Miscellaneous Conditions
II – Knee > Part B – Evaluation and Treatment of Knee Disorders >
21 – Miscellaneous Conditions
the vast majority of knee degeneration. A handful of other conditions,
however, can lead to significant morbidity. It is important for the
physician to be familiar with these less common entities to avoid
diagnostic pitfalls and to provide appropriate care. Although this
review stresses the orthopedic issues in caring for these patients,
treating these conditions often is best accomplished with coordinated
input from different specialties. These conditions (Table 21-1)
are a heterogeneous group with various causes. Although they are
uncommon, it is useful to be aware of the key features of these
conditions when evaluating a patient with knee complaints.
entities. The exact mechanism for development of this condition remains
elusive. An area of the involved bone sustains an ischemic insult that
initiates a process of remodeling and collapse. Depending on the
location and extent of this collapse, articular surface incongruity
leads to joint degeneration. Spontaneous osteonecrosis usually develops
in older patients (sixth or seventh decade) without any antecedent
trauma or other known risk factor. Younger patients also may develop
knee osteonecrosis, usually in association with trauma or other known
risk factors such as alcohol consumption or corticosteroid use.
which articular (hyaline) cartilage is produced in the soft tissues
around joints. These cartilaginous areas can then break free and become
loose bodies. Patients develop locking, catching, and other mechanical
symptoms based on the size and number of these cartilaginous lesions.
As a consequence of intra-articular loose bodies, patients develop
secondary degenerative changes. Most cases are monoarticular, with the
knee joint involved most commonly. Men are approximately two times more
likely than women to develop this disorder.
chondromatosis is an exceedingly rare phenomenon. If imaging or
clinical findings raise even the possibility of malignancy, it is
appropriate to refer the patient to an orthopedic oncologist for
further management.
recurrent intra-articular hemorrhages in patients with clotting factor
deficiencies. Hemophiliac arthropathy therefore begins with
intra-articular bleeding. Reaction to intra-articular blood leads to
varying degrees of synovitis. This inflamed synovium is then more
susceptible to further intra-articular bleeds, setting up a potential
cycle in which patients have recurrent hemarthroses. The extensive
chronic synovitis that ensues eventually leads to joint erosions and,
over time, end-stage arthropathy.
proliferative condition of synovium in which there is an accumulation
of giant cells and hemosiderin. PVNS does not have malignant potential
but can be locally aggressive, leading to considerable synovitis that
produces erosions and secondary degenerative changes. The knee joint is
most commonly involved and, as in synovial chondromatosis, most cases
are monoarticular. PVNS is a synovial disease but also can involve
periarticular sites such as tendon sheaths and bursae.
intra-articular reactions to the characteristic crystals of the two
conditions. The body mounts an inflammatory response to the crystals,
thereby leading to secondary joint inflammation and eventually
degeneration. Patients with calcium pyrophosphate deposition disease
(CPPD), or pseudogout, may have a spectrum of findings from acute
synovitis to a long-standing arthropathy with secondary degenerative
changes. These patients also can develop deposits in hyaline
and
meniscal cartilage. Gout is caused by symptomatic elevation of uric
acid, also leading to an inflammatory response to crystals. A
combination of dietary factors and medicines—especially thiazide
diuretics—can precipitate gouty flares.
|
TABLE 21-1 Less Common Causes of Knee Degenerative Joint Disease
|
|
|---|---|
|
patients begins with a careful history. The orthopedist should inquire
about onset and duration of symptoms, any antecedent of inciting
events, other joints involved, and systemic conditions for which the
patient requires medical treatment. Patients with hemophilia should be
asked about the number of prior intra-articular bleeds.
should include surface appearance, limb alignment, range of motion,
tenderness, instability, presence of effusion, and a thorough
neurovascular exam.
diagnostically useful and give considerable, albeit temporary,
symptomatic relief. Synovial fluid in gout and pseudogout will show
characteristic crystals under the microscope: Uric acid crystals will
be negatively birefringent, and calcium pyrophosphate crystals will be
positively birefringent. As some laboratories do not routinely examine
body fluid for crystals, it is important to specify this request on the
order. Synovial fluid may be bloody in patients with PVNS, but a
nonbloody tap does not necessarily exclude this diagnosis. Synovial
fluid should also be sent for further laboratory investigations
including cell count and, when warranted, Gram stain and culture.
having already had an MRI or other advanced cross-sectional imaging,
the accepted first step in radiographic evaluation should be orthogonal
plain x-ray films. In addition to these films, additional radiographs
may be useful. A standing anteroposterior (AP) view of both knees
affords the opportunity to evaluate the contralateral joint. A patellar
view is useful for evaluating the patellofemoral articulation. In
addition to the usual radiographic stigmata of joint degeneration,
films should be scrutinized for loose bodies, radiolucent bony changes,
effusions, and changes in the soft tissues. As noted in other chapters,
concerns about limb alignment should be addressed by long-leg films
that include the hip and ankle.
