General Spine
-
There are approximately 11,000 new spinal cord injuries requiring treatment each year.
-
Delayed diagnosis of vertebral injury is
frequently associated with loss of consciousness secondary to multiple
trauma or intoxication with alcohol or drugs. -
The ratio of male to female patients sustaining vertebral fractures is 4:1.
-
In older patients (>75 years of age), 60% of vertebral fractures are caused by a fall.
-
For patients with a spinal cord injury, the overall mortality during the initial hospitalization is 17%.
-
Approximately 2% to 6% of trauma patients sustain a cervical spine fracture.
-
The spinal cord occupies approximately
35% of the canal at the level of the atlas (C1) and 50% of the canal in
the lower cervical spine and thoracolumbar segments. The remainder of
the canal is filled with epidural fat, cerebrospinal fluid, and dura
mater. -
The conus medullaris
represents the caudal termination of the spinal cord. It contains the
sacral and coccygeal myelomeres and lies dorsal to the L1 body and L1-2
intervertebral disc. -
The cauda equina
(literally translated means horse’s tail) represents the motor and
sensory roots of the lumbosacral myelomeres. These roots are less
likely to be injured because they have more room in the canal and are
not tethered to the same degree as the spinal cord. Furthermore, the
motor nerve roots are composed of lower motor neurons, which are more
resilient to injury than are the upper motor neurons of the brain and
spinal cord. -
A reflex arc
is a simple sensorimotor pathway that can function without using either
ascending or descending white matter, long-tract axons. A spinal cord
level that is anatomically and physiologically intact may demonstrate a
functional reflex arc at that level despite dysfunction of the spinal
cord cephalad to that level.
classification systems based on presumed mechanism of injury is that
the same mechanism of injury can result in morphologically different
patterns of injury; similar morphologic patterns of injury can also be
the result of different injury mechanisms, and the patterns of head
deflection do not predict the spinal injury patterns. Several
characteristics of the injury force that determine the extent of neural
tissue damage have been identified. These include the rate of force
application, the degree of neural tissue compression, and the duration
of neural tissue compression.
-
Contusion: This sudden, brief compression
by a displaced structure affects central tissues primarily and accounts
for the majority of primary injuries and is thus responsible for the
majority of neurologic deficits. Contusion injuries are potentially
reversible, although irreversible neuronal death occurs along with
vascular injury with intramedullary hemorrhage. -
Compression: Injury results from
decreased size of the spinal canal; it may occur with translation or
angulation of the spinal column, as with burst injuries, or with
epidural hematomas. Injury occurs by:-
Mechanical deformation interrupting axonal flow.
-
Interruption of spinal vascularity resulting in ischemia of neurologic structures.
-
-
Stretch: Injury results in longitudinal
traction, as in the case of a flexion-distraction injury. Injury occurs
as a result of capillary and axonal collapse secondary to tensile
distortion. -
Laceration: This is caused by penetrating foreign bodies, missile fragments, or displaced bone.
damage resulting from the biologic response initiated by the physical
tissue disruption. Local tissue elements undergo structural and
chemical changes. These changes, in turn, elicit systemic responses.
Changes in local blood flow, tissue edema, metabolite concentrations,
and concentrations of chemical mediators lead to propagation of
interdependent reactions. This pathophysiologic response, referred to
as secondary injury, can propagate tissue destruction and functional
loss.
-
Assess the patient: airway, breathing,
circulation, disability, and exposure (ABCDE). Avoid the
head-tilt–chin-lift maneuver, hypoxia, and hypotension. -
Initiate resuscitation: address life-threatening injuries.
-
Evaluate the patient’s level of consciousness.
-
Evaluate injuries to head, chest,
abdomen, pelvis, and spine. The spine must be protected. Logroll the
patient to assess the spinal column, examine the skin for bruising and
abrasions, and palpate spinous processes for tenderness and diastasis.
