Staying Out of Trouble while Caring for the Pediatric Athlete
– Special Maladies and Concerns > 12 – Staying Out of Trouble while
Caring for the Pediatric Athlete
|
|
athlete. Although the conditions are not as grave as tumors, serious
infections, and trauma, the acute and overuse injuries that affect the
young active child are very common. Sports medicine, like much of
pediatric orthopaedics, is the treatment of low-energy trauma or
repetitive micro-trauma. Demographic evaluations now show that although
the total number of children involved in organized sports decreases as
the children get older, the intensity of the competition, and training
for that competition, increases—and with it, many injuries.1 Likewise, many adolescent athletes now focus on a single sport year round.
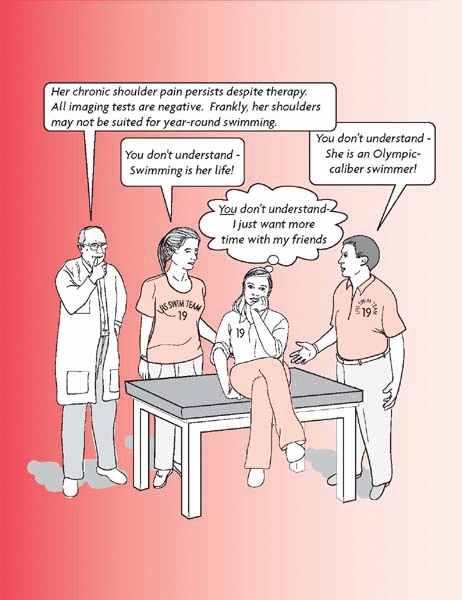
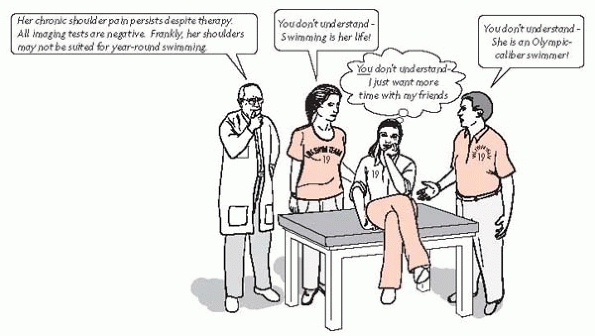
both clinical and psychosocial. The orthopaedic surgeon will have
frequent contact with the overzealous sports parent. Managing these
interactions is a key to staying out of trouble.
Sometimes, such a scenario is the true cause of swimmers with shoulder
pain or gymnasts with back pain. Unfortunately, the higher the level of
the athlete, the more difficult such issues are to sort out.
 |
|
▪ FIGURE 12-1 The overbearing sports parents.
|
athletically. Supplemental vitamins and minerals for the pediatric
athletic are usually expensive and unnecessary. Children and
adolescents are at risk for heat injury and dehydration just as pro
athletes are, maybe more so. Children are less efficient at regulating
heat because they perspire less when they are hot. Children also make
more metabolic heat per body mass than do adults. As a team doctor, you
must be proactive in preventing heat injury. You can recommend and
enforce a policy that includes mandatory periodic water drinking,
cancellation or modification of practice in unsafe weather, and the
discouragement of weight loss through water loss (e.g., wrestlers).
Helmets should be removed when children are not in contact situations,
so heat loss can occur through the head. Daily weights may be done
before and after practice to monitor fluid loss.
athletes who are put in dangerous situations due to limited budgets.
You should also insist on proper fitting equipment that is in good
repair. Sports equipment and playing fields should be age and size
appropriate.
trouble for young athletes. Chances are very good that if you care for
many young athletes, you care for a population that is taking a
performance-enhancing substance.2 It
has been estimated that 10% to 20% of adolescent athletes (depending on
the sport) use some kind of performance-enhancing substance. Although
anabolic steroids are the most risky and have received the most
attention, creatine, diuretics, amphetamines and other stimulants can
also be problems.
athlete are fractures covered elsewhere in this text. This section
emphasizes the most commonly encountered pediatric athletic injuries,
with the focus on staying out of trouble as you help these young
athletes return to sports.
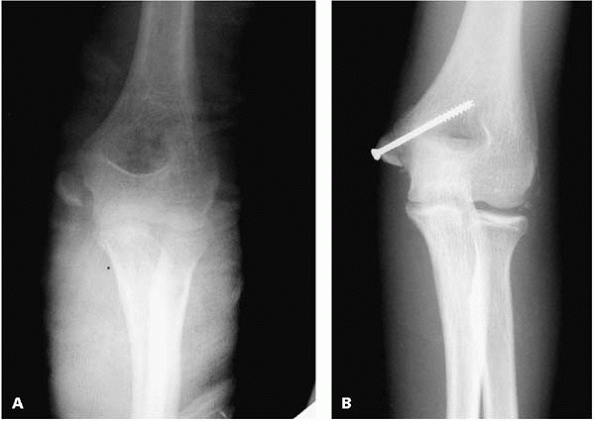
injuries in the pediatric athlete is the medial epicondyle fracture.
While the literature contains good evidence that these fractures can be
treated with or without reduction and fixation, operative treatment may
have value for athletes, especially if the throwing arm is injured or
there is an associated elbow dislocation. To avoid nonunion, refracture
or elbow stiffness, offer open reduction, screw fixation, and a short
period of immobilization (Fig. 12-2). Use a cast or a splint for a week or two, then therapy to regain full extension.
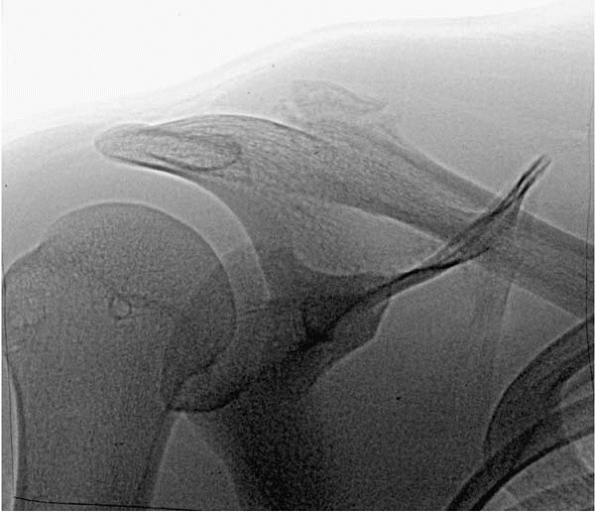
in adults. Unlike in adults, the ligaments are rarely disrupted.
