Airway Blocks
II – Single-Injection Peripheral Blocks > C – Miscellaneous Blocks
> 19 – Airway Blocks
cavities, as well as the trachea, depends on three pairs of cranial
nerves: the trigeminal (V), vagus (X), and glossopharyngeal (IX).
Consequently, there is no single nerve that can be blocked to produce
complete anesthesia. Most of the nasal cavity innervation involves the
sphenopalatine ganglion and the ethmoid nerve. Application of long
cotton-tipped applicators soaked in 4% lidocaine with epinephrine or
cocaine over the nasal mucosa allows a block of the sphenopalatine
ganglion (applicator angled at 45° to the hard palate) and the anterior
ethmoid nerve (applicator parallel to the dorsal surface of the nose).
of the oropharynx, including the posterior third of the tongue,
anterior surface of the epiglottis, posterior and lateral walls of the
pharynx, and the tonsillar pillars. The glossopharyngeal nerve also
provides motor innervation to the stylopharyngeus muscle, involved in
deglutition. The rest of the pharynx, as well as the upper larynx,
vocal cords, and trachea, are innervated by the vagus nerve and its
branches, especially the superior laryngeal and the recurrent laryngeal
nerves.
0.8 mg intravenous (i.v.) glycopyrrolate administered 30 to 45 minutes
prior to application of the local anesthetic to decrease the amount of
secretions and the use of a vasoconstrictor for the nasal mucosa (1%
phenylephrine) in the absence of contraindications.
-
Adequate preparation, including a
complete explanation to the patient and the surgeon of the reason for
performing the airway nerve blocks, is essential for patient
cooperation and comfort and for success of the procedure. -
The risk-to-benefit ratio has to be
established. The following should be considered: (a) an alternative
plan, including the direct spray of local anesthetic solution using 4%
lidocaine or 14% to 20% benzocaine (risk of methemoglobinemia) or
indirect spray with a nebulizer using 4% lidocaine; (b) the time
available; and (c) the patient’s condition, including level of
consciousness and degree of respiratory depression and insufficiency. -
The use of appropriate sedation using
usually a combination of 2 to 5 mg midazolam and 50 to 150 mg fentanyl
to maintain patient comfort. However, sedation should be
P.178
individually
titrated so that verbal contact with the patient is maintained
(oversedation may lead to hypoventilation, oxygen desaturation, and
respiratory arrest). -
These blocks should be practiced as much
as possible in nonemergency situations to gain experience in performing
airway blocks (often required for awake intubation), so that when their
success is required for a difficult intubation or when an emergency
arises, they can be performed appropriately.
AA, Monteny E, Dewachter B, et al. Intubation under topical
supra-glottic analgesia in unpremedicated and non-fasting patients:
amnesic effects of sub-hypnotic doses of diazepam and Innovar. Can Anaesth Soc 1974;21:467–474.
VS, Whitehead EM, Ainsworth QP, et al. A technique of awake fibreoptic
intubation: experience in patients with cervical spine disease. Anaesthesia 1993;48:910–913.
The glossopharyngeal nerve, which emerges from the skull through the
jugular foramen, travels along the lateral wall of the pharynx.
With the patient’s mouth wide open, a tongue blade held with the
nondominant hand is introduced in the mouth to displace the tongue
medially, creating a gutter between the tongue and the teeth. The
gutter ends posteriorly in a cul-de-sac formed by the base of the
palatoglossal arch. A 25-gauge spinal needle is inserted at the base of
the cul-de-sac and advanced slightly (0.25 to 0.5 cm). After negative
air and blood aspiration tests, 2 mL of 2% lidocaine is injected. The
procedure is repeated on the other side (Fig. 19-1).
 |
|
Figure 19-1. A 25-gauge spinal needle is inserted at the base of the cul-de-sac and advanced slightly.
|
-
The use of a tongue blade may be
facilitated by prior application to the mouth of a topical anesthetic
solution. Also, 2% lidocaine jelly may be used, spread directly on the
tongue blade. -
If air is aspirated, the needle needs to be withdrawn until no air can be aspirated.
-
If blood is aspirated, it is usually
arterial (carotid artery), because the needle is too posterior and too
lateral. The needle needs to be redirected medially.
The superior laryngeal nerve supplies the sensory innervation of the
larynx down to but excluding the vocal cords. At its origin, it travels
with the vagus deeply to the carotid artery, before becoming anterior.
At the level of the cornu of the hyoid, it divides into an internal
sensory branch and an external motor branch to the cricothyroid muscle.
The internal branch pierces the thyrohyoid membrane along with the
laryngeal artery and vein and splits into two branches. The ascending
branch supplies the epiglottis and the vestibules of the larynx,
whereas the descending branch supplies innervation to the mucosa at the
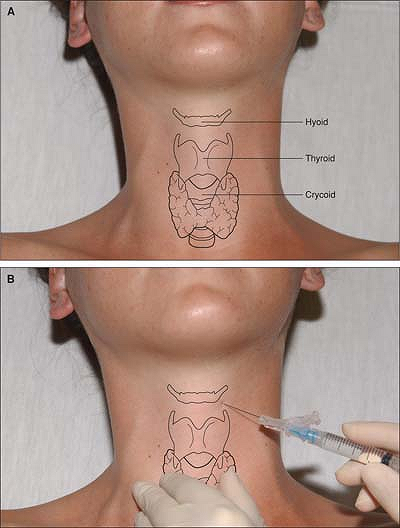
level of the vocal cords (Fig. 19-2A).