radiographic manifestations of knee degeneration, the conditions in
this chapter often require ancillary studies such as bone scan or
magnetic resonance imaging (MRI). As with all medical tests, advanced
imaging should be ordered to answer a specific question that will guide
diagnosis or treatment. MRI is also useful in the face of unusual or
unexpected findings on plain films, such as radiolucent changes on both
the tibial and femoral sides of the knee joint. Magnetic resonance
imaging is clearly superior to plain films for evaluating soft tissues,
bone marrow, and articular cartilage. Computed tomography (CT) scanning
is not usually indicated or helpful in the conditions outlined here.
Although orthopedists are increasingly comfortable with different
imaging modalities, a radiologist with specialized musculoskeletal
training is invaluable in choosing which imaging studies are most
appropriate and also in the subsequent interpretation of these studies.
difficult, especially in early stages. Plain films may be negative
initially. Traditionally, bone scans have been used for diagnosis. More
recent reports show a high sensitivity for MRI. Moreover, MRI is useful
in characterizing the exact location and extent of bony and
cartilaginous involvement. The classic location of knee osteonecrosis
is the medial femoral condyle, but the lateral condyle and proximal
tibia also may be involved.
As these bodies contain varying amounts of mineral, not all will
necessarily show up on plain films. MRI is useful in these cases to see
the extent and number of loose bodies. As with PVNS, the location and
extent of disease as characterized on MRI helps the surgeon plan the
appropriate operative treatment.
including joint erosions that may appear on both sides of a joint.
Occasionally, one may appreciate a soft tissue mass or large effusion
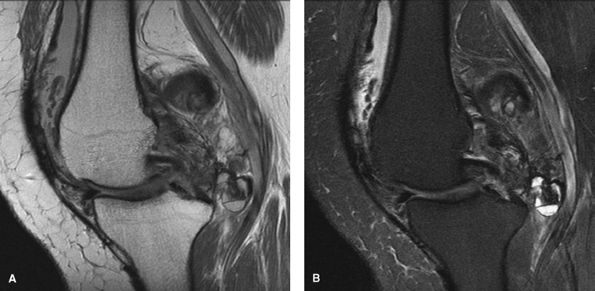
on plain film (Fig. 21-2). Because PVNS is a soft tissue process, MRI is the best imaging method to gauge the extent of disease (Fig. 21-3). MRI is extremely useful in preparing an appropriate treatment plan for PVNS of the knee.
Radiographic manifestations include calcifications of the articular
cartilage and the meniscus. Unless one suspects a superimposed meniscal
tear or other intra-articular pathology, MRI is not indicated as part
of the workup of CPPD.
 |
|
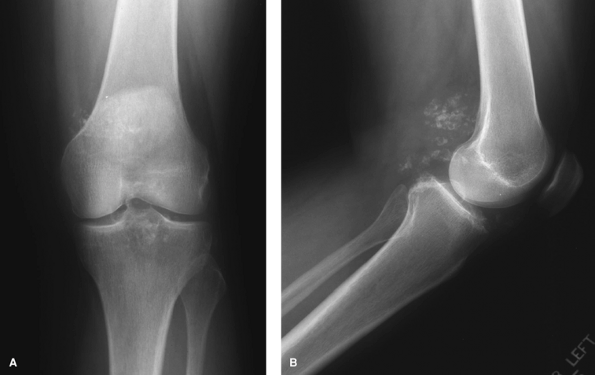
Figure 21-1 Anteroposterior (A) and lateral (B) knee x-ray views showing mineralized cartilaginous areas consistent with synovial chondromatosis.
|
 |
|
Figure 21-2
Lateral knee radiograph in a patient with pigmented villonodular synovitis. Note the considerable soft tissue mass posteriorly and the absence of significant osseous abnormalities. |
including symptom modification and anti-inflammatory medication.
Surgical management is indicated when nonoperative methods no longer
benefit the patient.
patients with hemophilia. Avoiding trauma and closely following
clotting factor levels are two straightforward ways to minimize the
number of intra-articular bleeds. Patients with recent bleeds also may
benefit from a brief period of joint immobilization to allow time for
soft tissues to recover. Because patients with hemophilic arthropathy
tend to develop soft tissue contractures, however, immobilization
should be used judiciously.
centers where the surgeon is supported by an active medical hemophilia
program. Hemophiliacs undergoing invasive procedures should be screened
for clotting factor inhibitors.
potentially dangerous, but also consumes considerable resources,
including the time and energy of consulting services and laboratory
surveillance of factor and inhibitor levels. For this reason, P-32
radiation synovectomy is attracting increasing interest in the
treatment of early arthropathy. Radiation synovectomy is especially
appropriate in patients without significant joint degeneration.
