Fractures of the Olecranon
IV – Elbow Reconstruction > Part B – Evaluation and Treatment of
Elbow Disorders > 56 – Fractures of the Olecranon
vulnerable to injury, and fractures are not uncommon following
low-energy trauma. Fractures of the olecranon are generally amenable to
treatment and usually have a favorable prognosis.
approximately 10% of fractures about the elbow, with an estimated
incidence of 1.08 per 10,000 person-years. Most olecranon fractures
follow low-energy trauma such as a fall from a height of <2 meters,
a direct blow to the elbow, or from forced hyperextension. A fall on a
partially flexed elbow may generate an avulsion fracture of the
olecranon from the pull of the triceps. Amis and Miller investigated
variable-impact mechanisms and the resultant fracture patterns in a
cadaveric model. Whereas radial head and coronoid fractures tended to
occur with forearm impacts with the elbow in ≤80 degrees of flexion,
olecranon fractures followed direct blows at 90 degrees of flexion, and
injuries occurring with the elbow in >110 degrees of flexion tended
to result in distal humerus fractures. The olecranon and coronoid
process constitute the semilunar or greater sigmoid notch of the ulna,
which articulates with the trochlea. The constraints of this
articulation confer stability to the elbow joint and facilitate
anterior-posterior motion. A transverse “bare area” devoid of cartilage
is found at the midpoint between the coronoid and the tip of the
olecranon. An appreciation of this anatomic structure is necessary to
avoid inadvertently discarding structurally significant portions of the
olecranon when reconstructing the fractured olecranon. The ossification
center of the olecranon generally appears by 9 to 10 years of age and
fuses to the proximal ulna by age 14 years. Persistence of the physis
into adulthood may occur and can be confused with a fracture; clues to
this condition include its commonly bilateral nature and often familial
tendency. In addition, patella cubiti, an accessory ossicle embedded in
the distal triceps, may be present and likewise be mistaken for a
fracture.
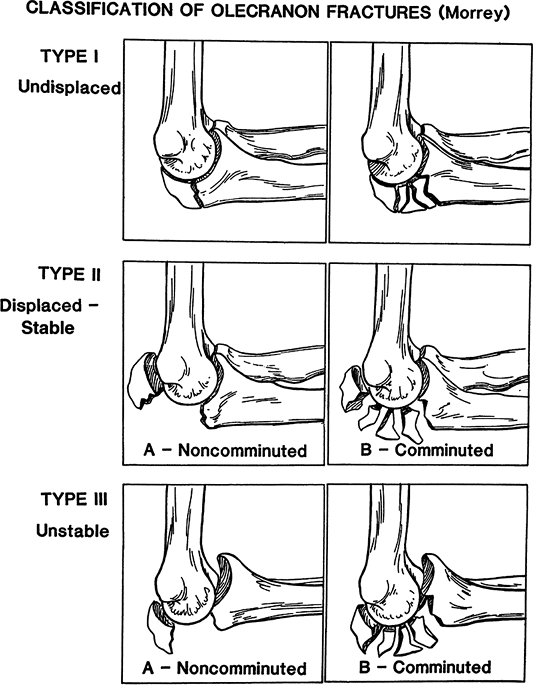
The Mayo Classification thus divides olecranon fractures into three
types, provides a basis for a rational treatment algorithm by fracture
type and subtype, and conveys prognostic value.
characterized by displacement of <2 mm with separation remaining
<2 mm with flexion of the elbow to 90 degrees or with extension
against gravity. Patients with these fractures are able to actively
extend the elbow against gravity. Type I fractures may be further
subdivided into type IA, noncomminuted fractures, and type IB,
comminuted fractures. Since these fractures are nondisplaced by
definition, the degree of comminution is not practically significant,
and types IA and IB may essentially be regarded as and treated as the
same lesion.
fractures, which are stable fractures with >3 mm of displacement,
may be noncomminuted (type IIA) or comminuted (type IIB). Because the
collateral ligaments are intact, the forearm is stable relative to the
humerus.
fractures may be subclassified into noncomminuted (IIIA) or comminuted (IIIB) types.
