FRACTURES OF THE ACETABULUM, HIP DISLOCATIONS, AND FEMORAL HEAD FRACTURES
II – FRACTURES, DISLOCATIONS, NONUNIONS, AND MALUNIONS > Pelvis and
Femur > CHAPTER 18 – FRACTURES OF THE ACETABULUM, HIP DISLOCATIONS,
AND FEMORAL HEAD FRACTURES
Professor, Chief Orthopaedic Trauma, Department of Orthopaedic Surgery,
University of California Davis, Medical Center, Sacramento, California,
95817.
in the innominate bone. The anterior column, which consists of the
iliac wing and pelvic brim, extends to the pubic symphysis and contains
the anterior one half of the acetabular articular surface. The
posterior column consists of the greater and lesser sciatic notches,
the retroacetabular surface, and the majority of the quadrilateral
surface (25). Similarly, the posterior column
contains the posterior one half of the acetabular articular surface.
The goal of surgical treatment of fractures of the acetabulum is an
accurate reconstruction of the articular surface (28).
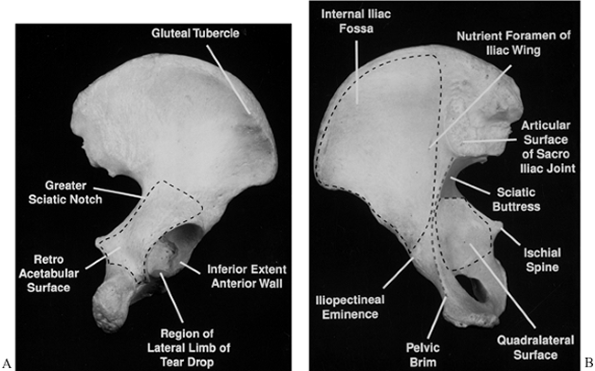
acetabular fractures. We emphasize several descriptive terms in the
discussion of acetabular fractures. The internal iliac fossa, the
quadrilateral surface, and the retroacetabular surface describe large
cortical surfaces of the innominate bone. The pelvic brim marks the
junction of the internal iliac fossa and quadrilateral surface. The
sciatic notch marks the junction of the quadrilateral surface and the
retroacetabular surface (Fig. 18.1).
 |
|
Figure 18.1. A:
Anatomic regions of the internal aspect of the innominate bone are illustrated. The pelvic brim is contiguous anteriorly with the internal iliac fossa and is its medial border inferior to the sacroiliac joint. The pelvic brim also serves as the anterior border of the quadrilateral surface, which is bounded by the pelvic brim anteriorly, the greater and lesser sciatic notches posteriorly, the obturator foramen inferiorly, and the sciatic buttress superiorly. The iliopectineal eminence lies directly over the anterior wall of the acetabulum. The nutrient foramen of the iliac wing is a consistent landmark found adjacent to the sacroiliac joint. B: The external aspect of the innominate bone is shown. The retroacetabular surface is outlined. The greater and lesser sciatic notches make up the posterior border of the retroacetabular surface. (Reproduced with permission from Fractures of the Acetabulum—Classification and Radiographic Assessment. In: Oxford Textbook of Orthopaedics and Trauma. Oxford Press, in press.) |
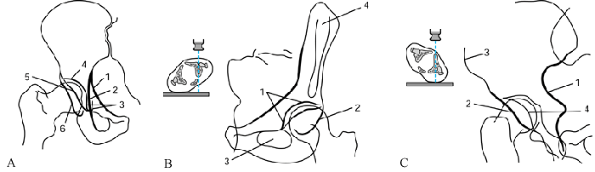
fractures, the surgeon must appreciate how the radiographic landmarks
of the pelvis correlate with the actual bony anatomy of the innominate
bone. Six basic landmarks of the acetabulum are described on the
anteroposterior (AP) view (Fig. 18.2A) (25).
The iliac oblique and obturator oblique radiographic views are 45°
oblique views of the pelvis. Both of these views are often referred to
as Judet views (Fig. 18.2B and Fig. 18.2C) (25).
 |
|
Figure 18.2. A: The normal radiographic lines of the acetabulum are shown as they appear in the anteroposterior radiographic view. 1, The iliopectineal line; 2, the ilioischial line; 3, the roentgenographic U, or teardrop; 4, the roof; 5, the anterior rim; and 6,
the posterior rim. The iliopectineal line corresponds to the inferior three fourths of the pelvic rim and is a landmark of the anterior column. The ilioischial line represents a posterior portion of the quadrilateral surface seen in tangent by the x-ray beam, and it is generally considered a landmark of the posterior column. Similarly, the roof of the acetabulum represents a portion of the superior acetabular subchondral bone seen in tangent by the x-ray beam. The medial limb of the teardrop is likewise formed from the obturator canal and inferior portion of the quadrilateral surface, seen in tangent by the x-ray beam. The anterior and posterior rims represent the lateral margin of the acetabular articular surface anteriorly and posteriorly, respectively. In the AP view, the anterior rim is typically medial to the posterior rim. B: The normal radiographic landmarks of the obturator oblique view. 1, The iliopectineal line; 2, posterior rim; 3, obturator ring; 4, anterosuperior iliac spine. The obturator oblique view is taken with a 45° rotation of the affected hip, away from the x-ray cassette. The iliopectineal line, as visualized on this view, has a similar relationship with the pelvic brim as on the AP view. The posterior rim of the acetabulum is best seen on this view. Fractures of the posterior wall and subtle amounts of anterior subluxation of the femoral head are best detected on the obturator oblique view. C: The normal radiographic landmarks of the iliac oblique view. 1, posterior border of innominate bone; 2, anterior rim; 3, anterior border of iliac wing; 4, posterior rim. Oblique views with appropriate rotation have the tip of the coccyx superimposed on the femoral head on the obturator oblique view. (All images reproduced with permission from Judet, R, Judet, J, Letournal E. Fractures of the Acetabulum: Classification and Surgical Approaches for Open Reduction. J Bone Joint Surg 1964;64A:1615.) |
In the majority of cases, the fracture pattern can be identified and
thus classified from plain films alone. Plain films are usually best
for assessing the congruence between the femoral head and the roof of
the acetabulum. Plain-film radiography
has
been the standard by which articular displacement has been measured,
both before and after surgery. In the emerging age of digital
radiography, however, in which the size of the AP pelvis and Judet
views is altered, the CT image may become a more reliable method of
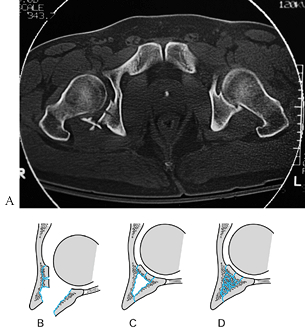
articular assessment. CT is better suited for evaluating certain
fracture characteristics including marginal impaction, rotation of
major fragments, coronal fracture lines, and incarcerated osteochondral
fragments (Fig. 18.3) (18,28,51).
 |
|
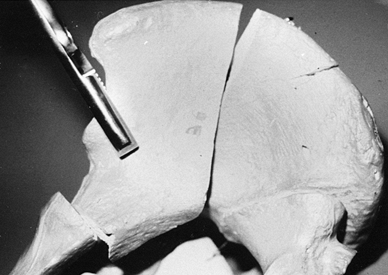
Figure 18.3. A:
Computerized tomography can demonstrate marginal impaction. (Reproduced with permission from Olson SA, Matta JM. Surgical Treatment of Acetabulum Fractures. In: Browner BD, Jupiter JB, Levine AM, Trafton PG, et al., eds. Skeletal Trauma, 2nd ed. Philadelphia: WB Saunders, 1997;1181.) B: The impacted articular surface and posterior wall fragments and posterior wall fractures are shown. C: The impacted articular fragments are elevated to match the contour of the femoral head, and bone graft is placed behind them to fill the defect created by their reduction. D: The posterior wall fracture is then reduced. (Modified from Letournel E, Judet R. Fractures of the Acetabulum. Berlin: Springer-Verlag, 1993.) |
gain a thorough understanding of the fracture and its displacement
pattern before intervening surgically. Such knowledge helps determine
what maneuvers may be necessary to reduce the displacement of a
particular pattern and which surgical approach will be used to treat
the fracture (28,38,62). Letournel’s classification is the most widely used system (25,28). It comprises five simple fracture types and five associated types (28).
-
Posterior wall fractures typically
disrupt the posterior rim of the acetabulum, a portion of the
retroacetabular surface, and a segment of the articular cartilage (28).
Instability of the hip (subluxation or dislocation of the femoral head)
can be associated with this fracture pattern. Marginal impaction of the
articular cartilage commonly occurs and should be diagnosed
preoperatively on plain films or CT scan (Fig. 18.3) (3).
Marginal impaction of the articular suface and underlying cancellous
bone occurs when the femoral head subluxes into a displaced major
fracture line. The articular
P.590
surface
of the edge of the major fracture line is displaced secondary to
impaction of the underlying cancellous bone, with malrotation of the
overlying articular surface. In Figure 18.3,
marginal impaction is noted as a change in the radius of curvature of
the articular surface. It is important for surgeons to recognize this
radiographic feature of articular displacement so that they can correct
the displacement. Complex posterior wall fractures can involve the
entire retroacetabular surface and include a portion of the greater or
lesser sciatic notch and the ischial tuberosity. The ilioischial line
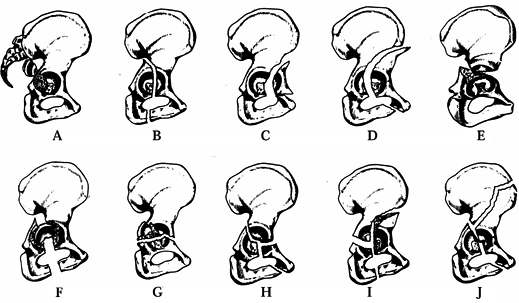
remains intact on the AP view (Fig. 18.4A).![]() Figure 18.4. Classification of acetabulum fractures according to Letournel. Posterior wall fracture (A); posterior column fracture (B); anterior wall fracture (C); anterior column fracture (D); transverse fracture (E); associated posterior column and posterior wall fractures (F); associated transverse and posterior wall fractures (G); T-shaped fracture (H); associated anterior and posterior hemitransverse fractures (I); fracture of both columns (J). (Reproduced with permission from Matta JM, Merrit PO. Trauma: Pelvis and Acetabulum. In: Fitzgerald RH, ed. Orthopaedic Knowledge Update II. American Academy of Orthopaedic Surgeons, 1987:348.)
Figure 18.4. Classification of acetabulum fractures according to Letournel. Posterior wall fracture (A); posterior column fracture (B); anterior wall fracture (C); anterior column fracture (D); transverse fracture (E); associated posterior column and posterior wall fractures (F); associated transverse and posterior wall fractures (G); T-shaped fracture (H); associated anterior and posterior hemitransverse fractures (I); fracture of both columns (J). (Reproduced with permission from Matta JM, Merrit PO. Trauma: Pelvis and Acetabulum. In: Fitzgerald RH, ed. Orthopaedic Knowledge Update II. American Academy of Orthopaedic Surgeons, 1987:348.) -
Posterior column fractures affect only the ischial segment of the bone (28).
