Trauma about the Knee, Tibia, and Foot
|
|
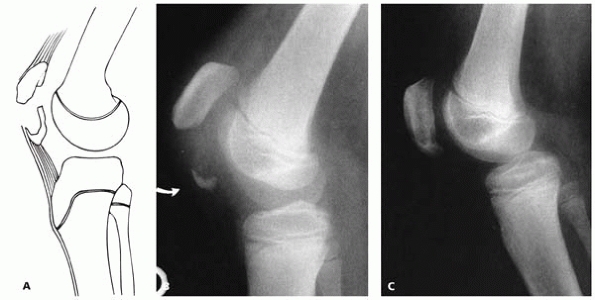
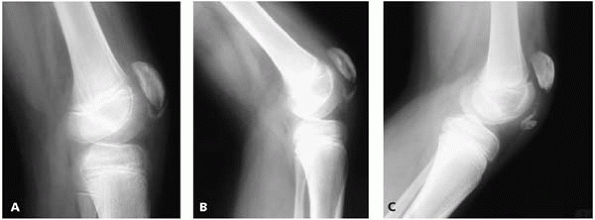
proximal pole of the patella, together with a significant sleeve of
articular cartilage, periosteum, and retinaculum, is pulled off the
remaining main body of the patella (Fig. 9-1). The easiest pitfall in this fracture is to miss it at initial presentation (Fig. 9-2)
as there may only be a hint of ossified bone on initial radiographs.
The clinical picture at presentation usually includes a palpable defect
at the affected patella pole and an inability to fully extend the knee.
 |
|
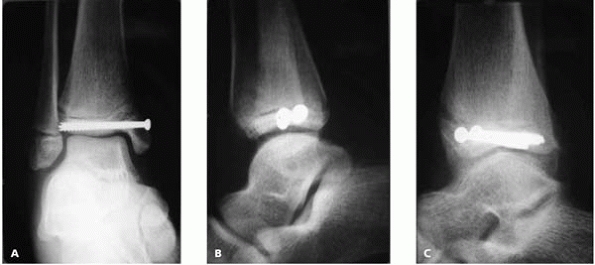
▪ FIGURE 9-1 Sleeve fracture of the patella. A: A small segment of the distal pole of the patella is avulsed with a relatively large portion of the articular surface. B: On lateral view, the small osseous portion of the displaced fragment is visible, but the cartilaginous portion is not seen. C:
Healed sleeve fracture after open reduction and internal fixation. (Reprinted with permission from Sponseller PD, Stanitski CL. Fractures and Dislocations about the Knee. In: Beaty JH, Kasser, JR, eds. Rockwood and Wilkins’ Fractures in Children, 5th ed. Philadelphia: Lippincott Williams & Wilkins, 2001:981.) |
as there may be a significant articular cartilage avulsion not
appreciated on plain radiographs. If displacement is questionable,
flexion/extension lateral films should be made in superior and inferior
sleeve avulsion fractures to assess intrinsic soft-tissue stability.
Widening of the fracture gap with lateral radiographs in flexion
usually indicates a need for surgical stabilization.1
During operative repair, retinacular repair is performed. If necessary,
sutures securing the patella tendon or quadriceps tendon may be passed
through drill holes through the patella for fixation. A nonoperative or
inadequate operative repair may progress to further displacement during
healing or rehabilitation (Fig. 9-3). A patella
sleeve fracture should not be confused with Sinding-Johansen-Larsen
disease, which is a chronic overuse injury that may be thought of as an
Osgood-Schlatter disease of the other side of the patella tendon.
 |
|
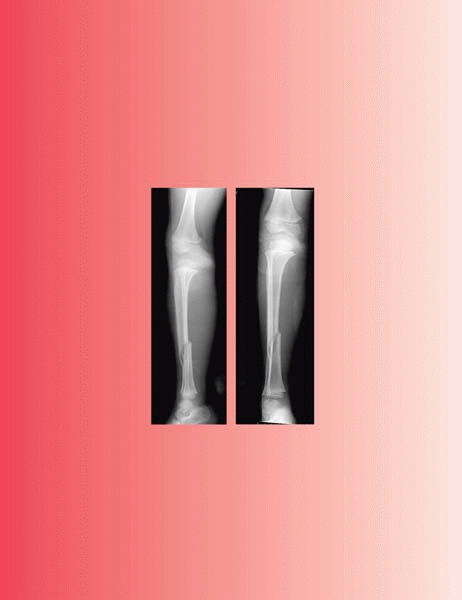
▪ FIGURE 9-2 A: Patella sleeve fracture of the superior pole. This was missed at presentation to an emergency department. B:
Two weeks later, ossification makes fracture more visible on radiographs. Surgical reconstruction at this stage is more involved. |
-
When repairing the
retinaculum, place all the sutures first without tying them. If the
sutures are tied as they are placed, it becomes increasingly difficult
to visualize the torn retinaculum and fracture. -
If closing the gap of the extensor mechanism is difficult:
-
Consider letting down the tourniquet which may be tethering the quadriceps.
-
If the fracture is
not acute, quadriceps contraction may have occurred, in which case
judicious musculotendinous lengthening of the quadriceps complex may be
needed.
