Foot Problems in Children
|
|
 |
|
How some parents seem to see their children
Adapted from Wenger DR, Rang M, eds. The Art and Practice of Children’s Orthopaedics. New York: Raven Press, 1993.
|
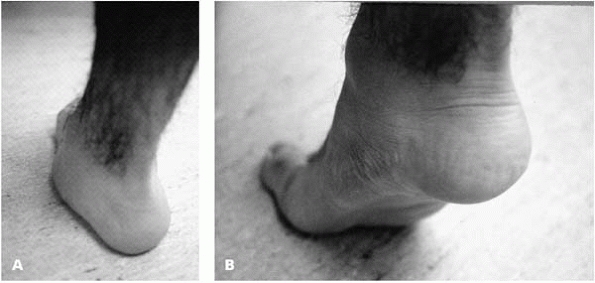
infants, due in part to excessive subcutaneous fat, but also due to
true valgus alignment of the bones and joints. As part of development,
the longitudinal arch of the foot becomes more pronounced and the fat
disappears. Flatfoot is present in 23% of adults, and is usually
asymptomatic.1 The key to staying
out of trouble with this condition is in recognizing that the flatfoot
is a normal foot shape in most affected children and adults (Fig. 25-1).
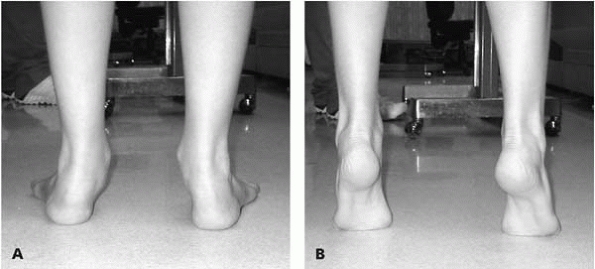
It is also important to differentiate flexible flat feet from
pathologic flat feet. This is accomplished by observing the appearance
of an arch when a flatfooted child stands up on the toes, or is
non-weight bearing with the foot dangling in the air. It is also
vitally important to verify hindfoot motion, which can also be done by
observing the child rising up to stand on the toes, as the flexible
hindfoot will move from a valgus to varus position (Fig. 25-2).
Hindfoot mobility can also be assessed by cupping the heel in the
examiner’s hand and shifting from side to side (inverting and everting)
(Fig. 25-3).
 |
|
▪ FIGURE 25-1 (A) In normal weight-bearing position, this patient has a very flat foot. (B) When standing on his toes, the arch is visible. This dynamic change with foot position defines a flexible flatfoot.
|
toes, or the hindfoot is not mobile, the child does not have a flexible
flat foot. Causes of rigid flatfoot include tarsal coalition, vertical
talus, neuromuscular condition, inflammatory arthritis, infection, etc.
An easily overlooked part of flatfoot assessment is contracture of the
Achilles tendon. This can be evaluated by passively dorsiflexing the
ankle while holding the subtalar joint in a neutral-to-slight varus
position, with the knee in full extension. If, when tested in this
manner, at least ten degrees of ankle
dorsiflexion
is not possible, the child will frequently complain of pain under the
medial midfoot. A painful flatfoot with a tight Achilles tendon
warrants treatment.
 |
|
▪ FIGURE 25-2 (A) Patient with flatfeet and hindfoot valgus. (B)
When standing on the toes, the hindfoot goes into varus, proving the hindfoot is mobile, and the arch elevates, thus confirming a flexible flatfoot. |
the first manifestation of a syndrome such as Ehlers-Danlos syndrome,
Marfan, Morquio, Down, cri-du-chat, fragile X, and others.
diagnosed, share with the parents that this is not a problem, but a
normal variation. It may be helpful to share with parents that studies
of both military recruits and grocery store employees who are on their
feet much of the day found that flexible flatfeet are not a source of
disability in adults.1,2 It has been shown that wearing corrective shoes or inserts does not influence the course of flexible flatfoot in children.3
Furthermore, wearing shoe modifications during childhood has been shown
to be a negative experience and associated with lower self-esteem in
adult life.4 While not prescribing “something” may get you in trouble with the parents, above all we must do not harm to the child.
flatfeet are prescribed orthotics. As one consultation letter from a
non-MD explains “Nontreatment for this condition could result in
further subluxation of the joints, producing symptoms in adulthood
including low back discomfort, weakness, instability, bunions,
hammertoes and internal foot problems” and the child may not get into
Harvard. This belief of the evilness of flatfeet may be widespread in
parts of your community. Stay out of trouble by finding out what
opinions your parents may have heard before seeing you.
 |
|
▪ FIGURE 25-3 Hindfoot mobility can be assessed by cupping the heel and shifting it from side to side (inverting and everting).
|
under an already flat foot may cause discomfort, particularly in those
with an Achilles tendon contracture. Children who have undergone
orthotic-ectomies with complete relief of pain and guilt are among our
most grateful patients.
