The Deep Tendon or Muscle Stretch Reflexes
passively stretched, its fibers resist the stretch by contracting.
Reflexes elicited by application of a stretch stimulus to either
tendons or periosteum, or occasionally to bones, joints, fascia, or
aponeurotic structures are usually referred to as muscle stretch or
deep tendon reflexes. The reflex is caused by sudden muscle stretch,
brought about by percussion of its tendon. Occasionally, the tendon is
stretched by percussing a structure to which it is attached, as in the
jaw jerk. Because of their critical roles in maintaining an erect
posture, the extensor muscles of the legs, quadriceps and calf muscles,
have better developed stretch reflexes than the flexors.
superficial or cutaneous reflexes, which are quite different. The term
deep tendon reflex (DTR) was introduced in 1875, and since at least
1885 some authorities have criticized it. The term DTR is in much wider
use than muscle stretch reflex, and for both pragmatic and
anti-pedantic reasons, the DTR abbreviation will be used in this text.
tools and poor technique. These reflexes are best tested using a
high-quality rubber percussion hammer. To properly obtain a reflex, a
crisp blow must be delivered to quickly stretch the tendon. A heavy,
high-quality reflex hammer is immensely helpful for this task. Proper
technique is much more difficult to describe than to demonstrate. The
hammer strike should be quick, direct, crisp, and forceful, but no
greater than necessary. The most effective blow is delivered quickly
with a flick of the wrist, holding the handle of the hammer near its
end and letting it spin through loosely held fingertips. Putting the
index finger on top of the handle and using primarily elbow motion,
common faults, make it much harder to achieve adequate velocity at the
hammer head. Another common mistake is “pecking”: striking the tendon
with a timid, decelerating blow, pulling back at the last instant.
positioned. It may help relaxation to divert the patient’s attention
with light conversation. Sometimes, as in the ankle reflex, positioning
includes passively stretching the muscle slightly. An adequate stimulus
must be delivered to the proper spot. Reinforcement methods are
necessary if the reflex is not obtainable in the usual way. The part of
the body to be tested should be in an optimal position for the
response, usually about midway in the range of motion of the muscle to
be tested. In order to compare the reflexes on the two sides of the
body, the position of the extremities should be symmetric. During the
reflex examination, the patient should keep the head straight, since
looking to one side may alter reflex tone, especially in the arms
(tonic neck reflex). The DTRs may be influenced to some degree by
voluntary mental effort. Merely by concentrating some individuals are
able to somehow alter reflex excitability. Mentally induced reflex
asymmetry is possible and may be clinically relevant in some cases.
|
TABLE 28.1 The Commonly Elicited Deep Tendon (Muscle Stretch) Reflexes
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Placing one hand over the muscle is often useful, especially when
responses are sluggish. A reflex quadriceps contraction can sometimes
be felt even when insufficient to produce visible contraction or knee
movement. The activity of a reflex is judged by the speed and vigor of
the response, the range of movement, and the duration of the
contraction. An absent reflex often makes a dull, thudding sound when
the tendon is struck.
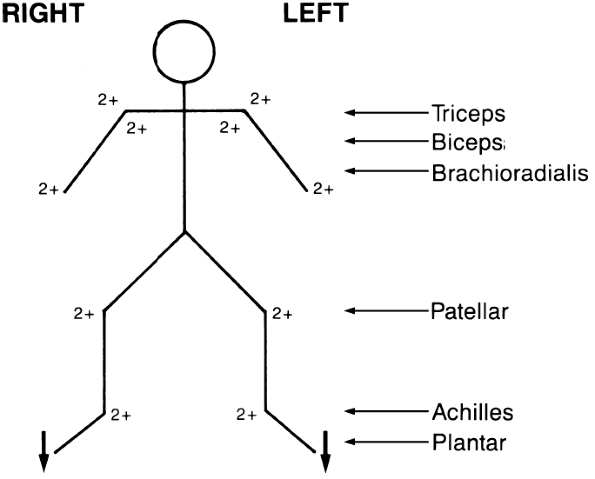
brachioradialis, knee (quadriceps), and ankle (Achilles) tendon
reflexes. Table 28.1 summarizes the reflex
levels. Reflexes may be graded as absent, sluggish or diminished,
normal, exaggerated, and markedly hyperactive. For the purposes of
clinical note taking, most neurologists grade the DTRs numerically, as
follows: 0 = absent; 1 + (or +) = present but diminished; 2+ (or + +) =
normal; 3+ (or + + +) = increased but not necessarily to a pathologic
degree; and 4+ (or + + + +) = markedly hyperactive, pathologic, often
with extra beats or accompanying sustained clonus. The “+” after the
number is more traditional than informative, and is sometimes omitted.
