Extensor Tendon
that of the flexors, is thinner, less substantial, and less likely to
hold sutures well. At the wrist and forearm, however, the extensors’
substance and cross-sectional area are much more like the flexor
tendons. Injuries to the extensor tendons are common, owing to their
relatively exposed and superficial location. The dorsal aspect of the
hand and wrist is covered with a thin layer of supple skin, with
minimal subcutaneous tissue. In many areas, such as the distal finger
joint, the tendon is very thin and subject to rupture with sufficient
force. Injury may be secondary to laceration, deep abrasion, crush, or
avulsion, and the majority of extensor tendon injuries are at joint
levels. Penetrating wounds that disrupt the tendon are also prone to
enter the joint; this is true not only at the interphalangeal joints,
but also at the MCP joint. The degree of joint contamination must be
evaluated and considered in the treatment plan.
extensor mechanism in the hand and fingers is usually not associated
with immediate retraction of the tendon ends because of the multiple
soft-tissue attachments and interconnections at various levels.
Furthermore, the extensor mechanism in the hand is extrasynovial,
except at the wrist, where the tendons are covered with a synovial
sheath. Paratenon surrounds the extensor tendons over the dorsum of the
hand, and tendons covered with paratenon do not separate widely when
lacerated. Therefore, divided extensor tendons are usually free to
retract only on the dorsum of the wrist. Because of this, many tendon
injuries, especially in the fingers, may be treated successfully by
splinting alone. In the hand and fingers, any gap in the tendon
following laceration or avulsion is usually caused by unopposed flexion
of the joints rather than retraction of the tendon.
considered to be more intricate than finger flexion. This mechanism is
composed of two separate and neurologically independent systems: the
extrinsic extensors innervated by the radial nerve, and the intrinsic
systems supplied by the ulnar and median nerves.
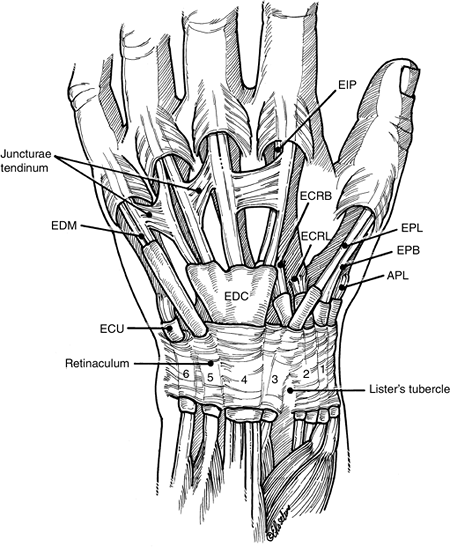
bellies in the forearm. The extensor pollicis longus (EPL), extensor
pollicis brevis (EPB), extensor indicis proprius (EIP), and extensor
digiti minimi (EDM) have a comparatively independent origin and action.
The proprius tendons at the MCP joint level are usually to the ulnar
side of the communis tendons. The little finger proprius tendon (EDM)
over the metacarpal and wrist level is usually represented by two
distinct tendinous structures (Figure 12.2-1).
The extensor digitorum communis (EDC) tendon to the little finger is
present less than 50% of the time. When it is absent, it is almost
always replaced by a junctura tendinum from the ring finger to the
extensor aponeurosis of the little finger.
by the proprius tendons to these digits. Loss of independent extension,
especially of the index finger, was said to be likely, but in the
majority of patients, independent extension of the index is still
possible if the EIP is absent due to injury or transfer. Extension lag
in the index finger may be avoided when taking the EIP as a transfer by
sectioning the EIP proximal to the hood.
the hand beneath the extensor retinaculum through a series of six
tunnels—five fibro-osseous and one fibrous (the fifth dorsal
compartment, which contains the EDM). The extensor retinaculum is a
wide fibrous band that prevents bowstringing of the tendons across the
wrist joint. Its average width is 4.9 cm (with a range of 2.9 to 8.4
cm), as measured over the fourth compartment (see Figure 12.2-1).
At this level, the extensor tendons are covered with a synovial sheath.
The extensor retinaculum consists of two layers: the supratendinous and
the infratendinous. The infratendinous layer is limited to an area deep
to the three ulnar compartments. The six dorsal compartments are
separated by septa that arise from the supratendinous retinaculum and
insert onto the radius.
tendons are joined together by oblique interconnections called
juncturae tendinum. These connecting bands usually run in a distal
direction from the ring finger communis to the little and middle
fingers, and from the middle to the index finger. The EDM tendon
receives a junctura from the ring finger extensor if the little finger
EDC is absent. It is because of these interconnections that laceration
of the middle finger communis tendon just proximal to this junctura may
result in only partial extension loss of the middle finger. The
juncturae tendinum have considerable interaction between adjacent
fingers, and may also decrease the stress on the web. Sectioning the
web virtually abolishes any movement between adjacent fingers, in
contrast to transection of the long extensors, which has no effect on
the interaction between the fingers. This finding is of significance
when evaluating an injured hand, because a lacerated tendon may be
overlooked if finger extension is partially maintained through
juncturae, intertendinous fascia, or the web structures between the
adjacent fingers.
held in place over the dorsum of the joint by the conjoined tendons of
the intrinsic muscles and the transverse lamina or sagittal band, which
together tether and keep the extensor tendons centralized over the
joint (Figure 12.2-2). The sagittal band arises
from the palmar plate and the intermetacarpal ligaments at the neck of
the metacarpals. Any injury to this extensor hood or expansion may
result in subluxation or dislocation of the extensor tendon. The
extensor
mechanism
at the level of the proximal aspect of the finger is composed of a
layered, crisscrossed fiber pattern that changes its geometric
arrangement as the finger flexes and extends. This arrangement allows
the lateral bands to be displaced volarly in flexion and to return to
the dorsum of the finger in extension.
 |
|
Figure 12.2-1 The extensor mechanism at the wrist, fingers, and thumb. Note the six compartments or canals.
|
the extensor mechanism at about the level of the proximal and
midportion of the proximal phalanx, and continue distally to the DIP
joint of the finger.
described as a trifurcation of the extensor tendon into the central
slip, which attaches to the dorsal base of the middle phalanx, and the
two lateral bands. The lateral bands pass on either side of the PIP
joint and continue distally to insert at the dorsal base of the distal
phalanx. The extensor mechanism is maintained in place over the PIP
joint by the transverse retinacular ligaments. The extensor tendon
achieves simultaneous extension of the two finger joints by a mechanism
in which the central slip extends the middle phalanx, and the lateral
bands bypass the PIP joint to extend the distal phalanx. The fibers
overlying the PIP joint are differentially loaded as the finger moves.