Evaluate for noncontiguous spinal injuries; many authors have
emphasized the need to evaluate the spinal column for injuries to more
than one level.-
Calenoff found a 5% incidence of multiple
noncontiguous vertebral injuries. Half of the secondary lesions were
initially missed, with a mean delay of 53 days in diagnosis; 40% of
secondary lesions occurred above the primary lesion, 60% below. The
region T2-7 accounted for 47% of primary lesions in this population,
but only 16% of reported spinal injuries in general. -
Injuries of the vertebral column tend to
cluster at the junctional areas: the craniocervical junction (occiput
to C2), the cervicothoracic junction (C7-T1), and the thoracolumbar
junction (T11-L2). These areas represent regions of stress
concentration, where a rigid segment of the spine meets a more flexible
segment. Also contributing to stress concentration in these regions are
changes at these levels in the movement constraints of vertebrae. -
Among these injuries, the most serious and most frequently missed is craniocervical dissociation.
-
In trauma patients, thoracic and lumbar
fractures are concentrated at the thoracolumbar junction, with 60% of
thoracic and lumbar fractures occurring between T11 and L2 vertebral
levels. -
Three common patterns of noncontiguous spinal injuries are as follows:
Pattern A: Primary injury at C5-7, with secondary injuries at T12 or in the lumbar spine Pattern B: Primary injury at T2-4 with secondary injuries in the cervical spine Pattern C: Primary injury at Tl2-L2 with a secondary injury at L4-5
P.67 -
-
Assess injuries to the extremities.
-
Complete the neurologic examination to evaluate reflexes, sensation (touch, pain), and motor function (Fig. 8.1 and Tables 8.1 and 8.2).Table 8.1. Elements of ASIA neurologic assessment
Examination Method Testing Locations Grading Required elements of ASIA neurologic impairment assessment Pinprick (sharp/dull) Discriminate sharp and dull ends of a standard safety pin 28 dermatomes specified by designated bony prominences 0, 1, 2, NT Light touch Identify contact with a cotton swab tip Deep anal sensation Digital rectal examination Pressure on rectal wall 0, 1 (absent, present) Key muscles Patient is in supine position 10 key muscles 0, 1, 2, 3, 4, 5, 5*, NT Optional element of ASIA neurologic impairment assessment Joint movement appreciation (proprioception) Support proximal portion and move distal portion by gripping medial and lateral edges Wrist
Thumb interphalangeal joint
Small finger proximal interphalangeal joint
Knee
Ankle
Great toe interphalangeal joint0, 1, 2, NT Deep pressure sensation Apply pressure with thumb or index finger Wrist radial styloid
Thumb nailbed
Small finger nailbed
Ankle medial malleolus
Great toe nailbed
Small toe nailbed0, 1 (absent, present) Diaphragm Observe under fluoroscopy Movement over two or more interspaces 0, 1 (absent, present) Deltoids Shoulder abduction C5–6±4 0, 1, 2, 3, 4, 5, 5*, NT Abdominal muscles Observe movement of umbilicus (Beevor’s sign: umbilicus moves up in T9–T11 lesions) T6–T12 0, 1, 2, 3, 4, 5, 5*, NT Hip adductors Palpate adductor longus L2–3 0, 1, 2, 3, 4, 5, 5*, NT Hamstrings Knee flexion Plurisegmental 0, 1, 2, 3, 4, 5, 5*, NT Motor Grades Score Description Sensory Grades Score Description 0 No visible or palpable contraction 0 Absent → unable to distinguish 1 Any visible or palpable contraction 1 Impaired → able to distinguish but intensity is abnormal 2 Able to move full range of motion of joint with gravity eliminated 2 Normal 3 Able to move full range of motion of joint against gravity NT Not testable 4 Able to move full range of motion of joint against some resistance 5* Able to exert sufficient resistance to be normal according to examiner’s judgement 5 Normal according to examiner’s judgement if inhibiting factors were not present NT Not testable ASIA, American Spinal Injury Association.