Signs are sometimes used to indicate subtle asymmetry, but generally a
grade of 2 means the same as 2+. Another level, trace (or +/-), is
frequently added to refer to a reflex, most often an ankle jerk, that
appears absent to routine testing but can be elicited with
reinforcement. Some add a grade of 5 + for the patient with extreme
spasticity and clonus. In the 0 to 4 scale, level 1 + DTRs are still
normal but somewhat sluggish and difficult to elicit, hypoactive but in
the examiner’s opinion not pathologic. Grade 3+ reflexes are “fast
normal,” quicker than 2+, sometimes very quick, but not accompanied by
any other signs of upper motor neuron pathology such as increased tone,
upgoing toes, or sustained clonus. Normality of the superficial
reflexes, normal lower-extremity tone, and downgoing toes are
reassuring evidence of fast normal rather than pathologically quick
reflexes. Some use 3+ to indicate the presence of spread or unsustained
clonus, with all other normal reflexes, even very fast ones, labeled as
2+. Grade 4+ reflexes are unequivocally pathological. The speed of the
response is very fast, the threshold low, the reflexogenic zone wide,
and there are accompanying signs of corticospinal tract dysfunction.
Other scales are in use, but not widely. Reflexes may be charted in
several ways, for example, as shown in Table 28.2, or as in Figure 28.1.
muscles that have not been directly stretched, even in normal patients.
The response may involve adjacent or even contralateral muscles, and
the contraction of one muscle may be accompanied by contraction of
other muscles. This is referred to as spread, or irradiation, of
reflexes. It is normal for percussion of the brachioradialis tendon to
also cause slight finger flexion. In the presence of spasticity and
hyperreflexia, contraction of the biceps or brachioradialis may be
accompanied by pronounced flexion of the fingers and adduction of the
thumb. Extension of the knee may be accompanied by adduction of the
hip, or there may be bilateral knee extension. Judging how much spread
is still within normal limits can be difficult. Under some
circumstances, the expected response to percussion of a tendon is
absent, but muscles innervated by adjacent spinal cord segments
contract instead (e.g., inverted brachioradialis reflex). On other
occasions, a reflex is absent and percussion of the tendon causes an
inverted or
paradoxical
contraction, e.g., elbow flexion on attempted elicitation of the
triceps reflex (see Inverted and Perverted Reflexes further on).
|
TABLE 28.2 Method of Recording the Commonly Tested Deep Tendon (Muscle Stretch) Reflexes
|
||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||
even apparently absent, although there is no other evidence of nervous
system disease. Under such circumstances, reinforcement techniques are
often useful. Reflex reinforcement probably involves supraspinal,
fusimotor, and longloop mechanisms. A reflex can be reinforced or
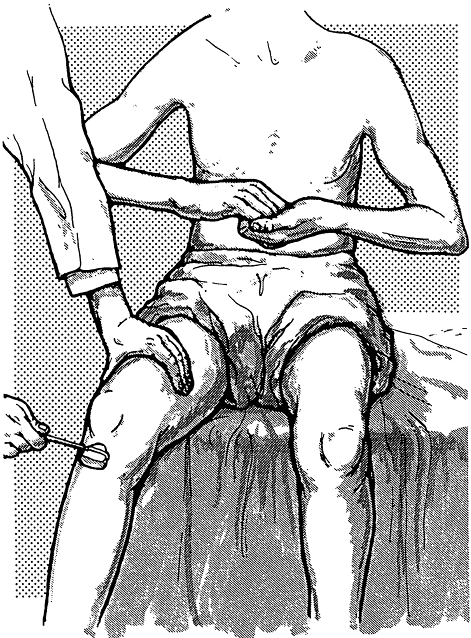
brought out using several methods. In the Jendrassik maneuver, the
patient attempts to pull the hands apart with the fingers flexed and
hooked together, palms facing, as the tendon is percussed (Figure 28.2).
