Anconeus Arthroplasty
Editors: Morrey, Bernard F.
Title: Master Techniques in Orthopaedic Surgery: The Elbow, 2nd Edition
Copyright ©2002 Lippincott Williams & Wilkins
> Table of Contents > Part IV – Reconstruction > 23 – Anconeus Arthroplasty
23
Anconeus Arthroplasty
Bernard F. Morrey M.D.1
Alberto G. Schneeberger M.D.2
1 Mayo Medical School and Department of Orthopaedics, Mayo Clinic and Mayo Foundation, Rochester, Minnesota.
2 Department of Orthopedic Surgery, Balgrist, University of Zurich, Zurich, Switzerland.
The management of posttraumatic proximal radiohumeral
and radioulnar dysfunction, pain, or instability is a challenging
problem without well-documented solutions. The unreliability or
unsuitability of prosthetic replacement and lack of an alternate
solution has prompted the development of a proximally based soft-tissue
rotational arthroplasty procedure employing the anconeus muscle. The
attractiveness of this procedure is that the muscle is innervated and
vascularized from distinct vascular pedicles originating from the
recurrent posterior interosseous artery and from the medial collateral
artery (3). This allows the entire muscle to be
mobilized, leaving it attached to the triceps fascial expansion,
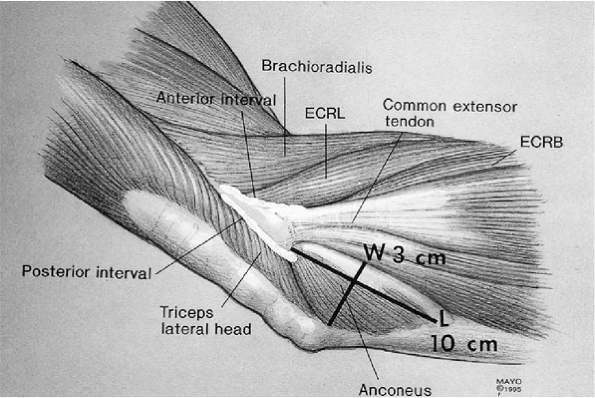
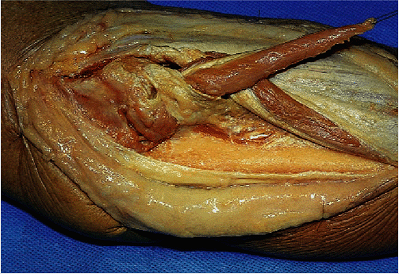
preserving its viability. Cadaver dissections have demonstrated a mean
length of approximately 9 to 10 cm and a width of about 3 cm (2) (Fig. 23-1),
sufficient to allow several variations of interposition procedures.
Furthermore, the absence of this muscle from its anatomic location does
not result in any measurable dysfunction or morbidity from a recovery
or functional perspective.
and radioulnar dysfunction, pain, or instability is a challenging
problem without well-documented solutions. The unreliability or
unsuitability of prosthetic replacement and lack of an alternate
solution has prompted the development of a proximally based soft-tissue
rotational arthroplasty procedure employing the anconeus muscle. The
attractiveness of this procedure is that the muscle is innervated and
vascularized from distinct vascular pedicles originating from the
recurrent posterior interosseous artery and from the medial collateral
artery (3). This allows the entire muscle to be
mobilized, leaving it attached to the triceps fascial expansion,
preserving its viability. Cadaver dissections have demonstrated a mean
length of approximately 9 to 10 cm and a width of about 3 cm (2) (Fig. 23-1),
sufficient to allow several variations of interposition procedures.
Furthermore, the absence of this muscle from its anatomic location does
not result in any measurable dysfunction or morbidity from a recovery
or functional perspective.
The procedure was first performed approximately 10 years
ago. Although there are few data regarding the long-term value of the
method (2), it is included here for the purpose
of introducing the concept as a potential but not necessarily a proven
or definitive solution for difficult reconstructive problems for which
reliable alternatives do not exist.
ago. Although there are few data regarding the long-term value of the
method (2), it is included here for the purpose
of introducing the concept as a potential but not necessarily a proven
or definitive solution for difficult reconstructive problems for which
reliable alternatives do not exist.
Indications/Contraindications
In general, this technique is employed in instances when
proximal radioulnar or radiohumeral dysfunction occurs following
trauma. The three primary indications for the procedure are:
proximal radioulnar or radiohumeral dysfunction occurs following
trauma. The three primary indications for the procedure are:
-
Radiohumeral impingement in which the interposition is principally directed at the proximal radiocapitellar articulation.
