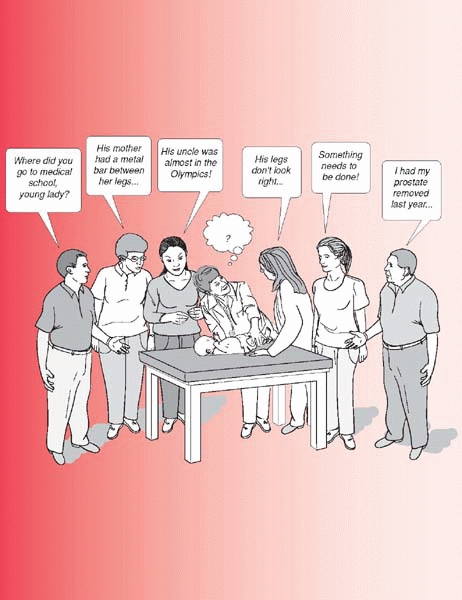
Dealing with Families
|
|
a significant amount of time and energy on the part of the doctor and
entire healthcare team. At times, the demands may seem unreasonable.
However, very few things in life compare to the sincere depth of
gratitude we receive from parents, grandparents, and children when
caring for a sick or injured child. One of the wonderful things about
caring for children’s orthopaedic problems is that we can significantly
improve, or cure, most of the children we care for.
perhaps the most painful thing a human may experience, worse than
divorce or loss of a spouse. By extension, when a child is in pain,
sick, or at risk of harm, a parent may actually suffer more than the
child. Anger or other irrational behavior on the parent’s part is a
common response to this stress. A child with health problems can be a
severe stress to a marriage. A recent study1
notes that the chances of the parents living together decreases by 10%
in the 6 months following the child’s first birthday if the child is in
poor health. Surgeons must have broad shoulders to carry the weight of
others’ problems. Acknowledging a parent’s suffering, and accepting
responsibility to care for the parent as well as the child, is an
important aspect of a healthy doctor-family relationship.
staying out of legal trouble in pediatric orthopaedic surgery may be
more dependent on the doctor’s relationship with the family than the
doctor’s clinic skill.
key step for staying out of trouble in pediatric orthopaedics. Parents’
satisfaction with their child’s care is dependent upon their
expectations almost as much as the outcome of surgery. Take this
example of a 3-year-old girl with a midshaft femur fracture: She was
treated in a spica cast that healed in five degrees of varus, with a
minor limp persisting three
months
after injury. At this point many parents are concerned and even upset
when they see that the bone has healed in a “crooked” position, and
that their daughter is not walking normally. The fact that the doctor
appears unconcerned may only amplify their unhappiness.
 |
|
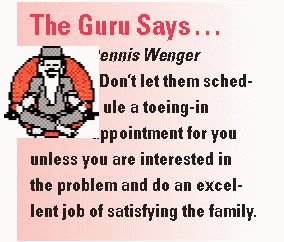
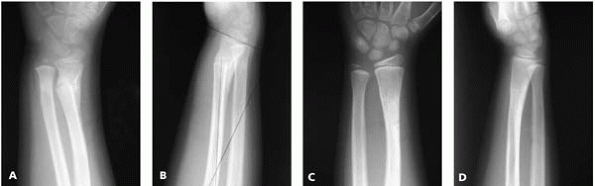
▪ FIGURE 3-1 A:
An 8-year-old boy with a proximal humerus fracture. The father is a medical malpractice plaintiff attorney and was referred to one of the authors (DLS) with a recommendation of surgery from the original orthopaedic surgeon. Treatment with a shoulder immobilizer was started. B: One month after injury. Patient’s range of motion is poor and father’s concern is increased. Teaching files showing remodeling of similar fractures helped relieve parents’ and surgeon’s anxiety. C: One year after injury. Full range of motion with no sequelae. |
 |
|
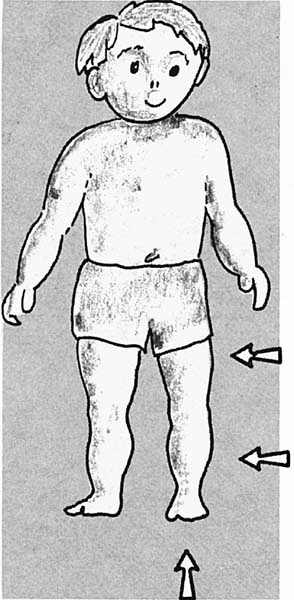
▪ FIGURE 3-2 A 6-year-old girl with angulation on x-ray and a bump on her arm 1 month after injury (A, B).
