Surgical Management of Traumatic Unidirectional and Atraumatic Multidirectional Instability
III – Shoulder Reconstruction > Part B – Evaluation and Treatment of
Shoulder Disorders > 35 – Surgical Management of Traumatic
Unidirectional and Atraumatic Multidirectional Instability
instability is a failure of conservative treatment modalities. The goal
of surgery is to reconstruct glenohumeral anatomy in a balanced fashion
avoiding excessive tightening in any one direction, in other words, to
obtain a stable yet mobile shoulder without causing stiffness.
Pathoanatomy will vary from case to case, so a versatile treatment
strategy is necessary allowing adjustment of operative technique based
on the pathology encountered. Instability presents in an extremely
variable fashion from one patient to another as mentioned in previous
chapters and is associated with various pathologic lesions.
(traumatic unidirectional instability due to a Bank-art lesion that
typically requires surgery) and AMBRI (atraumatic multidirectional
instability that is often bilateral and treated with rehabilitation or
inferior capsular shift when conservative treatment fails).
surgical planning must take this into account. As arthroscopic
techniques improve, a larger percentage of these operations may be
performed arthroscopically, but the principles of treatment remain the
same whether the surgery is performed open or arthroscopically. The
surgeon should strive to identify all pathoanatomy based on history,
physical examination, radiographic studies, evaluation under
anesthesia, and diagnostic arthroscopy. Surgery can then be performed
to repair all damaged structures and re-establish balanced stability of
the glenohumeral joint.
first reported on the results of the inferior capsular shift for
multidirectional instability in 1980, describing a group who had
uncontrollable, involuntary inferior subluxation or dislocation
associated with both anterior and posterior dislocations or
subluxations of the shoulder. These patients had both signs and
symptoms of instability in all three directions. Unfortunately, many
patients with unidirectional or bidirectional instability with
associated asymptomatic laxity of the shoulder in another direction
have been lumped into this extreme category. The balanced surgical
approach described in this chapter can be successfully adapted
irregardless of the degree of instability encountered, but in the
severely affected group described by Neer and Foster, a modified
rehabilitation program may be in order to allow greater time for soft
tissue healing.
greatly increased the surgeon’s diagnostic and therapeutic capabilities.3
A careful diagnostic arthroscopy prior to instability repair allows the
surgeon to identify all pathology contributing to the patient’s
instability.4 Bankart lesions have been reported in combination with superior labral tears5 as well as significant stretching of the glenohumeral joint capsule.6,7 Failure to identify and treat all contributing pathology may lead to failure of the instability repair.8,9
Some lesions such as superior labral tears are best treated
arthroscopically, emphasizing the importance of arthroscopic evaluation
even if open instability repair is planned. Other cited advantages of
arthroscopic instability techniques include lower morbidity, decreased
pain, shorter surgical time, improved cosmesis, and better maintenance
of motion postoperatively.3,10 The degree to which
these theoretical advantages apply will vary from surgeon to surgeon
depending on his or her own level of experience with arthroscopic
surgical technique. Currently arthroscopy does have its limitations,
with higher failure rates reported in cases of significant glenoid bone
loss (<25% loss of inferior glenoid).9,11,12 Modern arthroscopic techniques with suture anchors are well suited to manage labral pathology,13
whereas cases involving humeral avulsions of the glenohumeral ligaments
(HAGL lesion), capsular insufficiency following previous surgery,3
and multidirectional instability due to diffuse capsular laxity may be
better suited to open techniques. In cases in which the surgeon cannot
achieve stability with arthroscopic techniques, he or she should not
hesitate to proceed with an open instability repair.
pathologic lesions causing shoulder instability and surgical techniques
available to address pathology. Patients with traumatic shoulder
instability most commonly have a Bankart lesion whereas the hallmarks
of atraumatic instability are a redundant capsule and a widened rotator
interval.14 Although traumatic
instability is generally unidirectional, atraumatic instability is
generally bidirectional or multidirectional and can occur because of
congenital laxity, repetitive microtrauma to the shoulder, or traumatic
events superimposed on pre-existing laxity.15
As long as the surgeon understands that significant overlap exists in
these patient groups and is ready to treat all encountered pathology, a
successful surgery can be planned and expected.
management of labral pathology such as Bankart lesions and can be
adapted to treat associated capsular and rotator interval pathology.
Recent reports on suture anchor techniques have shown comparable
results to open Bankart repairs.16
The open inferior capsular shift offers a versatile and highly
effective approach to diffuse capsular laxity and has significant
advantages over other described open techniques. The capsular shift
procedure described by Neer can be modified to adjust the tightening of
the capsule depending on the amount and location of laxity in a
particular shoulder. It can be modified for unidirectional,
bidirectional, or multidirectional instability.14
The inferior capsular shift is designed to reduce capsular volume on
all sides including anterior, inferior, and posterior through a single
approach. It allows overlapping and therefore reinforcement of tissues
in the direction of greatest instability with tightening of the capsule
inferiorly and on the opposite side. This procedure also avoids
asymmetric tightening, which can lead to abnormal joint mechanics and a
fixed subluxation in the opposite direction.17
The operation is laterally based to allow for greater volume decrease
than medially based or centrally based techniques because the
glenohumeral joint capsule is a laterally based, truncated cone.18
This approach also allows treatment of associated labral avulsions
anteriorly and rotator interval closure. It does not allow adequate
exposure of the superior labrum, and diagnostic arthroscopy is
beneficial prior to open surgery to allow visualization of the superior
labrum and arthroscopic superior labral repair if needed
arthroscopically.
capsular shift will be described for the treatment of atraumatic
instability and the arthroscopic Bankart repair using a suture anchor
technique will be described for the treatment of traumatic instability.
