation and a relative
increase in glenoid anteversion, placing the anterior capsular
structures at risk. Associations between scapular dyskinesia and
anterior instability and impingement have been documented by several
authors.
rotation to the pitching arm, destabilization of the scapula results in
energy losses that decrease velocity. In an attempt to compensate for
the loss of power, the pitcher tries to regain velocity by increasing
the effort of the shoulder muscles, which results in increased strain
on the shoulder. For these reasons, rehabilitation of the throwing
athlete must have a strong emphasis on strengthening and conditioning
the scapular stabilizers.
-
The vast majority of scapula-related issues can be resolved by a physical therapy program directed at the scapular stabilizers.
-
Sometimes, however, surgical intervention
can be required for entities such as scapular bursitis or a snapping
scapula, which can be treated by excision of the offending tissues at
the inferior and/or superior margin of the scapula.
-
The Bennett lesion is a mineralization at
the posteroinferior glenoid present in approximately 20% of major
league pitchers, best seen on the Stryker-Notch view. -
The lesion is thought to be the result of enthesopathic changes of the posterior capsule and inferior glenohumeral ligament.
-
It is an infrequent cause of pain in the
overhead athlete and can be associated with tears of the posterior
labrum and rotator cuff. -
The diagnosis of a symptomatic Bennett
lesion is difficult but frequently presents with posterior shoulder
pain during throwing, especially in the follow-through phase. -
Tenderness to palpation of the
posteroinferior glenohumeral joint is common, whereas resolution of
pain with local injection can be both diagnostic and therapeutic. -
Symptomatic Bennett lesions can be treated by arthroscopic debridement.
-
True osteochondritis dissecans of the shoulder is a very rare occurrence, with less than 20 cases described in the literature.
-
Traumatic osteochondral defects are seen
more frequently as impression fractures of the humeral head (Hill-Sachs
lesion), and fractures involving the glenoid rim (Bankart lesion) after
anterior glenohumeral dislocation. -
Both can be the cause of recurrent
dislocations, in which case they should be corrected by grafting of the
Hill-Sachs lesion and fixation of the glenoid fracture.
-
Vascular compromise after shoulder injury is rarely seen outside major trauma such as scapulothoracic dissociation injuries.
-
Presenting predominantly as arterial
thrombosis rather than transection, these injuries occur in less than
1% of shoulder dislocations and proximal humerus fractures.
-
Effort thrombosis is a rare entity
presenting with symptoms of tiredness, heaviness, and gradual
development of swelling over the course of a few days. -
It has been described in a wide range of activities, including baseball, softball, hockey, swimming, wrestling, and backpacking.
-
Exam findings include slight discoloration, venous engorgement, and size difference, compared with the contralateral extremity.
-
Venography or more modern CT or MRI-based
imaging typically demonstrate thrombosis of the subclavian vein at the
level of the first rib. -
The cause, although still not
conclusively proven, is likely compression of the vascular structures
between the first rib and the clavicle, especially with the arm in
maximum abduction. -
Treatment options include
catheter-directed thrombolysis, balloon venoplasty, and staged
resection of the first rib with good results and return to preinjury
level of play within 6 to 36 months.
 |
|
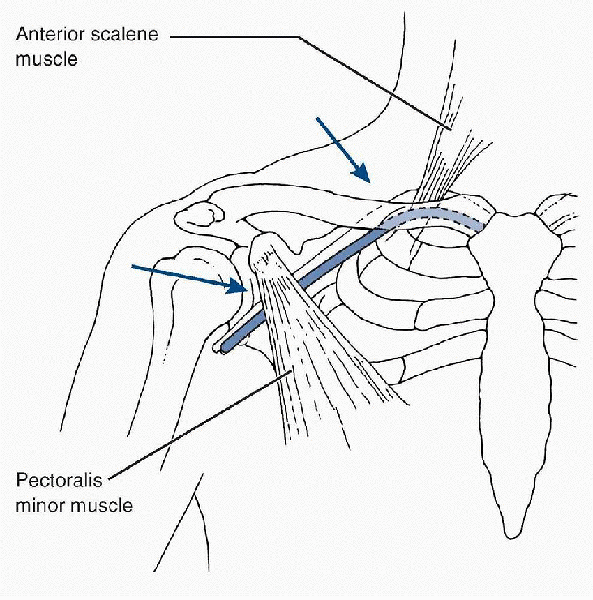
Figure 16-8
Common compression sites in thoracic outlet syndrome. (After Meister K. Injuries to the shoulder in the throwing athlete. Part 2: evaluation/treatment. Am J Sports Med 2000;28: 587-601.) |
-
This term describes the compression of
neurovascular structures that traverse the thoracic outlet, which is
formed by the clavicle, first rib, and the anterior scalene muscle (Fig. 16-8). -
A subset of patients has an identifiable
cause for the compression such as cervical ribs, exostosis of the first
rib, or malunions of the first rib or clavicle.-
In most cases, however, no such abnormality can be identified.
-
-
Presenting complaints are neurological in
greater than 90% of patients, and include pain, paresthesias, and
weakness—especially in a lower plexus distribution. -
Vascular symptoms occur rarely and commonly present as activity-related claudication, pulse, or blood-pressure deficits.
-
The workup is complicated by the lack of any specific diagnostic tests.