 |
|
Figure 56-1
Mayo Classification of olecranon fractures. Type I fractures are nondisplaced noncomminuted (IA) or comminuted (IB) fractures. Type II fractures are stable displaced fractures and may be noncomminuted (IIA) or comminuted (IIB). Type III fractures are unstable, displaced fractures and may be noncomminuted (IIIA) or comminuted (IIIB). (From Cabenela ME, Morrey BF. Fractures of the olecranon. In: Morrey BF, ed. The Elbow and Its Disorders. Philadelphia: WB Saunders; 2000
, with permission.) |
Classification categories well but are common in the elderly and may
result from forces generated by the triceps. In general, little
comminution is present.
radial head and or the coronoid process are typically multifragmentary,
complex injuries that may be adequately described by the Mayo
Classification scheme. Anterior fracture dislocations are often
referred to as transolecranon fracture-dislocations, as the mechanism
of injury appears to involve anterior displacement of the forearm
resulting in the trochlea being driven through the olecranon process.
The radial head is displaced anteriorly. This injury, unlike the Bado
type I Monteggia fracture, is characterized by instability of the
ulnohumeral joint with a preserved radioulnar relationship. Posterior
fracture dislocations of the olecranon are more similar to type II
Monteggia fractures, with posterior dislocation of the radial head, an
apex posterior fracture of the ulna, and similar implications for the
stability and function of both the ulnohumeral joint as well as the
forearm. These fractures may be considered a variant of the posterior
Monteggia lesion. Both posterior and anterior variants are commonly
associated with basal fractures of the coronoid. In anterior olecranon
fracture dislocations, reduction of the olecranon and coronoid fracture
fragments results in restoration of stability with little implications
for forearm dysfunction. Posterior olecranon fracture dislocations, in
contrast, have important implications with elbow instability and
forearm dysfunction common despite fracture reduction.
often be felt as palpable crepitation. With the exception of some
avulsion-type fractures of the olecranon, the fracture
by
nature is intra-articular, so hemarthrosis is frequently present in
conjunction with olecranon fracture. Although this sign may be
obfuscated by pain caused by the injury, inability to actively extend
the elbow against gravity may be an important indication of triceps
discontinuity. Because of the proximity of the ulnar nerve, the first
and each subsequent examination should document the status of the ulnar
nerve.
 |
|
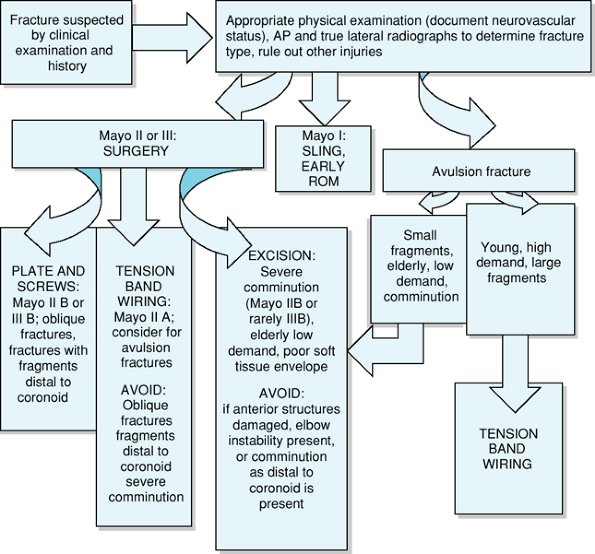
Figure 56-2
Flow chart representing the evaluation and decision-making processes involved in the workup and treatment of olecranon fractures. |
obtained to aid in diagnosis and treatment considerations. The true
lateral film should be examined to determine the extent and nature of
the fracture pattern and to evaluate for the presence of other lesions
such as a radial head fracture or dislocation, or distal humerus or
coronoid fractures. A radiocapitellar view may be helpful to assess
concomitant pathology.
