Elbow Dislocation
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > III – Upper Extremity Fractures and Dislocations > 18 – Elbow Dislocation
18
Elbow Dislocation
EPIDEMIOLOGY
-
Accounts for 11% to 28% of injuries to the elbow.
-
Posterior dislocation is most common.
-
Simple dislocations are those without fracture.
-
Complex dislocations are those that occur with an associated fracture and represent just under 50% of elbow dislocations.
-
Highest incidence in the 10- to 20-year
old age group associated with sports injuries, although recurrent
dislocation is uncommon.
ANATOMY
-
The elbow is a “modified hinge” joint
with a high degree of intrinsic stability owing to joint congruity,
opposing tension of triceps and flexors, and ligamentous constraints. -
The three separate articulations are:
-
Ulnohumeral (hinge).
-
Radiohumeral (rotation).
-
Proximal radioulnar (rotation).
-
-
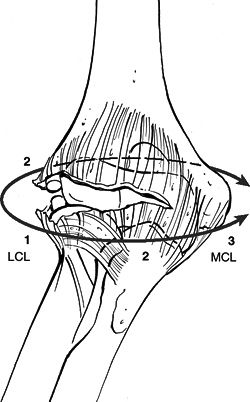
Stability (Fig. 18.1)
-
Anterior-posterior: trochlea-olecranon
fossa (extension); coronoid fossa, radiocapitellar joint,
biceps-triceps-brachialis (flexion). -
Valgus: The medial collateral ligament
(MCL) complex: the anterior bundle is the primary stabilizer in flexion
and extension, and the anterior capsule and radiocapitellar joint
function in extension. -
Varus: The lateral ulnar collateral ligament is static, and the anconeus muscle is dynamic.
-
Function of the MCL
-
It is the primary medial stabilizer, especially the anterior band.
-
Full extension provides 30% of valgus stability.
-
Ninety degrees of flexion provides >50% of valgus stability.
-
Resection of anterior band will cause gross instability except in extension.
-
-
Lateral ligaments
-
These prevent posterior subluxation and
rotation of the ulna away from the humerus with the forearm supination
(posterolateral rotatory instability).
-
-
-
Normal range of motion: 0 to 150 degrees flexion, 85 degrees supination, and 80 degrees pronation.
-
Functional range of motion requires: 30 to 130 degrees flexion, 50 degrees supination, and 50 degrees pronation.
MECHANISM OF INJURY
-
Most commonly, injury is caused by a fall
onto an outstretched hand or elbow, resulting in a levering force to
unlock the olecranon from the trochlea combined with translation of the
articular surfaces to produce the dislocation. -
Posterior dislocation: This is a combination of elbow hyperextension, valgus stress, arm abduction, and forearm supination.
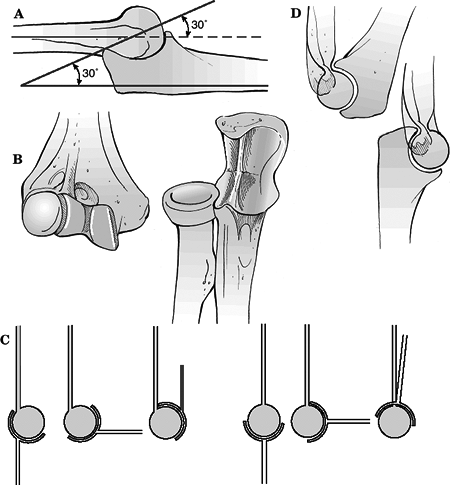 Figure
Figure
18.1. The elbow is an inherently stable joint. (A) The trochlear notch
of the ulna provides a nearly 180-degree capture of the trochlea, which
tilts posteriorly approximately 30 degrees. (B) The ridge in the center
of the trochlear notch interdigitates with a groove on the trochlea,
further enhancing stability. (C) Flexion of the elbow is enhanced by
the anterior translation of the trochlea with respect to the humeral
shaft as well as the coronoid and radial fossae on the anterior surface
of the humerus that accept the coronoid process and radial head
respectively. (D) Posteriorly, the olecranon fossa enhances extension
by accommodating the olecranon process.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Anterior dislocation: A direct force strikes the posterior forearm with the elbow in a flexed position.
