Single Thoracic Paravertebral Block
II – Single-Injection Peripheral Blocks > C – Miscellaneous Blocks
> 22 – Single Thoracic Paravertebral Block
The paravertebral space is a wedge-shaped space on either side of the
vertebral column. Boundaries: anteriorly—parietal pleura;
medially—vertebral body, intervertebral discs, and intervertebral
foramen; posteriorly—superior costotransverse ligament. The spinous
process is the main bony landmark for this block.
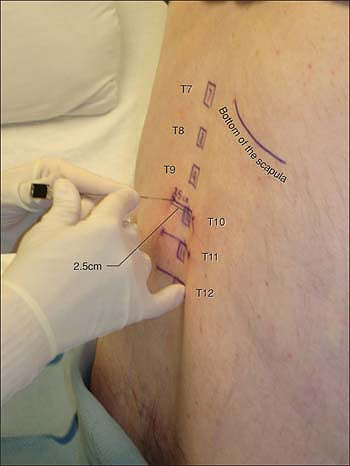
The spinous processes are palpated and marked with the skin marker. The
insertion points are marked 2.5 cm lateral to the superior border of
the spinal process and infiltrated with local anesthetic. Then the
Tuohy needle is placed perpendicular to the skin with bevel up and
advanced up to 3 to 5 cm (Fig. 22-1).
When the transverse process is found, the needle is pulled back to the
skin and redirected caudally to walk off the inferior aspect or the
transverse process, and is then advanced 1.0 cm past the premeasured
skin-to-bone distance until a “pop” through the superior
costotransverse ligament is appreciated. After the stylet is removed
from the needle, the syringe with 0.5% ropivacaine is connected to the
needle by extension tubing.
 |
|
Figure 22-1. The Tuohy needle is placed perpendicular to the skin with bevel up and advanced up to 3 to 5 cm.
|
-
Inferior angles of the scapulae are used to localize the spinous process of T7 vertebra.
-
Local anesthesia is performed with two
passes of the needle: one perpendicular to the skin (the transverse
process can be contacted in thinner patients), then pull the needle
back, redirect it caudally, and inject more along the pass to the
paravertebral space. -
Do not deviate from the parasagittal
plane to avoid medial spread and neuroaxial block (postdural puncture
headache has been reported after a paravertebral block). -
If the needle is redirected caudally and
contacts the bone at a shallow distance, reinsert the needle 0.5 cm
caudally. (First time was too cephalad and found the rib, instead of
the transverse process.) -
Too much resistance on injection suggests wrong needle position.
-
It is not uncommon to see
hypotension/bradycardia episodes with this technique in sitting
position. Safe practice requires minimal monitoring with noninvasive
blood pressure cuff and pulse oxymeter, reliable intravenous access,
and supplemental oxygen via nasal cannula. Glycopyrrolate 0.2 mg and
ephedrine 50 mg should be always available for treatment. After the
episode, extended vital signs monitoring and report to room nurse are
recommended.
Ga, Kahn RL, Gordon J, Gordon MA, Urban MK. The use of metoprolol and
glycopyrrolate to prevent hypotensive/bradycardic events during
shoulder arthroscopy in the sitting position under interscalene block. Anesth Analg 1998;87:1320–1325.
MZ, Ziade MF, Lonnqvist PA. General anesthesia combined with bilateral
paravertebral blockade (T5-6) vs. general anesthesia for laparoscopic
cholecystectomy: a prospective randomized trial. Eur J Anaesthesiol 2004;21:489–495.
T, den S, Cheema SPS, et al. A single injection, multisegmental
paravertebral block-extension of somatosensory and sympathetic block in
volunteers. Acta Anesthesiol Scandi 2001;45:30–33.
The paravertebral space is triangular in shape and bound medially by
the contiguous epidural space via the intervertebral foramen. The
posterior wall of the paravertebral space is made up of the anterior
costotransverse ligament. The anterior costotransverse ligament extends
between the rib and transverse process in the thoracic region. The
intercostal nerves and vessels are located in front of the ligament.