The retroacetabular surface is displaced with the posterior column. The
fracture line separating the anterior from the posterior column
commonly enters the obturator foramen, and an associated fracture of
the inferior pubic ramus is typical. Fractures that run just posterior
to the obturator foramen, splitting the ischial tuberosity, constitute
a transitional pattern between the posterior wall and posterior column.
The ilioischial line is typically displaced and disassociated from the
teardrop. Uncommonly, when a large portion of the quadrilateral surface
remains intact and in continuity with the posterior column, the
teardrop and a portion of the pelvic brim are displaced with the
posterior column (Fig. 18.4B). -
Fractures of the anterior wall disrupt the central portion of the anterior column (28).
Comminution of the quadrilateral surface occurs in most cases; fracture
of the inferior pubic ramus is less often seen. The AP and obturator
oblique radiographs show displacement of the iliopectineal line. The AP
and iliac oblique radiographs show interruption or displacement of the
anterior rim contour (Fig. 18.4C). -
Anterior column fractures can occur anywhere on the column (28).
Very low fractures involve only the superior ramus and pubic portion of
the acetabulum. High fractures can involve the entire anterior border
of the iliac wing. The fracture line typically runs in the coronal
plane through the superior acetabulum. The iliopectineal line is
displaced. Medial translation of a portion of the roof or the entire
roof can be seen with displacement of a high or intermediate type of
anterior column fracture. This type of displacement also can be seen
with anterior column and posterior hemitransverse fractures, and
both-column fracture patterns as well (Fig. 18.4D). -
Transverse fractures divide the innominate bone into two portions (28).
An oblique sagittal plane fracture line crosses the acetabulum at a
variable level and is often displaced. The innominate bone is then
divided into a superior part composed of the iliac wing and a portion
of the roof of the acetabulum; the lower part of the bone, the
ischiopubic segment, is composed of an intact obturator foramen with
the anterior and posterior walls of the acetabulum. Letournel
subdivided transverse fractures as transtectal, a transverse fracture line that crosses the superior acetabular articular surface; juxtatectal,
a transverse fracture line that crosses at the junction of the superior
acetabular articular surface and superior cotyloid fossa; and infratectal, a transverse fracture line that crosses through the cotyloid fossa (Fig. 18.4E).
-
The association of a posterior column and
posterior wall fracture splits the posterior column into a larger
posterior column component and an associated posterior wall component (28). The ilioischial line is typically displaced and disassociated from the teardrop (Fig. 18.4F). -
The association of a transverse fracture
with a posterior wall fracture shows features of both—a typical
transverse configuration with one or more separate posterior wall
fragments (28). A fracture of the inferior pubic ramus is not typically associated with this very common pattern (Fig. 18.4G).
In the case of a displaced posterior wall fracture, pay careful
attention to the plain films to avoid missing a nondisplaced transverse
fracture line. -
The T-shaped
fracture is similar to the transverse fracture except that a vertical
fracture line runs along the quadrilateral surface and acetabular fossa
(the stem of the T), which separates the anterior from the posterior column (28).
An associated fracture of the inferior pubic ramus is typically
present. This vertical fracture line can enter the obturator foramen or
leave it intact, exiting through the ischium (Fig. 18.4H). -
The anterior plus posterior
hemitransverse fracture combines an anterior wall or anterior column
fracture with a horizontal transverse component, which typically
traverses the posterior column at a low level (Figure 18.4I) (28). The distinction between the associated anterior column and posterior hemitransverse and T-shaped
patterns is often subtle. In the anterior column plus posterior
hemitransverse fracture, the anterior component is typically at a
higher level and is more displaced than the posterior component,
whereas the T-shaped fracture is a
transverse fracture with an additional fracture line splitting the
anterior and posterior columns of the ischiopubic portion. The femoral
head typically follows the displacement of the anterior column in the
associated anterior column plus posterior hemitransverse pattern,
whereas the femoral head typically follows the posterior column in a T-shaped pattern. -
Fractures of both columns constitute a
distinct category in which the anterior and posterior columns are
separated from each other. All articular segments are detached from the
intact portion of the posterior ilium, which remains attached to the
sacrum (Fig. 18.4J) (28). The surgeon should differentiate transverse, associated transverse plus posterior wall, T-shaped,
and anterior plus posterior hemitransverse fractures—all of which show
involvement of the anterior and posterior columns of the
acetabulum—from both-column fractures. In those four fracture types, a
portion of the articular surface remains in its normal position,
attached to the intact portion of the ilium. The both-column fracture
is therefore unique, with its division of all segments of articular
cartilage from the ilium. The both-column fracture is associated with
the spur sign, in which the obturator oblique radiographic view
P.592
prominently
reveals the fractured edge of the intact posterior iliac wing relative
to the medially displaced articular segments. This sign is
pathognomonic of a both-column injury (Fig. 18.5) (28). Figure 18.5.
Figure 18.5.
An obturator oblique view demonstrates the spur sign of a both-column
fracture. This spur represents the intact portion of the iliac wing as
seen prominent and laterally (arrow) on
this view because the remainder of the articular segments of the
acetabulum have been displaced medially. (Reproduced with permission
from Olson SA, Matta JM. Surgical Treatment of Acetabulum Fractures.
In: Browner BD, Jupiter JB, Levine AM, Tafton PG, eds. Skeletal Trauma, 2nd ed. Philadelphia: WB Saunders, 1997;1181.)
some overlap between fracture types in Letournel’s system. If this
system of classification were perfectly symmetric, there would be more
than 10 categories. The extra groups are included within the 10
fracture types; for example, associated anterior column and anterior
wall are included with anterior column fractures. Similarly, a fracture
of the anterior wall plus posterior hemitransverse fracture is included
with anterior column plus posterior hemitransverse fracture. Associated
posterior column and anterior hemitransverse fractures, as well as
associated transverse and anterior wall fractures, are considered T-shaped fractures. Table 18.1 outlines some tips for classification.
 |
|
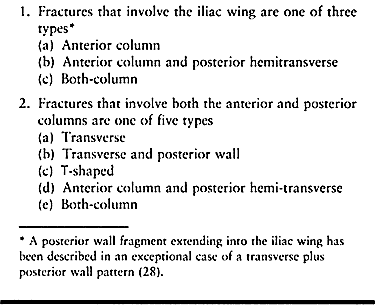
Table 18.1. Simple Tips for Classification of Fractures of the Acetabulum
|
acetabulum fractures to decrease the incidence of posttraumatic
arthritis. It also permits the patient to return to normal function
earlier than nonoperative treatment. Nonoperative treatment, however,
is successful in a minority of displaced acetabulum fractures.
Indications for nonoperative treatment are based on the condition of
the patient, analysis of the fracture configuration, and congruence of
the hip joint.
In patients who are candidates for surgery, attempts at closed
reduction by manipulation under anesthesia or skeletal traction are not
applicable for the treatment of displaced fractures of the acetabulum.
Typically, significant displacements tend to recur over time. If the
surgeon concludes from the initial radiographs that an accurate
reduction of the articular surface is necessary for a good prognosis,
surgery is usually indicated. Nonoperative treatment is reserved for
patients with nondisplaced fractures, those with tolerable incongruity
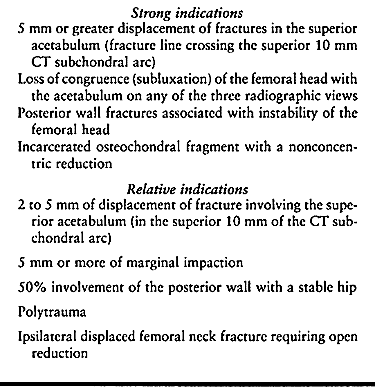
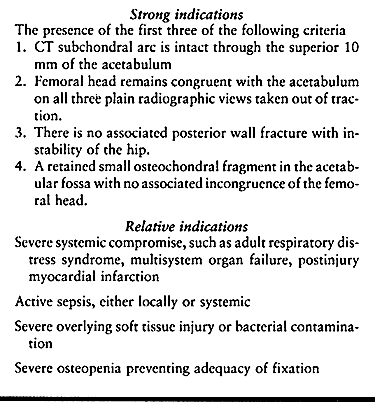
or displacement, and those in whom surgery is contraindicated. (See Table 18.2 and Table 18.3 for specific criteria.)
 |
|
Table 18.2. Indications for Surgical Treatment
|
 |
|
Table 18.3. Indications for Nonsurgical Treatment of Acetabular Fractures
|
In one group, a large portion of the acetabulum remains intact and the
femoral head remains congruous with this portion of the acetabulum. In
the other group, a secondary congruence is present following only
moderate displacement of a both-column fracture.
any of several different fracture types. Many low anterior column
fractures that involve only the pubic portion of the acetabulum can be
treated nonoperatively. Rarely, low T-shaped
or transverse fractures can be treated nonoperatively. In the case of
posterior wall fractures, indications for surgical stabilization
include in-stability or subluxation of the hip, associated marginal
impaction of the articular surface, and retainedosteochondral fragments with joint incongruence (54).
Each study reports three ranges of fracture size; in the first, the hip
is stable; in the second, the hip is unstable; and in the third,
instability is inconsistent, varying from 20% to 65% width of the
posterior wall, depending on the method of measuring the posterior wall
defect. Small posterior wall fractures associated with a stable hip
joint that have a congruent reduction can be managed nonoperatively.
Careful follow-up is needed to monitor for signs and symptoms of late
instability in the initial months following injury.
radiographs and CT images. Loss of the normal congruent relationship of
the femoral head with the acetabulum is frequently associated with
osteochondral fragments incarcerated within the acetabulum (54).
Review the three standard radiographic views of the pelvis (AP,
obturator oblique, and iliac oblique) to detect loss of parallelism
between the curvature of the femoral head and acetabular articular
surface on all three views (28). Similarly,
evaluate CT images to detect widening of the distance between the
anterior and posterior walls or acetabular fossa, and the femoral head (54).
Loss of congruency between the femoral head and acetabular articular
surface is often associated with the development of degenerative
arthritis of the hip.
assess the size of the intact portion of the acetabulum, which can be
determined using roof arc measurements (34,35 and 36).
We prefer to make them on CT scans. A CT scan of the superior
acetabular articular surface from the vertex to 10 mm inferior to the
vertex is equivalent to an area described by all three roof arc
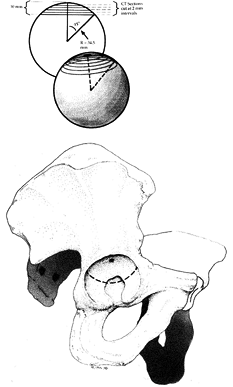
measurements of 45° (Fig. 18.6) (52). At 10 mm below the acetabular vertex, the subchondral bone appears as a ring or arc (Table 18.2 and Table 18.3).
 |
|
Figure 18.6.