-
Most elbow dislocations and
fracture-dislocations result in injury to all the capsuloligamentous
stabilizers of the elbow joint. The exceptions include
fracture-dislocations of the olecranon and injuries with fractures of
the coronoid involving nearly the entire coronoid process. -
The capsuloligamentous injury progresses from lateral to medial; the elbow can completely dislocate with the anterior band
P.195
of the MCL remaining intact. There is a variable degree of injury to the common flexor and extensor musculature (Fig. 18.2).![]() Figure
Figure
18.2. The capsuloligamentous structures of the elbow are injured in a
lateral to medial progression during dislocation of the elbow. The
elbow can dislocate with the anterior band of the medial collateral
ligament (MCL) remaining intact.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
P.194
CLINICAL EVALUATION
-
Patients typically guard the injured upper extremity, which shows variable gross instability and swelling.
-
A careful neurovascular examination is essential and should be performed before radiography or manipulation.
-
Following manipulation or reduction, repeat neurovascular examination should be performed to assess neurovascular status.
-
Serial neurovascular examinations should
be performed when massive antecubital swelling exists or when the
patient is felt to be at risk for compartment syndrome. -
Angiography may be necessary to evaluate vascular compromise.P.196
-
Following reduction, if arterial flow is
not reestablished and the hand remains poorly perfused, the patient
should be prepared for arterial reconstruction with saphenous vein
grafting. -
Angiography should be performed in the
operating room and should never delay operative intervention when
vascular compromise is present. -
The radial pulse may be present with brachial artery compromise as a result of collateral circulation.
-
ASSOCIATED INJURIES
-
Associated fractures most often involve the radial head and/or coronoid process of the ulna.
-
Acute neurovascular injuries are
uncommon; the ulnar nerve and anterior interosseous branches of the
median nerve are most commonly involved. -
The brachial artery may be injured, particularly with an open dislocation.
RADIOGRAPHIC EVALUATION
-
Standard anteroposterior and lateral radiographs of the elbow should be obtained.
-
Radiographs should be scrutinized for associated fractures about the elbow.
CLASSIFICATION
-
Simple versus complex (associated with fracture)
-
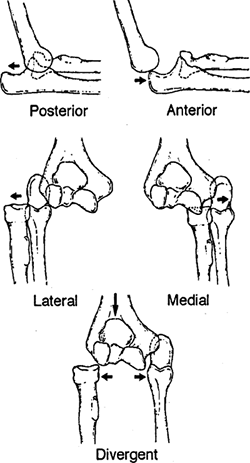
According to the direction of displacement of the ulna relative to the humerus (Fig. 18.3):
-
Posterior
-
Posterolateral
-
Posteromedial
-
Lateral
-
Medial
-
Anterior
-
TREATMENT PRINCIPLES
-
Restoration of the inherent bony stability of the elbow is the goal.
-
Restoration of the trochlear notch of the ulna, particularly the coronoid process, is also the goal.
-
Radiocapitellar contact is very important to the stability of the injured elbow.
-
The lateral collateral ligament is more important than the MCL in the setting of most cases of traumatic elbow instability.
-
The trochlear notch (coronoid and
olecranon), radial head, and lateral collateral ligament should be
repaired or reconstructed, but the MCL rarely needs to be repaired. -
If the elbow is stable, or can be made
stable with surgery on the lateral side, the MCL will heal properly
with active motion, and its repair will not be necessary for stability. -
Morrey recommended that the elbow should
not redislocate before reaching 45 degrees of flexion from a fully
flexed position; Jupiter and Ring recommended that the elbow should be
able to go to 30 degrees before substantial subluxation or dislocation.
P.197
Fracture-Dislocations
 |
|
Figure 18.3. Elbow dislocations.
(From Browner BD, Jupiter JB, Levine AM, eds. Skeletal Trauma. Philadelphia: WB Saunders, 1992:1142, with permission.)
|
This is an elbow dislocation with an associated fracture about the elbow.
-
Radial head: These make up 5% to 11% of cases.