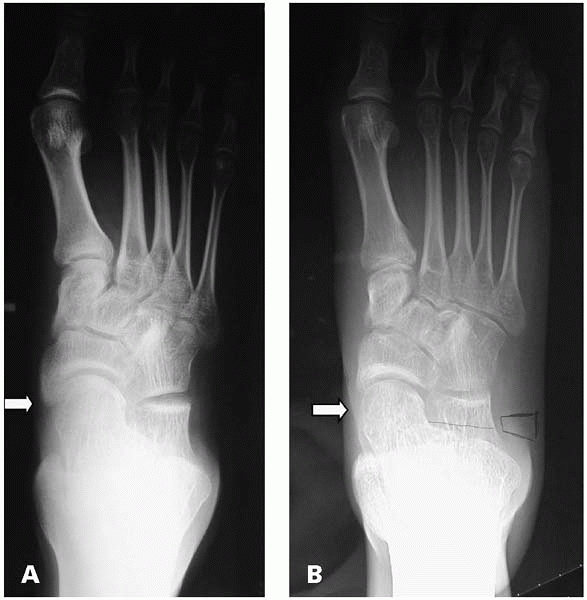
flatfoot. We should treat symptoms, not deformity. Painful flexible
flatfeet may be associated with an accessory navicular, tight heel
cords, or other conditions. It is essential that foot radiographs are
taken with the child bearing weight (Fig. 25-4), and be aware that
many of the radiographs patients bring with them will not be.
Over-the-counter soft shoe inserts, available at many sporting good
stores, will often relieve symptoms of diffuse foot aching. Consider
surgery only as the last resort. Avoid fusions, as the calcaneal
lengthening osteotomy has good results and preserves subtalar motion.5
Synthetic implants have been used frequently by non-physician
healthcare providers, and we have seen disasters. We recommend staying
away from implants until they have been shown to be equal in safety and
efficacy to the calcaneal lengthening osteotomy.
 |
|
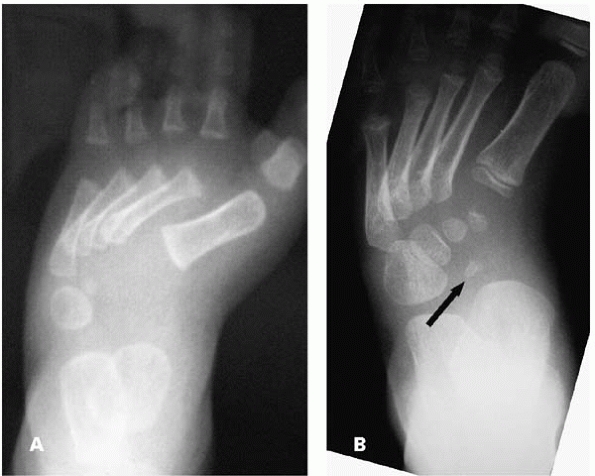
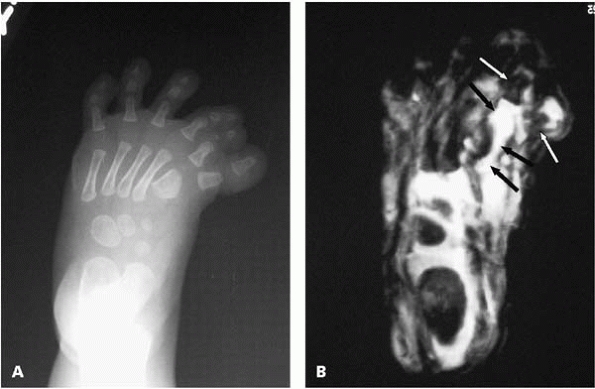
▪ FIGURE 25-4 (A) Non-weight bearing AP radiograph of the foot demonstrates reasonable alignment of the talonavicular joint (arrow). (B)
Weight-bearing view of the same child’s foot taken moments later demonstrates medial subluxation of the talar head relative to the navicular (arrow). |
fusions within the foot lead to degenerative changes at adjacent
joints. Fusions, and in particular triple arthrodesis, should be
avoided if possible, and used only as a last resort.6, 7, 8
Tendon transfers to address muscle imbalance and extraarticular
osteotomies should adequately manage the majority of children’s foot
deformities.
radiographs for minor trauma, and are mistaken for fractures. Remember
that more than 20% of children have at least one accessory bone that
can be seen on radiographs.9
have a symptomatic accessory navicular become asymptomatic when they
reach skeletal maturity, suggesting that surgery should be delayed and
used only as a last resort. Use of a medial longitudinal arch support
may exacerbate the symptoms by adding more pressure to the region,
whereas a UCBL (University of California Biomechanics Laboratory) shoe
insert may unweight the painful area by bringing the heel into varus
and elevating the arch of the foot. Surgical excision of the accessory
navicular without re-routing of the posterior tibial tendon has been
reported to have good results.10 However, any surgery in a painful weight-bearing region of the foot is prone to continued discomfort (Fig. 25-5).
