Wrist
-
Although wrist injuries are fairly
common, especially with athletic participation, the true incidence is
unknown owing to a failure to recognize carpal injuries in the presence
of associated, more obvious injuries.
-
The distal radius has articular facets
for the scaphoid and lunate separated by a ridge. The sigmoid notch
articulates with the distal ulna. -
The distal ulna articulates with the
sigmoid notch of the distal radius. The ulna styloid process serves as
the attachment for the triangular fibrocartilage complex (TFCC). -
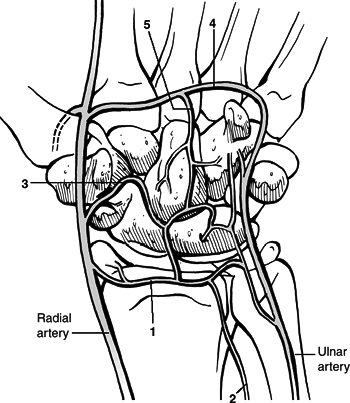
Carpal bones (Fig. 23.1)
-
Proximal row: This consists of the scaphoid (an oblique strut that spans both rows), lunate, triquetrum, and pisiform.
-
Distal row: The trapezium, trapezoid,
capitate, and hamate are connected to one another and to the base of
the metacarpals by strong ligaments, making the distal row relatively
immobile. -
The lunate is the key to carpal stability.
-
It is connected to both scaphoid and triquetrum by strong interosseous ligaments.
-
Injury to the scapholunate or
lunotriquetral ligaments leads to asynchronous motion of the lunate to
dissociative carpal instability patterns.
-
-
-
Joints: These are the distal radioulnar, radiocarpal, and midcarpal.
-
Normal anatomic relationships (see Fig. 23.1)
-
Radial inclination: averages 23 degrees (range, 13 to 30 degrees)
-
Radial length: averages 11 mm (range, 8 to 18 mm)
-
Palmar (volar) tilt: averages 11 to 12° (range, 0 to 28 degrees)
-
The 0-degree capitolunate angle: a
straight line drawn down the third metacarpal shaft, capitate, lunate,
and shaft of radius with wrist in neutral position -
The 47-degree scapholunate angle (normal range, 30 to 70 degrees); less than 2 mm scapholunate space
-
-
Wrist ligaments (Figs. 23.2 and 23.3)
-
Extrinsic ligaments connect the radius to the carpus and the carpus to the metacarpals.
-
Intrinsic ligaments connect carpal bone to carpal bone (e.g., scapholunate and lunotriquetral ligaments).
-
In general, the volar ligaments are stronger than the dorsal ligaments.
-
Important volar ligaments include:
-
The radioscaphocapitate (guides scaphoid kinematics).
-
The radioscapholunate (stabilizes the scapholunate articulation).
-
The radiolunate.
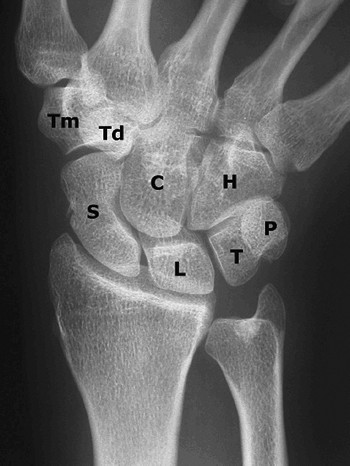 Figure 23.1. The wrist is composed of two rows of bones that provide motion and transfer forces: scaphoid (S), lunate (L), triquetrum (T), pisiform (P), trapezium (Tm), trapezoid (Td), capitate (C), hamate (H).(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 23.1. The wrist is composed of two rows of bones that provide motion and transfer forces: scaphoid (S), lunate (L), triquetrum (T), pisiform (P), trapezium (Tm), trapezoid (Td), capitate (C), hamate (H).(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
The radiolunotriquetral (supports the proximal row, stabilizes the radiolunate and lunotriquetral joints).
P.238 -
-
The proximal and distal carpal rows are attached by capsular ligaments on each side of the lunocapitate joint.
-
Injury to these ligaments leads to abnormal motion between the two rows and to nondissociative wrist instability patterns.
-
-
Space of Poirier: This ligament-free area in the capitolunate space is an area of potential weakness.
-
The TFCC is a major stabilizer of the ulnar carpus and distal radioulnar joint.
-
The TFCC absorbs about 20% of the axial load across the wrist joint.
-
It consists of several components,
including the radiotriquetral ligament (meniscal homologue), articular
disc, ulnolunate ligament, and ulnar collateral ligament.
-
-
-
Vascular supply (Fig. 23.4)
-
The radial, ulnar, and anterior
interosseous arteries combine to form a network of transverse arterial
arches both dorsal and volar to the carpus. -
The blood supply to the scaphoid is
derived primarily from the radial artery, both dorsally and volarly.