Although these techniques are by no means the only procedures
recommended for the treatment of shoulder instability, they are both
versatile and effective and afford surgeons the ability to adapt their
techniques to all encountered pathology.
regional anesthesia, general anesthesia, or a combination of both. The
interscalene block provides pre-emptive analgesia as well as excellent
postoperative analgesia and has been proven to be reliable and safe.19
Its shortcomings include the fact that the posterior shoulder
(posterior arthroscopic portal) and axilla are not adequately covered
by the block and require the addition of local or general anesthesia.
In addition, the pectoralis major is not completely included, and
tension in this muscle may limit exposure during deep dissection in
open repairs. For arthroscopic techniques, muscle paralysis is
generally not required although it is helpful for open approaches. This
author uses a combination of general anesthesia and interscalene block
for all instability repairs. A laryngeal mask airway is generally used
in arthroscopic cases unless airway issues require the use of an
endotracheal tube. In open cases, an endotracheal tube is used so that
muscle paralysis can be used to relax the pectoralis major.
performed in the beach-chair position. In open cases, the torso is
placed at a 30-degree angle to the floor. This position allows easy
access to the axilla if an axillary skin incision is to be used and
offers excellent access to the inferior pouch. The trunk is placed more
vertically in arthroscopic cases to allow easier access to the
posterior shoulder. In arthroscopic cases, the beach-chair position
allows easy conversion to open surgery if necessary. Distraction of the
humeral head away from the glenoid is most easily achieved, however, in
the lateral decubitus position with traction on the arm and the weight
of the patient’s dependent body as countertraction. In the beach-chair
position, distraction of the glenohumeral joint for improved
arthroscopic visualization runs the risk of displacement of the
patient’s body off the operating table. In these cases, the patient’s
torso can be tied to the operating table, using a sheet to prevent
displacement. A neurosurgical headrest is helpful with either approach
to allow better access to the shoulder.
direction and degree of instability. This rarely contradicts the
preoperative diagnosis but may be helpful, especially in muscular
patients who guard on examination in the office. It is also helpful in
defining the primary area of instability. The surgeon must be careful
to relocate the humeral head in the glenoid prior to each maneuver to
maintain a frame of reference. Translation of the humeral head over the
glenoid rim is abnormal in any direction. With the arm at the side, the
sulcus test in neutral will demonstrate laxity in the superior portion
of the glenohumeral capsule including the superior glenohumeral
ligament as well as the rotator interval. This is also indicative of an
enlarged inferior pouch. Failure of the sulcus sign to improve
significantly by placing the shoulder in an externally rotated position
is indicative of incompetence of the rotator interval tissue as this
should normally tension in external rotation. With the arm in 90
degrees of abduction and neutral rotation, the shoulder can be gently
forced anteriorly and posteriorly to test the laxity of the inferior
glenohumeral ligament and the anterior and posterior capsule. Crepitus
on dislocation and relocation is suggestive of labral pathology. If the
humeral head locks out of joint, this is suggestive of a Hill-Sachs
lesion.
identifying pathologic lesions contributing to the patient’s shoulder
instability whether an arthroscopic or open technique of repair is
planned. A standard posterior portal is established in the soft spot,
and a 30-degree arthroscope is used to perform a systematic evaluation
of the glenohumeral joint. Placement of the anterior portal must be
carefully planned as two anterior portals are required for arthroscopic
instability repair. For the diagnostic arthroscopy, an 8-mm cannula can
be placed anterosuperiorly through the rotator interval adjacent to the
glenoid and labrum. This allows space for later placement of an
additional cannula (usually 5 mm) farther inferiorly and laterally,
which enters the rotator interval laterally at the triangular
convergence of the supraspinatus and subscapularis tendons. Areas of
concern include the articular surfaces, the labrum, the capsule, and
the rotator cuff and biceps tendons.
have described a method to determine arthroscopically how much
anteroinferior glenoid bone is missing in the case of a bony Bankart
lesion. Bone loss >25% of the glenoid would be an indication for
open bone grafting. Secondary degenerative changes of the articular
surfaces owing to chronic instability or large chondral lesions from an
acute traumatic dislocation can be documented as these may affect
prognosis.
visual inspection and tactile examination with a probe. The superior
labrum may normally be meniscoid, with the diagnosis of a torn labrum
reserved for cases with fraying and granulation. A torn superior labrum
can generally be elevated off the glenoid rim by 1 cm. Anteriorly, the
labrum may be detached and clearly visible or it may be healed along
the anterior glenoid neck (anterior labroligamentous periosteal sleeve
avulsion lesion, or ALPSA lesion).20
In this latter case, the anteroinferior glenoid appears bare with the
capsule attaching medially on the glenoid neck. This lesion must be
identified so that the labrum can be elevated and reduced back onto the
rim of the glenoid.