-
fractures is not uncommon; consider this diagnosis in any trauma
patient who does not have full active extension of their knee.
 |
|
▪ FIGURE 9-3 A: Six weeks postoperative radiograph, lateral view, demonstrating migration of fracture fragment. B: Three months postoperative radiograph of the same patient. C: One year postoperative radiograph of the same patient.
|
edges comprised of cartilage or fibrous tissue can be delineated by
probing with a Keith needle or scalpel blade. Excision of the fragment
and reattachment of the overlying quadriceps tendon to the patella is
usually curative, as reported by Bourne and Bianco.2
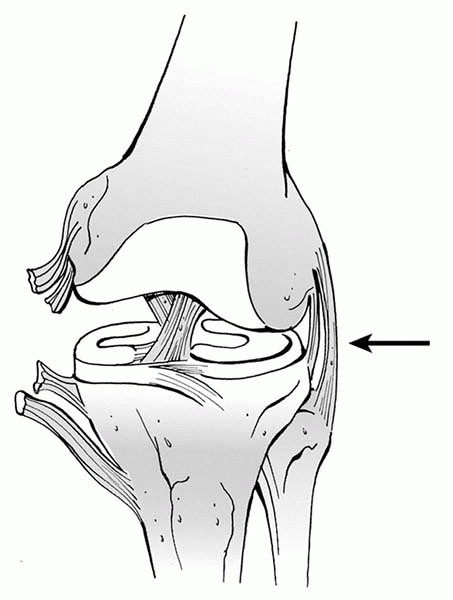
diagnosis. In the mature skeleton, ligaments usually fail before bone
when a bending stress is applied across the knee joint, thus following
a severe valgus stress across the knee a medial collateral ligament
(MCL) injury may occur (Fig. 9-4). As the
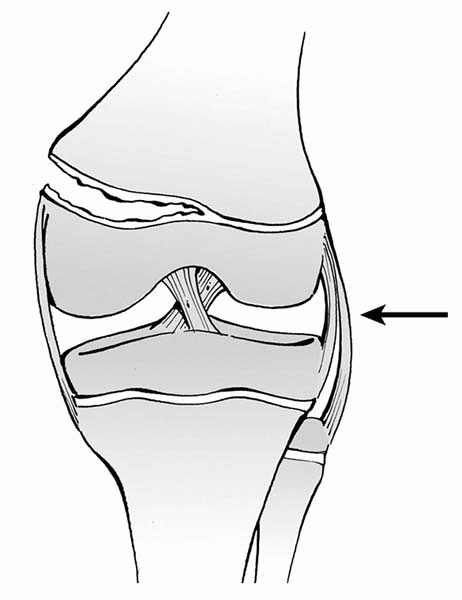
collateral ligaments originate on the epiphysis, in an immature
skeleton the physis will fail in tension and the knee will fall into
valgus though a Salter I or II fracture (Fig. 9-5).
A Salter I fracture may be nondisplaced and not radiographically
obvious. If suspicious of a Type I distal femoral undisplaced fracture,
the width of the physis is often greater than the contralateral physis
on radiograph. Clinically, there should be tenderness about the physis,
which is near the superior pole of the patella on either side of the
knee, and the knee may be unstable to valgus or varus stress. A stress
view radiograph or MRI can confirm the diagnosis; however, the need for
either test has been questioned as the initial treatment for both an
MCL injury and a nondisplaced distal femoral Salter I fracture is
immobilization. Repeat radiographic and clinical examination at 10 to14
days should help clarify the diagnosis.3
It is important to make a diagnosis at some point, because Salter
fractures about the knee require followup for evaluation of possible
growth plate injury.
 |
|
▪ FIGURE 9-4
Injury pattern with closed growth plates. In the mature skeleton, ligaments usually fail before bone when a bending stress is applied across the knee joint, so following a severe valgus stress across the knee a medial collateral ligament (MCL) injury may occur. Black arrow is direction of force. |
 |
|
▪ FIGURE 9-5
Injury pattern with open growth plates. As the collateral ligaments originate on the epiphysis, in an immature skeleton the physis will fail in tension and the knee will fall into valgus, though a Salter I or II fracture. Black arrow is direction of force. |
injuries is growth disturbance: either total arrest, which leads to
shortening, or partial arrest leading to angular deformity. Angular
deformity following distal femoral physeal injury is reported in 18% to
51% of recent series.4, 5, 6, 7
Growth injuries usually occur at the time of injury, and not a result
of mismanagement. Stay out of trouble (and depositions) by informing
parents before a growth disturbance that
the chances are nearly 50% for this problem occurring in their child,
and that surgery, including stopping the growth of the “normal” side,
may be needed in the future. While these injuries cannot be prevented,
one thing we can do is to follow children
with physeal injuries about the knee closely for at least one year. A
growth disturbance that is identified early may be treated with either
a contralateral epiphysiodesis (near the end of growth) or a
Langenskiöld procedure. An angular deformity recognized late may
require an osteotomy. An MRI with sequences chosen to highlight
cartilage can aid in the early diagnosis of a physeal bar formation.
One mechanism of injury that lies in wait to trap an unsuspecting
orthopaedic surgeon is an unrecognized physeal injury in association
with nonphyseal fractures in the femur or tibia. Hresko, et al.8
reported on seven children who had a physeal arrest about the knee in
association with nonphyseal fractures in the lower extremity.
reduction of these fractures. Series have reported rates of 43% to 70%
of distal femoral fractures treated without internal fixation have
displaced.9,10
Unless a fracture is truly nondisplaced and stable, stay out of trouble
by providing internal fixation. To avoid further injury to the physis,
reduction should be 90% traction and 10% manipulation, preferably in
the operating room with maximal relaxation. Salter I fractures may be
stabilized by smooth K-wires. Wires should not cross at the fracture,
but one should attempt to have the K-wires maximally separated at the
fracture line. Clinical experience and animal studies have demonstrated
that crossing the physis with smooth K-wires of the size commonly used
should not cause a growth disturbance.11
Anteriorly displaced Salter I fractures deserve special mention.
Previous texts have recommended closed reduction and casting with the
knee in a flexed position; however, this treatment may lead to knee
stiffness, and makes evaluation of frontal plane alignment quite
difficult. Stay out of trouble by pinning these fractures and providing
immobilization in near full extension. Of course, the knee should not
be immobilized in extension until the fracture has been reduced, as
vascular occlusion or peroneal nerve injury may result.
possibility of a superficial pin tract infection progressing to a
septic knee joint. Early fracture healing usually allows these pins to
be pulled at 3 to 4 weeks, which helps prevent this complication.