In the flexed position, the most central fibers are tensed, whereas in
extension, the lateral fibers are tensed. The most important feature of
this mechanism is that the three elements are in balance. Specifically,
the lengths of the central slip and two lateral bands must be such that
extension of the PIP and DIP joints takes place together, so that when
the middle phalanx is brought up into alignment with the proximal
phalanx, the distal phalanx reaches alignment at the same time. This
mechanism depends on the relative length of the central slip and two
lateral bands. This precise and consistent length relationship is what
is so difficult to restore when the mechanism has been damaged. Loss of
this critical relationship at the PIP joint level, with relative
lengthening of the central slip, results in the characteristic
boutonniere deformity. A unique arrangement is present at the dorsal
aspect of the PIP joint, where the central slip of the extensor tendon
invests a fibrocartilage plate prior to its attachment to the dorsal
base of the middle phalanx. The average thickness of the central slip
at this level is 0.5 mm, but because of the presence of this
fibrocartilage plate, the thickness is doubled over the PIP joint. This
structure is called the
dorsal
plate, and adds to the stability of the extensor tendon and PIP joint.
It also increases the moment arm of the extensor tendon at the PIP
joint, and prevents attrition of the central slip at the PIP joint. The
similarity of the dorsal plate and the patella is striking. In my
experience, this dorsal plate adds relative thickness and substance to
the extensor mechanism, and aids in the placement of sutures for
lacerations in this area
 |
|
Figure 12.2-2 The extensor mechanism at the MCP, PIP, and DIP joints of the finger.
|
and are based on the anatomic characteristics of the extensor mechanism
in each zone. This provides a useful basis for establishing a treatment
plan and comparing end results following various forms of treatment.
|
Table 12.2-1 The Zones of Extensor Tendon Injury in The Fingers, Thumb, and Forearm
|
|||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||
|
Table 12.2-2 Mallet Finger Classification
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
-
The most common type of mallet finger is
type I, which is caused by loss of continuity—either from tearing the
substance of the tendon just proximal to the joint, or from avulsion of
the tendon from its insertion, with or without a small piece of bone.-
The degree of deformity in this injury
may vary from a few degrees of extension loss to a 75 to 80 degree
flexion posture of the DIP joint (Figure 12.2-3).
-
-
A laceration (type II) over or near the DIP joint that transects the tendon also produces a characteristic mallet deformity.
-
Lacerations directly over the joint more
often than not enter the joint; this must be considered in treatment
because of the potential for joint contamination.
 Figure 12.2-3 Clinical appearance of a mallet finger deformity, type I, obtained when a ball struck the tip of the finger.
Figure 12.2-3 Clinical appearance of a mallet finger deformity, type I, obtained when a ball struck the tip of the finger. -
-
Deep abrasion injuries (type III) over
the distal joint may result in significant loss of soft-tissue cover,
and a loss of a portion or all of the underlying tendon mechanism. The
joint is almost always exposed.
-
Closed type I injuries are treated by continuous splinting of the DIP joint in full extension.
-
Only the DIP joint needs to be splinted, but the splinting must be continuous. Removal of the splint during the treatment interval and flexing the DIP joint may reverse the healing process.
-
When the DIP joint is capable of active
extension (usually after 6 to 8 weeks), the splint may be removed, and
cautious flexion activity may be started. -
If any recurrence of the deformity occurs, the splint is reapplied for another 2 to 3 weeks.
-
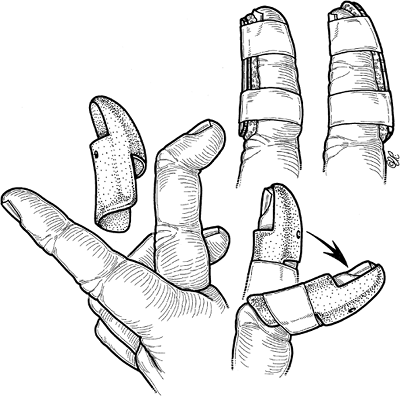
Various forms of splinting have been
used, and my favorite splints include the commercially available Stack
splint, which comes in multiple sizes, and dorsal or palmar splints
made from padded aluminum (Figure 12.2-4). -
Reconstitution of the tendon occurs by
fibroblastic proliferation, which produces a tendon callus that
subsequently contracts and re-forms into a type of tendon that restores
continuity. -
The success of this method depends on
continuous coaptation of the tendon ends, and avoidance of stretching
or tearing of the tendon callus. -
The precarious nature of this healing
process is further amplified by noting that the microvascular anatomy
of the distal digital extensor tendon often demonstrates an area of
minimal or deficient blood supply in this zone.
-
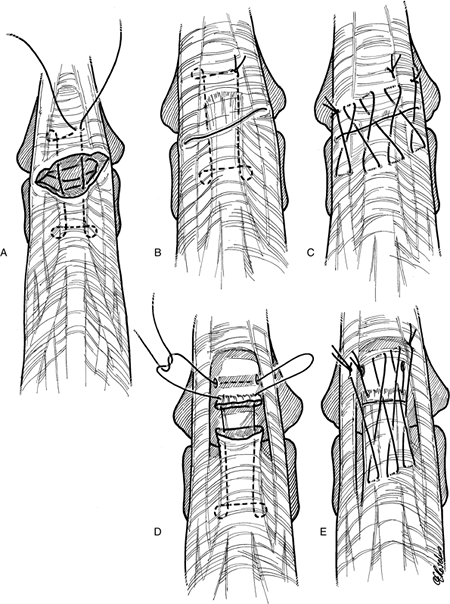
Lacerations over the DIP joint may produce a mallet deformity, and an appropriate suture technique that may be used is given in Figure 12.2-5.
-
Splinting is continuous for 6 weeks following surgical repair.
-
The management of this injury is far
different from that of a simple closed mallet deformity, and staged
surgical reconstruction is required.
-
Injuries in this zone are usually due to lacerations.
-
Lacerations over the dorsal aspect of the middle phalanx may result in partial rather than complete laceration of
P.194P.195the extensor mechanism, due to its increased breadth and curved shape.
![]() Figure 12.2-4 Useful splints for the treatment of type I closed mallet finger deformity. Note that the PIP joint is left free for motion.
Figure 12.2-4 Useful splints for the treatment of type I closed mallet finger deformity. Note that the PIP joint is left free for motion.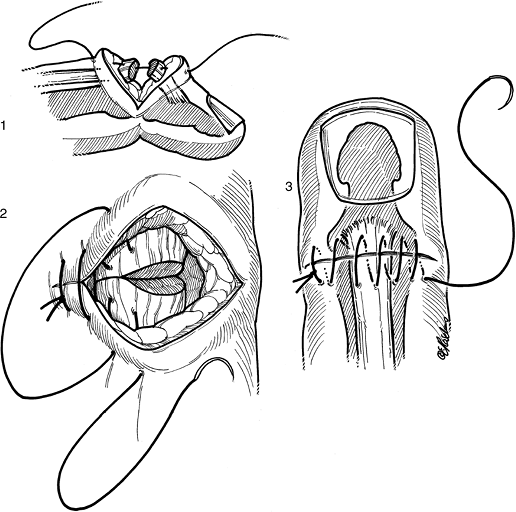 Figure 12.2-5 Suture technique for repairing an extensor tendon laceration over the DIP joint.
