HALLUX VALGUS
deviation of the proximal phalanx on the metatarsal head. In the
majority of patients, the deformity is due to improper shoe wear. It
occurs almost 10 times more frequently in women than in men.
-
Contracture of the lateral joint capsule
-
Attenuation of the medial joint capsule
-
A medial eminence of varying size
-
Pronation of the hallux as the deformity becomes more severe
-
Medial deviation of the first metatarsal,
giving rise to an increase in the intermetatarsal angle. This leads to
an uncovering of the sesamoids, which are anchored in their lateralward
position by the adductor hallucis.
impingement of the hallux against the second toe can lead to
destabilization of the second metatarsophalangeal joint, resulting in
an overlapping of the hallux by the second toe. Occasionally,
underlapping may occur.
hallux and first metatarsal is diminished, resulting in increased
weight bearing by the second metatarsal head, which results in
metatarsalgia, sometimes associated with a callus. The decreased weight
bearing is due to the lack of plantar flexion of the first metatarsal
in the last half of stance phase due to the decreased function of the
windlass mechanism of the plantar fascia.
When this condition is present, a first metatarsocuneiform joint fusion
should be carried out in conjunction with the hallux valgus repair.
with regard to the hallux valgus deformity. As a general rule, the
chief complaint is pain over the medial eminence, although sometimes,
despite a severe deformity, the patient’s main complaint is a second
toe deformity and associated symptoms.
lifestyle, and management of the disability. The history should answer questions such as the following:
-
Is the primary problem that the patient cannot wear certain dress shoes or even a wide soft shoe?
-
At work, how much time does the patient spend standing each day?
-
Does the patient participate in athletics?
-
Has the patient tried conservative care such as changing shoes or using a bunion splint?
-
Begin with the patient standing.
-
Observe the alignment of the foot and lower extremity. Note the deformity of the great toe and lesser toes.
-
Seat the patient and measure the range of
motion of the ankle, subtalar, and transverse tarsal joints with
particular attention to the first metatarsophalangeal joint. -
Carefully assess the neurovascular status
of the foot. If there is any question about the vascularity, obtain an
arterial Doppler study.
-
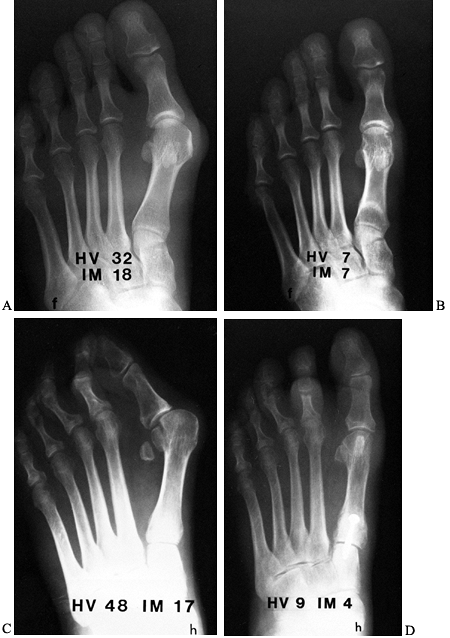
Always obtain anteroposterior (AP) and lateral radiographs of the foot weight bearing.
-
Measure the first metatarsophalangeal
joint angle, which should be less than 15°. The intermetatarsal angle
should be less than 8°. -
Note the position of the sesamoids and the size of the medial eminence (Fig. 112.1).
 Figure 112.1. The normal hallux valgus (HV) angle is less than 15°; the intermetatarsal (IM) angle less than 8°.
Figure 112.1. The normal hallux valgus (HV) angle is less than 15°; the intermetatarsal (IM) angle less than 8°. -
Look for arthrosis in the first
metatarsophalangeal joint and assess whether the joint is congruent or
incongruent. A congruent joint is one with no lateral deviation of the
proximal phalanx on the metatarsal head. An incongruent joint is one
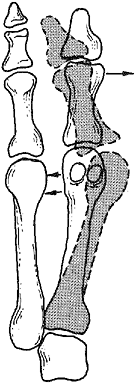
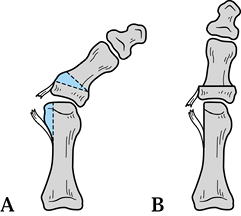
with lateral deviation of the proximal phalanx on the metatarsal head (Fig. 112.2).![]() Figure 112.2. A:
Figure 112.2. A:
A congruent metatarsophalangeal joint is one in which there is no
lateral subluxation of the proximal phalanx on the metatarsal head. B:
An incongruent metatarsophalangeal joint is one in which there is
lateral subluxation of the proximal phalanx on the metatarsal head. -
Measure the distal metatarsal articular
angle (DMAA), which is the relationship of the articular surface to the
long axis of the metatarsal. Normally, this should be less than 10° of
lateral deviation (Fig. 112.3). Figure 112.3.
Figure 112.3.
Radiograph demonstrating the distal metatarsal articular angle, which
measures the relationship between the articular surface of the
metatarsal and the long axis of the first metatarsal. Normal should be
less than 10° of lateral deviation.