midsubstance tearing, or tearing from its humeral insertion (HAGL
lesion). The drive through sign describes the ability to easily push
the arthroscope between the humeral head and glenoid, passing the scope
from the back to the front of the glenohumeral joint. The drive through
sign indicates capsular laxity, and if it persists following
arthroscopic labral repair, suggests a concomitant capsular stretching,
which may require further capsular imbrication or open repair.
with glenohumeral instability, and arthroscopy allows identification
and treatment. The biceps anchor may be involved with superior labral
tears and is readily identified arthroscopically.
release of the capsule far enough inferiorly and posteriorly to allow
obliteration of the inferior pouch and any associated posterior
capsular laxity. Understanding and performing several key maneuvers are
critical to success and should help give the surgeon confidence with
this operation. Proper takedown of the capsule is critical to avoid
bisecting the inferior pouch. The capsular insertion inferiorly on the
medial humeral neck is broad and somewhat variable anatomically.21
Safe techniques with release of both the superior capsular reflexion
and the more inferior capsular insertion under direct vision are
critical in avoiding potential injury to the axillary nerve. Simple
guidelines are available to determine the amount of capsular release
and amount of shift needed in each individual case.
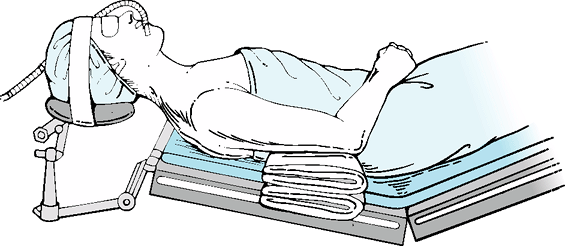
headrest is used to allow the assistant access to the superior
shoulder. A short arm board is built up with sheets to maintain arm
position anterior to the anterior axillary line (Fig. 35-1).
Local anesthesia is infiltrated in the axilla and the posterior portal
site as these areas are not adequately covered by the interscalene
block. The table back is elevated to position the trunk at a 30-degree
angle to the floor, and the table is placed in reverse Trendelenburg
during the diagnostic arthroscopy. The table back is then returned to
the 30-degree position for the open portion of the case. This maneuver
precludes the need to readjust the headrest between the arthroscopic
and open portions of the procedure.
for muscular men and typically measures 10 cm in line between the
coracoid and axillary fold.22 In
thin women, a 5- to 6-cm axillary incision can be made in the skin
folds. The axillary skin folds can be marked with a needle scratch
prior to draping, which allows the incision to be hidden.
Skin
flaps are elevated from the inferior rolled border of the pectoralis
major to the clavicle with either incision. A needle-point cautery is
useful for careful dissection while allowing hemostasis. The
deltopectoral interval is then developed using blunt and sharp
dissection taking the cephalic vein laterally. The clavipectoral fascia
is incised along the lateral border of the conjoined tendon, and this
structure is retracted medially. Excessive traction on this structure
is avoided to prevent damage to the musculocutaneous nerve. The
subacromial and subdeltoid bursal adhesions are released, and the
terminal branch of the posterior humeral circumflex vessel is
cauterized as it passes between the deltoid and proximal humerus just
lateral to the bicipital groove. The anterior humeral circumflex
vessels are ligated using no. 0 polyester sutures. This allows access
to the inferior portion of the capsule and has not been associated with
avascular necrosis. The sutures are placed 1 cm apart so that the
vessels can be cauterized in between and released. Care must be taken
to not grasp the joint capsule with the medial suture as this will not
allow the subscapularis to be separated from the capsule in later
dissection.
 |
|
Figure 35-1
In a beach chair position, the front and back of the shoulder are exposed to allow access to both sides. A neurosurgical headrest is helpful in positioning. A built-up arm rest with two sheets allows the arm to rest in the midaxillary line during capsular reconstruction. |
released sharply to the level of the ligament itself to allow clear
visualization of the rotator interval. The deep dissection is begun
with an incision of the subscapularis tendon 1 cm medial to the lesser
tuberosity. The superficial two-thirds of this tendon are dissected off
of the capsule using blunt and sharp dissection. Typically, a pointed
Adson clamp is used to spread the subscapularis fibers, and these are
cut with a long-handled no. 15 blade. The thickness of the
subscapularis can be determined by opening the rotator interval and
palpating the thickness of the tendon so that the superficial
two-thirds can be reliably peeled off of the underlying capsule while
leaving some tendinous tissue attached to the capsule for
reinforcement. During the inferior portion of this dissection, the
axillary nerve must be palpated and protected. The tug test, as
described by Flatow, is useful to localize the nerve.23
The surgeon passes the index finger of the inside hand along the
subscapularis muscle beneath the conjoined tendon. With the outer hand,
the surgeon palpates the axillary nerve on the undersurface of the
deltoid muscle lateral to the humerus. By gently tugging back and forth
with two hands, the surgeon can be sure which medial structure is
indeed the axillary nerve. The ability to tug the nerve medially and
feel tension on it laterally assures the surgeon of continuity of the
nerve through the axilla. The inferior portion of the subscapularis has
a very muscular insertion onto the capsule. This can be released using
electrocautery, and the plane between the subscapularis and the capsule
clearly visualized from this inferior portion of the approach. The
needle-point cautery is used to carefully cut through most of the
subscapularis thickness inferiorly until just a few muscle fibers are
visible overlying the capsule. These last few fibers are released using
a blunt elevator (a rounded blunt Cobb-like elevator is preferred).