-
Proximal radioulnar impingement with or without radiohumeral impingement.
-
Limitation of forearm rotation due to
synostosis or fibrosis of the proximal radioulnar relationship in which
an interposition material is desired to eliminate recurrence or
impingement following resection (1,2).
P.410
 |
|
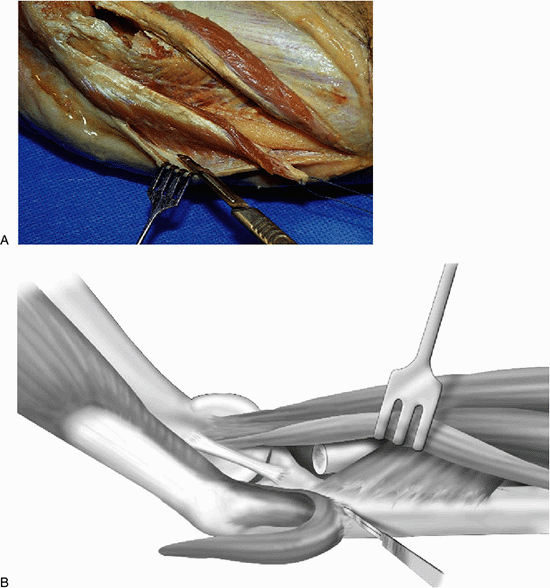
Figure 23-1.
The mean dimensions of the anconeus muscle are 9 to 10 cm in length and 3 to 3.5 cm in width at its fascial attachment to the triceps. |
The primary contraindication to this procedure is an
absent or devitalized anconeus muscle. A condition requiring a
procedure that resists high axial load along the radius would also rule
out use of an anconeus arthroplasty. Lastly, a deficient lateral ulnar
collateral ligament that cannot be reconstructed prohibits use of this
procedure.
absent or devitalized anconeus muscle. A condition requiring a
procedure that resists high axial load along the radius would also rule
out use of an anconeus arthroplasty. Lastly, a deficient lateral ulnar
collateral ligament that cannot be reconstructed prohibits use of this
procedure.
Surgery
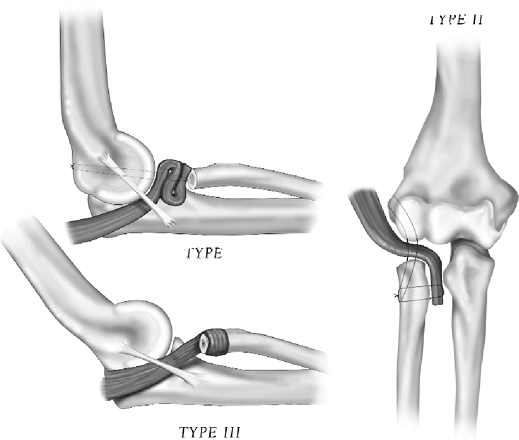
Several variations of the interposition have been used
and are classified as follows: type I, radiohumeral “roll-up”
interposition; type II, radiohumeral/radioulnar interposition; type
III, proximal radial “wrap” (Fig. 23-2). The
specific pathoanatomy determines which of the three types of
interposition is appropriate. The method of harvest is common for all
these applications.
and are classified as follows: type I, radiohumeral “roll-up”
interposition; type II, radiohumeral/radioulnar interposition; type
III, proximal radial “wrap” (Fig. 23-2). The
specific pathoanatomy determines which of the three types of
interposition is appropriate. The method of harvest is common for all
these applications.