Instead, the periosteum remains attached to the intact ligaments,
allowing excellent healing—sometimes so abundant that the
callus is mistaken for a tumor (Fig. 12-3). Avoid trouble by simply watching these injuries recover in the vast majority of children.
 |
|
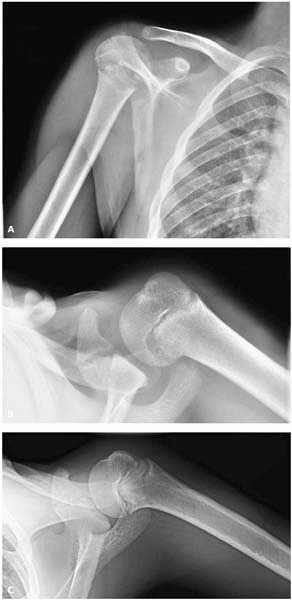
▪ FIGURE 12-2 A:
AP elbow radiograph of an elite gymnast who sustained an elbow dislocation (now reduced) and a medial epicondyle fracture with 1 cm of displacement. B: AP elbow after open reduction and internal fixation of the medial epicondyle fracture with an inter-fragmentary screw. |
trouble for the adolescent athlete. Regardless of immobilization and
rehabilitation, approximately 75% of teenagers will have a
redislocation.3 Although
controversial, surgical stabilization of a traumatic shoulder
dislocation after the first or second episode is being increasingly
recommended.
multidirectional shoulder instability is challenging. Many of these
children can dislocate their shoulders as a “party trick.” Staying out
of trouble with this population means avoiding surgery.4
There was a brief time when capsular shrinkage was attempted in this
group. The results were unsatisfactory and sometimes included reports
of injury to the axillary nerve. Surgery should not be offered for
multidirectional shoulder instability if possible. Swimmers often fall
into this category.
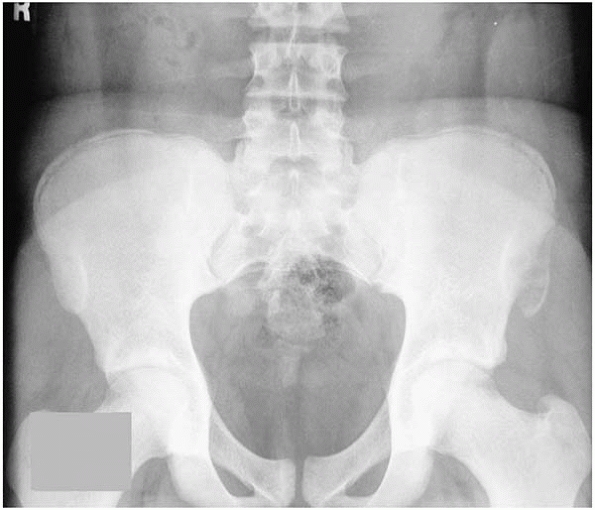
Sports commonly associated with this injury are soccer, gymnastics,
sprinting, hurdling, and jumping. The displacement of the fragment is
often an indication of the full extent of injury: the more displaced
the fragment, the more soft-tissue injury has occurred. The three types
of pelvic avulsion fractures that have the highest potential for
significant displacement are the iliopsoas from lesser trochanter, the
sartorius from the anterior superior iliac spine, and the hamstrings
from ischium. One of the most important principles in staying out of
trouble in the management of these injuries in young athletes is to
understand the importance of rehabilitation after the injury has
healed. If the athlete is permitted to return to play before motion and
strength are regained, reinjury is much more likely. Stay out of
trouble by explaining that most athletes will not be able to return to
sports for at least 4 to 6 weeks following one of these injuries.
Hamstring ischium avulsions are the only ones that seem to cause
persistent symptoms even after healing. Reattachment or resection is
occasionally beneficial.
 |
|
▪ FIGURE 12-3
This distal clavicle physeal fracture had so much associated bony callus that it presented as a concern for a shoulder tumor. (Case courtesy of C. Stanitski, MD.) |
 |
|
▪ FIGURE 12-4
Avulsion fracture of the left anterior superior iliac spine. These injuries can be easy to miss on plain radiographs or mistaken for some other process, thus they require a good understanding of the anatomic insertions of potentially avulsed muscle. Stay out of trouble by treating the young athlete, not the x-ray. |
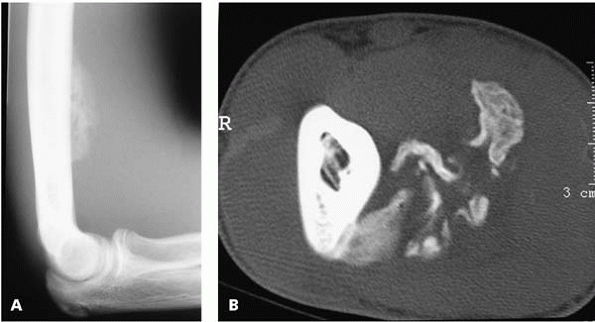
especially in soccer, lacrosse, and football players. Usually the
player will sustain a direct blow from another player’s knee, head,
stick, or some other piece of equipment. A key to managing this injury
is to be certain that the young athlete and family understand that
recovery can take several weeks. Allowing the child to return to play
too early can lead to increased bleeding in the compartments, making
the situation much worse. To stay out of trouble, it is important to
rule out another injury. The differential diagnosis of a painful
swollen thigh with calcification on x-ray includes tumors, infections,
fractures, and myositis ossificans. Remember that in contact sports
like football, a similar condition can occur in the arm (Fig. 12-5).
