ANKLE FRACTURES AND DISLOCATIONS INCLUDING PYLON FRACTURES
II – FRACTURES, DISLOCATIONS, NONUNIONS, AND MALUNIONS > Patella and
Tibia > CHAPTER 25 – ANKLE FRACTURES AND DISLOCATIONS INCLUDING
PYLON FRACTURES
treatment for displaced fractures and dislocations of the ankle has
been thoroughly demonstrated in the literature (14,22,32,33,37,38,39 and 40,43,47,53,56,60).
In this chapter, we devote little attention to closed methods of
treatment and discuss in detail modern internal fixation techniques.
See Chapter 10 for more detail on closed treatment.
tibia and the talus, the talus and the fibula, and the tibia and the
fibula, along with the capsule and stabilizing ligamentous structures,
and distal projections from the medial side of the tibia and from the
distal fibula, which form the malleoli. Together, these structures form
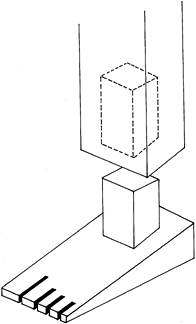
a geometric constraint to transverse movement of the talus (13,41,48,49 and 51,57). The ankle joint is commonly referred to as a mortise-and-tenon joint because of its appearance on the frontal radiograph (Fig. 25.1).
This carpentry term describes a technique in which wood is joined by
the insertion of a square peg into a square hole, thus offering great
rigidity and stability. This particular geometry is best suited to
resist rotation of the talus within the ankle mortise.
 |
|
Figure 25.1. carpenter’s mortise-and-tenon joint, showing the squared-off appearance of the ankle joint seen on the mortise view.
|
anteriorly than it is posteriorly and, depending on the shape of the
talus, requires a small amount of spreading of the malleoli during
dorsiflexion of the foot. In many ankles but not all, any loss of this
spreading motion can cause a loss of dorsiflexion. This shape of the
articular surface offers some restraint toward posterior subluxation of
the talus, but the greater restraint is the cup-shaped distal tibia,
which projects distally at its posterior margin.
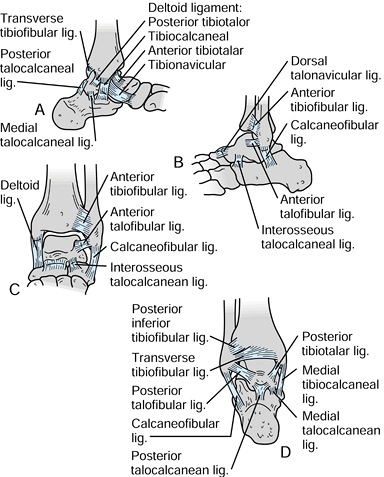
The medial ligamentous complex, called the deltoid ligament, consists
of a superficial and a deep portion. The superficial portion is large
and fan shaped and extends from the medial malleolus to a wide
attachment on the talus, calcaneus, and navicular (Fig. 25.2A).
The deep portion is a transverse ligamentous connection between the
deep surface of the medial malleolus and the talus. This ligament
inserts into the axis of rotation of the talus and is one constraint
against lateral subluxation of the talus. This portion of the ligament
is very short.
 |
|
Figure 25.2. A:
Ligamentous anatomy at the ankle, from the medial side. The fan-shaped deltoid ligament extends distally from the medial malleolus to the calcaneus, talus, and navicular. B: Lateral ligamentous anatomy, showing the anterior and posterior talofibular ligaments and the calcaneofibular ligament, extending distally and posteriorly. C: Anterior view of the ankle, showing primarily the anterior tibiofibular ligament. D: Posterior view showing the posterior tibiofibular ligament. |
helpful in preventing the tilting of the talus within the mortise. The
tibia and fibula articulate with each other distally and are held
together by a system of ligaments, including the interosseous membrane
and the anterior and posterior tibiofibular ligaments (Fig. 25.2C, Fig. 25.2D).
These ligaments allow the elastic widening of the ankle mortise during
dorsiflexion and, to a certain degree, rotation of the fibula.
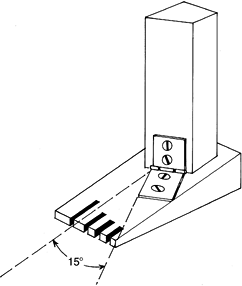
joint results in motion best described as a simple hinge whose axis is
parallel to the floor and externally rotated between 15° and 20° from
the frontal plane (Fig. 25.3). The range of movement averages 20° of dorsiflexion and 40° of plantar flexion.
 |
|
Figure 25.3.
The true axis of the ankle joint is externally rotated 15° from the axis of the foot. A radiograph through the axis of the foot will not give a true tangential view of the ankle joint. |
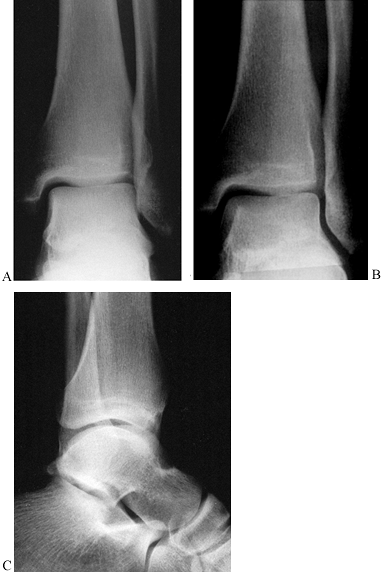
anteroposterior, lateral, and mortise views. The anteroposterior view
is taken with the beam centered on the ankle joint and directed in the
sagittal plane (Fig. 25.4A). The lateral view is taken with the beam centered on the ankle joint and directed in the frontal plane (Fig. 25.4B).
The mortise view is taken with the leg internally rotated about 15° so
the x-ray beam passes perpendicular to the axis of movement (Fig. 25.4C).
The anteroposterior view combined with the mortise view allows
detection of avulsion fractures of the malleoli, vertical fractures of
the medial malleolus, and lateral subluxation of the talus. The lateral
view is most helpful in outlining the configuration of the lateral
malleolar fracture and in detecting anterior and posterior tibial
fractures.
 |
|
Figure 25.4. A: A true anteroposterior view along the axis of the foot. B:
The true mortise view with the foot internally rotated 15° clearly shows the entire joint space extending from the tip of the medial malleolus to the tip of the lateral malleolus. C:The lateral view of the ankle joint, showing the fibula line posterior to the tibia. |
tibiofibular syndesmosis requires careful interpretation of the
radiographs, particularly for torsional injuries (Fig. 25.5).
Stress views, particularly under anesthesia, may be helpful. Marginal
impaction fractures, particularly in the anterolateral plafond of the
tibia, can often be seen on plain radiographs but may require tomograms
or CT scans. Full delineation of the various fracture fragments,
particularly those involving the articular surface in pylon fractures,
often requires CT with sagittal and frontal plane reconstructions.
