CHAPTER 6 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
CHAPTER 6 – Thermal Capsulorrhaphy
James R. Andrews, MD
With the advent of shoulder arthroscopy in the 1980s came the ability for surgeons to more closely examine the pathologic processes within the shoulder without significantly altering the status of the joint itself. Among the shoulder pathologic processes that became more appreciated with arthroscopy were superior labral tears, posterior capsulolabral injuries, intraarticular biceps disease, and partial rotator cuff tears. In throwing athletes, however, shoulder surgery had yielded only limited success with regard to return to play. Payne et al[13] demonstrated only a 40% return to play in patients treated with rotator cuff débridement who also had increased glenohumeral translation. Similarly, Speer et al[14] demonstrated that return to play was limited in throwers who underwent arthroscopic fixation of anterior labral tears for treatment of anterior instability. It was thought that the inability to control rotational laxity led to the lower rate of return to play.
Capsular and ligamentous tissues are composed predominantly of type I collagen. The application of heat to collagen causes a destruction of the heat-sensitive cross-links between fibrils, leading the collagen tissue to take on a more gel-like character rather than its normal crystalline-like state. This process, termed denaturation, has been shown to reproducibly occur at approximately 65°C, but the exact effect of heat application depends on exposure time, mechanical stress applied to the tissue during heat application, and method of application.[3] Thermal properties are not uniform in all connective tissues. The response to thermal energy depends on many factors, including species, age, hydration level, fibril orientation, and electrolyte concentration of the surrounding tissues. [4] [8] Increased temperatures have been shown to be required to produce denaturation in tissues with increased collagen content and in those under increased tensile loads.[4] The end result of heat application to collagenous tissues is visible shrinkage along the axis of the collagen fibril orientation.[2]
Thermal energy has been used to treat capsular disease of various degrees and causes in the shoulder. As mentioned earlier, thermal energy has been used to decrease rotational laxity in the thrower’s shoulder. It has also been used to address shoulder instability and multidirectional instability. Tibone et al[15] demonstrated that both anterior translation and posterior translation were decreased in human cadaveric shoulder specimens after thermal shrinkage of the anterior inferior capsule. In their study, anterior translation decreased more than 40% and posterior translation decreased 35% after application of thermal energy.
Fanton and Khan[6] began using radiofrequency as a modality to decrease capsular volume and capsular laxity in 1996. It was the work of these and other subsequent investigators that led to the increase in popularity of this modality as a means of improving the results of shoulder surgery in the overhead athlete by addressing the rotational laxity. The results of these works are discussed later.
Patients report a history of frank dislocation or, more commonly for this application, experience recurrent subluxation events. Overhead athletes, especially baseball pitchers, often describe a “dead arm” syndrome, with pain and subjective weakness occurring late in the throw.
A standard shoulder examination is performed, with special focus on assessing stability. Common tests include the apprehension sign, relocation test, sulcus sign, and load and shift test.
The diagnostic and imaging work-up includes conventional radiography and cross-sectional imaging modalities such as magnetic resonance imaging and computed tomography. Radiographic studies include standard anteroposterior and axillary lateral views as well as specialized views, such as the Stryker notch view, to rule out bone defects. Magnetic resonance imaging provides visualization of ligamentous and other soft tissue structures, such as the capsulolabral complex and rotator cuff. Computed tomography, especially when it is obtained in conjunction with arthrography, allows assessment of the bony structures to quantify or to rule out a Hill-Sachs defect or bony Bankart lesion.
Indications and Contraindications
Thermal capsulorrhaphy is indicated in mild to moderate cases of instability, especially when patients describe subluxation rather than dislocation events. It can be used as an adjunct to labral repair in patients with a capacious capsule.
Contraindications include bone defects of the glenoid and a compromised capsule.
This procedure can be performed under general anesthesia, interscalene block, or a combination of both. At our institution, we prefer to perform shoulder arthroscopy in the lateral decubitus position, although thermal capsulorrhaphy can be carried out in the beach chair position as well.
Surgical Landmarks, Incisions, and Portals
| • | Acromion | |
| • | Clavicle | |
| • | Coracoid | |
| • | Posterior soft spot |
| • | Posterior portal | |
| • | Anterior portal |
| • | Axillary nerve during application in the inferior pouch | |
| • | Musculocutaneous nerve during placement of the anterior portal |
Examination Under Anesthesia and Diagnostic Arthroscopy
After the induction of adequate general or regional anesthesia, examination under anesthesia is carried out on both shoulders to document and to confirm the amount of translation in each direction as well as the end feel of the translation. In addition, with the scapula braced, external rotation and internal rotation are measured with the arm abducted 90 degrees in the plane of the scapula. The patient is then positioned and prepared and draped with the shoulder exposed.