It is important to get good quality x-rays on the first presentation.
The treatment is rest, compression wrap, immobilization, and protective
weight bearing. When the athlete has regained active knee flexion of
90°, strengthening and conditioning can be gradually begun.
 |
|
▪ FIGURE 12-5 A:
Lateral elbow radiograph of a teenage football player who presented with pain and an enlarging anterior arm mass. Differential diagnosis included myositis ossificans vs. malignancy. B:This CT scan cut shows soft-tissue calcification that is mature at the periphery. The CT scan appearance is classic for myositis ossificans. (Case courtesy of J. Dormans, MD.) |
from a nondisplaced distal femoral physeal injury can be a source of
trouble. Although a short period of immobilization is satisfactory
treatment for both of these injuries, the real issue is followup:
distal femoral physeal fractures (Fig. 12-6)
should have late followup visits within the first year, while late
followup is unnecessary for a simple medial collateral ligament sprain.
adolescents are increasingly common and a potential important source of
trouble for the pediatric orthopaedists. An anterior cruciate ligament
injury should not be excluded just because the child is young. The
youngest reported anterior cruciate ligament disruption is 3 years of
age. Although an injury at this young age is extremely rare, anterior
cruciate ligament injuries are now being seen with increasing frequency
even in the 8- to 9-year-old age group. Remember that some
ACL-insufficient knees were born that way. If you encounter a child
with minimal knee trauma and instability on examination and a
hypoplastic tibial spine on x-ray, you may have found a congenital
problem, such as proximal focal femoral deficiency or fibular
hemimelia. A comparison radiograph of the opposite normal knee may be
helpful. The natural history is poor for children who sustain an ACL
disruption, are noncompliant with high-demand sports restrictions and
do not undergo reconstruction. There are a high percentage of such
children who sustain meniscal tears waiting for a reconstruction.7
 |
|
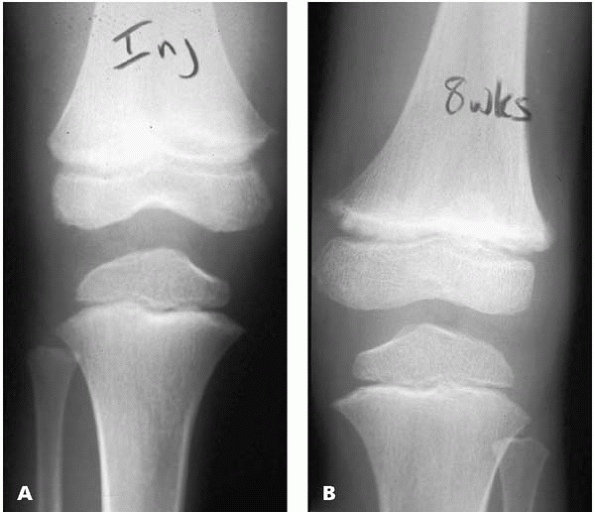
▪ FIGURE 12-6 A:
AP radiograph of the distal femur of a boy who presented to the sports medicine center with a “knee sprain.” He had a small knee effusion and tenderness at the distal femur both medially and laterally but no tenderness over the proximal tibia. Given his age and the physical exam findings, the orthopaedist was wise enough to suspect a physeal fracture and immobilize him for 4 weeks. B: This AP radiograph of the distal femur taken 8 weeks after injury shows widening of the physis consistent with a Salter Harris I or Salter Harris II distal femoral physeal fracture. |
 |
|
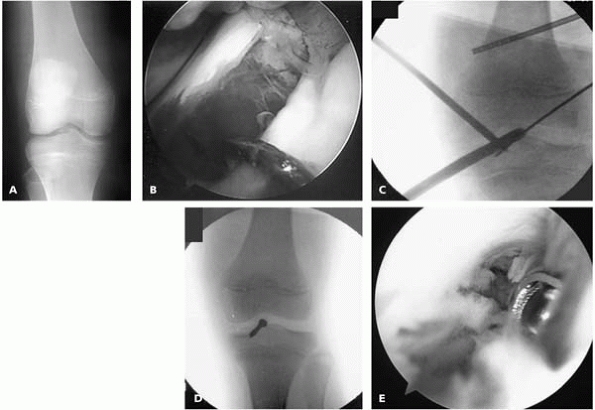
▪ FIGURE 12-7 A:
AP radiograph of another boy sent to the sports medicine center weeks after sustaining a “knee sprain.” The tibial spine fracture, evident as subtle fragmentation in the intercondylar notch, was missed by the initial treating physician. He had pain and motion loss. B: Arthroscopic view after best attempt at manual reduction. C: Intraoperative radiograph as the guidewire for a cannulated screw is being placed. D: Intraoperative radiograph after screw placement. E: Despite stable fixation and early mobilization, the boy developed debilitating arthrofibrosis. Arthrofibrosis can be a major source of trouble after treatment of tibial spine fractures. |
injury in a skeletally mature athlete means successfully stabilizing
the knee without causing a growth arrest.8,9
There are three types of reconstruction: physeal sparing, partial
transphyseal, and complete transphyseal. Most studies that have
reviewed adolescent ACL reconstruction focus on adolescents who are
very near skeletal maturity. There is not yet long-term data regarding
a large population of very skeletally immature patients who have had an
ACL reconstruction.
ligament reconstructions are due to errors in judgment (such as
inadequate physiologic age assessment) and/or technical errors such as
bone or hardware across the physis or direct damage to the lateral
femoral physis at the time of graft fixation.