Figure 12.2-5 Suture technique for repairing an extensor tendon laceration over the DIP joint. -
Incomplete lacerations may not be associated with a mallet deformity.
-
All wounds in this area should be
carefully inspected, and the underlying extensor mechanism evaluated
and repaired as indicated. -
Partial lacerations involving less than
50% of the substance of the extensor may be treated by wound care and
skin suture followed by protected range of motion. -
More extensive or complete lacerations
are repaired by a running suture near the cut edge, followed by a cross
stitch proximal and distal to the running suture (Figure 12.2-6). -
Splinting of the DIP joint is performed for 4 to 6 weeks, based on the nature of the laceration and the integrity of the repair.
 |
|
Figure 12.2-6 Extensor tendon suture technique for lacerations over the middle phalanx (zone II).
|
usually due to closed blunt trauma with acute forceful flexion of the
PIP joint, producing avulsion of the central slip from its insertion on
the dorsal base of the middle phalanx, with or without fracture and
laceration of the extensor tendon at or near its insertion. Volar
dislocation of the PIP joint may also result in avulsion of the central
slip and subsequent boutonniere deformity. Loss of integrity of the
central slip attachment at the dorsal base of the middle phalanx,
either from avulsion or laceration, starts a cascade of tendon
imbalance that results in a characteristic deformity of flexion at the
PIP joint and hyperextension of the DIP joint. This deformity, called
the boutonniere deformity, illustrates the
problem of imbalance in the finger, which is a chain of joints with
multiple tendon attachments. This chain collapses into an abnormal
posture or deformity when there is an imbalance of the critical forces
maintaining equilibrium. This abnormal cascade or sequence begins with
flexion of the PIP joint, owing to loss of the central slip and the
unopposed force of the flexor digitorum superficialis. Next, with
stretching of the expansion (transverse retinacular ligament and
triangular ligament) between the central and lateral slips, the lateral
bands migrate volarward to a position volar to the axis of joint
rotation. Finally, in this position of the lateral bands, the pull of
the intrinsic muscles is directed exclusively to the distal joint,
which progressively hyperextends. The MCP joint is also hyperextended
by action of the long extensor tendon.
-
Figure 12.2-7 demonstrates the appearance of the boutonniere deformity.
 Figure 12.2-7
Figure 12.2-7
The clinical appearance of the boutonniere deformity. Note the flexed
posture of the PIP joint and the hyperextension of the DIP joint of the
middle finger.P.196![]() Figure 12.2-8 The Elson test for diagnosis of boutonniere deformity.
Figure 12.2-8 The Elson test for diagnosis of boutonniere deformity. -
In closed injuries, the characteristic
boutonniere deformity may not be present at the time of injury, and
usually develops over a 10- to 21-day period following injury.-
This condition is often missed, even in an open wound.
-
-
A painful, tender, and swollen PIP joint
that has been recently injured should arouse suspicion. Active motion
is decreased, and the finger is held semiflexed. -
Diagnostic maneuvers include holding the
PIP joint in full extension and testing the amount of passive flexion
of the distal joint. -
With disruption of the central slip and volar migration of the lateral bands, flexion of the distal joint is markedly decreased.
-
Another useful test is the Elson test depicted in Figure 12.2-8.
-
The finger to be examined by the Elson
test is flexed comfortably to a right angle at the PIP joint over the
edge of a table, and firmly held in place by the examiner. The patient
is then asked to extend the PIP joint against resistance. -
Any pressure felt by the examiner over the middle phalanx can only be exerted by an intact central slip.
-
Further proof is that the DIP joint
remains flail during the effort because the competent central slip
prevents the lateral bands from acting distally. In the presence of a
complete rupture of the central slip, any extension effort perceived by
the examiner is accompanied by rigidity at the DIP joint with a
tendency toward extension. This is produced by the extensor action of
the lateral bands. -
This test, however, does not demonstrate
the presence of a partial rupture of the central slip, and it may be
impeded by pain or lack of patient cooperation.
-
-
Consideration may be given to nerve block for pain relief, as indicated.
-
Correction of this deformity is dependent
on restoration of the normal tendon balance, and on the precise length
relationship of the central slip and lateral bands. -
In acute cases, before fixed contractures have occurred, this may be achieved by two basic means:
-
Progressively splinting the PIP joint into full extension.
-
Insertion of an oblique transarticular K-wire to maintain the PIP joint in full extension.
-
-
At the same time, active and passive flexion exercises of the distal joint are performed.
-
Splinting of the PIP joint, and active
flexion of the DIP joint, are believed to draw the lateral bands
distally and dorsally, and to reduce the separation of the torn ends of
the central slip of the extensor tendon.P.197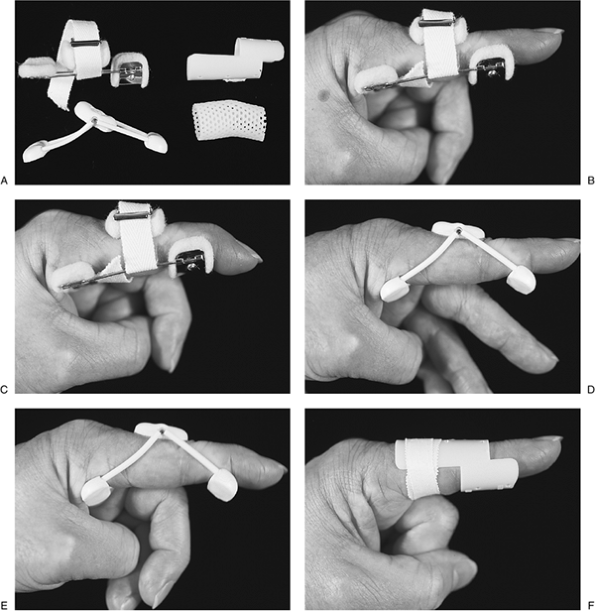 Figure 12.2-9 Various forms of static and dynamic splints used to treat a closed-boutonniere deformity.
Figure 12.2-9 Various forms of static and dynamic splints used to treat a closed-boutonniere deformity.-
This allows repair by contracture of the
disrupted tendon ends at their anatomic length, and by migration of the
lateral bands to their normal anatomic position above the joint axis of
rotation at the PIP joint.
-
-
Positioning and maintaining the PIP joint
in extension has been achieved by dynamic and static splinting, K-wire
fixation of the joint, and serial plaster casts. -
When the distal joint can be fully flexed
with the PIP joint extended, all components of the extensor mechanism
have been restored to their normal relationships and balance. At this
point, the splint may be discontinued.-
This may take 6 weeks or more of continuous splinting and DIP joint exercise.
-
-
Various forms of splints used for treatment of closed boutonniere deformity are depicted in Figure 12.2-9.
-
In closed boutonniere deformity, operative treatment is undertaken in two circumstances:
-
The central slip has been avulsed with a
bone fragment, and is lying free over the PIP joint. In this case, it
should be replaced or excised, and the tendon should be reattached with
a pullout suture. -
There is a long-standing boutonniére deformity in a young person.