Continued protected immobilization is still indicated until clinical
healing. In thin children, pins may be brought out of the skin proximal
to the fracture site, and thus not be intraarticular. Salter II
fractures may often be closed reduced and fixed with cannulated screws
in compression across the metaphyseal fragment.
injury; they should be evaluated following fracture fixation and again
following fracture healing. Knee stiffness can be expected in about 25%
of patients,12 so the surgeon should
warn parents ahead of time, as well as consider early physical therapy.
Fortunately, while peroneal nerve and popliteal artery injuries may
occur with distal femoral physeal fractures, they are not common.
 |
|
▪ FIGURE 9-6
AP radiograph of a 5-year-old boy in a stroller who was struck by a car. The Salter I fracture of the distal femoral physis was not recognized, and the child was initially treated with a short leg cast. This is an example of falling into the trap of “Satisfaction of Search.” When the first fracture is noted, human nature is to feel satisfied and not view the remainder of the radiograph with necessary diligence. |
This refers to a situation in which the detection of one radiographic
abnormality interferes with that of others. Once one fracture is found,
you are satisfied and stop looking. See Figure 9-6: Did you note the “other” fracture when looking at this same x-ray on the opening page of this chapter?
trying to treat a displaced fracture with casting without fixation. The
gastrocnemius muscle attaches to the distal femur, thus pulling the
distal femur into flexion. This tempts the surgeon to cast reduce and
cast this fracture in knee flexion. However, if the knee is casted in
flexion, exact alignment of varus/valgus positioning is nearly
impossible to verify. Unfortunately, once the knee is extended after
fracture healing, the full extent of varus or valgus malalignment
becomes apparent. Avoid this complication by providing fixation, often
with K-wires, flexible intramedullary nails, or an external fixator for
displaced distal femoral metaphyseal fractures.
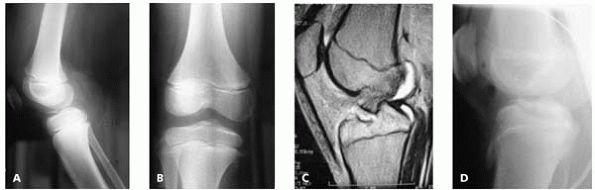
posterior cruciate ligaments in the skeletally mature results in
avulsion of the tibial spine in children. Stay out of trouble by not
missing the diagnosis on radiographs (Figs. 9-7A and B). If there is any doubt, an MRI or CT may be of assistance (Fig. 9-7C). The primary area to stay out of trouble is not to lose extension postoperatively (Fig. 9-7D). Some series have reported up to 60% of patients losing terminal extension following this injury.14
arthroscopically, an open reduction is not a sign of weakness.
Anecdotally we have heard of instances of severe arthrofibrosis and
permanent loss of motion of the knee in cases performed
arthroscopically more commonly than in cases treated with
open
reduction. In a tibial spine fracture that does not reduce with
extension of the knee, the meniscus or transverse meniscal ligament may
be under it and preventing reduction. There are many techniques
described in texts for fixation, which probably means they all work
well, more or less. To stay out of trouble, do not place any permanent
fixation across the proximal tibial physis if there is significant
growth remaining.
 |
|
▪ FIGURE 9-7 A: Lateral radiograph demonstrating a tibial spine avulsion. B: Note the fracture is not well visualized on an AP view. C:
MRI demonstrates this fracture as well, but was probably not necessary in this case as the lateral radiograph made the diagnosis. D: Following casting in full extension, the fracture reduction was accepted as adequate. The fracture healed and the knee did not lose extension. |
and positive antero drawer for a few weeks, my experience is that the
knee gradually “tightens up” with further growth and development and
has a normal range of motion 1 to 2 years postinjury.
boys, usually during jumping sports such as basketball. This fracture
occurs along the apophysis deep to the tibial tubercle, and should not
be confused with Osgood-Schlatter disease (Table 9-1).
completion of physical maturity, so growth disturbance is usually not a
problem in these older kids. The fracture may extend into the joint, in
which case anatomic reduction is needed, and associated intraarticular
injuries such as meniscus or ligamentous injuries should be searched
for. Beware that some active knee extension may still be present
through retinacular fibers, so active knee extension does not rule out
a tibial tubercle fracture.
soft-tissue avulsion requiring repair as well. Sleeve avulsion
fractures of the tibial tuberosity extending over the anterior
metaphyseal area of the tibia have been recently described.15
These injuries are similar to patellar sleeve fractures in that initial
radiographs may show no more than small subchondral fragments of bone.
Davidson and Letts15 report that
fixation of the Type V sleeve avulsion fracture is challenging because
of a lack of a large bony fragment. They recommend fixation with
small-diameter screws and heavy nonabsorbable sutures between the
intact periosteum or bone and the large avulsed segment of periosteum.
is prominent hardware requiring removal. The use of multiple smaller
screws (4.5 mm instead of 7.3 mm) may help minimize this complication.
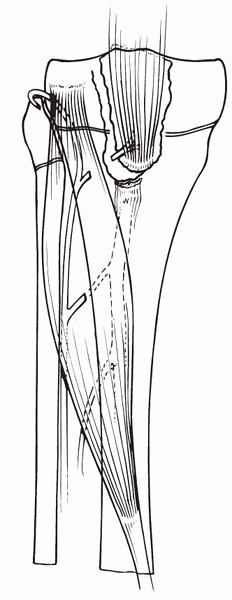
Because this fracture is associated with relatively low-energy trauma,
compartment syndrome may not be on the radar screen of the unsuspecting
surgeon. Compartment syndrome occurs presumably because of tearing of
anterior tibial recurrent vessels, which fan out at the tubercle but
retract into the anterior compartment when torn (Fig. 9-8). Close monitoring is necessary for patients treated
nonoperatively; careful inspection, possibly with prophylactic anterior
fasciotomy, is recommended for patients treated operatively.
