Disorders of the Acromioclavicular and Sternoclavicular Joints
III – Upper Extremity > 20 – Disorders of the Acromioclavicular and
Sternoclavicular Joints
joints serve as the primary links in the suspension of the upper
extremity from the axial skeleton. Despite its requisite strength, the
AC joint is one of the most commonly injured structures in the athletic
population, particularly in young males involved in collision sports.
It is also susceptible to overuse injury in the overhead athlete. More
than 60 different procedures have been described to treat these
injuries, indicative of the lack of consensus historically. More
recently, however, the treatment of AC joint pathology has evolved
dramatically, especially with the introduction of arthroscopic
techniques. This chapter will first describe the anatomy and
biomechanics of the AC joint to clarify the complex pathophysiology of
injuries to this area. This will facilitate an understanding of the
diagnosis and treatment options, which are then reviewed.
distal clavicle and the medial facet of the acromion with an extremely
variable orientation. A fibrocartilaginous disk of variable size,
shape, and composition resides within the joint. A complete disk is
seen in less than 10% of the general population. The frequency with
which it is found decreases dramatically with age; nevertheless, it
becomes nonfunctional in most individuals after about age 40.
clavicle, which is one of the first bones to ossify, appears first at
intrauterine week 5. It increases in diameter via intramembranous
ossification. Two epiphyses, one on the medial end and one on the
lateral end, contribute to the longitudinal growth via enchondral
activity. The medial epiphysis is responsible for the majority of this
growth, appearing at about age 18 and fusing between ages 22 and 25.
The lateral epiphysis is less consistent and is often mistaken for a
fracture in young adults. The acromion has between 2 and 5 ossification
centers that appear at puberty. They fuse by age 25. Failure of any of
these apophyses to fuse is known as an “os acromiale,” which can also
be mistaken for a fracture.
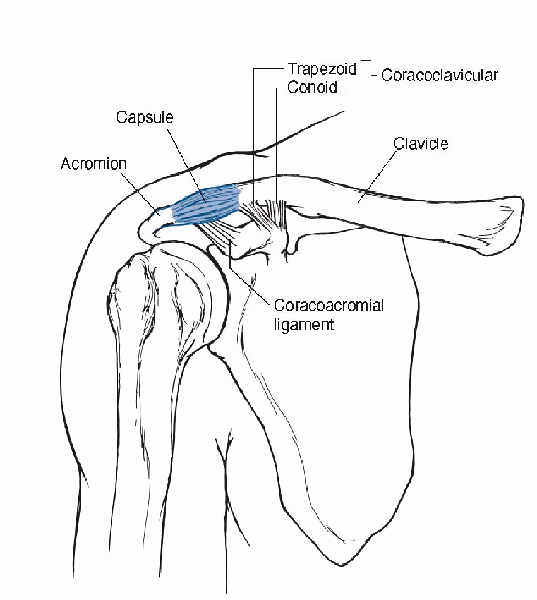
supported by the strong AC ligaments, as well as the fascia from the
deltoid and the trapezius muscles. The superior,
inferior, anterior, and posterior AC ligaments provide resistance to horizontal translation (Box 20-1).
Of these, the superior ligament is the strongest, providing 56% of the
resistance to horizontal translation of the clavicle in serial
sectioning studies, followed by the posterior ligament, which provided
25%. The insertion of these ligaments on the clavicle averaged about
1.5 cm from the AC joint. This is important when considering distal
clavicle resection for AC joint arthrosis (Fig. 20-1).
-
Anterior
-
Superior
-
Compression
-
Posterior
-
Distraction
 |
|
Figure 20-1
The AC joint is supported by the capsule, AC ligaments, and the CC ligament. (From Oatis CA. Kinesiology: The Mechanics and Pathomechanics of Human Movement. Baltimore: Lippincott Williams & Wilkins, 2004.) |
trapezoid—which provide resistance to vertical displacements, further
stabilize the AC joint. The more lateral trapezoid is a broad ligament
that runs obliquely from the superior surface of the coracoid process
to the inferior aspect of the clavicle about 1 cm medial to the AC
joint. The more medial conoid ligament is conical in shape and arises
along the posteromedial side of the coracoid process. It inserts
posteriorly along the undersurface of the clavicle at the junction of
the lateral and middle thirds. Both are posterior to the insertion of
the pectoralis minor on the coracoid. There is often a bursa separating
these two limbs of the CC ligament. The average distance between the
coracoid and the clavicle is 1.1 to 1.3 cm, which is important in the
diagnosis of complete disruptions of the joint. Sectioning studies have
shown the importance of these ligaments is a function of both the
direction and the magnitude of the deforming force.
aspect of the coracoid to the undersurface of the acromion. Its
function in the stability of the AC joint was originally thought to be
important; however, more recent studies imply that it does not have a
significant role with forces at or equal to 70 N. It is an important
secondary glenohumeral stabilizer, particularly in the presence of a
complete rotator cuff tear.
in the anterior/posterior and superior/inferior planes. Originally,
studies by Inman (1944) hypothesized 20 degrees of motion at the AC
joint, with forward elevation and abduction of the arm and 40 degrees
of clavicular rotation in total. This led many to the conclusion that
arthrodesis of the AC joint would limit motion of the shoulder.
Subsequent work by Rockwood and Kennedy and Cameron (1954) demonstrated
“synchronous scapuloclavicular rotation.” Thus, as the clavicle rotates
upward, the scapula rotates simultaneously downward. There is 40 to 50
degrees of clavicular rotation but only 5 to 8 degrees at the AC joint.
The majority of the rotation occurs at the SC joint.
population. In an early study, Thorndike and Quigley (1942) noted AC
joint injuries in 223 of 578 (39%) athletes with shoulder injuries.
Since then, AC joint injuries have been reported to be one of the most
common traumatic injuries in rugby, football, ice hockey, skiing,
cycling, and snowmobiling. Overuse injuries of the AC joint are also
commonly seen in players of golf, baseball, and tennis. AC injuries are
much more common in males than females (5 to 10:1) and in young adults.