-
-
In closed volar dislocations of the PIP
joint, there is usually a rupture of the central slip, along with a
rupture of a collateral ligament and volar plate and a subsequent
boutonniere deformity. -
These potentially disabling soft-tissue
injuries must be recognized and repaired by prompt reduction and
primary repair of all ruptured structures (central slip, collateral
ligament, and volar plate), combined with stabilization of the PIP
joint in extension with a K-wire for 3 weeks, followed by gradual
mobilization over the next 3 to 4 weeks while the PIP joint is
protected. -
Motion of the distal joint is encouraged in the early postoperative period.
-
It can be anticipated that this method
will produce satisfactory results, although joint stiffness can be a
problem because of extensive soft-tissue injury. -
Reconstructions of a chronic, closed
boutonniere deformity or of boutonniere lesions caused by burns or
rheumatoid disease are beyond the scope of this text.
-
Laceration of the extensor mechanism at
the PIP joint will result in loss of extension at that joint, which may
in turn develop into a secondary boutonniere deformity if not properly
treated. -
The average thickness of the central slip
just proximal to the PIP joint is 0.5 mm, but this measurement is
doubled by the fibrocartilaginous dorsal plate at the point of
insertion of the central slip into the dorsal base of the middle
phalanx. -
This dorsal plate provides a more substantial substance for suture retention.
-
The lateral bands at this level also are
approximately twice the thickness of the central slip portion of the
extensor tendon, and are likely to retain sutures better than the
proximal portion of the central slip. -
A useful repair technique is a modified Kessler suture of 4-0 synthetic suture beginning 1 cm from the lacerated tendon edge.
-
The knot is tied in the substance of the tendon so that two intact strands cross the laceration.
-
This suture begins in the substance of
the lateral bands on each side, and ends in the confluence of the
lateral bands and the dorsal plate over the PIP joint. -
Next, a 5-0 synthetic suture is used to
perform a cross stitch, as described by Silfverskiold. This is not a
circumferential suture, as is used for flexor tendons, because the
tendon is flat and thin, but it is placed from margin to margin of the
extensor. -
Both the Kessler and the cross-stitch
sutures are placed so that little or no shortening or side-to-side
deformity of the extensor mechanism is produced.
-
-
Figure 12.2-10 demonstrates some useful suture techniques for repair of lacerations in the region of the PIP joint.
-
Passive motion of the PIP joint in the
operating room to 30 degrees, without gapping of the repair site,
usually indicates that the repair is satisfactory. -
Some lacerations of the extensor
mechanism over the PIP joint are so near the insertion of the central
slip that inadequate length is present distally to place or retain the
suture material.-
In these cases, the distal aspect of the
suture must be placed through a small transverse tunnel made in the
dorsal base of the proximal phalanx with a 0.35 K-wire. -
A 5-0 cross stitch is placed as space permits to augment the repair (see Figure 12.2-10D, E).
-
Care is taken to ensure that the various
components are neither foreshortened nor lengthened, as this may result
in contracture or extensor lag, respectively. -
The PIP joint is splinted in full extension.
-
-
Under ideal circumstances, and when a hand therapist is available, the short arc motion protocol is begun (see Rehabilitation Protocol for Zone III–IV Injuries).
-
An alternative treatment option is as follows:
-
A safety-pin splint or a molded, palmar,
thermoplast splint, as described for treatment of the closed
boutonniere deformity, is applied, and active flexion exercises of the
distal joint are started. -
The splint is maintained on a continuous
basis for 5 to 6 weeks with the PIP joint in full extension, and active
flexion exercises of the distal joint are performed. -
When active exercises to the PIP joint
are started at 5 to 6 weeks, the patient is advised to support the
proximal phalanx in flexion as the PIP joint is extended. This directs
the force of the extensor tendon more distally, and the finger is in a
more effective position for extension. -
The PIP joint is splinted in extension between these exercise sessions for another 2 to 4 weeks.
-
At 8 to 10 weeks, active flexion and extension exercises are increased.
-
Dynamic flexion splinting of the PIP
joint can be used to augment recovery of flexion if there is no
extensor lag at the PIP joint. -
The recovery of flexion in the DIP joint
can be augmented by gentle and intermittent rubber band traction
between a dress hook attached to the fingernail distally and a small
proximal hook attached to a plaster finger cylinder cast.
-
-
Injuries at this level are usually
partial lacerations of the extensor mechanism, because of the broad
configuration of the tendon over the curved shape of the underlying
phalanx and consequent protection of the lateral bands.-
Functional loss may be minimal due to this fact.
-
-
These lesions are diagnosed by direct inspection of the wound.
-
Laceration of an isolated lateral band may be repaired with a 5-0 cross stitch, and early protected motion may be started.P.199
![]() Figure 12.2-10 Suture techniques for repair of lacerations of the central slip at the PIP joint. A–C. A Kessler stitch with a crisscross overlay is used if there is sufficient tendon at each end for repair. D, E.
Figure 12.2-10 Suture techniques for repair of lacerations of the central slip at the PIP joint. A–C. A Kessler stitch with a crisscross overlay is used if there is sufficient tendon at each end for repair. D, E.
If sufficient tendon is not available distally, the tails of the
Kessler suture are tied through a transverse tunnel made with a 0.035
K-wire through the dorsal base of the middle phalanx. The crisscross
stitch is used to complete the repair. The Kessler suture is tied with
suitable tension to avoid gapping or undue shortening of the tendon.
The distance between the longitudinal components of the suture is
adjusted to avoid side-to-side “bunching” or shortening. -
Complete lacerations of the central
tendon should be repaired using a modified Kessler suture of 4-0
nonabsorbable material, with a crisscross suture of 5-0 (see Figure 12.2-10A, C). -
Care is taken to avoid relative
lengthening or shortening of the central tendon, because this may
result in imbalance between the central slip and the lateral bands. -
Because of the relatively large interface
between the extensor mechanism and osseous phalanx, and the resultant
potential for adhesions, it is ideal to begin short arc motion
exercises as described for zone III injuries.
-
Tendon injuries at this level are most often associated with open wounds.
-
A small, penetrating wound over the MCP joint may be caused by striking someone in the mouth with a clenched fist.P.200
-
Although many patients deny this mechanism of injury, a careful history must be taken.
-
-
This is a contaminated wound, and the organisms involved are capable of producing significant wound infection.
-
Gram-positive bacteria (usually
staphylococci) alone, or in combination with gram-negative organisms,
are most frequently cultured.
-
-
The incidence of complications is directly related to the time span from injury to treatment.
-
A radiograph is obtained to note the presence or absence of a fracture or foreign body.
-
The wound must be extended proximally and distally to permit inspection of the joint, and a culture is taken.
-
The wound is debrided, irrigated, and left open.
-
Appropriate antibiotics are started immediately (preferably preoperatively).