Study Group documented 15 reported cases of growth disturbance: 8 cases
of distal femoral valgus deformity with arrest of the lateral distal
femoral physis, 3 cases of tibial recurvatum with arrest of the tibial
tubercle apophysis, 2 cases of genu valgum without arrest, and 2 cases
of leg length discrepancy. Associated factors included fixation
hardware across the lateral distal femoral physis in 3 cases, bone
plugs of a patellar tendon graft across the distal femoral physis in 3
cases, large (12 mm) tunnels in 2 cases, fixation hardware across the
tibial tubercle apophysis in 3 cases, lateral extraarticular tenodesis
in 2 cases, and over-thetop femoral position in 1 case. Based on this
experience, the authors recommended a guarded approach to ACL
reconstruction in the skeletally immature patient, with careful
attention to technique and followup.10
Children may sustain a partial tear of the ACL. If the child has a
skeletal age <14 years old and the knee is stable on Lachman
testing, nonoperative treatment is recommended.11
in adolescent athletes. The problem with false-positive MRIs in
pediatric meniscal evaluation has been well documented. A careful
physical examination, not MRI, is your best tool to avoid a diagnostic
error.12 The well-vascularized peripheral meniscus in a child can look like a torn meniscus to the uninitiated.
management of meniscal tears in children are neurovascular injury from
repair and meniscal implants.13 The risk to neurovascular structures during meniscal repair is well documented.14
To stay out of trouble the surgeon should use multiple closely spaced
nonabsorbable sutures, and then protect the child for a few weeks with
immobilization to ensure healing.
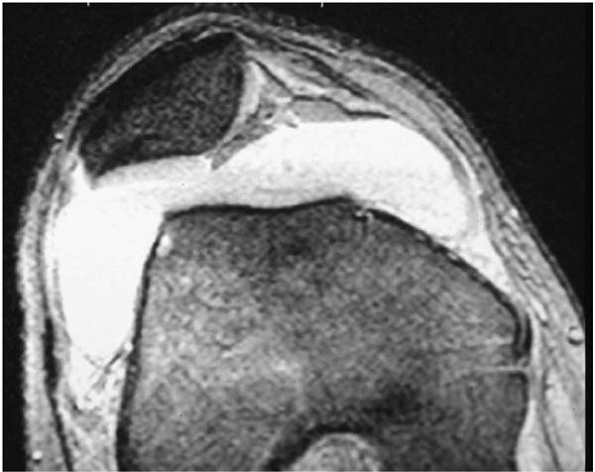
might suspect. It has been estimated that about 1% of all lateral
menisci are the discoid type. Certainly every toddler and young child
with a clicking knee does not need an MRI.
Sometimes plain radiographic findings, such as a wide lateral joint space, can be helpful in this population (Fig. 12-8).
-
Popliteus tendon instability
-
Tear of normal lateral meniscus
-
Iliac tibial band tendonitis
-
Proximal tibia/fibula joint instability
-
Osteochondritis dissecans
-
Loose body
-
Intraarticular loose body
-
Snapping hamstring tendon
 |
|
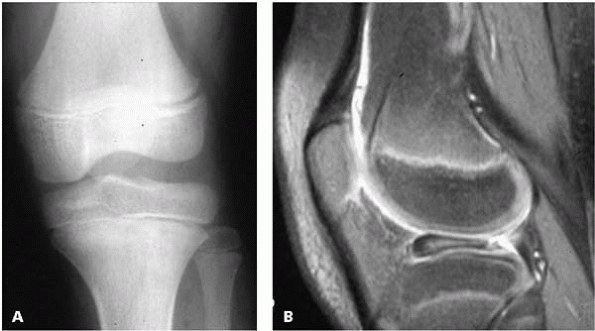
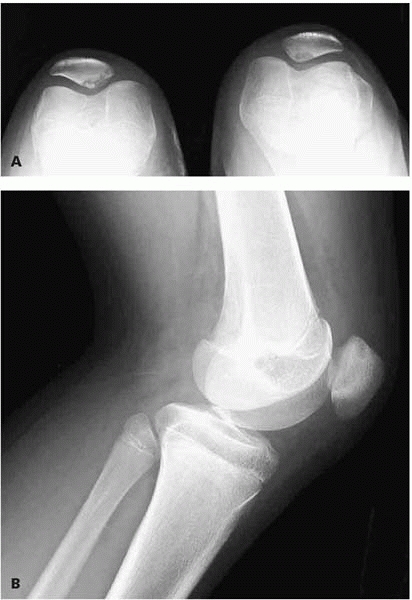
▪ FIGURE 12-8 A:
This AP radiograph of the knee in a girl with “clicking” shows widening of the lateral hemi-joint. The orthopaedist was suspicious for discoid meniscus. B: This sagittal MRI cut shows classic discoid meniscus with the bulk of the abnormal meniscus anterior. |
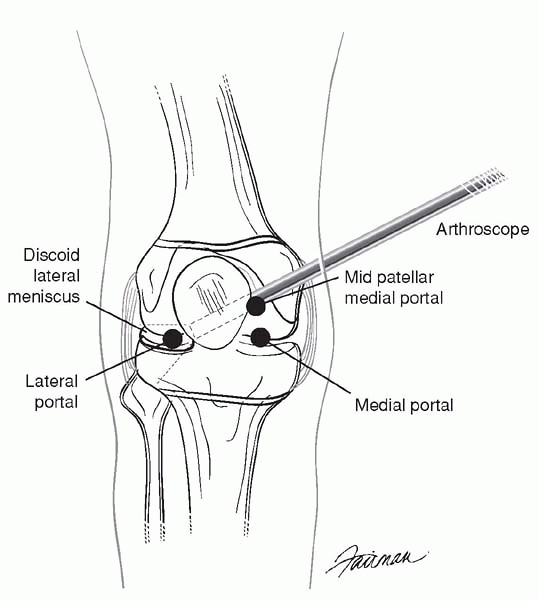
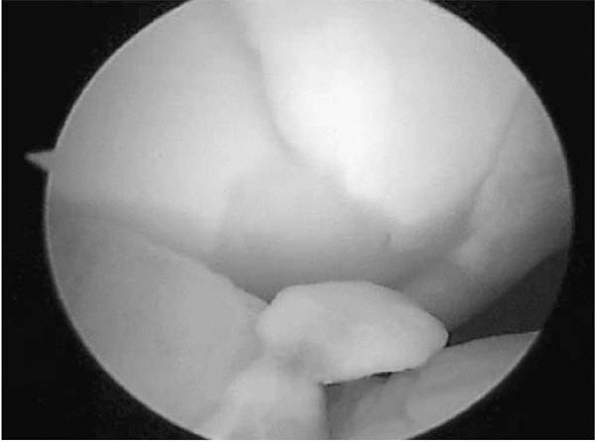
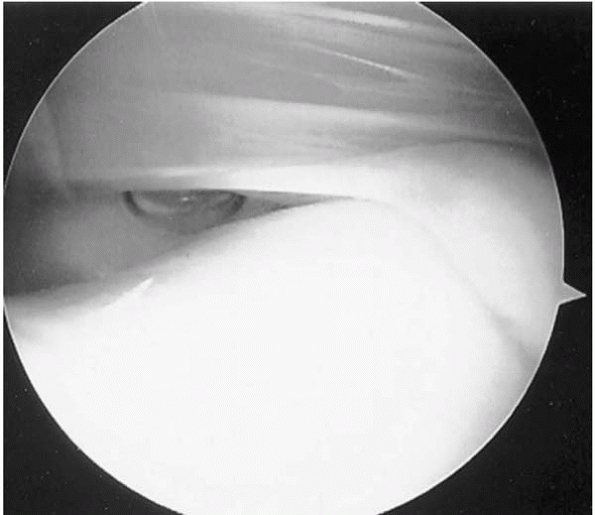
menisci includes appreciating the potential difficulty of arthroscopic
lateral meniscoplasty. The entire lateral compartment can be obscured
by the meniscus (Fig. 12-9). The arthroscopist should be comfortable using accessory arthroscopic portals to manage this difficult problem (Fig. 12-10).