From ASIA. Standards for Neurological Classification of Spinal Injury. Chicago: American Spinal Injury Association; 1996, with permission.Table 8.2. Definitions of terms describing spinal cord injuryImpairment Loss of motor and sensory function Disability Loss in daily life functioning Tetraplegia Loss of motor and/or sensory function in the cervical segments Paraplegia Loss of motor and/or sensory function in the thoracic, lumbar, or sacral segments Dermatome Area of skin innervated by sensory axons within each segmental nerve Myotome Collection of muscle fibers by the motor axons within each segmental nerve Neurologic level The most caudal segment with normal sensory and motor function on both sides Sensory level The most caudal segment with normal sensory function on both sides Motor level The most caudal segment with normal motor function on both sides Skeletal level Radiographic level of greatest vertebral damage Sensory score Numeric summary value of sensory impairment Motor score Numeric summary value of motor impairment Incomplete injury Partial preservation of
sensory and/or motor function below the neurologic level AND sensory
and/or motor preservation of the lowest sacral segmentComplete injury Absence of sensory and motor function in the lowest sacral segment Zone of partial preservation Dermatomes and myotomes caudal to the neurologic level that remain partially innervated Only used in complete injuries From ASIA Standards for Neurological Classification of Spinal Injury. Chicago: American Spinal Injury Association: 1996, with permission. -
Perform a rectal examination to test for perianal sensation, resting tone, and the bulbocavernosus reflex.
-
Spinal shock is defined as spinal cord
dysfunction based on physiologic rather than structural disruption.
Resolution of spinal shock may be recognized when reflex arcs caudal to
the level of injury begin to function again, usually within 24 hours of
injury. -
Spinal shock should be distinguished from
neurogenic shock, which refers to hypotension associated with loss of
peripheral vascular resistance in spinal cord injury.
-
Neurogenic shock refers to flaccid
paralysis, areflexia, and lack of sensation to physiologic spinal cord
“shutdown” in response to injury. -
It is most common in cervical and upper thoracic injuries.
-
It almost always resolves within 24 to 48 hours.
-
The bulbocavernosus reflex (S3-4) is the first to return. (Table 8.4).Table 8.4. Spinal cord and conus medullaris reflexes
Reflex Location of Lesion Stimulus Normal Response Abnormal Response Babinski Upper motor neuron Stroking the plantar aspect of foot proximal lateral to distal medial Toes plantarflex Toes extend and splay Oppenheim Upper motor neuron Rubbing the tibial crest proximal to distal Toes plantarflex Toes extend and splay Cremasteric T12–L1 Stroking the medial thigh proximal to distal Upward motion of the scrotum No motion of the scrotum Anal wink S2–S4 Stroking skin around anus Anal sphincter contracts No anal sphincter contraction Bulbocavernosus S3–S4 Squeezing the penis in males, applying pressure to clitoris in females, or tugging the bladder catheter in either Anal sphincter contracts No anal sphincter contraction From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006. -
It occurs secondary to sympathetic outflow disruption (T1-L2) with resultant unopposed vagal (parasympathetic) tone.