 |
|
▪ FIGURE 25-5 Accessory navicular (arrow).
|
children, where the flexor hallucis longus passes in the groove along
the posterior talus. The trouble with this accessory bone is that it
can fracture and cause pain or become symptomatic in ballet dancers
presumably due to prolonged weight bearing in equinus. A fractured os
trigonum may have a rough or sharp border along the talus, in contrast
to an unfused os trigonum with a smooth border (Fig. 25-6).
 |
|
▪ FIGURE 25-6 Os trigonum (arrow). Note that the edges are smooth, suggesting that this is not a fracture.
|
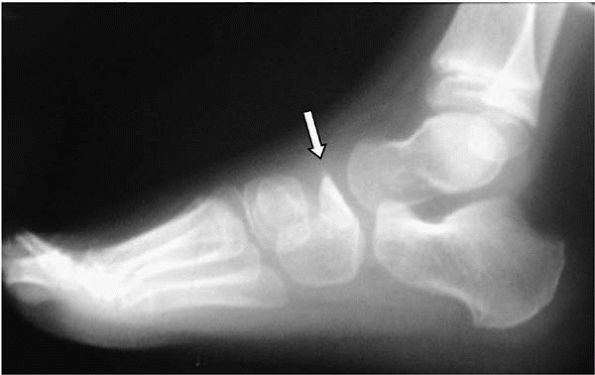
the base of the fifth metatarsal where the peroneus brevis attaches is
often confused with a fracture by the unknowing (Fig. 25-7).
 |
|
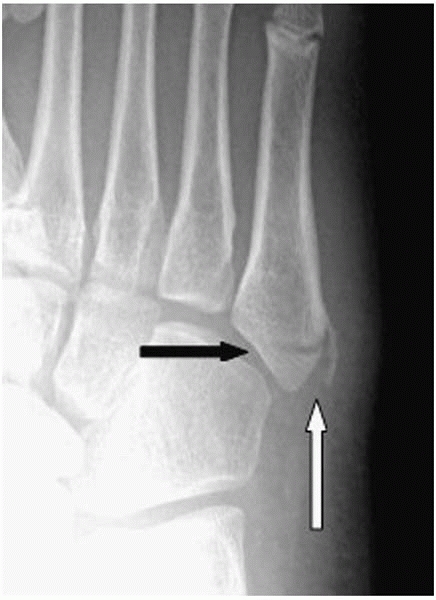
▪ FIGURE 25-7
AP radiograph of a child’s foot demonstrating the normal apophysis of the fifth metatarsal where the peroneus brevis tendon attaches (white arrow), which is more or less parallel to the long axis of the metatarsal. This normal apophysis is not to be confused with a fracture of the proximal fifth metatarsal (black arrow), which tends to occur perpendicular to the long axis of the metatarsal. |
just stick to a limited number of pitfalls. Clubfoot is frequently part
of an underlying syndrome, thus a complete history and physical is
warranted to uncover other abnormalities. Clubfoot is also associated
with tarsal coalition11 and fibular hemimelia.12
-
This problem involves the whole leg, not just the foot. The entire leg will be thinner and slightly shorter than the other.
-
Make them aware of
the Ponseti method as the recently accepted form of treatment in the
USA. Parents of patients who underwent months of casting or surgery for
clubfoot and believe a vastly superior alternative was hidden from them
can be very upset. -
Following the
standard surgical treatments that have been in common use during the
past half century, the reported rate of secondary surgery approximates
50%, and stiffness and pain have been common sequelae. -
Dynamic supination
of the foot is seen in perhaps 30% of children with clubfoot and may
require transfer of the tibialis anterior to the lateral cuneiform in
children over the age of 3 to 4 years.
All children being evaluated for musculoskeletal problems should have a
careful hip exam. Imaging of hips should be based purely on risk
factors or findings suggestive of DDH.
manipulations and cast applications which, when combined with a heel
cord tenotomy, has been reported to provide complete correction of the
idiopathic clubfoot in 95% of patients.14
In our opinion, the main pitfalls in use of the Ponseti approach result
from deviation from the prescribed technique as described by the
originator.15
-
Indications: idiopathic clubfoot and those with associated chromosomal abnormalities or ligamentous laxity syndromes.
-
Pitfalls: Pressure
sores from the manipulation and casting in patients with spina bifida
or arthrogryposis. It is important to apply the cast only to the limits
that may be obtained via manipulation.
-
Hyperpronation of
the first ray; the foot should be initially supinated. The foot should
remain supinated throughout the casting procedure; as increased
correction is obtained, the supination is decreased to a more normal
alignment. -
Maintain the foot in
equinus during the sessions of manipulation and casting. Attempting to
place the foot in a dorsiflexed position prior to correcting the
hindfoot will block the eversion and abduction of the calcaneus
underneath the talus, subsequently preventing full correction of the
clubfoot. -
Fulcrum of pressure
should be positioned over the head of the talus. Errantly positioning
pressure over the calcaneal cuboid joint16 will block the reduction of the calcaneus underneath the talus and prevent subtalar correction.