This elevator can then be passed medially gently to define the plane
between the capsule and the subscapularis tendon. The tendon dissection
off the capsule can then proceed both from a medial-to-lateral and a
lateral-to-medial direction. It is important to free all subscapularis
fibers off of the capsule so that the capsule is free to be shifted and
not tethered by the subscapularis muscle. This also allows a Bankart
repair to be performed more easily if this is required. If
subscapularis fibers are left attached to the capsule medially at the
level of the glenoid, visualization for passage of sutures during the
open Bankart repair will be obscured. Suturing the subscapularis to the
capsule with the Bankart sutures can potentially tether the
subscapularis and limit motion. After release of the subscapularis, the
capsule can be clearly visualized.
interval. The capsule is transected 5 mm medial to the stump of
subscapularis tendon. This leaves enough capsule laterally to anchor
the repair later during capsular reconstruction. Traction sutures are
placed in the medial limb of the capsule during this maneuver. At the
inferior border of the subscapularis insertion, it is critical to
deviate the incision in the capsule in a hockey stick fashion laterally
along the neck of the humerus, essentially vertical and parallel to the
line of the humerus. This avoids amputation of a portion of the
inferior pouch. The axillary pouch is now palpated to determine its
size. The pouch does have a variable pattern of insertion on the
anatomic neck of the humerus. The periosteum and broad capsular
insertion are incised vertically along the anterior humerus just distal
to the most inferior aspect of the subscapularis stump. Inferior to
subscapularis tendon, the entire capsule can be released from the
humerus without leaving a lateral cuff as capsular repair will not
require suture placement that far inferiorly. The vertical portion of
the capsular and periosteal release
is
carried to the level of the latissimus dorsi tendon. An elevator can
then be used to elevate the capsule off the medial anatomic neck,
placing the elevator just inferior to the articular reflection of the
capsule. This allows any capsular reflection adjacent to the articular
surface (usually superior to the elevator) to be incised under direct
vision without risk of damage to the axillary nerve. Flexion and
external rotation will bring that portion of the neck of the humerus
into the surgical field and allow the capsule to be released from the
humerus under direct vision. This arm position also reduces tension on
the axillary nerve and allows it to fall away from the inferior pouch.
Additional traction sutures are placed into the margin of the capsule
as more capsule is liberated from the humerus. The more inferior
portion of the capsular insertion (that part inferior to the elevator)
is cut under direct vision with scissors just superior to the
latissimus dorsi tendon. This dissection can be carried posteriorly to
the level of the posterior band of the inferior glenohumeral ligament
if needed. The amount of capsular release and amount of shift required
will vary from patient to patient. Guidelines for capsular release are
the following. The capsule should be released from the anatomic neck of
the humerus until traction on the anterior capsule obliterates the
inferior pouch and also eliminates posterior subluxation of the
glenohumeral joint with the arm in neutral rotation. These two
observations at surgery indicate that the inferior and posterior
pouches are adequately tightened by anterior tension to allow for a
balanced reconstruction of the shoulder joint capsule.
Fukuda ring retractor) is inserted and the anterior labrum is carefully
inspected. If a Bankart lesion is noted, it can be repaired at this
time. The labrum is freed from the anterior glenoid neck, and the
glenoid neck is debrided down to bleeding bone. This can be done with a
curette, osteotome, or burr. This creates a fresh bleeding bed for
healing of the labrum. Suture anchors are generally placed on the rim
of the glenoid between the equator and most inferior point of the
defect depending on the amount of labrum avulsed. The labrum is shifted
superiorly with the sutures to afford a medial as well as lateral shift
with this procedure. Both suture limbs can be brought underneath the
labrum and out of the capsule, tying the knots extra-articularly. If
the patient has a hypoplastic labrum and the labral repair does not
create an adequate bumper, a no. 2 polyester suture can be placed
parallel to the glenoid through the labrum from approximately the 5
o’clock to the 3 o’clock position to create a purse-string type
imbrication of the labrum in that location. Palpation of the Bankart
repair should demonstrate a firm bumper of the labrum at the location
of the repair.