-
Initial tachycardia and hypertension
immediately after injury are followed by hypotension accompanied by
bradycardia and venous pooling.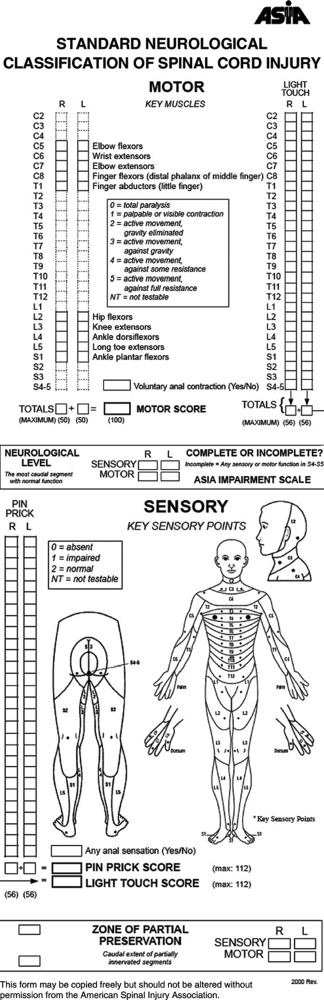 Figure 8.1. Neurologic examination recommended by the American Spinal Injury Association (ASIA).(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 8.1. Neurologic examination recommended by the American Spinal Injury Association (ASIA).(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Hypotension from neurogenic shock may be
differentiated from cardiogenic, septic, and hypovolemic shock by the
presence of associated bradycardia, as opposed to tachycardia. -
Treatment is based on administration of isotonic fluids, with careful assessment of fluid status (beware of overhydration).
-
Recognizing neurogenic shock as distinct
from hemorrhagic shock is critical for safe initial resuscitation of a
trauma patient. Treatment of neurogenic shock is pharmacologic
intervention to augment peripheral vascular tone. It may be essential
for effective resuscitation. Fluid overload from excessive fluid volume
administration, typical in treatment of hemorrhagic shock, can result
in pulmonary edema in the setting of neurogenic shock.
-
The absence of this reflex indicates spinal shock.
-
The return of the bulbocavernosus reflex, generally within 24 hours of the initial injury, hallmarks the end of spinal shock.
-
The presence of a complete lesion after
spinal shock has resolved portends a virtually nonexistent chance of
neurologic recovery. -
The bulbocavernosus reflex is not prognostic for lesions involving the conus medullaris or the cauda equina.
-
The lateral cervical spine radiograph is
routine in the standard evaluation of trauma patients. Patients
complaining of neck pain should undergo complete radiographic
evaluation of the cervical spine, including anteroposterior and
odontoid views. -
Lateral radiographic examination of the
entire spine is recommended in patients with spine fractures when
complete clinical assessment is impaired by neurologic injury or other
associated injuries. -
Computed tomography scans or tomograms
may be necessary for cervical spine clearance in patients with
questionable or inadequate plain radiographs or to assess
occipitocervical and cervicothoracic junction. -
Magnetic resonance imaging may aid in assessing spinal cord or root injury, as well as degree of canal compromise.
usually described by terms that refer to the severity and pattern of
neurologic dysfunction: complete spinal cord injury, incomplete injury,
and transient spinal cord dysfunction describe different grades of
severity of neurologic injury. Names for different types of spinal
cord
injury syndromes, such as anterior cord syndromes, central cord
syndrome, and Brown-Séquard syndrome, refer to patterns of neurologic
dysfunction observed during clinical evaluation.
-
No sensation or voluntary motor function
is noted caudal to the level of injury in the presence of an intact
bulbocavernosus reflex (indicating intact S3-4 and resolution of spinal
shock). -
Reflex returns below the level of the cord injury.
-
It is named by last spinal level of partial neurologic function.
-
One can expect up to one to two levels of additional root return, although the prognosis for recovery is extremely poor.
-
Some neurologic function persists caudal to the level of injury after the return of the bulbocavernosus reflex.
-
As a rule, the greater the function distal to the lesion and the faster the recovery, the better the prognosis.
-
Sacral sparing is represented by perianal
sensation, voluntary rectal motor function, and great toe flexor
activity; it indicates at least partial continuity of white matter long
tracts (corticospinal and spinothalamic) with implied continuity
between the cerebral cortex and lower sacral motor neurons. It
indicates incomplete cord injury, with the potential for a greater
return of cord function following resolution of spinal shock.
|
Table 8.5. Descriptions of incomplete cord injury patterns
|
||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||
-
This is a hemicord injury with
ipsilateral muscle paralysis, loss of proprioception and light touch
sensation, and contralateral hypesthesia to pain and temperature. -
The prognosis is good, with >90% of patients regaining bowel and bladder function and ambulatory capacity.