The acetabulum with a line at the level of CT image at 10 mm inferior to the vertex of the acetabulum. The area of the acetabular articular surface, superior to this line, represents the minimum amount of intact bearing surface necessary for consideration of nonoperative treatment. This area is equivalent to the area intact when all three roof arc measurements are 45°. The inset diagram illustrates evaluation of the superior acetabulum by CT to 10 mm inferior to the vertex, in 2 mm intervals. (Reproduced with permission Olson SA, Matta JM. The Computerized Tomography Subchondral Arc: A New Method of Assessing Acetabular Articular Continuity After Fracture (A Preliminary Report). J Orthop Trauma 1993;7:402.) |
a unique situation. In both-column fractures, all articular segments
are detached from the intact ilium (28). Even
though displacement of the fracture has occurred, the fracture
fragments can remain congruously grouped around the femoral head
despite medial and proximal displacement of the femoral head and some
rotational displacement of the fragments (28,54).
Assess the three standard radiographic views of the pelvis to detect
loss of parallelism between the curvature of the femoral head and
acetabular articular surface. Consider loss of parallelism on any of
the three views to be an indication for surgery.
fracture and to prevent displacement from worsening. Skeletal traction
through a proximal tibia pin is often used. Neufeld roller traction is
a useful form of treatment
that allows motion of the hip and knee while the patient is in traction (40).
Traction should not be so great that it distracts the femoral head from
the acetabulum. Skeletal traction, particularly if initiated early
while the fracture hematoma is liquid, can occasionally produce a
surprisingly good reduction (62). Release of
traction before complete healing, however, typically results in
redisplacement of the fracture. We believe that lateral skeletal
traction through the greater trochanter is not beneficial and can even
cause severe problems such as infection of the greater trochanter or
soft tissues lateral to the hip joint. Do not use traction through the
greater trochanter if any surgical treatment is being considered.
Percutaneous fixation of moderately displaced (2–5 mm) acetabular
fractures may not improve the reduction and often provides
less-than-optimal fixation. Percutaneous fixation has also been used in
nondisplaced fractures to allow early patient mobilization (58).
In our experience, patients with nondisplaced acetabular fractures can
be moved from bed to chair without risk of significant displacement.
Percutaneous fixation techniques may have potential benefits, but at
this time definitive indications for percutaneous fixation have not
been developed.
injury, when the initial bleeding from the fracture and intrapelvic
vessels has subsided. Generally, use skeletal traction preoperatively
for posterior fracture patterns with hip instability out of traction.
In displaced transtectal fracture patterns, traction can help prevent
erosion of the femoral head cartilage on the residual intact acetabular
roof. It is also indicated for associated femoral fractures.
improving patient comfort preoperatively, but we have not found it
necessary. Schedule surgery before 10 days, ideally, so that the
fracture fragments remain mobile. Three weeks after injury, bony callus
is usually present, which makes reduction of the fracture more
difficult. Advanced age is not an absolute contraindication to surgery (19). Factors such as general medical status, pre-existing arthrosis, and bone quality may affect decision making.
the acetabulum. Following radiographic analysis and classification of
the fracture, the surgeon should be able to draw the fracture
configuration on a model or drawing of the innominate bone (32).
Preoperative considerations should include an understanding of the
fracture configuration on the outside and inside of the innominate
bone, and of the orientation of the fracture planes. This information
combined with appreciation of the benefits and limitations of each
surgical approach will allow the surgeon to select the appropriate
surgical procedure.
anterior and posterior columns, but each has its advantages and
disadvantages. We prefer to use the Kocher-Langenbeck, the
ilioinguinal, or the extended iliofemoral approach. Alternatively, the
triradiate approach gives an exposure roughly comparable to that of the
extended iliofemoral but provides limited access to the posterior
portion of the iliac wing.
to the posterior column. The ilioinguinal approach gives the best
access to the anterior column and the inner aspect of the innominate
bone. The extended iliofemoral approach gives the best simultaneous
access to the two columns, but it does not expose the anterior column
as well as the ilioinguinal approach does (28,37,61).
We prefer to choose a surgical approach with the expectation that the
entire reduction and fixation can be performed through that single
approach.
approach—that is, prone for the Kocher-Langenbeck approach, supine for
the ilioinguinal approach, and lateral for the extended iliofemoral
approach. Although the extended iliofemoral provides the best access,
it has the longest recovery period and the highest incidence of ectopic
bone formation (16,53). It is therefore preferable to choose the ilioinguinal or Kocher-Langenbeck approach, if feasible. See Table 18.4 for indications for the extended iliofemoral approach.
 |
|
Table 18.4. Indications for the Extended Iliofemoral Approach
|
successively are required less frequently and are usually less
desirable than the single approach. Concurrent use of the ilioinguinal
and Kocher-Langenbeck limits the access of the anterior column through
the Kocher-Langenbeck approach and posterior column through the
ilioinguinal approach. Successive ilioinguinal and Kocher-Langenbeck
approaches allow full use of both exposures but require intraoperative
repositioning (54). The use of combined
exposures is reserved for injuries such as an associated anterior
column and posterior hemitransverse pattern with significant
displacement of both the anterior column and low posterior
hemitransverse components, or juxtatectal or infratectal T-shaped fractures with significant displacement of both anterior and posterior columns. See Chapter 2 for a description of the approaches.
evaluation and has chosen the approach, re-duction of the fracture
remains the primary problem.Reduction of an acetabular fracture can be
extremely challenging. The technique of reduction is always tailored to
fracture type. Even for a specific fracture type, the choice of
technique frequently depends on the exact configuration of the
individual fracture (28,33,54).
maximizes the possibilities of each surgical approach. The fracture
table lessens the need for extensile as well as dual approaches (28).
It does not directly reduce the fracture but facilitates reduction by
returning the femoral head to normal position and aiding visualization
of the interior of the joint. An alternative to the fracture table is
the A-O femoral distractor (Synthes USA, Paoli, PA), which can be
placed between the ilium and proximal femur to apply distraction across
the hip joint. Although the femoral distractor can be effective, the
direction of pull it provides is sometimes not ideal and it can block
access to the wound.
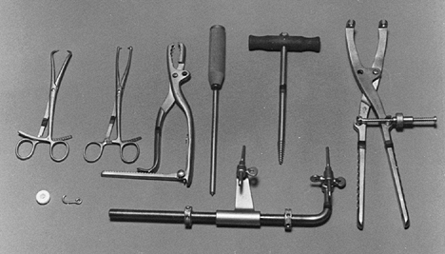
reducing acetabulum fractures. Several different types can grasp the
heads of screws, including Farabeuf clamps, adapted to grasp 3.5 mm or
4.5 mm diameter screws, and Jungbleuth forceps (A-O pelvic reduction
forceps, Synthes USA, Paoli, PA). Pointed reduction forceps are
helpful, as is a ball spike-tipped instrument that can be used for
pushing fracture fragments. A femoral head corkscrew or Schantz screw
can be inserted into the bone to control rotational displacement (Fig. 18.7).
 |
|
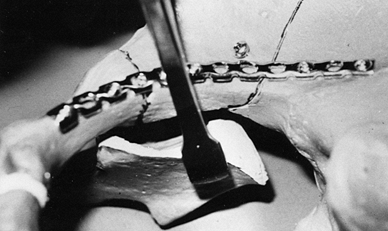
Figure 18.7. Instruments for acetabulum fracture reduction are shown.
|
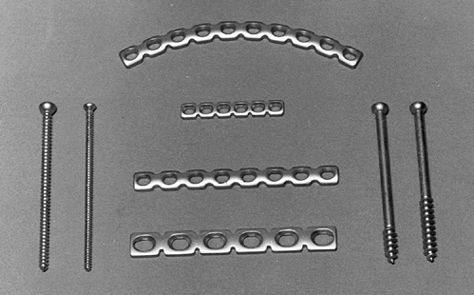
fashion, with reduction followed by fixation of individual fragments,
with progressive assembly of the fracture fragments. Initial lag screw
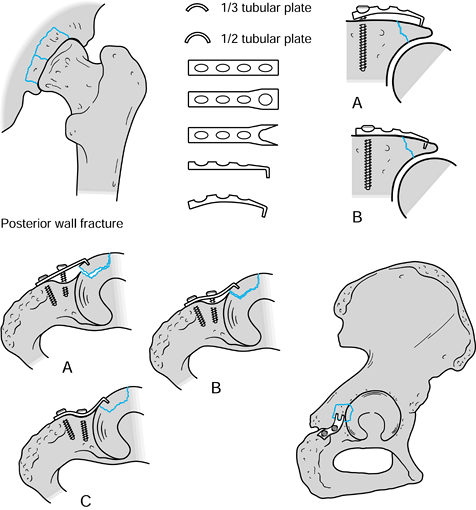
fixation (28,54) usually allows removal of the reduction forceps, followed by more definitive plate fixation (Fig. 18.8) (50).
Assess the reduction by visualization and palpation of the accessible
fracture lines. It is usually preferable to visualize the final
reduction on the articular surface, although sometimes the surgical
approach might preclude visualization. The final articular reduction
can be inferred to be correct by reduction of the fracture lines on the
extraarticular cortex of the innominate bone.
 |
|
Figure 18.8. Plates and screws used for acetabulum fixation are illustrated.
|
fragments in the reduction and fixation; these fragments are commonly
found along the pelvic brim, sciatic notch, and iliac crest. These
small fragments often provide an essential guide to the reduction of
the larger articular fragments and aid in providing final stability (28).
In reducing the initial fragments, it is important to obtain absolutely
accurate reduction. Any errors in reduction will be magnified as other
fracture fragments are reduced. Preliminary fixation with Kirschner
wires may be useful, but we prefer to use interfragmentary screws.
Screws work best that are 3.5 mm (or similar sizes) and must be
available in lengths exceeding 100 mm. Unless you need to penetrate
thick cortical bone, insert these screws without tapping; their
purchase in the bone is enhanced by the compression of cancellous bone
adjacent to the screw. The AO (Synthes U.S.A., Paoli, PA) oscillating
drill attachment is useful to minimize the risk of injury to soft
tissues. You need special long, flexible-handled drill guides and depth
gauges, and a full set of straight and precontoured 3.5 mm or similar
reconstruction plates. Make certain that a set of large fragment screws
is available.
-
Use the Kocher-Langenbeck approach.
-
Maintain capsular attachments to
posterior wall fragments to enhance vascularity of the posterior wall
fragment and improve postreduction stability. -
Expose the entire fracture and clean it of hematoma.
-
In the case of marginal impaction,
elevate the impacted articular surface with underlying cancellous bone.