-
Under no circumstances should a human bite wound be closed.
-
Most tendon injuries associated with this type of wound are partial, and need not be repaired immediately.
-
The hand is splinted, with the wrist in 40 to 45 degrees extension and the MCP joints in 15 to 20 degrees of flexion.
-
The soft tissues, including the capsule and extensor hood, are allowed to seek their own position over the joint.
-
Partial or even complete lacerations are seldom—if ever—associated with significant retraction at this level.
-
-
The tendon laceration may be repaired
secondarily as needed in 5 to 7 days, or even later depending on the
nature of the wound at the time of inspection. -
When the infection is under control, dynamic splinting is started.
-
Lacerations of the extensor tendon or
hood at the MCP joint level are repaired using core-type sutures of 4-0
nonabsorbable material. -
Injuries of the extensor tendon at this
level are not associated with retraction of the ends, and a modified
Kessler with a cross-stitch is used (see Figure 12.2-10A, C). -
Postoperative management includes dynamic
splinting using the methods described in the section on Rehabilitation
of Extensor Tendon Injuries.
-
Spontaneous rupture of the radial
sagittal band with subsequent ulnarward subluxation or dislocation of
the extensor tendon in the nonrheumatoid patient may occur following
forceful flexion or extension of the finger. -
The lesion is secondary to a tear of the
sagittal band and oblique fibers of the hood, usually on the radial
side, although rupture of the ulnar sagittal band and radial
dislocation have been reported. -
Ulnar subluxation or dislocation of the
extensor tendon, sometimes accompanied by painful snapping of the
extensor tendon when making a fist, is the usual finding. -
In some cases, this may be associated with incomplete finger extension and ulnar deviation of the involved digit (Figure 12.2-11).
-
The middle finger is the most commonly involved.
-
This may be the result of an inherent
anatomic weakness, because the extensor tendon of the long finger is
situated on top of the transverse fibers, and has a comparatively loose
attachment at this level.
-
-
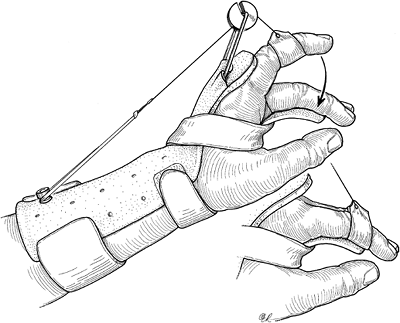
Patients seen within 2 weeks of the
injury may be treated by closed means using a plaster or orthotic
device that maintains the MCP joint in a flexion block splint (Figure 12.2-12).
The splint maintains the finger in neutral abduction-adduction,
allowing full extension but blocking flexion at 10 to 20 degrees. -
The splint is used for 6 weeks.
-
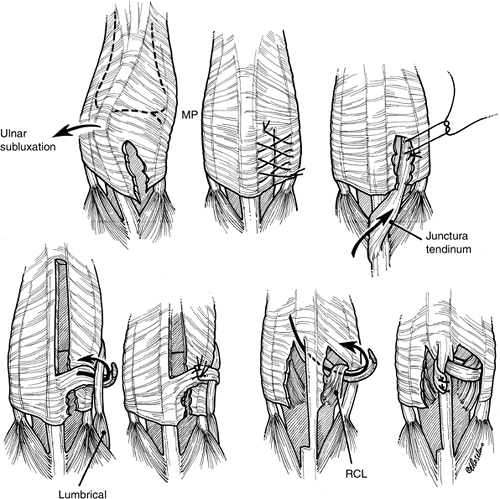
Dislocations that are diagnosed long
after the injury, or that fail initial splinting, are best treated with
surgical release and realignment of the extensor mechanism by one of
the methods depicted in Figure 12.2-13.
-
Lacerations of the hood or sagittal bands
at this level must be repaired so that the extensor tendon will remain
centralized over the dorsum of the joint. -
Failure to repair this type of injury may result in subluxation of the extensor tendon and an associated loss of extension.
-
A cross stitch of 4-0 or 5-0 nylon is used to repair these lacerations.
-
Gentle flexion and extension exercises are started in 3 to 5 days.
-
Abduction and adduction motions are
avoided, and these forces are minimized by “buddy strapping” the
injured finger to an adjacent finger.
-
Zone VI injuries have a better prognosis than more distal lesions (zones II to V) for several reasons:
-
They are unlikely to have associated joint injuries.
-
The decreased tendon surface area in zone VI lessens the potential for adhesion formation.P.201
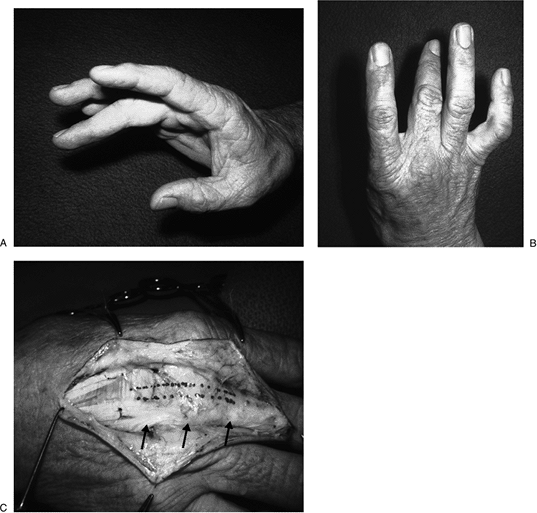 Figure 12.2-11 Traumatic ulnar dislocation of the extensor tendon at the MCP joint. A. Note the lack of complete extension of the middle finger. B. There is ulnar deviation of the middle finger when the patient attempts to extend the finger. C. Operative appearance of the dislocated extensor tendon (arrows) and the anatomic or normal position of the extensor (dotted lines).
Figure 12.2-11 Traumatic ulnar dislocation of the extensor tendon at the MCP joint. A. Note the lack of complete extension of the middle finger. B. There is ulnar deviation of the middle finger when the patient attempts to extend the finger. C. Operative appearance of the dislocated extensor tendon (arrows) and the anatomic or normal position of the extensor (dotted lines). -
The increased subcutaneous tissue lessens the potential for adhesions.
-
There is greater tendon excursion in zone VI.
-
Complex tendon imbalances are less likely to occur.
-
-
The extensor tendons in this zone have
sufficient substance to accept core-type sutures of the surgeon’s
choice, and dynamic splinting can be performed with the assurance that
disruption of the suture site is unlikely. -
Postoperative management includes dynamic
splinting beginning at 3 to 5 days with the wrist in 40 to 45 degrees
of extension and the MCP joints in 0 to 15 degrees flexion. This lasts
for 5 weeks. See the section on extensor tendon rehabilitation.
persistent hard edema on the dorsum of the hand, all associated with
work-related injuries. All patients were covered by worker’s
compensation insurance, had sustained trauma insufficient to produce
fracture, and had prolonged symptoms and findings. This condition has
been called dorsal hard edema of the hand, peritendinous fibrosis of
the dorsum of the hand, and factitious lymphedema of the hand.