management is preferred. The patient is placed in sling immobilization
for comfort with early active gentle range of motion exercises
commencing no later than 7 to 10 days postinjury. Close follow-up
(weekly) with radiographs is essential to rule out displacement and
need for alternative treatment. Restrictions on active resisted elbow
extension and weight bearing should be maintained for 6 to 8 weeks with
gradual increases in these activities as tolerated. Rarely, in select
patients, type I fractures may benefit from open reduction and internal
fixation to allow immediate motion and stability. Some type I fractures
may be treated with immobilization in a long arm cast at 90 degrees of
flexion for 3 to 4 weeks. Thereafter, protected range of motion with
avoidance of flexion >90 degrees until radiographic evidence of bony
healing occurs, usually at 6 to 8 weeks, is recommended. Range of
motion exercises may be commenced at an earlier time point in select
patients, such as the elderly, in whom stiffness occurs more frequently.
treated surgically with either excision or open reduction and internal
fixation. Goals of surgical management include restoring the articular
congruity and stability of the elbow, maintaining extension power, and
providing stable anatomic fixation such that early range of motion is
possible, thereby lessening the risk of postoperative stiffness.
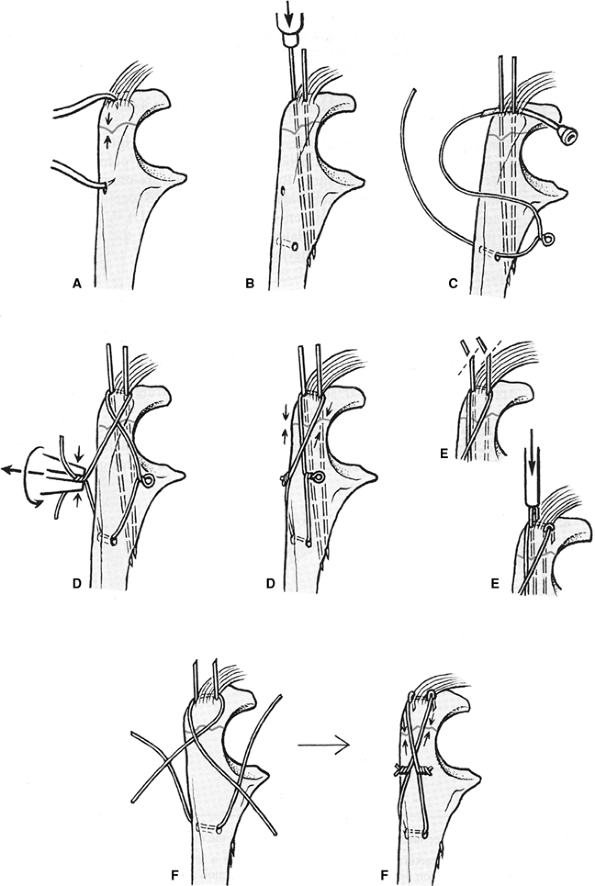
Options include tension band wiring, intramedullary screw placement,
plate-and-screw constructs, bioabsorbable pins, or excision. Tension
band wiring using standard AO technique is generally accepted and
widely used as treatment for most olecranon fracture patterns amenable
to this fixation technique (Fig. 56-3).
Tension band wiring converts tensile forces across the fracture to
compressive forces that, with motion, exert compression across the
fracture site. It may be favored over plate-and-screw fixation due to
requirements for less soft tissue dissection and less periosteal
stripping. However, this fixation technique may have technical
challenges and be associated with undesirable postoperative sequelae.
Because of the subcutaneous nature and location of the elbow, prominent
hardware may be problematic, with many patients in one series reporting
hardware-related pain (24%) and functional difficulties (32%) relieved
by hardware removal. Hardware removal rates are ≤81% in some series.
Nevertheless, ≤97% good to excellent results have been widely reported
with use of tension band wiring using proper technique. However, for
fractures with fragments distal to the coronoid, plate-and-screw
osteosynthesis is preferred, as these more distal fragments are usually
not adequately fixed by tension band wiring. Likewise, more comminuted
fractures
or oblique patterns are best treated with plate-and-screw fixation to
optimize stability. In the authors’ experience, plate-and-screw
osteosynthesis provides the optimal fixation stability with minimal
complications.