Anconeus Harvest
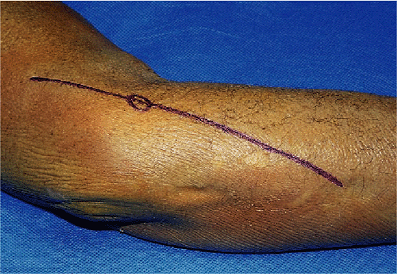
The patient is placed supine with the forearm brought
across the chest. Any previous incision in the region is entered, or a
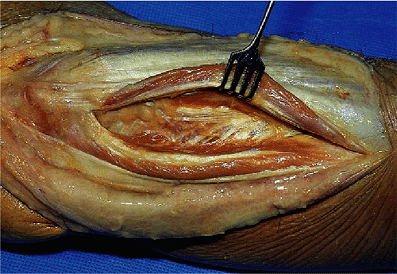
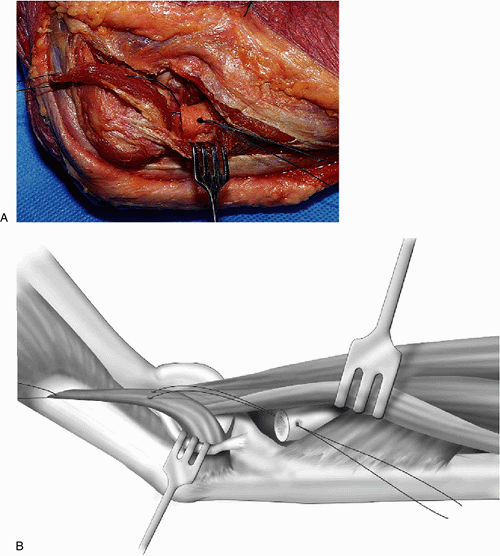
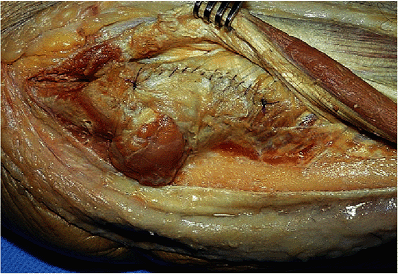
Kocher’s-type skin incision is made (Fig. 23-3). The interval between the anconeus and extensor carpi ulnaris is entered and expanded to expose the anconeus muscle (Fig. 23-4).
The dissection must be carried distally approximately 10 cm from the
lateral epicondyle to expose the distal-most aspect of this muscle
insertion. The tip of the anconeus is identified. The muscle is then
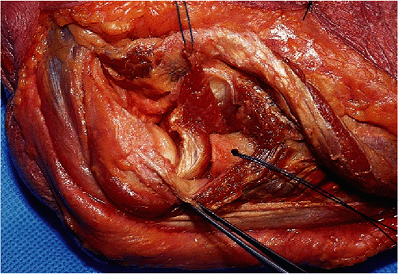
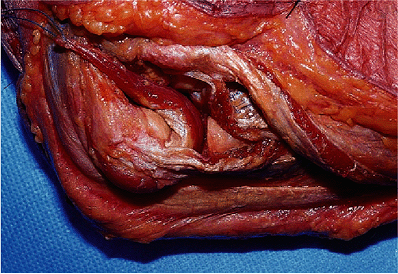
reflected from the ulna and from the common retinaculum (Fig. 23-5).
The dissection is carried proximal to the point of origin from the
fascial expansion and attachment to the triceps, retaining its
innervation and vascularity (Fig. 23-6).
across the chest. Any previous incision in the region is entered, or a
Kocher’s-type skin incision is made (Fig. 23-3). The interval between the anconeus and extensor carpi ulnaris is entered and expanded to expose the anconeus muscle (Fig. 23-4).
The dissection must be carried distally approximately 10 cm from the
lateral epicondyle to expose the distal-most aspect of this muscle
insertion. The tip of the anconeus is identified. The muscle is then
reflected from the ulna and from the common retinaculum (Fig. 23-5).
The dissection is carried proximal to the point of origin from the
fascial expansion and attachment to the triceps, retaining its
innervation and vascularity (Fig. 23-6).
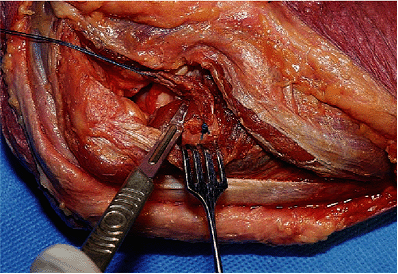
The lateral joint is entered anterior to the collateral
ligament and the relevant pathology is identified. The posterior margin
of the ligament is then identified. As in all instances, the transposed
muscle is placed under the lateral ulnar collateral ligament (Fig. 23-7).
ligament and the relevant pathology is identified. The posterior margin
of the ligament is then identified. As in all instances, the transposed
muscle is placed under the lateral ulnar collateral ligament (Fig. 23-7).
 |
|
Figure 23-2.