|
TABLE 9-1 Do Not Confuse a Tibial Tubercle Fracture with Osgood-Schlatter Disease
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
▪ FIGURE 9-8
Probable mechanism of development of compartment syndrome after tibial tubercle avulsion. The anterior tibial recurrent artery, and possibly its branches, is torn and retracts into the anterior compartment musculature. (Reprinted with permission from Sponseller PD, Stanitski CL. Fractures and Dislocations about the Knee. In: Beaty JH, Kasser, JR, eds. Rockwood and Wilkins’ Fractures in Children, 5th ed. Philadelphia: Lippincott Williams & Wilkins, 2001:981.) |
tibial physis has intrinsic anatomic stability from the proximal
fibula, an overhanging tibial tubercle, and the MCL extending beyond
the physis to insert into the upper metaphysis. Because of this
protection, separation of the proximal tibial epiphysis is relatively
rare and requires significant force.
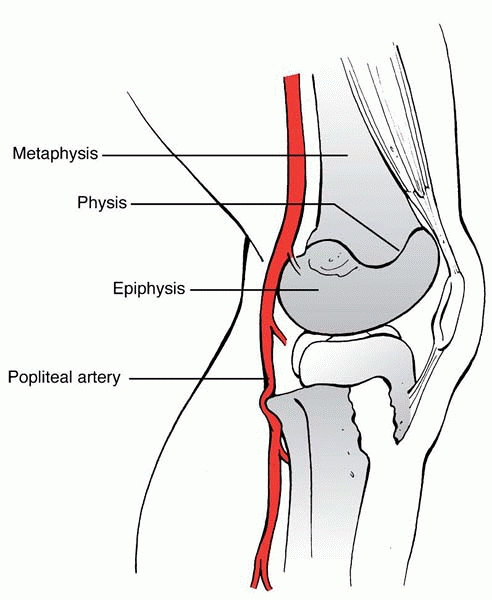
physeal fracture is vascular compromise. The popliteal artery is
tethered by its major branches to the posterior surface of the proximal
tibial epiphysis, with the anterior tibial artery passing forward just
proximal to the interosseous membrane. A hyperextension injury that
results in posterior displacement of the upper end of the metaphysis
may stretch and tear the bound popliteal artery (Fig. 9-9). It is important to remember that even a fracture that appears minimally displaced at presentation
in an emergency department may have had significantly more displacement
at the time of injury, particularly in motor vehicle accidents (Fig. 9-10).
 |
|
▪ FIGURE 9-9
Posterior displacement of the epiphysis following fracture-separation at the time of injury can cause arterial injury. In addition, a posteriorly displaced fragment can cause persistent arterial occlusion by direct pressure. |
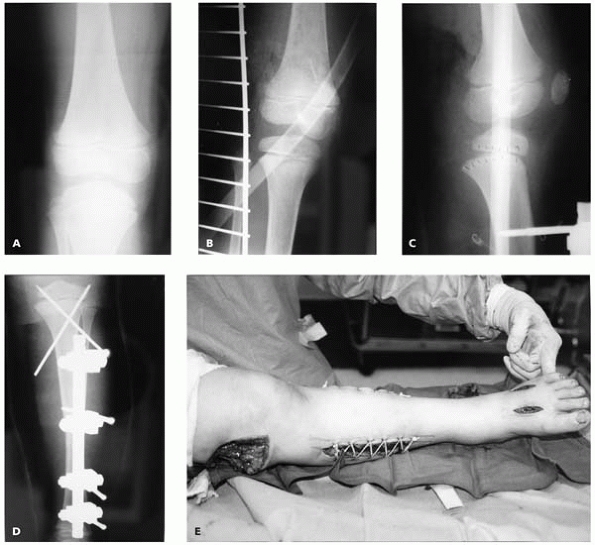
physeal fractures because of mechanical blockage of the vascular
structures from a displaced fracture following the injury or damage to
the popliteal artery at time of injury, including an intimal tear that
may not be clinically significant at presentation. It
is
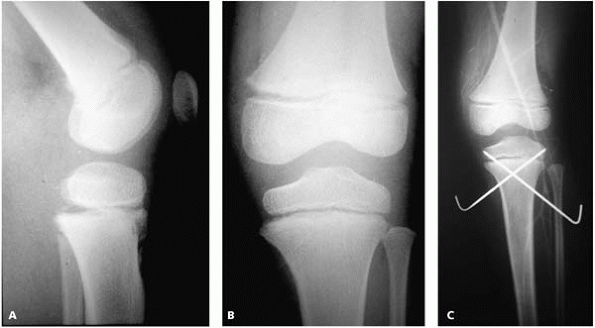
important to remember in this injury that even a small posterior
displacement of the metaphysis may obstruct popliteal blood flow, as
the artery is tethered anteriorly against the metaphysis by the
anterior tibial artery (Fig. 9-11).
 |
|
▪ FIGURE 9-10 Child on back of bicycle struck by car sustained ipsilateral proximal femoral and tibial shaft fracture. A,B: proximal tibial physeal fracture on initial radiographs were not appreciated. C:
Following external fixation of the tibial diaphyseal fracture, a Salter-Harris Type I fracture of the proximal tibial physeal is evident. D: Closed reduction and K-wire fixation were used to treat the proximal tibial physeal fracture. E: Compartment syndrome occurred, which is associated with proximal physeal fractures of the tibia. In this case, the contribution of concomitant injuries to the compartment syndrome is difficult to discern. |
 |
|
▪ FIGURE 9-11 A: Lateral radiograph demonstrating minimal posterior displacement of a Salter-Harris I fracture of the proximal tibia. B: No significant displacement is noted on the AP radiograph. C: Although angiogram demonstrates good flow past the fracture site, a compartment syndrome developed.