-
Casting children who are agitated. Babies are comforted with bottle-feeding during the casting procedure.
-
Long leg cast
application is always used and is integral to the success of the
method. Failure to use long leg casts will result in poor outcome. -
Not using a well-molded plaster cast as opposed to fiberglass cast material.
-
Placing too much or
too little padding around the foot and ankle. Two to three layers of
cotton roll is sufficient before application of the plaster cast. -
Casting the foot in correction beyond that obtained by manipulation.
-
Pressure in the popliteal fossa from the proximal trim line of the short leg cast when converting to the long leg cast.
-
When trimming the
cast down, don’t expose too much of the dorsal aspect of the foot
proximal to the metatarsal-phalangeal joints, as this will often lead
to a tourniquet effect and swelling of the toes.
-
Performing tenotomy
before the heel is in valgus and foot abduction of greater than 60
degrees is noted. This will block the eversion of the calcaneus in the
subtalar joint and lead to midfoot breech and a rocker bottom deformity. -
Excessive dorsiflexion prior to tenotomy will result in difficulty in palpation of the Achilles tendon.
-
Injecting large amounts of lidocaine around the tendon will make palpation difficult.
-
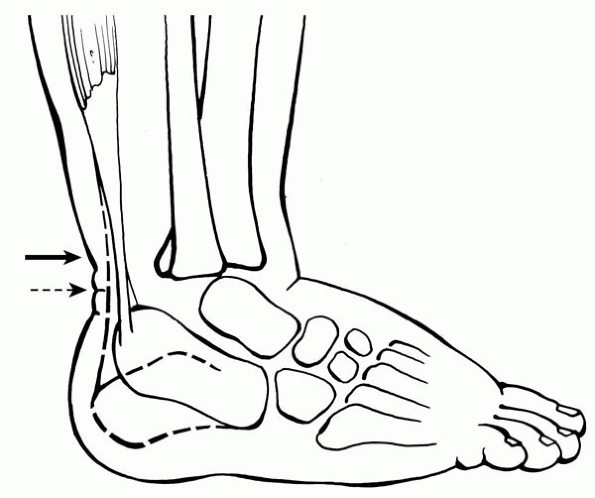
Performing a tenotomy at the cutaneous heel crease (Fig. 25-8, dashed arrow)
can be difficult and potentially detrimental, as you will be too distal
and potentially into the substance of the Achilles tendon insertion on
the calcaneus. Tenotomy needs to be approximately one half centimeter
proximal to the distal heel crease (Fig. 25-8, solid arrow). -
Incomplete tenotomy
should be suspected when there is no palpable ‘pop’ and an immediate
increase in dorsiflexion of approximately 15 to 30 degrees. The tendon
should be revisited with the knife to complete the transection. -
Transection of local venous structures, and presumably the peroneal artery, has been noted.17
When excessive bleeding occurs, simple pressure on the heel cord for an
additional 3 to 4 minutes before placing in a long leg cast is usually
all that is necessary.
-
Noncompliant use of the abduction orthosis.14,18 Successful use of an orthosis is associated with prevention of deformity recurrence.
-
Errors in fitting of
the abduction orthosis include deviation from the shoulder width
positioning of the shoes and standard external rotation of the feet of
50 to 60 degrees. -
Pressure sores can
result from poor fit of the shoes. For the first week the skin should
be checked at each diaper change to detect and treat potential blisters
or other pressure phenomena.
 |
|
▪ FIGURE 25-8
|
should be the number one priority. Absence or a substantial reduction
in the size and flow of the anterior tibial artery occurs in
approximately 90% of limbs with clubfoot. Preservation of the posterior
tibial artery should be a surgeon’s number one priority. One should
consider not fully exsanguinating the foot prior to tourniquet
inflation in order to visualize the posterior tibial neurovascular
bundle. Although uncommon, the posterior tibial artery may be absent in
a clubfoot.19 If the posterior
tibial vascular bundle cannot be located at the time of surgery, even
after the tourniquet is taken down, a hypertrophied peroneal vascular
bundle may be present, and should be carefully identified and protected.
-
In order to correct equinus of the calcaneus, the calcaneofibular ligament must be sectioned.
-
Leave wound open if needed—otherwise bringing the foot out of equinus may be difficult and require serial postoperative casting.
-
Do not cut the talocalcaneal interosseous ligament—otherwise lateral translation of calcaneus is a disaster.
-
Do not position the navicular dorsal to the talar head, as that is associated with a poor outcome.20
-
Part of syndrome? Arthrogryposis.
-
Unossified bones make radiograph interpretation unreliable.
-
When releasing the talonavicular joint, aim distally or risk cutting across the talar neck.
-
Make Cincinnati incision at least 1 cm proximal to heel crease or risk heel slough if more distal.