In a review of dislocations of the shoulder complex, dislocations of
the glenohumeral joint occurred in 85%, the AC joint in 12%, and the SC
joint in 3% (Cave, 1958). However, incomplete injuries are twice as
common as complete injuries. As the population ages (and more
specifically the athletic population), there will likely be an increase
in acute injuries to the AC joint in older individuals as well as an
increase in AC joint arthrosis, which has been correlated with previous
traumatic injury.
joint. The most common etiology is a fall onto the anterior, superior
edge of the acromion (“point of the shoulder”) with the arm in an
adducted position. This drives the acromion downward, away from the
fixed clavicle. The resulting appearance of the shoulder is secondary
to this movement, not an upward displacement of the clavicle, despite
its prominence. Injury can also occur indirectly, via a fall onto an
adducted, outstretched arm or elbow, which can cause the humerus to
translocate superiorly, forcing the humeral head up and into the
acromion. Another indirect mechanism that has been described is a
sudden downward force on the upper extremity, such as a change in the
position of a heavy load, which pulls the scapula downward. Both of
these indirect mechanisms are rare, compared with direct trauma from a
fall onto the acromion.
 |
|
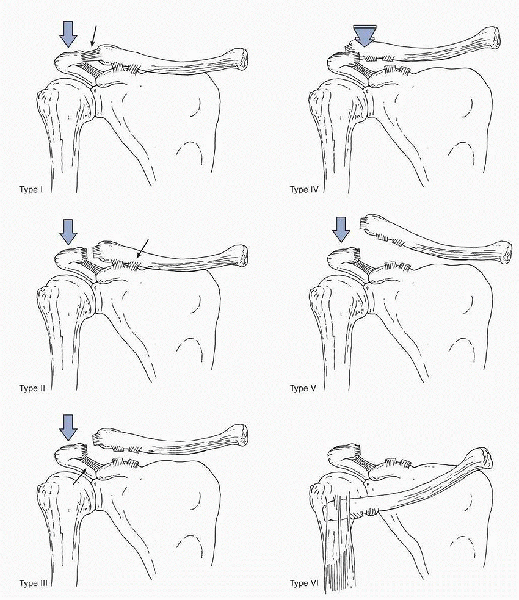
Figure 20-2 Classification of AC joint instability.
|
originally classified AC joint injuries into types I, II, and III on
the basis of x-rays and clinical examination. This was later revised by
Rockwood (1989) to account for differences he saw within “type III”
injuries. He added types IV, V, and VI to account for these differences
(Fig. 20-2 and Table 20-1).
ligaments (type I). When the force continues, further energy is
absorbed by the CC ligaments (type II) and may result in even greater
displacement of the joint as these ligaments rupture
(type
III). An even more severe injury may occur with larger forces that
result in the disruption of the deltotrapezial fascia, as well as the
ligaments (type V). If the deforming force is directed posteriorly and
is of sufficient magnitude, the clavicle can be displaced into or
through the trapezius muscle (type IV). Type VI is a subcoracoid
dislocation of the clavicle. It is associated with extreme trauma and
is rare. A type VII, which is complete dislocation of the AC and SC
joints, has been described but is extremely rare.
|
TABLE 20-1 CLASSIFICATION OF AND CLINICAL FINDINGS FOR AC JOINT INJURIES
|
|||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||
-
The diagnosis of an AC joint disruption is usually made by history and confirmed by physical examination and x-ray.
-
With acute traumatic injuries, the diagnosis can be obvious.
-
Classification of injury (e.g., Rockwood
type II vs. III) and assessing for other concomitant injuries can be
more difficult (see Table 20-1). -
In general, palpation of the area and assessment of joint stability are important.
-
X-ray analysis is also important (see below).
-
In patients without a history of acute trauma, localization of the pathology to the AC joint can be more involved.
-
The innervation of the AC joint is provided by the lateral pectoral nerve anteriorly and the suprascapular nerve posteriorly.
-
Gerber (1998) evaluated patterns of pain
for both AC joint and subacromial pathologies. Irritation of the AC
joint produced pain directly over the joint, in the anterolateral neck,
and over the anterolateral deltoid—areas that were subtly distinct from
the subacromial irritation. -
The cross-shoulder adduction test,
performed with the arm elevated to 90 degrees and the elbow bent 90
degrees, can be helpful if it produces pain localized to the AC joint
because the arm is adducted across the chest, thereby compressing the
joint. -
In general, a triad of point
tenderness—positive cross-shoulder adduction test and relief of
symptoms with an injection of a local anesthetic into the AC joint—is
indicative of AC joint pathology. -
Clinical features for each type are summarized in Table 20-1. See also Figure 20-3.
 |
|
Figure 20-3 Physical examination findings in acute injury: type V.
|
-
The assessment of the AC joint can be done well with only plain films, but special views and technique are required.
-
Because of its relatively superficial
location, less penetration strength of the beam (approximately 50%) is
needed compared with standard views. -
A Zanca anteroposterior (AP) view, which
tilts the beam 15 degrees cephalad, can visualize the AC joint better
than a standard AP view by preventing the scapular spine from being
superimposed on the AC joint and should be routinely performed.-
Normal x-ray findings on a Zanca AP view
and an axillary lateral include a joint space of 1 to 3 mm, which
diminishes significantly with age to about 0.5 mm by age 60. -
A space of greater than 7 mm in males and 6 mm in females is abnormal.
-
A CC distance of 1.1 to 1.3 cm is normal.
-
Although an incongruent AC joint can be
seen in as many as 30% of controls, an increase of 25% to 50% in the CC
distance, compared with the unaffected side, can signify complete AC
joint dislocation.
-
-
An axillary lateral is critical to assess
horizontal displacements, especially in a type IV injury, and should
also be done routinely. -
To assess for a coracoid fracture, the Stryker notch view is helpful if indicated.
-
Previously, stress views were recommended to differentiate type II, type III, and type V injuries.
-
These were typically done in the AP plane with a 5-lb weight attached to each arm.
-
However, several studies have questioned the efficacy of the routine use of these x-rays.
-
-
Of historical interest, Alexander (1949), described the lateral stress view or “shoulder-forward” view.
-
It is taken from both the uninjured and
injured sides as a scapular Y view, with the patient thrusting his or
her shoulders forward. -
On the injured side, the displacement of the acromion anteriorly and inferiorly can be seen.