Variations of anconeus rotation/interposition arthroplasty: type I, radiohumeral; type II, radiohumeral/radioulnar; type III, radial “wrap.” |
 |
|
Figure 23-3. A Kocher skin incision is made.
|
 |
|
Figure 23-4. The interval between the anconeus and extensor carpi ulnaris is identified and developed.
|
 |
|
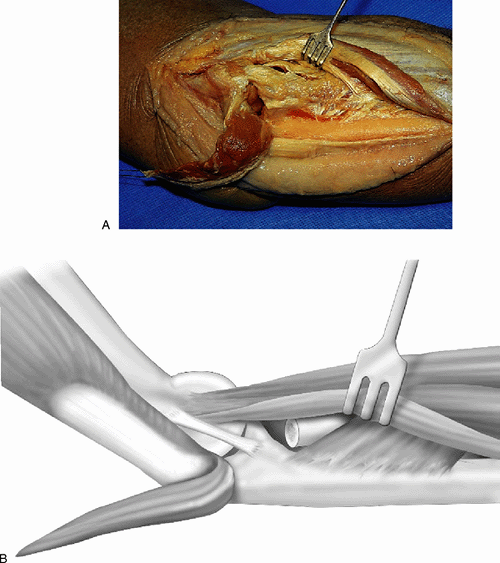
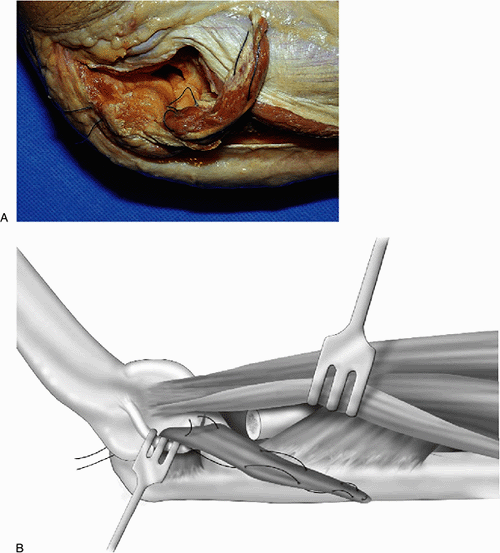
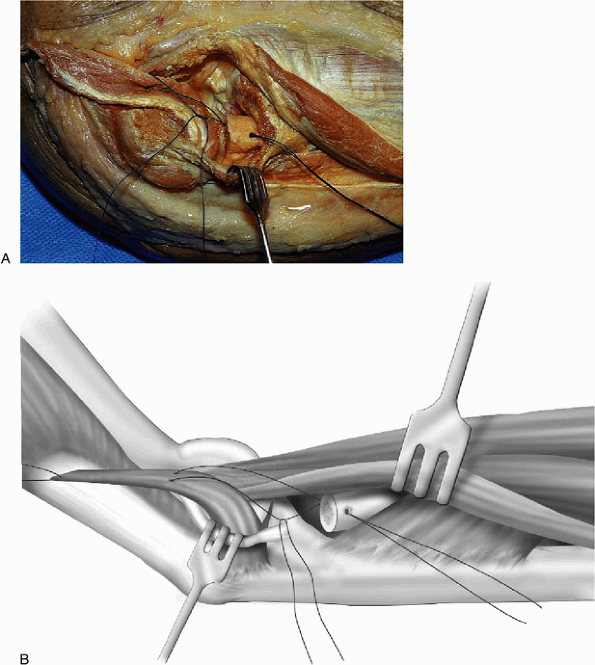
Figure 23-5. A,B: The distal aspect of the anconeus is isolated and the muscle is elevated from its bed and from the forearm fascia.
|
 |
|
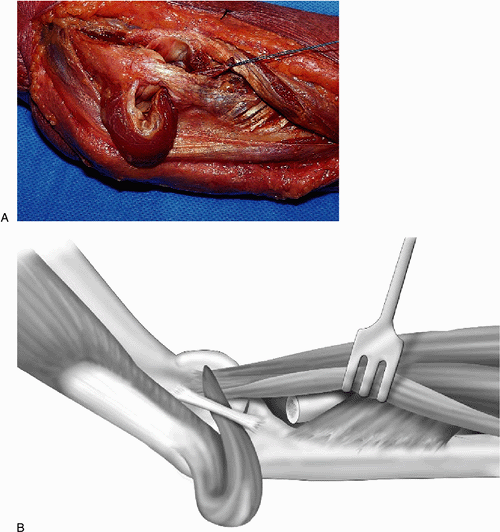
Figure 23-6. A,B: The anconeus is reflected proximally on its pedicle attachment to the triceps.