-
Explain the nature of the problem to the
patient. Try to talk the patient into using broad, soft-soled shoes,
preferably with a low heel, that provide adequate room for the great
toe and the medial eminence. Many patients can be made comfortable with
just a change of shoe style. Some women, particularly young women,
enjoy wearing stylish shoes and have difficulty with this type of
conservative management; not infrequently, they will request surgery. -
Advise the patient that, after bunion
surgery (in our experience), only two thirds of patients can wear shoes
in an unrestricted manner, leaving a third requiring restricted shoe
wear. People in this latter group typically have broad, wide feet, so
that even after corrective surgery, even though they now have straight
metatarsophalangeal joints, their feet still cannot fit into small,
narrow, pointed-toe shoes.
bunion surgery is the correct selection of the operative procedure. Not
all bunion deformities are alike. Therefore, a single operative
procedure will not result in a satisfactory outcome for all types of
deformities.
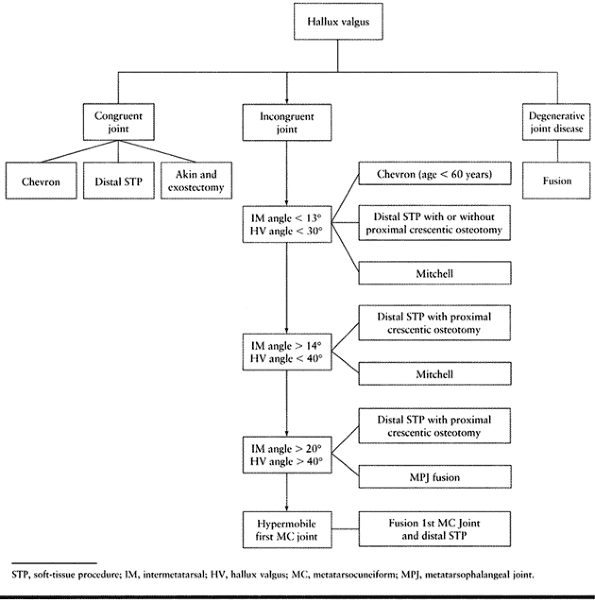
congruent or an incongruent joint. This is important because if the
joint is congruent, the proximal phalanx cannot be rotated on the
metatarsal head to correct the deformity; if the deformity is
incongruent, however, the proximal phalanx can be rotated on the
metatarsal head to correct the deformity. The algorithm in Table 112.1 can help in the decision-making process.
 |
|
Table 112.1. Algorithm for Treating Hallux Valgus
|
-
If the DMAA is increased, use a medial
closing wedge with a chevron osteotomy, rotating the metatarsal head
medially and thereby correcting the DMAA (14). -
Other procedures include a distal
soft-tissue procedure or an Akin procedure (osteotomy of the proximal
phalanx) along with excision of the medial eminence.
incongruent joint, the operative procedure depends on the severity of
the deformity. The numbers presented in Table 112.1 should be used as suggested values: They are not etched in stone.
-
If the hallux valgus is mild with a
hallux valgus angle of less than 30°, and the intermetatarsal angle is
less than 13°, use a chevron osteotomy or distal soft tissue procedure
to correct the deformity. -
If the deformity is severe with a hallux
valgus angle of more than 40° and the intermetatarsal is greater than
20°, use a distal soft-tissue procedure with proximal osteotomy if
there is minimal arthrosis. If arthrosis is present or the deformity is
too severe, then consider an arthrodesis. -
If there is significant arthrosis of the
metatarsophalangeal joint, an arthrodesis is probably the procedure of
choice. Place the hallux at about 15° of valgus and 10° to 15° of
dorsiflexion in relation to the ground.
It can be utilized as an isolated procedure or in conjunction with
excision of the medial eminence. Do not perform this procedure if the
metatarsophalangeal joint is incongruent. It is a useful salvage
procedure for a mild recurrent hallux valgus deformity with a stable
metatarsophalangeal joint. It is the procedure of choice to correct a
hallux valgus interphalangeus.
 |
|
Figure 112.4. The Akin procedure. A:
Location of the osteotomy in the base of the proximal phalanx. Be sure the base of the osteotomy is distal to the concavity of the articular surface. B: Closure of the osteotomy site and plication of the medial capsule. |
-
Perform the Akin procedure through a
medial incision starting along the medial aspect of the proximal
phalanx and carried proximally to the metatarsal head. Create dorsal
and plantar full-thickness skin flaps, exposing two thirds of the
proximal phalanx and the medial eminence. -
Approach the metatarsophalangeal joint through a vertical capsulotomy and excise approximately 2–3 mm of capsule.
-
Make a dorsomedial capsular incision to expose the medial eminence by hinging the capsule plantar medially.
-
Expose the medial eminence by sharp
dissection and excise it with a sharp thin osteotome. Begin at the
sagittal sulcus in line with the medial aspect of the metatarsal shaft.
Take care not to cut into the shaft. -
Close the capsule, pulling the toe into correct alignment. Avoid a varus position.