-
Isolate neurovascular bundle early in the procedure.
 |
|
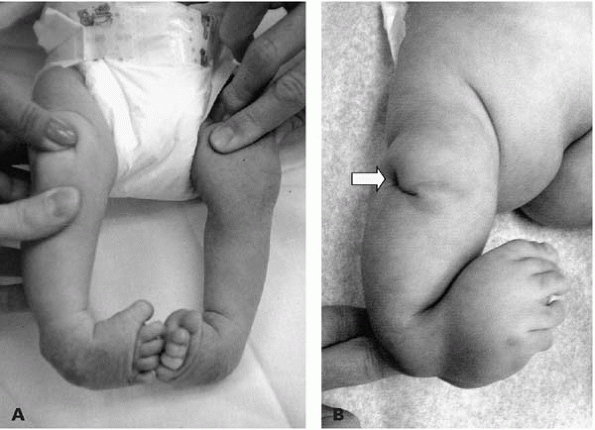
▪ FIGURE 25-9 (A) Baby with bilateral clubfeet. (B) Baby with tibial hemimelia. Note that the dimple over the knee (arrow)
is a red flag that there is an underlying osseous disorder. Dimples are often seen over the apex of the tibial bow in fibula hemimelia. |
point out that ankle valgus is common in children with clubfoot, and
recommend a weight-bearing anteroposterior radiograph of the ankles in
children presenting with clubfoot “overcorrection.” When ankle valgus
is the cause of hindfoot valgus, a hemiepiphysiodesis treats the site
of deformity rather than inappropriate hindfoot surgery.
as you make the right diagnosis and don’t treat it. First, make certain
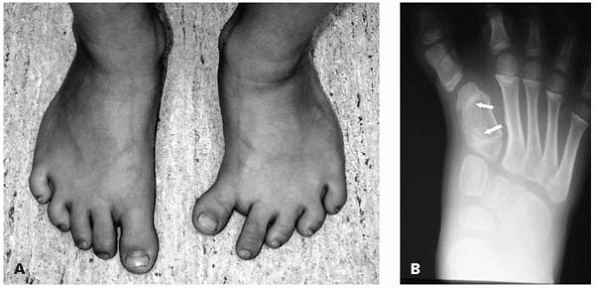
there is normal ankle dorsiflexion; if not, it is not metatarsus adductus (MTA), and may be a clubfoot. Look at the hindfoot; if there is significant valgus, think of a skewfoot (Fig. 25-10).
It may be difficult to differentiate between MTA and skewfoot with
radiographs in infants as the navicular is not yet ossified (Fig. 25-11). MTA may also be confused with a metatarsal longitudinal epiphyseal bracket (Fig. 25-12).
 |
|
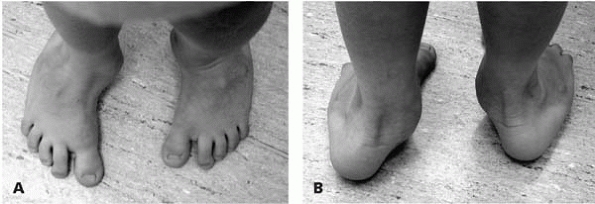
▪ FIGURE 25-10 (A) At first glance, this child may appear to have severe metatarsus adductus. (B)
When viewed from behind, the significant heel valgus (which does not correct when standing on his toes) suggests something other than metatarsus adductus. This child has a skewfoot. |
 |
|
▪ FIGURE 25-11 (A) AP radiograph of a 1-year-old. Is this metatarsus adductus? (B) AP radiograph of the same foot, at age 4 years. Note that the navicular is now ossified (arrow)
and can be appreciated in its position far lateral to the center of the talar head, making the diagnosis of skewfoot easier to appreciate. |
 |
|
▪ FIGURE 25-12 (A)
This child has a metatarsal bracket of the left foot. An increased space between the first and second toes is a clue that this foot has something other than metatarsus adductus. (B) AP radiograph demonstrating the longitudinal epiphyseal bracket (arrows) of the first metatarsus in this child. |
needed for MTA, do not do a capsular release as this leads to poor
results. We recommend an osteotomy of the medial cuneiform, rather than
the first metatarsal, both to avoid the proximal physis of the first
metatarsal, and for better correction. Lateral osteotomies may be of
the second to fifth metatarsals or the cuboid.
underlying neurologic condition. It has been reported that two thirds
of patients with painful high arches have an underlying neurologic
problem that turns out to be Charcot-Marie-Tooth about 50% of the time.23
If there are bilateral cavus feet, think of neuromuscular disease. If
the occurrence is unilateral, think of a spinal problem and order an
MRI of the entire spine. As a spine examination is not complete without
inspection of the feet, examination of a child with a cavus foot is not
complete without inspection of the spine. If the underlying
neuromuscular problem is treatable, get on with it before treating the
foot. Treatment for progressive cavus deformity with pain and
instability is surgical. Make certain the parents understand that the
foot deformity is not the problem, but is the result of the problem. It
is possible that future surgery will be needed, as the underlying
disease progresses in many cases.
associated with underlying neuromuscular conditions or syndromes. The
surgeon’s first job is to identify those other conditions.