After insufflation of the glenohumeral joint with saline, a standard posterior arthroscopic portal is established and diagnostic arthroscopy is performed. Visualization of the glenoid and humeral articular surfaces is obtained, and the cartilage integrity is noted. Next, the biceps tendon is identified and viewed throughout its entire intraarticular course, including the anchor origin on the visible portion of the labrum. The anterior, posterior, and inferior recesses are viewed from the posterior portal. The undersurface of the rotator cuff is assessed for integrity. Next, a standard anterior portal is established under direct visualization. A blunt trocar is inserted through the cannula, and the rotator cuff, labrum, biceps tendon, and subscapularis tendon are probed to ensure integrity. Specific attention is placed on viewing and assessing the biceps anchor at the superior glenoid rim. In throwing athletes, this area is the most commonly affected as it pertains to the labrum. Careful attention is paid to retract the biceps tendon into the glenohumeral joint to view the most distal portion of the intraarticular tendon as it enters the bicipital groove. The arthroscope is then placed in the anterior portal to view the posterior capsule and posterior labrum and cuff. Any fraying of the articular surface, rotator cuff, or labrum is addressed at this time with use of a standard arthroscopic shaver, and portals are switched as needed to address the pathologic changes. If any labral or rotator cuff detachment is present, these pathologic processes are addressed appropriately before any capsular treatment.
Specific Steps (
Box 6-1
)
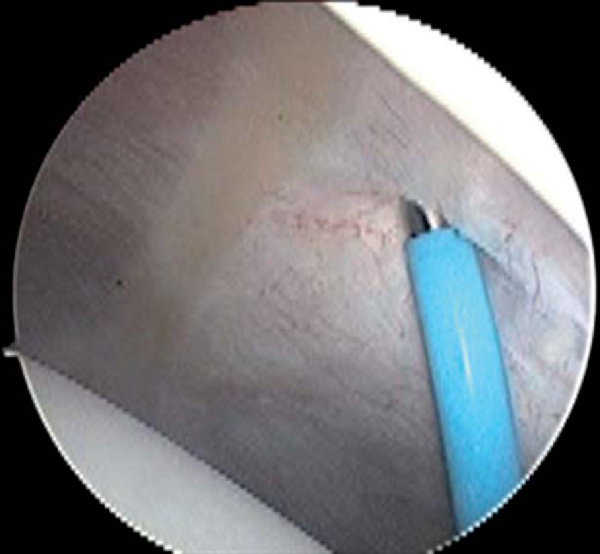
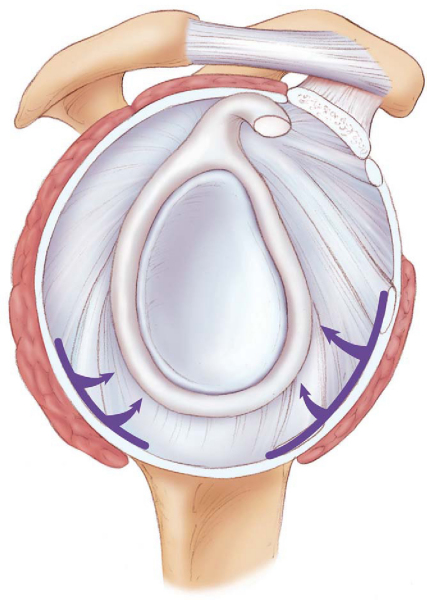
Once any other intraarticular pathologic process has been addressed, attention is turned to the joint capsule. If thermal capsulorrhaphy is to be carried out, the arthroscope is first placed in the anterior portal, and a plastic cannula with a flow diaphragm is placed in the posterior portal. The tip of the thermal probe is slightly bent (20 to 30 degrees) several centimeters from the tip to allow easier access to the capsule. The arthroscope is positioned anterior and inferior to the humeral head with the camera directed posteriorly to see the posterior inferior capsule in the region of the posterior band of the inferior glenohumeral ligament. The thermal probe is then directed to the area visualized through the scope, and the capsule is striped from the glenoid to the capsular insertion onto the humerus (Figs. 6-1 and 6-2 [1] [2]), leaving intervening normal unshrunk tissue between each stripe. The probe begins at the most inferior position and gradually moves proximally to the posterior portal.