Use the femoral head as a template for reduction of the impacted
articular segment. Be certain that the femoral head is in a reduced
position (Fig. 18.3A) (3,28). -
Stabilize the marginal impaction. Use
bone grafting behind the elevated articular surface to fill the void
left by impacted bone. (The role of bone graft substitutes in
supporting marginal impaction is unclear at this time.) Bone graft is
commonly obtained from the ipsilateral greater trochanter (Fig. 18.3B, Fig. 18.3C and Fig. 18.3D). -
Reduce the posterior wall fragments using
the acetabular rim and the retroacetabular surface as guides. Consider
using screws for provisional interfragmentary fixation. -
Contour a 3.5 mm or similar
reconstruction plate to buttress the posterior wall fragment. The plate
should curve to parallel the rim of the acetabulum (Fig. 18.9).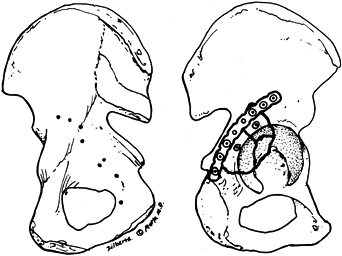 Figure 18.9. Fixation of a posterior wall fracture through the Kocher-Langenbeck approach is shown.
Figure 18.9. Fixation of a posterior wall fracture through the Kocher-Langenbeck approach is shown. -
Undercontour the plate to buttress the posterior wall.
-
Apply the first screw into the ischial
tuberosity (in an inferior and anterior direction), initially leaving
it three to five turns loose. -
Apply a screw superior to the posterior
wall fragment, through the plate. Hold the plate and fracture in a
reduced position with a ball spike to ensure that the plate is
congruent superiorly with the iliac wing. -
Tighten the ischial screw to tension the plate, and buttress the posterior wall fracture.
-
Ideally, insert one or two interfragmentary screws through the posterior wall fragment, either through or outside of the plate.
-
Use springplates to hold small rim pieces with capsular attachments in place (30).
We recommend not excising bony fragments from the capsular attachments,
because it is difficult to reattach the hip capsule securely (Fig. 18.10).![]() Figure 18.10.
Figure 18.10.
Springplates are illustrated. This type of fixation can be used to
secure small periarticular fragments. Top Figures: A one-third tubular
or reconstruction plate is flattened. The end hole is divided, and the
remaining two tines bent. Bottom Figures: The spring effect of applying
the plate allows the prongs to stabilize as small fragments. Often
these plates can be buttressed with an overlying posterior wall plate,
using a common hole to allow a screw to secure both plates at once.
(Modified from Mast J, Jakob R, Ganz R. Planning and Reduction Technique in Fracture Surgery. Berlin: Springer-Verlag, 1989.)
-
Position the patient prone and use the Kocher-Langenbeck approach.
-
Reduce the fracture with Farabeuf or
Jungblueth forceps. Insert a Shantz pin, if necessary, in the ischial
tuberosity to control rotation (Fig. 18.11) (28).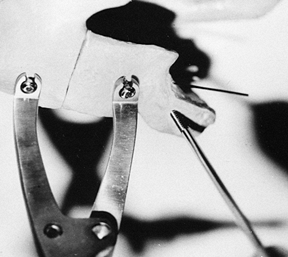 Figure 18.11.
Figure 18.11.
A pelvic reduction (Jungbleuth) forceps is used to reduce the posterior
column fracture line. A Shantz pin in the ischial tuberosity is used to
help control rotation of the posterior column fragment. -
Assess reduction, using the fit to the
posterior rim and greater sciatic notch as guides. Assess the
retroacetabular surface and quadrilateral surface for rotation of the
posterior column fragment. -
Obtain fixation with an interfragmentary screw and, if possible, double plates.
-
Position the patient supine and use an ilioinguinal approach.
-
Fractures that are incomplete near the iliac crest usually must be completed to gain access to and reduce the joint.
-
Initially, reconstruct comminuted
fragments at the level of the pelvic brim. These small fragments often
provide important keys to reduction of the larger anterior column
segment. -
The displacement of the anterior column
fragment is typically in external rotation, medial translation, and
flexion. Reduction requires that these elements of displacement be
addressed. Internal rotation, lateral translation, and a posteriorly
directed force usually are required to reduce the anterior column
segment. Lateral or distal traction can aid in obtaining the reduction (Fig. 18.12).![]() Figure 18.12.
Figure 18.12.
Control of the anterior column rotation can be performed with a
Farabeuf forceps about the inner spinous notch, as shown. A ball spike
or other instrument applied to the inferior iliac fossa in combination
with a Farabeuf forceps can provide a force to counteract the
deformation and displacements of the anterior column. -
Impaction of the articular surface should
be recognized preoperatively. Occasionally, by externally rotating or
distracting the anterior column fragment, the surgeon is able to work
through the fracture to reduce the impacted fragment. In other cases,
you may need to reduce the anterior column first. Then use a tamp or
other instrument to reduce the articular surface through a drill hole
in the innominate bone, the way you would to reduce the articular
surface in a centrally depressed tibial plateau fracture. -
Assess the fracture reduction along the
internal iliac fossa and at the pelvic brim. It is often necessary and
important to palpate a fracture line that extends posterior to the
pelvic brim on the quadrilateral surface. You must be certain that
there is no excessive residual medial translation of the anterior
column segment. -
For initial fixation, insert
interfragmentary screws perpendicular to the fracture plane; insert
additional interfragmentary screws or plates at the iliac crest. -
In most cases, neutralize the interfragmentary screws with a reconstruction plate along the pelvic brim.
-
Position the patient supine and use an ilioinguinal approach.
-
It is necessary to mobilize all windows of the ilioinguinal approach.
-
Quadrilateral surface comminution is commonly associated with significantly displaced anterior wall fractures.
-
Use lateral and distal traction to assist in the reduction.
-
It may be impossible to insert
interfragmentary screws into the anterior wall directly because of the
risks of intraarticular screw placement. Reduce the anterior wall under
direct vision and buttress it with a plate on the pelvic brim. -
Quadrilateral surface comminution can
often be secured with a lagscrew from the lateral surface of the iliac
wing inserted just above the acetabulum into the quadrilateral surface.
Leave the screw slightly long (approximately 5 mm) to act as a buttress
inside the quadrilateral surface.
-
For most fracture patterns, position the patient prone and use the Kocher-Langenbeck approach.
-
Use a Jungbleuth forceps to distract the fracture. Clean the fracture of hematoma, and reduce the ischiopubic segment.
-
Reduce the fracture by levering the
ischiopubic segment posteriorly and laterally. Insert a Schantz pin, if
needed, in the ischium for rotational control. Avoid excessive
compression of the transverse fracture. The transverse fracture is most
often an oblique fracture line in the sagittal plane. Excessive
compression leads to malreduction with the shearing of the fracture
fragments along the fracture line. Place a small angled forceps through
the greater sciatic notch, if necessary, to control rotation. -
An alternative reduction technique is to
use an antiglide plate on the retroacetabular surface. This technique
requires accurate contouring of the plate before application. -
Use the posterior rim and the greater
sciatic notch as guides to the reduction. Palpate the retroacetabular
surface and quadrilateral surface to assess rotation of the ischiopubic
segment. -
Gain initial fixation with a lag screw
across the anterior column. Begin the anterior column screw
approximately 1 cm lateral to the apex of the greater sciatic notch and
run it parallel to the quadrilateral surface. Direct the screw toward
the superior pubic ramus. Use fluoroscopy to place this screw. -
If possible, place a posterior column interfragmentary screw as well. At this point, remove the Jungbleuth forceps.
-
Apply a posterior plate to tension the fracture posteriorly, as described for posterior wall fractures.
-
Note that applying the posterior plate in
an undercontoured manner, as described for a posterior wall fracture,
before placing the anterior column interfragmentary screw causes a gap
in the anterior portion of the transverse fracture line.
-
Position the patient prone and use the Kocher-Langenbeck approach.
-
Reduce and provisionally stabilize the transverse component first.
-
Use the posterior wall fracture as a window to view the articular reduction of the transverse fracture.
-
The reduction techniques are similar to those used for a transverse fracture.
-
Use anterior and posterior column lag
screws or an anterior column lag screw and posterior column plate for
provisional fixation. -
Reduce the posterior wall, as described above in the posterior wall fracture section.
-
Stabilize the posterior wall with a buttress plate, as described above (Fig. 18.13).
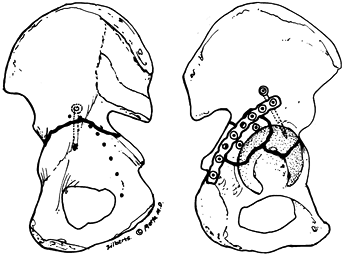 Figure 18.13. Fixation of an associated transverse and posterior fracture through the Kocher-Langenbeck approach.
Figure 18.13. Fixation of an associated transverse and posterior fracture through the Kocher-Langenbeck approach.
-
Position the patient prone and use the Kocher-Langenbeck approach.
-
Reduce the posterior column segment first, as described above in the posterior column section.
-
Provisionally fix the posterior column
fragment with an interfragmentary screw or with a plate that will not
interfere with the reduction or fixation of the posterior wall fracture. -
Reduce the posterior wall fracture and plate it (see posterior wall section, above).
-
Position the patient supine and use an
ilioinguinal approach. Fractures with a markedly displaced anterior
column component and a displaced low posterior column component may
benefit from sequential ilioinguinal and Kocher-Langenbeck approaches. -
First address the anterior column or anterior wall component.
-
Reduce the anterior column, as detailed above, in the anterior column section.
-
Insert interfragmentary screws in the anterior column to gain initial fixation.
-
Often, you can assess the reduction of
the posterior column fracture on the quadrilateral surface. The typical
displacement is medial translation of the posterior column. Use a large
or so-called King Tong clamp or an offset clamp from the AO pelvic
reduction instruments (Synthes USA, Paoli, PA) to reduce the
quadrilateral surface segment. Place one tine on the external surface
of the iliac wing, and one tine on the quadrilateral surface to provide
a lateral displacement force through the posterior hemitransverse
component. -
Use posterior column screws to fix the
posterior hemitransverse fracture. Insert the screws through the most
lateral window of the ilioinguinal approach, parallel to the greater
sciatic notch and contained within the posterior column. Use the C-arm fluoroscope to confirm position; obtain an iliac oblique view. -
Neutralize the entire construct with a plate on the anterior pelvic brim (Fig. 18.14).
![]() Figure 18.14. Fixation of an associated anterior column and posterior hemitransverse fracture through the ilioinguinal approach.
Figure 18.14. Fixation of an associated anterior column and posterior hemitransverse fracture through the ilioinguinal approach.
-
Significant displacement of both anterior and posterior column segments of the T-type fracture are especially difficult to manage. Displaced transtectal T-shaped
fractures can be managed through an extended iliofemoral approach.