|
 |
|
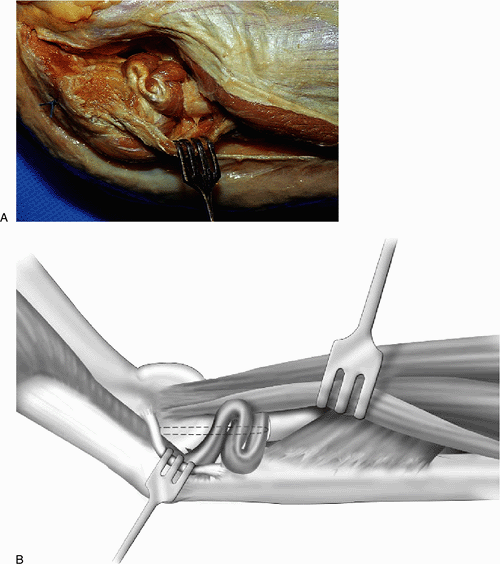
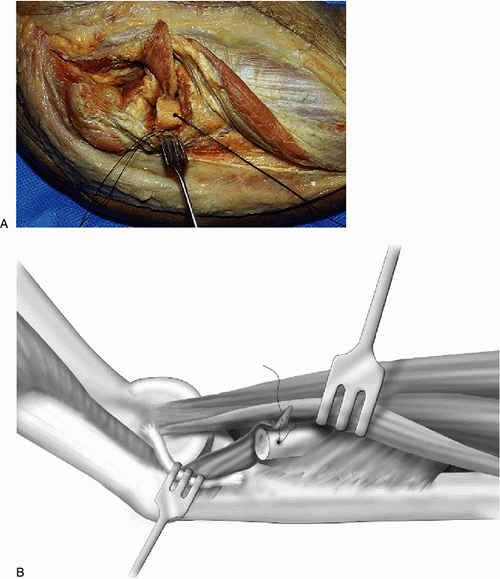
Figure 23-7. A,B: In all instances, the muscle is inserted into the joint under the lateral ulnar collateral ligament.
|
P.411
P.412
P.413
P.414
Type I: Interposition at the Radiohumeral Joint
The integrity of the lateral collateral ligament is assessed. If this is inadequate, it is reconstructed as described in Chapter 15 or is reinforced with a No. 5 nonabsorbable suture as described in Chapters 5 and 7.
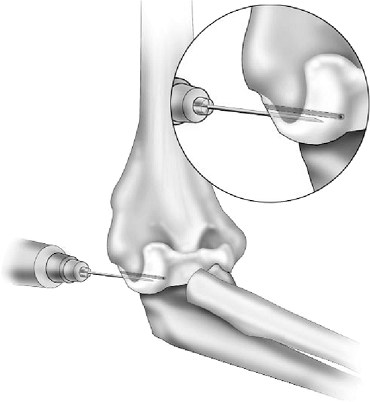
If reconstructed, the graft is usually positioned first and then
secured at the conclusion of the anconeus reconstructive procedure. Two
drill holes are placed from posterior to anterior through the
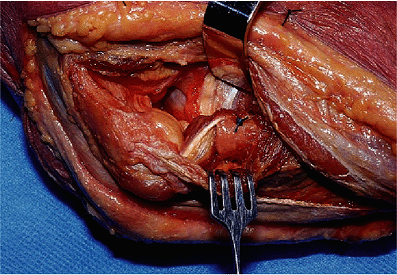
midportion of the capitellum approximately 5 to 7 mm apart (Fig. 23-8), and the anconeus is brought under the intact or reconstructed lateral ulnar collateral ligament (Fig. 23-9).
A nonabsorbable suture is passed through one of the two drill holes,
then into the anconeus from proximal to distal in such a way as to
allow the anconeus to fold on itself when tension is placed on the
suture (Fig. 23-10). The suture then passes
through the second drill hole in the capitellum and is pulled taut,
allowing the anconeus to fold on itself and fill the space created by
the absent radial head (Fig. 23-11). The
remnants of the collateral ligament are repaired or reinforced. The
fascia is approximated to the posterior aspect of the extensor carpi
ulnaris (see Fig. 23-22). The remainder of the closure is routine.
If reconstructed, the graft is usually positioned first and then
secured at the conclusion of the anconeus reconstructive procedure. Two
drill holes are placed from posterior to anterior through the
midportion of the capitellum approximately 5 to 7 mm apart (Fig. 23-8), and the anconeus is brought under the intact or reconstructed lateral ulnar collateral ligament (Fig. 23-9).