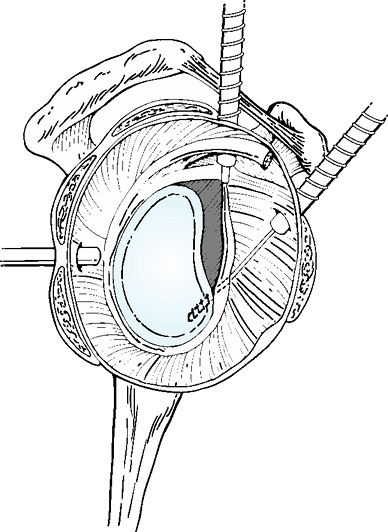
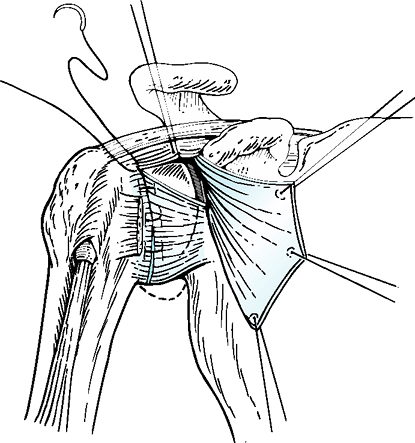 |
|
Figure 35-2
The inferior limb of the capsule is pulled superiorly as far as possible with the arm in the 30/30 position and typically can be repaired to the stump of the capsule laterally at the level of the rotator interval. Note the two rotator interval sutures, which will later anchor the superior limb of the capsule prior to overlap. |
cannot be effectively performed if the labrum and capsule are not
attached to the glenoid. A Bankart lesion must be repaired prior to
performing the capsular shift. Once the labral repair is performed, a T
cut can be made in the capsule obliquely along the superior border of
the inferior glenohumeral ligament (IGHL). Scissors are generally used
to cut the capsule. This T cut can also be performed prior to the
Bankart repair to help exposure. The IGHL is usually visible, but in
patients with hypoplastic ligaments, the capsular incision should
proceed obliquely superiorly to end at the equator of the glenoid. This
capsular incision generally passes anterior to the labrum, and the
labrum should not be incised.
amount of shift performed will vary from case to case and will depend
on the amount of capsule released, degree of capsular redundancy, and
the arm position selected for reattachment of the capsule. Deep
retractors are now removed, and for the average patient, the arm is
positioned in approximately 30 degrees of abduction and 30 degrees of
external rotation for performance of the capsular shift. In overhead
throwing athletes, this position can be adjusted even up to 80 degrees
of external rotation and abduction to allow for greater mobility in the
abducted/externally rotated position. The 30/30 position, however, is
the most common recommended position. The first step of capsular repair
involves placement of two sutures of no. 0 polyester at the lateral
aspect of the rotator interval superiorly. These are placed prior to
repair of the inferior pouch to avoid having to position the arm in
extension to visualize this area following repair of the inferior
portion of the capsule. These sutures will be later passed through the
superior margin of the superior limb of the capsule both to close the
lateral aspect of the rotator interval and to anchor the superior
portion of the capsule as it is pulled over the inferior capsule to
complete the capsular reconstruction. With the arm in 30 degrees of
abduction and external rotation, the inferior capsule is then pulled
superiorly as far as possible and is repaired to the lateral stump of
capsule using multiple no. 0 polyester interrupted figure-of-8 sutures (Fig. 35-2). The
amount of shift possible will vary from patient to patient, customizing
the repair to that particular patient’s degree of instability. The
superior limb of the capsule is then repaired to the rotator interval
using the previously placed polyester sutures. The superior limb of the
capsule is then pulled in a vest-over-pants fashion over the inferior
limb and is sutured laterally to the stump of capsule using multiple
no. 0 polyester interrupted figure-of-8 sutures. The two limbs of the
capsule are then sutured together medially (Fig. 35-3).
The subscapularis is now repaired anatomically using no. 0 polyester
interrupted figure-of-8 sutures back to the stump of subcapularis left
laterally. The continuity of the axillary is verified using the tug
test. Routine deltopectoral closure and skin closure are then
performed. Suction drainage is generally not required.
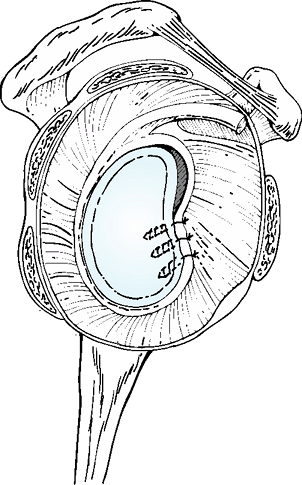
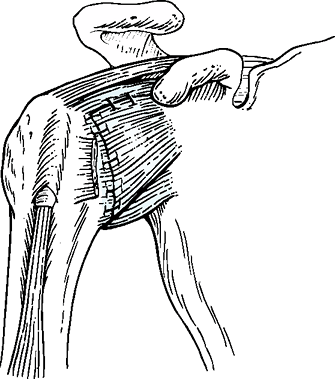 |
|
Figure 35-3
The final capsular reconstruction following inferior capsular shift. Notice that the anterior capsule is double thickness whereas the inferior pouch and posterior capsule have both been tightened with this approach. |
beach-chair or the lateral decubitus position. The lateral decubitus
position has the advantage of easier joint distraction without tying up
an assistant or running the risk of displacing the patient’s torso off
the table. If the beach-chair position is used, some type of
restraining device to hold the patient’s torso firmly to the operating
table is recommended to avoid pulling the patient off the table. We
generally use a combination of general anesthetic and interscalene
block for patient comfort both during and after the procedure, but
paralysis is not required for the arthroscopic procedure. Three
arthroscopic portals are required for arthroscopic Bankart repair, one
posterior and two anterior portals. The posterior portal is made in the
soft spot centrally in the posterior aspect of the glenohumeral joint.