-
Medial or lateral epicondyle (12% to
34%): They may result in mechanical block following closed reduction
owing to entrapment of fragment. -
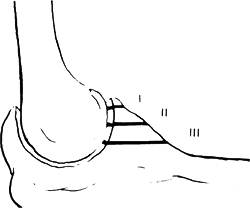
Coronoid process (5% to 10%): These are
secondary to avulsion by brachialis muscle and are most common with
posterior dislocation.-
Types I, II, and III, based on size of fragment (Fig. 18.4):
-
Type I, avulsion of the tip of the coronoid process.
-
Type II, a single or comminuted fragment involving 50% of the coronoid process or less.
-
Type III, a single or comminuted fragment involving >50% of the process.
-
-
-
Elbow dislocations that are associated
with one or more intraarticular fractures are at greater risk for
recurrent or chronic instability. -
Fracture-dislocations of the elbow usually occur in one of several distinct, recognizable injury patterns, including:
-
Posterior dislocation with fracture of the radial head.
-
Posterior dislocation with fractures of the radial head and coronoid process—the so-called terrible triad injury.
-
Varus posteromedial rotational instability pattern injuries.
-
Anterior olecranon fracture-dislocations.
-
Posterior olecranon fracture-dislocations.
-
-
The following observations may be useful in guiding treatment:
-
Terrible triad injuries nearly always
have a small transverse fracture of the tip of the coronoid including
the anterior capsular attachment. Much less commonly, the coronoid
fracture is either very large or involves the anteromedial facet of the
coronoid preferentially.![]() Figure 18.4. Regan and Morrey classification of coronoid fractures.(From Regan W, Morrey BF. Fractures of coronoid process of the ulna. J Bone Joint Surg 1989;71:1348–1354, with permission.)
Figure 18.4. Regan and Morrey classification of coronoid fractures.(From Regan W, Morrey BF. Fractures of coronoid process of the ulna. J Bone Joint Surg 1989;71:1348–1354, with permission.) -
Varus posteromedial rotational
instability pattern injuries are defined by a fracture of the
anteromedial facet of the coronoid process. -
In the setting of an olecranon
fracture-dislocation, the coronoid fracture can be one simple large
fragment, it can be fragmented in to two or three large pieces
(anteromedial facet, central, and lesser sigmoid notch) with or without
a tip fragment, or it can be more comminuted.
-
P.198
Types of Elbow Instability
-
Posterolateral rotatory instability (elbow dislocations with or without associated fractures)
-
Varus posteromedial rotational instability (anteromedial coronoid facet fractures)
-
Olecranon fracture-dislocations
Posterolateral Rotatory Instability (Fig. 18.5)
-
This results in dislocation of the elbow with or without fractures of the radial head and coronoid.
-
This occurs during a fall on to the
outstretched arm that create a valgus, axial, and posterolateral
rotatory force. The ulna and the forearm supinate away from the humerus
and dislocate posteriorly. -
This may result in injury to the radial head or coronoid.
-
The soft tissue injury proceeds from lateral to medial, with the anterior band of the MCL being the last structure injured.
-
It is possible to dislocate the elbow with the anterior band of the MCL remaining intact.
Varus, Posteromedial Rotational Instability
-
This occurs with a fall onto the
outstretched arm that creates a varus stress, axial load, and
posteromedial rotational force to the elbow.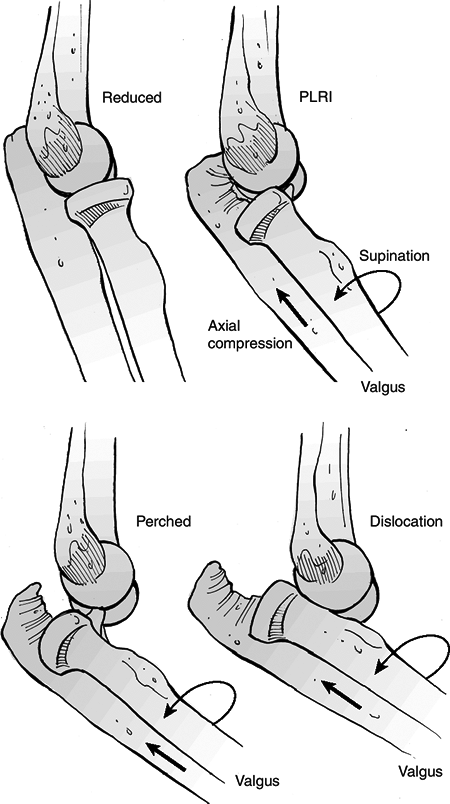 Figure 18.5. Posterolateral rotatory instability (PLRI) occurs in several stages. Elbow dislocation is the final stage.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 18.5. Posterolateral rotatory instability (PLRI) occurs in several stages. Elbow dislocation is the final stage.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
This results in fracture of the
anteromedial facet of the coronoid process and (1) injury to the
lateral collateral ligament, (2) fracture of the olecranon, or (3) an
additional fracture of the coronoid at its base.