-
Several provocative tests have been
described, such as placing the affected extremity in maximum abduction
and external rotation, which leads to recreation of symptoms in more
than 80% of patients. -
Management should be conservative
initially, with activity modification, nonsteroidal anti-inflammatory
drugs, strengthening of the shoulder girdle, and scapular stabilizers.
This is successful in more than 70% of patients. -
Surgical treatment is reserved for those severely affected or for those with refractory pain after conservative management.
-
Studies have demonstrated a greater than
90% success rate with surgical decompression, frequently by resection
of the first rib through a transaxillary approach.
-
Quadrilateral space syndrome is defined
as compression of the axillary nerve and posterior humeral circumflex
artery as they traverse the quadrilateral space.-
This space is defined by the humerus
laterally, the long head of the triceps medially, and the teres minor
and major muscles superiorly and inferiorly, respectively.
-
-
This rare condition presents in overhead
athletes with nonspecific symptoms such as dull, aching, or burning
pain in the posterolateral aspect of the shoulder, exacerbated by
activity, especially with repetitive exercise with the arm abducted and
externally rotated. -
Physical findings include deltoid
weakness and wasting, pain to palpation over the quadrilateral space,
and reproduction of symptoms with the arm in the
flexion-abduction-external rotation (FABER) position. -
Angiography frequently demonstrates
occlusion of the posterior humeral circumflex artery when the arm is
placed in the FABER position, whereas electromyographic studies can
demonstrate denervation in the deltoid and teres minor muscles. -
Due to the rarity of the syndrome, no
definite treatment guidelines have been established, but current
recommendations include conservative treatment initially, with surgical
exploration and release of the neurovascular structures reserved for
refractory cases.
is multifactorial. Overlapping signs and symptoms exist, as well as
numerous causes of disability. The problems appear to be a combination
of abnormal mechanics, muscle fatigue and imbalance, scapular
dyskinesia, increased humeral retroversion, posterior capsular
contractures, anterior capsular laxity, and repetitive microtrauma. As
a result, throwers commonly develop multiple areas of pathology
involving the posterior superior labrum, the articular surface of the
rotator cuff, cartilage lesions and bony exostoses of the posterior
glenoid, cystic changes at the insertion of the rotator cuff,
thickening of the posterior capsule, and redundancy of the anterior
capsule.
controversial and are complicated by the difficulty of recreating an
accurate in vitro model of the complex kinetic chain. Different schools
of thought exist regarding the initiating event for many of the
problems seen in the thrower’s shoulder—whether it is anterior capsular
laxity or posterior capsular tightness. Fortunately, for the
practitioner, regardless of the conflicting theories regarding the
pathomechanics at work in the throwing shoulder, the evaluation and
treatment algorithms of the injured athlete are, with few exceptions,
very similar.
stresses experienced typically during the late cocking and early
acceleration phase result in damage to the posterior glenoid, the
biceps-labral complex, and the articular surface of the rotator cuff.
The forces acting on these posterior structures are a combination of
compressive, tensile, and torsional forces, which culminate in actual
fiber failure of both the biceps-labral complex and the rotator cuff.
Conditioning of the entire kinetic chain, and respecting adequate
recovery periods between games, is imperative, and it is the
responsibility of the coaches, trainers, and physicians to educate the
players.
LU, Codd TP, Connor PM, et al. Shoulder motion and laxity in the
professional baseball player. Am J Sports Med 1997;25: 609-613.
SS, Morgan CD. The peel-back mechanism: its role in producing and
extending type II SLAP lesions and its effect on SLAP repair and
rehabilitation. Arthroscopy 1998;14:637-640.
SS, Morgan CD, Kibler WB. Current concepts: the disabled shoulder:
spectrum of pathology. Part I: pathoanatomy and biomechanics.
Arthroscopy 2003;19:404-420.
SS, Morgan CD, Kibler WB. Current concepts: the disabled shoulder:
spectrum of pathology. Part II: evaluation and treatment of SLAP
lesions in throwers. Arthroscopy 2003;19:531-546.
GS, Andrews JR, Dillman CD, et al. Kinetics of baseball pitching with
implications about injury mechanisms. Am J Sports Med 1995; 23:233-239.
JL, Tirman P, Atkin D. Internal impingement of the shoulder: comparison
of findings between throwing and nonthrowing shoulders in college
baseball players. Arthroscopy 1999;15: 253-258.
WB. The relationship of glenohumeral rotation deficit to shoulder and
elbow injuries in tennis players: a prospective evaluation of posterior
capsular stretching. In: Annual Closed Meeting of the American Shoulder
and Elbow Surgeons. New York: ASES, 1998.
JE. Comprehensive evaluation and treatment of the shoulder in the
throwing athlete: biomechanics, pathomechanics, clinical evaluation,
and diagnostic testing. Arthroscopy 2002;18:74-81.
C. Shoulder flexibility to reduce impingement. In: 3rd Annual
Professional Baseball Athletic Trainers Society. Mesa, AZ: PBATS, 1991.
G, Boileau P, Noel E, et al. Impingement of the deep surface of the
supraspinatus tendon on the posterosuperior glenoid rim: an
arthroscopic study. J Shoulder Elbow Surg 1992;1:238-245.
JJP, Micheli LJ, Arslanian LE, et al. Scapulothoracic motion in normal
shoulders and shoulders with glenohumeral instability and impingement
syndrome. Clin Orthop Relat Res 1992;285: 191-199.