Significant displacement of juxtatectal and infratectal T
shapes may require sequential Kocher-Langenbeck and ilioinguinal
approaches. In the situation in which there is significant displacement
of both anterior and posterior portions of the T-shaped fracture, address the less comminuted portions first (Fig. 18.15).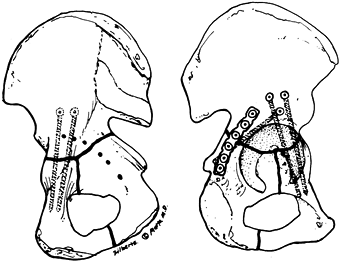 Figure 18.15. Fixation of a T-shaped fracture through the extended iliofemoral approach.
Figure 18.15. Fixation of a T-shaped fracture through the extended iliofemoral approach. -
Carefully inspect the level of the fracture. It is often possible to treat a low anterior column fracture component in a T
pattern (below the superior 10 mm CT subchondral arc) without surgery,
addressing only the posterior column component of the injury. -
Reduce and fix the anterior and posterior column components, as described in the sections on the anterior and posterior columns, above.
-
In the majority of instances of
both-column fractures, position the patient supine and use the
ilioinguinal approach. Approximately one quarter to one third of cases
require an extended iliofemoral approach. The ilioinguinal is
preferable, when possible, because it involves minimal stripping of the
outer aspect of the innominate bone, which decreases the postoperative
recovery time and decreases the amount of heterotopic ossification
postoperatively. -
When choosing the ilioinguinal approach, first reduce the anterior column and fix it provisionally.
-
Lateral traction is frequently necessary to lateralize the femoral head before the anterior column can be adequately reduced.
-
The anterior column fracture is reduced and internally fixed, as described in the section on the anterior column.
-
Reduce the posterior column segment
through the second window of the ilioinguinal approach. The posterior
column is typically medially displaced, with occasional distal
translation. Reduce the fracture with a reduction forceps, placing one
tine on the quadrilateral surface, and the other tine on the outer
aspect of the iliac wing. Assess the reduction both visually and by
palpating the quadrilateral surface and the contour of the greater
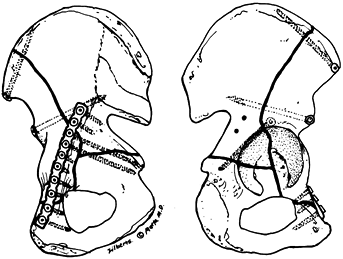
sciatic notch (Fig. 18.16).![]() Figure 18.16.
Figure 18.16.
Reduction of the posterior column component of a both-column fracture
through the ilioinguinal approach is shown. The posterior column is
visualized through the second window of the approach. The reduction is
performed by lateralizing the medially displaced posterior column
following provisional fixation of the anterior column. -
To fix the posterior column, insert lag
screws from the internal iliac fossa, near the pelvic brim, into the
posterior column. Use an image intensifier to confirm reduction and
screw placement. -
When choosing the extended iliofemoral
approach, position the patient in the lateral position on the fracture
table. The extended iliofemoral approach allows the surgeon to perform
a nearly circumferential capsulotomy (avoiding transsection of the
capsular attachments to the posterior wall fragments) and provides the
most commanding view of the articular surface. -
In most cases, reduce the anterior column and fix it initially to the intact portion of the ilium.
-
Occasionally, if the posterior column
segment is large and involves a portion of the sacroiliac joint, it is
often easiest to proceed with reduction of the posterior column first. -
In most cases, use a two-screw technique
to reduce the fragment. Use the Farabeuf forceps to grasp the screw
left prominent in each fracture fragment. -
Following reduction, fix the posterior wall and column as described in previous sections (Fig. 18.17).
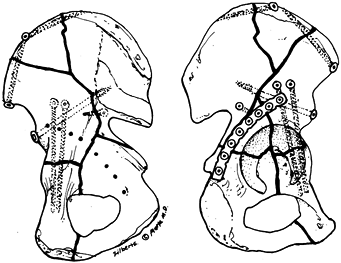 Figure 18.17. Fixation of a both-column fracture through the extended iliofemoral approach.
Figure 18.17. Fixation of a both-column fracture through the extended iliofemoral approach.
AP pelvis radiograph in the operating room. The iliac oblique and
obturator oblique views can be obtained in the operating room or later.
Following gait training, and prior to discharge, obtain another AP
pelvic radiograph to confirm that loss of reduction has not occurred
during ambulation. Obtain a single AP pelvic radiograph at each
follow-up examination.
postoperative day, or longer if you have used the extended iliofemoral
approach. Have a physical therapist institute passive motion of the hip
and extremity. Alternatively, use the continuous passive motion
machine. At 3 to 7 days after surgery, pain has usually subsided enough
so that the patient can start gait training. Allow up to 15 kg of
weight bearing. Encourage the patient to ambulate with a step-through
gait and a heel-toe walking motion, using crutches or a walker.
extension exercises to be performed at the hip while standing (active
abduction and passive adduction are prohibited for the first 4 weeks
with the extended iliofemoral approach). Continue limited weight
bearing for 8 weeks postoperatively. At that point, the patient can
bear weight to tolerance using external support only, as needed. If the
fracture has been reduced accurately and ectopic bone does not develop,
the range of motion can be expected to return to about 90% of normal.
Physical therapy is therefore directed primarily toward regaining
muscle strength at the hip, particularly abductor muscle strength (53).
is to restore the normal shape and contour of the acetabular or
articular surface accurately and thereby to restore the hip joint’s
normal capacity. The results of surgical treatment of acetabular
fractures are generally reported on those who underwent surgery within
the first 3 weeks after injury and those who waited longer than 3
weeks. Letournel observed that in delayed surgeries, fractures were
more difficult to reduce and had less favorable outcomes (28).
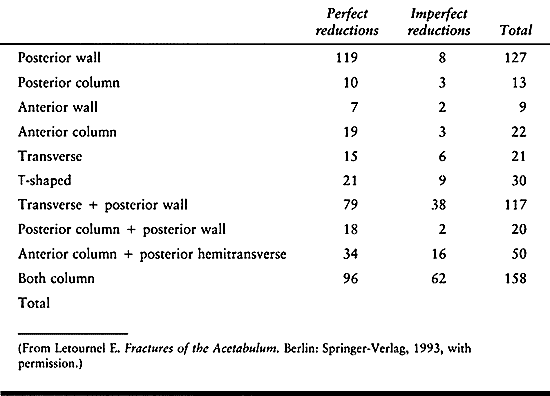
articular reductions were reported as perfect, implying that the
articular surface and radiologic landmarks of the acetabulum were
returned to normal alignment on the AP pelvis and 45° oblique views of
the pelvis. Osteoarthritis was reported in 97 cases (23%), 43 (10.2%)
had a perfect reduction, and 54 (12.9%) had an imperfect reduction (Table 18.6).
Of 492 cases available for a minimum of 2 years of follow-up, 366 had a
perfect reduction. An excellent or very good clinical grade applied in
283 (77%) cases, and 316 (86%) had a good, very good, or excellent
result. Of 126 imperfect reductions (including secondary congruence),
24 (19%) had an excellent clinical grade and 81 (64%) had a good, very
good, or excellent result (28).
 |
|
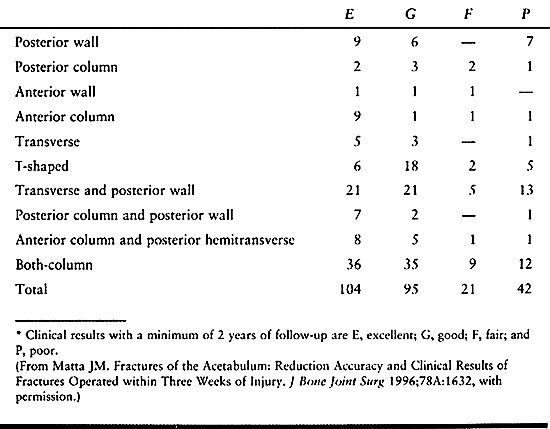
Table 18.5. Accuracy of Reduction by Fracture Type for 567 Acetabular Fractures Surgically Repaired within 21 Days of Injury
|
 |
|
Table
18.6. Number of Cases Developing Osteoarthritis (OA) Versus Accuracy of Reduction by Fracture Type for 492 Acetabular Fractures Surgically Treated within 21 Days of Injury |
that 28 of 35 cases initially graded excellent remained excellent (40
of 75 cases were lost to follow-up) (28). The
outcome of fractures followed for more than 20 years showed that none
of three very good results and four of eight good results maintained
the initial clinical grade. Letournel also noted that patients with
initially excellent clinical results who had developed an asymptomatic
collarette of osteophytes about the femoral head had an increased
incidence of osteoarthritis, 22% and 53% at 20- and 25-year follow-up,
respectively (28).
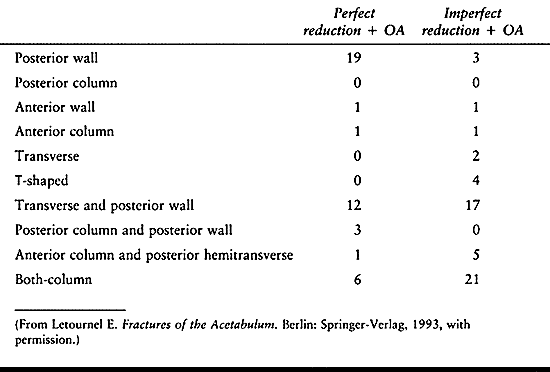
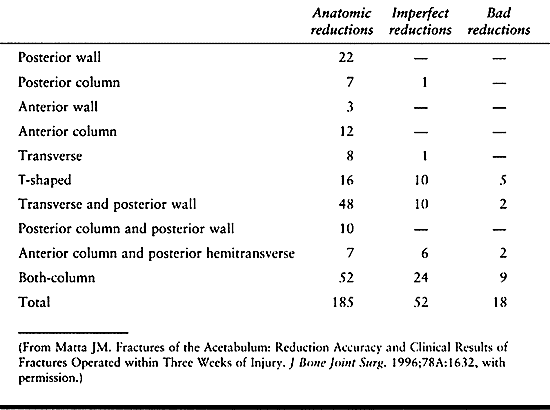
treated surgically within 21 days of injury and followed for 2 to 13
years (38). Reductions were graded on the
maximum articular displacement seen on the AP pelvis and 45° oblique
radiographic views of the pelvis. Reductions were categorized as
anatomic: 0 to 1 mm maximal
displacement;
imperfect: 2 to 3 mm maximal displacement; and bad: more than 3 mm
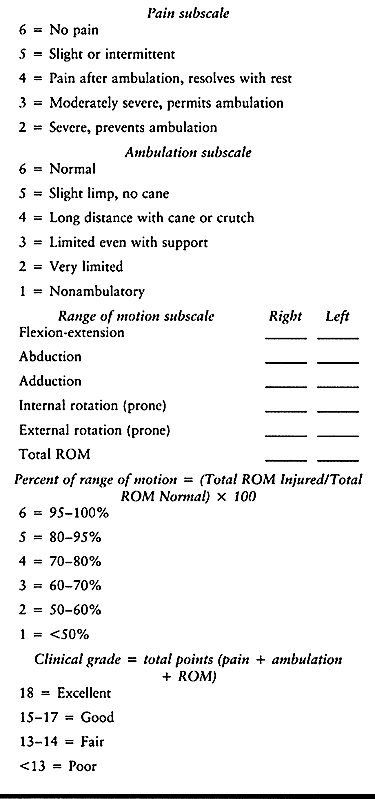
maximal displacement. Clinical outcome was determined by a modified
d’Aubigne and Postel hip score (Table 18.7). The quality of reduction per fracture type is listed in Table 18.8.
 |
|
Table 18.7. Modified d’Aubigne and Postel Clinical Grading System
|
 |
|
Table 18.8. Accuracy of Reduction by Fracture Type for Acetabular Fractures Treated Surgically within 21 Days of Injury
|
and 92% of excellent and good clinical results were also graded
excellent or good radiologically with no or minimal changes of
osteoarthritis (38). Anatomic reductions (p = .002) paired with a congruent relationship of the femoral head to the superior acetabulum (p = .04) were associated with a good or excellent outcome (38).