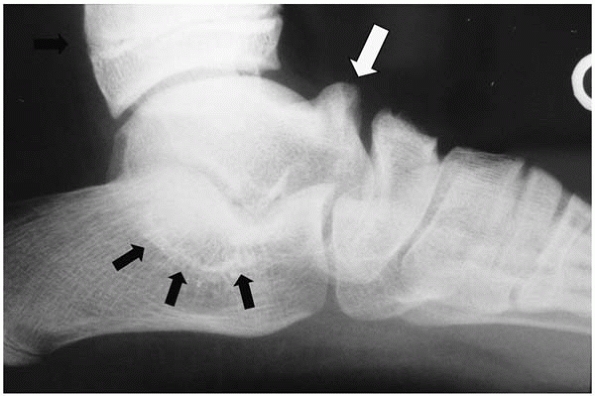
obvious as some other foot deformities. A prominent talar head in the
setting of a rigid foot is suspicious, but avoid confusing an oblique
talus, positional calcaneovalgus, posteromedial bowing of the tibia, or
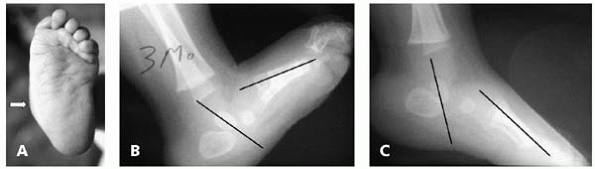
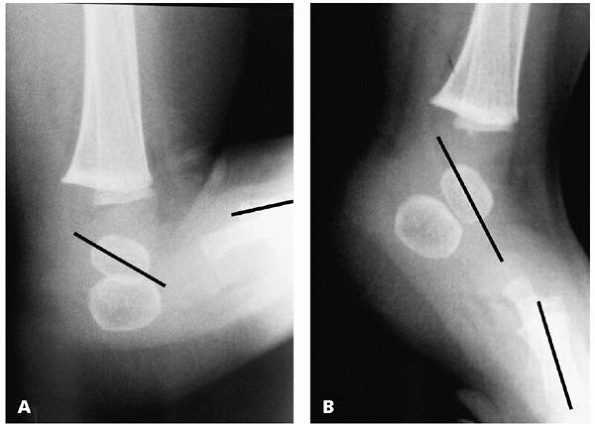
just a really flat foot, with a vertical talus (Fig. 25-13A).
By definition, a vertical talus is a fixed dorsal dislocation of the
navicular on the head of the talus. As the navicular is not ossified
until about age 3 years, and cannot be seen on plain radiographs, we
rely on the relationship of the axis of the talus and the first
metatarsal. The diagnosis is confirmed on the plantar flexed lateral
radiograph by observing that the axis of the talus passes plantar to
that of the first metatarsal (Figs. 25-13B and C).
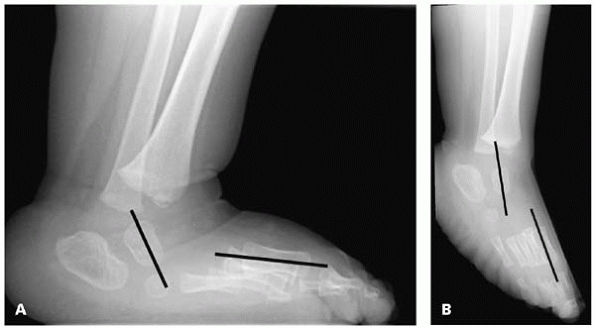
Avoid the pitfall of believing that if the two axes become parallel,
there is not a vertical talus. Dorsal translation of the first
metatarsal axis in relation to that of the talus indicates dorsal
dislocation at the talonavicular joint (Fig. 25-14). The axis of the talus remains vertically aligned with the axis of the tibia on the dorsiflexion lateral radiograph.
 |
|
▪ FIGURE 25-13 Three-month-old with vertical talus. (A) Rocker bottom medial prominence characteristic of vertical talus. (B)
Lateral radiograph of foot is nondiagnostic. Although the axis of the talus is plantar to that of the first metatarsal, this radiograph is consistent with an oblique talus as well as vertical talus. (C) A forced plantarflexion lateral radiograph confirms the diagnosis of vertical talus as the axis of the talus and first metatarsal still do not line up, and the talus remains quite vertical relative to the first metatarsal. |
unlikely to correct the vertical talus deformity, though Dr. Matthew
Dobbs in St. Louis has reported some success.