The effect is very brief, lasting only 1 to 6 seconds, and is maximal
for only 300 milliseconds. The Jendrassik maneuver is obviously only
useful for lower-extremity reflexes. Other techniques include having
the patient clench one or both fists, firmly grasp the arm of the
chair, side of the bed, or the arm of the examiner. Reinforcement may
also be carried out by having the patient look at the ceiling, grit the
teeth, cough, squeeze the knees together, take a deep breath, count,
read aloud, or repeat verses at the time
the
reflex is being tested. A sudden loud noise, a painful stimulus
elsewhere on the body—such as the pulling of a hair or a bright light
flashed in the eyes—may also be a means of reinforcement.
 |
|
FIGURE 28.1 • Alternate method of recording the commonly tested muscle stretch reflexes. For grading, see text and Table 28.2.
|
 |
|
FIGURE 28.2 • Method of reinforcing the patellar reflex.
|
reflex reinforcement. A slight increase in tension of the muscle being
tested may reinforce the reflex response. A simple and effective method
to reinforce a knee or ankle jerk is to have the patient maintain a
slight, steady contraction of the muscle whose tendon is being tested
(e.g., slight plantar flexion by pushing the ball of the foot against
the floor or the examiner’s hand to reinforce the ankle jerk). The
patient may tense the quadriceps by extending the knee slightly against
resistance as the knee jerk is being elicited. Reinforcement may
increase the amplitude of a sluggish reflex or bring out a latent
reflex not otherwise obtainable. Reflexes that are normal on
reinforcement, even though not present without reinforcement, may be
considered normal. Slight muscle contraction due to inability to relax
may be one reason for the slightly hyperactive reflexes often seen in
patients who are tense or anxious.
Under most circumstances, weakness accompanied by hyporeflexia is of
lower motor neuron origin, and weakness accompanied by hyperreflexia of
upper motor neuron origin. The presence of pathologic reflexes and
abnormalities of associated movements are also helpful in the
differential diagnosis (Table 28.3).
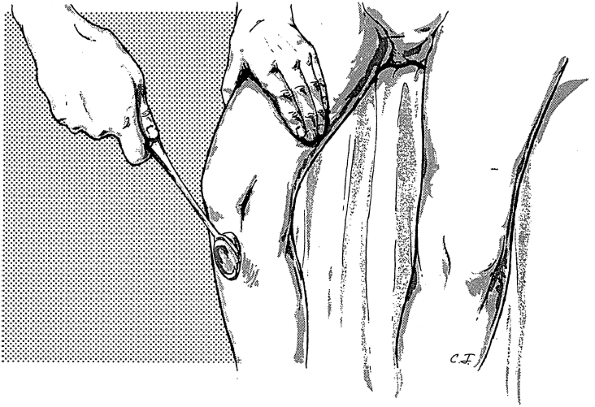
and midway between flexion and extension, the examiner places the
palmar surface of her extended thumb or finger on the patient’s biceps
tendon, and then strikes the extensor surface with the reflex hammer (Figure 28.3).
Pressure on the tendon should be light; too much pressure exerted with
the thumb or finger against the tendon makes the reflex much harder to
obtain. The hands may lie in the patient’s lap, or the examiner
may
hold the patient’s arm with the elbow resting in her hand. The major
response is a contraction of the biceps muscle with flexion of the
elbow. Since the biceps is also a supinator, there is often a certain
amount of supination. If the reflex is exaggerated, the reflexogenic
zone is increased and the reflex may even be obtained by tapping the
clavicle; there may be abnormal spread with accompanying flexion of the
wrist and fingers and adduction of the thumb.
|
TABLE 28.3 Reflex Patterns with Different Neurologic Disorders
|
||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
FIGURE 28.3 • Method of obtaining the biceps reflex.