The volar scaphoid branches supply the distal 20% to 30% of the
scaphoid, whereas branches entering the dorsal ridge supply the
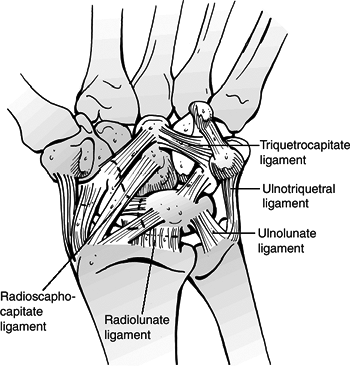
proximal 70% to 80%.![]() Figure
Figure
23.2. The palmar capsule consists of two major ligamentous inclusions:
the radiolunate ligament is the deeper of the two, which proceeds to
the triquetrum and composes in effect the radiolunotriquetral ligament.
The more distal and superficial component is often referred to as the
arcuate ligament or distal V. The radial component of this ligament is
the radioscaphocapitate ligament. The ulnar component of the arcuate
ligament is the triquetrocapitate ligament.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
The lunate receives blood supply from
both its volar and dorsal surfaces in most cases (80%). About 20% of
lunates have only a volar blood supply.
P.239 -
-
Kinematics
-
The global motion of the wrist is
composed of flexion and extension, radioulnar deviation at the
radiocarpal joint, and axial rotation around the distal radioulnar
joint. -
The radiocarpal articulation acts as a
universal joint allowing a small degree of intercarpal motion related
to rotation of individual carpal bones. -
The forearm accounts for about 140 degrees of rotation.
-
Radiocarpal joint motion is primarily
flexion and extension of nearly equal proportions (70 degrees), and
radial and ulnar deviation of 20 and 40 degrees, respectively. -
The scaphoid rests on the
radioscaphocapitate ligament at its waist. Using the ligament as an
axis, it rotates from a volar flexed perpendicular position to a
dorsiflexed longitudinal position.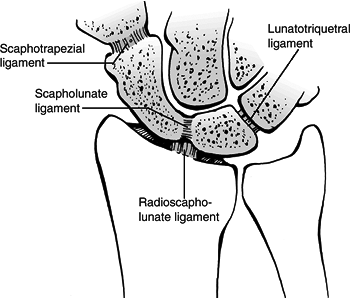 Figure 23.3. The intraarticular intrinsic ligaments connect adjacent carpal bones.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 23.3. The intraarticular intrinsic ligaments connect adjacent carpal bones.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
P.240 -
-
Pathomechanics (Fig. 23.5)
-
Classically, the radius, lunate, and capitate have been described as a central “link” that is colinear in the sagittal plane.
-
The scaphoid serves as a connecting
strut. Any flexion moment transmitted across the scaphoid is balanced
by an extension moment at the triquetrum. -
When the scaphoid is destabilized by
fracture or scapholunate ligament disruption, the lunate and triquetrum
assume a position of excessive dorsiflexion (dorsal intercalated
segmental instability [DISI]) and the scapholunate angle becomes
abnormally high (>70 degrees). -
When the triquetrum is destabilized
(usually by disruption of the lunotriquetral ligament complex) the
opposite pattern (volar intercalated segmental instability [VISI]) is
seen as the intercalated lunate segment volarflexes.
-
-
The most common mechanism of carpal
injury is a fall onto the outstretched hand, resulting in an axial
compressive force with the wrist in hyperextension. The volar ligaments
are placed under tension with compression and shear forces applied
dorsally, especially when the wrist is extended beyond its physiologic
limits.
 |
|
Figure
23.4. Schematic drawing of the arterial supply of the palmar aspect of the carpus. Circulation of the wrist is obtained through the radial, ulnar, and anterior interosseous arteries and the deep palmar arch: 1, palmar radiocarpal arch; 2, palmar branch of anterior interosseous artery; 3, palmar intercarpal arch; 4, deep palmar arch; and 5, recurrent artery. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
The clinical presentation of individual
carpal injuries is variable, but in general, the most consistent sign
of carpal injury is well-localized tenderness. -
Gross deformity may be present, ranging from displacement of the carpus to prominence of individual carpal bones.
-
Provocative tests may reproduce or
exacerbate pain, crepitus, or displacement indicative of individual
carpal injuries (see specific carpal injuries).
-
Posteroanterior (PA) and lateral x-rays are each taken in the neutral position.
-
Gilula lines (three smooth radiographic arcs) should be examined on the PA view. Disruption of these arcs indicates ligamentous instability.
-
-
For further diagnosis of carpal and mainly scaphoid fractures.P.242
-
A scaphoid view (anteroposterior [AP] x-ray with wrist supinated 30 degrees and in ulnar deviation) is obtained.