Although it obviously cannot reverse existing articular damage, the
procedure can help break the vicious and destructive cycle of synovial
irritation and intra-articular hemorrhage.
 |
|
Figure 21-3 Proton density (A) and T2 (B) magnetic resonance images of the same knee as Figure 21-2 showing extensive pigmented villonodular synovitis (PVNS).
|
Anti-inflammatory medicines and colchicine are useful in acute flares.
For long-term control of high blood uric acid levels, patients should
be managed in conjunction with colleagues
in internal medicine. Pharmacologic treatment (allopurinol) in combination with dietary modifications is recommended.
first. However, symptoms frequently persist and operative treatment,
usually with arthroplasty, commonly is needed.
amenable to nonsurgical treatment. The natural history of PVNS,
especially the diffuse form, is progressive joint erosions and
arthropathy. As with hemophiliac arthropathy, there is some interest in
using radioactive synovectomy in these patients. Although synovial
chondromatosis typically is considered to be less aggressive and
self-limiting, the loose bodies of this condition often cause pain,
loss of function, and eventually secondary joint degeneration.
managed with open synovectomies. Current trends favor the use of
arthroscopic treatment. These procedures require less clotting factor
support and are less morbid than open surgical approaches.
on several issues, including the amount of pain and desired level of
function and activity. These patients can have compromised bone stock,
distorted osseous architecture, and severe soft tissue contractures
from superimposed arthrofibrosis. In spite of these potential
difficulties, outcomes of knee replacements in this population may be
favorable, but are associated with a higher rate of infection.
choice for synovial chondromatosis. When possible, arthroscopic
procedures allow the surgeon to remove synovium and loose bodies while
avoiding the morbidity of an open approach. Occasionally, extensive
disease and difficult location require open synovectomy and
debridement. Because patients with these conditions often begin with
decreased range of motion, an early and closely supervised physical
therapy program is essential postoperatively.
usually is favorable. Some patients develop recurrent disease, but the
natural history commonly involves regression of disease. Patients may
develop secondary arthritis from loose bodies and may require joint
replacement.
nonoperative care to osteotomies, condylar allografts, and joint
replacement. Core decompression and arthroscopic debridement also have
been recommended with varying rates of success. The main determinants
of treatment choice include the location of the lesion, the amount of
joint involvement, the extent of secondary degenerative changes,
overall limb alignment, and patient age. Historically, outcomes of knee
replacement in osteonecrosis have not been as successful as in other
conditions. More recent reports have been more encouraging, however.
self-limiting course over time, diffuse PVNS is locally aggressive.
Inadequate removal of involved synovium can lead to recurrent disease;
local recurrence rates are reported as high as 50% in the literature.
Localized nodular forms of PVNS may be amenable to arthroscopic
removal, but diffuse PVNS should be treated with an open total
synovectomy. For patients with advanced degenerative changes, treatment
options are nonoperative management versus total joint replacement.
Knee fusion has fallen out of favor and should be considered a salvage
procedure.
In patients with long-standing disease and extensive surface damage,
total knee arthroplasty may be indicated with an expectation of success
equal to that for osteoarthritis.
Patients with gout should continue their preoperative medical regimen to prevent flares in other joints.
the principles of postoperative care outlined in previous chapters.
Coordinated multispecialty input often is in the patient’s best
interest. Patients with long-standing adrenal suppression from oral
corticosteroids may need perioperative stress dosing. Hemophiliacs
obviously must have appropriately titrated clotting factor levels and
perioperative input from a hematology service. These patients need
clotting factor support for several weeks following the procedure as
they embark on a therapy program. Again, close collaboration with
colleagues in internal medicine is essential for appropriate
perioperative care.
synovectomies, early institution of a physical therapy program is
critical. Patients with synovial chondromatosis and PVNS can be
affected by a vicious cycle of decreased motion that is further
compromised by open and extensive surgery around the involved joint.
These patients should receive particularly close attention from
therapists and begin working on range of motion as soon as the
periarticular soft tissues allow. Hemophiliacs often have considerable
preoperative flexion contractures and they, also, should have
especially close follow-up with therapy.
diagnoses discussed above can be treated with reasonable expectations
of success if one is aware of the potential difficulties in diagnosis
and treatment. Multispecialty care is important and can minimize
morbidity and perioperative complications.