Preoperative plantar flexion casting will stretch the dorsal skin and tendons, thus facilitating surgical deformity correction.
 |
|
▪ FIGURE 25-14 Example of a child with vertical talus (A) in which the axes of the talus and first metatarsal become nearly parallel in plantar flexion (B),
but the axis of the first metatarsal is translated dorsal to that of the talus. Recall that the definition of a vertical talus is a fixed, dorsal dislocation of the navicular relative to the talus to help understand why this radiograph is consistent with a vertical talus. |
 |
|
▪ FIGURE 25-15 (A)
Child with an oblique talus. Note that this radiograph shows a quite similar relationship between the talus and first metatarsal as that seen in Fig. 25-14. (B) With plantar flexion, the axis of the talus and first metatarsal significantly change their relationship. |
bunion surgery in adolescents than in adults. Stay out of trouble by
delaying surgery until skeletal maturity, if possible. If surgery is
needed, consider an opening wedge osteotomy of the medial cuneiform, if
the intermetatarsal angle is greater than 8 degrees. This will help
correct a medially deviated cuneiform-first metatarsal joint, as well
as avoid potential damage to the first metatarsal growth plate.
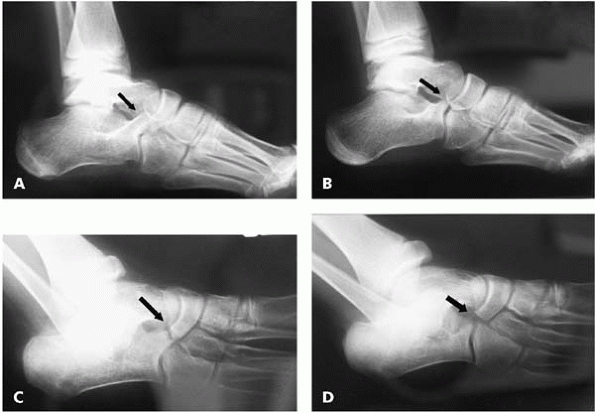
diagnosis of a tarsal coalition should be strongly suspected from the
physical examination, based on decreased subtalar joint motion and
inability to voluntarily invert the foot (see Fig. 25-3). Many children with a tarsal coalition present with rigid heel valgus and tightness of the peroneal tendons (Fig. 25-16).
clearly demonstrate tarsal coalitions, but they do provide lots of
clues. Oblique views are usually diagnostic of a calcaneonavicular
coalition, (Fig. 25-17) though a fibrous
coalition is best visualized on an MRI. A talocalcaneal coalition may
be seen on a Harris view if you are lucky enough to get a perfect shot,
but is most reliably seen on a CT scan (Figs. 25-17 and 25-18).
A recent series of 48 patients found the C-sign of Lateur on the
lateral radiograph to be present in all patients with flatfeet, but
present in only 40% of those with tarsal coalitions,24 (Fig. 25-18)
so an absence of the C-sign does not rule out a tarsal coalition. A CT
scan should be considered for all feet in which a calcaneonavicular
coalition has been identified on plain radiographs because of the
possibility of a coincidental talocalcaneal coalition in the same foot.
A second coalition was identified in 20% of patients undergoing CT
scans for tarsal coalition at the Texas Scottish Rite Hospital, though
this population from a tertiary pediatric center may be skewed towards
more severe cases.25
 |
|
▪ FIGURE 25-16
Photo of one of the authors sitting next to a patient with frequent recurrent ankle sprains. Both are trying to invert their feet, but the patient cannot due to bilateral tarsal coalitions. |
 |
|
▪ FIGURE 25-17 (A)
On a lateral radiograph of the foot, a calcaneonavicular coalition is difficult to identify conclusively. The arrow points to an elongated anterior process of the calcaneus (“anteater” sign), which is suggestive of a calcaneonavicular coalition. (B) The contralateral normal foot for comparison. (C) An oblique view clearly demonstrates the calcaneonavicular bar (arrow). (D) The contralateral normal foot for comparison demonstrates no coalition (arrow). |
 |
|
▪ FIGURE 25-18 Talar calcaneal bar is difficult to appreciate on plain radiographs, however talar beaking (white arrow) and the C-sign (black arrows) suggest this coalition may be present.
|
coalitions are asymptomatic, so the second pitfall here is in treating
something that doesn’t need treatment. Pain onset is usually between
ages 8 and 16 years in those who become symptomatic. The exact site(s)
and source(s) of pain in tarsal coalitions are not well established. A
few weeks of immobilization in a cast or walking boot may get a child
through a symptomatic period, and save the child from surgery.