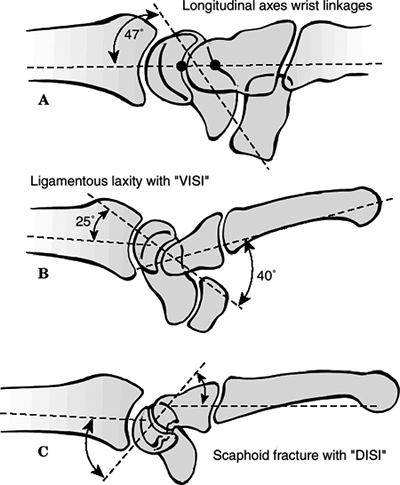 Figure
Figure
23.5. Schematic drawing of carpal instability. (A) Normal longitudinal
alignment of the carpal bones with the scaphoid axis at a 47-degree
angle to the axes of the capitate, lunate, and radius. (B) A volar
intercalated segmental instability (VISI) deformity is usually
associated with disruption of the lunatotriquetral ligament. (C) A
dorsal intercalated segmental instability (DISI) deformity is
associated with scapholunate ligament disruption or a displaced
scaphoid fracture.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Baltimore: Lippincott Williams & Wilkins, 2005.) -
A pronated oblique view is indicated.
-
-
If there is the suspicion of carpal
instability, additional views in maximal radial and ulnar deviation are
recommended as well as a clenched-fist PA. -
Further views can be done in maximal flexion and extension.
-
Arthrography, magnetic resonance (MR),
wrist arthrography, videoradiography, and arthroscopy can assist in the
diagnosis of carpal ligament injuries. -
Computed tomography (CT) scans are helpful in evaluating carpal fractures, malunion, nonunion, and bone loss.
-
MRI scans are sensitive to detect occult
fractures and osteonecrosis of the carpal bones as well as detecting
soft tissue injury, including ruptures of the scapholunate ligament and
TFCC.
-
Fractures of the scaphoid are common and account for about 50% to 80% of carpal injuries.
-
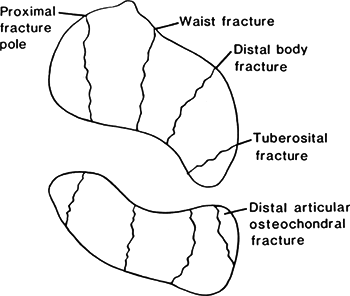
Anatomically, the scaphoid is divided
into proximal and distal poles, a tubercle, and a waist; 80% of the
scaphoid is covered with articular cartilage (Fig. 23.6). -
Ligamentous attachments to the scaphoid
include the radioscaphocapitate ligament, which variably attaches to
the ulnar aspect of the scaphoid waist, and the dorsal intercarpal
ligament, which provides the primary vascular supply to the scaphoid. -
The major vascular supply is derived from
scaphoid branches of the radial artery, entering the dorsal ridge and
supplying 70% to 80% of the scaphoid, including the proximal pole. The
remaining distal aspect is supplied through branches entering the
tubercle. Fractures at the scaphoid waist or proximal third depend on
fracture union for revascularization (Fig. 23.7). -
The most common mechanism is a fall onto
the outstretched hand that imposes a force of dorsiflexion, ulnar
deviation, and intercarpal supination. -
Clinical evaluation
![]() Figure 23.6. Types of scaphoid fractures. The scaphoid is susceptible to fractures at any level.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 4th ed., vol. 1. Philadelphia: Lippincott-Raven, 1996:826.)
Figure 23.6. Types of scaphoid fractures. The scaphoid is susceptible to fractures at any level.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 4th ed., vol. 1. Philadelphia: Lippincott-Raven, 1996:826.)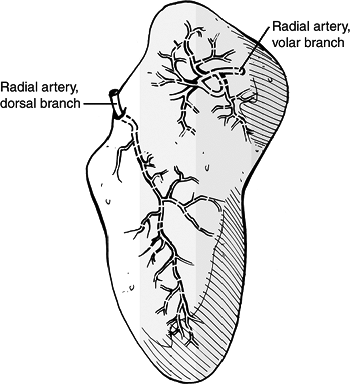 Figure 23.7. The vascular supply of the scaphoid is provided by two vascular pedicles.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 23.7. The vascular supply of the scaphoid is provided by two vascular pedicles.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Patients present with wrist pain and
swelling, with tenderness to palpation overlying the scaphoid in the
anatomic snuffbox. Provocative tests include:-
The scaphoid lift test: reproduction of pain with dorsal-volar shifting of the scaphoid.
-
The Watson test: painful dorsal scaphoid
displacement as the wrist is moved from ulnar to radial deviation with
compression of the tuberosity.
-
-
Differential diagnoses
-
Scapholunate instability
-
Lunate dislocation
-
Flexor carpus radialis tendon rupture
-
Radial styloid fracture
-
Trapezium fracture
-
De Quervain disease
-
Carpometacarpal (basal) joint arthrosis
-
-
Radiographic evaluation
-
This includes a PA view with the hand
clenched in a fist to extend the scaphoid, a lateral, a radial oblique
(supinated AP) and an ulnar oblique view. -
Initial films are nondiagnostic in up to 25% of cases.
-
If the clinical examination suggests
fracture but radiographs are not diagnostic, a trial of immobilization
with follow-up radiographs 1 to 2 weeks after injury may demonstrate
the fracture. -
Technetium bone scan, MRI, CT, and ultrasound evaluation may be used to diagnose occult scaphoid fractures.