Comparison views of the opposite side occasionally prove useful for
preoperative planning. Plain radiographs taken in traction are
particularly useful in pylon fractures, as the traction achieves a
rough reduction, restores length, and makes the fracture configuration
easier to understand (24).
 |
|
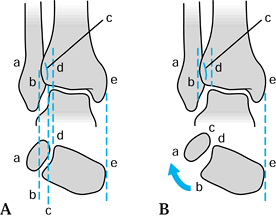
Figure 25.5. A: Anteroposterior projection of an ankle joint: a, lateral border of the lateral malleolus; b, lateral border of the anterior aspect of the tibia; c, medial border of the fibula; d, lateral border of the posterior aspect of the tibia. B: Rupture of the anterior syndesmosis with external rotation of the fibula does not affect the apparent width of the syndesmosis (c–d) or the intermalleolar distance (a–e). However, the amount of overlap of the anterior portion of the tibia on the fibula, distance a–b and distance b–c, change. Distance a–b increases, and b–c decreases. In most ankles, distance b–c is over 50% of a–c
on anteroposterior projections. Comparison radiographs of the normal ankle are very helpful. (Modified from Chapman MW. Fractures and Fracture-Dislocations of the Ankle (Chapter 34). In Mann RA, Coughlin MJ, eds. Surgery of the Foot and Ankle,6th edition. Philadelphia: Mosby, 1992:1448.) |
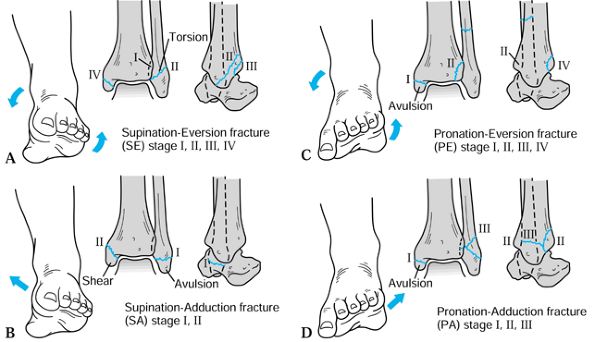
It divides ankle fractures into categories by mechanism of injury and
secondarily into groups of increasing severity. Lauge-Hansen determined
the mechanisms of injury in various fracture types by cadaveric
experiment in which he created these fractures in a laboratory setting.
He classified ankle fractures into four categories determined by the
position of the foot at the time force is applied (pronated or
supinated) and by the direction that force is applied (external
rotation or straight) (Fig. 25.6). An external
rotation force applied as the patient’s body twists over the planted
foot causes a supination–external rotation or pronation–external
rotation injury. Straight forces, such as when the supinated foot is
forced into further adduction, result in the injuries described as
supination–adduction. The opposite is the pronation–abduction injury.
Each of these four categories is subdivided into stages indicating
increasing severity of injury. The higher the stage, the greater is the
severity of the injury and, thus, the poorer the prognosis.
 |
|
Figure 25.6. The Lauge-Hansen classification of ankle fractures. A: The supination–eversion fracture. Stage I: The avulsion of the anterior talofibular ligament from the tibia or simple rupture of the ligament. Stage II:
The classic oblique fracture of the distal fibula, beginning anteriorly at the joint line and extending obliquely and posteriorly toward the shaft of the bone. Stage III: Avulsion or rupture of the posterior tibiofibular ligament. Stage IV: Avulsion fracture of the medial malleolus. B: The supination–adduction fracture. Stage I: Avulsion of the tip of the lateral malleolus or rupture of the associated ligaments. Stage II: Vertical fracture of the medial malleolus, usually beginning at the plafond. C: The pronation–eversion fracture. Stage I: Avulsion of the medial malleolus or ruptured deltoid ligament. Stage II: Rupture or avulsion of the anterior tibiofibular ligament. Stage III: A high, short, oblique fracture of the fibula. Stage IV: A posterior lip fracture of the tibia. D: The pronation–abduction fracture. Stage I: Avulsion of the medial malleolus or ruptured deltoid ligament. Stage II: Rupture or avulsion of the syndesmotic ligaments. Stage III: A short, oblique fracture of the distal fibula at about the level of the ankle joint. |
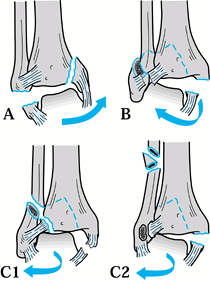
distal to the syndesmotic ligaments, and the medial malleolus is
fractured vertically (Fig. 25.7A). This
fracture type, which roughly corresponds to Lauge-Hansen’s
supination–adduction type, is usually unstable, requiring internal
fixation. There is often a small compression of the articular surface
of the tibia, which should be elevated for complete reduction of the
medial malleolus.
 |
|
Figure 25.7. The Weber classification of ankle fractures. A: Fracture of the fibula below the level of the tibial plafond and vertical fracture of the medial malleolus. B:
Avulsion fracture of the medial malleolus and fracture of the fibula, beginning at the level of the tibial plafond. The posterior rim may also be fractured, as shown. C: An avulsion fracture of the medial malleolus or ruptured deltoid ligament with a short oblique fracture of the fibula, well above the level of the tibial plafond. Also, a posterior rim fracture of the tibia may be seen. |
includes an oblique fracture of the fibula, beginning at the level of
the tibial plafond and extending proximally and posteriorly through the
fibular shaft. The posterior lip of the tibia is usually fractured; the
fragment may be large or small. Also included is an avulsion of the
medial malleolus or rupture of the deltoid ligament. This category
corresponds to the supination–external rotation type of Lauge-Hansen.
When undisplaced, according to criteria to be detailed below, these can
be treated by immobilization alone.
characterized by a fibular fracture that is entirely above the level of
the tibial plafond. A large or small posterior lip fracture often
accompanies this injury, as does a medial malleolar avulsion or deltoid
ligament rupture. This category corresponds to Lauge-Hansen’s
pronation–external rotation type. The syndesmosis is always ruptured;
the need for repair of this part of the injury is detailed later.
well known and widely used. The Lauge-Hansen classification is of
greater value in comparing the results of treatment because it
accurately describes the severity of the injury. The Weber
classification is more useful in deciding on the appropriate form of
treatment.
surface but also the metaphysis. On occasion, it extends into the
distal diaphysis as well. Most pylon fractures in urban trauma centers
result from higher-energy vertical compressive forces during a fall
from a height or a motor vehicle accident. Lower-energy injuries, often
incorporating a torsional component, may result from activities such as
snow or water skiing. The extent to which pure compressive loads are
responsible for the injury is related to the final outcome. High-energy
injuries not only produce greater comminution and compression of the
fracture fragments but also produce greater soft-tissue damage,
worsening the eventual outcome (54). (Note: The term pylon is from the French word “pilon” meaning to ram or hammer, referring to the mechanism of injury of this complex fracture.)
Foot dorsiflexion during impact produces anterior articular impaction
and comminution, whereas a plantarflexed foot is associated with
posterior articular damage. Loading a supinated or pronated foot
produces a characteristic pattern of articular damage, referred to in
the European literature as medial or lateral gap patterns, respectively.
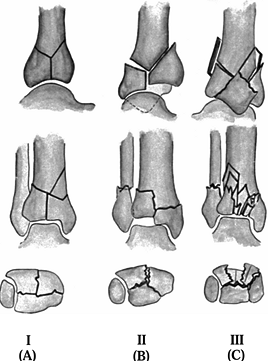
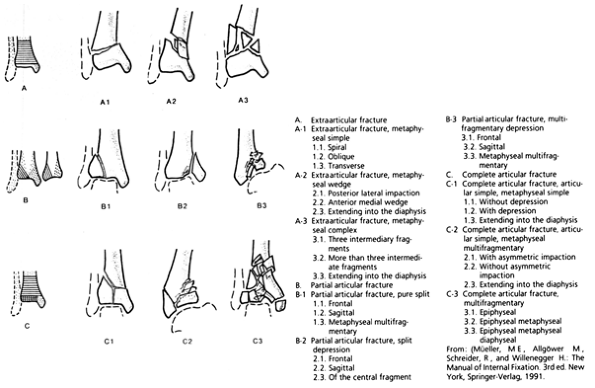
Type A fractures describe an intraarticular cleavage-type fracture
without joint displacement. Type B fractures demonstrate intraarticular
displacement with limited comminution. Type C fractures have
intraarticular displacement with marked comminution. The classification
has been further subdivided using the AO classification scheme (Fig. 25.9).
 |
|
Figure 25.8. Reudi and Allgöwer classification of pylon fractures.
|
 |
|
Figure 25.9. AO classification of pylon fractures.
|
the level before the insult. Restoring the original anatomy is the
single best means to restore normal function. For this reason, closed
treatment of ankle fractures is not recommended except when the initial
displacement is within acceptable limits. Closed reduction of displaced
ankle fractures is fraught with difficulty; it usually does not exactly
restore the anatomy, it is often a tedious exercise, and it may require
repeated reduction attempts to maintain the alignment within acceptable
limits (9,16,27,45,59).