One anterior portal should be placed to allow an 8-mm cannula to enter
the joint along the most medial and superior aspect of the rotator
interval into the joint. The second anterior portal is placed laterally
and slightly inferior to the first but not so inferior that the cannula
is aimed superiorly. This cannula will be used to drill holes and pass
suture anchors into the glenoid rim. Inferior orientation of this
cannula facilitates placement of the 5 o’clock anchor anteroinferiorly.
A 5-mm cannula is placed through this portal, entering the rotator
interval at its most lateral apex. A diagnostic arthroscopy is
performed to visualize all damaged structures. The Bankart lesion
classically presents as an avulsion of the labrum from the 3 o’clock to
approximately the 6 o’clock position. The labrum must be carefully
inspected circumferentially, however, as superior labral tears are
commonly seen in association with an anteroinferior labral avulsion.
The status of the biceps and rotator cuff are also carefully inspected.
The posterior aspect of the humeral head is carefully evaluated for the
presence of the Hills-Sachs lesion. The anterior labrum is often healed
along the anterior neck of the glenoid and may not therefore be
visualized on initial arthroscopic inspection. Presence of the ALPSA
lesion can be confirmed by looking at the anterior glenoid neck through
one of the anterior portals. An arthroscopic elevator is placed through
the more superior medial portal while the surgeon views from posterior,
and the displaced labrum is then elevated sharply off the anterior neck
of the glenoid. This will allow the labrum to float laterally and lie
adjacent to the rim of the glenoid. A 5.5-mm full-radius resector is
then used to debride the anterior glenoid neck down to bleeding bone.
This creates a good healing surface for labral repair.
using 3-mm bioabsorbable suture anchors. Two or three suture anchors
are typically used at the 5 o’clock, 4 o’clock, and 3 o’clock positions
along the anteroinferior glenoid rim. Metal suture anchors are also
acceptable.
rim of the glenoid to re-establish the anteroinferior “bumper” and
deepen the socket to increase the concavity compression effect of the
shoulder.13 To achieve this, anchors
must be placed either on the apex of the glenoid rim or slightly onto
the face of the glenoid. Anchor placement on the anterior glenoid neck
will not allow the labrum to be repaired to its anatomic position and
may result in recurrent instability postoperatively.9
Just as in the open Bankart repair, a superior shift of the labral
tissues is desirable during repair. A traction suture through the
labrum will assist in achieving this shift prior to placement of suture
anchors. This technique described by Boileau and Ahrens24
consists of passing a traction suture through the labrum via the
superior portal using either a Caspari-type punch or a suture shuttle.
This suture is then placed outside the superior medial cannula and is
used as a traction suture to pull the labrum superiorly. This allows
the suture shuttle to pass sutures from the anchors more inferiorly
through the labrum. If significant capsular laxity is noted along with
the Bankart lesion, more
capsule
can be grasped with the suture shuttle to create a shift of tissue
medially and superiorly while simultaneously making the labrum more
bulky by the addition of capsular tissue. Specific guidelines for the
amount of shift of capsular tissues needed during arthroscopic repair
are not as well defined as they are for open inferior capsular shift.
The surgeon can view inferiorly while tension is applied to the
traction suture to determine how much of a shift is needed to
obliterate the inferior pouch. There are no reports available to judge
the efficacy of this technique. The first anchor is placed at the 5
o’clock position directly onto the rim of the glenoid via the more
inferior-lateral cannula. The drill cannula is tapped with the mallet
to secure its position on the rim of the glenoid. The drill hole is
made to the depth of the drill stop, and the 3-mm bioabsorbable anchor
is tapped into place. One suture limb is then grasped and retrieved out
the anteromedial cannula. A 90-degree cannulated suture hook is then
placed through the more anteromedial cannula and is used to pass a
suture shuttle through the labrum inferior to the position of the
suture anchor while tension is applied via the traction suture. This
shuttle is retrieved using a suture grasper via the more inferior
lateral portal and is used to pass the one suture limb in that cannula
back through the labrum (Fig. 35-4).
One suture limb then passes directly from the anchor out through the
superior cannula while the second suture limb passes through the labrum
and out through the superior cannula. The labrum can now be secured at
this location using a sliding knot. This sliding knot is best tied via
the more inferior lateral portal as it is in line with the anchor. The
post of the sliding knot is the suture limb passing through the labrum
itself as this will more reliably keep the knot off the articular
surfaces (Fig. 35-5). Suture anchors are now
placed at the 4 o’clock and 3 o’clock positions, and these steps are
repeated to create a bumper of labrum along the anteroinferior glenoid
rim (Fig. 35-6). The normal sublabral foramen
superior to the 3 o’clock position should not be closed as this will
not enhance the repair and will lead to a loss of external rotation.
The most difficult anchor to place and suture to pass is the first. The
next two suture anchors are relatively straightforward.