|
proximal tibial physeal fractures have associated ligamentous injuries,
primarily anterior and valgus laxity.18
We suspect that these are underrecognized injuries and recommend
assessment of ligaments by physical exam following operative fixation
and fracture healing.
inherently stable, separations of the proximal tibial epiphysis may be
surprisingly unstable. There should be no hesitation to provide
fixation with K-wires or other means if there is any question about
stability of fracture reduction.
radiographs, and are associated with patellar dislocations. Despite the
fact that these fractures involve articular cartilage, they do not
always require surgery if they are in non-weight-bearing areas and
stuck in synovium out of the way of weight-bearing surfaces.
tibial metaphysis without a fibula fracture may develop a valgus
deformity over 50% of the time.19
Maximum valgus occurs about one year following injury. A 15-year
followup of seven patients with this fracture demonstrated a mean of 8
degrees of improvement of the proximal tibia valgus from the point of
maximal deformity. Less well known is that every patient had a limb
length discrepancy (mean = 9 mm) at time of last followup.19
valgus, and even a little varus if possible. It is unclear, and
probably unlikely, that anatomic operative reduction will prevent
future valgus.20 Stay out of trouble
by expecting varus remodeling to be sufficient in most patients, and
wait at least 2 to 3 years following injury before considering
intervention in most cases. Valgus deformity has been shown to recur
following early osteotomies.21
However, if malalignment does not remodel over time, joint degeneration
of the lateral compartment requiring an osteotomy has been reported.19
For those rare cases in which intervention for the valgus deformity is
necessary, we recommend consideration of staple hemi-epiphysiodesis in
children with growth remaining.
well with casting, though loss of reduction is common in unstable
fractures. Fractures may be manipulated up to 2 to 3 weeks when the
callus is “sticky,” with good results.
fibula intact, tend to drift into varus and/or posterior angulation
over the first three weeks and deserve close monitoring during this
time.22 The initial cast should
attempt to mold maximum valgus; especially in lower third fractures,
consider casting the foot in equinus to prevent posterior angulation.
Residual or recurrent varus and posterior angulation of ≤10 degrees has
been shown to correct spontaneously with growth and remodeling.22 We would observe for remodeling a fracture with even more deformity prior to recommending open realignment or osteotomy.
injuries than tibia fractures alone. While many may be managed by
casting alone, unstable fractures may require fixation. Unlike adults,
stabilization with K-wires alone is frequently sufficient for many
fractures, including open fractures. Wires may be left out of the skin
and removed in about 4 weeks in clinic after early callus formation.
tibia fractures are quite encouraging and applicable for most fracture
patterns, except truly length-unstable fractures. For open fractures,
intramedullary nails avoid the soft-tissue tethering of external
fixation and keep the plastic surgeons happy by maximizing their access
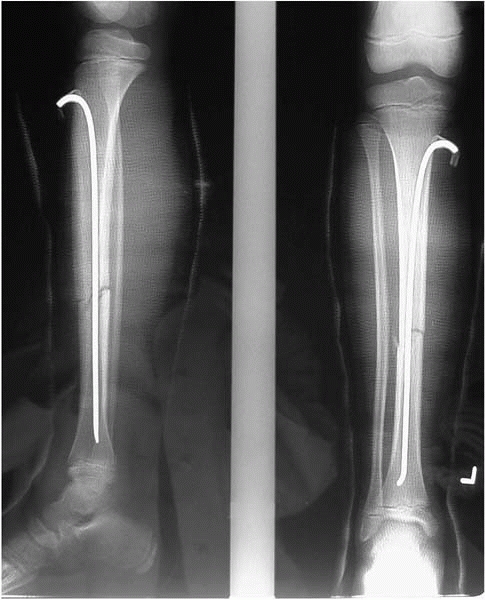
to the wound. In some cases, only one intramedullary nail may be used (Fig. 9-12). Flexible nails may by left out of the skin and removed in clinic after callus formation. External fixation, (a.k.a.
nonunion generators) may be indicated in length-unstable fractures and those near joints.
malaligned tibia fracture, be cognizant of potential for pressure sores
as there is little soft tissue in this region, especially in thin
children.
rotational alignment by evaluating and matching the other side. This is
especially easy to forget when casts are placed in the emergency
department under questionable sedation.
ankle equinus do not develop ankle stiffness. Lower tibial fractures
tend to drift into apex posterior angulation, which will be exacerbated
by an ankle casted in neutral, and improved by an ankle casted in
equinus.
 |
|
▪ FIGURE 9-12
Example of a tibia fracture that was not stable to closed reduction treated with a single intramedullary rod left out of the skin proximally. The rod was removed in the office at 4 weeks following injury, at which time adequate callus formation stabilized the fracture. |
soft-tissue openings, beware of forceful irrigation (i.e., jet lavage)
forcing fluid into compartments and causing a compartment syndrome.
fibula intact, often results from a young child falling while running.
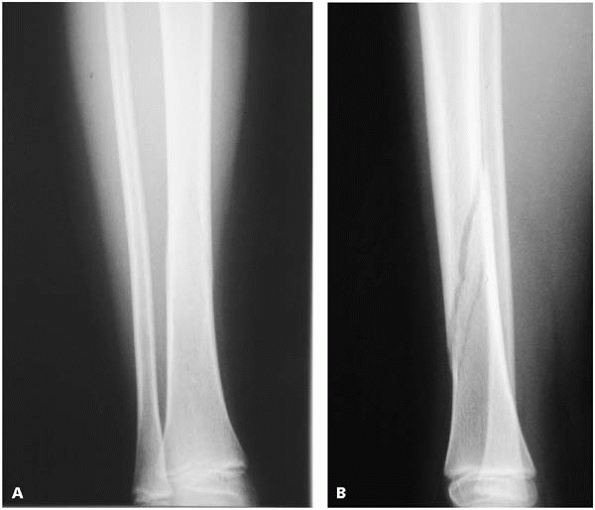
The big pitfall here is missing the fracture (Fig. 9-13).