|
 |
|
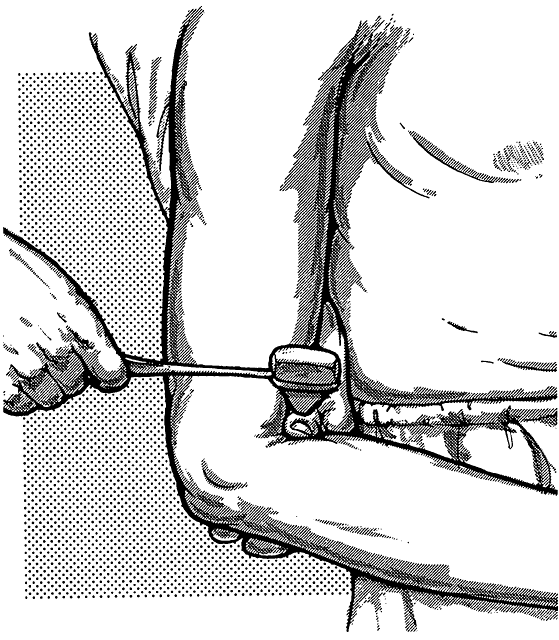
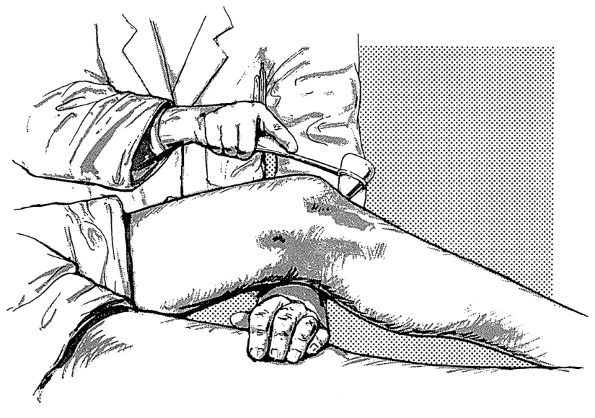
FIGURE 28.4 • Method of obtaining the triceps reflex.
|
just above its insertion on the olecranon process of the ulna. The arm
is placed midway between flexion and extension, and may be rested in
the patient’s lap, on her thigh or hip, or on the examiner’s hand (Figure 28.4).
The response is contraction of the triceps muscle with extension of the
elbow. The most common error in eliciting the triceps jerk is simply
too timorous a blow.
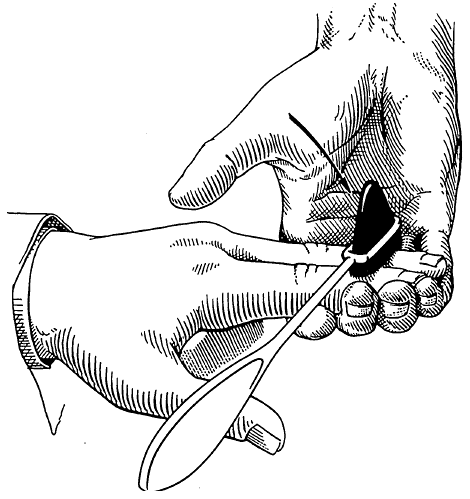
with the forearm in semiflexion and semipronation causes flexion of the
elbow, with variable supination (Figure 28.5). The supination is
more marked with the forearm extended and pronated, but there is less
flexion. The principal muscle involved is the brachioradialis. The
tendon can be percussed not only at its insertion on the lateral aspect
of the base of the styloid process of the radius, but also at about the
junction of the middle and distal thirds of the forearm or at its
tendon of origin above the lateral epicondyle of the humerus. The most
common error is hitting the muscle belly rather than the tendon. The
muscle becomes tendinous at about midforearm. A local contraction can
be elicited from any muscle by directly striking the muscle belly. The
point in eliciting a DTR is to lengthen the muscle by stretching its
tendon. An idiomuscular contraction can be obtained by striking the
brachioradialis muscle belly in the proximal third of the forearm; this
is not a DTR. If the reflex is exaggerated, there is associated flexion
of the wrist and fingers, with adduction of the forearm. When the
afferent limb of the reflex is impaired, there may be a twitch of the
flexors of the hand and fingers without flexion and supination of the
elbow; this is termed inversion of the reflex.
 |
|
FIGURE 28.5 • Method of obtaining the brachioradialis reflex.
|
 |
|
FIGURE 28.6 • Method of obtaining the finger flexor reflex.