-
This is most common and is frequently associated with an extension injury to an osteoarthritic spine in a middle-aged person.
-
It presents with flaccid paralysis of the
upper extremities (more involved) and spastic paralysis of the lower
extremities (less involved), with the presence of sacral sparing. -
Radiographs frequently demonstrate no
fracture or dislocation, because the lesion is created by a pincer
effect between anterior osteophytes and posterior infolding of the
ligamentum flavum. -
The prognosis is fair, with 50% to 60% of
patients regaining motor and sensory function to the lower extremities,
although permanent central gray matter destruction results in poor hand
function.
-
This is common and involves motor and
pain/temperature loss (corticospinal and spinothalamic tracts) with
preserved light touch and proprioception (dorsal columns). -
The prognosis is good if recovery is
evident and progressive within 24 hours of injury. Absence of sacral
sensation to temperature or pinprick after 24 hours portends a poor
outcome, with functional recovery in 10% of patients, according to one
series.
-
This is rare and involves a loss of deep
pressure, deep pain, and proprioception with full voluntary power,
pain, and temperature sensation.
-
This is seen in T12-L1 injuries and
involves a loss of voluntary bowel and bladder control (S2-4
parasympathetic control) with preserved lumbar root function. -
It may be complete or incomplete; the bulbocavernosus reflex may be permanently lost.
-
It is uncommon as a pure lesion and more common with an associated lumbar root lesion (mixed conus-cauda lesion).
-
Isolated root lesions may occur at any level and may accompany spinal cord injury.
-
This may be partial or complete and results in radicular pain, sensory dysfunction, weakness, hyporeflexia, or areflexia.
-
This is caused by multilevel lumbosacral root compression within the lumbar spinal canal.
-
Clinical manifestations include saddle
anesthesia, bilateral radicular pain, numbness, weakness, hyporeflexia
or areflexia, and loss of voluntary bowel or bladder function.
| Grade A: | Absent motor and sensory function |
| Grade B: | Absent motor function, sensation present |
| Grade C: | Motor function present, but not useful (2 or 3/5), sensation present |
| Grade D: | Motor function present and useful (4/5), sensation present |
| Grade E: | Normal motor (5/5) and sensory function |
| Grade A: | Complete: No motor or sensory function is preserved in sacral segments S4-5. |
| Grade B: | Incomplete: Sensory but not motor function is preserved below the neurologic level and extends through the sacral segment S4-5. |
| Grade C: | Incomplete: Motor function is preserved below the neurologic level; most key muscles below the neurologic level have a muscle grade <3. |
| Grade D: | Incomplete: Motor function is preserved below the neurologic level; most key muscles below the neurologic level have a muscle grade >3. |
| Grade E: | Normal: Motor and sensory function is normal. |
level is the most caudal segment of the spinal cord with normal motor
and sensory function on both sides: right and left sensation, right and
left motor function. For functional scoring, ten key muscle segments
corresponding to innervation by C5, C6, C7, C8, T1, L2, L3, L4, L5, and
S1 are each given a functional score of 0 to 5 out of 5. For sensory
scoring, both right and left sides are graded for a total of 100
points. For the 28 sensory dermatomes on each side of the body, sensory
levels are scored on a 0- to 2-point scale, yielding a maximum possible
pinprick score of 112 points for a patient with normal sensation.
-
A rigid cervical collar is indicated
until the patient is cleared radiographically and clinically. A patient
with a depressed level of consciousness (e.g., from ethanol
intoxication) cannot be cleared clinically. -
A special backboard with a head cutout
must be used for children to accommodate their proportionally larger
head size and prominent occiput. -
The patient should be removed from the backboard (by logrolling) as soon as possible to minimize pressure sore formation.
-
Intravenous methylprednisolone:
-
May improve recovery of neurologic injury.