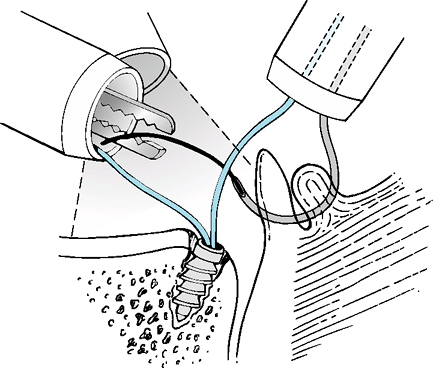 |
|
Figure 35-4
A 90-degree curved suture hook is used to pass a shuttle through the labrum and a portion of capsule. The suture limb from the anchor can then be transported through the labrum. |
 |
|
Figure 35-5
The three-portal technique of arthroscopic Bankart repair. The arthroscopic anchor is placed at the 5 o’clock position via the more inferior and lateral of the anterior portals. The suture shuttle is used to pass one limb of suture from the suture anchor through the labrum. Notice the traction suture pulling the labrum superiorly to facilitate a superior shift of the labrum and capsule. |
is noted, an additional anchor can be placed at the 1 o’clock position
easily through these two cannulas. The surgeon must be cautious in
placing the 1 o’clock anchor because the most superior cannula is
relatively medial and the drill must be aimed medially to avoid
penetrating the glenoid face. Again, one suture limb can be pulled out
the inferior cannula. A bird-beak tissue penetrator can be passed
through the superior cannula and through the labrum grasping the suture
limb that is passing out the inferior cannula. This suture is then
pulled back through the labrum, and a sliding knot is again used for
repair. The 11 o’clock suture anchor posterosuperiorly can usually be
reached using the aforementioned cannulae. If not, a midlateral portal
can be established using a spinal needle as a guide, and a 5-mm working
cannula is placed directly through the rotator cuff to allow access to
the 11 o’clock position posterosuperiorly. The glenoid neck superiorly
in the area of the SLAP lesion is debrided
down
to bleeding bone. The 3-mm bioanchor is placed in a similar fashion to
the previous anchors. One suture limb is grasped out an anterior
portal. The 90-degree cannulated suture hook is placed through the
anteromedial cannula and is used to pass the suture shuttle through the
labrum just posterior to the biceps anchor. This shuttle is retrieved
out the midlateral cannula and is used to pass the suture through that
cannula through the labrum. Both sutures are retrieved out the
midlateral cannula, and a sliding knot (using the suture limb through
the labrum as the post) is used to secure the labrum.
|
TABLE 35-1 Postoperative Rehabilitation Following Open and Arthroscopic Instability Repair
|
||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||
 |
|
Figure 35-6
The final repair with arthroscopic Bankart repair showing suture anchors at the 3 o’clock, 4 o’clock, and 5 o’clock positions re-establishing a normal attachment for the inferior glenohumeral ligament and recreating an anatomic bumper. |
arthroscopic instability repair can begin an identical postoperative
rehabilitation program. The exception to this is the patient with true
multidirectional instability who had signs and symptoms of true
instability in all three directions preoperatively and who had an
extremely patulous capsule of questionable quality at the time of
surgery. That particular patient will benefit from a brace
postoperatively holding the arm in neutral rotation to protect both the
anterior and posterior capsule evenly and supporting the arm to avoid
inferior subluxation for the first 6 weeks following surgery. Patients
with instability this extreme rarely develop stiffness following
capsular reconstruction, and this type of delay will allow for more
scar tissue formation in the capsule.
repairs involves the detachment of the subscapularis tendon and the
subsequent need for its protection in the early postoperative period.
Protection of the capsular and labral repair in these two patient
groups, however, is identical and requires greater restrictions than
those typically needed for the protection of the subscapularis alone.
Following open repair, patients are cautioned for the first 6 weeks to
avoid lifting >5 pounds, avoid excessive external rotation outside
the treatment protocol, and avoid using the arm to get up from a seated
position. The act of pushing oneself up from a seated position with the
arm in the internally rotated position places significant stress on the
subscapularis and should be avoided during the first 6 weeks following
open surgery. Other than these few restrictions, the therapy protocol
is identical for both groups (Table 35-1).
and reported uniformly satisfactory results in a series of 40 patients
with multidirectional instability. A follow-up series of 100 additional
patients in 1990 revealed similar results.14 Pollock et al.25
demonstrated the versatility of this procedure with 94% excellent and
good results in a series of patients with unidirectional and
bidirectional instability. Multiple other authors have subsequently
shown the procedure’s reliability sometimes with slight modification in
technique.7,25,26,27,28,29,30
Good and excellent results are noted routinely in approximately 90% of
patients with recurrent instability ranging from 4% to 11%
postoperatively. Although 70% to 90% of athletes return to play
following open inferior capsular shift surgery, elite overhead athletes
have only about a 50% chance to return to play at the same level.
suture anchors have demonstrated results equal to open techniques and
are laying to rest the notion that arthroscopic techniques are
unreliable for instability surgery.16 Although older techniques using bioabsorbable tacks and transglenoid techniques were not as reliable as open Bankart repair,31 newer series reporting on suture anchor techniques routinely demonstrate good and excellent results between 91% and 95%.4,8,12,32,33,34 Fabricciani et al.16
reported no recurrences in a prospective series of 60 patients, half of
whom were treated with open Bankart repair while the other half were
treated arthroscopically. Better final range of motion was noted in the
arthroscopic group, supporting one of the major theoretical advantages
of this arthroscopic technique. Recurrent instability has been reported
ranging from 0% to 11% with this arthroscopic technique. Return to
sports ranges between 74% and 100%,4,12,32,33
but overhead athletes still have more difficulty in returning to sport
at the same level of play, with results between 55% and 68% reported.4,33 Glenoid bony defects greater than 25% to 30% remain a significant cause of failure9,11,12 and are an indication for open repair and bone grafting.