-
Make the osteotomy of the proximal
phalanx about 4–5 mm distal to the proximal articular surface. Keep in
mind that the articular surface of the proximal phalanx is concave. Be
certain that the osteotomy is distal to this concavity. -
Remove a wedge of proximal phalanx
measuring 2–4 mm in thickness, depending on the deformity. Once the toe
is straight, fix the osteotomy with crossed Kirschner (K-) wires or
heavy suture material placed through drill holes in the proximal
phalanx.
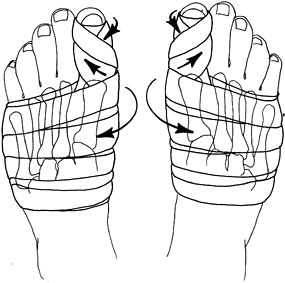
in a dressing for 8 weeks, holding the hallux in a slight varus
position. Use 2-inch Kling and half-inch adhesive tape to firmly hold
the hallux in correct alignment. This permits the patient to ambulate
more comfortably in a postoperative wooden shoe (Fig. 112.5).
 |
|
Figure 112.5.
Radiograph after an Akin procedure. The osteotomy site is often visible for many months, but it is clinically healed in 6–8 weeks. |
subluxation of the metatarsophalangeal joint. If the joint is subluxed
preoperatively, as a rule it will tend to sublux even further following
the procedure (18). Therefore, subluxation is
the main contraindication to an Akin procedure. Only rarely does a
nonunion occur in the proximal phalanx.
-
Develop full-thickness dorsal and plantar skin flaps. Retract the digital nerves out of the way.
-
Having exposed the medial joint capsule,
make a vertical capsulotomy with a #11 blade, excising a 3–5 mm piece
of capsule. Then make an incision through the dorsal medial aspect of
the capsule and strip the capsule off of the medial eminence. -
Remove the medial eminence with an osteotome starting at the sagittal sulcus on a slight oblique angle (Fig. 112.6A).
This is in contradistinction to the plane of the osteotomy that is done
to remove the medial eminence for the Akin or the distal soft-tissue
procedure. This oblique angle is used to create a wide base for the
chevron osteotomy, which is displaced laterally.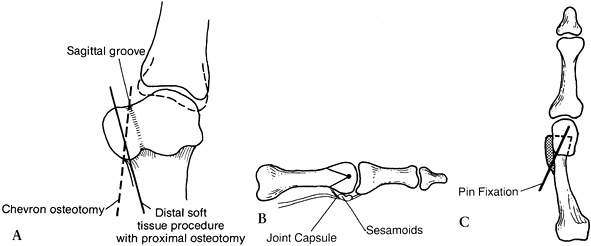 Figure 112.6. Chevron procedure. A: The medial eminence is removed starting at the sagittal sulcus to the base of the medial eminence. B:
Figure 112.6. Chevron procedure. A: The medial eminence is removed starting at the sagittal sulcus to the base of the medial eminence. B:
The apex of the chevron osteotomy starts in the center of the
metatarsal head and is brought proximally. The plantar aspect of the
line of the osteotomy should be proximal to the joint capsule, thereby
avoiding the sesamoid bones. C: The osteotomy site is displaced laterally 20% to 30% of the width of the shaft. -
Make the chevron cut by first drilling a
horizontal hole in the middle of the metatarsal head, and then cutting
the chevron with a small oscillating saw (Fig. 112.6B, Fig. 112.6C).
It is important that the plantar limb of the osteotomy exit proximal to
the sesamoid bones, so that they are not inadvertently damaged. -
Make the cut dorsally at about a 60°
angle to the plantar cut. Do not cut too far through the lateral
cortex, to avoid damage to the vessels along the lateral aspect of the
metatarsal head. -
Once the osteotomy has been completed and the metatarsal head is free, displace it laterally 4–5 mm (3).
Then secure it with an oblique pin passed from proximal to distal. Some
surgeons advocate using a small screw with a larger dorsal bony cut,
but we believe that a single 0.62-inch K-wire is adequate. -
Once this is achieved, remove the medial
prominence of the metatarsal that remains by using the oscillating saw
and buffing any sharp edges. -
Now hold the hallux in a completely
neutral position. Plicate the medial joint capsule by using interrupted
2-0 chromic sutures. If insufficient capsule has been removed, remove
more prior to plicating the capsule. -
After the capsule has been plicated and
the hallux is released, it should stay in a neutral position. If it
tends to drift into valgus, consider excising more joint capsule. If it
is in a slight degree of varus, correct this with the postoperative
dressings.
shoe and a firm, spica-type dressing consisting of 2-inch Kling and
half-inch adhesive tape holding the first metatarsophalangeal joint in
satisfactory alignment. Change this dressing weekly for 8 weeks. When a
K-wire is used to stabilize the metatarsal osteotomy, it can usually be
removed after 4 weeks. Sometimes, premature removal is necessary
because of a minor infection about the pin. After removing the
dressings (at 8 weeks), begin exercises to restore motion in the
metatarsophalangeal joint (Fig. 112.7).
 |
|
Figure 112.7. A: Preoperative radiograph of a mild hallux valgus deformity. B: After a chevron procedure with pin fixation. C: Final result demonstrating satisfactory alignment of the metatarsophalangeal joint.