P.245 -
-
Classification
-
Based on fracture pattern (Russe)
-
Horizontal oblique
-
Transverse
-
Vertical oblique
-
-
Based on displacement
-
Stable: nondisplaced fractures with no step-off in any plane
-
Unstable: displacement with 1 mm or more
step-off scapholunate angulation >60 degrees or radiolunate
angulation >15 degrees
-
-
Based on location
-
Tuberosity: 17% to 20%
-
Distal pole: 10% to 12%
-
Waist: 66% to 70%
-
Horizontal oblique: 13% to 14%
-
Vertical oblique: 8% to 9%
-
Transverse: 45% to 48%
-
-
Proximal pole: 5% to 7%
-
-
-
Indications for nonoperative treatment
-
Nondisplaced distal third fracture
-
Tuberosity fractures
-
-
Nonoperative treatment
-
Long arm thumb spica cast for 6 weeks
-
Immobilization in slight flexion and slight radial deviation
-
Replacement with short arm thumb spica cast at 6 weeks until united
-
Expected time to union:
-
Distal third: 6 to 8 weeks
-
Middle third: 8 to 12 weeks
-
Proximal third: 12 to 24 weeks
-
-
-
Management of suspected scaphoid fractures
-
In patients with an injury and positive
examination findings but normal x-rays, immobilization for 1 to 2 weeks
(thumb spica) is indicated. -
Repeat x-rays if the patient is still symptomatic.
-
If pain is still present but x-rays continue to be normal, consider MRI (or bone scan).
-
If an acute diagnosis is necessary, consider MRI or CT immediately.
-
-
Healing rates with nonoperative treatment depends on fracture location:
Tuberosity and distal third 100% Waist 80% to 90% Proximal pole
Proximal fractures are prone to nonunion and osteonecrosis60% to 70% -
Operative treatment
-
Indications for surgery
-
Surgical techniques
-
Most involve the insertion of screws.
-
Controversy exists about open versus percutaneous techniques.
-
Open techniques are needed for nonunions and fractures with unacceptable displacement.
-
Closed techniques are appropriate for acute fractures with minimal displacement.
-
-
The volar approach between the flexor
carpi radialis and the radial artery provides good exposure for open
reduction and internal fixation and repair of the radioscapholunate
ligament. The volar approach is the least damaging to the vascular
supply of the vulnerable proximal pole. -
Postoperative immobilization consists of a long arm thumb spica cast for 6 weeks.
-
-
Complications
-
Delayed union, nonunion, and malunion:
These are reported to occur with greater frequency when a short arm
cast is used as compared with a long arm cast, as well as with proximal
scaphoid fractures. They may necessitate operative fixation with bone
grafting to achieve union. -
Osteonecrosis: This occurs especially with fractures of the proximal pole, owing to the tenuous vascular supply.
-
-
The lunate is the fourth most fractured carpal bone after the scaphoid, triquetrum, and trapezium.
-
Fractures of the lunate are often
unrecognized until they progress to osteonecrosis, at which time they
are diagnosed as Kienboeck disease. -
The lunate has been referred to as the
“carpal keystone,” because it rests in the well-protected concavity of
the lunate fossa of the distal radius, anchored by interosseous
ligaments to the scaphoid and triquetrum, and distally is congruent
with the convex head of the capitate. -
Its vascular supply is derived from the
proximal carpal arcade dorsally and volarly, with three variable
intralunate anastomoses. -
The mechanism of injury is typically a
fall onto an outstretched hand with the wrist in hyperextension, or a
strenuous push with the wrist in extension. -
Clinical evaluation reveals tenderness to
palpation on the volar wrist overlying the distal radius and lunate,
with painful range of motion. -
Radiographic evaluation: PA and lateral
views of the wrist are often inadequate to establish the diagnosis of
lunate fracture because osseous details are frequently obscured by
overlapping densities. -
Classification: Acute fractures of the lunate can be classified into five groups:
-
Frontal fractures of the palmar pole with involvement of the palmar nutrient arteries
-
Osteochondral fractures of the proximal articular surface without substantial damage to the nutrient vessels
-
Frontal fractures of the dorsal pole
-
Transverse fractures of the body
-
Transarticular frontal fractures of the body of the lunate
-
-
Treatment
-
Nondisplaced fractures should be treated
in a short or long arm cast or splint with follow-up at close intervals
to evaluate progression of healing. -
Displaced or angulated fractures should
be treated surgically to allow adequate apposition for formation of
vascular anastomoses.
-
-
Complications
-
Osteonecrosis: Established Kienboeck
disease represents the most devastating complication of lunate
fractures, with advanced collapse and radiocarpal degeneration. This
may require further operative intervention for pain relief, including
radial shortening, radial wedge osteotomy, ulnar lengthening, or
salvage procedures such as proximal row carpectomy, wrist denervation,
or arthrodesis.
-
-
The triquetrum is the carpal bone that is most commonly fractured after the scaphoid.
-
Most fractures of the triquetrum are avulsion injuries that may be associated with ligament damage.
-
Most commonly, injury occurs with the
wrist in extension and ulnar deviation, resulting in an impingement
shear fracture by the ulnar styloid against the dorsal triquetrum. -
Clinical evaluation reveals tenderness to
palpation on the dorsoulnar aspect of the wrist as well as painful
range of wrist motion. -
Radiographic evaluation
-
Transverse fractures of the body can generally be identified on the PA view.