P.199
P.200
Anterior Olecranon Fracture-Dislocations
-
These result from a direct blow to the flexed elbow.
-
Some authors suggest that these injuries
may result from the same mechanism that usually creates elbow
dislocations, particularly in older osteopenic individuals.
Instability Scale (Morrey)
| Type I: | Posterolateral rotatory instability; positive pivot shift test; lateral ulnar collateral ligament disrupted |
| Type II: | Perched condyles; varus instability; lateral ulnar collateral ligament, anterior and posterior capsule disrupted |
| Type IIIa: | Posterior dislocation; valgus instability; lateral ulnar collateral ligament, anterior and posterior capsule, and posterior MCL disrupted |
| Type IIIb: | Posterior dislocation; grossly unstable; lateral ulnar collateral ligament, anterior and posterior capsule, anterior and posterior MCL disrupted |
TREATMENT
Simple Elbow Dislocation
Nonoperative
-
Acute simple elbow dislocations should
undergo closed reduction with the patient under sedation and adequate
analgesia. Alternatively, general or regional anesthesia may be used. -
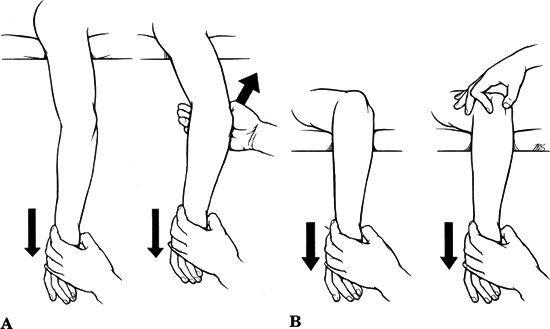
Correction of medial or lateral
displacement followed by longitudinal traction and flexion is usually
successful for posterior dislocations (Fig. 18.6). -
For posterior dislocations, reduction should be performed with the elbow flexed while providing distal traction.
-
Neurovascular status should be reassessed, followed by evaluation of stable range of elbow motion.
-
Postreduction radiographs are essential.
-
Postreduction management should consist of a posterior splint at 90 degrees and elevation.
-
Early, gentle, active range of elbow
motion is associated with better long-term results. Prolonged
immobilization is associated with unsatisfactory results and greater
flexion contracture. -
A hinged elbow brace through a stable arc of motion may be indicated in cases of instability without associated fracture.
-
Recovery of motion and strength may require 3 to 6 months.
Operative
-
When the elbow cannot be held in a
concentrically reduced position, redislocates before postreduction
radiography, or dislocates later in spite of splint immobilization, the
dislocation is deemed unstable, and operative treatment is required. -
There are three general approaches to
this problem: (1) open reduction and repair of soft tissues back to the
distal humerus, (2) hinged external fixation, or (3) cross-pinning of
the joint.
P.201
 |
|
Figure
18.6. (A) Parvin’s method of closed reduction of an elbow dislocation. The patient lies prone on a stretcher, and the physician applies gentle downward traction of the wrist for a few minutes. As the olecranon begins to slip distally, the physician lifts up gently on the arm. No assistant is required, and if the maneuver is done gently, no anesthesia is required. (B) In Meyn and Quigley’s method of reduction, only the forearm hangs from the side of the stretcher. As gentle downward traction is applied on the wrist, the physician guides reduction of the olecranon with the opposite hand. (A, redrawn from Parvin RW. Closed reduction of common shoulder and elbow dislocations without anesthesia. Arch Surg
1957;75:972–975. B, redrawn from Meyn MA, Quigley TB. Reduction of posterior dislocation of the elbow by traction on the dangling arm. Clin Orthop 1974;103:106–108.) |
Elbow Fracture-Dislocations
Nonoperative
-
This is a reasonable treatment option in patients with dislocation and fracture of the radial head only.