|
a stiffening of the metatarsophalangeal joint, and varus deformity,
usually due to overplication of the medial joint capsule or inadvertent
tilting of the metatarsal head into lateral deviation. This is possibly
due to loss of fixation of the osteotomy site or a recurrence of the
deformity because the preoperative deformity was too severe (10,11).
by the chevron procedure may be inadequate. To correct, remove more
bone from the proximal limb of the chevron cut. Remove 2–3 mm of bone,
which includes the width of the saw blade, from the medial aspect of
the metatarsal, allowing the head to be angulated in a medialward
direction, thereby correcting the abnormal DMAA. Some authors believe
that release of the lateral joint capsule can be carried out with a
chevron osteotomy, and the literature seems to support this (17,21).
If a capsule release is carried out, it should be at the level of the
joint and distally to avoid the blood supply coming into the metatarsal
head through the joint capsule.
complication but certainly can be disastrous. The incidence is low,
probably 1% or 2%. Exactly why this occurs in some cases is unknown. It
may be due to excessive stripping of the lateral joint capsule, thereby
disrupting the blood supply to the metatarsal head (17,19,22).
If there is complete avascular necrosis of the head associated with
significant collapse, severe disability results. Minor radiographic
changes are usually not of any clinical significance. If a patient
develops avascular necrosis, treat it conservatively for as long as
possible until a painful joint requires arthrodesis. Treat
arthrofibrosis of the metatarsophalangeal joint with vigorous physical
therapy.
correction of the hallux valgus deformity. This results from treating
too severe a hallux valgus deformity, or from failure to recognize an
increased DMAA, so that it was not corrected at the time the chevron
osteotomy was done.
proximal crescentic metatarsal osteotomy is indicated for a wide range
of deformity from mild to severe. It is a procedure that is technically
challenging and needs to be meticulously carried out to achieve the
best clinical results (Fig. 112.8).
 |
|
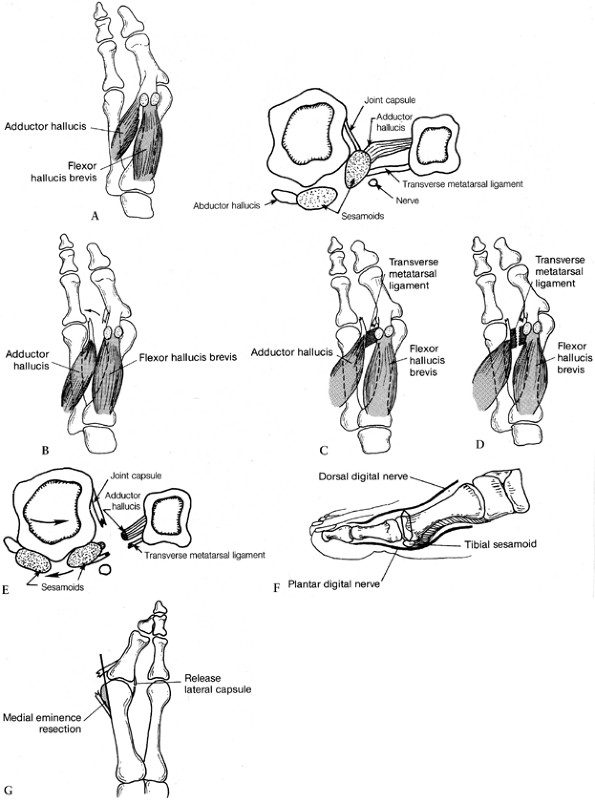
Figure 112.8. Distal soft-tissue procedure. A: The adductor tendon inserts into the lateral aspect of the fibular sesamoid and into the base of the proximal phalanx. B:
The adductor tendon is released from its insertion into the lateral side of the fibular sesamoid and the base of the proximal phalanx. C: The transverse metatarsal ligament passes from the second metatarsal into the fibular sesamoid. D: The transverse metatarsal ligament is transected. E: The three contracted structures on the lateral side of the metatarsophalangeal joint are released. F: The medial capsular incision begins 2–3 mm proximal to the base of the proximal phalanx, and a piece of tissue 3–8 mm is removed. A dorsal medial incision is then made to create a plantar proximally based flap. G: The medial eminence is removed in line with the medial aspect of the first metatarsal shaft. (From Mann RA, Coughlin MJ.Video Textbook of Foot and Ankle Surgery. St. Louis, MO: Medical Video Productions, 1991.) |
-
Make the initial incision on the dorsal
aspect of the first web space in the midline, avoiding the superficial
branches of the deep peroneal nerve. -
Through this incision, release the
lateral joint capsule and the adductor hallucis tendon from its
insertion along the lateral side of the fibular sesamoid and base of
the proximal phalanx (Fig. 112.8B). -
Section the transverse metatarsal ligament, which inserts into the lateral aspect of the fibular sesamoid (Fig. 112.8C, Fig. 112.8D, Fig. 112.8E).
-
Center the second incision over the
medial aspect of the first metatarsophalangeal joint. Carry it down to
the joint capsule and create a full-thickness dorsal and plantar flap.