|
is in supination, resting on a table or a solid surface, with the
fingers slightly flexed. The examiner places her fingers against the
patient’s fingers, and taps the backs of her own fingers lightly with
the reflex hammer (Figure 28.6). The response
is flexion of the patient’s fingers and the distal phalanx of the
thumb. The reflex may be reinforced by having the patient flex her
fingers slightly as the blow is delivered. An alternate technique is
for the patient to hold the hand in the air, palm down, the examiner
touching fingers with palm up, with the blow delivered in an upward
direction from below.
femoris muscle, with resulting extension of the knee, in response to
percussion of the patellar tendon. A firm tap on the tendon draws the
patella down, stretching the quadriceps, provoking reflex contraction.
If the reflex is brisk, the contraction is strong and the amplitude of
the movement is large. If the examiner places one hand over the muscle,
and with the other hand taps the patellar tendon just below the
patella, she can palpate the contraction as well as observe the
rapidity and range of response. Palpation helps in judging the latency
between the time of the stimulus and the resulting response. The knee
jerk can be elicited in various ways.
The
patient may sit in a chair with the knees slightly extended and the
heels resting on the floor, or sit on an examination table with the
legs dangling (Figure 28.7).
If the patient is lying in bed, the examiner should partially flex the
knee by placing one hand beneath it and then tap the tendon (Figure 28.8).
 |
|
FIGURE 28.7 • Method of obtaining the patellar (quadriceps) reflex with the patient seated.
|
accompanied by adduction of the hip, which on occasion is bilateral, or
there may be bilateral knee extension. If the reflex is exaggerated,
the response may be obtained not only by tapping the tendon in the
usual spot, but also just above the patella (suprapatellar or
epipatellar reflex); the tendon can be tapped directly, or, with the
patient recumbent, the examiner can place her index finger on the upper
border of the patella and tap the finger to push down the patella.
Contraction of the quadriceps causes a brisk upward movement of the
tendon, together with extension of the leg (Figure 28.9). Marked exaggeration of the patellar reflex may be accompanied by patellar clonus.
 |
|
FIGURE 28.8 • Method of obtaining the patellar (quadriceps) reflex with the patient recumbent.
|
 |
|
FIGURE 28.9 • Method of obtaining the suprapatellar reflex.
|
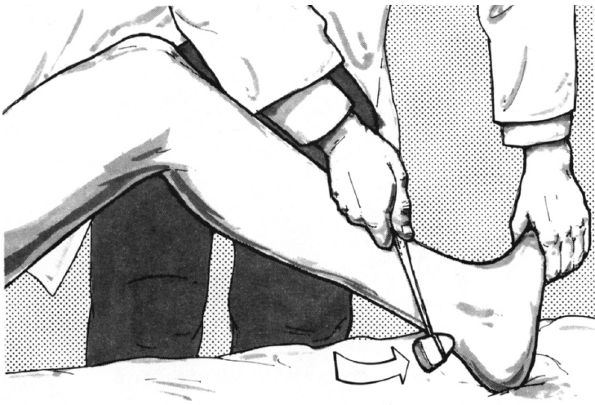
tendon just above its insertion on the calcaneus. The resulting
contraction of the posterior crural muscles, the gastrocnemius, soleus,
and plantaris, causes plantar flexion of the foot at the ankle. If the
patient is seated or lying in bed, the thigh should be held in moderate
abduction and external rotation and the knee flexed. If the patient is
supine, access to the tendon requires placing the legs into a frog-leg
position with the knees apart and the ankles close together. Some
prefer to have the patient cross the leg to be examined atop the other
shin or ankle (“figure four position,” as the legs form a 4). The
examiner should place one hand under the foot and pull upward slightly
to passively dorsiflex the ankle to about a right angle (Figure 28.10). The Achilles reflex is mediated by the tibial nerve (S1).