A nonabsorbable suture is passed through one of the two drill holes,
then into the anconeus from proximal to distal in such a way as to
allow the anconeus to fold on itself when tension is placed on the
suture (Fig. 23-10). The suture then passes
through the second drill hole in the capitellum and is pulled taut,
allowing the anconeus to fold on itself and fill the space created by
the absent radial head (Fig. 23-11). The
remnants of the collateral ligament are repaired or reinforced. The
fascia is approximated to the posterior aspect of the extensor carpi
ulnaris (see Fig. 23-22). The remainder of the closure is routine.
 |
|
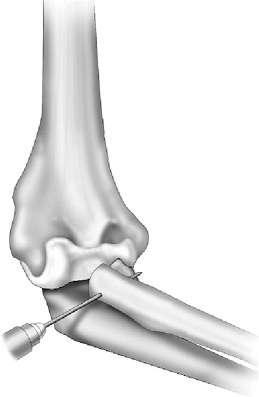
Figure 23-8. Two drill holes 5 to 7 mm apart are placed through the center of the capitellum.
|
 |
|
Figure 23-9. The anconeus is brought under the lateral ulnar collateral ligament.
|
 |
|
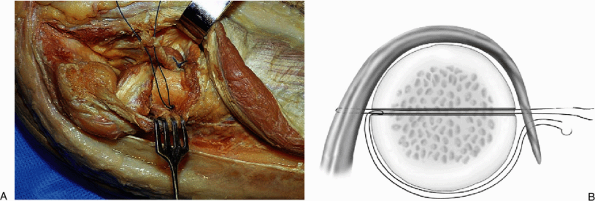
Figure 23-10. A,B:
A looping-type stitch proceeding from proximal to distal, then distal to proximal in a parallel fashion is used to collapse the anconeus on itself. |
 |
|
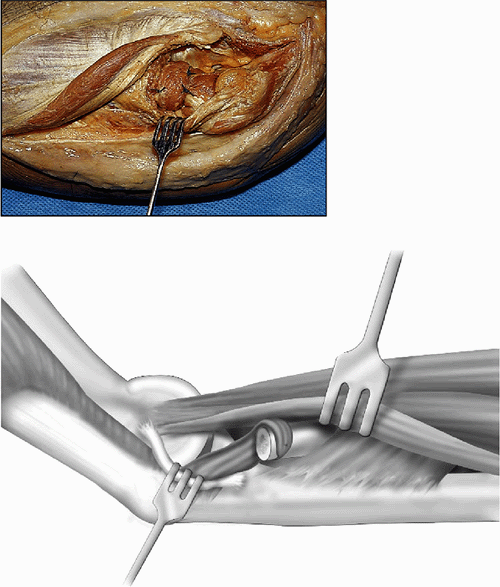
Figure 23-11. A,B: By tightening the suture the anconeus is folded on itself and interposed between the proximal radius and capitellum.
|
P.415
P.416
Type II: Radiohumeral/Radioulnar Interposition
The goal of the procedure is to interpose the anconeus
between the proximal radius and between the capitellum and ulna. The
lateral collateral ligament is managed as described earlier. The
interval between the proximal radius and the ulna is developed. If
capitellar fixation is desired, two drill holes are placed in the
capitellum approximately 5 to 7 mm apart, as earlier. A drill hole is
then placed across both cortices of the resected proximal radius from
lateral to medial with the forearm in neutral rotation (Fig. 23-12).
The anconeus is brought posterior to the lateral ulnar collateral
ligament. If capitellar approximation is sought, a No. 1 nonabsorbable
suture is placed through the capitellum to fix the interposed muscle
between the capitellum and proximal radius. A suture is then placed in
the margin of the anconeus that passes through the proximal radius (Fig. 23-13). The suture then passes through the free portion of the anconeus and is tied (Fig. 23-14). The excessive distal aspect of the anconeus is excised (Fig. 23-15). Finally, the free margin is secured with the original suture (Fig. 23-16). The closure is as described earlier.
between the proximal radius and between the capitellum and ulna. The
lateral collateral ligament is managed as described earlier. The
interval between the proximal radius and the ulna is developed. If
capitellar fixation is desired, two drill holes are placed in the
capitellum approximately 5 to 7 mm apart, as earlier. A drill hole is
then placed across both cortices of the resected proximal radius from
lateral to medial with the forearm in neutral rotation (Fig. 23-12).
The anconeus is brought posterior to the lateral ulnar collateral
ligament. If capitellar approximation is sought, a No. 1 nonabsorbable
suture is placed through the capitellum to fix the interposed muscle
between the capitellum and proximal radius. A suture is then placed in
the margin of the anconeus that passes through the proximal radius (Fig. 23-13). The suture then passes through the free portion of the anconeus and is tied (Fig. 23-14). The excessive distal aspect of the anconeus is excised (Fig. 23-15). Finally, the free margin is secured with the original suture (Fig. 23-16). The closure is as described earlier.
 |
|
Figure 23-12. A through-and-through drill hole is placed in the proximal radius.
|
 |
|
Figure 23-13. A,B:
The anconeus is brought under the lateral collateral ligament and a suture is placed in such a manner as to draw the muscle between the ulna and radius, and is threaded through the holes in the proximal radius. |
 |
|
Figure 23-14. The anconeus is secured to the proximal radius by the nonabsorbable through-and-through suture.
|
 |
|
Figure 23-15.