The mother, who is a doctor, and married to author (DLS), was less than happy. Teaching files of remodeling helped restore marital bliss. Six months later the fracture has nearly fully remodeled (C, D). |
may be thrilled that the femur healed in a nearly straight position
without their child having scars or facing the risks of surgery. And
furthermore, they are quite excited that her limp is almost gone
already, as they expected her to limp for six months.
fracture remodeling (forearm, femur, and proximal humerus are good
examples) is a highly efficient means of guiding parental expectations
and defusing unwarranted anxiety. Feel free to make copies of Figures 3-1 and 3-2
for your patients. Time spent at the beginning of treatment often saves
time later explaining “unexpected” progress, and pays rich dividends
towards the families’ satisfaction and the doctor’s reputation.
guardian. Too many surgeons discover at the time of surgical consent
that the child’s legal guardian is unaware of the planned surgery.
Beware that some parents going through a divorce consciously or
unconsciously use their child’s healthcare as a weapon against each
other. A surgeon may help diffuse this dynamic with a clear reminder to
both parents of the common goal of doing what is best for the child.
Although it takes more time, it may be best to meet with each parent
separately or follow-up with a phone call to the absent parent at the
end of the day. It is important that neither parent senses you are
taking sides or have secrets with the other parent; maintain
neutrality. Make certain your responsibility to the child presides over
any social discomfort on your part.
relationship in terms of authority. A common scenario is that the
parent wants you to pronounce what is “best” for the child, with the
understanding that the parents will enforce your will. This may be
wonderful for the toddler who needs to take antibiotics, but can be
devastating for the 13-year-old girl considering brace treatment for
scoliosis. The point at which children turn into self-aware people, in
charge of their own destiny, varies by family, social setting, and
child.
to the parents; most experts recommend erring in the other direction.
Early in the exam, talk to the child. Even if young children may not
grasp all you say, looking them in the eye, speaking gently, and
showing them respect convinces them you are on their side. The parents
will still hear your words, and just as important, they will recognize
your caring approach to their child.
with newly diagnosed scoliosis who may be a candidate for brace
treatment. Parents will often make it clear that they will do anything
possible to avoid surgery and their child will wear a brace at all
times even before the child has a chance to express an opinion. At this
point the stage has been set for brace compliance to become a major
issue between parent and child.
potential impasse is to present information for and against bracing and
ask the families not to make a decision now, but to return after their
decision has been made or for further discussion. Assure the teenager
that you are there to help, and you recognize that wearing a brace is
physically and emotionally difficult. It has been said that the teenage
girl who does not cry when brace treatment is recommended has already
decided not to wear it.
children and teenagers in open-minded Los Angeles in situations where
the best medical treatment is open to debate. Tell older children or
adolescents that you work for them, not
their parents, and within reason you will not do anything to their body
without their permission. While this amount of “teenage empowerment”
will not work for all families or surgeons, many parents are happy with
this, as they realize you are addressing the emotional and physical
needs of their child. It often helps to assure parents that older
children, when given such responsibility, and an open dialog with their
doctor, will almost always choose a rational course.
at Columbia University College of Physicians and Surgeons, television
personality Larry King said, “The special thing about doctors, is
people listen to their doctors more than any other profession.”
Although this may not be true for hospital administrators, it probably
is true for the rest of the population. Be wary of how various
treatment options are presented, because your prejudices will almost
certainly come through. To use the example of bracing for scoliosis, if
the world’s literature has not conclusively established the efficacy of
bracing, should we use our authoritative position to present a
one-sided opinion to patient and family? Often providing a balanced
view of various options, with your guiding opinion, allows a family to
participate in treatment decisions. If children, especially teenagers,
feel they have chosen their course of treatment, everyone is happier,
and compliance is more likely.