Take care to avoid the dorsomedial and plantar medial cutaneous nerves (Fig. 112.8F). -
Remove a wedge of capsule from the medial
aspect of the metatarsophalangeal joint. Begin the initial capsular
incision about 2–3 mm proximal to the base of the proximal phalanx.
Make the second portion of the incision more proximal, between 4 and 8
mm, depending on the degree of the deformity that needs to be
corrected. Dorsally, this incision ends about 1 cm medial to the
extensor hallucis longus tendon and plantarly the passes through the
abductor hallucis tendon, ending at the medial aspect of the tibial
sesamoid. -
Expose the medial eminence either by
carefully dissecting the medial joint capsule off the medial eminence
or by making an incision along the dorsomedial aspect of the joint
capsule to create a flap to expose the medial eminence. -
Remove the medial eminence about 1 mm medial to the sagittal sulcus and in line with the medial aspect of the metatarsal shaft (Fig. 112.8G). Smooth the edges with a rongeur.
-
At this point, decide if the metatarsus
primus varus can be corrected without a proximal metatarsal osteotomy.
This is determined by pressing on the first metatarsal to see if it can
be reduced to the second metatarsal. If this occurs without the first
metatarsal springing medially again, then no osteotomy is necessary.
If, however, there is a tendency for the two metatarsals to spring
apart, then an osteotomy at the base of the metatarsal is required. We
use an osteotomy in 80% to 90% of cases (Fig. 112.9) (7).![]() Figure 112.9.
Figure 112.9.
To determine whether an osteotomy is necessary after the distal
soft-tissue release has been done, push the first metatarsal head
laterally. If there is any tendency for the metatarsal head to spring
open, consider an osteotomy. We perform an osteotomy about 90% of the
time. -
Expose the osteotomy site at the base of the metatarsal through a dorsal incision distal to the first metatarsocuneiform joint (Fig. 112.10).
Do the osteotomy about 1 cm distal to the metatarsocuneiform joint. We
prefer to use a crescentic osteotomy with the concavity directed
proximally. The osteotomy is produced perpendicular to neither the
metatarsal shaft nor the bottom of the foot, but halfway between. Cut
the osteotomy with a crescentic blade by using an oscillating handpiece.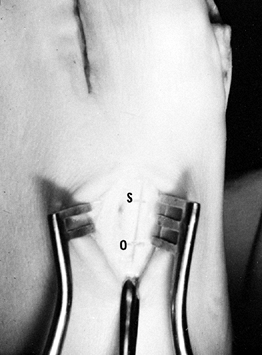 Figure 112.10. The Freer elevator is pointing at the metatarsocuneiform joint. The osteotomy site (O)
Figure 112.10. The Freer elevator is pointing at the metatarsocuneiform joint. The osteotomy site (O)
is about 1 cm distal. If a screw will be used for fixation of the
osteotomy site, it is placed about 1 cm distal to the osteotomy site (S). -
Next, correct the hallux valgus by
placing three sutures in the first web space between the first and
second metatarsals, incorporating the adductor tendon. Pass the suture
through the medial aspect of the capsule of the second
metatarsophalangeal joint, through the adductor
P.3015P.3016
tendon,
and then through the dorsal capsule on the lateral aspect of the first
metatarsal. Tie these sutures after the proximal osteotomy has been
fixed. -
Correct the increased intermetatarsal
angle by freeing all the soft tissues around the osteotomy site, so the
osteotomy can be easily moved. Place a Freer elevator on the proximal
portion of the metatarsal and displace it medially as the metatarsal
shaft is rotated laterally. Displacement of only 2–3 mm allows rotation
of the metatarsal shaft at the osteotomy site, correcting the
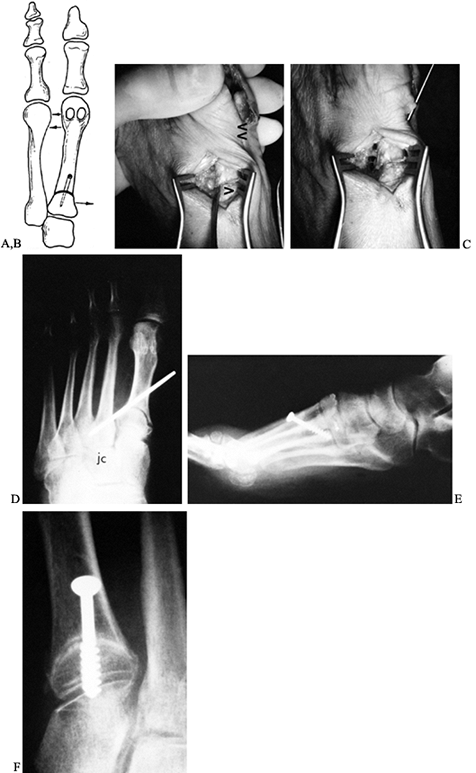
metatarsus primus varus (Fig. 112.11). We prefer to stabilize the osteotomy site with a 4.0 mm, cannulated AO screw, although an oblique 5/564-inch Steinmann pin or multiple smaller K-wires may be used.![]() Figure 112.11.