 |
|
Figure 56-3
Line drawing demonstrating optimal AO technique for tension band wiring. Reduction of the fracture is performed with pointed forceps (A), and parallel Kirschner wires are driven obliquely from proximal to distal until the volar cortex is penetrated (B). A 2.5-mm drill is used to create a transverse hole distally to accept the tension wire (B). The 1.0- or 1.2-mm wire with a prefabricated loop is introduced under the triceps and the two K-wires, then through the transverse hole (C). As an alternative, two separate wires may be used (C). The wires are grasped at the base and twisted together and the twists laid down flat on the bony surfaces (D′ and F′). Subsequently, the K-wires are pulled back slightly, cut obliquely, and bent into hooks. The hooks are then impacted into bone over the tension band (E, E′, and F′). (From Heim U. Forearm and hand/mini-implants. In: Muller ME, et al., eds. Manual of Internal Fixation: Techniques Recommended by the AO-ASIF Group. 3rd ed. New York: Springer-Verlag; 1991
, with permission.) |
 |
|
Figure 56-4
This 84-year-old right hand–dominant woman experienced a syncopal episode and fell down the stairs at home. She sustained concomitant fractures of the left proximal humerus, left distal radius, left ulnar styloid, and a fracture of the left olecranon (A) treated with excision of the proximal fragment (B and C). At 6 months postoperatively, she was painfree and her range of motion in the flexion extension arc was from 20 to 135 degrees; pronation was to 70 degrees and supination was to 70 degrees. |
for nonunions, in those with poor soft tissue viability, for
avulsion-type extra-articular fractures, and in cases with severe
comminution as in Mayo type IIB, or rarely, type IIIB fractures (Fig. 56-4).
Disadvantages of excision include subsequent risks of triceps weakness,
instability, stiffness, and a theoretical risk for increased arthrosis.
Biomechanical studies suggest that decreased extension strength may be
minimized with reattaching the triceps at a more posterior site.
McKeever and Buck determined that one may excise ≤80% of the olecranon
without sacrificing stability if the coronoid and anterior soft tissues
are intact. If anterior damage is present or if comminution extends as
far distally as the coronoid process, instability is a sequela if too
much proximal ulna is excised. In addition, An et al. noted increasing
instability of the elbow with olecranon excision. However, satisfactory
clinical outcomes (Fig. 56-4A, B) have been
described for treatment of olecranon fracture by excision when used in
appropriate patient populations. The nature of the procedure, in which
hardware is absent, may lead to decreased local complications and need
for subsequent procedures relative to other surgical treatment options.
Despite documented satisfactory outcomes with excision, some speculate
that excision may lead to development of arthrosis. Biomechanical
studies document increased forces across the ulnohumeral joint
following excision relative to fixation with tension band wiring,
suggesting that abnormal joint forces that may predispose to arthrosis
may follow excision.
recommended because of their less reliable fixation stability in vivo.
In addition, potentially problematic with intramedullary nailing are
fracture malreduction secondary to off-axis placement of the nail,
possible damage to the triceps muscle or the ulnar nerve during
locking-screw placement, and the effect of cyclical loading as well as
union rate.
potential to avoid future operations for hardware removal. Satisfactory
outcomes in a few patients have been noted; however, further clinical
experience is needed to determine the role that bioabsorbable fixation
techniques will assume in the future.
for most fractures and are necessary to treat all oblique fractures,
fractures with extensive comminution, and fractures with fragments
distal to the coronoid.
with tension band wiring. Intramedullary fixation has also been
described for selected patients, although reported outcomes have been
variable and biomechanical data is less supportive of this technique.
activity level of the patient. In patients younger than 60 years of
age, anatomic reduction of fracture fragments followed by
plate-and-screw fixation is the treatment of choice. Care should be
taken to avoid shortening the articular groove of the ulna between the
olecranon process and the coronoid process, as doing so may lead to
early arthritis. In older patients, or when comminution is severe,
excision of proximal fragments with advancement and reinsertion of the
triceps tendon may be preferred.
represent the most difficult treatment challenge of all olecranon
fractures and are associated with the highest complication rates and
least satisfactory outcomes. Type III fractures are associated with a
high incidence of concomitant pathology, such as ligamentous trauma or
bony injuries of the radial head or coronoid or distal humerus; these
should be addressed at the time of olecranon fixation. Type III
olecranon fractures typically require plate fixation and ligamentous
reconstruction. One may consider application of a hinge fixator if
stability is not restored.