Open treatment, on the other hand, offers the best possibility of
restoring the anatomy to its original condition without forced
manipulations or prolonged immobilization.
group offers the best chance of restoring the anatomy and maintaining
that restoration throughout healing (30). One
of the basic principles is the compression of fracture surfaces, one
against the other, which causes friction and eliminates motion between
the fractured parts (20). This compression
usually is obtained with lag screws or sometimes with compression
plates. One thing worse than inadequate closed reduction of ankle
fractures is a poorly performed internal fixation. These techniques are
exacting, and the surgeon must be attentive to detail to obtain a good
result.
articular surface of the ankle with displacement greater than 2 mm
lateral or posterior at the lateral or medial malleolus (18).
In the absence of a medial malleolar fracture, widening of the medial
clear space greater than 2 mm must be considered an unacceptable
displacement. Some surgeons would not accept widening of more than 1 mm
in young active individuals.
minimally comminuted fracture patterns with mild to moderate
soft-tissue injury. Lower-energy ankle fractures commonly occur in an
elderly population with osteopenic bone, so fixation may be
compromised. Although judicious soft-tissue handling and appropriate
surgical timing are still necessary to avoid wound breakdown and
infection, surgery usually can proceed immediately after presentation
to the emergency room and preparation of the patient for surgery (6).
collisions and falls from significant heights pose problems in the
management of the bony and soft-tissue injuries. Early closed reduction
of these fractures is important to minimize further soft-tissue
compromise and to decrease the risk of fracture blister formation.
Soft-tissue swelling, as well as abrasions and blisters, may make early
open reduction and fixation hazardous. Sometimes temporary external
fixation may be advisable, but usually incorporation in well-padded
long-leg splints or a cast with elevation of the limb suffices until
the soft tissues recover sufficiently to permit fixation.
antibiotics to the patient as soon as possible. Open ankle and pylon
fractures require immediate and thorough irrigation and debridement of
nonviable tissue (10) (see Chapter 12).
Whereas grade 1 injuries may be primarily closed following a thorough
debridement, grade 2 and grade 3 injuries usually require repeated
irrigation and
debridement
to minimize the risk of infection. Open injuries do not necessarily
dictate the type of fixation that should be used to stabilize a
fracture because both internal and external fixation principles can be
applied, assuming thorough debridement and early soft-tissue coverage
are performed. In severe open grade 3 pylon fractures, generally the
soft tissues will not tolerate extensive internal fixation of the
comminuted metaphyseal portion of the fracture. Most authorities treat
these with limited fixation of the articular surface and hybrid or
other external fixation (3,29). In some cases, conversion to biological internal fixation, once the soft tissues have recovered, is appropriate (3,48).
thorough neurovascular examination and evaluation for compartment
syndrome. If the patient has a history of vascular insufficiency or
clinical findings suggestive of distal arterial compromise, perform
noninvasive arterial Doppler studies preoperatively and consider
vascular consultation to insure that the wound will have the capability
of healing.
structures, including the proximal fibula, lateral and medial malleoli,
syndesmosis, and lateral and medial ligaments, to fully delineate all
aspects of the injury. Carefully palpate the hindfoot, midfoot, and
forefoot to rule out associated injuries.
fracture patterns without disruption of the ankle mortise do not
require operative treatment (59). The most
common fractures treated closed are Weber A and B fractures without
medial injury. All other displaced fractures about the ankle are
optimally treated with anatomic reduction, stable internal fixation,
and early range-of-motion exercise (15,26,60).
Failure to restore the anatomic relationships and articular congruity
of the ankle joint increases the risk of pain and loss of motion.
Noncongruent ankles can quickly progress to severe degenerative
arthritis.
conditions precluding safe operative intervention and vascular
insufficiency or other skin conditions preventing safe wound healing.
Patients with diabetes mellitus, particularly if they have peripheral
neuropathy, have a much higher-than-average occurrence of infection and
other serious complications.
dislocation, can lead to skin necrosis as a result of tension over bony
prominences as well as increased swelling and neurovascular compromise.
For that reason, markedly displaced ankles should have a provisional
reduction performed before radiography unless it will be performed
immediately.
reduced ankle injury in a well-padded cast that has been univalved or
in gutter splints, which will hold the provisional reduction. A
long-leg cast or splint is required for most ankle fractures. Those
that are rotationally stable can be immobilized in a short-leg device.
Elevate the limb 10 cm above the heart. Perform surgery as soon as
practical. Delay of surgery more than 24 hours may lead to excessive
swelling and fracture blisters, which may preclude surgery for a week
or more, and that delay could compromise the ability to achieve an
anatomic reduction.
equivalent as well as screws are available in the operating room, then
templating of routine ankle fractures is rarely necessary. Complex or
very long lateral malleolus fractures may require templating to ensure
that appropriate implants are available for fixation. Pylon fractures
require detailed radiographic assessment of the articular surface of
the tibial plafond and the fracture. For complex fractures, draw out
the fracture lines on a line drawing traced from plain radiographs of
the opposite normal side and use templates to sketch in the implants
you plan to use. If staged open treatment following fixation of the
fibula and external fixation is planned, radiographs following fibular
reduction and provisional tibial–calcaneal fixation are useful in
planning the definitive internal fixation.
with stable patterns and all nondisplaced fractures of the ankle are
suitable for nonoperative treatment. Usually a well-molded short-leg
cast suffices, and immediate weight bearing is possible. Univalve all
circumferential casts applied acutely and have patients elevate the
injured limb 10 cm above their heart until swelling subsides. Fracture
braces can be used for some stable lateral malleolus fractures (59).
exception of avulsion fractures of the nonarticular tip of the
malleolus, require open reduction and internal fixation (ORIF) because
they have a significant incidence of nonunion as a result of
soft-tissue interposition.
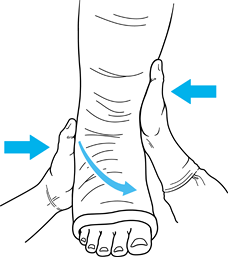
surgery, displaced fractures can be reduced, closed, and managed in
well-molded long-leg casts. Precise knowledge of the mechanism of
injury based on the Lauge-Hansen classification is necessary to provide
appropriate three-point molding of the cast (Fig. 25.10).
 |
|
Figure 25.10. Molding a cast.
|
-
Perform closed reduction as soon as possible.
-
Use a general or regional anesthetic.
-
Most fractures require a combination of
adduction, internal rotation, and varus forces and positioning to
achieve a satisfactory reduction. -
Apply a short-leg cast with three-point
molding and check the reduction on AP, lateral, and mortise
radiographs. Fluoroscopy alone is not adequate. Comparisons to the
opposite side may be necessary to assure reduction of the syndesmosis
if it is torn. -
If the reduction is adequate, extend the short-leg cast to a long-leg with the knee bent 10° to 15°.
-
Postreduction, prevent swelling and routinely univalve the cast.
-
Follow weekly with radiographs until you
are comfortable that the fracture is stable. One or more cast changes
may be necessary to maintain the reduction. The patient can usually be
transitioned to a short-leg walking cast by 6 to 8 weeks.
essential. Meticulous handling of the soft tissues cannot be
overemphasized. The surgeon’s obligation is to minimize additional
trauma to the ankle. Gentle reductions and careful technique are the
best means of obtaining satisfactory results.
-
Perform ORIF in a conventional operating room under general or regional anesthesia.
-
Give appropriate antibiotics
intraoperatively before the tourniquet is inflated, and continue them
for 24 hours (three total doses). -
Tourniquets are useful when bleeding
interferes with visualization of the reduction. Because of the rebound
edema that occurs after tourniquet use, we now prefer to use good
surgical hemostasis and operate without a tourniquet, if possible.