Age greater than 40 years and increasing complexity of the fracture
decreased the likelihood of a perfect reduction. Anatomic reductions in
patients over the age of 40 years, however, are not associated with a
decreased incidence of good or excellent clinical results. Kaplan-Meyer
survivorship analysis of these data indicates that an excellent
radiographic appearance of the hip joints at 2 years after surgery
indicates an 85% likelihood of excellent hip function at 10 years after
fracture (56).
 |
|
Table
18.9. Clinical Result (Modified d’Aubigne and Postel Score) by Fracture Type for Acetabular Fractures Treated Surgically within 21 Days of Injury* |
following surgical treatment of acetabular fractures, with up to 43%
incidence of poor results (21,26,68).
These reports typically represent the outcomes of patients at a single
institution whose operations were performed by a number of different
surgeons. As a result, the statistics cannot be compared with any one
surgeon’s experience with these complex injuries. The results of
Letournel and Matta emphasize the correlation of accuracy of articular
restoration with improved clinical outcome (28,38). Mayo has reported similar results (39).
dedicated interest in the treatment of acetabular fractures. The
importance of the knowledge, interest, and experience of the operating
surgeon in the treatment of these complex injuries cannot be
overemphasized. We disagree with the philosophy of approaching
acetabular fracture reconstruction as restoration of bone stock for a
future total hip replacement. Inherent in this way of thinking is the
assumption that the development of osteoarthritis is inevitable. This
misconception may lead some surgeons to accept significant
malreductions of the articular surface, leading to the development of
unnecessary disability caused by osteoarthritis of the hip. We believe
the goal of obtaining a perfect reduction must be in the mindset of the
operating surgeon as she undertakes reduction and fixation of
acetabular fractures (54).
outcome, it is difficult to predict which fractures will have a poor
outcome following open reduction and internal fixation. The long-term
follow-up data of Letournel and Matta suggest that a minority of
patients will require further hip surgery following acetabular fracture
reconstruction (28,38). We do not recommend total hip arthroplasty as a primary treatment for fractures of the acetabulum.
than 21 days after injury are challenging to even the most experienced
surgeons. There is increased difficulty in mobilizing
fracture
fragments and reducing the articular surface. Johnson et al. reported
on 188 fractures treated surgically between 21 and 120 days after
injury (24).
There was an increased incidence of sciatic nerve palsies (12%) and
osteonecrosis of the femoral head (13%), with 50% of the osteonecrosis
occurring with persistent dislocation for more than 3 weeks. Overall,
there was a 65% incidence of good or excellent results. The poorest
results occurred in simple anterior wall fractures, simple posterior
wall fractures, associated transverse and posterior wall fractures, and
T-shaped fractures.
treatment of an acetabulum fracture include infection of the surgical
wound, iatrogenic sciatic nerve palsy, periarticular ectopic bone
formation, and thromboembolic complications. Posttraumatic arthritis is
the most common late complication (28).
associated injuries, the risk of infection should be no higher than for
other types of major hip surgery. Most patients with acetabular
fractures, however, have associated injuries, including injuries to the
abdominal and pelvic viscera, chest, or the extremities. A bladder
rupture or a bowel, rectal, or vaginal injury can increase the chance
of infection in the surgical wound and can influence the indications
for surgery.
fracture is local soft-tissue injury, including local wounds,
abrasions, and a closed degloving injury (17).
With the closed degloving injury, the subcutaneous tissue is torn away
from the underlying fascia. There is a significant cavity that contains
hematoma and liquefied fat between the subcutaneous tissue and deep
fascia. The degloving injury occurs as a result of the blunt trauma
that has caused the acetabular fracture. When this lesion is present
over the greater trochanter, it is known as a Morel-Lavalle lesion (17).
Drain and debride these areas before or at the start of surgery to
decrease the risk of infection. After drainage and debridement, it is
advisable to leave this area open through the surgical incision or a
separate incision. Dressing changes and wound packing are sometimes
necessary over a prolonged period, until the wound has closed
secondarily or with delayed primary closure. In our experience, primary
excision of the necrotic fat and immediate closure over drainage tubes
has been unsuccessful.
even without associated injuries. There is an increased risk of
postoperative hematoma formation in the large wounds that are necessary
for acetabular surgery. Make liberal use of suction drains. Good
hemostasis at the time of wound closure is essential. During the
procedure, keep the large areas of exposed soft tissue moist and
irrigated frequently with antibiotic solution. It is often helpful to
place moist sponges over exposed soft tissue to prevent desiccation.
bone fragments to maintain the blood supply to the bone. If a fragment
is devascularized, it generally revascularizes rapidly, as long as no
infection develops. In the presence of infection, however, bacteria
rapidly colonize an avascular fragment, and it will usually need to be
debrided and excised. Some bloody drainage can seep from the wound for
the first 1 or 2 days after surgery, but it should subside rapidly. It
is not uncommon for a clear, yellow, serous drainage to be present for
as long as 10 days after surgery without infection being present. If
the wound has been benign for a number of days, and bloody or cloudy
yellowish drainage then occurs, the patient should be returned to the
operating room immediately for irrigation and debridement of the wound.
If a wound hematoma is present, the amount of hematoma is usually much
greater than initially suspected, and surgical drainage is indicated.
culture of a wound aspiration but proceed with reopening the wound. If
it is later found that no infection was present, little harm has been
done. If an infection is in fact present at the time of the earliest
clinical suspicion, then you have acted properly by treating the
infection expeditiously. Hip aspiration may be particularly helpful in
evaluating fractures in which the surgical approach has been
ilioinguinal.
controlled successfully and the functional result will not be impaired.
In the case of an intraarticular infection, however, the cartilage of
the joint is almost invariably destroyed and hip function is
significantly impaired.
This event occurs primarily with the Kocher-Langenbeck approach and
mainly involves the peroneal branch of the sciatic nerve (28).
There is also a small chance of a stretch injury to the sciatic nerve
with the extended iliofemoral approach and a slight possibility of
injuring the femoral nerve by stretch injury during the ilioinguinal
approach, but these outcomes are unusual. The surgeon must constantly
monitor the force and duration of pull that surgical assistants place
on retractors in the vicinity of the sciatic nerve. It is helpful to
keep the patient’s knee flexed at least 60° and preferably at 90°, and
the hip extended whenever the Kocher-Langenbeck or extended iliofemoral
approach is used (28). Several authors have reported using neurologic monitoring with somatosensory evoked potentials or electromyography (20,44,65).
This technique is not available in every center. If a nerve palsy
develops, it is best treated with an ankle-foot orthosis. Iatrogenic
nerve palsies are often a form of axonotmesis (13). Electromyography can be helpful in determining reinnervation of affected muscle groups.
approach and probably also by the initial muscle trauma suffered by the
patient (16,45,46).
The combination of the two injuries creates an inflammatory response
that triggers the formation of bone. Several factors have been
correlated with heterotopic ossification: the extended iliofemoral
approach, multiple (two or more) findings at time of surgery, T-shaped fractures, associated head or chest trauma, and male sex (16,26,45,66).
(HO), most commonly occurs with the lateral exposure of the innominate
bone. The incidence of significant ectopic bone formation is highest
with the extended iliofemoral approach, followed by the
Kocher-Langenbeck approach; it is almost nonexistent with the
ilioinguinal approach (28). Prevention of
ectopic bone formation should, in part, be directed toward choosing the
ilioinguinal approach whenever possible and limiting muscle trauma
during surgery.
perioperatively, and for several months following surgery, has been
reported to be helpful in decreasing the incidence and extent of
ectopic bone formation (46). A prospective
randomized series comparing indomethacin to no prophylaxis, however,
showed no difference in the incidence of HO (31).
Postoperative radiation has been shown to be effective in decreasing
the incidence of ectopic bone formation, but the long-term carcinogenic
effects are unknown (42). The combination of
indomethacin and postoperative radiation has been reported to be very
effective in preventing nearly all HO (47). The
risk of HO may be reduced by avoiding elevation of the periosteum,
minimizing muscle trauma, preventing hematomas, and by debridement of
devitalized tissue following completion of internal fixation of the
acetabular fracture.
as seen on radiographs, but muscle function and range of motion may
remain satisfactory. Radiographic evaluation should include AP and 45°
oblique views of the pelvis (48). In other
patients, rotation and abduction are limited; if patients can extend
the hip to the neutral position and have flexion of at least 90°,
however, they might be happy with the result and have no need for
further surgery. CT is important to locate HO about the hip when
excision is being considered (54).
should be delayed for 6 to 12 months following injury. If it is
performed at this time, there is usually no problem with recurrence and
motion can be expected to return to more than 80% of normal, assuming
no arthritis is present. Some patients show a spontaneous regression of
ectopic bone over several years. If the indications for excision of the
bone are equivocal, it might be best to wait, with the hope of some
spontaneous regression of the ectopic bone with improvement of motion.
See Chapter 124 for more details.
We normally use pneumatic compression boots on both lower extremities
from the time of admission until the patient is fully ambulatory. In
older and high-risk patients, partial anticoagulation is begun with
heparin following surgery. Patients are discharged to home with
warfarin anticoagulation until they are ambulating actively, typically
for 3 to 4 weeks following surgery (14). The
level of anticoagulation with warfarin is maintained at about 1.5 times
normal, an international ratio (INR) of 2 to 3. Although the potential
for thromboembolic complications is always present, the surgeon must be
cautious about too much anticoagulation, because a large-wound hematoma
can have a devastating effect on the patient if a deep infection in the
hip results.
trauma to the hip joint. Motor vehicle accidents or other high-energy
traumas account for the majority of hip dislocations. Athletic
injuries, falls, and other causes are less common. Hip dislocations are
generally categorized by the direction of dislocation of the femoral
head, either posterior or anterior. Posterior dislocation accounts for
approximately 90% of all traumatic hip dislocations (12).