The anterior and lateral borders of the paravertebral space are defined
by the parietal pleura.
The superior aspect of the iliac crest is identified and a line is
drawn to identify the spinous process of L4. Counting in a cephalad
direction from L4, T11 and L2 are identified. The site of introduction
of the needle is marked 2.5 cm lateral to the superior aspect of their
respective spinous processes. Next, the skin is cleaned with
chlorhexidine. This is followed by a local anesthesia with 5 ml
lidocaine 1% at T11 and L2. A 22-gauge insulated needle attached to a
nerve stimulator (3 to 5 mA, 2 Hz, 1.0 ms) is advanced in a
posterior-anterior direction approximately 10° to 20° lateral until it
touches the transverse process, or a stimulation of the external and
internal oblique muscles, the transverse abdominal muscles, and the
rectus abdominis is elicited. If the transverse process is contacted,
the needle is “walked off” caudad at T11 and cephalad at L2 and
advanced until the proper stimulation is elicited. After correct
positioning of the needle the local anesthetic solution is slowly
injected after negative aspiration for blood.
-
Because the paravertebral space and the
epidural space are contiguous, one must specifically avoid the
paravertebral block in cases where epidural spread is contraindicated,
including aortic stenosis and hemodynamic instability, though it is
impossible to predict which block will result in epidural spread. The
reason for placing the needle 10° to 20° lateral, rather than
perpendicular, is to help avoid the medial structures, including the
epidural space, the dural cuff, and the subarachnoid space. -
The distance between the posterior aspect
of the transverse process and the parietal/visceral pleura on CT scan
is approximately 2.6 cm with some variability based on the patient’s
weight. -
Pneumothorax requiring an intervention is
a risk associated with thoracic paravertebral block, but is extremely
rare. The combination of carefully measuring the depth to the
transverse process, using the nerve stimulator initially on
supramaximal mode (3–5 mA), and using small needles (22-gauge) provide
a margin of safety prior to penetrating the visceral pleura. The
visceral pleura will often self-seal following an
P.194
iatrogenic
needle puncture. COPD is an independent risk factor that portends an
increased risk for pneumothorax despite the use of smaller needles,
because the pathologic pleura does not readily self-seal. The
supramaximal current assists the anesthesiologist in finding the
general location of the desired nerves at T11 and L2, serving as an
anatomic GPS. In case of doubt, chest x-rays can help the diagnostic. -
Nerve stimulator guided paravertebral blocks are more difficult in thin patients than in average-sized patients.
-
This block can be used as sole anesthetic. In this case versed and/or propofol can be used for sedation.
-
Potential complications of paravertebral
block include epidural spread, leg weakness, inadvertent intravascular
injection, pneumothorax and spinal headache. These complications are
rare, occurring in less than 1% of patients, and in most cases resolve
with time. -
Paravertebral blocks can also be performed for bilateral inguinal hernia repairs.
-
Inguinal hernia is associated with
moderate to severe pain. The use of paravertebral blocks also minimize
PONV related to the use of narcotics.
SM, Pietrobon R, Nielsen KC, et al. Paravertebral somatic nerve block
compared with peripheral nerve block for outpatient inguinal
herniorrhaphy. Reg Anesth Pain Med 2002;27:476–480.
MZ, El Hassan MJ, Ziade MF, Owaydat M, Zbibo R, Lonnqvist PA.
Paravertebral blockade vs. general anesthesia or spinal anesthesia for
inguinal hernia repair: reduced incidence of postoperative nausea and
vomiting and shorter hospital stay. Middle East J Anesthesiol 2001 June; 16(2):201–10.
MR, Randazzo T, Ward W. The paravertebral nerve root block for inguinal
herniorrhaphy: a comparison with field-block approach. Reg Anesth Pain Med 1998;451–456.