At times, in addition to standard AP and lateral views, oblique views
may be needed to see a nondisplaced spiral fracture of the tibia. If
the surgeon is convinced there is localized pain in the tibia (which
may be difficult in a toddler), and the child is not walking, many
recommend treatment for a
presumed
toddler’s fracture. However, always beware of the possibility of
infection, and counsel the family that if the symptoms are worsening
despite casting, return for reevaluation soon.
 |
|
▪ FIGURE 9-13 A,B:
A spiral fracture of the tibia may be difficult to appreciate if only one radiographic view is obtained. These radiographs illustrate the importance of orthogonal radiographs when evaluating a child with the possibility of a fracture. |
To stay out of trouble with pediatric ankle fractures, be aggressive in
treating Salter fractures that enter the joint (Salter III and IV).
These fractures have been reported to have up to a 38% rate of
premature physeal closure even with modern treatment methods. These
fractures tend to do poorly with closed treatment23
and degenerative changes are common in these fractures healing in a
nonanatomic position. Any displacement of ≥2 mm should be treated with
anatomic reduction and fixation. For medial malleolar fractures (Salter
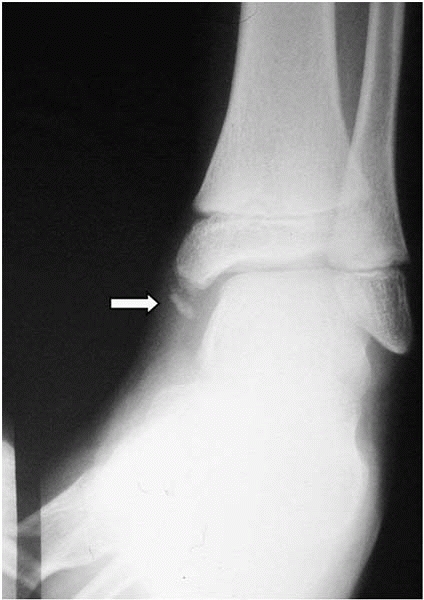
III or IV), also be aware of subtle medial angulation of the fracture,
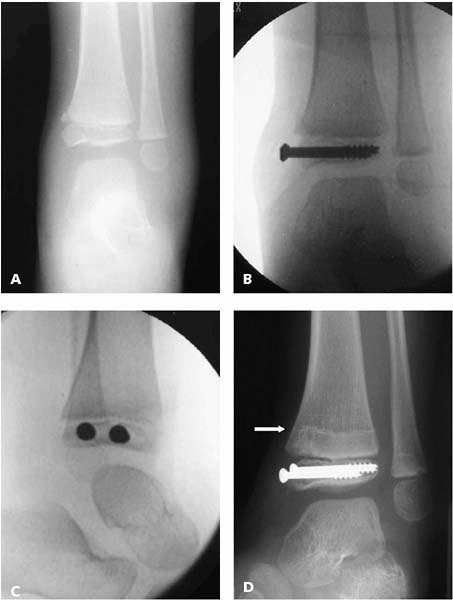
which is indicative of displacement and an indication for surgery (Fig. 9-15).
To stay out of trouble, remember that the plafond of the tibia is
arched, so both AP and lateral images are needed to ensure that the
screws are not in the joint (Fig. 9-16).
 |
|
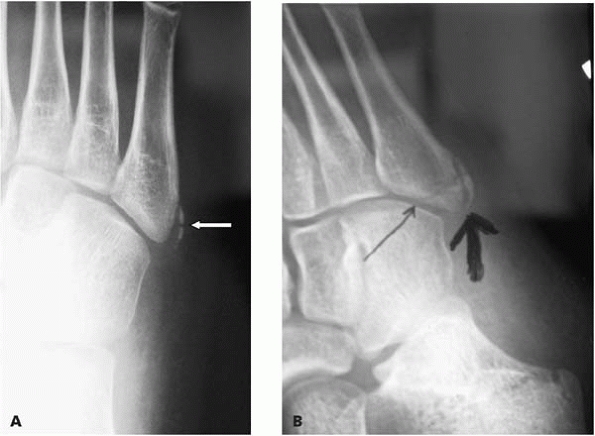
▪ FIGURE 9-14 Ossification of the tip of the medial malleolus is common (arrow).
One can often quickly establish that this is not a fracture in children who have sprained their ankles and have only lateral tenderness. |
displacement is usually considered acceptable, and operative reduction
is traditionally considered uncommonly needed. This approach has been
recently questioned by one study, in which the rate of premature
physeal closure was found to be 3.5 times higher (60% premature
closure) in Salter I and II fractures if there was residual fracture
displacement of >3 mm in postreduction films. The authors attributed
this to interposed periosteum (see box).24 These fractures often occur in older children, in whom a premature physeal closure may not have clinical relevance.