traumatic unidirectional instability, usually associated with labral
pathology such as a Bankart lesion, and atraumatic multidirectional
instability, usually associated with capsular laxity. Glenohumeral
instability is a spectrum with significant overlap in presentation and
pathologic lesions contributing to the problem. The surgeon must be
able to identify all pathoanatomy contributing to the instability
through a careful preoperative and intraoperative evaluation. Surgery
is reserved for failure of conservative management, but when performed,
should address all pathology contributing to the instability. The
capabilities of arthroscopy are expanding continuously, and current
arthroscopic techniques have been proven equal to open techniques for
Bankart repair, the usual lesion of traumatic instability. Inferior
capsular shift enjoys similar success in treating the usual lesions of
atraumatic instability, a patulous capsule, and widened rotator
interval. Successful management with arthroscopic or open procedures
depends on identification of pathology, adequate mobilization and
balanced repair of tissues, protection of the axillary nerve, and a
safe rehabilitation program that allows adequate healing time for the
repaired tissues. Current contraindications for the arthroscopic
technique include glenoid bone loss >25% and an inability to repair
capsular avulsions or defects. Each surgeon should use techniques with
which he or she feels comfortable to achieve the above stated goals for
successful management of either traumatic or atraumatic glenohumeral
instability.
EG, Kim TK, Park HB, et al. The effect of variation in definition on
the diagnosis of multidirectional instability of the shoulder. J Bone Joint Surg. 2003;85A:2138–2144.
CS II, Foster CR. Inferior capsular shift for inferior and
multidirectional instability of the shoulder: a preliminary report. J Bone Joint Surg. 1980;62A:897–908.
DW, Warren RF, Skyhar MJ, et al. T-plasty modification of the Bankart
procedure for multidirectional instability of the anterior and inferior
types. J Bone Joint Surg. 1991;73A:105–112
GM, Roddey TS, Hammerman SM. Arthroscopic treatment of bidirectional
glenohumeral instability: two-to five year follow up. J Shoulder Elbow Surg. 2001;10(1):28–36.
LF, Caspari RB, Savoie FH III. The arthroscopic treatment of
multidirectional shoulder instability: two-year results of a multiple
suture technique. Arthroscopy. 1997;13:418–425.
SS, DeBeer JF. Traumatic glenohumeral bone defects and their
relationship to failure of arthroscopic Bankart repairs: significance
of the inverted-pear glenoid and the humeral engaging Hill-Sachs
lesion. Arthroscopy. 2000;16:677–694.
K, Takiuchi T, Aoki M, et al. Labral shape after arthroscopic Bankart
repair: comparisons between the anchor and Caspari methods. Arthroscopy. 2005;21(2):194–199.
LU, Flatow EL. History, physical examination, and diagnostic
modalities. In: McGinty JB, Caspari RB, Jackson RW, et al., eds. Operative Arthroscopy. New York: Raven Press; 1991:453–464.
C, Milano G, Demontis A, et al. Arthroscopic vs. open treatment of
Bankart lesion of the shoulder: a prospective randomized study. J Bone Joint Surg Am. 2004;86A:2574.
VM, Sugalski MT, Levine WN, et al. Comparison of glenohumeral mechanics
following a capsular shift and anterior tightening. J Bone Joint Surg Am. 2005;87:1312–1322.
P, Ahrens P. The TOTS: a new technique to allow easy suture placement
and improve capsular shift in arthroscopic Bankart repair. Arthroscopy. 2003;19:672–677.
RG, Owens JM, Flatow EL, et al. Operative results of the inferior
capsular shift procedure for multidirectional instability of the
shoulder. J Bone Joint Surg Am. 2000;82A:919–928.
CH, Ogilvie-Harris DJ. Inferior capsular shift operation for
multidirectional instability of the shoulder in players of contact
sports. Br J Sports Med. 2002;36(4):190–294.
LU, Kurzweil PR, Schwartzbach CC, et al. Inferior capsular shift
procedure for anterior inferior shoulder instability in athletes. Am J Sports Med. 1994;22:578–284.
K, Spring BJ, Henderson JP. Inferior capsular shift procedure in
athletes with multidirectional instability based on isolated capsular
and ligamentous redundancy. Am J Sports Med. 2000;28(4):466–471.
KB, Smith AP, Romeo AA, et al. Open Bankart repair vs. arthroscopic
repair with transglenoid sutures or bioabsorbable tacks for recurrent
anterior instability of the shoulder: a meta-analysis. Am J Sports Med. 2004;32:1520–1527.
J, Maeda S, Takagi K. Arthroscopic Bankart repair using suture anchors
in athletes: patient selection and postoperative sports activity. Am J Sports Med. 2004;32:1899–1905.
W, Witt KA, Hackenberg L, et al. Results of suture anchor repair of
anteroinferior shoulder instability: a prospective clinical study of 85
shoulders. J Shoulder Elbow Surg. 2003;12:322–326.