Typically, a worker, usually male, describes a blow to the dorsum of
the hand without fracture or laceration and then develops firm,
persistent swelling over the back of the hand with subsequent loss of
finger flexion and resulting prolonged time out of work.
 |
|
Figure 12.2-12
Orthotic device for treatment of extensor tendon dislocation at the MCP joint. (Courtesy of Inoue and Tamara, from Inoue G, Tamura Y. Dislocation of the extensor tendon over the metacarpophalangeal joints. J Hand Surg 1996;21A:464–469.) |
with this disorder, including proven or suspected self-inflicted
trauma, such as repeated blows to the back of the hand or application
of tourniquets, compensable work-related injuries, and neurosis,
psychosis, or suicidal tendency. Although abnormal tissues have been
removed in Secretan’s disorder, these tissues are merely the natural
response to trauma, and the pathology reports on the tissue specimens
and MRI findings are not unexpected. Such findings do not indicate an
etiology other than self-inflicted trauma.
and treatment. In my opinion, Secretan’s is a disorder with a known
etiology and pathogenesis, and it is not a disease, which implies some
unique pathologic process that occurs for some as yet undiscovered
reason.
-
Diagnosis is based on the history and on physical findings.
-
Both T1- and T2-weighted MRI have shown
soft-tissue and tendon edema in combination with diffuse peritendinous
fibrosis extending to the fascia of the interosseous muscles. -
Operative findings (not advised) have
shown fibroadipose tissue with areas of focal myxoid or cystic
degeneration similar to ganglion tissue.
-
Most experts advise nonoperative
management of this condition, which has included studious neglect and
avoidance of passive manipulation, heat, and massage. They do, however,
encourage the patient to exercise by voluntary means. -
The condition may improve by plaster-cast protection.
-
This condition must be recognized as a factitious disorder.
-
Patients with factitious disorders are not feigning the disorder; they are causing it.
-
Confrontation in the form of accusation can potentially be harmful to both the patient and the doctor, and should be avoided.
-
The physical problem or lesion may resolve when compensation is terminated. This condition is not a surgical lesion.
-
Best results have been achieved by psychotherapy.
-
Protective casting, although it may
result in immediate improvement and can confirm the diagnosis, may not
be effective as a definitive treatment, as this disorder is
self-inflicted and is characterized by recidivism. However, this
technique may somehow demonstrate, in a conscious or unconscious way,
the self-inflicted nature of the problem. -
Active physical therapy may be useful in many cases when combined with psychotherapy.
-
are associated with damage to the retinaculum. The retinaculum prevents
bowstringing of the extensor tendons, and lacerations of the extensors
at this level are thought to be associated with subsequent adhesions to
the overlying retinaculum. For this reason, many authors in the past
advised that portions of the extensor retinaculum located over the site
of tendon repair be excised to prevent adhesions. However, some
surgeons have noted no statistical differences in their results when
comparing zones VI, VII, and VIII. They repaired each retinacular rent
primarily, and used traditional postoperative immobilization. The
excellent results with early dynamic splinting suggest that excision of
portions of the retinaculum over the tendon repair site may not be as
important as previously believed. However, limited excision of portions of the retinaculum does no harm, and may facilitate tendon exposure and gliding, especially in repairs
in which there might be some impingement between the suture site and the adjacent retinaculum.
 |
|
Figure 12.2-13 Techniques for secondary reconstruction of extensor tendon dislocation at the MCP joint.
|
-
If the surgeon is concerned about
maintaining the anatomic integrity of the retinaculum, the traumatic
openings in the retinaculum may be extended distally and proximally at
each end of the retinacular laceration to facilitate tendon repair and
then reapproximated. -
The tendon is repaired using a standard core-type suture of appropriate nonabsorbable material.
-
The adequacy of the retinacular restraint is verified by passive flexion and extension of the fingers and wrist.
-
Multiple tendon injuries at this level may be dealt with by appropriate excision of the retinaculum as needed.
-
Portions of the retinaculum should be
preserved either proximal or distal to the suture line to prevent
bowstringing; this is usually technically feasible. -
Although it has been recommended that
complete excision of the extensor retinaculum be performed in
lacerations at multiple levels, it is my opinion that complete excision
of the retinaculum is seldom, if ever, necessary, even in this type of
injury. Some portion of the retinaculum can usually be preserved, and
adhesions that limit function are unlikely, especially if early dynamic
splinting is used. -
Tendons lacerated at this level retract, and traumatic wounds must be extended proximally and distally to find the tendon ends.
-
In many instances, the surgeon must deal
with multiple tendon lacerations, and the sorting out and matching of
these tendon ends for later suture may be quite tedious and time
consuming. -
A method of intraoperative tendon
labeling has been described, and avoids the repetitive identification
of tendon ends and thus saves operative time.-
The method involves the placement of a
4-0 nonabsorbable suture into each cut end using a grasping suture
technique such as the two-suture, modified Kessler. -
The free ends of the suture material are
then clamped in a hemostat and a Steri-Strip is placed through the
thumb or finger hole, or around one of the proximal shanks of the
hemostat. It is then folded on itself. -
A sterile marking pen is used to write the name of the tendon on the Steri-Strip.
-
After all tendons have been labeled, they
are easily matched and repaired using the same suture that initially
tagged the tendon ends.
P.204 -
tendons may rupture following a closed fracture or may dislocate
following injury to the retinaculum. The EPL and EDC tendons may
rupture following a Colles’ fracture, and the extensor carpi ulnaris
(ECU) tendon may dislocate ulnarward with forceful supination, palmar
flexion, and ulnar deviation. The radially situated extensor tendons
(EIP and EDC to index and EPL to the thumb) may be entrapped, and may
rupture in Smith’s and Galeazzi’s fractures. In Galeazzi’s fracture,
the ECU may be trapped between the dorsally displaced ulnar head and
avulsed ulnar styloid, or the extensor digiti minimi (EDM) tendon may
be caught beneath the radial border of the dorsally dislocated ulnar
head.
-
Impending rupture of the EPL has been treated by subcutaneous transposition from its canal.
-
Treatment of acute ruptures of the EPL
tendon is by transfer of the EIP tendon (or intercalary graft) and the
ruptured communis tendons by intercalary graft, or by suturing the
distal tendon stump to the adjacent extensor tendons. -
Dislocation of the ECU tendon is treated
by repairing the fibro-osseous sheath with a free tendon graft or a
portion of the extensor retinaculum.
by laceration or traumatic rupture. Although extensor tendon rupture at
the musculotendinous junction is rare, such injuries may be due to
sudden, forceful traction forces caused by gloves caught in revolving
machines.