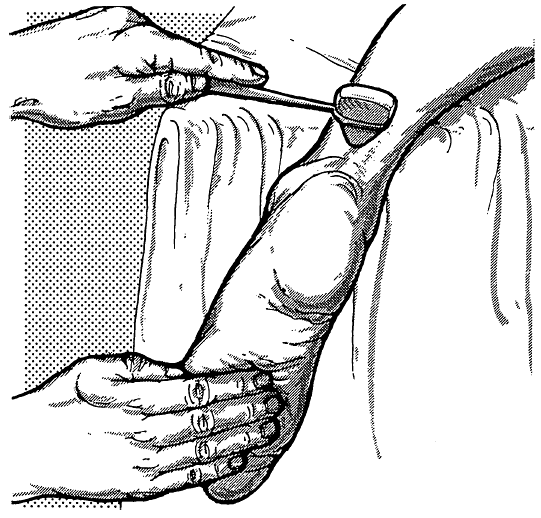
master. There are two critical variables: proper stretch and efficient
striking. Of the two, proper stretch is the more difficult to learn. If
the reflex is difficult to obtain, the patient may be asked to press
her foot lightly against the examiner’s hand in order to tense the
muscle and reinforce the reflex. Using a driving analogy and asking the
patient to imagine pressing on an accelerator enough to go “17 mph”
communicates the need for
a
low-level but precisely graded contraction, which is then easy to
adjust up or down to the proper level. The reflex may also be elicited
by having the patient kneel on a chair or similar surface, with the
feet projecting at right angles; the Achilles tendons are percussed
while the patient is in this position (Figure 28.11).
This method is particularly useful for comparing reflex activity on the
two sides. Another method for supine examination is to strike the ball
(sole) of the foot, or strike the examiner’s hand placed flat against
the sole. This plantar stretch reflex is considered equivalent to the
ankle jerk for clinical purposes. Although the Achilles reflex, when
carefully elicited, should be present in normal individuals, it tends
to diminish with age and its bilateral absence in elderly individuals
is not necessarily of clinical significance.
 |
|
FIGURE 28.10 • Method of obtaining the Achilles (triceps surae) reflex with the patient recumbent.
|
 |
|
FIGURE 28.11 • Method of obtaining the Achilles (triceps surae) reflex with the patient kneeling.
|
under most circumstances, and using good technique, these are
elicitable in every normal person. One or more of these reflexes may be
absent in occasional individuals with no other evidence of disease of
the nervous system. They are present even in the majority of premature
infants. The activity of a DTR is judged by the latency, speed, vigor,
and duration of contraction, and the range of movement. Of these, the
latent period between the time the stimulus is applied and the time the
response occurs is most important for clinical evaluation of disease
states.
hypoactive, the response varies from diminished or sluggish to complete
absence of the reflex. Hyperactive reflexes are characterized by
varying degrees of decreased latency, increased speed and vigor of
response, increased range of movement, decrease in threshold, extension
of the reflexogenic zone, and prolongation of the muscular contraction.
Table 28.3 summarizes the patterns of reflex responses seen with lesions at various sites.
Clearly hyperactive or hypoactive reflexes speak for themselves. But a
reflex that is normal in absolute terms may be judged abnormal in
comparison to the patient’s other reflexes. The reflexes should be
compared on the two sides of the body, the arms to the legs, and the
knees to the ankles. The DTRs are normally symmetric, and reflexes
otherwise normal may be abnormal if different from expected. For
example, a 1 + biceps jerk in a patient with suspected cervical
radiculopathy, while “normal,” may be judged abnormal if the
opposite
biceps jerk is 2+. The DTRs are usually comparable in the upper and
lower extremities. Slight differences are permissible but a pronounced
difference may be significant (e.g., in thoracic myelopathy the DTRs in
the legs may be much brisker than in the arms, even though not clearly
pathologic). A proximal to distal gradient may also be significant.
Symmetric 1+ ankle jerks when all of the other reflexes are 2+ may
signal mild peripheral neuropathy. When asymmetry is the main finding,
it is sometimes difficult to tell whether one side is increased or the
other side decreased.
 |
|
FIGURE 28.12 • Method of obtaining the biceps femoris reflex.
|
response and/or a diminution in the range of response. An increase in
stimulus intensity may be necessary to elicit the reflex, or repeated
blows may be necessary, for a single stimulus may be subliminal. A DTR
is absent if it is not obtained even with reinforcement. A depressed or
absent reflex results from dysfunction of some component of the reflex
arc. Interference with the afferent limb may be caused by lesions
involving the sensory nerve, posterior root, dorsal root ganglion, or
intramedullary pathways between the dorsal root entry zone and the
anterior horn (e.g., syringomyelia). Abnormalities of the motor unit
and final common pathway that make up the efferent limb of the reflex
arc occur in many conditions, but particularly with radiculopathy and
peripheral nerve lesions. In neurogenic processes, DTRs are lost out of
proportion to atrophy and weakness. With a peripheral nerve lesion, a
reflex may not return until much of the motor function has recovered.