-
-
Computed tomography (CT) and magnetic
resonance imaging are not used routinely, although each may be utilized
as an adjuvant in more complicated situations.
-
The goals of both nonoperative and
operative management of AC injuries are full pain-free strength and
motion and restoration of normal anatomy and appearance.
-
Type I and II injuries are treated nonoperatively, with a sling for up to 2 to 3 weeks, ice, and nonsteroidal medications.
-
The sling is used only as needed for comfort, with gradual return to regular daily activities.
-
A type I injury is treated purely symptomatically, and the patient is usually back to unrestricted activities within 2 weeks.
-
With a type II injury, the patient is not
allowed to do any heavy lifting, pushing, pulling, or contact sports
for up to 8 to 12 weeks to allow the ligaments to heal. -
Continued, unrelieved pain can be treated with an injection of steroid into the AC joint.
-
-
The management of type III injuries is
controversial; however, there has been no shown benefit of surgery and
should be treated in the same way as a type II injury with a sling use
of up to 4 weeks for comfort.-
When in doubt, opt for nonoperative management and treat on the basis of symptoms.
-
Many devices have been described to try to reduce the AC joint with pressure, such as braces, straps, harnesses, and casts.
-
The problems with these devices include
skin breakdown from continuous pressure, discomfort, inconvenience,
noncompliance, and joint stiffness. -
Many authors use a sling for simplicity and comfort, and accept the minimal deformity of the injury.
-
-
In type VII injuries, the SC dislocation
is treated nonoperatively with good results, and treatment of the AC
joint is controversial.
-
On radiographs, there is calcification of ligaments postinjury in 40% of patients but it does not correlate with function.
-
This occurs whether or not the patient has an operation.
-
It can be an isolated bone structure or bridge between the coracoid and clavicle.
-
-
The prognosis for patients with type I
and II injuries is good, but they may be more prone to degenerative
disease and osteolysis. -
X-ray changes seen in the distal clavicle may include osteoporosis, osteolysis, tapering, or osteophytes.
-
Dull aches usually resolve within a year on their own.
-
If the joint is still painful, then excision of the distal clavicle can be performed.
-
Nonunion of a coracoid base fracture can be very painful.
-
This should be treated with bone graft and stabilization.
-
-
Neurologic injuries may occur early or late, such as brachial plexopathy.
-
Fractures of the clavicle, acromion, or coracoid can occur with the initial injury.
-
Persistent pain in the AC joint after a
stable type I or II injury may be due to osteolysis of the distal
clavicle or interposed tissue, such as torn ligaments, loose cartilage,
or meniscus.-
This should be treated with distal clavicle excision and joint debridement.
-
-
With stable type I and II injuries, the CC ligament is intact and thus the AC joint is stable.
-
There is some discussion about “unstable” type II injuries.
-
These may be under diagnosed type III injuries.
-
-
There is also a group of patients who have increased AP instability without superior migration.
-
These do not respond well to a distal clavicle resection.
-
-
Operative management of acute (<6
weeks) type III injuries is often reserved for open injuries, brachial
plexopathy, severe type III dislocations, and rarely high-level
overhead athletes. -
Operative management of chronic (>6
weeks) type III injuries is indicated for failure of nonoperative
treatment with continued AC joint pain and instability. -
Type IV, V, and VI injuries require early
operative reconstruction because of the severe displacement of the
joint, pain, and deformity.
-
Many surgical procedures have been
described for the management of AC separations. There is controversy
over the proper surgical technique, and no treatment has emerged as
ideal.-
These procedures can be broken down into
five groups: excision of the distal clavicle, dynamic muscle transfer,
reconstruction of the CC ligaments, fixation between the clavicle and
coracoid, and fixation across the AC joint. -
With most operative techniques, authors recommend debridement of the AC joint and repair of the deltotrapezial fascia.
-
-
This is used mainly for degenerative but stable AC joints that have failed nonoperative management.
-
The procedure can be done open (Mumford) or arthroscopically (Flatow).
-
Follow-up studies on open and arthroscopic distal clavicle excisions yield similar results, with 80% to 90% success rates.
-
Surgeons who are comfortable with
arthroscopic techniques have the opportunity to also visualize the
glenohumeral joint and look for undiagnosed superior labral
anterior-posterior (SLAP) tears.-
Berg and Ciullo noted that, of 20
patients who had a failed distal clavicle excision with presumed
osteoarthritis of the AC joint, 15 of these patients had superior
labral tears on arthroscopic evaluation at repeat procedure, and 9 of
the 15 patients improved after definitive management of this problem.
-
-
-
The patients who undergo distal clavicle
excision should be warned about weakness of the bench press motion but
no other significant long-term disability. -
The amount to resect is controversial, with some authors recommending 5 to 7 mm and some 20 to 25 mm.
-
The resection should be even and the superior capsule and ligament, as well as the CC ligament should be protected.
-
Inferior osteophytes on the distal clavicle should be excised.
-
Patients with unstable AC joints and distal clavicle fractures are not good candidates for excision.
-
Using distal clavicle excision alone fails to address instability if it exists.
-
Postoperatively, the patients are placed in a sling and allowed to do active and passive range of motion.
-
They are encouraged to use the arm for everyday activities but to refrain from overhead activities until the pain has subsided.
-
At 1 week postoperatively, strengthening exercises are begun and patients are allowed to return to all activities as tolerated.
-
This procedure involves transferring the
tip of the coracoid process and the attached coracobrachialis and short
head of the biceps to the undersurface of the clavicle, fixing in place
with a screw. -
The muscles then act as an active depressor of the clavicle.
-
There is a risk of injury to the musculocutaneous nerve.
-
Another problem with this technique is
that it reconstructs a static restraint with dynamic tissue, allowing
motion and leading to continued pain.