-
In lacerations, the distal aspect of the
junction (the tendon) accepts and holds sutures satisfactorily, but the
muscle component is less likely to retain the suture. -
Although it is theoretically possible to
place the sutures in the muscle through the fibrous tissue origins of
the tendon in the muscle belly, it is not always possible to obtain a
suitable repair. -
If such repairs are tenuous, the surgeon
may elect to restore function by tendon transfer or by side-to-side
suture, as recommended for management of musculotendinous ruptures.
little-finger proprius, arise from the region of the lateral epicondyle
at the elbow. The thumb extensors and abductors, along with the
proprius tendon of the index finger, arise from the forearm below the
elbow. Injuries at this level are usually caused by penetrating wounds
with knives or pieces of broken glass. The size of the skin wound may
give little indication of the magnitude of the injury. Single or
multiple functional units may be injured. The demonstrated loss of
function may be the result of muscle transection, nerve injury, or
both. Such loss of function in a penetrating injury in the proximal
forearm may defy accurate preoperative diagnosis. The radial nerve at
the level of the distal arm gives off branches to the brachialis,
brachioradialis, and the extensor carpi radialis longus (ECRL). A major
division of this nerve then occurs into the sensory branch and the
posterior interosseous nerve (PIN). The superficial (sensory) branch
continues distally under cover of the brachioradialis into the forearm,
wrist, and hand areas. The posterior interosseous nerve gives branches
to the extensor carpi radialis brevis (ECRB) and supinator, which it
penetrates and supplies, and then innervates the remainder of the
extensor muscle group.
-
Experimental data on repaired muscle
lacerations in laboratory animals (rabbits) imply that useful but
incomplete function can be restored with adequate repair of skeletal
muscle. -
A muscle segment totally isolated from its motor point may not contribute to the contractile function of the innervated muscle.
-
In a series of patients with forearm
flexor muscle lacerations, it was noted that tendon grafting was an
effective method of repair to overcome extensive defects. -
The indication for this technique is
laceration of two or more muscle bellies with at least 50% of the
muscle substance lacerated. -
A penetrating wound with functional loss
in the proximal third of the forearm must be carefully explored to
determine the exact etiology of the loss. -
Under tourniquet control and appropriate
anesthesia, the wound margins are debrided and then extended proximally
and distally and the extent of damage noted. -
For muscle grafting, the palmaris longus
and long toe extensor tendons are used and passed through the
superficial epimysium, muscle belly, and deep epimysium proximally and
distally and sutured to themselves with a Pulvertaft side-weave
technique.-
One to three grafts are used, as required.
-
-
The limb is immobilized for 3 weeks, with the elbow at 90 degrees.
-
Protected motion is started at 3 weeks, and progressive motion is started at 6 weeks.
-
Many times it is impossible to determine nerve damage at the time of surgery in the immediate postinjury period.
-
After 7 to 10 days, however, a denervated
muscle will spontaneously contract for several minutes under the
influence of succinylcholine used during induction of general
anesthesia. -
Additional information may be gained by electrodiagnostic studies at 3 to 4 weeks postinjury.
-
The decision to undertake secondary nerve
repair or reconstruction versus tendon transfer depends on the judgment
and experience of the surgeon. -
If there is evidence of nerve involvement, the appropriate branches are identified and traced out to their insertions.
-
Penetrating wounds often injure the nerve at or near its entrance into the muscle belly.
-
Retraction of the distal nerve stump into the muscle belly may occur, and may defy location and subsequent repair.
-
-
If the lesion is confined to the muscle
belly, definitive repair is carried out using sutures or tendon grafts
and sutures, as previously described. -
The muscle is usually quite hemorrhagic, and muscle planes are difficult to identify.
-
Identification is aided by evacuation of the hematoma, irrigation, and gentle sponging of the cut muscle ends.
-
Identifying intramuscular fibrous septa
and fascia for the placement of sutures aids in preventing the sutures
from pulling out of the muscle.
-
-
Coaptation of the cut ends of those muscles that arise at or distal to the elbow is aided by wrist extension.
-
If suitable repair cannot be obtained by these methods, tendon transfers may be required.
-
Postoperatively, the extremity is
supported in a plaster splint or cast that maintains the wrist in 45
degrees of extension and the MCP joints in 15 to 20 degrees flexion. -
The elbow joint is immobilized in 90 degrees of flexion if the muscles involved arise at or above the lateral epicondyle.
-
Immobilization is continued for 4 weeks
postinjury, and then protected range of motion is permitted—but a night
splint is used to maintain the wrist in extension for another 2 weeks.
been immobilized in extension for 3 to 4 weeks. However, in some
instances, this has resulted in adhesions between the extensor tendon
and the surrounding tissues. This has been especially true when the
tendon injury was associated with a crush injury, surrounding
soft-tissue loss, infection, underlying fracture, or joint-capsule or
flexor-tendon injury. Significant and extensive research (both basic
and clinical) has focused on the best methods of postoperative
management of flexor tendon injuries, and controlled and early passive
motion of the tendon suture site provided by dynamic splinting has
proved to be a useful method to promote a well-healed, smooth,
nonadherent, gliding flexor tendon surface, with improved tensile
strength. This body of evidence regarding the rehabilitation of flexor
tendon injuries with dynamic splinting is applicable to extensor tendon
injuries, and many clinical studies have supported this concept.
dynamic splinting and early active motion in extensor tendon injuries,
even in the most problematic zone III injuries. At this time, only zone
I and II injuries and zone III closed boutonniere injuries are treated
by static splinting. The protocols that follow have proven to be useful
in my practice. However, the reader should note that improvements and
changes might be made to these protocols in the future as more
experience is gained.
applicable when multiple extensor tendons are injured beneath the
extensor retinaculum and when there are associated injuries. The
extensor tendons at the wrist level are surrounded by a synovial sheath
and constrained by fibro-osseous and fibrous tunnels. Indiscriminate
sacrifice of the extensor retinaculum results in altered biomechanics
and poor function. The use of controlled passive motion has been
clearly shown to improve results in flexor tendon injuries, and these
principles are now applied to extensor tendon injuries:
-
Extensor tendon injuries can be placed in
an outrigger splint that maintains passive extension using elastic
traction, but that allows limited active flexion (Figure 12.2-14). -
Excursion of the repaired extensor tendon is achieved by active flexion.P.206
![]() Figure 12.2-14 Dynamic splint for early motion of extensor tendon injuries in zones V to VI.
Figure 12.2-14 Dynamic splint for early motion of extensor tendon injuries in zones V to VI. -
Splinting is started 3 to 5 days after surgery and is maintained for 5 weeks.
-
Active flexion is performed 10 times an hour.
historically demonstrated higher percentages of extensor lag and loss
of flexion. This led to the development of a rehabilitation protocol
based on protected movement of the injured finger. The efficacy of the
short arc motion for zone III extensor injuries was based on the fact
that 30 degrees of flexion at the PIP joint results in a calculated
tendon excursion of 3.75 mm.
-
In this protocol, developed by Evans, a
thermoplastic palmar static splint is used to immobilize the PIP and
DIP joints in full extension, except during exercise.-
The splint is taped directly over the PIP and DIP joints.