Figure 112.11.
The osteotomy site is reduced by completely freeing the soft tissue
about the osteotomy, then pushing the proximal fragment medially with a
small Freer elevator while pushing the metatarsal head laterally. This
locks the lateral aspect of the osteotomy site, and the internal
fixation is inserted. A: Drawing shows the bones involved. B,C,D: Fixation of the osteotomy site using an oblique 5/64-inch Steinmann pin. E,F: Fixation of the osteotomy site using a 4.0 mm screw. -
When using the cannulated screw, place
the guide pin approximately 1 cm distal to the osteotomy site and at an
angle of about 45° to the long axis of the metatarsal before cutting
the osteotomy. -
After correction is obtained, drive the guide pin across the osteotomy site for fixation.
-
Make a 4 mm drill hole over the guide pin
because the self-tapping screw cannot cut through the cortical bone in
this area at a 45° angle. Countersink the hole along its distal aspect
to ensure that the head of the screw will not cam against the
metatarsal and fracture the island of bone between the osteotomy site
and the hole. Countersinking also lowers the profile of the screw. We
usually use a 4.0 mm screw of 26 mm length. In a large person, use a
28–30 mm screw. -
Plicate the medial joint capsule using
four to five sutures of 2-0 chromic. As the sutures are placed, an
assistant must hold the first metatarsophalangeal joint in neutral
position for dorsiflexion-plantarflexion and varus-valgus. The hallux
must be rotated to correct any pronation, which rotates the sesamoids
under the metatarsal head. Because the capsule on the plantar half of
the metatarsophalangeal joint is the strongest, be certain that the
suture line in this area is well secured. The alignment of the hallux
should now be anatomic.
walk in a postoperative shoe. The next day, rewrap the foot into a firm
dressing consisting of 2-inch Kling and half-inch adhesive tape. The
postoperative dressing is extremely important. The main principles are
to bind the metatarsal heads together to support the osteotomy site, to
derotate the hallux to ensure that any pronation deformity is
corrected, and to hold the toe in neutral alignment to correct any
residual valgus or varus. While standing at the patient’s foot, dress
the right hallux counterclockwise and the left hallux clockwise to
correct pronation, which maintains the sesamoid beneath the hallux (Fig. 112.12). Maintain dressing for 8 weeks and change it weekly. If a pin is used to fix the osteotomy site, remove it at 4 weeks.
 |
|
Figure 112.12.
The postoperative dressings are critical in maintaining proper alignment. Notice that the metatarsal heads are firmly bound with the gauze, and the great toe is rotated so as to keep the sesamoids aligned beneath the metatarsal head. This necessitates dressing the right toe in a counterclockwise direction and the left toe in a clockwise direction (from the point of view of someone standing at the foot of the bed). |
 |
|
Figure 112.13. Preoperative (A) and postoperative (B)
radiographs demonstrating satisfactory correction of a moderate hallux valgus deformity using a distal soft-tissue procedure and proximal osteotomy. Notice satisfactory realignment of the sesamoids and minimal shortening of the first metatarsal. Preoperative (C) and postoperative (D) radiographs demonstrating satisfactory correction of a severe hallux valgus deformity using the distal soft-tissue procedure and proximal crescentic osteotomy. |
in 14 cases and averaged 5.4°. Nine were less than 6°, which was of no
clinical significance, and five were greater than 6°. Of these, two
patients were dissatisfied with the result (7,16).
Bear in mind that when a severe deformity is corrected, some loss of
motion of the metatarsophalangeal joint may occur. If slight
undercorrection of the hallux valgus occurs, and this is bothersome to
the patient, an Akin procedure can be utilized in the future to
complete the correction of the deformity. If overcorrection occurs and
a hallux valgus deformity results, this may be corrected by an extensor
tendon transfer, as described by Johnson and Spiegel (12) and modified by Mann (13).
deformity depends on several factors. If there is symptomatic arthrosis
of the metatarsophalangeal joint, an arthrodesis is the procedure of
choice. If there is no arthrosis present, then one might consider a
soft-tissue reconstruction utilizing a split extensor hallucis longus
repair. The principle of the repair is that all soft-tissue contracture
along the medial aspect of the joint, which would include the joint
capsule, abductor hallucis tendon, and the displaced tibial sesamoid,
if present, needs to be sufficiently released to permit the proximal
phalanx to be rotated laterally on the metatarsal head. The proximal
phalanx is then stabilized in its normal position by transferring
either a portion of or the entire extensor hallucis longus tendon
beneath the transverse metatarsal ligament and suturing it into the
base of the proximal phalanx through a transverse drill hole. If an
interphalangeal joint contracture of more than 15° to 20° is present,
usually an arthrodesis of the interphalangeal joint is added to the
procedure.
satisfactory, although the patient does lose some motion at the
metatarsophalangeal joint. If the alignment of the joint is
satisfactory, however, the clinical problem of the hallux varus
deformity is usually solved.