 |
|
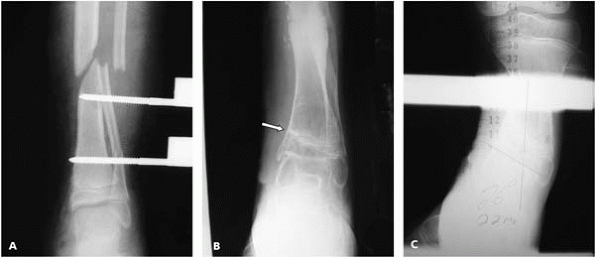
▪ FIGURE 9-15 A:
Displaced Salter IV fracture of the distal tibia in a 5-year-old. Unlike diaphyseal or metaphyseal fractures that will remodel with growth, fractures with displacement of the joint or physis should be treated aggressively with anatomic reduction and fixation. B,C: AP and lateral imaging intraoperatively ensure both screws are not in the joint or the physis. D: Ten months following the injury a growth arrest line parallel to the physis confirms normal growth of the physis. |
 |
|
▪ FIGURE 9-16 A: Fixation for a medial malleolar fracture appears to be in acceptable position on a mortise radiograph of the ankle. B,C:
Lateral and oblique views demonstrate one screw is intra-articular. These views should have been obtained with intraoperative imaging to allow the screws to be replaced prior to leaving the operating room. |
 |
|
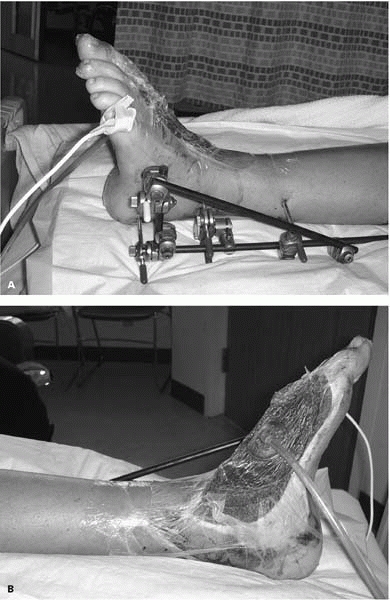
▪ FIGURE 9-17 This 10-year-old boy had a grade three open tibia and fibula fracture with severe soft-tissue loss medially. A: The shear injury to the medial malleolus and physis were initially not appreciated. B:
Thirteen months later a growth arrest of the medial physis is evident by the angulation of the growth plate. The lack of a normal sized medial malleolus is appreciated in this radiograph as well. C: Twenty-two months later there is 26 degrees of angulation. |
reported a histologic study in rats to examine the role of interposed
periosteum in proximal tibial physeal fractures. If the physis was
intentionally ablated, a physeal bar predictably resulted. If the
physis was left intact, they found the physis was able to repair itself
even in the presence of interposed periosteum. They concluded that
“Based on our present findings, interposed periosteum seems to play a
passive role in physeal fracture healing… [with] no histologic evidence
of any osteogenic potential.”
lawnmower. The soft tissue and portion of the bone and physis about the
medial malleolus are removed in shear, usually in a high-energy, dirty
setting. Customarily, care efforts are focused on the open injury, and
the consequences of the physeal damage are not apparent until much
later (Fig. 9-17). While it is unproven,
covering the exposed physeal edge in an effort to prevent the formation
of a peripheral bony bar may be worthwhile. We have used bone wax for
this. Warning the family ahead of time, and recognizing and addressing
the growth disturbance early, may improve outcome and minimize surgery.
injuries. Skin grafts and flaps are often needed, but plastic surgeons
warn us they are at risk of not “taking” due to motion about the ankle.
An external fixator spanning the ankle, with pins in the calcaneus and
metatarsals, allows wound care, promotes soft-tissue healing of graft
or flap, and prevents the development of ankle equinus (Fig. 9-18).
 |
|
▪ FIGURE 9-18
A pedestrian child was hit by a car and dragged, causing a distal tibia and fibular fracture, in addition to severe soft-tissue loss exposing bone and joint. A: An external fixator across the ankle helps maintain stability of the tibia fracture, prevents ankle equinus, and immobilizes the area of soft-tissue injury to maximize chances of a future skin graft being successful. B: In this child a wound VAC was used to prepare the area of exposed bone and joints prior to skin grafting. |
has recommended that children less than 12 years of age should not
operate a walk-behind power mower. Of the 69 children with lawnmower
amputations in a recent study by Loder,26
68 were 13 years old or less at the time of the injury. Simply
following the American Academy of Pediatrics guidelines would have
eliminated nearly all of those injuries.27
The treating physician needs to be aware of the potential for family
psychosocial issues following these injuries, in which a family member
may be considered “at fault.”
medial to lateral direction over about an 18-month period. Fractures
through the partially opened lateral growth plate deserve mention
because they are usually intraarticular, often require operative
reduction, and have potential for being missed or undertreated.
Children’s Hospital, of 26 patients with so-called Tillaux fractures,
nine could be diagnosed only by the oblique radiograph and five were
initially missed.
corner of the distal tibial epiphysis by the anteroinferior
tibiofibular ligament. These fractures are believed to occur secondary
to external rotation of the ankle, so the maneuver for closed reduction
is internal rotation. A triplane fracture has a more complex geometry,
with the fracture extending into the metaphysis. The fracture may be in
three planes (hence the name): the sagittal plane within the epiphysis
and extending into the joint; the transverse plane along the open
growth plate; and the frontal plane extending proximally into the
metaphysis. The metaphyseal component of the fracture is surprisingly
easy to miss at times, and often best appreciated in the lateral view,
which demonstrates a posterior metaphyseal fragment. The fracture may
be in one piece, or multiple pieces, but do not be distracted by the
exact nature of the fracture pattern—it is of secondary importance.
fractures: the joint surface. The amount of displacement, and more
important, the amount of intraarticular stepoff, is notoriously
difficult to assess on plain films, particularly when the child is in
plaster. To stay out of trouble, consider a CT scan for a Tillaux or
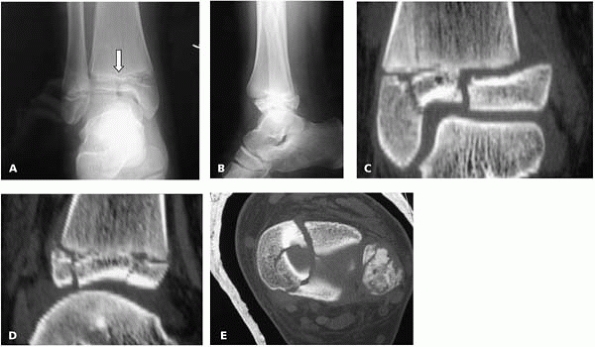
triplane fracture with any displacement seen on plain films (Fig. 9-19).