Unfortunately, it is our experience that in most children who present
with painful tarsal coalitions, pain will return after immobilization,
and surgery is likely eventually.
exist in the foot and have a plan for your approach to each. Recurrent
discomfort occurs at times due to inadequate resection, particularly of
the talocalcaneal coalitions. Make certain that adequate bone is
removed at the primary surgery so that normal cartilage and joint is
seen at the periphery of the resection, and full inversion of the heel
does not cause impingement at the region of resection. Last, but not
least, as with any operation to treat pain in the feet, make the
patient and family aware that pain relief cannot be guaranteed.
the appearance of the foot may be striking, spontaneous correction is
the rule (Fig. 25-19). Having the parents
perform stretching exercises may help the babies, and will keep the
parents happy that something is being done. The thing to watch out for,
on tests more than in real life, is the true diagnosis of posterior
medial bowing of the tibia, which usually corrects spontaneously but
may result in a 3- to 4-cm leg length discrepancy. See Chapter 10 on newborns for more discussion of this subject.
 |
|
▪ FIGURE 25-19 Calcaneal valgus in a newborn. It is not unusual for the dorsum of the foot to be touching the leg anterior to the tibia.
|
and do not confuse it with infection, fracture, or something more
serious. Do not treat if there are no symptoms, but immobilization for
a few weeks should help relieve discomfort.
Multiple ossification centers of the navicular may be confused with Köhler disease (Fig. 25-20).
 |
|
▪ FIGURE 25-20 Lateral view of a child with foot pain demonstrates Köhler disease. Arrow points to collapsed, avascular navicular.
|
although it can be associated with Ellis-Van Creveld syndrome, Down
syndrome and tibial hemimelia. Thus you should be on the lookout for
underlying disorders when encountering polydactyly.
longitudinal deficiency, most commonly fibular hemimelia, and may be
associated with other conditions such as a leg length discrepancy, ball
and socket ankle, or absent ACL.
 |
|
▪ FIGURE 25-21 (A)
AP radiograph of a foot with preaxial duplication in a 1-month-old. The abnormally shaped first MT is characteristic of a longitudinal epiphyseal bracket. (B) An MRI of the same foot at age 7 months demonstrates the cartilage (black arrows) wrapping around the first MT, confirming the diagnosis or a longitudinal epiphyseal bracket. The proximal phalange of each of the two great toes is shown by white arrows. |
made much worse with surgery. Excessive scarring and unhappiness with
cosmetic appearance is not uncommon following surgical resection. But
don’t worry, plastic surgeons don’t read this book, so you may refer
patients who demand surgery to them.
-
Curly toes: almost
everyone has them at birth. Very rarely a 3- to 4-year-old will have
pain if the distal phalanx of the curly toe remains completely under
the adjacent toe. Tenotomy of the flexor digatorum longus of that toe
is usually curative. -
Congenital
overriding fifth toe: only about 50% will be painful in older children
and adults. Wait for symptoms. This is not just a tight extensor
tendon. It is a dorsomedial translation of the toe. Although the Butler
procedure has been shown to effectively correct the deformity, the
procedure is associated with risk to the vascularity of the toe. -
Flatfeet
-
Coalitions
-
Accessory navicular
-
Köhler disease
-
Flatfoot: really coalition or vertical talus in infant
-
MTA: really metaphyseal bar—needs surgery
-
Valgus foot: really fibular hemimelia
-
Fifth MT apophysis vs. fracture
-
Cavus foot: underlying neurologic problem if bilateral, spine problem if unilateral
-
Vertical talus: syndromes
-
Clubfoot
-
Flatfoot is a normal variant. An asymptomatic, isolated flatfoot does not require treatment.
-
Perform fusions of the foot only as an absolute last resort.
-
For the Ponseti
clubfoot method, long leg casts are essential, and results are
dependent on parental follow-through with bracing. -
For a cavus foot, look for an underlying neurologic condition.
-
For a vertical talus, look for an underlying neurologic condition or syndrome.
-
For a tarsal coalition, consider a CT to look for a second coalition.
DR, Mauldin D, Speck G, et al. Corrective shoes and inserts as
treatment for flexible flatfoot in infants and children [see comment]. J Bone Joint Surg Am. 1989;71(6):800-810.
VS. Calcaneal lengthening for valgus deformity of the hindfoot: results
in children who had severe, symptomatic flatfoot and skewfoot. J Bone Joint Surg Am. 1995;77(4):500-512.
DE, Davids JR, Pugh LI. Clubfoot and developmental dysplasia of the
hip: value of screening hip radiographs in children with clubfoot. J Pediatr Orthop. 2003;23(4):503-507.
JA, Dolan LA, Dietz FR, et al. Radial reduction in the rate of
extensive corrective surgery for clubfoot using the Ponseti method. Pediatrics. 2004;113(2):376-380.
MB, Gordon JE, Walton T, et al. Bleeding complications following
percutaneous tendoachilles tenotomy in the treatment of clubfoot
deformity. J Pediatr Orthop. 2004;24(4):353-357.
MB, Rudzki JR, Purcell DB, et al. Factors predictive of outcome after
use of the Ponseti method for the treatment of idiopathic clubfeet. J Bone Joint Surg Am. 2004;86A(1):22-27.
DA, Albanese EL, Levinsohn EM, Hootnick DR, et al. Pulsed color-flow
Doppler analysis of arterial deficiency in idiopathic clubfoot. J Pediatr Orthop. 2003;23(1):84-87.