Sometimes there is persistent areflexia following lesions of the nerve
root or peripheral nerve, even after complete return of both motor and
sensory functions.
a decrease in reflex threshold; a decrease in the latency, the time
between tendon percussion and the reflex contraction; an exaggeration
of the power and range of movement; prolongation of the reflex
contraction; extension of the reflexogenic zone (or zone of
provocation); and spread of the reflex response. When the reflex
threshold is decreased, a minimal stimulus may evoke the reflex, and
reflexes that are not normally obtained may be elicited with ease. Very
hyperactive DTRs may sometimes be elicited with extremely slight
percussion. Another manifestation of decreased reflex threshold may be
a widening of the area from
which
the reflex may be elicited, and application of the stimulus to sites at
some distance from the usual one may evoke the response; the patellar
reflex may be elicited by tapping the tibia or dorsum of the foot, and
the biceps and other arm reflexes by tapping the clavicle or scapula.
There may also be abnormal spread of the response. One stimulus may
provoke repetitive responses and sometimes elicit sustained clonus.
corticospinal or pyramidal system. Spasticity and hyperreflexia are
likely related to involvement of a variety of structures in the
descending motor pathways at cortical, subcortical, midbrain, and
brainstem levels. Hyperreflexia results from a lowering of the reflex
threshold due to increased excitability of the lower motor neuron pool
related to dysfunction of some or all of these structures. A lesion at
any level of the corticospinal system or other related upper motor
neuron components, from the motor cortex to just above the segment of
origin of a reflex arc, will be accompanied by spasticity and
hyperreflexia. The characteristic posture in hemiplegia is flexion of
the upper extremities, with more marked weakness of the extensors; and
extension of the lower extremities, with more marked weakness of the
flexors. Consequently, the flexor reflexes are exaggerated to a greater
degree in the upper extremities, and the extensor reflexes in the
lower. The reflexes may be present in spinal cord lesions in spite of
the absence of sensation.
The reflexes vary in these conditions; they may be normal, or they may
be decreased owing to voluntary or involuntary tension of the
antagonistic muscle, but they are most frequently increased.
Hyperactivity may be marked, but it is an exaggeration not in the speed
of the response but in the excursion or range of response. The foot may
be kicked far into the air and held extended for a time after the
patellar tendon is tapped, but the contraction and relaxation takes
place at a normal rate. There is often a bilateral response with
extraneous and superfluous jerking of remote parts, including whole
body jerks, when a reflex is tested. There is no increase in the
reflexogenic zone in psychogenic lesions, and although there may be
irregular repeated jerky movements (spurious clonus), no true clonus is
present. Furthermore, there are no other signs of organic disease of
the corticospinal system.
and pendular: Eliciting the patellar reflex while the foot is hanging
free may elicit a series of to-and-fro pendular movements of the foot
and leg before the limb finally comes to rest.
results. In the presence of hyperreflexia, there may be spread to other
muscles, as in the crossed adductor response. Inverted or paradoxical
reflexes are contractions the opposite of those expected. With an
inverted triceps or patellar reflex there is elbow or knee flexion
instead of extension. Under these circumstances, the segmental reflex
is absent, but there is an underlying hyperreflexia lowering the
threshold for activation of the antagonist muscle, perhaps because of
transmitted vibration. Degenerative spine disease with
radiculomyelopathy is the usual mechanism. An inverted brachioradialis
(often referred to as an inverted radial periosteal) reflex does not
result in true inversion (i.e., elbow extension), but instead produces
a perverted response with finger flexion. When the brachioradialis
reflex is present this finger flexion is simply referred to as spread;
when the brachioradialis reflex is absent and the only response is
finger flexion, the reflex is commonly said to be inverted.