The cornu of the hyoid bone is palpated transversally with the thumb
and index finger on the side of the neck immediately beneath the angle
of the mandible and anterior to the carotid artery. To facilitate its
identification, the hyoid bone is displaced toward the side being
blocked. One hand displaces the carotid artery laterally
and
posteriorly. With the other hand, a 23-gauge, 25-mm needle is walked
off the cornu of the hyoid bone in an anterocaudal direction, aiming in
the direction of the thyroid ligament. At a depth of 1 to 2 cm, 2 mL of
2% lidocaine with epinephrine is injected after negative air and blood
aspiration (Fig. 19-2B). The block is repeated on the opposite side.
 |
|
Figure 19-2. A: Anatomic landmarks. B: Lidocaine with epinephrine is injected after negative air and blood aspiration.
|
-
Exercise caution not to insert the needle
into the thyroid cartilage, since injection of local anesthetic at the
level of the vocal cords may cause edema and airway obstruction. -
If air is aspirated, the laryngeal mucosa has been pierced and the needle needs to be retrieved.
-
If blood is aspirated (superior laryngeal
artery or vein), the needle needs to be redirected more anteriorly.
Pressure should be applied to avoid hematoma formation. -
If laryngeal evaluation is performed for
vocal cord movement, only the internal laryngeal nerve needs to be
blocked. For this purpose, the patient is asked to open the mouth
widely. The tongue is depressed with a tongue blade and pulled
medially. A Krause forceps with cotton soaked with 4% lidocaine is
placed over the lateral posterior curvature of the tongue (along with
the downward continuation of the tonsillar fossa) until resistance is
met. The forceps should remain in this position for 5 minutes, and the
same procedure is then repeated on the opposite side. -
In case of a bronchoscopy or an awake intubation, the superior laryngeal and the recurrent laryngeal nerves need to be blocked.
LA, Boyd GL. Superior laryngeal nerve block as a supplement to total
intravenous anesthesia for rigid laser bronchoscopy in a patient with
myasthenic syndrome. Anesth Analg 1992;75:458–460.
VS, Whitehead EM, Ainsworth QP, et al. A technique of awake fibreoptic
intubation: experience in patients with cervical spine disease. Anaesthesia 1993;48:910–9 13.
The right recurrent laryngeal nerve originates at the level of the
right subclavian artery and loops around the innominate artery on the
right and the aortic arch on the left. This nerve supplies the sensory
innervation of the vocal cords and the trachea, as well as motor
innervation to the vocal cords.
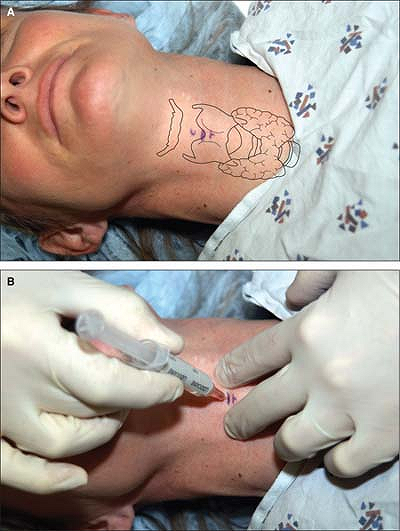
The cricothyroid membrane is located, and a small amount of local
anesthesia is administered subcutaneously using a tuberculin syringe
filled with 1% lidocaine (Fig. 19-3A).
The nondominant hand is used to identify the cricothyroid membrane and
to hold the trachea in place by placing the thumb and third finger on
either side of the thyroid cartilage. A 10-mL syringe containing 2%
lidocaine, mounted on a 22-gauge, 35-mm plastic catheter over a needle,
is introduced into the trachea through the cricothyroid membrane at an
angle of 45° in a caudal direction. Immediately after the introduction
of the catheter into the trachea, a loss of resistance and the ability
to aspirate air should occur. The catheter is advanced into the lumen
of the airway and the needle is
removed. The syringe is reattached and it should be confirmed that air can be aspirated (Fig. 19-3B).
The patient is then asked to take a deep breath. At the end of the
inspiratory effort, 3 to 4 mL of local anesthetic solution is injected
into the trachea.
 |
|
Figure 19-3.
The cricothyroid membrane is located and a small amount of local anesthesia is administered subcutaneously using a tuberculin syringe. |
-
The patient needs to be informed that the injection of local anesthetic solution will likely make him or her cough.
-
This block is contraindicated in patients diagnosed with an unstable neck, because it induces coughing.
-
During performance of the block, the patient should not talk, swallow, or cough, if possible.
-
The catheter should be left in place
until the intubation is completed for the purpose of injecting more
local anesthetic, if necessary, and to decrease the likelihood of
subcutaneous emphysema.