-
Dorsal triquetral fractures are not
easily appreciated on AP and lateral views of the wrist owing to
superimposition of the lunate. An oblique, pronated lateral view may
help to visualize the dorsal triquetrum.
-
-
Treatment
-
Nondisplaced fractures of the body or
dorsal chip fractures may be treated in a short arm cast or ulnar
gutter splint for 6 weeks. -
Displaced fractures may be amenable to open reduction and internal fixation.
-
-
Fractures of the pisiform are rare.
-
The mechanism of injury is either a
direct blow to the volar aspect of the wrist or a fall onto an
outstretched, dorsiflexed hand. -
Clinical evaluation demonstrates
tenderness on the volar ulnar aspect of the ulnar wrist with painful
passive extension of the wrist as the flexor carpi ulnaris is placed
under tension. -
Radiographic evaluation: Pisiform
fractures are not well visualized on standard views of the wrist;
special views include a lateral view of the wrist with forearm
supination of 20 to 45 degrees or a carpal tunnel view (20-degree
supination oblique view demonstrating an oblique projection of the
wrist in radial deviation and semisupination). -
Treatment of nondisplaced or minimally
displaced fractures consists of an ulnar gutter splint or short arm
cast for 6 weeks. Displaced fractures may require fragment excision,
either early, in the case of a severely displaced fragment, or late, in
the case of a pisiform fracture that has resulted in painful nonunion.
-
Fractures of the trapezium comprise approximately 3% to 5% of all carpal bone fractures.
-
About 60% of the reported cases have an unsatisfactory outcome secondary to degenerative changes.
-
Most are ridge avulsion fractures or vertical fractures of the body.
-
The mechanism of injury is axial loading
of the adducted thumb, driving the base of the first metacarpal onto
the articular surface of the trapezium.-
Avulsion fractures may occur with forceful deviation, traction, or rotation of the thumb.
-
Direct trauma to the palmar arch may result in avulsion of the trapezial ridge by the transverse carpal ligament.
-
-
Clinical evaluation reveals tenderness to
palpation of the radial wrist, accompanied by painful range of motion
at the first carpometacarpal joint. -
Radiographic evaluation: Fractures are usually identifiable on standard PA and lateral views.
-
Superimposition of the first metacarpal
base may be eliminated by obtaining a Robert view, or a true PA view of
the first carpometacarpal joint and trapezium, taken with the hand in
maximum pronation. -
A carpal tunnel view may be necessary for adequate visualization of dorsal ridge fractures.
-
-
Treatment
-
Nondisplaced fractures are generally
amenable to thumb spica splinting or casting to immobilize the first
carpometacarpal joint for 6 weeks. -
Indications for open reduction and
internal fixation include articular involvement of the carpometacarpal
articulation, comminuted fractures, and displaced fractures. -
Comminuted fractures may require supplemental bone grafting.
-
-
Complications
-
Posttraumatic osteoarthritis may result
in decreased or painful range of motion at the first carpometacarpal
joint. Irreparable joint damage may necessitate fusion or excisional
arthroplasty.
-
-
Because of the shape and position of the
trapezoid, fractures are rare. An axial load transmitted through the
second metacarpal may lead to dislocation, more often dorsal, with
associated capsular ligament disruption. -
Direct trauma from blast or crush
injuries may cause trapezoid fracture, although this is often in
conjunction with other injuries. -
Clinical evaluation demonstrates
tenderness proximal to the base of the second metacarpal with a
variable dorsal prominence representing a dislocated trapezoid. Range
of motion of the second carpometacarpal joint is painful and limited. -
Radiographic evaluation: fractures can be
identified on the PA radiograph based on a loss of the normal
relationship between the second metacarpal base and the trapezoid.
Comparison with the contralateral, uninjured wrist may aid in the
diagnosis. The trapezoid, or fracture fragments, may be superimposed
over the trapezium or capitate, and the second metacarpal may be
proximally displaced.-
Oblique views or CT may aid in the diagnosis if osseous details are obscured by overlap.
-
-
Treatment
-
Nondisplaced fractures may be treated with a splint or short arm cast for 6 weeks.
-
Indications for open reduction and
internal fixation include displaced fractures, especially those
involving the carpometacarpal articulation. These may be addressed with
open reduction and internal fixation with Kirschner wires with
attention to restoration of articular congruity.
-
-
Complications
-
Posttraumatic osteoarthritis may result at the second carpometacarpal articulation if joint congruity is not restored.
-
-
This is uncommon as an isolated injury owing to its relatively protected position.
-
A fracture of the capitate is more
commonly associated with greater arc injury pattern (transscaphoid,
transcapitate perilunate fracture-dislocation). A variation of this is
the “naviculocapitate syndrome,” in which the capitate and scaphoid are
fractured without associated dislocation. -
The mechanism of injury is typically
direct trauma or a crushing force that results in associated carpal or
metacarpal fractures. -
Clinical evaluation reveals point
tenderness as well as variable painful dorsiflexion of the wrist as the
capitate impinges on the dorsal rim of the radius. -
Fractures of the capitate can usually be
identified on standard scaphoid views, although motion studies are
recommended to look for displacement. -
Diagnosis may require an MRI scan.