| Surgical Steps | ||||||||||||
|
|
|
|
|
Figure 6-1 |
|
|
|
|
Figure 6-2 (Redrawn from Fanton GS, Zwahlen BA, Savoie FH III. Radiofrequency technique for shoulder instability. In Miller MD, Cole BJ, eds. Textbook of Arthroscopy. Elsevier, Philadelphia, 2004.) |
The arthroscope is then placed through the posterior portal and the plastic cannula is placed anteriorly. The arthroscope is directed posterior to the humeral head with the camera directed anteriorly to view the anterior band of the inferior glenohumeral ligament. The thermal probe is then inserted through the anterior portal and directed to the area of visualization. By the same technique, the anteroinferior capsule is striped with the probe, and gradual progression is made toward the anterior portal. In general, no thermal energy is used above the middle glenohumeral ligament.
If specific directional laxity is to be addressed with thermal capsular shrinkage, the probe can be used in only the area of interest. For example, in patients in whom anterior instability or anteroinferior capsular redundancy is the main pathologic process, thermal application to only the anterior or anterior inferior capsule may be chosen. Likewise, if the main direction of instability is posterior, thermal shrinkage of the posterior capsule with or without rotator interval closure or shrinkage may be sufficient.
The arthroscopy portals are closed with interrupted or subcuticular stitches. The arm is placed in a shoulder-immobilizing device before transport from the operating room.
Like many shoulder procedures, thermal capsulorrhaphy for the purpose of reducing rotational or directional laxity requires a closely supervised rehabilitation protocol for success to be achieved. Experience with this procedure has taught us that frequent hands-on treatment by a qualified physical therapist is vital to success. In each case, we seek to achieve external rotation in abduction to between 115 and 118 degrees by 12 weeks postoperatively. We do not allow any throwing until 16 weeks postoperatively, with the early rehabilitation focused on range of motion, followed by light strengthening and plyometric drills. By keeping in line with the therapy protocol, difficult situations like overtightening and premature stretching are avoided. Verbal communication of the goals and phases of the rehabilitation and the obligation of the patient to abide by the therapy protocol is essential.
Despite the predominance of good results with use of this modality, failure and complications are not uncommon. In our practice, we have decreased the frequency with which we use thermal energy for the treatment of the throwing athlete as we have become more proficient and knowledgeable in capsular plication. Reports of “vanished capsule” or obliterated tissue, chondral damage, and comparatively high recurrence rate have decreased the enthusiasm for this technique.
Study results with use of thermal energy are summarized in
Table 6-1
.
| Author | No. of Subjects | Followup | Outcome |
|---|---|---|---|
| Fanton and Khan[6] (2001) | 42 | 28 months | 91% returned to preinjury level |
| Mishra and Fanton[12] (2001) | |||
| Levitz et al[9] (2001) | 31 | 30 months | Thermally treated group: 90% returned to play at same or higher level |
| Traditionally treated group: 67% returned to play at same or higher level | |||
| Dugas and Andrews[5] (2002) | 170 | 8.5 months | 81% returned to competition |
| Lyons et al[11] (2001) | 24 months | 96% | |
| Frostick et al[7] (2000) | 28 | 83% | |
| Levy et al[10] (2001) | 40 months | Laser: 59% better | |
| 23 months | Radiofrequency: 76% better | ||
| Anderson et al[1] (2002) | 106 | 6.3 months | 14% failure rate |
Fanton et al [6] [12] reported the 2-year results of 42 young, active patients who underwent shoulder arthroscopy with thermal capsulorrhaphy. These patients underwent capsulolabral fixation with tacks or anchors and thermal capsular shrinkage for treatment of recurrent shoulder instability. At an average of 28 months of followup, 91% had returned to their preinjury level of sports. These authors also noted similar rate of success with thermal treatment of mild subluxation without the addition of capsulolabral repair.
Levitz et al[9] in 2001 described 31 overhead baseball players who underwent shoulder arthroscopy with thermal capsular shrinkage and compared them with 51 overhead baseball players who underwent shoulder arthroscopy with traditional treatment only, without thermal capsular shrinkage. In this report, at a mean of 30 months postoperatively, the thermal group demonstrated a 90% return to play at the same or higher level, whereas the traditional treatment group had only a 67% return to play at the same or higher level. Early results in this study showed an 80% return to competition at a mean of 7.2 months in the nonthermal group and a 93% return at an average of 8.4 months in the thermal group. In a subsequent review of our patients published in 2002,[5] 138 of the 170 total patients (81%) returned to competition at a mean of 8.5 months. The mean Athletic Shoulder Outcome Rating Scale score was 77 of 90, and the mean stability was rated 9.1 of 10. In the group who had knowledge of their velocity, 76% noted a decreased velocity of 3.4 mph on average.