-
Patients who elect nonoperative treatment
need to be aware of the potential for instability and the substantial
potential for restriction of motion or arthrosis from the radial head
fracture. -
Under close supervision, it is reasonable
to remove the splint and to begin active motion at the patient’s first
visit to the office, typically about a week after injury.
Operative
-
This includes radial head resection, repair or replacement, and lateral collateral ligament repair.
-
If the radial head cannot be repaired,
resection and replacement with a metal prosthesis will enhance
immediate and long-term stability. -
Most authors do not support acute collateral ligament reconstruction.
-
Some authors however, stress the
importance of the lateral collateral ligament to elbow stability and
advocate reattachment of this ligament to the lateral epicondyle. -
When the lateral collateral ligament is
repaired, immediate active motion is usually possible (particularly if
radiocapitellar contact has also been restored), but up to 10 days of
immobilization is reasonable.
P.202
“Terrible Triad” Fracture-Dislocations
-
The addition of a coronoid fracture, no
matter how small, to a dislocation of the elbow and fracture of the
radial head dramatically increases the instability and the potential
for problems. -
The term “terrible triad of the elbow” was coined by Hotchkiss to refer to this injury pattern.
-
Not all terrible triad injuries will be unstable, but it can be difficult to predict which injuries will be unstable.
-
Nonoperative treatment is risky because the elbow can dislocate in a cast, unknown to the patient.
-
Radial head resection without prosthetic replacement is unwise because recurrent dislocation of the elbow is common.
-
Good results have been reported with
repair of the coronoid or anterior capsule, repair or replacement of
the radial head, and lateral collateral ligament repair. -
This restores stability in most cases, but in some patients MCL repair or hinged external fixation is also necessary.
COMPLICATIONS
-
Loss of motion (extension): This is
associated with prolonged immobilization. Some authors recommend
posterior splint immobilization for 3 to 4 weeks, although recent
trends have been to begin early (1 week) range of elbow motion. -
Neurologic compromise: Sustained neurologic deficits at the time of injury should be observed.
-
Spontaneous recovery usually occurs; a
decline in nerve function (especially after manipulation) and severe
pain in nerve distribution are indications for exploration and
decompression. -
Exploration is recommended if no recovery is seen after 3 months following electromyography.
-
-
Vascular injury: The brachial artery is most commonly disrupted during injury.
-
Prompt recognition of vascular injury is essential, with closed reduction to reestablish perfusion.
-
If, after reduction, perfusion is not
reestablished, angiography is indicated to identify the lesion, with
arterial reconstruction when indicated.
-
-
Compartment syndrome (Volkmann
contracture): This may result from massive swelling due to soft tissue
injury. Postreduction care must include elevation and avoidance of
hyperflexion of the elbow. Serial neurovascular examinations and
compartment pressure monitoring may be necessary, with forearm
fasciotomy when indicated. -
Instability/redislocation: This is rare
after isolated, traumatic posterior elbow dislocation; the incidence is
increased in the presence of an associated coronoid process and radial
head fracture (terrible triad of the elbow). It may necessitate
capsuloligamentous reconstruction, internal fixation, prosthetic
replacement of the radial head, or hinged external fixation. -
Heterotopic bone/myositis ossificans:
-
Anteriorly it forms between the
brachialis muscle and the capsule; posteriorly it may form medially or
laterally between the triceps and the capsule. -
The risk is increased with multiple
reduction attempts, a greater degree of soft tissue trauma, or the
presence of associated fractures. -
It may result in significant loss of function.
-
Forcible manipulation or passive stretching increases soft tissue trauma and should be avoided.
-
Indomethacin or local radiation therapy
is recommended for prophylaxis after surgery and in the presence of
significant soft tissue injury and/or associated fractures.
P.204 -
P.203