-
Treatment: Capitate fractures require
reduction to diminish the risk of osteonecrosis. If closed reduction is
unattainable, open reduction and internal fixation are indicated,
usually with Kirschner wires or lag screws, to restore normal anatomy. -
Complications
-
Midcarpal arthritis: This is caused by capitate collapse as a result of displacement of the proximal pole.
-
Osteonecrosis: This is rare but results
in functional impairment; it emphasizes need for accurate diagnosis and
stable reduction.
-
-
Hamate fractures are quite rare.
-
The hamate may be fractured through its
distal articular surface, through other articular surfaces, or through
its hamulus, or hook. -
A distal articular fracture accompanied
by fifth metacarpal subluxation may occur when axial force is
transmitted down the shaft of the metacarpal, such as with a fist
strike or a fall. -
Fractures of the body of the hamate generally occur with direct trauma or crush injuries to the hand.
-
Fracture of the hook of the hamate is a
frequent athletic injury sustained when the palm of the hand is struck
by an object (e.g., baseball bat, golf club, hockey stick), and it
generally occurs at the base of the hook, although avulsion fractures
of the tip may occur. -
Clinical evaluation: Patients typically
present with pain and tenderness over the hamate. Ulnar and median
neuropathy can also be seen, as well as rare injuries to the ulnar
artery. -
Radiographic evaluation: The diagnosis of
hamate fracture can usually be made on the basis of the PA view of the
wrist. Fracture of the hamate is best visualized on the carpal tunnel
or a 20-degree supination oblique view (oblique projection of the wrist
in radial deviation and semisupination). CT and bone scan are sometimes
necessary to visualize the fracture. A hamate fracture should not be
confused with an os hamulus proprium, which represents an ossification
center that has failed to fuse. -
Classification of hamate fractures is descriptive.
-
Treatment
-
Nondisplaced hamate fractures may be treated with immobilization in a short arm splint or cast for 6 weeks.
-
Displaced fractures of the body may be
amenable to Kirschner wire or screw fixation. Fractures of the hook of
the hamate may be treated with excision of the fragment for displaced
fragments or in cases of symptomatic nonunion.
-
-
Complications
-
Symptomatic nonunion: This may be treated with excision of the nonunited fragment.
-
Ulnar or median neuropathy: This is
related to the proximity of the hamate to these nerves and may require
surgical exploration and release. -
Ruptures of the flexor tendons to the small finger: They result from attritional wear at the fracture site.
-
-
The lunate, which is normally securely
attached to the distal radius by ligamentous attachments, is commonly
referred to as the “carpal keystone.” -
Greater arc injury: This passes through
the scaphoid, capitate, and triquetrum and often results in
transscaphoid or transscaphoid transcapitate perilunate
fracture-dislocations (Fig. 23.8). -
Lesser arc injury: This follows a curved
path through the radial styloid, midcarpal joint, and lunatotriquetral
space and results in perilunate and lunate dislocations. -
The most common injury is transscaphoid perilunate fracture-dislocation (de Quervain injury).
-
Mechanism of injury
-
Perilunate injuries: Load is applied to the thenar eminence, forcing the wrist into extension.
-
Injury progresses through several stages (Mayfield progression):
-
It usually begins radially through the body of scaphoid (fracture) or thru scapholunate interval (dissociation).
-
The scaphoid bridges the proximal and distal carpal rows.
-
With dislocation between these rows, the scaphoid must either rotate or fracture.
-
Force is transmitted ulnarly through the space of Poirier (between the lunate and capitate).
-
Finally, force transmission disrupts the lunotriquetral articulation (Fig. 23.9).
-
-
-
Clinical evaluation: Scapholunate or perilunate injuries typically cause tenderness just distal to Lister tubercle. Swelling is
P.252
generalized about the wrist with variable dorsal prominence of the entire carpus in cases of frank perilunate dislocation.![]() Figure
Figure
23.8. Vulnerable zones of the carpus. (A) A lesser arch injury follows
a curved path through the radial styloid, midcarpal joint, and the
lunatotriquetral space. A greater arc injury passes through the
scaphoid, capitate, and triquetrum. (B) Lesser and greater arc injuries
can be considered as three stages of the perilunate fracture or
ligament instabilities.(From Johnson RP. The acutely injured wrist and its residuals. Clin Orthop 1980;149:33–44.)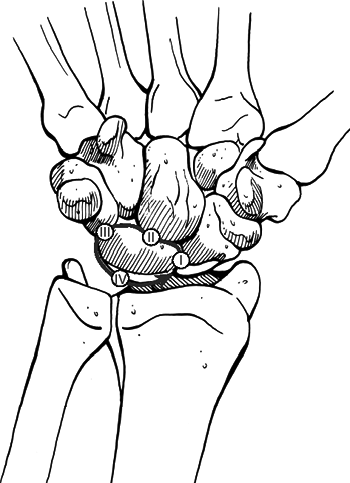 Figure
Figure
23.9. Mayfield stages of progressive perilunate instability. Stage I
results in scapholunate instability. Stages II to IV result in
progressively worse perilunate instability.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Radiographic evaluation: Diagnosis can
often be made without accompanying radiographs, but PA and lateral
views should be obtained to confirm the diagnosis and rule out
associated injuries. CT, MRI, and arthrography are generally
unnecessary but may be useful in further defining injury pattern.-
PA view: The dislocated lunate appears to be wedge-shaped, with an elongated volar lip.