Avoid prolonged tourniquet time and under no circumstances exceed a
total of 2 hours. -
Generally, the supine position with a
bump under the ipsilateral hip to facilitate lateral exposures
suffices. The prone position is useful for some difficult trimalleolar
fractures requiring posterior-lateral exposure of the ankle. -
Gently prepare and drape the extremity
from the toes to the upper thigh. Use adhesive, povidone-impregnated
plastic drapes where incisions will be made. Expose no bare skin or
toes to the operative field.
Some additional advice is appropriate here, however. In general, skin
incisions should be longitudinal, straight, and located directly over
the fracture. The posterior ankle can be exposed through the medial or
lateral incisions by making them longer and shifting them somewhat
posteriorly. A gentle curve in their distal portion may be helpful, but
avoid creating flaps.
-
The utilitarian incision for a pylon
fracture is a straight anterior approach just lateral and parallel to
the anterior tibial tendon. If the fracture pattern allows, rather than
curve it medially distally, a straight incision carried well out onto
the neck of the talus facilitates complete exposure of the anterior
tibia and syndesmosis. -
Use a separate incision for the lateral
malleolus and a separate short incision directly over the tip of the
medial malleolus, if necessary, to insert malleolar screws (Fig. 25.11).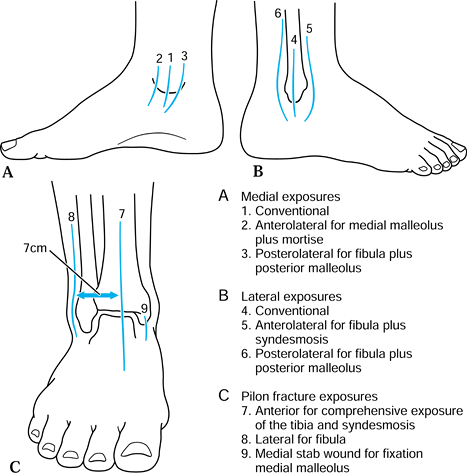 Figure 25.11. Surgical incisions around the ankle.
Figure 25.11. Surgical incisions around the ankle. -
Avoid injury to subcutaneous sensory nerves.
-
Carry dissection directly down to the periosteum. Expand exposure at the level of the periosteum.
-
Minimize stripping of the periosteum. Expose only a 1- to 2-mm edge along the fracture lines.
-
Thoroughly clean the fracture surfaces of hematoma.
-
Explore the ankle as possible through the
available surgical exposure and thoroughly irrigate to identify
chondral injury and osteochondral fractures, and remove any loose
fragments. -
In bimalleolar or trimalleolar fracture,
consider exposing all of the fractures before inserting any internal
fixation because this permits better inspection and irrigation of the
ankle as well as facilitating ORIF. -
Obtain anatomic reductions and render
them stable with one or more double sharp-pointed bone reduction
forceps of appropriate size. -
Use completely stable fixation.
-
Always obtain postoperative radiographs intraoperatively prior to wound closure.
-
Close wounds in three layers: the
periosteum if possible, subcutaneous tissue, and skin. Use atraumatic
skin closure technique. Use 1/8-in. suction drains in pylon fractures and severe trimalleolar fractures or when there is enough bleeding to justify their use. -
Apply a postoperative dressing and well-padded splints or a Robert-Jones dressing with splints (Fig. 25.12).
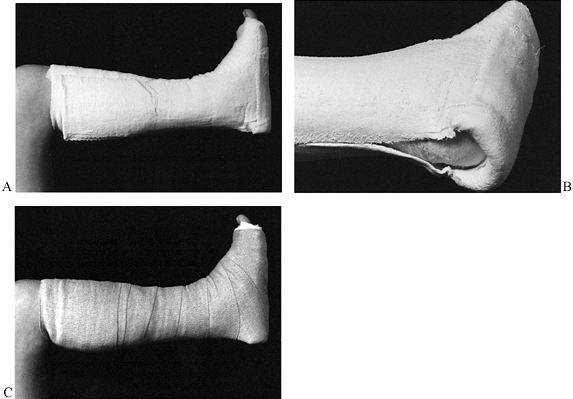
![]() Figure 25.12. The postoperative dressing. A:
Figure 25.12. The postoperative dressing. A:
The dressing is well padded with cotton before plaster application; a
foot plate is made of plaster splints, and a plaster stirrup on both
medial and lateral sides covers the foot plate. The foot plate is then
reversed over the stirrup for further strengthening. B: Close-up view showing the posterior aspect of the plaster. Plaster does not contact the patient’s heel. C:
A light coating of cotton is placed over the plaster to prevent the
compression dressing from sticking to the plaster and becoming
ineffective. Then it is wrapped with an elastic bandage. The foot is in
neutral position.
with a lateral injury and should be approached after the lateral
malleolus has been exposed. It is usually better to fix the lateral
side first.
-
Make an appropriate incision. Develop
exposure utilizing dull retractors (Ragnals, Langenbecks), taking care
to avoid damage to the saphenous nerve and vein. Strip the thick
periosteal layer overlying the medial malleolus only enough to allow
for visualization and reduction. It is imperative to visualize the
anterior aspect of the fracture to insure an anatomic reduction. -
Inspect the medial gutter of the ankle
joint to assess the talus for osteochondral injuries and to ensure that
no loose fragments or infolded soft tissue is blocking the reduction.
This is best accomplished by distracting the distal fragment with a
dental pick. -
After anatomically reducing the fragment
with a towel clip, sharp-tipped bone forceps, or dental pick,
provisionally hold the reduction with a large Weber (two-point
reduction) clamp (Fig. 25.13). Occasionally two small Weber forceps are required. Check for stepoffs between the fragments using a dental pick. Figure 25.13. Provisional reduction of medial malleolar fracture utilizing a large two-point reduction clamp.
Figure 25.13. Provisional reduction of medial malleolar fracture utilizing a large two-point reduction clamp. -
Screw fixation is usually optimal for
most medial malleolus fractures. Place two parallel screws in lag
fashion directed perpendicular to the fracture place. Screw diameter
(4.0 mm, 3.5 mm, 2.7 mm) can be varied to accommodate the size of the
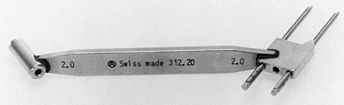
distal fragment. The sharp-tipped triple drill guide depicted in Fig. 25.14 is useful to provide preliminary fixation with drill points and to assure that the screws are parallel (Fig. 25.15).![]() Figure 25.14.
Figure 25.14.
This drill guide enables the operator to drill parallel holes to
facilitate parallel screw placement. One hole can be drilled, and the
drill bit left in place while the second drill bit is used to complete
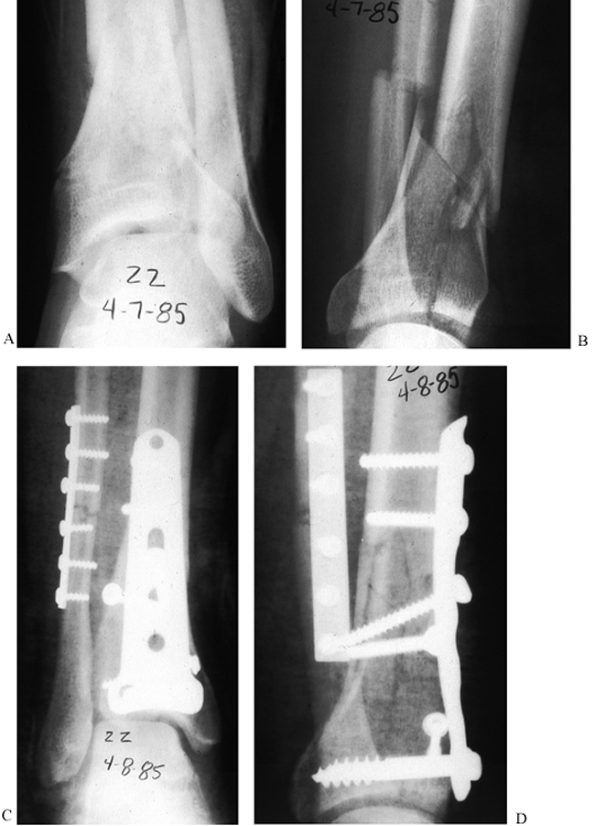
the procedure.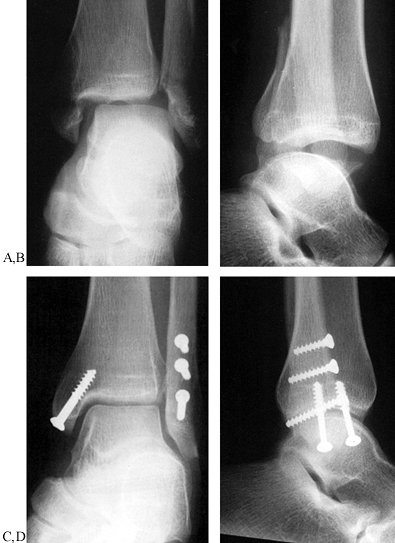 Figure 25.15. A,B: Preoperative view of an SEIV fracture type or Weber type B fracture. C,D: Postoperative radiographs showing the use of lag screws alone on the oblique fracture of the distal fibula.