Posterior dislocation is typically caused by axial load on the femoral
shaft with the hip in the position of flexion and adduction. The most
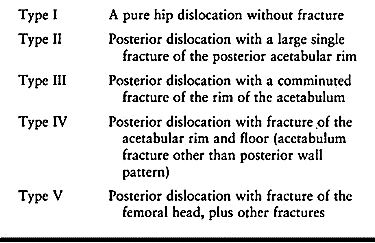
commonly cited classification is that of Thompson and Epstein (Table 18.10) (12).
Acetabular fractures associated with posterior hip dislocations have
been postulated to result from impact of the femoral head on the hip
with the thigh in a flexed and adducted position. Epstein reported that
fractures of the femoral head occurred in 9% of posterior hip
dislocations (12).
 |
|
Table 18.10. The Classification System of Posterior Dislocations of Thompson and Epstein (11).
|
Anterior dislocations can be divided into pubic or obturator
dislocations. Well over 90% of all anterior dislocations are obturator
in nature. We have not personally managed a patient with a pubic
anterior dislocation.
were impaction fractures of the femoral head. The articular impaction
presumably resulted from impingement of the femoral head against the
anterior rim of the acetabulum as it rebounded against the anterior rim
of the acetabulum. Anterior dislocation typically occurs when the hip
is overabducted and overextended.
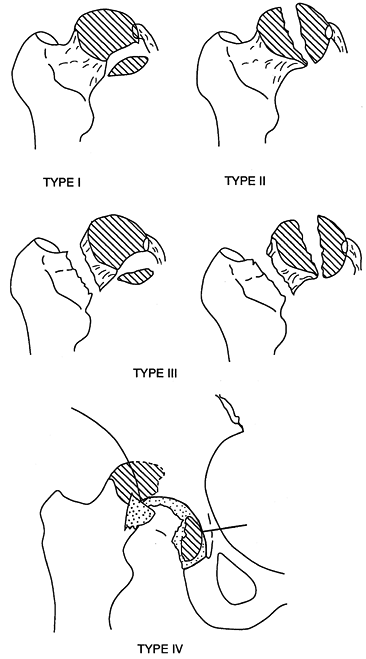
Pipkin’s classification is commonly used with or without a hip
dislocation when there is a displaced osteochondral fragment of the
femoral head. Brumback et al. proposed a classification system that
separates anterior dislocations of the hip with either a femoral head
impaction fracture or transchondral loss into a distinct group (4). No uniform system exists to quantify femoral head impaction following hip dislocation.
injury, ranging from isolated trauma to significant polytrauma. The
classic position of the lower extremity with a posterior hip
dislocation is one of shortening of the involved extremity, with
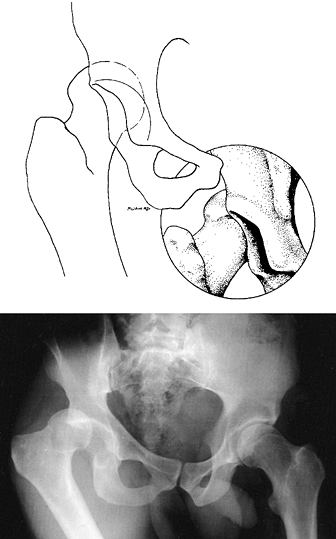
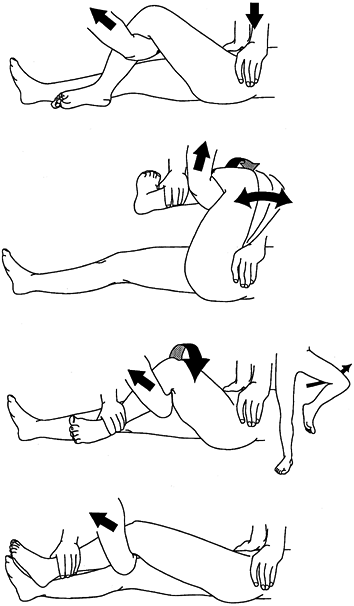
flexion, adduction, and internal rotation of the extremity at the hip (Fig. 18.19) (1,2,12).
This classic position may not be seen if a significant acetabular
fracture or fracture of the femoral shaft coexists with the hip
dislocation. Injury to the sciatic nerve has been reported to occur in
approximately 10% of all hip dislocations (12).
The involvement of the sciatic nerve may be partial or complete. More
severe involvement of the peroneal division of the sciatic nerve is
typical. A detailed neurologic exam, which may be difficult to obtain
in the
emergency setting, is important. Carefully examine the patient’s neurologic status both before and after reduction of the hip.
 |
|
Figure 18.19.
Posterior dislocation of the hip is shown. The adducted and internally rotated position of the femur is classic for this type of dislocation. The overlapped appearance of the femoral head and the roof of the acetabulum on the radiograph is pathognomonic for dislocation of the femoral head. |
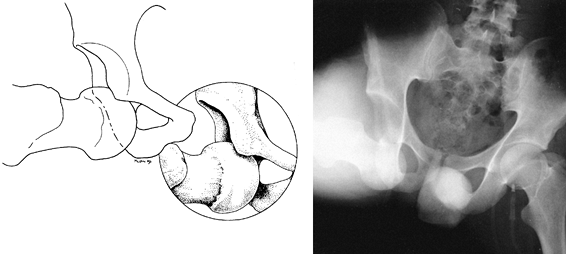
displaced anteriorly and inferior to the acetabulum in the region of
the obturator foramen, with the extremity held in extension, wide
abduction, and external rotation at the hip (Fig. 18.20) (12). Carefully examine for possible injury to the femoral artery and femoral nerve.
 |
|
Figure 18.20.
Anterior dislocation of the hip is shown in these drawings. The obturator (inferior) presentation shown is by far the most common pattern. It is characterized by abduction and external rotation of the femur. Impaction fractures of the femoral head are common with this type of dislocation. |
dislocation requires an AP view of the pelvis. The majority of hip
dislocations can be diagnosed on this view. The addition of a
cross-table lateral view should confirm an anterior or posterior
dislocation. Following reduction of the hip dislocation, repeat the AP
radiograph of the pelvis and lateral view of the hip, looking for
evidence of incongruent reduction of the femoral head. If there is a
question of an acetabular fracture, 45° oblique views of the pelvis
(Judet views) are indicated (54). CT is helpful for evaluation of
residual incongruence between the femoral head and the acetabulum,
evaluation of acetabular fractures identifying femoral head fractures,
and identification of retained osteochondral fragments within the hip
joint (15).
established, perform reduction of the hip as soon as possible, ideally
with complete muscular relaxation under a regional or general
anesthesia to minimize the risk of chondral injury to cartilage of the
femoral head. In addition, it is possible to examine the hip while the
patient is still under anesthesia to assess the stability following
reduction. Such assessment may aid in deciding postoperative care.
emergency room setting with appropriate intravenous sedation. Use
short-acting paralyzing agents with caution and only when appropriate
airway management is available. Delay in reduction of hip dislocations
has been shown to increase the incidence of avascular necrosis. Yue et
al. reported that posterior dislocation of the hip causes kinking of
the external iliac artery over the pelvic brim, impeding flow through
the medial femoral circumflex artery in cadaver specimens (69). Perform reduction of the femoral head early, ideally within 6 hours of injury, to minimize the risk of avascular necrosis (12,22).
associated fractures of the femoral head and femoral neck. When these
associated fractures are present, the reduction should be accomplished
under general anesthesia, preferably with image intensifier control to
ensure that significant displacement of the femoral neck fracture does
not occur. In selected cases, fixation of the femoral neck fracture
before reduction may be necessary.
been described that involve traction in line with the existing
deformity. For posterior dislocations, the Allis and Bigelow maneuvers
are performed with the patient supine; an assistant provides
countertraction to the pelvic ring (Fig. 18.21) (1,2).
The Stimpson maneuver, performed with the patient prone, eliminates the
need for countertraction on the pelvis. Other injuries and the need for
sedation may contraindicate the prone position (59).
 |
|
Figure 18.21. The Bigelow reduction maneuver for a posterior dislocation of the hip.
|
on the involved hip in a flexed and adducted position. Gentle
rotational oscillation of the hip may assist in easing it over the
acetabular rim into the socket.
lateral decubitus position. Use of a sheet around the pelvis for
countertraction provides the surgeon added mechanical advantage. Once
the femoral head has been located, the hip is easily abducted and
extended accompanied by restoration of leg lengths and external
rotation of the hip. In rare instances, the dislocation may be
irreducible and requires open reduction through a posterior approach (5).
applying traction in line with the deformity in abduction, with
progressive flexion of the hip and neutral rotation (12).
This technique allows the femoral head to move superiorly and
posteriorly into the acetabulum. Rarely it may be converted,
temporarily, to a posterior dislocated position before location of the
hip.
of the pelvis and look for incongruence between the femoral head and
acetabulum, as well as for fractures of the femoral head and femoral
neck, and retained osteochondral fragments. Obtain a cross-table
lateral view of the hip if there is a question about the adequacy of
the reduction or of a femoral neck fracture. Persistent incongruence of
the hip joint with retained osteochondral fragments requires open
reduction and removal of the intraarticular debris. CT can also be used
to assess the hip joint for incongruence and retained osteochondral
fragments following reduction of a hip dislocation (7,51).
CT is indicated, however, whenever the surgeon suspects the presence of
a significant retained osteochondral fragment or other foreign body
within the hip joint. Occasionally, small osteochondral fragments are
seen in the acetabular fossa which are attached to the ligamentum
teres. When these osteochondral fragments are present, AP and Judet
views of the hip, CT, or both are indicated to assess the femoral head
for a congruent reduction. There is no need for surgical intervention
as long as a congruent reduction between the femoral head and
acetabulum is present (54). Perform neurovascular examination immediately after reduction.
Several authors have speculated that postreduction traction would
provide the benefit of decompressing the injured hyaline cartilage
while the torn capsule heals (12,57). This observation, however, has not been borne out in clinical results.
stability by gently flexing the hip from 0° to 90° with the hip in
neutral rotation. Those patients who have a stable hip to 90° of hip
flexion must avoid excessive flexion, adduction, and internal rotation
of the hip and can be permitted to walk with crutches with limited
weight bearing for 4 to 7 days after reduction. Weight bearing can be
gradually increased after that point. Continue these precautions for at
least 6 weeks after dislocation as healing of the soft tissues takes
place.
instability between 45° and 90° of flexion, protect against dislocation
with an orthosis. Use either a knee mobilizer or hip abduction brace
for 6 weeks and allow the patient to walk using crutches as described
above. If the hip is unstable at 45° or less of flexion, we recommend
skeletal traction for approximately 3 weeks postoperatively, followed
by bracing or crutches as described above.
acetabulum require treatment of the acetabular fracture, as outlined in
the first part of this chapter. Hip dislocations associated with
femoral neck fractures are, fortunately, a rare occurrence. Treatment
of these injuries requires careful reduction of the hip under image
intensification control.