-
Two thermoplastic exercise splints are used:
-
Type I, for PIP joint motion, is a palmar splint with 30 degrees of PIP flexion and 20 to 25 degrees for the DIP joint.
-
Type II, for DIP flexion, is a palmar static splint that maintains the PIP joint in full extension and keeps the DIP joint free.
-
-
-
The exercise regimen is as follows:
-
First 2 weeks:
-
The static splint is removed on the hour
for 20 repetitions of PIP and DIP joint exercise, with the wrist at 30
degrees of flexion and the MCP joint at or near 0 degrees of extension. -
The patient holds the type I splint in
place beneath the proximal phalanx, maintains the MCP joint in full
extension, and, beginning from full extension, actively flexes the PIP
and DIP joints to the restraints of the splint. -
Each exercise is performed slowly and sustained briefly in full extension for 20 repetitions.
-
The type II splint is then held in place
to maintain the PIP joint in full extension, and the DIP joint is fully
flexed and extended. -
If lateral band repair was required, the flexion is limited to 30 to 35 degrees.
-
The patient is instructed in what Evans terms “minimal active muscle tendon tension,” which represents a force of about 300 g.
-
-
Third week:
-
The type I splint is altered to allow 40 degrees flexion at the PIP joint if no extensor lag has developed.
-
-
Fourth week:
-
The type I splint is altered to allow 50 degrees of flexion if no extensor lag is present.
-
This is increased to 70 to 80 degrees by the end of the 4th week if the PIP joint is actively extending to 0 degrees.
-
If an extensor lag develops, flexion
increments should be less, and active extension exercises and extension
splinting should be emphasized.
-
-
with other dynamic protocols for extensor tendon injuries, is most
suitably used in patients who are reliable and well-motivated, and is
based on the availability of an experienced and capable hand therapist.
safe as well as effective in limiting adhesions after extensor tendon
injury. This amount of gliding is achieved by active MCP-joint flexion
ranging from 27.5 degrees to 40.9 degrees (index, 28.3 degrees; long,
27.5 degrees; ring, 40.9 degrees; little, 38.3 degrees).
-
The method of postoperative management
for extensor tendon injuries in finger zones V to VII begins with
dynamic splinting 3 to 5 days after surgery. -
The wrist is positioned in an appropriate
amount of extension to relieve tension at the repair site. This is
usually 40 to 45 degrees. -
The MCP and IP joints are supported at 0 degrees in elastic traction slings attached to an outrigger device (see Figure 12.2-14).
-
A palmar block limits MCP flexion to the arc of motion previously noted to result in 5 mm of extensor tendon excursion.
-
The patient is instructed to actively
flex the MCP joints, but to allow the elastic traction on the outrigger
device to passively return the digital joints to 0 degrees. This
exercise is done 10 times per hour. -
Dynamic splinting is discontinued between
the 3rd and 4th weeks; active motion is then started using gentle
active and active assistive exercises that emphasized extension at the
MCP joint with the wrist supported in extension. -
Between 4 and 5 weeks postsurgery,
individual finger extension and the claw position are emphasized to
direct controlled stress to the adhesions. -
At 5 to 6 weeks, finger flexion is emphasized.
-
At 7 weeks, resistance, functional
electric stimulation, and dynamic flexion splinting are used as needed
to encourage full finger flexion. -
During the phase of dynamic splinting,
resting the digital joints at 0 degrees prevents extensor lag.
Controlled MCP motion prevents extension contractures, maintains the
integrity of the collateral ligaments, and lessens the effects of
adhesions at the repair site. -
With the wrist and MCP joints fully
extended, passive movement of the IP joints may be performed without
affecting tendon excursion in zones V, VI, and VII, thus avoiding
stiffness in these joints.
-
Postoperative management of lacerations
of the ECRL, ECRB, and ECU includes immobilization of the wrist at 40
to 45 degrees extension for 4 to 5 weeks with the fingers free. -
Progressive active and gentle passive
range of motion is started after 4 to 5 weeks, and a night splint that
keeps the wrist in 40 to 45 degrees of extension is used for an
additional 2 weeks.
-
Postoperative management includes static
immobilization of the wrist in 40 to 45 degrees of extension and the
MCP joints in 15 to 20 degrees of flexion for 4 weeks, followed by a
static night splint that maintains the wrist in extension for an
additional 2 weeks. -
Flexion of the MCP joints may be started at 2 weeks against elastic traction resistance.
JG, Heminger H, Mass D. Comparative biomechanical performance of
4-strand core suture repairs for zone II flexor tendon lacerations. J
Hand Surg 2002;27:508–517.
MJ, Gelberman RH, Smith DG, Silver MA, Gellman H. Repair of severe
muscle belly lacerations using a tendon graft. J Hand Surg
1987;l2A:406–412.
E. Experimental studies of tendon injuries. In: Trumble TE, ed. Hand
surgery update 3, hand, elbow and shoulder. Rosemont, Il: Amer. Soc
Surg Hand, 2003:233–251.
JR. Boutonniere deformity. In: Strickland JW, ed. Master techniques in
orthopedic surgery: the hand. 2nd Ed. Philadelphia: Lippincott Williams
& Wilkins, 2005.
JR. Extensor tendons-acute injuries. In: Green DP, Hotchkiss RN,
Pederson WC, eds. Green’s operative hand surgery. 4th Ed. New York:
Churchill Livingstone, 1999:1950–1987.
JR, Botte MJ. Palmar hand. In: Surgical anatomy of the hand and upper
extremity. Philadelphia: Lippincott Williams & Wilkins,
2002:532–641.
RB. An update on extensor tendon management. In: Hunter JM, Schneider
LH, Mackin EJ, et al., eds. Rehabilitation of the hand, 4th Ed. St.
Louis: CV Mosby, 1996:655–706.
RB, Thompson DE. An analysis of factors that support early active short
arc motion of the repaired central slip. J Hand Ther 1992;5:187–210.
WW, Manske PR, Bollinger BA, et al. Effect of pulley excision on flexor
tendon biomechanics. J Orthop Res 1986;4:96–101.
LH. Flexor tendons-late reconstruction. In: Green DP, Hotchkiss RN,
Pederson WC, eds. Green’s operative hand surgery. 4th Ed. New York:
Churchill Livingstone, 1999:1898–1949.
JG. Flexor tendon repair. In: Trumble TE, ed. Hand surgery update 3,
hand, elbow and shoulder. Rosemont, Il: Amer. Soc Surg Hand,
2003:253–259.
KL, Andersson CH. Two new methods of tendon repair: an in vitro
evaluation of tensile strength and gap formation. J Hand Surg
1993;18A:58–65.
JW. Flexor tendons-acute injuries. In: Green DP, Hotchkiss RN, Pederson
WC, eds. Green’s operative hand surgery. 4th Ed. New York: Churchill
Livingstone, 1999:1851–1897.
CJ, Johnson G, Doyle JR, et al. A mechanical study of six digital
pulley reconstruction techniques: part I. Mechanical effectiveness. J
Hand Surg1989;14A:821–825.