-
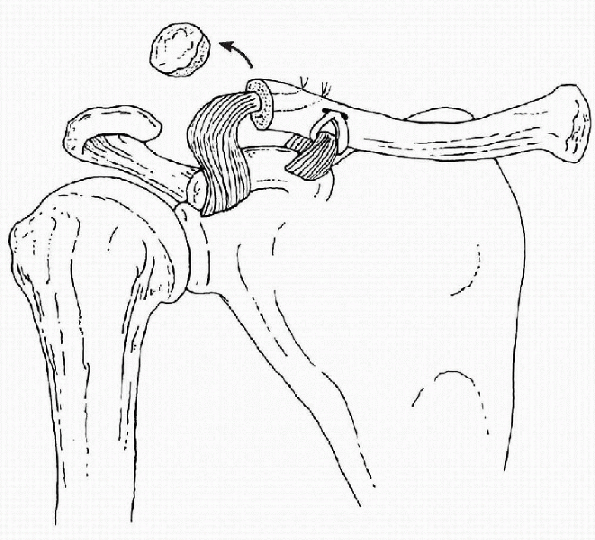
In the Weaver-Dunn technique (Fig. 20-4),
the distal clavicle is excised, and the acromial end of the CA ligament
is transferred to the remaining distal clavicle as a reconstruction for
the CC ligaments.-
A problem with this technique is weak initial fixation to the clavicle, which is via sutures.
-
Another issue is that the AC joint is not anatomically reduced in this procedure.
-
-
These problems have been addressed by
Morrison and Lemos via a Modified Weaver-Dunn technique, which consists
of passing an augmentation device through the clavicle and through or
around the coracoid, anatomically reducing the clavicle and stabilizing
the reconstruction while the CA ligament transfer matures.-
The augmentation device can wear through
the bone, amputating the clavicle or coracoid, and may produce a
foreign body response in the local tissue, leading to a hypertrophic
scar and osteolysis.
-
-
The CA ligament has an important role in shoulder stability, preventing superior migration of the humeral head.
-
Lee et al. showed
that the CA ligament also restrains anterior and inferior translations
of the humeral head through an interaction with the coracohumeral
ligament.
-
-
Jones and Lemos have described
reconstructing the CC ligaments by passing a semitendinosus tendon
autograft or tibialis anterior tendon allograft around the base of the
coracoid and through a 6-mm drill hole in the anterior third of the
clavicle.-
This has been done both in revision and primary procedures.
-
This reconstruction is augmented by
suture fixation between the coracoid and clavicle to prevent early
failure of the graft while it is healing. -
Revascularization of the graft, as with
anterior cruciate ligament reconstructions, is assumed and the graft
may stretch out over time.
-
-
Lee et al.
performed a biomechanical study on cadaveric shoulders, comparing the
strength of the native CC ligaments with reconstructions using CA
ligament transfer, suture repair, tape repair, and tendon grafts.-
They found that tendon grafts had the
same peak load as the native ligaments, were stronger than the CA
ligament transfers and suture repairs, and were stiffer than CA
ligament transfers.
-
 |
|
Figure 20-4 Modified Weaver-Dunn technique for reconstruction of the CC ligaments.
|
-
The goal of this technique is to keep the
clavicle and coracoid in a reduced position long enough to allow
primary healing of the CC ligaments, assuming that the ligaments will
heal at the preinjury length and strength. -
Bosworth described placing a screw
through the clavicle into the base of the coracoid process, which
requires later surgical removal.-
A stab wound is made 4 cm medial to the distal end of the clavicle.
-
A drill hole is made in the clavicle.
-
The clavicle is depressed and reduced to
the coracoid, an awl is used to make a hole in the superior aspect of
the base of the coracoid, and a screw is inserted.
-
-
Others have placed cerclage material
around the clavicle and coracoid, such as wire or Dacron tape, which
can lead to similar problems with the augmentation device used in the
modified Weaver-Dunn, such as coracoid or clavicle amputation, scar,
and osteolysis.
-
Fixation has been described using pins, suture, suture wires, and hook plates.
-
Any hardware, like CC screws, requires later removal at 6 to 8 weeks.
-
Usually, reconstruction of the AC or CC ligaments is also done.
-
The pin is inserted laterally to the AC joint, across the joint, and into the clavicle.
-
Alternatively, the pin can be drilled
retrograde from the joint through the acromion, then drilled antegrade
across the joint into the clavicle.
-
-
With pin fixation, there is a risk of
breakage and migration of the pins into the lung, heart, great vessels,
spinal cord, mediastinum, and many other vital structures, which leads
to serious consequences, including death.-
There is also a reported increased risk of AC arthritis.
-
-
Hook plates violate the joint, requires later surgical removal, have a risk of infection, and may bend or dislocate.
-
This fixation is rarely used now a result
of the complications; however, there have been recent reports of
bioabsorbable devices not requiring later removal.
-
-
More recently, several authors have discussed arthroscopic reconstruction of the AC joint.
-
We prefer a combination of an autograft
CA ligament transfer or a tibialis anterior tendon allograft around the
coracoid and through the clavicle with a synthetic augmentation between
the clavicle and the coracoid.
-
The patient is placed in the modified beach chair position.
-
A large radiograph cassette is placed under the patient’s AC joint.
-
Routine prepping and draping of the extremity are carried out.
-
A horizontal skin incision is made, 5 cm
long, beginning 1 cm lateral to the AC joint and taken medially along
the anterior edge of the clavicle. -
Similarly, a vertical skin incision just lateral to the coracoid may be used.
-
Subcutaneous flaps are developed superior
and inferior to the AC joint to allow adequate exposure of the
deltotrapezial fascia and distal 6 cm of clavicle. -
The deltotrapezial fascia is incised, exposing the lateral clavicle and AC joint.
-
Next, the clavicular periosteum is
incised along the anterior edge, and subperiosteal dissection is done,
exposing the distal 3 cm of clavicle.
-
In cases in which the articular surfaces
of the clavicle and acromion are normal, distal clavicle excision need
not be performed. This is rare in our experience. -
In most cases in which there is damage to
the articular cartilage (or in revision cases), 5 to 8 mm of the
lateral clavicle is resected with a sagittal bone saw. -
This is done in line with the AC joint, slightly obliquely, from superior lateral to posterior medial.
-
The coracoid is identified.
-
The deltoid is split along the line of the fibers using electrocautery.
-
The CA ligament is identified and kept intact.
-
Using electrocautery, a subperiosteal
incision is made on the superior aspect of the coracoid base, and the
coracoid is exposed medially and laterally. -
A looped suture passer is passed around the base.