the most popular procedure for repair of hallux valgus deformity, is
now used only in the patient who has limited ambulatory capacity, or
possibly as an alternative to an arthrodesis in the more sedentary
patient. The problem with the Keller procedure is that, in an active
individual, the stability of the first metatarsophalangeal joint is
lost and, as a result, a transfer lesion beneath the second metatarsal
head
often occurs. (Since the windlass mechanism of the first
metatarsophalangeal joint, which brings about plantar flexion of the
first metatarsal during the last half of stance phase, is disrupted,
weight is transferred to the second metatarsal head, often resulting in
a transfer lesion.) The great toe itself may drift into dorsiflexion,
varus or valgus, because of its lack of ability to stabilize itself due
to the excision of the proximal portion of the proximal phalanx.
management of foot problems, however. When utilized in the less active
individual, it can bring about adequate decompression of the
metatarsophalangeal joint and relieve pressure on the skin on the
medial side of the first metatarsal.
approach, exposing the medial joint capsule. This is dissected off the
metatarsal head, creating a distally based flap. The medial eminence is
removed, and the proximal 20% of the proximal phalanx is removed. The
metatarsophalangeal joint is then usually adequately decompressed, but,
if the joint still remains somewhat tight, excise a little bit more of
the proximal phalanx. If the deformity is severe, the adductor hallucis
insertion into the lateral sesamoid sling is released. Try to reattach
the sesamoid mechanism to the base of the proximal phalanx through
small drill holes; if this is not possible, however, at least suture
the sesamoid mechanism into the flexor hallucis longus tendon to help
prevent dorsiflexion at the metatarsophalangeal joint. A longitudinal
pin is then placed retrograde through the tip of the toe and back into
the metatarsal head, after which the medial capsule is sutured closed.
The pin is left in place for 3 weeks and the toe is kept dressed for
approximately 6 weeks. During the postoperative period, the patient is
permitted to ambulate in a postoperative shoe.
performed for arthrosis of the joint or a failed hallux valgus repair.
It is carried out routinely in the rheumatoid foot.
-
Make an incision over the dorsal aspect
of the first metatarsophalangeal joint. Dissect through subcutaneous
fat to expose the extensor hallucis longus tendon. -
Retract the tendon medially or laterally to expose the underlying joint.
-
Open the joint capsule and remove the osteophytes and the surrounding synovial tissue if present.
-
Remove the distal portion of the
metatarsal head and the base of the proximal phalanx with a sagittal
saw, keeping the bone resection to a minimum. Make the bony cuts to
produce 10° to 15° of valgus and about 30° of dorsiflexion in relation
to the first metatarsal shaft, or 10° to 15° of dorsiflexion in
relation to the plantar aspect of the foot (Fig. 112.14). If a medial eminence is present, remove it.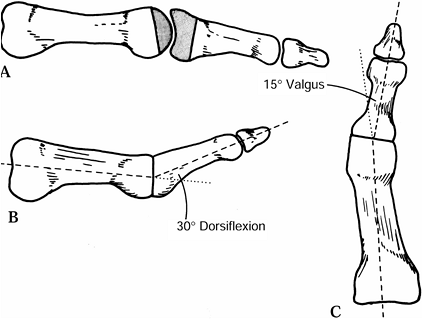 Figure 112.14. Arthrodesis of a metatarsophalangeal joint. A: Shaded area represents amount of bone surface usually removed when arthrodesis is carried out. B:
Figure 112.14. Arthrodesis of a metatarsophalangeal joint. A: Shaded area represents amount of bone surface usually removed when arthrodesis is carried out. B:
Lateral view of metatarsophalangeal joint demonstrating that the
arthrodesis site should be placed in about 30° of dorsiflexion in
relation to the metatarsal shaft. C:
Anteroposterior view of metatarsophalangeal joint demonstrating that
there should be about 15° of valgus at the arthrodesis site. -
I prefer to stabilize the fusion site
with an interfragmentary compression screw, and a five- or six-hole
quarter-tubular small fragment plate with 4.0-mm screws. After the bone
cuts are made, stabilize the arthrodesis in proper alignment with
0.045-inch K-wires. Place the interfragmentary screw from the medial
flare of the proximal phalanx obliquely into the metatarsal head.
P.3021
Usually
a six-hole plate can be applied to the dorsal surface if adequate
exposure is obtained; if not, use a five-hole plate. Although the plate
is placed on the compression side of the fusion site, it is usually
sufficient to neutralize the forces and permit fusion to occur. Secure
the plate with 4.0 mm cancellous or cortical screws, depending on the
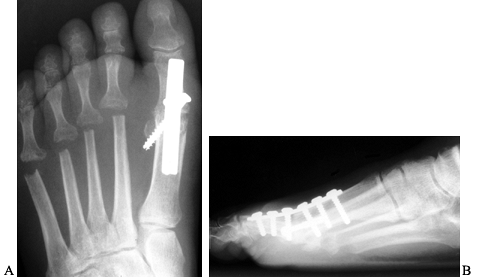
quality of the bone (Fig. 112.15).![]() Figure 112.15. AP (A) and lateral (B)
Figure 112.15. AP (A) and lateral (B)
radiographs demonstrating an arthrodesis of the first
metatarsophalangeal joint in a patient with rheumatoid arthritis. The
fusion site should be placed in approximately 15° of valgus, and at 10°
to 15° of dorsiflexion in relation to the ground.
postoperative shoe with weight bearing as tolerated. Remove the sutures
in 10–14 days. Use the postoperative shoe until fusion occurs, which
usually is by 10–12 weeks. The plate needs to be removed in only about
10% of patients.
an arthrodesis of the first metatarsophalangeal joint, patients are
quite functional (4,8).