plate-and-screw construct and anatomic reduction. Comminuted (type
IIIB) fractures may likewise be treated with plate osteosynthesis or
very rarely be treated with excision of fracture fragments, although
instability is likely.
considerations for treatment. Because of inherent instability of these
fracture patterns, they are best treated with plate-and-screw
osteosynthesis. Contoured plates are preferred; one-third tubular
plates lack the stiffness necessary to withstand early range of motion
and have been associated with early loosening or fatigue fractures. If
a concomitant anteromedial coronoid fracture fragment is present, it
should be fixed to optimize stability of the elbow. The integrity of
the lateral collateral ligament (LCL) and the anteromedial coronoid are
important factors in stability of the fracture.
temporary external fixation device may be helpful to facilitate
reduction; after satisfactory reduction is obtained, definitive
fracture fixation using plate and screws with or without augmentation
with tension band wiring is usually possible. If extensive comminution
is present such that plate and screw fixation does not provide
sufficient fracture stability, augmentation with tension band wiring
through the triceps insertion may facilitate stable fixation.
-
Mayo type IA and IB:
-
-
Undisplaced (<2 mm) fractures with no comminution (IA) or with comminution (IIB).
-
Sling immobilization, early active range of motion, close follow-up.
-
-
Mayo type II A:
-
-
Stable fractures with >3 mm displacement, no comminution.
-
Tension band wiring usually adequate.
Consider plate-and-screw constructs if fracture lines are distal to
coronoid; consider excision in low-demand patients or when small
fragments are present.
-
-
Mayo type II B:
-
-
Stable fractures with >3 mm displacement; comminution is present.
-
Plate-and-screw constructs preferred, especially in patients <60 years old.
-
Consider excision in low demand patients
or those older than age 60 years, fractures with extensive comminution,
or when small fragments are present.
-
-
Mayo type III A:
-
-
Unstable, displaced fracture-dislocations. No comminution is present.
-
Plate-and-screw constructs preferred.
-
-
Mayo type III B:
-
-
Unstable, displaced fracture-dislocations. Comminution is present.
-
Plate-and-screw constructs preferred.
-
-
Avulsion fractures
-
-
Tension band wiring or excision may be used.
-
olecranon is recommended to avoid placing the incision over the
subcutaneous bone. Medial and or lateral flaps may be raised to access
other bone or ligamentous structures; alternatively, concomitant radial
head or coronoid fractures may be treated through the window created by
the olecranon fracture.
fracture fragments from the triceps aponeurosis, and longitudinal drill
holes made through the proximal ulna to secure the triceps tendon down
to bone (Fig. 56-4).
Bone reduction clamps are used to reduce the fracture. A superficial
drill hole in the distal fragment may be useful to give a traction site
for the jaws of the bone reduction forceps. Following reduction, two
parallel 1.6-mm K-wires are introduced from the posterior aspect of the
olecranon aiming anteriorly and obliquely just through the anterior
cortex. A 2.5-mm hole is
drilled
transversely in the distal fragment for placement of a 1.0-mm or 1.2-mm
cerclage wire with a prefabricated loop; alternatively, two cerclage
wires may be used. The wire is then routed under the triceps tendon and
K-wires to create a figure-of-8 construct. Tensioning is performed
symmetrically on each side. The K-wires are pulled back slightly, cut
and bent, and finally the bend ends are impacted into bone.
 |
|
Figure 56-5 This 60-year-old nurse practitioner fell while running and sustained a type IIA olecranon fracture (A and B). She underwent open reduction and internal fixation with tension band wiring (C and D).