is suspected. The language used in this setting should be chosen very
carefully. The phrase “child abuse” is associated with parental blame
or inadequacy, and will most likely lead to defensiveness on the part
of the parents. Saying, “There is a possibility that someone may have
injured the child” may be less likely to alienate the parents. This
conversation should be held in
a
private setting, in an unrushed manner. If necessary, the physician may
add that by law, if there is any question of the possibility of child
abuse, the child must be evaluated or the physician could lose his or
her license. This may help the parents understand that the physician is
not acting out of malevolence. Again, in keeping with the central theme
of this chapter, if the parents sense that you genuinely care for the
child, problems are uncommon. To stay out of trouble on the topic of
child abuse, if there is any suspicion, get the proper specialists
involved. Be cognizant that some parents may react violently,
particularly if drugs or alcohol are involved.
ground when things get heated. In this case, the common ground is easy
to find: parents and the doctor want what is best for the child. Simply
telling parents, “My job is to give your child the very best care
possible, we are on the same team” is generally all it takes. But
remember, actions and body language speak louder than words. If you
really don’t feel that you are giving 100% for that child and family,
for whatever reason, you should probably not be the child’s doctor. For
those cases in which the doctor and parents really do not get along,
stay out of trouble and suggest a second opinion before doing surgery (if possible).
anything. I am not dumb, and I can see that junior’s (feet turn in/feet
are flat/legs are bowed, etc.). I want something done about this.” This
is the time to take a Taoist approach, avoid confrontation, and go with
the parent’s spirit of wanting what is best for the child. Your opinion
that nothing needs to be done is based on knowledge that the parent
does not have. Before stating your opinion, share your knowledge with
the parent, and they are quite likely to arrive at the same opinion.
Remember that parents generally want what is best for their children.
If they are asking for something else, it is usually due to a lack of
medical understanding.
technically possible to cut junior’s leg in half, and untwist it.
Explain the risks to nerves and blood vessels, the possibility of
infection, scarring, compartment syndrome, multiple surgeries, etc. And
provide the parent with other alternatives as well, such as the fact
that in most children the tibias untwist over time without any
treatment. While this may seem a bit theatrical, it makes for an
efficient appointment and a satisfied parent.
complication is recognizing it and accepting it yourself. The next
difficulty is explaining it to the family. If you have a complication,
a doctor they see for a second opinion or the plaintiff’s expert
witness is likely to recognize it. Parents would certainly appreciate
hearing it from you first. It would be nice to be perfect, but most of
us (especially husbands) should simply aspire to recognize and accept
fault early and often. There may be some benefit both legally and
clinically to sharing the case with trusted peers for advice. Tell the
family you did this, so they know you are taking the situation
seriously and giving it extra attention. If handled correctly, families
of children who have had complications often become your staunchest
supporters.
surgeons caring for children and physical therapists. Physical
therapists spend more time with your patients than you do and develop a
bond with the families, especially with long-term patients. Therapists’
recommendations for bracing and other treatments may bare no semblance
to anything you learned in medical school or residency. For example, a
therapist may recommend custom-made foot orthoses for back pain (or
horseback riding for cerebral palsy). You may not agree with this
treatment. How do you respond? One, simply say no orthotics. Two,
suggest a trial of less-expensive off-the-shelf shoe inserts. Three,
feign agreement and write a prescription for expensive custom-made
orthoses and contribute to the rising cost of healthcare.
biomechanics. Which treatment or brace you order may have a positive or
negative placebo effect depending on the therapist’s opinion of it.
Avoid the pitfall of belittling the therapist’s opinions, as it makes
the doctor look unprofessional, creates conflicting loyalties in the
family, and just possibly, the therapist may be right. We have all
learned from therapists over the years.
-
The doctor and the parents both want what is best for the child. You are on the same team.
-
When a child suffers, the parent suffers. Take care of the parent as well.
-
Parent satisfaction
is directly dependent on pretreatment expectations: parents are
happiest if expectations are restrained in the beginning and later
surpassed. -
When a problem occurs: recognize it, accept it, and explain it to the family as soon as possible.