Women can wear shoes with 1½-inch heels. Proper alignment of the joint
must be achieved, however; otherwise, abnormal stress may be placed
across the interphalangeal joint. Degenerative changes at the
interphalangeal joint may occur in about 20% of patients. As a general
rule, although radiographic changes occur in the interphalangeal joint,
they rarely become clinically symptomatic if the alignment of the first
metatarsophalangeal joint is correct. If insufficient valgus or too
much plantar flexion is placed at the arthrodesis site, the patient
tends to vault over the toe or externally rotate the foot to prevent
excessive pressure across the great toe. Occasionally, a nonunion of
the arthrodesis site occurs; if symptomatic, it should be repaired.
procedure, or in the case of severe rheumatoid arthritis with
osteopenic bone), use Steinmann pins to stabilize the fusion site (6). Use two threaded double-ended 3/32– or 1/8-inch
Steinmann pins. Drill each pin retrograde starting in the proximal
phalanx, crossing the interphalangeal joint, and passing out through
the tip of the great toe. Once the first pin has been drilled out
completely, place a second pin parallel to it. Hold the cut bone
surfaces in apposition and drill one Steinmann pin back across the
metatarsophalangeal joint. As this is being done, place compression
across the joint. The pin can usually be driven in 2–3 cm. Cut the pin,
leaving it protruding from the tip of the toe by about 4–5 mm.
Carefully check the toe for alignment and rotation by aligning the
toenails, and then drill the second pin across the metatarsophalangeal
joint (Fig. 112.16). Place the patient in a
compression dressing and permit walking in a postoperative shoe until
the arthrodesis heals, usually 10–12 weeks. Remove the pins under
digital block using a Craig pin remover.
 |
|
Figure 112.16. Preoperative and postoperative radiographs of first metatarsophalangeal joint arthrodesis. A: Severe recurrent hallux valgus deformity. B: Fixation with 1/8-inch threaded Steinmann pins. C: Postoperative result following satisfactory arthrodesis. D: Fixation of arthrodesis site using minifragment plate and interfragmentary screw.
|
correction of the deformity and a painless functional first
metatarsophalangeal joint. The surgical procedure must be carefully
selected; if one attempts to use a procedure such as a chevron when the
deformity is too severe, it will provide less than an optimal result.
It is extremely important to carefully select the indicated procedure
and not to “stretch’ indications (5).
integral part of the procedure if a satisfactory outcome is to be
achieved.
usually is not symptomatic. When the hallux varus is greater than 8° to
10°, it may be symptomatic and surgical correction utilizing a split
extensor hallicus longus transfer may be indicated.
the foot surgery. This prevents surprises for the patient, which makes
for a much better physician–patient relationship.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
TM, Dutkowsky JP, Graves SC, Richardson EG. An Anatomical Basis for the
Degree of Displacement of the Distal Chevron Osteotomy in the Treatment
of Hallux Valgus. Foot Ankle Int 1997;18:213.
ME, Kiebzak GM, Davis WH, Anderson RB. Prospective, Randomized
Comparison of Proximal Crescentic and Proximal Chevron Osteotomies to
Correct Hallux Valgus Deformity. Foot Ankle Int 1996;17: 307.
JE, Clanton TO, Baxter DE, et al. Comparison of Chevron Osteotomy and
Modified McBride Bunionectomy for Correction of Mild to Moderate Hallux
Valgus Deformity. Foot Ankle 1991;12:61.
RA, Rudicel S, Graves SC. Hallux Valgus Repair Utilizing a Distal Soft
Tissue Procedure and Proximal Metatarsal Osteotomy: A Long Term
Followup. J Bone Joint Surg Am 1992;74:124.
LA, Thompson FM. Proximal Metatarsal Osteotomy and Hallux Valgus
Correction: A Comparison of Crescentic and Chevron Procedures. Foot Ankle Int 1997;18:71.
DA, Zilberfarb JL, Greene MA, Colegrove RC. Avascular Necrosis of the
First Metatarsal Head: Incidence and Distal Osteotomy Combined with
Lateral Softtissue Release. Foot Ankle Int 1994;15:59.
DJ, Schlehr FJ, Murphey MD, Hamilton JJ. Distal Chevron Osteotomy with
Lateral Release for Treatment of Hallux Valgus Deformity. Foot Ankle Int 1994;15:457.
RL, Espinosa FJ, Richardson EG. Radiographic Changes in the First
Metatarsal Head after Distal Chevron Osteotomy Combined with Lateral
Release Through a Plantar Approach. Foot Ankle Int 1995;15(6):285.