 |
|
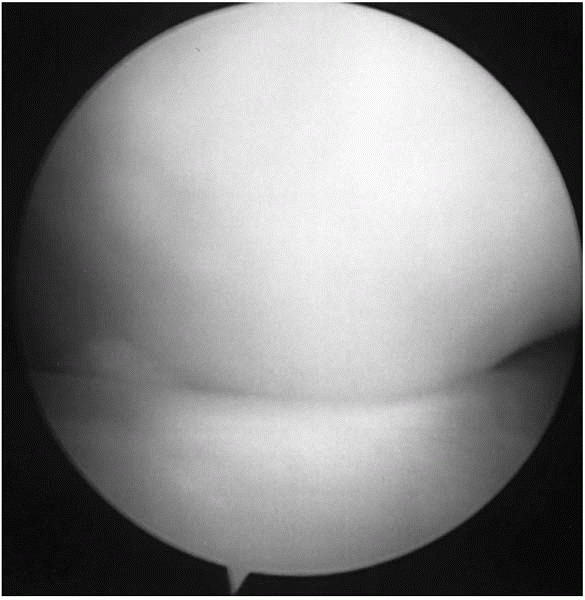
▪ FIGURE 12-9
This arthroscopic picture of the lateral compartment of the knee shows the “white wall of worry.” In some cases of discoid meniscus, the orthopaedic surgeon will immediately encounter the bulk of discoid lateral meniscus in the anterior aspect of the knee. This large amount of abnormal tissue completely blocks the ability to see and enter the lateral hemi-joint. For the uninitiated, this can be very difficult to work around. (Case courtesy of T. Ganley, MD.) |
 |
|
▪ FIGURE 12-10
This drawing shows the position of the medial mid-patellar portal, which is extremely valuable in discoid meniscoplasty. Use of the medial mid-patellar portal for the arthroscope allows optimal visualization of the discoid meniscus and room for working instruments in standard portals. |
for a visit to the pediatric sports medicine doctor. Complaints can be
either patellofemoral pain or instability, or both pain and instability.
patellofemoral pain syndrome a diagnosis of exclusion, being certain
that there is not some other problem causing pain around the knee.
rule out other causes of symptoms; to evaluate the patellofemoral
relationship a merchant view can be valuable, especially if it shows
malalignment. Don’t be fooled by views done with more knee flexion
(like the “sunrise view”). These views may give the mistaken impression
that the patella is centered in the trochlear groove. Patellofemoral
pain is much less common in boys. Stay out of trouble by looking for
other diagnoses in the male adolescent athlete. Most treatment for this
condition should be rehabilitation, particularly stretching and
strengthening of the quadriceps.
instability is a major source of trouble. After treatment, patients can
have persistence of their pain, recurrent instability, regional pain
syndrome, or a surgical complication.
differential diagnosis of anterior knee pain, either before or after
surgery. The primary complaint is out of proportion to the inciting
event. Early in the condition skin trophic changes are not present and
imaging changes are also lacking.
patellofemoral problems are beyond the scope of this text, a few
specific issues are worth mentioning. The surgeon should not detach the
vastus lateralis from the superior lateral pole of the patella. It is
very important to control bleeding during a lateral release or the
patient will develop a significant hemiarthrosis. Many surgeons prefer
a drain for 12 to 24 hours after a lateral release.
scenario is the child with malalignment or significant ligamentous
laxity, whose patellar dislocation happens with minimal trauma. Usually
there is little effusion or other injuries. Symptoms resolve rapidly,
there is rarely intraarticular damage, and the risk of recurrence is
very high (60% in some series).15 The second type is patellar dislocation in the strong, tight, well-aligned knee (Fig. 12-11). This group is usually
boys, the injury occurs with much more trauma, and there is an
associated effusion or hemiarthrosis and more pain. In these cases,
there are often intraarticular loose bodies—look for signs on plain
radiographs. An MRI may also be helpful.16 Intraarticular loose bodies can also be detected by arthroscopic means (Fig. 12-12).
 |
|
▪ FIGURE 12-11 This MR image shows attenuation of the medial patellofemoral ligament with a large effusion.
|
 |
|
▪ FIGURE 12-12 Arthroscopic evaluation after patellar dislocation revealed multiple loose bodies.
|
list when an adolescent athlete presents with a swollen knee.