-
Loss of normal carpal greater and lesser “arcs” and abnormal widening of the scapholunate interval are noted.
-
Look for associated fractures, such as “transscaphoid” injuries.
-
Lateral view: The “spilled teacup sign” occurs with volar tilt of the lunate.
-
A clenched-fist PA view obtained after
closed reduction of the midcarpal joint is useful for checking residual
scapholunate or lunotriquetral dissociation as well as fractures.
-
-
Classification: A sequence of progressive perilunate instability is seen as the injury spreads:
-
From the scapholunate joint (radioscapholunate ligament) → midcarpal joint (radioscaphocarpal ligament) →
P.253
lunotriquetral joint (distal limb of radiolunotriquetral ligament) →
dorsal radiolunotriquetral ligament → volar dislocation of the lunate.Stage I: Disruption of the scapholunate joint: The radioscapholunate and interosseous scapholunate ligaments are disrupted. Stage II: Disruption of the midcarpal (capitolunate) joint: The radioscaphocapitate ligament is disrupted. Stage III: Disruption of the lunotriquetral joint: The distal limb of the radiolunotriquetral ligament is disrupted. Stage IV: Disruption of the radiolunate
joint: The dorsal radiolunotriquetral ligament is disrupted, ultimately
causing volar dislocation of the lunate.
-
-
Treatment
-
Closed reduction should be performed with adequate sedation.
-
Technique of closed reduction
-
Longitudinal traction is applied for 5 to 10 minutes.
-
For dorsal perilunate injuries, volar pressure is applied to the carpus while counterpressure is applied to the lunate.
-
Palmar flexion then reduces the capitate into the concavity of the lunate.
-
-
Early surgical reconstruction is
performed if swelling allows. Immediate surgery is needed if there are
signs of median nerve compromise. -
Closed reduction and pinning
-
The lunate is reduced and pinned to the radius in neutral alignment.
-
The triquetrum or scaphoid can then be pinned to the lunate.
-
-
Transscaphoid perilunate dislocation
-
This requires reduction and stabilization of the fractured scaphoid.
-
Most of these injuries are best treated by open volar and dorsal reduction and repair of injured structures.
-
Open repair may be supplemented by pin fixation.
-
-
Delayed reconstruction is indicated if early intervention is not feasible.
-
-
Complications
-
Median neuropathy: This may result from carpal tunnel compression, necessitating surgical release.
-
Posttraumatic arthritis: This may result from the initial injury or secondarily from small, retained osseous fragments.
-
Chronic perilunate injury: This may
result from untreated or inadequately treated dislocation or
fracture-dislocation resulting in chronic pain, instability, and wrist
deformity, often associated with tendon rupture or increasing nerve
symptoms. Repair may be possible, but a salvage procedure, such as
proximal row carpectomy or radiocarpal fusion, may be necessary.
-
-
Carpal dislocations represent a continuum
of perilunate dislocations, with frank lunate dislocation representing
the final stage. All such injuries reflect significant ligamentous
injury. -
Associated fractures are common and may
represent avulsion injuries (e.g., volar or dorsal intercalated
segmental instability with associated radial rim fracture). -
Mechanism of injury: A fall onto an
outstretched hand represents the most common cause, although direct
force can cause traumatic carpal dislocations as well. -
Clinical evaluation: Patients typically
present with painful, limited wrist range of motion. Median neuropathy
may be present. Specific tests for carpal instability include the
following:-
Midcarpal stress test: Dorsal-palmar
stressing of the midcarpal joint results in a pathologic clunk
representing subluxation of the lunate. -
Dynamic test for midcarpal instability:
Wrist extension with radioulnar deviation produces a “catchup” clunk as
the proximal row snaps from flexion to extension.
-
-
Radiographic evaluation: Most dislocations may be diagnosed on PA and lateral views of the wrist.
-
CT and MRI may aid in further injury definition.
-
-
Treatment of carpal dislocations consists
of closed reduction of the midcarpal joint, which is often accomplished
with traction, combined with direct manual pressure over the capitate
and lunate.-
Irreducible dislocations or unstable
injuries should be treated with open reduction and internal fixation
utilizing a combined dorsal and volar approach. Dorsally, the osseous
anatomy is restored and stabilized using Kirschner wire fixation.
Volarly, the soft tissues are repaired.
-
-
Complications
-
Posttraumatic arthritis: This may result
from unrecognized associated fractures or malreduction, with subsequent
functional limitation and pain. -
Recurrent instability: This may result
from inadequate repair of ligamentous structures on the volar aspect or
insufficient fixation dorsally.