Figure 25.15. A,B: Preoperative view of an SEIV fracture type or Weber type B fracture. C,D: Postoperative radiographs showing the use of lag screws alone on the oblique fracture of the distal fibula.
screw fixation alone may be suboptimal because the distal fragment
tends to displace proximally during screw tightening. In this instance,
place an antiglide plate first (an appropriately contoured quarter
tubular plate or one-third tubular plate), followed by the distally to
proximally directed lag screws. An alternative method is to be certain
that screws are at right angles to the fracture surface.
malleolus fractures are dependent on the fracture pattern and
mechanism. For most fractures about the ankle, reduce and fix the
lateral malleolus first, restoring length and rotational alignment.
-
Approach the majority of lateral malleolar fractures using incision 4 in Figure 25.11B.
If posterior fixation or concomitant posterior malleolar reduction is
anticipated based on preoperative planning, use incision 6, which is
posterior. -
Consider the anatomic variations of the sural and superficial nerves to avoid inadvertent injury.
are optimally treated with tension-band fixation because the fragment
is usually too small for screws and a plate. This can be accomplished
with Kirschner (K-) wires
and
malleable wire. Occasionally, a one-third tubular plate and screws work
well. An intramedullary screw can be used as well but provides less
rotational stability (Fig. 25.16).
 |
|
Figure 25.16. A: Preoperative anteroposterior radiograph of a supination-adduction type fracture or Weber type A. B,C: Postoperative radiographs illustrate the usex of an axial lag screw for the avulsion fracture of the distal fibula.
|
the level of the plafond can be stabilized with either a posterior
antiglide plate (Fig. 25.17) or a lateral interfragmentary lag screw and a buttress plate (Fig. 25.18). Even though antiglide plating shows some biomechanical advantage (46),
it should be reserved for short, oblique noncomminuted fracture
patterns. For antiglide plating, a one-third tubular plate is optimal.
 |
|
Figure 25.17. A:
Anteroposterior and lateral radiographs of a SER type lateral malleolar fracture. Notice the medial clear space widening consistent with medial ligamentous injury and dynamic instability. B: Postoperative radiographs demonstrating fixation with a posterior, antiglide technique. C: Radiographs 1 year postoperatively demonstrating osseous union and anatomic restoration of the ankle mortise. |
 |
|
Figure 25.18. A: Anteroposterior and lateral radiographs of a SER type bimalleolar fracture. B:
Postoperative radiographs demonstrating various fixation techniques including stacked one-third tubular plates, push-pull screw (empty screw hole proximal to plate), and 2.7-mm screws utilized to secure small medial malleolar fragment. |
-
Minimally strip the posterior soft tissue
extraperiosteally. Insert a 3.5-mm screw through the posterior
antiglide plate from posterior to anterior just proximal to the
fracture line. As the screw is tightened, the plate will reduce the
fracture. -
Fine-tune the reduction with small Weber clamps until an anatomic reduction is achieved.
-
With the fracture held anatomically
reduced, place a 3.5-mm or 2.7-mm distal-posterior to proximal-anterior
lag screw though the plate across the fracture. The 2.7-mm screw head
is less prominent for the peroneal tendons and can be angled
perpendicular to the fracture line. -
Place a 3.5-mm bicortical screw through the plate proximally to serve as a derotation screw (4) (Fig. 25.17).
tubular plate, stacked one-third tubular plates, or 2.7-mm
reconstruction plates provide satisfactory fixation.
-
Mallet a one-third tubular plate flat
distally and contour and rotate it to match the contours of the distal
fibula. In cases where distal fixation is problematic, a hook can be
fashioned out of the distal screw hole and impacted into the bone as an
additional point of fixation (26). Do this by
cutting the distal end of the plate off through the screw hole and then
bending the resulting sharp ends toward the bone. -
Rather than placing a short unicortical
4.0-mm cancellous screw in the distal holes, 2.7- or 3.5-mm cortical
screws can be angled proximally or distally to obtain additional
cortical purchase and still avoid penetrating the articular surface in
the lateral gutter. -
Two proximal bicortical screws and an anterior-to-posterior interfragmentary screw complete the fixation (Fig. 25.18). Additional screw fixation proximal to the fracture is rarely necessary and results in unbalanced fixation.
on in a delayed manner, indirect reduction techniques are helpful in
gaining the appropriate length and rotation.
-
After anatomic length has been achieved, correct rotational discrepancies before placing proximal screws.
length and rotational deformities of the distal fragment of the fibula
as well as anatomic reduction and fixation of the syndesmosis (1).
In a few of these injuries the anterior and interosseous ligaments of
the syndesmosis are torn, but the posterior ligaments remain intact.
Anatomic reduction and plate fixation of the fibula alone then restores
the syndesmosis and renders it stable. Independent fixation of the
syndesmosis then is unnecessary. Indirect reduction techniques are
ideal for restoring appropriate length. Single one-third tubular plates
are usually not strong enough to allow for distraction through the
plate. Stacked one-third tubular or 3.5-mm dynamic compression plates
(DCP) function well for this task. These plates require precise
contouring, as they are too stiff to assume the contour of the lateral
fibula when the screws are tightened.
-
Following a lateral approach to the
distal fibula, dissect along the anterior fibula to expose the anterior
syndesmosis. Careful preoperative and intraoperative planning is
required for precise placement of a screw from lateral to medial across
the syndesmosis parallel to and 2 to 3 cm above the joint line. -
After fixing the plate to the distal fragment along the posterolateral aspect of the fibula, place a push-pull
P.825P.826P.827P.828
screw proximal to the plate. Distract through the plate until anatomic
length, rotation, coronal plane alignment, and anatomic reduction of
the syndesmosis have been accomplished. If there is cortical continuity
between the distal and proximal fragments, the fracture can be loaded
through the plate using the push-pull screw and a small Verbrugge clamp
(24). -
Secure the plate proximally with two 3.5-mm bicortical screws.
-
Then fix the syndesmosis.