Typically, the injury story may suggest an ACL injury. The possibility
of patellar dislocation should not be overlooked, as it is more common
than ACL disruption in children and adolescents. On examination, look
for tenderness along the medial retinaculum at the patellofemoral and
meniscopatellar ligaments. Initial radiographs should be scrutinized
closely to rule out an osteochondral injury or a loose body. To avoid
trouble when operating for recurrent patellar dislocation, be sure your
patient will cooperate with rehabilitation. Postoperative pain,
especially after tubercleplasty, can be substantial, hindering
essential rehabilitation. Also, do not plan a surgical procedure on the
tibial tubercle if the physis is still open. In younger children growth
arrest can lead to recurvatum of the knee.
also the source of trouble for both adolescent athletes and their
doctors. Plicae can be a great imitator, causing anterior knee pain
like many other intraarticular problems. Plicae should be a diagnosis
of exclusion. The surgeon should search out all other
problems—particularly patellofemoral problems or meniscal pathology—
before deciding that the plica is the problem (Fig. 12-13).
arthroscopy, completely resect it. Otherwise, the operation will lead
to more scarring, adhesions, and problems. Be certain to do a very
thorough diagnostic arthroscopy and rule out any other pathology before
shaving the plica.
anterior knee pain differential. It is usually seen in the female
adolescent athlete, often after a direct blow to the anterior knee, or
after repetitive floor or mat contact activities in sports such as
volleyball, wrestling and gymnastics. Diagnosis can be made by
detecting pain over the fat pad at the terminal part of passive
extension. The key to staying out
of
trouble with Hoffa syndrome is to persist with nonoperative measures:
don’t do an arthroscopic resection of a normal-looking fat pad.
 |
|
▪ FIGURE 12-13
Staying out of trouble with plica means knowing which ones will benefit from surgical resection. Arthroscopic view of a plica that is substantial in size and notching the articular cartilage of the femoral condyle. |
misdiagnosis or overtreatment. The vast majority of children who
present with a popliteal mass will have a classic popliteal cyst, which
requires no treatment other than observation. Although soft-tissue
sarcomas are rare, they can occur in this area and should not be
dismissed as a Baker cyst.17 If the
cyst is soft, in the classic location, and appears fluid-filled by
transillumination, observation is warranted. If the cyst is in an
unusual location or is firm or does not transilluminate, an ultrasound
is a simple, relatively inexpensive, noninvasive way to confirm the
diagnosis. If ultrasound does not show the classic fluid-filled cyst,
MRI may be valuable to stay out of trouble. Another source of trouble
with popliteal cysts is overtreatment. Families should be counseled
that these cysts will generally resolve in children, but resolution may
take several years. The popliteal cysts should not be routinely
resected— observation is recommended as most will resolve or become
smaller and asymptomatic.18 After
resection, scarring and soft-tissue problems can be significant, and
neurovascular structures can be at risk with misguided surgery.
Finally, the recurrence rate of these cysts can be over 70%, which is
discouraging to all involved.
most recover with short periods of rest. Loss of full extension, or
persistent swelling of the elbow, may indicate more serious trouble;
radiographs are indicated to assess the joint. Management of these
problems generally involves striking a delicate balance between proper
rest and rehabilitation and rapid return to sports (Fig. 12-14).
extremity pain in children, they must be on the differential diagnostic
list when a young athlete presents with activity-related pain.19 The tibia is one of the most common sites of stress fractures in children (Fig. 12-15).
Tumors and infections share some presenting features with stress
fractures: however, most stress fractures cause pain primarily
with activity, while tumors and other conditions can cause pain at rest or during the night.
 |
|
▪ FIGURE 12-14
Inability to extend the arm or persistent swelling are good reasons to get radiographs when evaluating a young throwing athlete. This AP radiograph of the elbow is of a 14-year-old pitcher told repeatedly by his coach and pediatrician that he had little league elbow. No prior radiographs were taken. He was told only to “stop throwing curveballs.” He now presented after feeling a pop while pitching. The radiograph shows a medial epicondyle stress fracture. It was fixed with an interfragment screw (as in Fig. 12-2). |
stress fracture: healing bone may have a histologic appearance that can
be difficult to distinguish from malignant bone; further, the biopsy
can become a stress riser, leading to a complete fracture.
Be sure to rule out more common causes, such as slipped capital femoral
epiphysis (SCFE).20 An MRI will help
distinguish a femoral neck stress fracture from a very mild SCFE. More
aggressive treatment is usually needed for adolescent femoral neck
stress fractures, especially on the tension side. Completion of the
fracture and displacement can lead to avascular necrosis (AVN).
 |
|
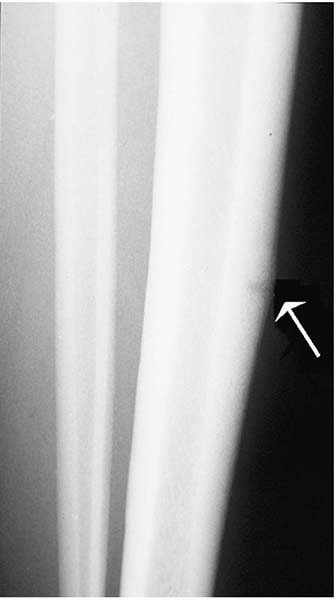
▪ FIGURE 12-15 “The dreaded black line” (arrow).
This teenage runner was treated for bad shin splints that would not get better. Eventually she presented to the orthopaedist and was diagnosed with a tibial stress fracture. Although the two can be difficult to distinguish, this girl had very dramatic point tenderness localized to the anterior tibia, rather than diffuse medial tibial pain. |
stress injuries. Distal radial epiphysiolysis occurs in gymnasts, and
they do not have to be Olympic caliber to get into trouble.21
Symptoms can take a very long time to improve, but complete resolution
is possible with sufficient rest. Proximal humeral epiphysiolysis
(“little league shoulder”) should be in the differential diagnosis of
shoulder pain in young pitchers (Fig. 12-16).
Comparison side-to-side radiographs of the shoulder are helpful.