-
An augmentation device is passed through or around the coracoid and tagged for later use.
-
The clavicle is identified.
-
Any sharp edges are beveled.
-
A 2 × 6 mm burr hole is placed in the
clavicle at the junction of its anterior and middle third, 3 cm medial
to the AC joint, and directly above the base of the coracoid. -
Medial placement of this drill hole
allows the graft to provide tension along the same vector as the normal
CC ligaments, and an anatomic reduction of the clavicle can be obtained. -
Two smaller drill holes are placed medial and lateral to the burr hole for later passing of the augmentation sutures.
-
If a CA ligament transfer is performed,
the acromial insertion of the ligament is identified and harvested with
a small 3 to 5 mm wafer of acromion. -
The coracoid attachment is left intact.
-
The acromial side is sutured with a no. 2 nonabsorbable braided material.
-
This construct is then passed through the end of the clavicle.
-
The ends of the tibialis anterior allograft are secured with a no. 2 suture using a tendon suture technique.
-
Many different synthetic augmentations have been used.
-
The graft and augmentation sutures are
placed into the previously placed suture loops around the coracoid base
and then passed around the base of the coracoid. -
The augmentation suture is passed through the two smaller drill holes in the clavicle.
-
The clavicle is overreduced by 5 mm to the acromion.
-
A knot is tied under tension inferior to the clavicle to prevent knot prominence.
-
The augmentation suture will provide provisional fixation while the graft reconstruction reorganizes.
-
The graft is passed through the inferior aspect of the burr hole in the clavicle and reapproximated.
-
The sutures are tied together, then supplemented with additional no. 2 sutures.
-
Residual graft tissue is excised.
-
Copious irrigation is performed.
-
The deltotrapezial fascia is carefully reapproximated with a no. 2 suture using a mattress suture technique.
-
Routine closure of the subcutaneous tissue and skin then follows.
-
A compressive dressing, sling, and swathe are applied.
-
The patient is placed in a sling and swathe postoperatively.
-
For activity, the patient starts gentle, active-assisted range of motion on postoperative day 1.
-
The swathe can be removed in a few days, and the sling is used for 6 weeks.
-
At 6 weeks, the patient may progress to active range of motion and strengthening.
-
No heavy lifting or pushing is allowed for 6 months.
-
Any hardware should be removed at 6 to 8 weeks.
-
Morrison and Lemos looked at 14 patients
with minimum 2-year follow-up, with a 34 of 36 University of
California-Los Angeles (UCLA) score.-
Similarly good to excellent results can be obtained using allograft reconstruction.
-
-
Harris et al. did a cadaver study comparing various methods of reconstruction.
-
They found that CC slings and suture anchors provided good strength but with greater deformations.
-
Screw fixation provided good stiffness and strength but only if bicortical purchase was obtained.
-
CA transfers were the weakest, the least stiff, and required augmentation.
-
There are many complications related to
operative treatment, including wound and bone infection, hardware
migration or failure, erosion or fracture due to augmentation devices,
arthritis, and recurrent pain and deformity. -
Death from migrating pins from the AC joint to the lungs, chest, heart, and mediastinum has been described.
-
Physeal injuries and pseudodislocation through an intact periosteal sleeve occur in children and adolescents.
-
Radiographs show a large increase in the CC interspace.
-
This can be a Salter Harris I or II
injury, in which the epiphysis remains congruous with the acromion
while the distal clavicle metaphysis is displaced. -
The CC ligament is intact and attached to the periosteal sleeve.
-
This is treated nonoperatively with good results.
-
Coracoid process fractures, usually of the base, can occur with AC joint dislocation but are an uncommon injury.
-
Usually, the CC ligaments remain attached to the coracoid process fragment.
-
The fracture through the coracoid base allows the clavicle to become high-riding, compared with the acromion.
-
Axillary and Stryker notch views can be helpful with showing this fracture, or a CT scan can be done.
-
Both operative and nonoperative treatments have been described, with similar results.
-
Any AC joint injury can lead to posttraumatic osteoarthritis of the AC joint.
-
Osteoarthritis can also occur in conjunction with rotator cuff tears and glenohumeral osteoarthritis.
-
The patient will present with shoulder pain.
-
On physical examination, the patient will
have tenderness to palpation over the AC joint and have pain with
crossed-body adduction. -
Radiographs will reveal narrowing of the AC joint, cystic changes, and osteophytes.
-
Conservative therapy is the first line of
treatment and consists of nonsteroidal anti-inflammatory medications,
activity modification, passive range of motion, strengthening
exercises, iontophoresis, and ice. -
An intra-articular steroid injection can
also be done as both a diagnostic and therapeutic test, taking care not
to inject the subacromial space. -
If symptoms persist after 12 months of
conservative treatment, then excision of the distal clavicle can be
performed either openly or arthroscopically.
associated with significant trauma. The spectrum of injury includes SC
subluxation and dislocation, injuries to the medial clavicular physis,
and degenerative joint arthritis. These injuries carry potential risks
due to the proximity of the great vessels and mediastinal structures
(such as the trachea and esophagus) that lie directly beneath the SC
joint.
intrauterine week 5 and is the first long bone to ossify. However, the
medial clavicular physis is the last to appear, the last to ossify at
age 18 to 20 years old, and fuses with the shaft of the clavicle at age
23 to 25 years old. A complete union may not even be present until age
31. This is important to remember because an SC joint dislocation in a
young patient may actually represent a fracture through the medial
clavicle physis.
articulation between the upper extremity and axial skeleton and, as a
result of this, almost any motion of the upper extremity is transferred
to the SC joint. The articular surfaces are covered with
fibrocartilage. The medial end of the clavicle is large, bulbous,
concave front to back, and convex vertically. It articulates with the
clavicular notch of the sternum to form a saddle-shaped joint. Less
than 50% of the clavicle articulates with the sternum, and the joint
surfaces are not congruent, leading to the least amount of osseous
stability of any joint in the body. In 2.5% of patients, the medial
clavicle has an inferior facet that articulates with the first rib. The
SC joint has motion in all planes (Fig. 20-5).
forces with all movements of the upper extremity, it is rarely
dislocated because of the stout ligaments supporting it. The SC
ligaments are important in preventing downward displacement of the
distal clavicle. This includes the intra-articular disc ligament, the
costoclavicular ligament, the interclavicular ligament, and the
capsular ligament.
synchrondral junction of the first rib and sternum, passes through the
SC joint dividing it into two spaces, and attaches to the superior and
posterior aspects of the medial clavicle. The disc then blends in with
the capsular ligament. It is a dense fibrous structure that rarely has
a perforation
connecting the two spaces. It acts to prevent medial displacement of the inner clavicle.