-
Position the hindfoot in slight inversion
and the ankle in neutral dorsiflexion and hold the syndesmosis reduced
with a two-point reduction forceps. The screw should parallel the joint
and be directed from posterolateral to anteromedial at approximately a
15° angle (Fig. 25.19).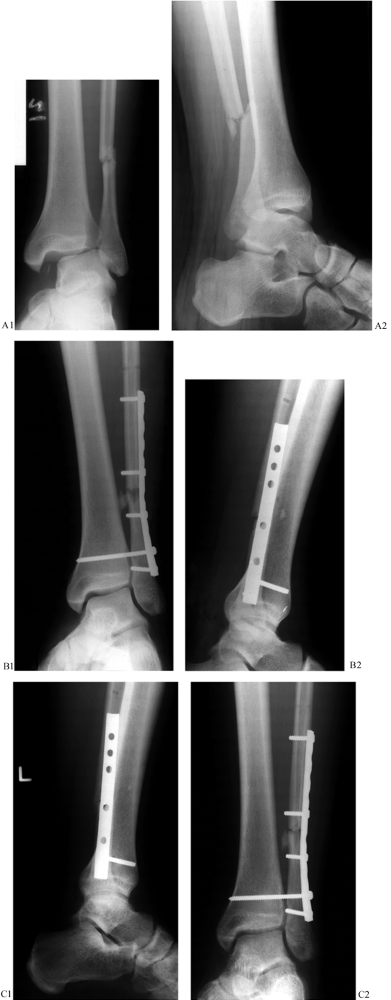 Figure 25.19. A:
Figure 25.19. A:
Radiographs demonstrating a pronation type ankle fracture with
syndesmotic disruption. Notice the avulsion fracture at the medial
joint line. B: Radiographs following ORIF of the fibula and open reduction of the syndesmosis with transsyndesmotic fixation. C: Radiographs following union of the fracture. Radiolucency around the syndesmotic screw without failure is evident. -
Use a fully threaded 3.5-mm cortical
screw across all four cortices of the fibula and tibia to secure
fixation. In larger individuals, two 3.5-mm screws may be necessary.
The fully threaded screw functions as a “position” screw by holding the
reduced position, avoiding excessive compression of the syndesmosis.
Fractures can involve only the nonarticular portion of the posterior
malleolus, and fragments that are attached to the fibula by the
posterior distal tibiofibular ligaments are well reduced and stable
after fixation of the fibula. If the fracture involves 25% or more of
the articular surface, the talus tends to subluxate posteriorly,
so fixation is indicated (8,31).
Because the fracture can be oblique, there is a tendency to
underestimate the size of the fragment. Computed tomography (CT) is
useful in delineating the size and location of the fragment.
-
Posteromedial fragments can usually be fixed through incision 3 on Figure 25.11A,
which is used to fix the medial malleolus as well. Lengthen it as
needed to gain adequate exposure. Posterolateral fragments can be
approached in a similar way laterally through incision 6 on Figure 25.11B.
Use the interval between the peroneal tendons and the flexor hallicus
tendon. This incision must be large enough to permit tension-free
exposure. The prone position is very helpful for this exposure and
fixation. -
Use a dental tool, large Weber
double-pointed forceps, or spiked ball-tip pusher to reduce the
fragment. Lock the proximal edge of the fractured fragment into place
first and then close the articular surface. Hold it securely with the
reduction forceps. -
After provisional K-wire fixation, obtain
definitive fixation with percutaneous anterior-to-posterior 3.5-mm or
2.7-mm lag screws placed through anterior stab wounds. Do not
overtighten the screws because this may cause the posterior fragment to
displace proximally and anteriorly (Fig. 25.20).![]() Figure 25.20.
Figure 25.20.
A 28-year-old woman was involved in a high speed motor vehicle accident
sustaining multiple injuries including this comminuted intraarticular
pylon fracture of the left ankle. A: AP radiograph. B: Lateral radiograph, note the large posterior fragment. C:
AP radiograph following open reduction and internal fixation through an
anterior approach for the tibia with application of a spoon plate.
Today we would prefer the use of a smaller combination of plates. D:
A lateral view showing management of the larger posterior malleolar
fragment with anterior to posterior lag screw fixation accomplished
through the anterior approach using a sharp-tipped tenaculum forceps to
reduce the articular fragment by percutaneous means avoiding direct
exposure of the posterior fragment.
-
Expose the syndesmosis anteriorly as previously described.
-
Before reducing the distal tibial–fibular
joint, confirm that the distal anterior tibial–fibular ligaments have
not “buttonholed” into the joint, blocking the reduction. Clean out the
syndesmosis but do not disturb the articular cartilage or curette the
bone in order to prevent a synostosis from forming. -
Reduce the syndesmosis using a large
pointed reduction forceps. Be certain that the fibula slides
posteriorly into the sulcus in the tibia and is anatomic. -
Proceed with screw placement as described for Weber C fractures (8). A two-hole one-third tubular plate on the fibula may be used as well, particularly if two screws are placed (Fig. 25.21).
 Figure 25.21. A: Radiographs following pronation injury resulting in a medial ligamentous injury with syndesmotic disruption.B: Stress radiograph demonstrating syndesmotic disruption with comparative stress view of the uninjured ankle. C: Intraoperative radiograph with compression across the reduced syndesmosis. D: Radiographs following open reduction of the syndesmosis and internal transsyndesmotic fixation. E:
Figure 25.21. A: Radiographs following pronation injury resulting in a medial ligamentous injury with syndesmotic disruption.B: Stress radiograph demonstrating syndesmotic disruption with comparative stress view of the uninjured ankle. C: Intraoperative radiograph with compression across the reduced syndesmosis. D: Radiographs following open reduction of the syndesmosis and internal transsyndesmotic fixation. E:
Follow-up radiographs demonstrating maintenance of the syndesmotic
reduction and development of (asymptomatic) intramembranous
calcification. -
Repair of the anterior distal
tibia–fibula ligaments can be performed with a nonabsorbable suture,
although this is less important than anatomic reduction with stable
screw placement. -
Repair of a concomitant rupture of the
deltoid ligament is unnecessary. If the medial side is explored for
other reasons, repair the ligament.
-
Use the lateral incision for lateral
malleolar fixation to reduce and stabilize the tubercle of Chaput.
Dissect anteriorly with a periosteal elevator along the anterior
tibial–fibular ligament to provide access to the tubercle of Chaput. -
Use a dental pick, spiked pusher, or Weber clamp for reduction.
-
Provisionally stabilize the fracture with K-wires and then place a lag screw from lateral to medial, securing the fragment.
anatomic reduction rarely require repair. Deltoid ligament tears in
combination with lateral malleolar fractures do not require open
treatment unless they prevent an anatomic reduction of the ankle
mortise (12).
joint surface maintained by stable internal fixation. If this can be
achieved, functional postoperative treatment with early use of the
muscles of the leg and physiologic activity of the joint can be
instituted (34,35). Early use of the muscles prevents atrophy, and motion helps to repair injured cartilage (44).
The fixation maintains the fracture in the correct position through the
period of bone healing. Operatively achieved anatomic reduction and
stable internal fixation can produce results impossible to achieve with
other therapeutic approaches (2).
injury. This window for intervention extends to about 10 to 12 hours
after injury. If more time passes, interstitial edema increases, the
skin loses its pliability, and fracture blisters appear. During this
later period, surgery is contraindicated.
compression dressing, and elevation of the extremity may salvage the
situation if it is too late to operate. Proper management during this
period enables operative intervention when the skin starts to wrinkle,
at about 8 to 10 days.
unstable for emergent surgery into calcaneal pin traction on a Boehler
frame and allow the traction to regain length and alignment of the
limb. Elevation, reduction, and time allow the posttraumatic
inflammatory period to pass. An idea of the relative ease of open
reduction and internal fixation may be obtained by viewing radiographs
of the reduction obtained by pure distraction during the traction
period (23,24) (Fig. 25.22).
 |
|
Figure 25.22. A:
Anteroposterior (AP) radiograph of a type C pylon fracture. Notice the shortening that contributes to displacement of the diaphyseal and articular fracture fragments. B: An AP radiograph of the same fracture with 10 kg (22 lb) of skeletal traction applied through the calcaneus. Notice how simple distraction has reduced most of the diaphyseal and epiphyseal fracture displacements. This is a good prognostic sign, indicating that indirect methods of reduction during surgery can allow an atraumatic reduction of the fracture, which then may be fixed by standard methods of internal fixation. C: Another AP projection of a type C pylon fracture. Although this fracture is more comminuted than the previous example, a more important indicator of problems in reduction during surgery is shown by its failure to reduce or improve with skeletal traction. D: Ten kilograms (22 lb) of traction applied to the calcaneal pin have not markedly improved the radiographic situation. Failure to improve during skeletal traction can be attributed to the interposition of soft tissue. In this fracture, the flexor hallucis and neuromuscular bundle have been displaced into the joint and block reduction of the posterior fragment. |
have subsided. This does not represent the ideal situation, however.