The free margin of the anconeus is then brought over the radius and secured with the original suture while the excess is removed. |
 |
|
Figure 23-16. The completed interposition rests between the radius and ulna and between the radius and capitellum.
|
P.417
P.418
Type III: Wrap of the Proximal Radius
The radius is exposed and freed from the proximal ulna.
The site of resection of the synostosis or fibrosis is identified. A
through-and-through drill hole is placed in the proximal radius, as
earlier described. The anconeus is brought under the collateral
ligament and a suture is placed in the medial margin (Fig. 23-17).
A free suture is looped through one of the arms of the suture that has
been placed in the anconeus. The muscle is drawn between the proximal
radius and ulna, and the free suture is brought under the radius (Fig. 23-18). The second suture is used to wrap the proximal portion of the anconeus around the proximal radius, (Fig. 23-19) resulting in a circumferential “wrap” of the proximal radius by the anconeus (Fig. 23-20).
The site of resection of the synostosis or fibrosis is identified. A
through-and-through drill hole is placed in the proximal radius, as
earlier described. The anconeus is brought under the collateral
ligament and a suture is placed in the medial margin (Fig. 23-17).
A free suture is looped through one of the arms of the suture that has
been placed in the anconeus. The muscle is drawn between the proximal
radius and ulna, and the free suture is brought under the radius (Fig. 23-18). The second suture is used to wrap the proximal portion of the anconeus around the proximal radius, (Fig. 23-19) resulting in a circumferential “wrap” of the proximal radius by the anconeus (Fig. 23-20).
Closure
In all instances the capsule is closed and the fascia is
approximated to the posterior aspect of the extensor carpi ulnaris and
closed with a running, absorbable suture (Figs. 23-21 and 23-22).
approximated to the posterior aspect of the extensor carpi ulnaris and
closed with a running, absorbable suture (Figs. 23-21 and 23-22).
 |
|
Figure 23-17. A,B:
The anconeus is inserted into the joint and a suture is placed into its margin so as to draw the muscle between the radius and ulna. A second free suture is looped over one of the sutures at the site of emergence from the anconeus. |
 |
|
Figure 23-18. A,B: The through-and-through suture is used to secure the anconeus muscle to the ulnar aspect of the proximal radius.
|
 |
|
Figure 23-19. A,B:
The free suture is passed through the distal free end of the anconeus. The free suture is drawn into the hole on the ulnar aspect of the radius and brought under the proximal radius. |
 |
|
Figure 23-20. The completed “wrap.”
|
 |
|
Figure 23-21. The capsule is cased and the collateral ligament is reinforced if necessary.
|
 |
|
Figure 23-22. Routine closure of the fascia with running absorbable sutures.
|
P.419
P.420
P.421
P.422
Postoperative Management
The postoperative management is predicated on the
features of the underlying pathology. The anconeus interposition itself
prompts immobilization for 5 to 7 days. Passive motion is then
preferred for 2 to 3 weeks. Active and full motion is encouraged a
month after surgery. Typically, a concurrent reconstruction or
reinforcement of the lateral collateral ligament is also carried out
during the surgery. If this has been done because of demonstrated
instability, the forearm is placed in full pronation and protected for
about 6 weeks in a hinged splint. Flexion and extension are encouraged.
Carefully controlled pronation and supination are begun on the sixth to
eighth day.
features of the underlying pathology. The anconeus interposition itself
prompts immobilization for 5 to 7 days. Passive motion is then
preferred for 2 to 3 weeks. Active and full motion is encouraged a
month after surgery. Typically, a concurrent reconstruction or
reinforcement of the lateral collateral ligament is also carried out
during the surgery. If this has been done because of demonstrated
instability, the forearm is placed in full pronation and protected for
about 6 weeks in a hinged splint. Flexion and extension are encouraged.
Carefully controlled pronation and supination are begun on the sixth to
eighth day.
Results
Limited results are available. Our assessment of the
initial 10 procedures demonstrated that four patients received a type I
or type II and that two received a type III interposition. Eight of the
10 patients expressed subjective satisfaction with the procedure,
primarily because of reduced pain. Using the Mayo Elbow Performance
Score (MEPS), seven were rated satisfactory. Bell has reported three
cases in which the distal anconeus was interposed to prevent recurrence
of radioulnar synostosis, all with a satisfactory outcome (1).