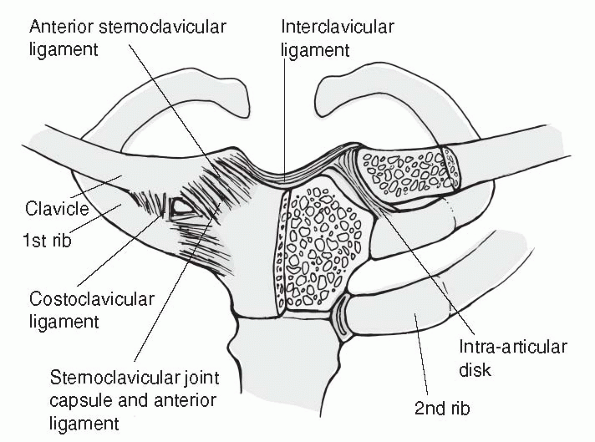 |
|
Figure 20-5
SC joint. (From Oatis CA. Kinesiology: The Mechanics and Pathomechanics of Human Movement. Baltimore: Lippincott Williams & Wilkins, 2004.) |
ligament, has a twisted appearance and anterior and posterior fasciculi
with a bursa between the two. The anterior fasciculus originates from
the anteromedial aspect of the first rib and passes upward and
laterally to attach to the clavicle. The anterior fibers act as a
checkrein against upward rotation and lateral displacement of the
clavicle. The posterior fasciculus fibers are shorter, arise laterally
to the anterior fasciculus fibers on the first rib, and pass upward and
medially. The posterior fibers resist downward rotation and medial
displacement of the clavicle. The costoclavicular ligament is short and
strong, and the crossing of the fasciculi provides stability to the
joint, similar to the CC ligament.
aspect of the clavicle with the capsular ligaments and the upper
sternum and also helps to hold up the shoulder.
capsule anteriorly and posteriorly, and the clavicular attachment is
mainly onto the epiphysis. The capsular ligament has been shown to be
the most important ligament in preventing anterior, posterior, and
upward displacement of the medial clavicle, as well as downward
displacement of the distal clavicle.
know that anatomy well because there are vital structures in this area.
Posterior to the SC joint and medial clavicle is a curtain of
muscles—the sternohyoid, sternothyroid, and scalenes—which covers the
vital structures. The vital structures include the brachiocephalic
artery, brachiocephalic vein, vagus nerve, phrenic nerve, internal
jugular vein, trachea, and esophagus. The arch of the aorta, superior
vena cava, and right pulmonary artery are also very close to the SC
joint. The anterior jugular vein also runs between the curtain of
muscles and the clavicle, and can vary in size up to 1.5 cm.
shoulder injuries. Bilateral dislocations are reported infrequently. A
significant amount of force is needed to produce a traumatic
dislocation of the SC joint. This can be direct or indirect. With a
direct force to the anteromedial clavicle, the clavicle is displaced
posteriorly into the mediastinum. An indirect force to the
anterolateral or posterolateral aspect of the shoulder can lead to a
posterior or anterior dislocation of the SC joint, respectively. An
indirect mechanism is more common than direct.
and sports account for 21%. The dislocation usually occurs anteriorly
because the posterior capsular ligaments are stronger than the
anterior. Atraumatic subluxation of the SC joint has been described in
individuals with generalized ligamentous laxity and in a patient with
pseudarthrosis of the first and second ribs.
-
A patient with an SC joint injury will complain of severe pain with any movement of the arm.
-
The head may be tilted toward the injured side.
-
The injured arm will be held across the trunk and supported by the uninjured arm.
-
With a dislocation, the affected shoulder is shortened and thrust forward.
-
The pain is worse when supine.
-
With an anterior SC joint dislocation, the medial end of the clavicle is prominent and palpable anterior to the sternum.
-
With a posterior dislocation, the medial
clavicle is posterior to the sternum, not palpable, and less prominent,
whereas the sternum is more easily palpable. -
With a posterior dislocation, the
subclavian and mediastinal structures may be compressed, leading to
venous congestion in the neck or upper extremity, breathing
difficulties, choking sensation, decreased blood flow to the arm, and
even hypotension and shock.
-
-
Clinically, it can be difficult to tell the difference between an anterior and posterior dislocation.
-
An SC dislocation can sometimes be picked up on a routine chest x-ray.
-
Rockwood described the serendipity view, which is a 40-degree cephalic tilt view of both SC joints.P.264
-
With an anterior dislocation, the clavicle will appear to be superiorly displaced compared with the uninjured side.
-
With a posterior dislocation, the clavicle will lie inferiorly.
-
-
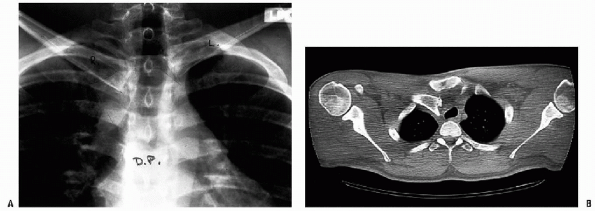
CT is the best radiographic study for evaluating SC joint injuries (Fig. 20-6).
-
It can show fractures of the medial clavicle, physeal injuries, and subtle subluxations.
-
It is important to compare the uninjured side with the injured side.
-
-
With chronic posterior SC dislocations, other imaging modalities have been described.
-
Dynamic ultrasound of the subclavian artery has been used to show compression of the artery during elevation of the arm.
-
-
Nerve conduction studies can also confirm a suspected brachial plexus neuropathy.
