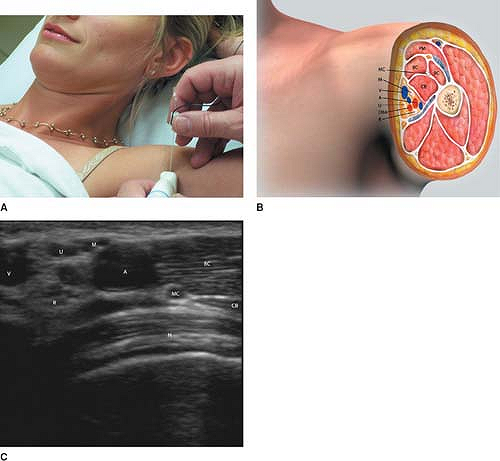
Ultrasound Guided Axillary Block
The biceps muscle lies anterosuperior to the neurovascular bundle,
while the coracobrachialis muscle is superior to the neurovascular
bundle, and the triceps muscle, inferior to neurovascular bundle. The
humerus lies deep to the neurovascular bundle. The brachial artery and
1 to 2 brachial veins are evident in the neurovascular bundle. The
radial, median, and ulnar nerves are found within the neurovascular
bundle (Fig. 36-1A, C).
Most commonly, the median nerve is anterior or cephaloanterior to the
artery. The radial nerve is most commonly posterior or posteroinferior
to the artery, while the ulnar nerve is most commonly found inferior or
anteroinferior to the artery. Proximal in the axilla, the
musculocutaneous nerve may be found cephaloposterior to the artery. In
more distal sites in the axilla, the musculocutaneous nerve is usually
found in the fascia between the biceps and coracobrachialis muscles 1
to 2 cm cephaloposterior to the artery. Cutaneous nerves of the arm or
forearm may also be visualized.
Place sterile skin prep solution on the field. Cover the transducer
with a sterile cover, and place sterile sonographic gel over the skin
in the field. A wheel of local anesthetic should be injected beneath
the skin along a 5 cm arc from medial to lateral to the brachial artery
pulsation (Fig. 36-1A).
This allows needle placement from either side of the artery, without
repeatedly injecting subcutaneously local anesthetic, as well as
providing anesthesia for the intercostobrachial nerve and the medial
brachial cutaneous nerve.
The
artery should be localized with the transducer, and the hyperechoic
nerves sought at its periphery. Initially, the block needle is inserted
in-plane, along the long axis of the transducer, from the superior side
of the artery (Fig. 36-1A).
In the posterocephalad region, the musculocutaneous nerve is sought.
The peripheral nerve stimulator may be left on throughout the
procedure, with a current level of 0.5 to 1 mA, or it may be switched
on as each nerve is approached, then turned off after confirmation.
When elbow flexion occurs, the nerve is localized. The stimulator can
be switched off, and incremental injections of 2 to 3 mL of local
anesthetic are begun. A “halo” of local anesthetic should be created
around the nerve. A total of 5 mL is injected here.
 |
|
Figure 36-1.
PM, pectoralis major; MC, musculocutaneous; BC, biceps; CB, coracobrachialis; M, median; V, axillary vein; A, axillary vein; U, ulnar; DBA, deep brachial artery; R, radial; H, humerus. |
median nerve, if evident, or to the region anterior and/or superior to
the artery. The nerve stimulator may be left on throughout the
procedure, or turned on at this time. When appropriate motor or
cutaneous stimulation confirms contact with the nerve, local anesthetic
is incrementally injected (5 mL) until a halo appears around the nerve.
The needle is then removed from the skin,
and
its entry point shifted to the caudal edge of the transducer. After
insertion in-plane, it is directed to the ulnar nerve, if evident, or
to the inferior edge of the artery. When motor or sensory stimulation
of the ulnar nerve occurs, 5 mL of local anesthetic is injected as
described previously. Finally, the needle is redirected more posterior,
and guided to the radial nerve. After confirmation of the nerve with
motor or sensory stimulation, 5 mL of local anesthetic is injected
incrementally, following the procedure outlined above.
-
Veins may vary in number, with one, two,
or even more being present. They are easily compressed, and care must
be taken to note their position, as even mild pressure with the
transducer can obliterate the lumen on the ultrasound image. Five to
ten percent of patients will have an accessory axillary artery located
deep or posterior to the primary axillary artery. -
It is difficult to contact and
anesthetize all four nerve blocks from one needle insertion site due to
the location of the nerves around the circumference of the artery and
the variable location of the musculocutaneous nerve.
A, Danelli G, Baciarello M, et al. A prospective, randomized comparison
between ultrasound and nerve stimulation guidance for multiple
injection axillary brachial plexus block. Anesthesiology 2007;106:992–996.