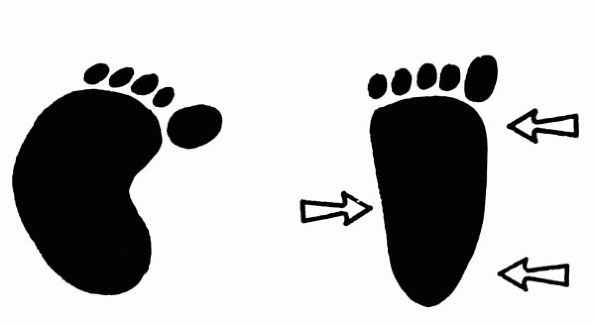
not a serious problem. It may be caused by the child’s position while
in the mother’s uterus and usually corrects over time without
treatment. These conditions generally do not cause any limitation in
activity or delay normal growth and development.
first few years of life. It develops from one of three areas: the foot,
the shin, or the thigh (Figure 1).
 |
|
▪ FIGURE 1. The origin of intoeing may lie in the thigh, the shin, or the foot.
|
and is very common. If the foot can be easily put in the correct
position, no treatment is necessary, though your doctor may ask you to
stretch the feet at home, and return to the office to make certain the
feet are straightening with growth (Figure 2).
In the unusual case that the foot cannot be easily straightened by
gentle manipulation, your physician may recommend treatment, most
frequently a cast. Scientific studies do not support using a brace or
special shoes to help straighten the foot faster than normal growth.
twisted or rotated inward and cause the foot to turn in. It is often
first noticed when your child starts walking. Many parents believe the
turned-in feet cause their children to trip more frequently.
Fortunately, children usually grow out of this condition before age 10.
If a child does not grow out of this condition, there is scientific
evidence suggesting that internal tibial torsion is associated with
being a faster sprinter. Many famous athletes have tibial torsion.
There is no scientific evidence that bracing, special shoes, exercises
or any other treatment short of surgery can correct the torsion.
Surgery is very rarely needed in otherwise normal children (Figure 3).
 |
|
▪ FIGURE 2. Three point pressure straightens the foot.
|
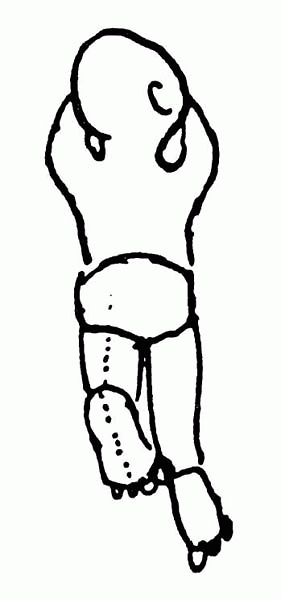
When your child starts walking you may notice the feet and knee caps
point inward. When the child runs, the feet may fly out sideways and
make running appear clumsy. The turning in of the feet and knees may
even appear to worsen in the first few years during the normal period
of relaxation of the child’s hips. Your child may be able to twist legs
or sit in positions that would be uncomfortable for most adults (Figure 4).
Fortunately, this condition will gradually improve over time (up till
age 10) as your child grows and does not require treatment. Surgery is
very rarely needed in otherwise normal children. There is no scientific
evidence that braces, sitting position, exercises, or any treatment
corrects or speeds up the natural improvement of this condition.
 |
|
▪ FIGURE 3. Thigh-foot angle.
|
and grandparents want something done, and feel that special shoes or
braces couldn’t hurt. Frequently, members of the family may have been
treated with braces during childhood and their feet stopped turning in.
It is important to remember that even if these people had not been
treated with braces, their feet would have probably stopped turning in
as a part of natural growth.
shoes as children had lower selfesteem, a poorer self image, and recall
being teased about their shoes. Corrective shoes or braces may hurt the
child, and should not routinely be used to make the family feel that
“something is being done.”
 |
|
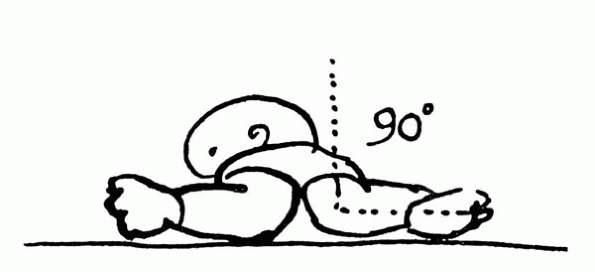
▪ FIGURE 4. Hip Rotation.
|