Surgical intervention is rendered more difficult by the passage of time
because the soft tissues are less pliable and the bony fragments become
softer and somewhat adherent.
in determining the final outcome. In high-energy injuries, impaction of
the subchondral bone, fragmentation of the epimetaphyseal cortex, and
irreparable abrasion of the cartilage of tibia and talus may dictate a
poor result regardless of the surgeon’s experience. Under these
circumstances, the condition of the soft-tissue sleeve becomes critical.
approach and surgical tactic for the reduction and fixation must be
carefully planned. In these fractures, a preoperative drawing may be
very enlightening. If the key fragments to be reduced and fixed cannot
be identified and drawn, it may be that at surgery they cannot be
reduced and fixed (48). A misguided attempt at
anatomic reduction and internal fixation under circumstances in which
stable fixation cannot be achieved can deteriorate into a lengthy
struggle, resulting in frustration for the surgeon, intraoperative
acceptance of malreduction, unstable fixation and ensuing skin slough,
wound dehiscence, bone and tendon necrosis, and infection. Worse, the
patient may be deprived of delayed reconstructive procedures that could
produce an acceptable result.
enacting a reduction, pylon fractures, like all articular fractures,
should be reduced directly. Regardless of which operative approach to
pylon fractures is employed, distraction techniques are required to
restore alignment and reduce compressed articular fragments.
technique should be reserved for undisplaced or anatomically reducible
articular fracture patterns without metadiaphyseal extension that are
potentially unstable and require additional stabilization. Isolated
percutaneous screw fixation of periarticular fragments rarely provides
sufficient stability to allow for early range of motion and likely
necessitates
cast immobilization to provide stability. This technique is best combined with external fixation, which is described below.
Reduction via external fixation relies on traction and resulting
ligamentotaxis to help reduce the fracture fragments. Without direct
visualization of the articular surface via open or arthroscopic means,
treatment by external fixation relies on radiographic joint reduction,
which is subject to errors. Although some small wire hybrid techniques
do not cross the ankle joint, most large pin fixators rely on fixation
that spans the ankle and often the subtalar joints, precluding early
joint motion. If external fixation is used as a temporary treatment
regimen while soft tissue swelling is allowed to subside, ensure that
pin placement does not compromise future open treatment. Specific
surgical techniques vary, depending on the type of external fixation
employed. Correction of angular, rotational, and length discrepancies
is accomplished by distracting through the fixator after connecting the
fixator to proximal and distal pins and/or wires. Regardless of the
fixator, it is essential that pins and wires be placed without causing
thermal necrosis to the bone and soft tissue, which leads to infection
and ring sequestrum formation (see Chapter 11 for more details).
stabilize the articular fractures followed by “connecting” the restored
joint to the tibial shaft with external fixation. Indirect reduction
techniques aid in repositioning of fragments via ligamentotaxis (48).
-
Before attempting reduction of the
articular fracture fragments, connect a universal distactor to tibial
and talar or calcaneal Schanz screws and correct for length and
rotational and angular malalignments. Alternatively, some fixation
systems allow for distraction through the fixator. -
Utilize limited well-planned incisions
and stab wounds near the plafond to reduce fracture fragments under
fluoroscopic radiographic control. Small elevators, dental picks,
pushers, and K-wires are helpful in positioning fragments in a reduced
position. -
After obtaining anatomic reduction and
provisional stabilization with K-wires or guide wires for cannulated
screws, secure the articular and periarticular fragments with
interfragmentary screws. -
Following reduction and stabilization of
the articular fragments, use the external fixator to secure the ankle
and distal tibia to the tibial diaphysis.
are available. Small-wire or hybrid fixator fixation that provides
stable fixation without spanning the tibial–talar or talocalcaneal
joints is preferable when technically feasible because it allows for
early ankle (and subtalar) motion, satisfying one of the goals of
operative pylon treatment (Fig. 25.23).
 |
|
Figure 25.23. Radiograph of a pylon fracture in a hybrid or Orthofix fixator with percutaneous screws. A,B: AP and lateral radiographs demonstrating an AO C type pylon fracture with marked metadiaphyseal comminution. C,D:
Radiographs with a tibial-calcaneal spanning external fixator, reducing the fracture via ligamente taxis with limited internal fixation of the major articular fragments. |
Poor soft-tissue handling, inappropriate surgical timing, excessive
soft-tissue stripping, and use of excessively large implants, however,
can lead to disastrous results.
injury principles. The safest time periods for open treatment are
within 6 hours of the injury or at least 6 days from the injury (34).
Staging of open treatment takes advantage of both these “windows of
opportunity,” provisionally stabilizing the fracture to aid in
soft-tissue healing and allowing for careful radiographic evaluation
and preoperative planning.
fracture presents to the trauma center, preferably within 6 hours from
time of injury, perform ORIF of the fibula and provisional
tibial–calcaneal external fixation.
-
Carefully plan the fibular incision to
allow for a 7-cm skin bridge between this and the future anterior
tibial incision. Approach the distal fibula fracture essentially the
same as for routine lateral malleolar fractures. Direct the incision
slightly posteriorly to insure a safe skin bridge. Fibula fractures
associated with pylon fractures typically occur proximal to the ankle
mortise, but varying patterns may occur. -
Shortened fibulas from lateral
compression modes of failure reduce well with indirect means. Following
fixation to the distal fragment, place a 3.5-mm bicortical push-pull
screw proximal to the plate. After distracting the fracture out to
anatomic length with a bone spreader and correcting rotational
malalignments, secure the plate to the proximal fragment. If cortical
continuity exists, the fracture can be loaded using the push-pull screw. -
Place a 5.0-mm Schanz screw in the medial
aspect of the tibia and calcaneus perpendicular to the ankle joint
using standard techniques. Make sure the tibial pin is far enough
proximal to avoid communication with the future tibial incision. -
Connect the pins to a single medial carbon fiber bar and distract the distal tibia out to length using the
P.838P.839
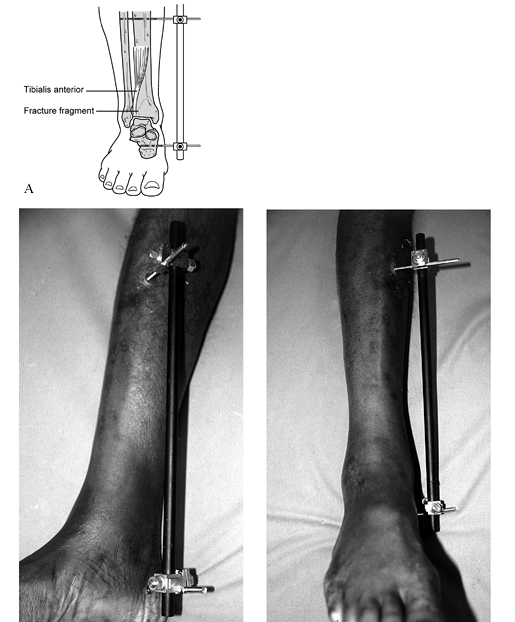
compression device (Fig. 25.24).
Do not place any pins into the talus because this may compromise any
incision required for definitive open treatment in the future.![]() Figure 25.24. A: Appropriate provisional external fixator placement following first stage of open treatment of a pylon fracture. B: Photographs following ORIF of the fibula fracture and application of a tibial–calcaneal fixator.
Figure 25.24. A: Appropriate provisional external fixator placement following first stage of open treatment of a pylon fracture. B: Photographs following ORIF of the fibula fracture and application of a tibial–calcaneal fixator.
soft-tissue swelling diminishes. This usually occurs within 7 to 10
days but may take up to 3 weeks.