Subsequently, at latest follow-up she had range of motion from 10 to 100 degrees in the flexion/extension arc. She complained of prominent hardware and underwent hardware removal at 20 months after her fracture fixation. |
The plate may be applied over part of the triceps insertion without
muscle or periosteal elevation to optimize bone healing, or the triceps
may be split longitudinally and mobilized. If a concomitant
anteromedial coronoid fracture fragment is present, it should be fixed
to optimize stability of the elbow. When comminution is extensive, a
skeletal distractor or temporary external fixation device may be
helpful to facilitate reduction; after satisfactory reduction is
obtained, definitive fracture fixation using plate and screws with or
without augmentation with tension band wiring is usually possible. If
extensive comminution is present such that plate-and-screw fixation
does not provide sufficient fracture stability, augmentation with
tension band wiring through the triceps insertion may facilitate
stable
fixation. Restoration of the olecranon and coronoid facets is key as
the intervening segment, the transverse ridge of the olecranon,
contributes little surface contact area to the articular interface.
 |
|
Figure 56-6
This 66-year-old right hand–dominant retired laboratory technician slipped on the ice and fell, sustaining a direct blow to her left elbow and this Mayo type IIA fracture of the olecranon (A and B). She underwent plate-and-screw osteosynthesis (C and D). At 18 months postoperatively, she was painfree and her range of motion was 0 to 140 degrees, with supination to 70 degrees and pronation to 80 degrees. |
posterior plaster dressing is applied in full extension. The arm should
be elevated overnight and the initial dressing changed on the second
day. Active and passive motion is then initiated. Alternatively, if for
any reason the operative fixation was felt to be less than optimal,
splinting may be continued for 3 to 4 weeks to allow for some bony
healing. Protected use of the extremity is maintained with minimal
weight bearing and no resistance greater than that of gravity for 6
weeks or until radiographic evidence of healing is seen.
malunion, infection, loss of motion, ulnar nerve symptoms, arthrosis,
and need for additional procedures, such as hardware removal. Loss of
motion may be problematic, particularly a 10- to 15-degree extension
lag. This appears to be
related
to immobilization. Radiographic evidence of degenerative changes in the
ulnohumeral joint has been documented in 20% to 50% of patients ≤15 to
25 years following olecranon fracture, but is generally asymptomatic.
Symptomatic hardware is the most frequent complication, requiring
removal in 11.4% to 81% of patients. Hardware prominence is more common
in tension band wiring relative to other fixation techniques, such as
figure-of-8 wiring or plate-and-screw constructs. The risk of
problematic hardware with tension band wiring is decreased if attention
to proper AO technique is observed and wires are bent 180 degrees and
impacted into bone with the triceps securely sutured over the wires.
to excellent, with most series noting satisfactory outcomes and
restoration of normal or near-normal function in >95% of patients.
orthopedic practice and with appropriate treatment, generally have good
to excellent outcomes with little adverse sequelae. Decreased range of
motion, radiographic evidence of degenerative changes, and requirement
for hardware removal are common but generally are not devastating
complications, and may be obviated by attention to proper technique,
anatomic reduction, and proper postoperative management.
MI, Galatz LM, Borrelli J, Jr, et al. Intra-articular fractures of the
upper extremity: new concepts in surgical treatment. Instr Course Lect. 2003;52:591–605.
ML, Fernandez JJ, Lim TH, et al. Partial olecranon excision: the
relationship between triceps insertion site and extension strength of
the elbow. J Hand Surg Am. 2003;28(1):117–122.
JD, Ring JD, Jupiter JB. Effective treatment of fracture-dislocations
of the olecranon requires a stable trochlear notch. Clin Orthop. 2004;429:292–300.
MC, Graham HK. Olecranon fractures in children. Part 1: a clinical
review; Part 2: a new classification and management algorithm. J Pediatr Orthop. 1999;19:559–569.
MK, Hasserius R, Besiakov J, et al. Comparison of tension-band and
figure-of-eight wiring techniques for treatment of olecranon fractures.
J Shoulder Elbow Surg. 2002;11(4): 377–382.
FM, Buck RM. Fracture of the olecranon process of the ulna: treatment
by excision of fragment and repair of triceps tendon. JAMA. 1947;135:1–5.
BR, Ede DE, Brown TD. Fractures of the olecranon: an in vitro study of
elbow joint stresses after tension-band wire fixation versus proximal
fracture fragment excision. J Trauma. 2002;53:1088–1093.
S, Jasper LE, Elliott DS, et al. Biomechanical evaluation of
intramedullary nail versus tension band fixation for transverse
olecranon fractures. J Orthop Trauma. 2004;18(3): 170–174.