Make
every attempt to ensure that the femoral neck is not displaced during
reduction. If there is any question regarding displacement of the
femoral neck during the attempt at reduction, fixate the femoral neck
before performing open or closed reduction of the femoral head
dislocation. Place a Schantz pin from the lateral cortex up into the
femoral head, attached to a T-handle
to reduce the shear forces across the femoral neck and aid the
reduction. Hip dislocations with a displaced femoral neck fracture are
an absolute indication for open reduction of the femoral neck fracture
and femoral head dislocation.
It is important to characterize the inferior femoral head fragment and
fracture line on plain films. Moed et al. described the use of CT to
determine the plane of inclination of the femoral head fracture
relative to the sagittal plane (43). Plain
radiographs taken with the x-ray beam oriented at this inclination were
shown to provide good evaluation of the fracture and subsequent healing.
 |
|
Figure 18.18.
The figure shows the classification of femoral head fractures, as described by Pipkin type I, a fracture of the femoral head below the fovea. Type II is a fracture of the femoral head that extends above the fovea. Type III is a fracture of the femoral head, either type I or type II, with an associated fracture of the femoral neck, and type IV is a fracture of the femoral head, either type I or type II, with an associated acetabulum fracture. |
may be successfully managed in postoperative traction or, on occasion,
in pelvic-hip orthoses for 6 weeks (22,29). Displaced Pipkin type I fragments treated nonsurgically have poor clinical outcomes (11,22,29).
Excise comminuted fragments. Large fragments without comminution can be
successfully treated with open reduction and internal fixation. Epstein
(10) recommended a posterior approach for open
reduction and internal fixation of these fractures, but recently
Swionkowski et al. and other authors (8,29,60)
have advocated an anterior approach. Typically a Smith-Peterson
approach or direct anterior approach to the hip can be used with an
arthrotomy along the acetabular rim, with a T
extension in the anterior hip capsule. These fragments can be
stabilized with various small fragment screws countersunk below the
articular cartilage or with absorbable screws (Fig. 18.22).
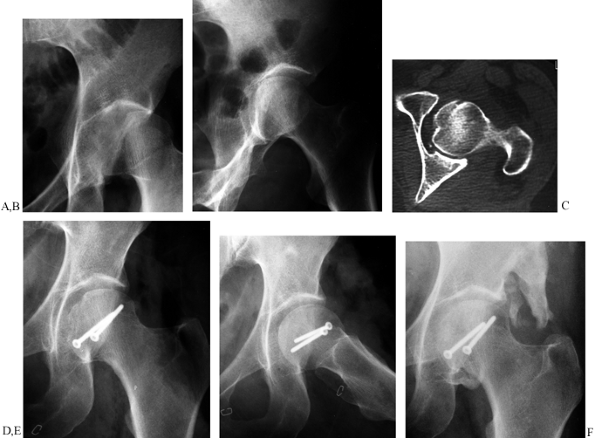 |
|
Figure 18.22. A: An anteroposterior (AP) view of the left hip demonstrates a dislocation of the femoral head with a femoral head fracture. B:
An iliac-oblique view of the involved hip after closed reduction. This demonstrates continued subluxation of the femoral head, and displacement of the inferior Pipkin type I fragment. C: Computerized tomography scan of the left hip demonstrates a mismatch between the Pipkin fragment and the residual femoral head. D, E: AP and lateral views of initial fixation with two small countersunk screws with anatomic restoration of the femoral head and normal congruence of the hip joint. The surgery was performed through an iliofemoral approach. F: AP view of the left hip at 1 year of follow-up. There is a small amount of heterotopic ossification that does not limit the patient’s range of motion. The joint space is maintained, and the fracture is healed. |
Reserve internal fixation of anatomically reduced Pipkin type II
injuries for those patients in whom prolonged traction is
contraindicated. Displaced Pipkin type II fractures require open
reduction of the fragment through an anterior approach (60).
this procedure requires redislocation of the hip. Additionally,
soft-tissue attachments of the head fragment to the ligamentum teres
must be cut in order to reduce and fix the fracture. Visualization of
the fragment is limited, compromising the procedure.
A fracture of the femoral neck can accompany either a type I or type II
femoral head fracture. In this situation, reduction and fixation of the
femoral neck fracture are of paramount importance to help restore
normal blood supply to the femoral head. An anterior approach to the
hip joint provides direct access to both the femoral neck and femoral
head, allowing the surgeon to perform an open reduction of both
fractures.
Carefully inspect prereduction radiographs for evidence of a femoral
neck fracture. If you find a nondisplaced femoral neck fracture, it is
advisable to perform percutaneous fixation of the femoral neck before
attempting reduction of the hip. In this case, use either a posterior
or anterior approach to the hip. The outcome of type III Pipkin
injuries is frequently poor; satisfactory outcomes have been reported
in a minority of cases (11,22,29).
For this reason we recommend open reduction and internal fixation,
particularly in the young patient with this complex injury.
If the femoral head fracture is nondisplaced, it can be treated with 3
to 4 weeks of traction postoperatively. If mobilization is
contemplated, however, it may be necessary to perform internal fixation
or excision of the femoral head fragment. Consider sequential surgical
approaches for an unstable inferior posterior wall fracture that
requires open reduction. Use internal fixation, followed by an anterior
approach, to repair or excise a femoral head fragment. Occasionally, a
superior posterior wall segment can be treated through a Smith-Peterson
approach at the time of incision or repair of the femoral head fragment.
associated with anterior dislocation of the hip. This kind of injury
has been shown to predispose patients to posttraumatic arthritis (9).
At this time, there is no effective treatment for reduction and
fixation of femoral head impaction injuries. Intertrochanteric
osteotomy to move the fracture away from the typical superior location
has been proposed as a treatment method to prevent the development
of
arthritis in small femoral head impaction injuries. There are no data,
however, to demonstrate that this method prevents the development of
posttraumatic arthritis in the long term.
Recent work by Yue et al. has demonstrated that posterior dislocation
is associated with kinking of the external iliac artery over the pelvic
brim and causes obstruction of flow in the medial femoral circumflex
artery (69). Prompt reduction of the femoral
head is recommended following the diagnosis of dislocation to decrease
the incidence of osteonecrosis. Osteonecrosis often does not manifest
clinically for 12 to 36 months following injury. Letournel reported an
incidence of osteonecrosis of 7% with posterior fracture dislocation of
the hip associated with acetabular fractures (28).
They noted a 16% incidence of traumatic arthritis, with an additional
8% incidence of arthritis secondary to avascular necrosis. In their
series, manual laborers were more likely than sedentary workers to
develop traumatic arthritis of the hip following hip dislocation.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
RW, Wheeless G. Irreducible Posterior Fracture-Dislocations of the Hip.
The Role of the Iliofemoral Ligament and the Rectus Femoris Muscle. Clin Orthop 1982;167:118.
MS, Zych G, Latta L, et al. Computerized Tomography Evaluation of
Stability in Posterior Fracture Dislocations of the Hip. Clin Orthop 1988;227:152.
AJ, Green RA, Brooks LR, Matta JM. Prevention of Deep Vein Thrombosis
and Pulmonary Embolism in Acetabular and Pelvic Fracture Surgery. Clin Orthop 1994;305:133.
N, Matta JM, Bernstein L. Heterotopic Ossification Following Operative
Treatment of Acetabular Fracture: An Analysis of Risk Factors. Clin Orthop 1994;305:96.
DJ, Olson SA, Matta JM. Diagnosis and Management of Closed Internal
Degloving Injuries Associated with Pelvic and Acetabular Fractures: The
Morel-Lavalle Lesion. J Trauma 1997;42:1046.
DL, Schmeling GJ. Somatosensory Evoked Potential Monitoring in the
Surgical Treatment of Acute, Displaced Acetabular Fractures. Results of
a Prospective Study. Clin Orthop 1994;301:213.
FA, Bone LB, Border JR. Open Reduction and Internal Fixation of
Acetabular Fractures: Heterotopic Ossification and Other Complications
of Treatment. J Orthop Trauma 1991;5:439.
JE, Brashear HR, Guilford WB. Stability of Posterior
Fracture-Dislocations of the Hip: Quantitative Assessment Using
Computed tomography. J Bone Joint Surg 1988;70A:711.
JM, Siebenrock KA. Does Indomethacin Reduce Heterotopic Bone Formation
After Operations for Acetabular Fractures? A Prospective Randomized
Study. J Bone Joint Surg 1997;79B:959.
JM. Fractures of the Acetabulum: Accuracy of Reduction and Clinical
Results in Patients Managed Operatively within Three Weeks after the
Injury. J Bone Joint Surg 1996;78A:1632.
MD, Garay ME, Schemitsch EH, Kreder HJ, Stephen DJ. Irreducible
Fracture-Dislocation of the Hip: A Severe Injury with a Poor Prognosis.
J Orthop Trauma 1998;12:223.
BR, Karges DE. Prophylactic Indomethacin for the Prevention of
Heterotopic Ossification after Acetabular Fracture Surgery in High-Risk
Patients. J Orthop Trauma 1994;8:34.
KD, Potter HG, Helfet DL. Magnetic Resonance Venography to Evaluate the
Deep Venous System of the Pelvis in Patients Who Have an Acetabular
Fracture. J Bone Joint Surg 1995;77A:1639.
SA, Matta JM. The Computerized Tomography Subchondral Arc: A New Method
of Assessing Acetabular Articular Continuity After Fracture (A
Preliminary Report). J Orthop Trauma. 1993;7:402.
MC, Matta JM. The Correlation between Early Radiographic Results and
Long-Term Clinical Outcome Following Fracture of the Acetabulum. J Am Acad Orthop Surg 1998.
MF, Thorpe M, Seiler JG, Hansen ST. Operative Management of Displaced
Femoral Head Fractures: Case-Matched Comparison of Anterior Versus
Posterior Approaches for Pipkin I and Pipkin II Fractures. J Orthop Trauma 1992;6:437.
SS, Moulton A, Burwell RG. Biological Factors Predisposing to Traumatic
Posterior Dislocation of the Hip. A Selection Process in the Mechanism
of Injury. J Bone Joint Surg 1985;67:232.
M, Gordon RG, Mears DC, et al. Intraoperative Somatosensory Evoked
Potential Monitoring of Pel-vic and Acetabular Fractures. J Orthop Trauma 1992;6:50.
LX, Bosse MJ, Mayo KA, et al. Results in Patients with Craniocerebral
Trauma and an Operatively Managed Acetabular Fracture. J Orthop Trauma 1990;4:376.
RH, Goulet JA, Bray TJ, et al. Deep-Vein Thrombosis after Fracture of
the Pelvis: Assessment with Serial Duplex-Ultrasound Screening. J Bone and Joint Surg 1990;72A:495.
R, Barrett K, Christie MJ, Johnson KD. Acetabular Fractures: Long-Term
Follow-up of Open Reduc-tion and Internal Fixation. J Orthop Trauma 1994;8:397.