In our series, ulnar shortening was performed in three, and two of the
three described minimal, if any, wrist pain. Two patients indicated
that elbow pain persisted with no benefit from the surgery. There were
no incidences of instability. The value of this procedure continues to
be observed and investigated.
initial 10 procedures demonstrated that four patients received a type I
or type II and that two received a type III interposition. Eight of the
10 patients expressed subjective satisfaction with the procedure,
primarily because of reduced pain. Using the Mayo Elbow Performance
Score (MEPS), seven were rated satisfactory. Bell has reported three
cases in which the distal anconeus was interposed to prevent recurrence
of radioulnar synostosis, all with a satisfactory outcome (1).
In our series, ulnar shortening was performed in three, and two of the
three described minimal, if any, wrist pain. Two patients indicated
that elbow pain persisted with no benefit from the surgery. There were
no incidences of instability. The value of this procedure continues to
be observed and investigated.
Complications
There were no specific complications with the procedure.
One patient who underwent a type II procedure experienced persistent
pain, so re-exploration was conducted. At the time of exploration the
anconeus was viable, and the interposition appeared to be functioning
as
One patient who underwent a type II procedure experienced persistent
pain, so re-exploration was conducted. At the time of exploration the
anconeus was viable, and the interposition appeared to be functioning
as
P.423
desired.
As workers’ compensation issues are being debated, the patient
continues to complain of pain after reexploration and ligament
imbrication.
 |
|
Figure 23-23. A 33-year-old male had painful radiohumeral symptoms after fracture dislocation with radial head excision.
|
Illustrative Case
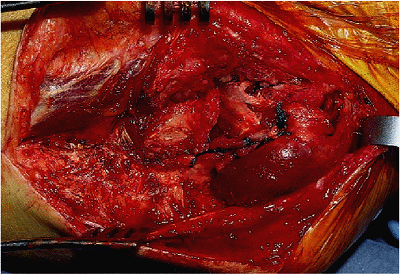
A 33-year-old man had persistent radiocapitellar pain with an associated radioulnar impingement (Fig. 23-23)
after radial head excision and distal radioulnar symptoms from an ulna
plus deformity from the Essex-Lopresti lesion. From radial shortening (Fig. 23-24) the anconeus is brought under the collateral ligament (Fig. 23-25),
which, because it was insufficient, required further stabilization by
reinforcement with a Krachow stitch; an ulnar-shortening procedure was
also completed (Fig. 23-26). The patient had minimal pain at the wrist and elbow, and no symptoms of impingement at the elbow at 1 year (Fig. 23-27).
after radial head excision and distal radioulnar symptoms from an ulna
plus deformity from the Essex-Lopresti lesion. From radial shortening (Fig. 23-24) the anconeus is brought under the collateral ligament (Fig. 23-25),
which, because it was insufficient, required further stabilization by
reinforcement with a Krachow stitch; an ulnar-shortening procedure was
also completed (Fig. 23-26). The patient had minimal pain at the wrist and elbow, and no symptoms of impingement at the elbow at 1 year (Fig. 23-27).
 |
|
Figure 23-24. Proximal radial impaction occurred because of description of the distal radioulnar stabilizers.
|
 |
|
Figure 23-25. The anconeus is elevated and brought under a lax lateral ulnar collateral ligament for a type I repair.
|
 |
|
Figure 23-26. The lax lateral collateral ligament is reinforced with a Krachow stitch.
|
 |
|
Figure 23-27. The patient had minimal pain and a stable elbow at 1 year.
|
P.424
Recommended Readings
1. Bell
SN, Benger D. Management of radioulnar synostosis with mobilization,
anconeus interposition, and a forearm rotation assist splint. J Should Elbow Surg 1999;8:621–624.
SN, Benger D. Management of radioulnar synostosis with mobilization,
anconeus interposition, and a forearm rotation assist splint. J Should Elbow Surg 1999;8:621–624.
2. Morrey
BF, Schneeberger A. Anconeus arthroplasty: an anatomical study and
clinical experience with a new technique for reconstruction of the
radiohumeral/radioulnar joints. Submitted for publication.
BF, Schneeberger A. Anconeus arthroplasty: an anatomical study and
clinical experience with a new technique for reconstruction of the
radiohumeral/radioulnar joints. Submitted for publication.
3. Schmidt CC, Kohut GN, Greenberg JA, et al. The anconeus muscle flap: its anatomy and clinical application. J Hand Surg 1999;24A:359–369.