Reviews on the treatment of multidirectional instability with thermal energy have also been completed. Lyons et al[11] reviewed their experience with arthroscopic laser capsulorrhaphy for the treatment of multidirectional instability. At 2-year followup, 96% of the laser-treated group was asymptomatic and had not had any further instability. In another report, Frostick et al[7] showed 83% satisfactory results in 28 patients with use of radiofrequency for the treatment of multidirectional instability.
Levy et al[10] published a combined series of patients in which one group was treated with laser capsulorrhaphy and the other group with radiofrequency capsulorrhaphy. mean follow-ups were 40 months and 23 months, respectively. In the laser group, early outcome measure averaged a score of 90 of a possible 100 but subsequently declined to an average of 80 at final followup. At a mean of 40 months postoperatively, only 59% rated their shoulders much better or better than before surgery. In the radiofrequency group, the mean outcome score throughout the followup period averaged 80 of 100, but 76% of patients rated their shoulders much better or better than before surgery.
Anderson et al[1] reported a 14% failure rate in 106 patients at a mean of 6.3 months. In their study, multiple previous dislocations and previous surgery were associated with a higher risk for failure.
1.
Anderson K, Warren RF, Altchek DW, et al: Risk factors for early failure after thermal capsulorrhaphy.
Am J Sports Med 2002; 30:103-107.
2.
Arnoczky SP, Aksan A: Thermal modification of connective tissues: basic science considerations and clinical implications.
J Am Acad Orthop Surg 2000; 8:305-313.
3.
Chen SS, Wright NT, Humphrey JD: Heat-induced changes in the mechanics of a collagenous tissue: isothermal, isotonic shrinkage.
J Biomech Eng 1998; 120:382-388.
4.
Chvapil M, Jensovsky L: The shrinkage temperature of collagen fibers isolated from the tail tendons of rats of various ages and from different places of the same tendon.
Gerontologia 1963; 1:18-29.
5.
Dugas JR, Andrews JR: Thermal capsular shrinkage in the throwing athlete.
Clin Sports Med 2002; 21:771-776.
6.
Fanton GS, Khan AM: Monopolar radiofrequency energy for arthroscopic treatment of shoulder instability in the athlete.
Orthop Clin North Am 2001; 32:511-523.
7.
Frostick SP, Sinopidis CT, Maskari SA, Richmond JC. Treatment of shoulder instability using electrothermally-assisted capsular shift. Presented at the 67th annual meeting of the American Academy of Orthopaedic Surgeons; Orlando, Fla; March 2000.
8.
Le Lous M, Cohen-Solal L, Allain JC, et al: Age related evolution of stable collagen reticulation in human skin.
Connect Tissue Res 1985; 13:145-155.
9.
Levitz CL, Dugas JR, Andrews JR: The use of arthroscopic thermal capsulorrhaphy to treat internal impingement in baseball players.
Arthroscopy 2001; 17:573-577.
10.
Levy O, Wilson M, Williams H, et al: Thermal capsular shrinkage for shoulder instability.
J Bone Joint Surg Br 2001; 83:640-645.
11.
Lyons TR, Griffeth PL, Field LD, Savoie FH: Laser assisted capsulorrhaphy for multidirectional instability of the shoulder.
Arthroscopy 2001; 17:25-30.
12.
Mishra DK, Fanton GS: Two-year outcome of arthroscopic Bankart repair and electrothermal assisted capsulorrhaphy for recurrent traumatic anterior shoulder instability.
Arthroscopy 2001; 17:844-849.
13.
Payne LZ, Altchek DW, Craig EV, Warren RF: Arthroscopic treatment of partial rotator cuff tears in young athletes.
Am J Sports Med 1997; 25:299-305.
14.
Speer K, Warren RF, Pagnani M, et al: Arthroscopic technique for anterior stabilization of the shoulder with a bioabsorbable tack.
J Bone Joint Surg Am 1996; 78:1801-1807.
15.
Tibone JE, Lee TQ, Black AD, et al: Glenohumeral translation after arthroscopic thermal capsuloplasty with a radiofrequency probe.
J Shoulder Elbow Surg 2000; 9:514-518.