Usually only minimal widening of the lateral portion of the physis is
seen. This injury generally resolves without long-term problems,
although getting the young pitcher to rest can be quite difficult. The
differential diagnosis of shoulder pain in the adolescent athlete
should include epiphysiolysis, unicameral bone cyst or other bone
tumors, rotator cuff tendonitis, acromioclavicular joint injury, and
shoulder instability.
source of trouble. Children younger than 9 years old tend to undergo
ossification changes, also known as Panner disease. Older children may
develop a true osteochondral of the capitellum lesion, which can be a
potentially career-ending injury for a pitcher. Loss of elbow extension
is an important sign of trouble when a young pitcher presents with
elbow pain. Good quality plain radiographs of the elbow should be
obtained. An MRI may be valuable in older children. To stay out of
trouble, it is important to warn parents that the prognosis to return
to full pitching is limited in children with true osteochondritis
dissecans of the capitellum, especially if they need a debridement or
other surgery.
 |
|
▪ FIGURE 12-16
Humeral epiphysiolysis in a 13-year-old pitcher. Mom said that her son was so good that she had him pitching in 3 different leagues. A,B: Views of the right proximal humerus at presentation. He had significant shoulder pain. There is widening of the physis consistent with proximal humeral epiphysiolysis. C: This lateral image of the proximal humerus after 6 months of rest shows that the physeal appearance has returned to normal. |
different types of apophysitis. Hip pain in an adolescent athlete may
be due to apophysitis, but it is important to rule out other causes of
local pain. SCFE, femoral neck stress fractures, or other bone lesions
should be sought. Obtain good quality radiographs of the hips and
pelvis when a child presents with a suspected apophysitis. As mentioned
earlier in the section on avulsion fractures, rehabilitation is
important to prevent recurrent symptoms.
knee: Osgood-Schlatter lesion (OS), Sinding-Larsen-Johansson (SLJ),
osteochondritis dissecans, and popliteus tendonitis. OS lesion is an
exceedingly common diagnosis for the pediatric sports medicine doctor.
To stay out of trouble in its management, it is important to eliminate
rare but serious bony lesions around the knee, and understand the
pathophysiology so that rapid rehabilitation can be performed and the
child does not suffer through unnecessarily long periods of rest and
activity restriction.
radiographs in unilateral cases. OS occurs at the same age and region
as osteosarcoma (Fig. 12-17). If there is
sudden pain, be sure there is not an acute tibial tubercle avulsion
fracture. The key to rescuing children from their OS pain is to
emphasize quadriceps flexibility. Most children who present with OS
have recently gone through a period of rapid growth and have
significant quadriceps and hamstring contractures. Restoring
flexibility through good stretching exercises is essential. Icing the
inflamed
tibial tubercle and doing effective quadriceps and hamstring stretching
exercises will lead to pain relief in the vast majority of children.
The best way to stay out of never-ending circular arguments regarding
activity restriction is to recommend that children be allowed to do any
activities unless they are limping on the field. If they limp, they are
out for the rest of that day’s game or practice. If they limp for two
days in a row, they are out for a week. Another key to staying out of
trouble with OS is to avoid casting. Although casting will give the
knee a rest, it just leads to more atrophy and contracture at the
quadriceps, thus aggravating the underlying cause and assuring
recurrence upon return to sports.
 |
|
▪ FIGURE 12-17
This 14-year-old boy presented with pain over his tibial tubercle. In many ways his symptoms were classic for Osgood-Schlatter. Fortunately, the orthopaedist obtained knee x-rays, which demonstrated a destructive process in the proximal tibia. The biopsy: osteosarcoma. (Case courtesy of J. Dormans, MD.) |
pole of the patella. The pathophysiology is very similar to OS; most of
these young athletes also have a quadriceps contracture and an overuse
injury. To stay out of trouble, it is important to clarify the
difference between SLJ and a true patellar sleeve fracture. Just
because a child will not do active extension does not mean that the
extensor mechanism is disrupted (Fig. 12-18).
 |
|
▪ FIGURE 12-18
This lateral knee radiograph is of a 9-year-old girl who presented with anterior knee pain and swelling after a fall. She would not voluntarily extend her knee and could not hold it extended against gravity. The surgeon diagnosed a patellar sleeve fracture and rushed her to the OR. At surgery, her extensor mechanism was found to be intact—final diagnosis was Sinding-Larsen-Johannson syndrome. |
an important problem in the pediatric athlete. There are often months
or years of low-level symptoms in these patients. Be certain not to
mistake physiologic ossification variances of the distal femoral
epiphysis for OCD. On examination, quadriceps atrophy may be the only
finding.
joints to see if there is a more generalized disorder of epiphysis
ossification. To stay out of trouble, be on the lookout for truly
unstable OCD lesions that have a poor prognosis.22 OCD lesions in unusual locations, like the patella (Fig. 12-19),
are also trouble. If an effusion is present or the child has mechanical
symptoms, much more aggressive treatment is warranted.
in predicting whether you might encounter a flap lesion or an unstable
lesion, both of which have a low likelihood of healing. Bone
scans
may be accurate in predicting healing in juvenile lesions but not in
adolescent lesions. To stay out of trouble, understand that with
increasing age, time for resolution is diminished and surgical
intervention is much more likely to be necessary (Fig. 12-20).
 |
|
▪ FIGURE 12-19 Bilateral merchant (A) and lateral views (B)
of the knee showing patellar OCD. These are trouble—much more difficult to “cure” than juvenile OCD lesions in the typical location on the distal femoral condyle. |
knee that is usually seen in running athletes who train on hills or
banked roads. Obtain knee radiographs at presentation to rule out bone
lesions. Popliteus tendonitis often presents as lateral joint line
pain. Pain can be elicited by placing the involved leg in a
figure-of-four position, with tibial internal rotation.