-
Because the medial clavicular physis is
the last to ossify at age 18 to 20 years of age and fuses with the
shaft of the clavicle at age 23 to 25 years old, an SC joint
dislocation in a young 20-year-old may actually be a physeal injury to
the medial clavicle. -
Closed reduction of posterior physeal injuries should be performed if they are less than 10 days from the injury.
-
After 10 days, if there are no signs of
mediastinal compromise, the injury should be treated symptomatically,
because the majority of physeal injuries will heal with time without
surgery and remodeling will eliminate any deformity. -
If there are symptoms from pressure on
the subclavian vessels and mediastinum—such as difficulty breathing,
difficulty swallowing, arm swelling, or poor circulation—a closed
reduction should be attempted, no matter how far out from the injury
and an open reduction is indicated if there is failure of closed
reduction. -
At the time of surgery, the
intra-articular disk and the more lateral epiphysis have been found to
stay with the sternum and be held in place by the capsular ligament.-
This is important to note because the epiphysis should not be excised with the intra-articular disk ligament.
-
 |
|
Figure 20-6 A: Routine AP x-ray of posteriorly dislocated right SC joint. B:
The AP view is suggestive of a posterior dislocation. However, the CT scan clearly demonstrates the posteriorly displaced right medial clavicle. Note the displacement of the trachea. (From Bucholz RW, Heckman JD. Rockwood and Green’s Fractures in Adults, 5th ed. Lippincott Williams & Wilkins, 2001.) |
-
Acute sprains of the SC joint can be mild or moderate.
-
With a mild sprain, the ligaments are all intact and the joint is stable.
-
This can be painful and is treated with ice, a sling for 3 or 4 days, and then gradual use of the arm as tolerated.
-
-
With a moderate sprain, the joint is subluxated anteriorly or posteriorly and the ligaments may be partially disrupted.
-
This should be treated by holding the
shoulders back with a clavicle strap to keep the joint reduced and a
sling and swathe to prevent arm motion for 4 to 6 weeks.
-
-
-
Atraumatic subluxation of the medial clavicle usually occurs in adolescents and young adults.
-
It can be due to generalized ligamentous laxity or a pseudarthrosis between the first and second ribs.
-
This is treated nonoperatively.
-
If the patient continues to be symptomatic, a CT scan should be performed to look for any bony anomalies.
-
Surgery should be reserved for patients with persistent pain, instability, or limitation in activities of daily living.
-
-
It can be difficult to differentiate between an anterior and posterior dislocation of the SC joint on physical examination only.P.265
-
A CT scan is recommended to further evaluate SC joint injuries.
-
There is controversy over the treatment of anterior dislocations.
-
-
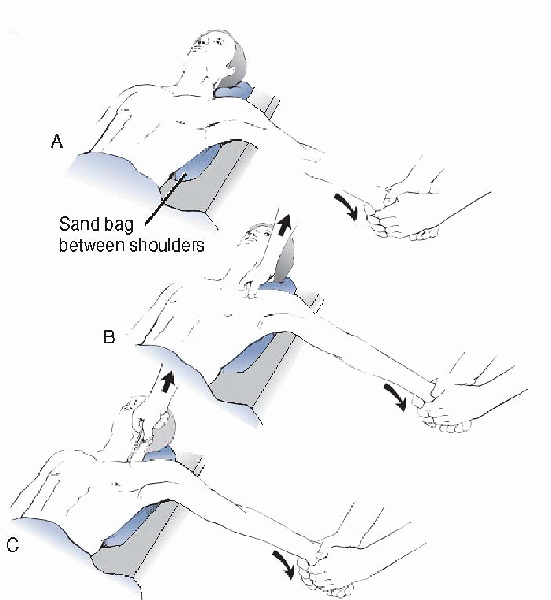
Although most acute anterior dislocations
are unstable after reduction, it is nonetheless recommended that closed
reduction be attempted if the patient presents less than 10 days from
the injury (Fig. 20-7).-
This can be done under local or general anesthesia.
-
The patient is placed supine with a 3- to 4-inch roll between the scapulae.
-
Gentle pressure over the anteriorly
displaced medial clavicle may reduce the dislocation; however, when the
pressure is released, the joint usually redislocates.
-
-
If the patient already has fusion between
the medial clavicle physis and the clavicular shaft, then the anterior
clavicle would be expected to have an anterior prominence of the medial
clavicle.-
This does not seem to cause problems, even with heavy manual labor.
-
-
If the SC joint remains reduced with the shoulders held back, a figure-eight strap can be used.
-
Some authors have recommended a bulky pad over the anteromedial clavicle to hold it reduced.
-
The shoulder should be immobilized for 6 weeks, and strenuous activities should not be done until 8 weeks.
-
-
If the SC joint redislocates after the
immobilization is discontinued, a figure-eight strap or sling can be
used until the patient is comfortable. -
Open operative procedures should not be
done for an anterior SC joint dislocation because the complications are
too great, end results are unsatisfactory, and the patient usually does
fine with residual prominence.
 |
|
Figure 20-7 Technique for closed reduction of the SC joint. A:
The patient is positioned supine with a sandbag placed between the two shoulders. Traction is then applied to the arm against countertraction in an abducted and slightly extended position. In anterior dislocations, direct pressure over the medial end of the clavicle may reduce the joint. B: In posterior dislocations, in addition to the traction, it may be necessary to manipulate the medial end of the clavicle with the fingers to dislodge the clavicle from behind the manubrium. C: In stubborn posterior dislocations, it may be necessary to prepare (sterilely) the medial end of the clavicle and use a towel clip to grasp around the medial clavicle to lift it back into position. (From Bucholz RW, Heckman JD. Rockwood and Green’s Fractures in Adults, 5th ed. Lippincott Williams & Wilkins, 2001.) |
-
A posterior dislocation of the SC joint requires prompt examination and reduction, either closed or open.
-
Because of pressure on the hilar
structures, it has been associated with respiratory distress, venous
congestion, arterial insufficiency, brachial plexus compression, and
myocardial conduction abnormalities. -
Damage to the pulmonary and vascular systems needs to be ruled out.
-
When indicated, aortography, pulmonary consult, and vascular consult should be obtained before reduction.
-
-
If the patient presents within 10 days of the injury, closed reduction should be attempted.