-
Is currently considered the “standard of
care” for spinal cord injury if it is administered within 8 hours of
injury; it improves motor recovery among patients with complete and
partial cord injuries. -
Has a loading dose of 30 mg/kg.
-
5.4 mg/kg/hour over the next 24 hours if started within 3 hours of spinal cord injury
-
5.4 mg/kg/hour over the next 48 hours if started within 8 hours of spinal cord injury
-
-
Has no benefit, similar to other to steroids, if started more than 8 hours after injury.
-
Is not indicated for pure root lesions.
-
-
Experimental pharmacologic agents include:P.79
-
Naloxone (opiate receptor antagonist).
-
Thyrotropin-releasing hormone.
-
GM1 gangliosides: a membrane
glycolipid that, when administered within 72 hours of injury, resulted
in a significant increase in motor scores. Administer 100 mg/day for up
to 32 days after injury. It is not recommended for simultaneous use
with methylprednisolone.
-
-
Gastrointestinal: Ileus, regurgitation
and aspiration, and hemorrhagic gastritis are common early
complications, occurring as early as the second day after injury.
Gastritis is thought to be the result of sympathetic outflow disruption
with subsequent unopposed vagal tone resulting in increased gastric
activity. Passage of a nasogastric tube and administration of histamine
(H2) receptor antagonists should be used as prophylaxis against these potential complications. -
Urologic: Urinary tract infections are
recurrent problems in the long-term management of paralyzed patients.
An indwelling urinary catheter should remain in the patient during the
acute, initial management only to monitor urinary output, which is
generally low with neurogenic shock because of venous pooling and a
low-flow state. Following this, sterile intermittent catheterization
should be undertaken to minimize potential infectious sequelae. -
Pulmonary: Acute quadriplegic patients
are able to inspire only using their diaphragm, because their abdominal
and intercostal muscles are paralyzed. Vital capacity ranges from 20%
to 25% of normal, and the patient is unable forcibly to expire, cough,
or clear pulmonary secretions. Management of fluid balance is essential
in the patient in neurogenic shock, because volume overload rapidly
results in pulmonary edema with resolution of shock. Positive pressure
or mechanical ventilation may be necessary for adequate pulmonary
function. Without aggressive pulmonary toilet, pooling of secretions,
atelectasis, and pneumonia are common and are associated with high
morbidity and mortality. -
Skin: Problems associated with pressure
ulceration are common in spinal cord–injured patients owing to
anesthesia of the skin. Turning the patient every 2 hours, careful
inspection and padding of bony prominences, and aggressive treatment of
developing decubitus ulcers are essential to prevent long-term sequelae
of pressure ulceration.
-
A cleared spine in a patient implies that
diligent spine evaluation is complete and the patient does not have a
spinal injury requiring treatment. -
The necessary elements for a complete spine evaluation are:
-
History to assess for high-risk events and high-risk factors.
-
Physical examination to check for physical signs of spinal injury or neurologic deficit.
-
Imaging studies based on an initial evaluation.
-
-
Patients with a diagnosed cervical spine
fracture have at least one of the following four characteristics:
midline neck tenderness, evidence of intoxication, abnormal level of
alertness, or several painful injuries elsewhere. -
Therefore, criteria for clinical clearance are:
-
No posterior midline tenderness.
-
Full pain-free active range of motion.
-
No focal neurologic deficit.
-
Normal level of alertness.
-
No evidence of intoxication.
-
No distracting injury.
-
-
Radiographs are not necessary for
patients who are alert, are not intoxicated, have an isolated blunt
trauma, and have no neck tenderness on physical examination. -
The process of clearing the thoracolumbar
spine is similar to that for clearing the cervical spine. Only
anteroposterior and lateral view radiographs are necessary. Patients
with clear mental status, no back pain, and no other major injuries do
not need radiographs of the entire spine to exclude a spinal fracture.