-
-
This is the ligamentous analog of a
scaphoid fracture; it represents the most common and significant
ligamentous disruption of the wrist. -
The underlying pathologic process is a disruption of the radioscapholunate and the interosseous scapholunate ligaments.
-
The mechanism of injury is loading of the extended carpus in ulnar deviation.
-
Clinical findings include ecchymosis and
tenderness on the volar wrist. The proximal pole of the scaphoid is
prominent dorsally. Signs of scapholunate dissociation include a
vigorous grasp that induces pain, decreasing repetitive grip strength,
a positive Watson test (see earlier, under scaphoid fractures), and painful flexion-extension or ulnar-radial deviation of the wrist. -
Radiographic evaluation: PA, lateral,
clenched fist PA, and radial and ulnar deviation views are obtained.
Classic signs of scapholunate dissociation on the PA view include:-
The “Terry Thomas sign”: widening of the scapholunate space (normal, <3 mm).
-
The “cortical ring sign” caused by the abnormally flexed scaphoid.
-
A scapholunate angle of >70 degrees visualized on the lateral view.
-
-
Treatment
-
The scaphoid can often be reduced with an
audible and palpable click, followed by immobilization for 8 weeks in a
long arm thumb spica cast. Good results with anatomic reduction are
reported. -
Arthroscopically assisted reduction with percutaneous pin fixation has been described with good results.
-
An inability to obtain or maintain
reduction is an indication for open reduction and internal fixation.
This may be accomplished by a combined dorsal and volar approach with
reduction and stabilization of the scapholunate joint dorsally using
Kirschner wires and repair of the ligaments volarly.
-
-
Complications
-
Recurrent instability: Failure of closed
or open reduction and internal fixation with ligament repair may
necessitate ligament augmentation, intercarpal fusion, proximal row
carpectomy, or wrist fusion. It may progress to a DISI pattern or a
scaphoid-lunate advanced collapse of the wrist.
-
-
These injuries involve disruption of the
distal limb of the volar radiolunotriquetral ligament either as a stage
III lesser arc injury of perilunate instability or as a result of a
force causing excessive radial deviation and intercarpal pronation. The
lunotriquetral interosseous and dorsal radiolunotriquetral ligaments
are also injured. -
Clinical findings include swelling over
the peritriquetral area and tenderness dorsally, typically one
fingerbreadth distal to the ulnar head.-
Ballottement test (shear or shuck test):
Dorsal-volar displacement of the triquetrum on the lunate results in
increased excursion as compared with the normal, contralateral side, as
well as painful crepitus.
-
-
Radiographic evaluation: PA radiographs
of the hand rarely reveal frank gapping of the lunotriquetral space,
but a break in the normal smooth contour of the proximal carpal row can
be appreciated.-
Radial deviation view: This may
demonstrate the triquetrum to be dorsiflexed with the intact
scapholunate complex palmar-flexed. A lateral projection may reveal a
volar intercalated segmental instability pattern.
-
-
Treatment
-
Acute lunotriquetral dissociation with minimal deformity may be treated with a short arm cast or splint for 6 to 8 weeks.
-
Closed reduction with pinning of the lunate to the triquetrum may be necessary to maintain reduction.
-
Angular deformity or unacceptable
reduction from nonoperative treatment may necessitate open reduction
and internal fixation utilizing a combined dorsal and volar approach,
with pinning of the triquetrum to the lunate and ligamentous repair.
P.256 -
-
Complications
-
Recurrent instability may necessitate
ligament reconstruction with capsular augmentation. If recurrent
instability persists, lunotriquetral fusion may be necessary, with
possible concomitant ulnar shortening to tension the volar ulnocarpal
ligaments.
-
-
Avulsion or rupture of the TFCC from the ulnar styloid results in a loss of “sling” support for the ulnar wrist.
-
The lunate and triquetrum “fall away”
relative to the distal ulna and assume a semisupinated and palmar
flexed attitude, with the distal ulna subluxed dorsally. -
Clinical evaluation reveals dorsal prominence of the distal ulna and volar displacement of the ulnar carpus.
-
Radiographic evaluation: The PA view may
reveal avulsion of the ulnar styloid. Dorsal displacement of the distal
ulna on true lateral views suggests disruption of the TFCC in the
absence of an ulnar styloid avulsion fracture.-
MRI may demonstrate a tear of the TFCC and may additionally provide evidence of chondral lesions and effusion.
-
-
Treatment: Operative repair of the TFCC may be achieved via a dorsal approach between the fifth and sixth extensor compartments.
-
Open reduction and internal fixation of large displaced ulnar styloid fragments are necessary.
-
-
Complications
-
Recurrent instability: This may occur
with or without previous operative intervention and may result in pain
and functional debilitation that may be progressive. -
Ulnar neuropathy: Transient sensory
symptoms may result from irritation of the ulnar nerve in Guyon canal
or its dorsal sensory branch. Permanent damage is rare, but persistence
of symptoms beyond 12 weeks may necessitate exploration.
-