-
The reduction should be done as early as
possible because there have been reports of greater difficulty reducing
dislocations more than 48 hours from the injury. -
Once the joint is reduced, it is almost always stable.
-
General anesthesia is usually needed because of pain and spasm.
-
-
There are two techniques used for closed reduction: abduction traction and adduction traction.
-
With the abduction-traction technique, the patient is placed supine with the injured shoulder near the edge of the table.
-
A 3- to 4-inch roll is placed between the scapulae.
-
The arm is abducted and lateral traction is applied.
-
The arm is then brought into extension, the clavicle reduces with an audible pop, and it is almost always stable.
-
It may be necessary to grasp the medial clavicle with one’s fingers to dislodge it from behind the sternum.
-
If this fails, then the skin is prepped
and a sterile towel clamp or reduction tenaculum is used to grasp the
medial clavicle and apply anterior traction, whereas lateral traction
is applied to the arm.
-
-
-
With the adduction-traction technique, the patient is also placed supine with a 3- to 4-inch roll between the scapulae.P.266
-
The arm is held adducted, whereas
downward pressure is exerted on the shoulders, and the medial clavicle
is levered over the first rib back into place.
-
-
After closed reduction, the patient should be placed into a figure-eight strap for 4 to 6 weeks.
-
If closed reduction fails, open reduction should be done for a posterior SC joint dislocation.
-
Most patients cannot tolerate the
symptoms associated with pressure on the mediastinal structures, and
even patients who are initially asymptomatic develop symptoms later on. -
It is important to be totally familiar
with the anatomy all around the SC joint. It is also recommended that a
thoracic surgeon be available in the case of rupture of a major vessel.
-
-
Wirth and Rockwood recommend resection of
the medial clavicle with maintenance, repair, or reconstruction of the
costoclavicular ligaments to stabilize the joint. This can be done
using suture, internal fixation across the joint, fascia lata, or
subclavius tendon.-
First, the medial clavicle is resected.
-
Next, two or three nonabsorbable sutures
are placed around the remaining medial end of the clavicle and through
the stump or scar of the costoclavicular ligaments, taking care not to
tighten the medial clavicle down to the first rib too much. -
If present, the capsular and intraarticular disk ligaments can also be sutured to the medial clavicle for stabilization.
-
Last, the periosteal sleeve is closed, which will stabilize the medial clavicle.
-
Metallic pin fixation should be avoided
because these have been reported to migrate and cause serious
complications, including death.
-
-
For a chronic posterior SC dislocation
with an associated thoracic outlet syndrome, resection of the first rib
has been performed with good success.-
This approach avoids iatrogenic damage to
the mediastinal structures and instability of the medial clavicle after
resection, and leads to a cosmetic scar in the axillomammary skin
crease.
-
-
This is an uncommon injury but can be
quite disabling, and it should be considered in any patient with an
acute or chronic injury of the SC joint. -
A patient with an intra-articular disk
injury will present with complaints of clicking, grating, and popping
in the SC joint similar to a knee meniscal tear but have a stable joint. -
CT scan and arthrography have been used in diagnosis.
-
Keep in mind that 6% of intra-articular disks are incomplete and may be read as a tear.
-
These injuries are treated conservatively with ice and rest.
-
-
If symptoms persist, a local injection can be done as both a therapeutic and diagnostic test.
-
If the injection relieves the symptoms,
then the patient may benefit from an operation with an arthrotomy to
remove the disk and resect the medial clavicle if it is degenerative,
because this can also be a source of pain.
-
Degenerative arthritis of the SC joint results from a traumatic injury.
-
Conservative treatment with heat, anti-inflammatory medications, and rest is usually successful.
-
If the patient has persistent pain after
6 to 12 months of conservative treatment, a local injection can be done
as both a therapeutic and diagnostic test.-
If the pain is relieved temporarily, then resection of the SC joint is indicated.
-
-
The medial clavicle is resected, being careful to leave the costoclavicular ligament intact.
-
The residual stability of the distal clavicle should be constantly checked.
-
If too much of the medial clavicle is
resected, the patient will have recurrence of pain due to loss of
stability of the clavicle. -
This can lead to limited shoulder mobility, neurologic symptoms, thoracic outlet syndrome, and fatigue.
-
This problem presents as an anterior dislocation of the SC joint and a posterior dislocation of the AC joint.
-
Wirth et al. reviewed 22 cases of dislocations of both ends of the clavicle.
-
Most patients with this problem have been treated conservatively with satisfactory results.
-
One patient developed a brachial plexus neuropathy treated with excision of part of the clavicle.
-
Four patients had persistent pain localized to the AC joint and were treated with AC joint reconstruction.
-
-
Complications related to pressure on
hilar structures are mainly seen with posterior SC joint dislocations;
however, there is some concern for these problems late with posterior
physeal injuries. -
The only complications occurring after an anterior dislocation are cosmetic deformity and late degenerative changes.
-
The incidence of complications has been reported at 25%; however, only two deaths have been reported as a result of this injury.
-
Early complications after a posterior dislocation can affect the trachea, esophagus, or great vessels.
-
These can be very serious and include
pneumothorax, laceration of the superior vena cava, respiratory
distress, neck venous congestion, rupture of the esophagus with abscess
and osteomyelitis of the clavicle, fatal tracheoesophageal fistula,
pressure on the subclavian artery, occlusion of the subclavian artery,
heart conduction abnormalities, compression of the right common carotid
artery, brachial plexus compression, and voice changes.
-
-
Late complications after nonreduced retrosternal injuries can occur in patients who were initially asymptomatic.
-
Metallic pin fixation across the SC joint
should be avoided because these have been reported to migrate and cause
serious complications, including death. -
Smooth pins, threaded Kirschner pins,
pins with bent ends, and Hagie pins have all been reported to migrate
either intact or broken into the heart, pulmonary artery, innominate
artery, aorta, spinal cord, breast, subclavian artery, and base of the
neck.
SJ, Nicholas SJ, Akizuki KH, et al. Reconstruction of the
coracoclavicular ligaments with tendon grafts. Am J Sports Med 2003;31:
648-659.
MA, Rockwood CA Jr. Acute and chronic traumatic injuries of the
sternoclavicular joint. J Am Acad Orthop Surg 1996;4: 268-278.