-
Make an anterior tibial incision (Fig. 25.11C),
leaving a 7-cm skin bridge between it and the fibular incision. This
will vary somewhat based on the fracture pattern. The standard incision
starts just lateral to the crest of the tibia and courses just anterior
to the tibialis anterior tendon at the distal limb (34).
A posterior (European) approach may occasionally be preferable to
accommodate open fracture wounds, but this approach provides limited
exposure of the articular surface. -
Dissect directly down to bone just
lateral to the anterior tibial tendon and develop the exposure medially
and laterally at the level of periosteum. Incise the anterior
compartment fascia just lateral to the tibial crest and reflect the
flap medially in an extraperiosteal manner, exposing the medial face of
the tibia. Avoid violating the paratenon of the anterior tibial tendon
at the distal aspect of the incision. Should the skin slough
anteriorly, the paratenon will accept a split-thickness skin graft. In
the absence of the paratenon, the tendon will desiccate, leading to
infection and other problems. -
Make an anterior ankle arthrotomy and
carry the exposure out onto the neck of the talus to visualize the
reduction. Perform minimal periosteal stripping of the fracture
fragments. -
Additional distraction through the medial fixator may aid in the reduction (23).
-
Use a variety of dental picks, reduction
forceps, and pushers to tease the fragments into anatomic alignment.
Forceful reduction maneuvers are rarely beneficial and increase the
risk of further fracture fragmentation. Thoughtful, methodic,
fragment-by-fragment reduction and provisional fixation are essential. -
After reducing the fragments, perform
provisional fixation with K-wires. If significant crush of metaphyseal
bone exists, place autologous bone graft into the osseous defect to
prevent collapse of the reduction and promote osseous union. -
After confirming an anatomic articular
reduction visually and radiographically, replace the provisional
K-wires with limited lag screw fixation. -
Various small and minifragment plates may
additionally be contoured to adequately stabilize the periarticular
fracture fragments and stabilize the metaphyseal component to the
distal diaphysis of the tibia (Fig. 25.25). It is
P.841P.842P.843
rare that a plate larger than 3.5-mm limited-contact DC plates is required. Figure 25.25. A: Anteroposterior radiographs of a C-type tibial pylon fracture. B:
Figure 25.25. A: Anteroposterior radiographs of a C-type tibial pylon fracture. B:
Radiographs following ORIF of the lateral malleolar component and
application of a provisional tibial–calcaneal external fixator. C: Clinical photo before second stage of surgery. D: Anteroposterior radiographs following ORIF of tibial plafond and autogenous bone grafting of the metaphyseal defect. E: Weight-bearing radiographs following osseous union. F:
Weight-bearing radiographs following hardware removal, demonstrating
articular congruity and maintenance of tibial–talar joint space.
close all deep tissues over the bone and implants, leaving the fibular
incision open, allowing for primary closure of the tibial wound with
delayed closure or split-thickness skin grafting of the fibular
incision. Delayed closures under sterile conditions are far safer than
attempting to primarily close an overly tight wound.
a well-padded compression dressing and splints to prevent the foot from
dropping into equinus. Elevate the limb until swelling subsides. Gentle
range-of-motion exercises can begin as tolerated if the surgeon feels
the fixation is stable. On the first postoperative office visit, apply
a removable below-knee cast. Keep patients touch-down weight bearing
but remove the cast or brace daily to perform active, active-assisted,
and gentle passive ankle and subtalar range-of-motion exercises.
Patients with persistent swelling despite stable internal fixation and
an anatomically reduced fracture often benefit from a knee-high medium
compression stocking. Based on the fracture pattern, continue limited
weight bearing for at least 6 weeks. Most fractures require limited
weight bearing and protection for 12 weeks.
anatomic reductions and failure to adequately stabilize the fracture.
Articular incongruity and inability to restore the anatomic
relationships of the ankle mortise increase the probability of
postoperative pain and early posttraumatic arthrosis (52).
Failure to achieve stable fixation allowing for early range of motion
leads to “fracture disease” and chondrolysis. Malreductions that have
yet to result in significant levels of joint destruction are amenable
to restorative osteotomies (55). Advanced ankle
joint destruction often requires arthrodesis as a salvage procedure.
Early total ankle arthroplasty results from newer generation ankle
prostheses are an encouraging alternative to joint fusion.
operative treatment of ankle and pylon fractures present a difficult
challenge to the orthopaedic surgeon. Frequently, these postoperative
complications stem from decisions made before and during operative
treatment. Proper surgical timing, avoidance of undue soft-tissue and
osseous devascularization, utilizing appropriate-sized implants, and
adhering to principles of treatment of open fractures prevent the
majority of these potentially disastrous complications. Even though
operative treatment utilizing external fixation is usually considered
safer than open techniques, complications can result from either
treatment protocol. Superficial wound infections and breakdowns may be
amenable to local wound care and oral antibiotics. Deep infection and
full-thickness wound sloughs must be treated with aggressive
debridements of devitalized tissue, full-thickness soft-tissue
coverage, and intravenous antibiotics. Salvage following these grave
complications may require extraordinary techniques such as free tissue
transfer or bone transport procedures in order to achieve osseous union
and restore limb length and function. Failure to eradicate deep
infection or achieve union may necessitate a below-knee amputation.
is frequently underestimated, leading to pitfalls in treatment.
Although various surgical modalities (internal fixation, external
fixation) may be employed in the operative treatment of ankle
fractures, ideal surgical treatment should produce anatomic restoration
of the articular congruity of the tibial plafond and restoration of the
ankle mortise with sufficient stability to allow for early joint
motion. Each surgeon will choose different treatment modalities in
order to accomplish these goals. We routinely treat ankle and pylon
fractures by open reduction and internal fixation. By protecting the
soft tissues, operating during safe periods, preserving the osseous
vascular supply, and utilizing appropriately sized implants, we have
been able to avoid the majority of complications associated with ORIF.
Other, less-invasive techniques may potentially minimize the risk of
morbidity, but they often preclude anatomic restoration of the
articular surface and prevent early restoration of ankle and subtalar
motion.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
I, Salama R, Goodwin DRA, Weissman SL. An Evaluation of Surgical and
Conservative Treatment of Fractures of the Ankle in 200 Patients. J Trauma 1978;18:271.
J, Greiff J, Riegels-Nielsen P. Malleolar Fractures Treated with Rigid
Internal Fixation and Immediate Mobilization. Injury 1981;13:191.
JW, Teipner WA. A Reproducible Approach to the Internal Fixation of
Adult Ankle Fractures: Rational, Technique and Early Results. Orthop Clin North Am 1980;11:6.
RP, Batten RL. External Rotation and Abduction Fractures Around the
Ankle Joint Treated by Internal Fixing Using AO Instrumentation. Injury 1979;11:33.
FA, Mitchell G, Pee D, et al. Quantitative Criteria for Prediction of
the Results after Displaced Fracture of the Ankle. J Bone Joint Surg 1983;65-A:667.
RB, Simmonds DF, Malcomb BW, et al. The Biological Effect of Continuous
Passive Motion on the Healing of Full-Thickness Defects of Articular
Cartilage: An Experimental Investigation in the Rabbit. J Bone Joint Surg 1980;62-A:1232.
D, Pick RY, Klein HA, Heskiaoff D. The Role of the Lateral Malleolus as
a Stabilizing Factor of the Ankle Joint: Preliminary Report. Foot Ankle 1981;2:25.
SM, Wiss DA. Open Reduction and Internal Fixation of Tibial Plafond
Fractures. Variables Contributing to Poor Results and Complications. Clin Orthop 1993;282:108.
J, Kristensen KD. Ankle Fractures. Supination–Eversion Fractures of
Stage II. Primary and Late Results of Operative and Non-Operative
Treatment. Acta Orthop Scand 1980;51:695.
J, Kristensen KD. Ankle Fractures. Supination-Eversion Fractures of
Stage IV. Primary and Late Results of Operative and Non-Operative
Treatment. Acta Orthop Scand 1980;51:981.