For fractures of questionable displacement, the child may be placed in
a long leg cast with internal rotation of the ankle, prior to the CT to
evaluate the fracture after attempted closed reduction.
 |
|
▪ FIGURE 9-19 A: AP view of a triplane fracture. Note that on the plain radiographs the intraarticular component of the fracture (arrow) does not appear to be very displaced or have a stepoff. B: Lateral view of fracture. C, D, E: CT further reveals extent of intraarticular stepoff and comminution.
|
treatment has been recommended for fragments with >2 mm
displacement, with series reporting an increased risk of poor results
in fractures healing with >2 mm displacement. We think an important
distinction should be made between joint stepoff and fracture gap. Some
surgeons will accept up to 5 mm of fracture gap in triplane fractures,
and possibly even more in a Tillaux fracture that does not involve a
significant amount of bone in a weight-bearing region. However, no more
than 2 mm of intraarticular stepoff can be accepted, and if present,
closed or open reduction using standard surgical principles is
indicated. Cannulated screws are helpful in these fractures. Often the
posterior metaphyseal fragment can be reduced and fixed through an
anterior incision.
are associated with fibular fractures nearly 50% of the time, an
ipsilateral tibial shaft fracture nearly 10% of times, and can even be
associated with a proximal fibula fracture and syndesmotic injury
(Maisonneuve equivalent).28,29
there is no significant growth potential left in the growth plate, so
in terms of treatment the growth of the physis can be ignored. This is
one of the few times you can put a screw across an open growth plate
with a clean conscience.
fracture from an ankle sprain in a child with an open physis may be
difficult on physical examination, and initial radiographs in both
conditions may be normal. In a fresh injury, the location of tenderness
usually allows one to make the diagnosis with some confidence. If there
is tenderness (and swelling) anterior to the distal fibula, along the
anterior talofibular ligaments, assume there is a sprain. Fibular
tenderness may be assessed by tapping with your finger on the posterior
half of the distal fibula that is free of the anterior talofibular
ligament. If there is bony tenderness, assume an occult Salter I
fracture. The bottom line, however, is that either injury could be
treated with functional bracing.
the peroneus brevis attaches is frequently mistaken for a fracture by
the unknowing. Remember that the normal apophysis is roughly parallel
to the metatarsal, while a fracture tends to be roughly perpendicular
to the metatarsal (Fig. 9-20A and B).
misdiagnosed and easily overlooked in children. Fractures of the base
of the second metatarsal are usually an indication of an associated
tarsometatarsal joint injury. Remember that the fourth metatarsal
should line up with the medial cuboid and the second metatarsal with
the lateral border of the medial cuneiform. In Lisfranc injuries in
children at times the proximal findings may be subtle, whereas the
distal separation of the first and second metatarsals may be more
obvious.
significant soft-tissue injury, presumably from a combination of shear
and compressive forces. Compartment syndrome is common in this instance—even in the absence of fractures.
Anecdotal reports suggest that compartment syndrome of the foot may be
present even with relatively pain-free active motion of the toes, and
neurologic or vascular symptoms are uncommon. We suggest the 3-incision
technique (incision over the second and fourth metatarsus and the
medial border of the foot) to make certain all compartments are
released.
septic joint or osteomyelitis can result from this injury as well. In
phalangeal fractures, blood at the nail bed suggests an open fracture
that should be treated accordingly.
 |
|
▪ FIGURE 9-20 A: A normal apophysis of the base of the fifth metatarsal at the attachment of the peroneus brevis (arrow) in a 10-year-old girl. B: The thicker arrow points to the normal apophysis, which is roughly parallel to the metatarsal. The thinner arrow points towards a fracture, which is roughly perpendicular to metatarsal.
|
and a laceration proximal to the nail bed should alert physicians to
the presence of a possible open fracture. These injuries can be easily
missed, with delay in diagnosis leading to osteomyelitis and even
growth arrest.30
-
In any traumatic knee lacking active extension, consider the possibility of a patella sleeve fracture—palpate for a defect.
-
Distal femoral fractures—use fixation for any displaced fractures.
-
Reduction is 90% traction and 10% manipulation.
-
Beware that intra-articular pins can lead to a septic knee.
-
-
Make a concerted
effort to look for a proximal tibial physeal fracture in children with
high-force injuries about the knee. It is frequently minimally
displaced, and easy to overlook.-
Have high suspicion for arterial injury and compartment syndrome with proximal tibial physeal fractures.
-
-
In length-stable
open tibia fractures, flexible intramedullary nails may lead to quicker
healing than an external fixator, as well as leave the soft tissues
more accessible for the plastic surgeon. -
Plan for reduction and fixation of even minimally displaced medial malleolar fractures.
-
For any fracture
line extending into the tibial plafond on an AP or mortise radiograph,
consider a triplane fracture and a obtain CT scan. -
A “stubbed” toe with bleeding about the proximal nailbed may be an open fracture.
M, Moulies D, Longis B, et al. [Traumatic epiphyseal separation of the
lower end of the femur]. Revue de Chirurgie Orthopedique et Reparatrice
de 1 Appareil Moteur. 1988; 74:69-78.
PM, Wikstrom B, Hirsch G. The influence of transphyseal drilling and
tendon grafting on bone growth: an experimental study in the rabbit. J Pediatr Orthop. 1998;18(2):149-154.
DL. Extraarticular Injuries of the Knee. In Beaty JH, Kasser JR, eds.
Rockwood and Wilkins’ Fractures in Children, 6th ed. Philadelphia:
Lippincott Williams & Wilkins, 2005.
A, Gaynor T, Mubarak SJ. Premature physeal closure following distal
tibia physeal fractures: a new radiographic predictor. J Pediatr Orthop. 2003;23(6):733-739.
DR, Guille JT, Horn BD, et al. The stubbed great toe: importance of
early recognition and treatment of open fractures of the distal
phalanx. J Pediatr Orthop. 2001;21(1):31-34.