-
Popliteus tendonitis
-
Discoid meniscus
-
Iliotibial band tendonitis
-
Lateral meniscus tear
-
Proximal tibia fibula joint pain
-
Hamstring tendonitis
knee pain in the adolescent athlete. The main trouble with this
condition is a diagnostic error. The patient is point tender where the
nerve exits Hunter’s canal. The patient often will have a positive
Tinel sign along the course of the nerve. Localized injection of
lidocaine can be helpful in the diagnosis.
lower extremity pain in runners. Compartment contents expand with
exercise and cause pain, but rarely
result
in muscle necrosis. Pain typically develops after a specific duration
of exercise. This pattern contrasts with the symptoms in a stress
fracture, in which pain occurs early and intensifies with use. The most
commonly involved compartment is the anterior compartment. To stay out
of trouble, don’t do a unilateral compartment release if there are any
symptoms on the contralateral side (if you do, after the first release,
the runner will feel much better and push her activity up to the point
where she has symptoms on the opposite side).
 |
|
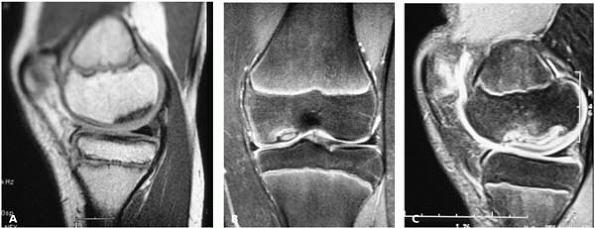
▪ FIGURE 12-20 The good, the bad, and the ugly of OCD lesions of the distal femur. Stay out of trouble by recognizing the difference. A:
The good (probably will heal with immobilization). This sagittal image shows that the articular surface is completely intact. There is no effusion and the lesion is not marginated. B: The articular surface is intact but the lesion is marginated and the child is approaching skeletal maturity. Drill and pray. C: In this case the articular surface is disrupted and the lesion is partially detached. Major trouble—prepare the family for more than one operation. |
-
Stress fracture
-
Sciatica
-
Tumor
-
Infection
-
Chronic compartment syndrome
-
Muscle herniation thru a fascial defect
problem, should be in the differential diagnosis of a runner with lower
extremity pain. Look for a lower extremity malalignment, especially
knee varus. To stay out of trouble, stick to rehabilitation and avoid
surgical management. Release of the iliotibial band or bursa excision
is rarely indicated and often does not give the kind of pain relief the
young athlete expects.
young athletes. To stay out of trouble, be certain the diagnosis is
correct. Good quality radiographs are recommended for heel pain
(especially unilateral heel pain) to rule out bone cysts, acute
fractures and other conditions. Recent evidence suggests that at least
some cases may be calcaneal stress fractures.24
Staying out of trouble also means understanding that the calcaneal
apophysis in a school-age child usually has an “injured” appearance:
sclerotic, fragmented, or cracked. Sometimes it is hard to convince
parents that there is not an injury in this area. The essential
elements of managing Sever’s apophysitis include relative rest from
high-impact activities, stretching a tight gastrocsoleus muscle, and
counseling the family about proper shoes. Many children with Sever’s
apophysitis are running on hard surfaces in cleated shoes. A turf shoe,
true running or silicone heel pad shoe often gives much relief.
Recommend the same guidelines for return to play described above for
Osgood-Schlatter—limping from Sever’s apophysitis gets the child pulled
out of the game or practice.
-
Identify the
overzealous sports parent, and the occasional burned-out child
athlete—don’t let them get in the way of making sound recommendations. -
Just like in the pros, the high school team physician should be on the lookout for performance-enhancing substance use.
-
Consider fixing
medial epicondyle fractures in athletes, especially if there has been
an associated elbow dislocation—you will want to move them quickly. -
Avoid surgery on the ligamentously lax, habitual shoulder dislocator.
-
After severe quadriceps contusion, discourage return to play until ROM and strength equal the uninjured side.
-
Consider distal femoral physeal injury when you diagnose MCL sprain.
-
A hemarthrosis of the knee suggests high likelihood of significant injury.
-
Children and
adolescents should have their ACL reconstructed. If they are too young,
restrict activity and brace until the physes are closing. -
In ACL reconstruction, never put bone or hardware across a growing physis.
-
Discoid
meniscoplasty can be a very challenging arthroscopy. Be prepared for
extra portals, extra time, and the need for suture stabilization
(repair).
-
In overuse injuries around the elbow, loss of full extension is a worrisome sign. Get radiographs.
-
Knee pain is referred from the hip until proven otherwise. Examine the hips in every case of knee pain.
-
Obtain plain
radiographs of the knee in most adolescents who present with knee pain.
A tumor or infection is much less frequent than an Osgood-Schlatter
lesion, but a disaster to miss. -
For extensor
mechanism overuse injuries (OS, SLJ), focus on relative rest and
quadriceps and hamstring flexibility, not immobilization and a total
ban from all sports.
PJ, Willis AA, Warren RF. Associated injuries in pediatric and
adolescent anterior cruciate ligament tears: does a delay in treatment
increase the risk of meniscal tear? Arthroscopy. 2002;18(9):955-959.
KG, Apel PJ, Pfeiffer RP. Anterior cruciate ligament injury in
paediatric and adolescent patients: a review of basic science and
clinical research. Sports Med. 2003;33(6):455-471.
MS, Saxon HS, Hovis WD, et al. Management and complications of anterior
cruciate ligament injuries in skeletally immature patients: survey of
the Herodicus Society and the ACL Study Group. J Pediatr Orthop. 2002;22(4):452-457.
CL. Correlation of arthroscopic and clinical examinations with magnetic
resonance imaging findings of injured knees in children and
adolescents. Am J Sports Med. 1998;26(1):2-6.
KA, Greene PW III, Shirkhoda A. Peroneal nerve dysfunction as a
complication of lateral meniscus repair: a case report and anatomic
dissection. Arthroscopy. 1989;5(2):141-147.
CL, Paletta GA Jr. Articular cartilage injury with acute patellar
dislocation in adolescents. Arthroscopic and radiographic correlation. Am J Sports Med. 1998;26(1):52-55.
JP, Puffer JC, Mandelbaum BR, et al. Distal radial growth plate injury
and positive ulnar variance in nonelite gymnasts. Am J Sports Med. 1997;25(6):763-768.
SG, Ganley TJ, Milam RA, et al. Role of magnetic resonance imaging and
clinical criteria in predicting successful nonoperative treatment of
osteochondritis dissecans in children. J Pediatr Orthop. 2003;23(1):102-108.